Obstructive lung diseases 1 Emphysema Is characterized by
Obstructive lung diseases
1. Emphysema Is characterized by abnormal permanent enlargement of the airspaces distal to the terminal bronchioles, accompanied by destruction of their walls without obvious fibrosis
Types of Emphysema - - Emphysema is classified according to its anatomic distribution within the lobule The acinus is the structure distal to terminal bronchioles, and a cluster of three to five acini is called a lobule.
a. Centriacinar Emphysema - Is the most common type of emphysema - The distinctive feature of this type of emphysema is involvement of the central or proximal parts of the acini, formed by respiratory bronchioles, are affected, while distal alveoli are spared.
- This type of emphysema is most commonly seen as a consequence of cigarette smoking in people who do not have congenital deficiency of α 1 -antitrypsin
Panacinar Emphysema The acini are uniformly enlarged from the level of the respiratory bronchiole to the terminal blind alveoli Is the type of emphysema that occurs in α 1 -antitrypsin deficiency. b. - -
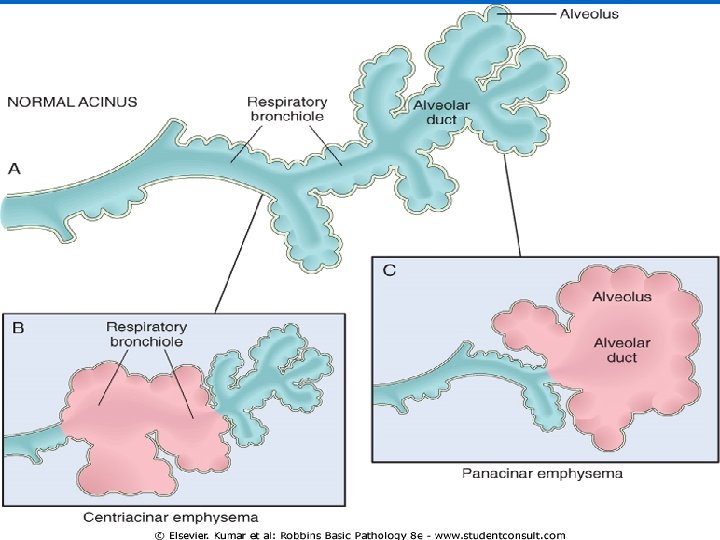
c. Distal acinar emphysema - - - In this form, the proximal portion of the acinus is normal but the distal part is primarily involved. The emphysema is more striking adjacent to the pleura, The characteristic findings are the presence of multiple, contiguous
enlarged airspaces that range in diameter from less than 0. 5 mm to more than 2. 0 cm sometimes - forming bullae This type of emphysema probably underlies many of the cases of spontaneous pneumothorax in young adults.

emphysema
Clinical Course - - Dyspnea is usually the first symptom; which is insidious and steadily progressive. The patients are too breathless to eat so weight loss is common and may be so severe as to suggest a hidden malignant tumor.
- The classic presentation in individuals who have no "bronchitic" component is one in which the patient is barrel-chested and dyspneic, with obviously prolonged expiration, sitting forward in a hunched-over position
- - attempting to squeeze the air out of the lungs with each expiratory effort. In these patients, airspace enlargement is severe and diffusing capacity is low. ,
- - Dyspnea and hyperventilation are prominent, so that until very late in the disease, gas exchange is adequate and blood gas values are relatively normal. Because of prominent dyspnea and adequate oxygenation of hemoglobin, these patients are sometimes called "pink puffers
Conditions Related to Emphysema 1. Compensatory emphysema (overinflation) - Is a term used to designate the compensatory dilation of alveoli in response to loss of lung substance elsewhere, such as occurs in residual lung parenchyma after surgical removal of a diseased lung or lobe.
2. Obstructive overinflation - Refers to the condition in which the lung expands because air is trapped within it. - A common cause is subtotal obstruction by a tumor or foreign object. -
- Obstructive overinflation can be a life -threatening emergency if the affected portion extends sufficiently to compress the remaining normal lung.
