Occupational Hazard in Operating Theater Wear shoes designed

- Slides: 33
Occupational Hazard in Operating Theater
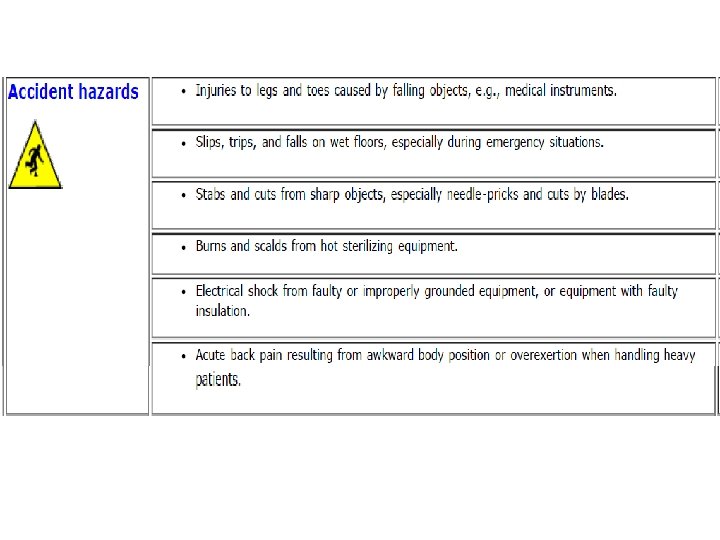
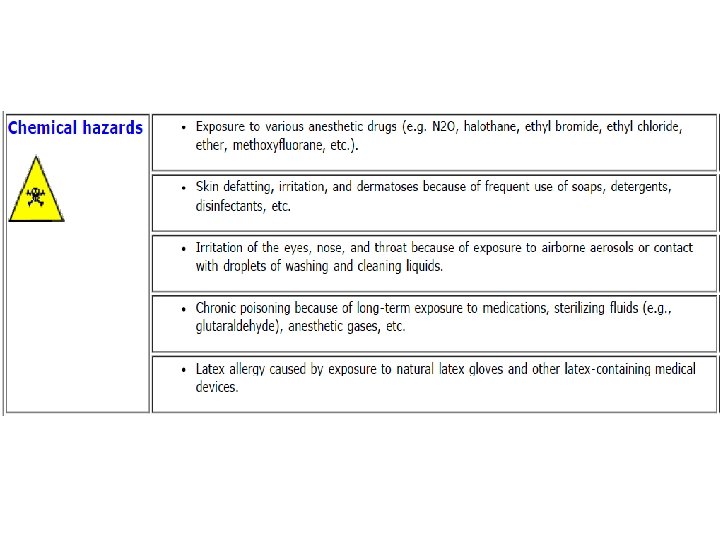
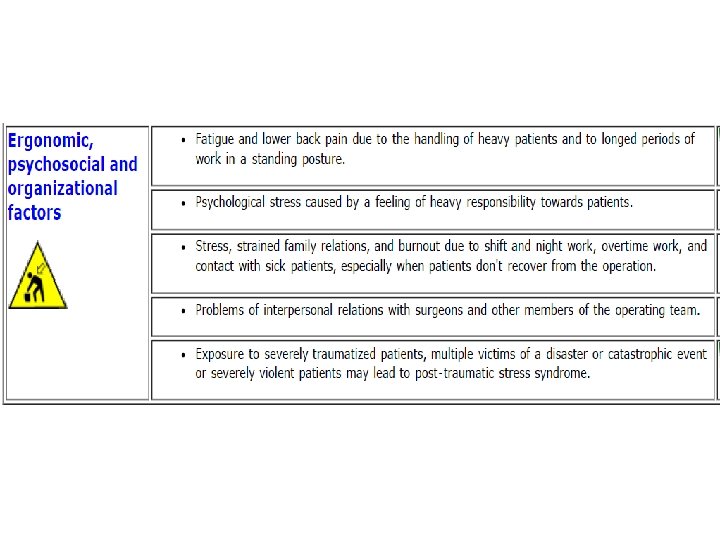
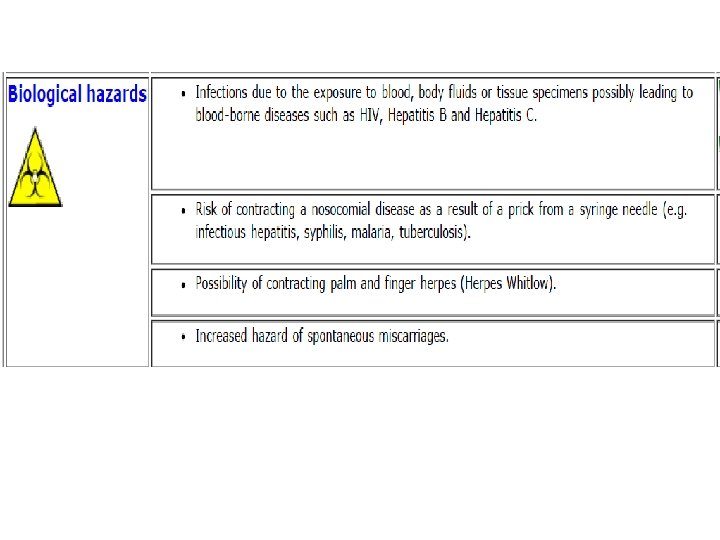
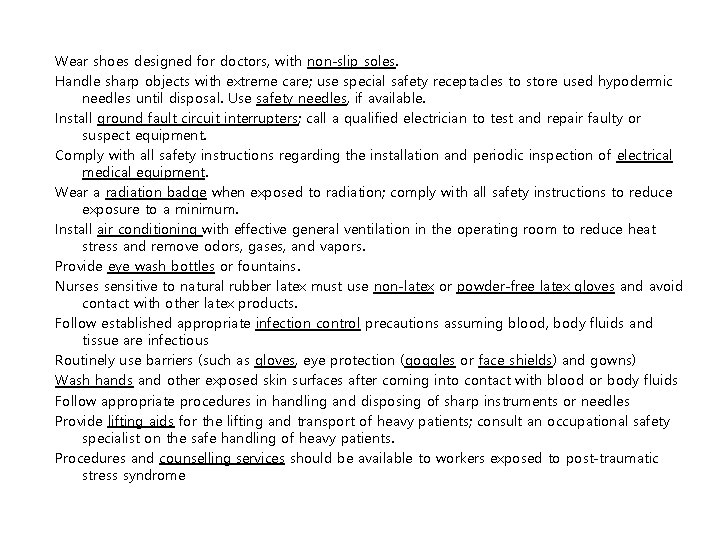
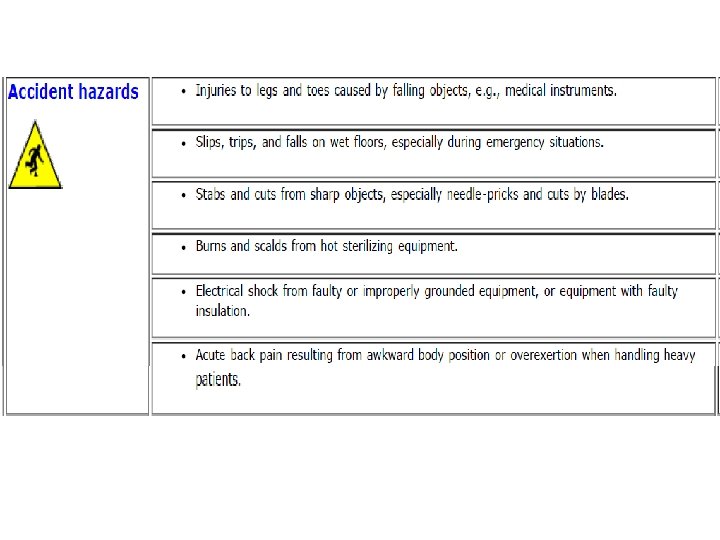
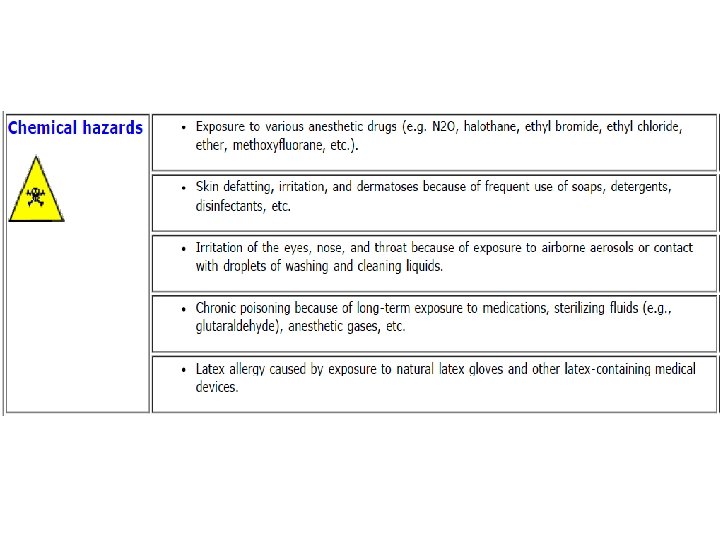
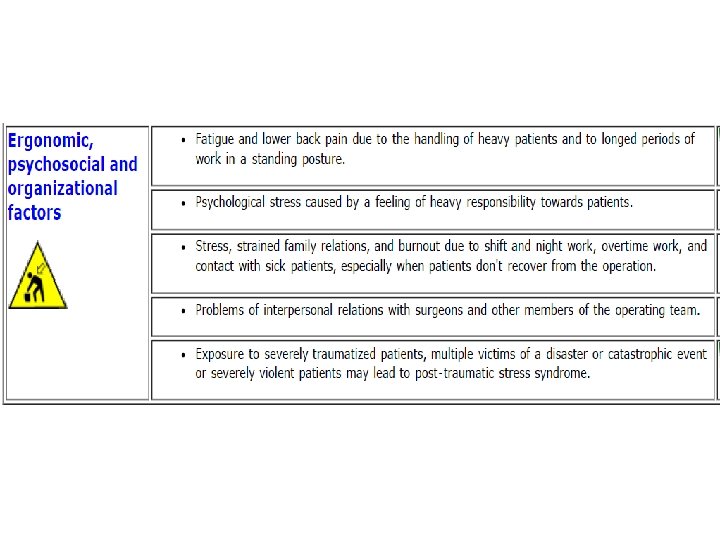
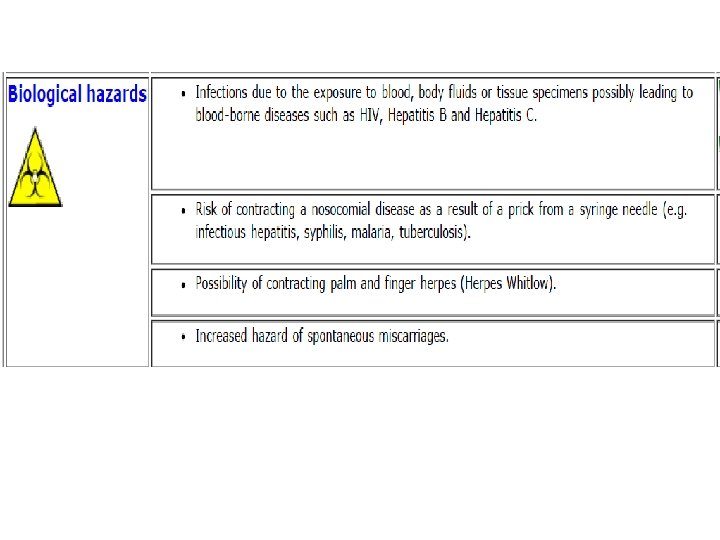
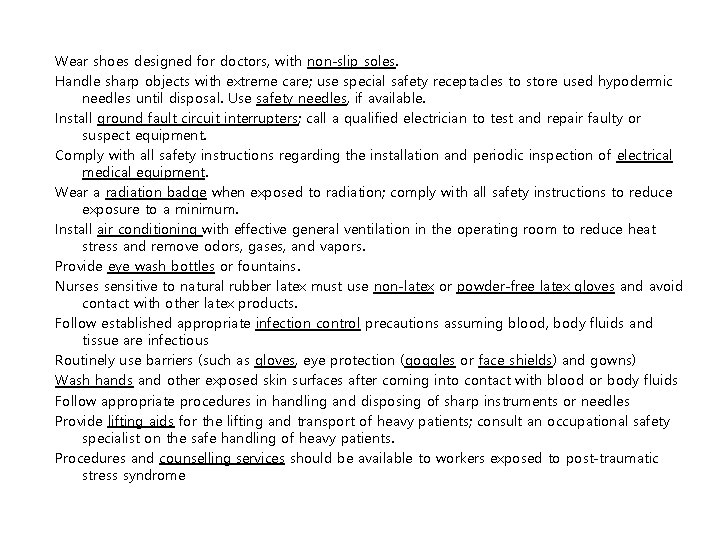
Wear shoes designed for doctors, with non-slip soles. Handle sharp objects with extreme care; use special safety receptacles to store used hypodermic needles until disposal. Use safety needles, if available. Install ground fault circuit interrupters; call a qualified electrician to test and repair faulty or suspect equipment. Comply with all safety instructions regarding the installation and periodic inspection of electrical medical equipment. Wear a radiation badge when exposed to radiation; comply with all safety instructions to reduce exposure to a minimum. Install air conditioning with effective general ventilation in the operating room to reduce heat stress and remove odors, gases, and vapors. Provide eye wash bottles or fountains. Nurses sensitive to natural rubber latex must use non-latex or powder-free latex gloves and avoid contact with other latex products. Follow established appropriate infection control precautions assuming blood, body fluids and tissue are infectious Routinely use barriers (such as gloves, eye protection (goggles or face shields) and gowns) Wash hands and other exposed skin surfaces after coming into contact with blood or body fluids Follow appropriate procedures in handling and disposing of sharp instruments or needles Provide lifting aids for the lifting and transport of heavy patients; consult an occupational safety specialist on the safe handling of heavy patients. Procedures and counselling services should be available to workers exposed to post-traumatic stress syndrome
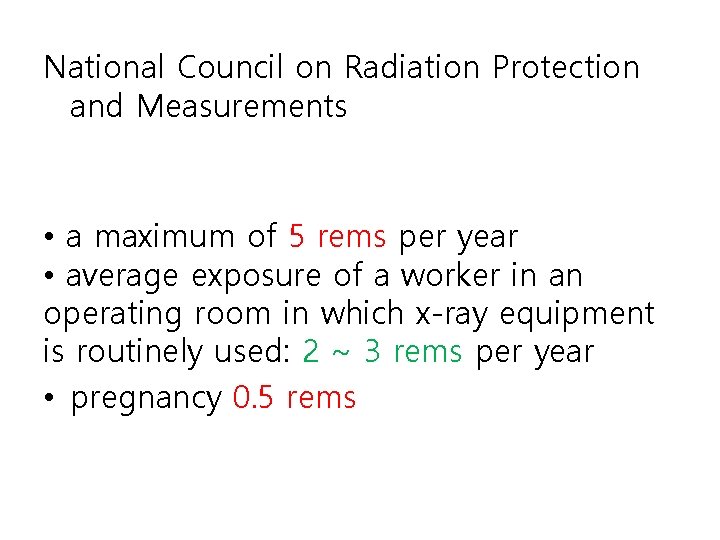
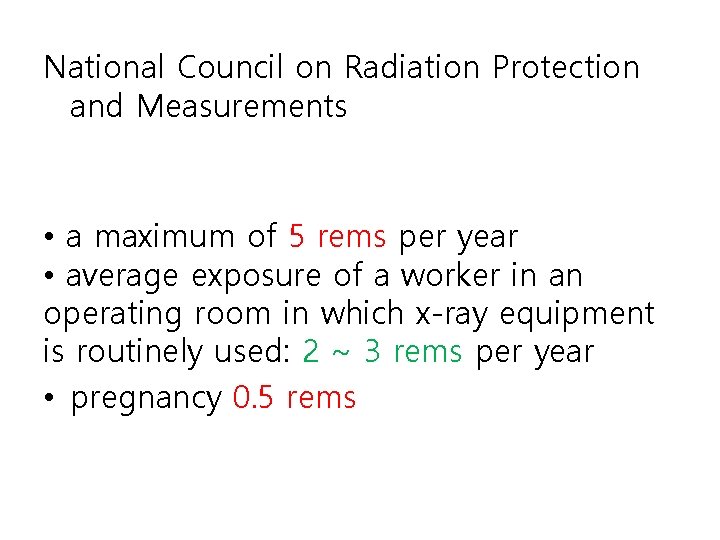
National Council on Radiation Protection and Measurements • a maximum of 5 rems per year • average exposure of a worker in an operating room in which x-ray equipment is routinely used: 2 ~ 3 rems per year • pregnancy 0. 5 rems
Latex allergy • 13 latex proteins (Hev b) are known to be potent allergens: – Elicit human Ig. E antibody – Leading to sensitization in exposed individuals – Allergic reactions upon subsequent exposure • Hevea indicator allergens – Hev b 1 (rubber elongation factor) and Hev b 3 (prenyltransferase) - most commonly induce Ig. E antibody responses in individuals who become sensitized through direct mucosal exposure to Hevea rubber products. – Hev b 5 (acidic protein) and Hev b 6. 02 (mature hevein) released from dipped rubber products, mainly latex gloves, and transported via aerosolized powder used for glove donning, or sloughed directly into the environment. Exposure to these allergens through direct contact or inhalation occurs most frequently in occupations in which protective rubber gloves are frequently worn.
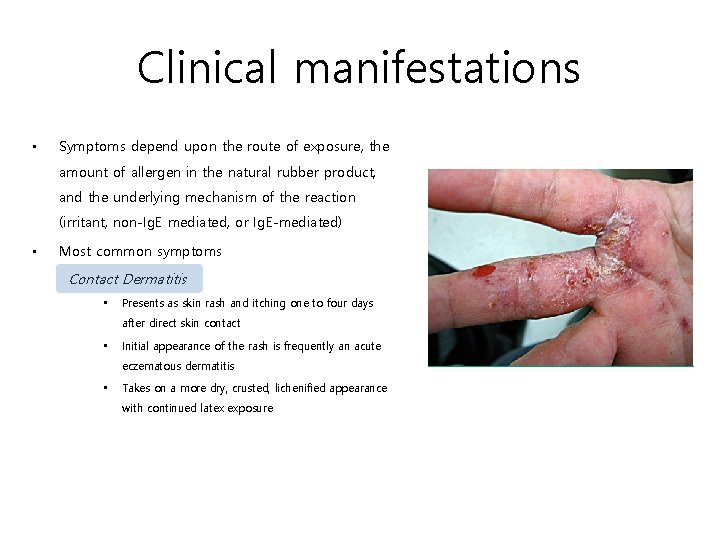
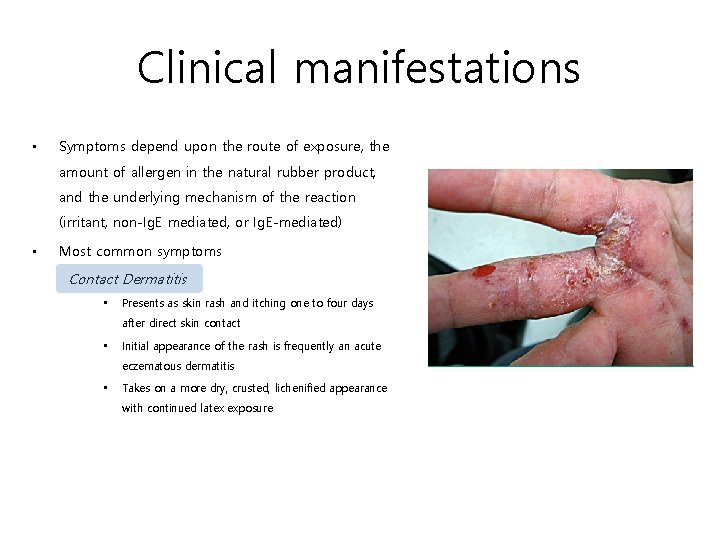
Clinical manifestations • Symptoms depend upon the route of exposure, the amount of allergen in the natural rubber product, and the underlying mechanism of the reaction (irritant, non-Ig. E mediated, or Ig. E-mediated) • Most common symptoms Contact Dermatitis • Presents as skin rash and itching one to four days after direct skin contact • Initial appearance of the rash is frequently an acute eczematous dermatitis • Takes on a more dry, crusted, lichenified appearance with continued latex exposure
Clinical Manifestations • Most common symptoms (con’t) Allergic contact urticaria • Contact urticaria is the most common allergic reaction reported by healthcare workers who use latex medical gloves • Redness, itching, and wheal and flare reactions occur at the site of rubber-skin contact within 10 to 15 minutes Rhinoconjunctivitis and asthma • Manipulation of powdered latex gloves produces an aerosol of Hevea allergens that can trigger rhinitis and asthma symptoms in latex sensitive individuals • Pre-existing asthma is not a prerequisite for the development of latex -related asthma Anaphylaxis Anaphylactic reactions have occurred after use of various latexbased products in both medical and nonmedical settings
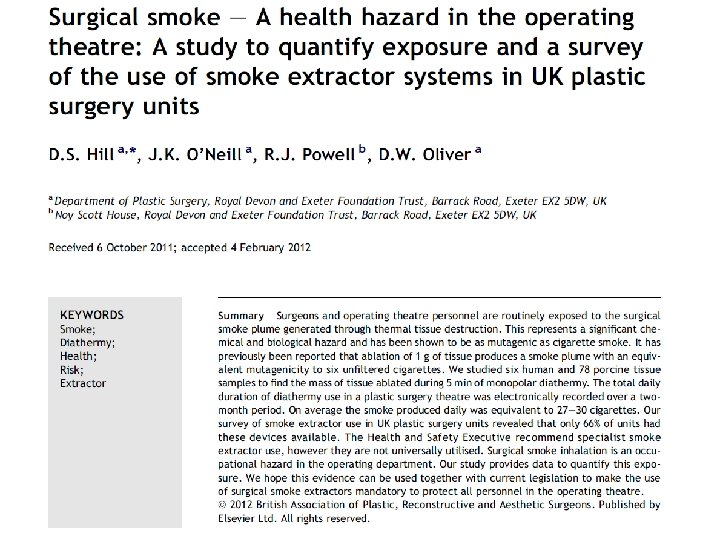
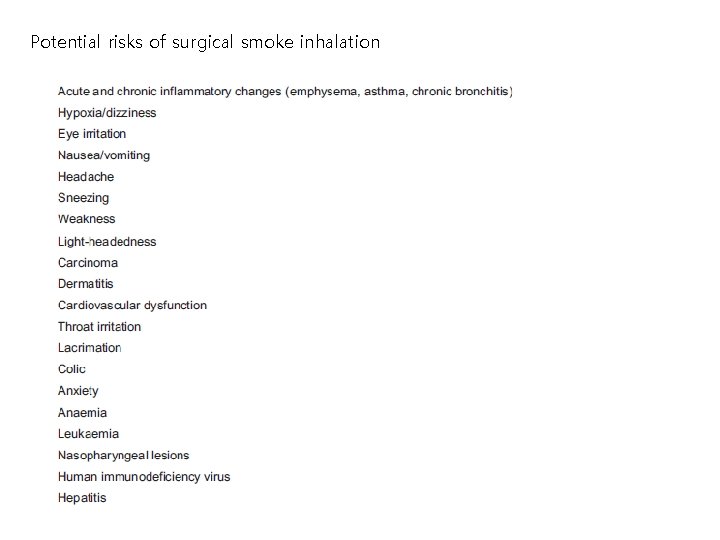
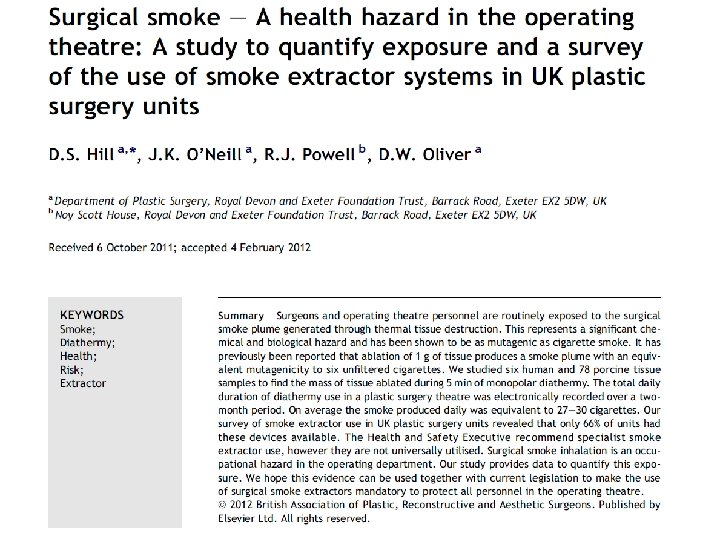
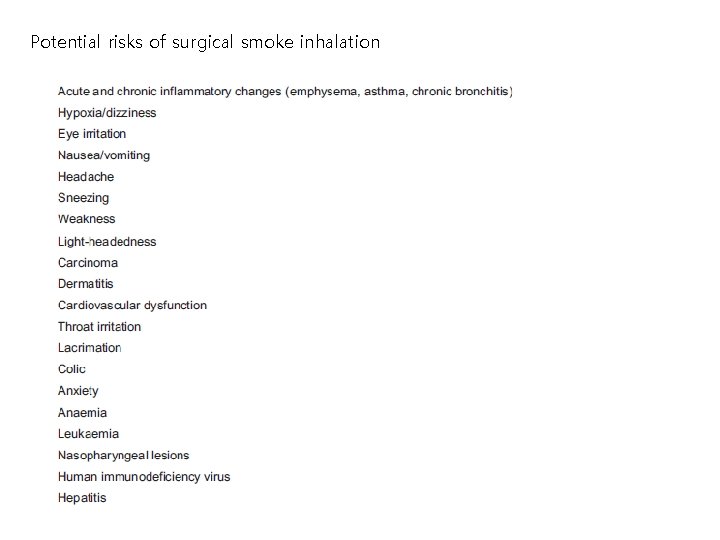
Potential risks of surgical smoke inhalation

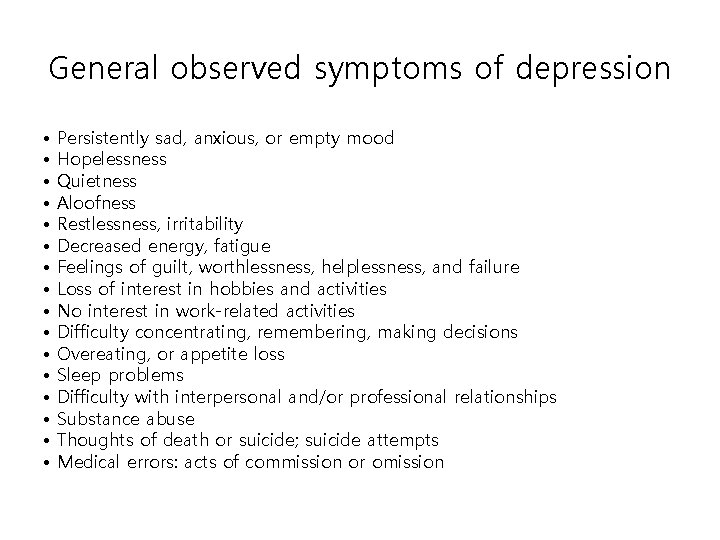
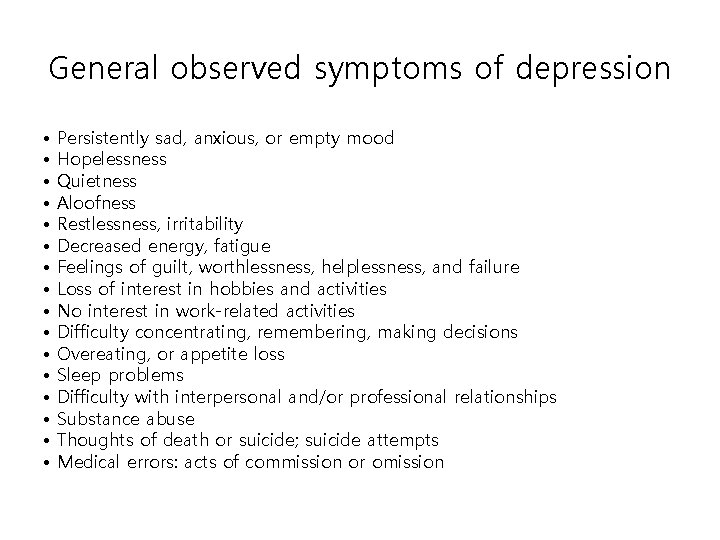
General observed symptoms of depression • • • • Persistently sad, anxious, or empty mood Hopelessness Quietness Aloofness Restlessness, irritability Decreased energy, fatigue Feelings of guilt, worthlessness, helplessness, and failure Loss of interest in hobbies and activities No interest in work-related activities Difficulty concentrating, remembering, making decisions Overeating, or appetite loss Sleep problems Difficulty with interpersonal and/or professional relationships Substance abuse Thoughts of death or suicide; suicide attempts Medical errors: acts of commission or omission
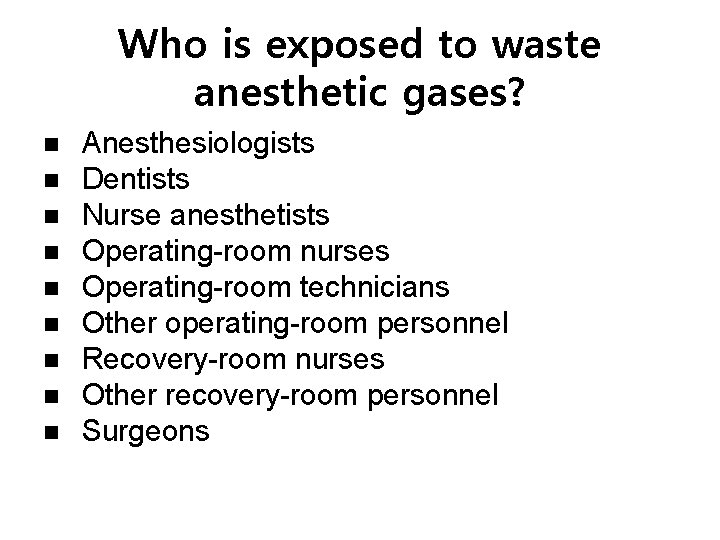
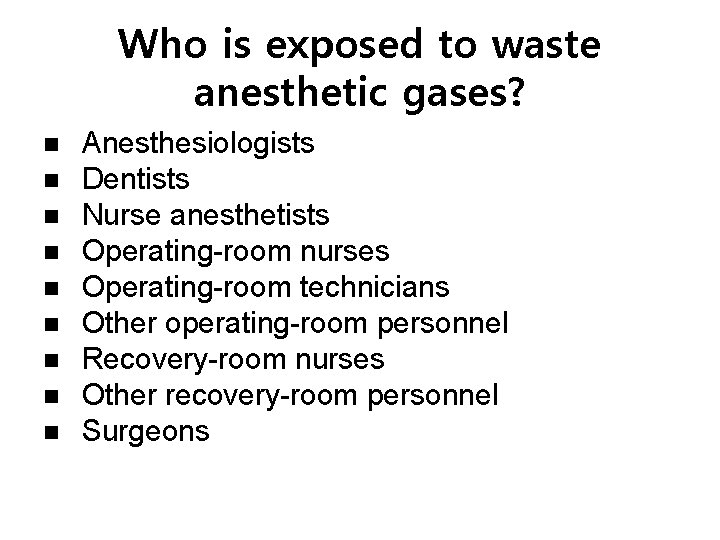
Who is exposed to waste anesthetic gases? Anesthesiologists Dentists Nurse anesthetists Operating-room nurses Operating-room technicians Other operating-room personnel Recovery-room nurses Other recovery-room personnel Surgeons
Effects of exposure to high concentrations Headache Irritability Fatigue Nausea Drowsiness Difficulties with judgment and coordination Liver and kidney disease
Effects of exposure to low concentrations • no adverse health effects • miscarriages, genetic damage, and cancer among operating-room workers • miscarriages in the spouses of exposed workers • birth defects in their offspring
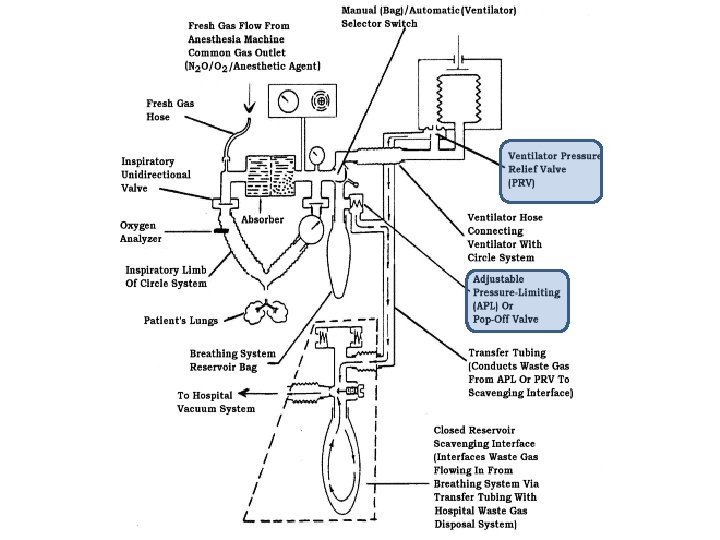
Most likely to be exposed to waste anesthetic gases • operating facilities with no automatic ventilation or scavenging systems, • operating facilities where these systems are in poor condition, • recovery rooms where gases exhaled by recovering patients are not properly vented or scavenged.
Even when scavenging and venting systems are in place • When leaks occur in the anesthetic breathing circuit (which may leak gas if the connectors, tubing, and valves are not maintained and tightly connected) • When anesthetic gases escape during hookup and disconnection of the system � • When anesthetic gas seeps over the lip of the patient’s mask or from endotracheal coupling (particularly if the mask is poorly fitted—for example, during pediatric anesthesia) • During dental operations • During induction of anesthesia
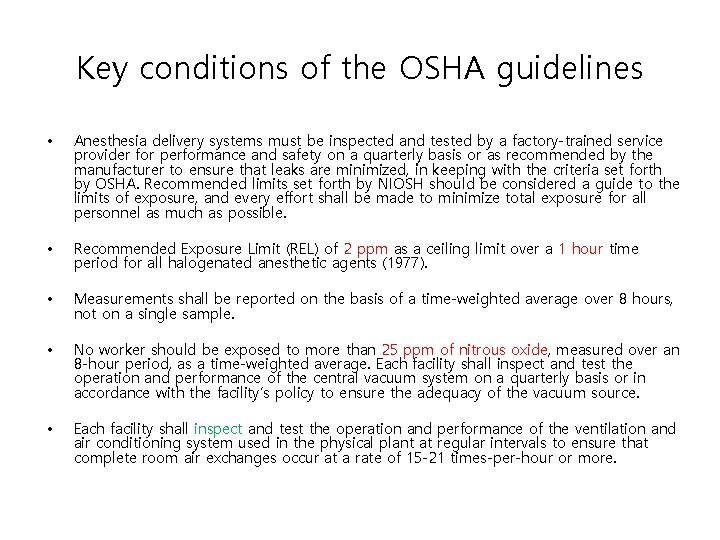
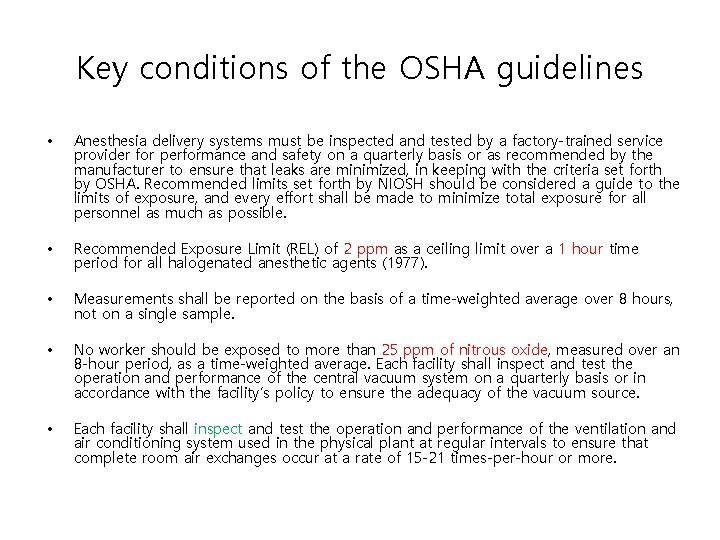
Key conditions of the OSHA guidelines • Anesthesia delivery systems must be inspected and tested by a factory-trained service provider for performance and safety on a quarterly basis or as recommended by the manufacturer to ensure that leaks are minimized, in keeping with the criteria set forth by OSHA. Recommended limits set forth by NIOSH should be considered a guide to the limits of exposure, and every effort shall be made to minimize total exposure for all personnel as much as possible. • Recommended Exposure Limit (REL) of 2 ppm as a ceiling limit over a 1 hour time period for all halogenated anesthetic agents (1977). • Measurements shall be reported on the basis of a time-weighted average over 8 hours, not on a single sample. • No worker should be exposed to more than 25 ppm of nitrous oxide, measured over an 8 -hour period, as a time-weighted average. Each facility shall inspect and test the operation and performance of the central vacuum system on a quarterly basis or in accordance with the facility’s policy to ensure the adequacy of the vacuum source. • Each facility shall inspect and test the operation and performance of the ventilation and air conditioning system used in the physical plant at regular intervals to ensure that complete room air exchanges occur at a rate of 15 -21 times-per-hour or more.
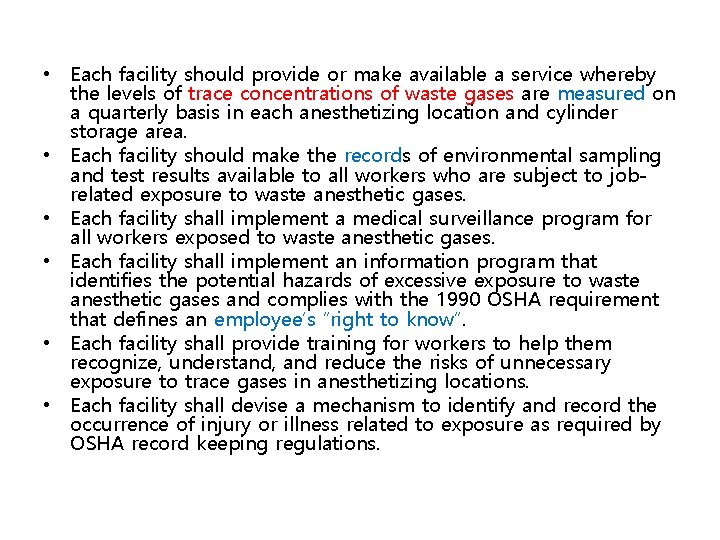
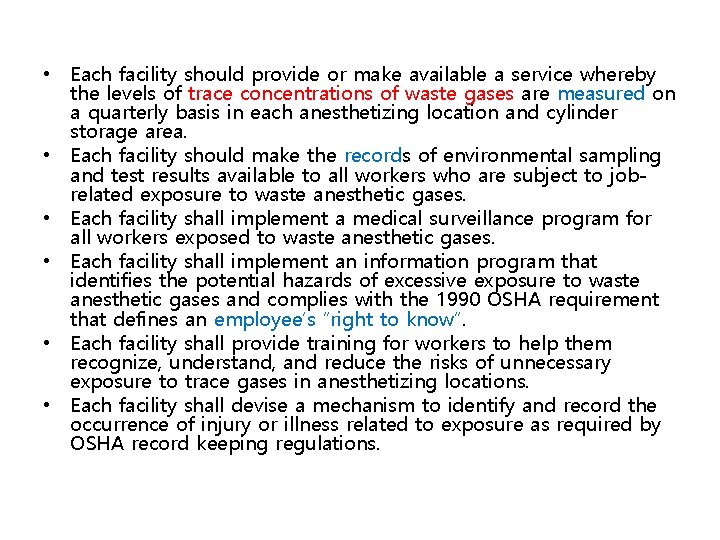
• Each facility should provide or make available a service whereby the levels of trace concentrations of waste gases are measured on a quarterly basis in each anesthetizing location and cylinder storage area. • Each facility should make the records of environmental sampling and test results available to all workers who are subject to jobrelated exposure to waste anesthetic gases. • Each facility shall implement a medical surveillance program for all workers exposed to waste anesthetic gases. • Each facility shall implement an information program that identifies the potential hazards of excessive exposure to waste anesthetic gases and complies with the 1990 OSHA requirement that defines an employee’s “right to know”. • Each facility shall provide training for workers to help them recognize, understand, and reduce the risks of unnecessary exposure to trace gases in anesthetizing locations. • Each facility shall devise a mechanism to identify and record the occurrence of injury or illness related to exposure as required by OSHA record keeping regulations.
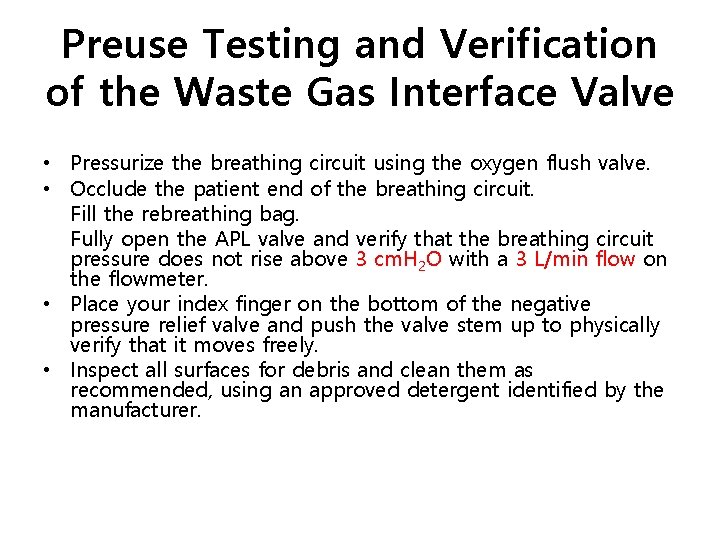
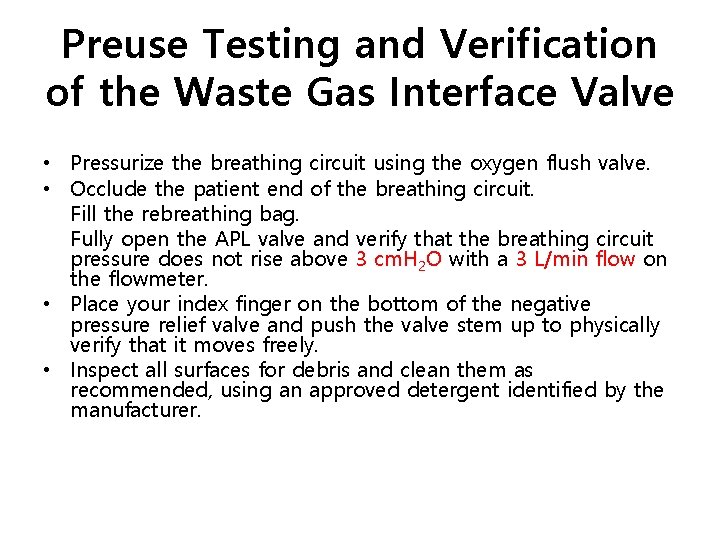
Preuse Testing and Verification of the Waste Gas Interface Valve • Pressurize the breathing circuit using the oxygen flush valve. • Occlude the patient end of the breathing circuit. Fill the rebreathing bag. Fully open the APL valve and verify that the breathing circuit pressure does not rise above 3 cm. H 2 O with a 3 L/min flow on the flowmeter. • Place your index finger on the bottom of the negative pressure relief valve and push the valve stem up to physically verify that it moves freely. • Inspect all surfaces for debris and clean them as recommended, using an approved detergent identified by the manufacturer.
• Disconnect oxygen and nitrous oxide pipeline hoses from the wall outlets and close cylinder valves at the end of the workday to reduce the levels of nitrous oxide in the ambient air and to conserve gases. • Never sniff an anesthetic agent. The odor threshold for liquid anesthetic agents has been reported to be approximately 50 ppm, which represents 25 times more than the recommended exposure limit. Intentionally inhaling an agent, even briefly, is an unnecessarily high exposure and should be avoided. • Conduct all leak tests using oxygen flow only. • Avoid turning on nitrous oxide or any halogenated agent until the face mask is securely attached to the patient’s face. • Avoid unnecessary disconnection of the breathing circuit.
• Turn off nitrous oxide and any halogenated agent, when feasible, and empty the rebreathing bag into the waste gas scavenging system before disconnecting the breathing circuit from the patient. • Administer 100% oxygen, when possible, before removing the airway maintenance device. • Avoid breathing anesthetic agents exhaled by patients as they emerge from general anesthesia. • Avoid spilling the anesthetic agent when filling calibrated vaporizers. Turn to off position when not in use. • Install key-fill models of calibrated vaporizers, where possible, on all anesthesia delivery systems. • Connect Bain Circuits and other nonrebreathing patient systems to specialized waste gas disposal adapters recommended by the manufacturer and designed for waste gas applications.
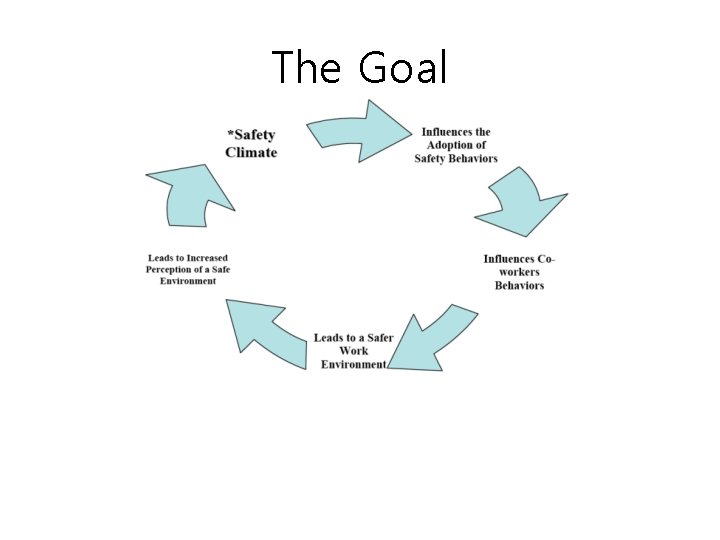
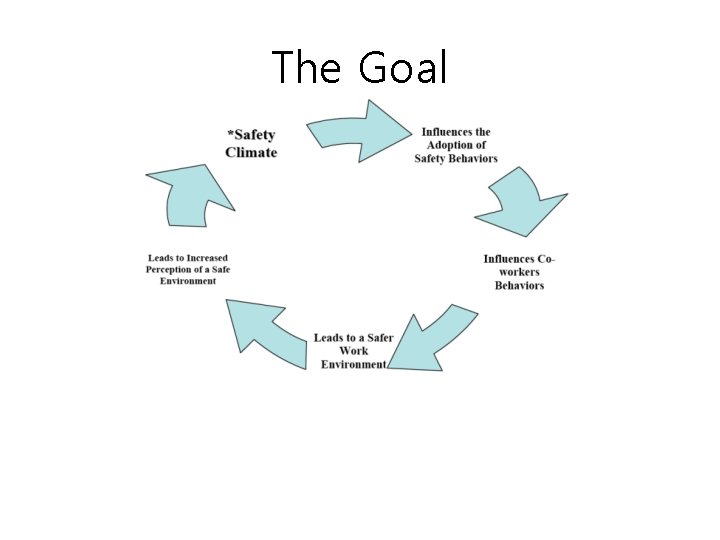
The Goal