3. Bullous emphysema refers to any form of emphysema that produces large subpleural blebs or bullae (spaces >1 cm in diameter They represent localized accentuations of any form of emphysema, are most often subpleural, and on occasion, rupture leading to pneumothorax
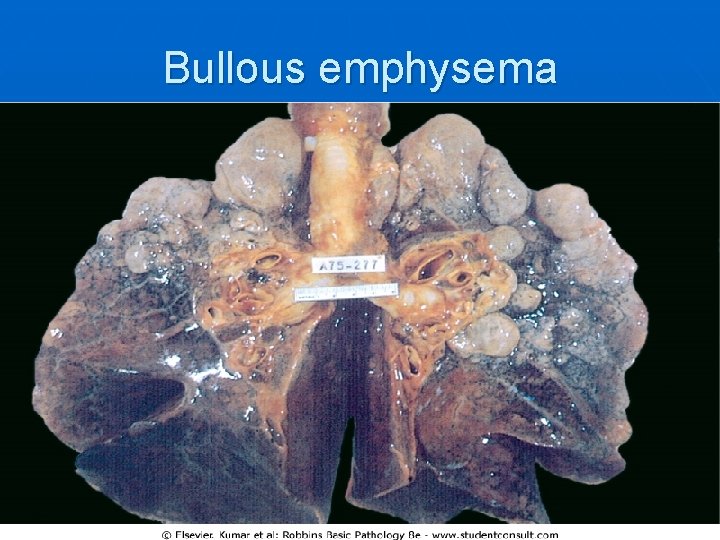
Bullous emphysema
d. Mediastinal (interstitial) - emphysema designates the entrance of air into the connective tissue stroma of the lung, mediastinum, and subcutaneous tissue. This may occur spontaneously with a sudden increase in intra-alveolar pressure (as with vomiting or violent
coughing) that causes a tear, with dissection of air into the interstitium. - Sometimes it occurs in children with whooping cough - It occurs in persons who suffer a perforating injury (e. g. , a fractured rib).
- - When the interstitial air enters the subcutaneous tissue, the patient may blow up like a balloon, with marked swelling of the head and neck In most instances, the air is resorbed spontaneously when the site of entry is sealed
2. Chronic Bronchitis - - Is common among cigarette smokers and urban dwellers The diagnosis of chronic bronchitis is made on clinical grounds: it is defined as a persistent productive cough for at least 3 consecutive months in at least 2 consecutive years.
It can occur in several forms: A. Most patients have simple chronic bronchitis: the productive cough raises mucoid sputum, but airflow is not obstructed. - A subpopulation of bronchitic patients, especially heavy smokers, develops chronic outflow obstruction -
usually with evidence of associated emphysema, and these individuals are said to have chronic obstructive bronchitis
The morphologic basis of airflow obstruction in chronic bronchitis is more peripheral and results from socalled : a. "small airway disease, " induced by goblet cell metaplasia with mucus plugging of the bronchiolar lumen, inflammation, and bronchiolar wall fibrosis, -
2. coexistent emphysema. It is generally believed that while small airway disease (also known as chronic bronchiolitis) is an important component of early and relatively mild airflow obstruction, chronic bronchitis with significant airflow obstruction is almost always complicated by emphysema. -
n n n Clinical Course In individuals with chronic bronchitis, a prominent cough and the production of sputum may persist indefinitely without ventilatory dysfunction. However, some sufferers develop significant COPD (chronic obstructive pulmonary disease) with outflow obstruction.
n n This is accompanied by hypercapnia, hypoxemia, and (in severe cases) cyanosis. The patients are called ("blue bloaters").
n n With progression, chronic bronchitis is complicated by pulmonary hypertension and cardiac failure Recurrent infections and respiratory failure are constant threats
3. Asthma - is a chronic inflammatory disorder of the airways that causes recurrent episodes of wheezing, breathlessness, chest tightness, and cough, particularly at night and/or early in the morning. - This clinical picture is caused by repeated immediate hypersensitivity and late-phase reactions in the lung that give rise to the triad of
- - - intermittent and reversible airway obstruction, chronic bronchial inflammation with eosinophils, and bronchial smooth muscle cell hypertrophy and hyperreactivity.
Types: A. Atopic Asthma: - About 70% of cases are said to be "extrinsic" or "atopic" and are due to immune responses to environmental antigens. 1. This is the most common type of asthma 2. usually begins in childhood.
3. A positive family history of atopy (type I hypersensitivity reaction)is common
, 4. and asthmatic attacks are often preceded by allergic rhinitis, urticaria, or eczema. 5. The disease is triggered by environmental antigens, such as dusts, pollen, animal dander, and foods, but potentially antigen is implicated.
B. In the remaining 30% of patients, asthma is said to be "intrinsic" or "non -atopic" and is triggered by 1. pulmonary infections, especially those caused by viruses; 2. Cold; 3. psychological stress; 4. Exercise; and 5. Inhaled irritants. .
Drug-Induced Asthma : -Several pharmacologic agents provoke asthma, - aspirin being the most striking example. - Individuals with aspirin sensitivity present with recurrent rhinitis and nasal polyps, urticaria, and bronchospasm.
- It is presumed that aspirin inhibits the cyclooxygenase pathway of arachidonic acid metabolism without affecting the lipoxygenase route, thereby shifting the balance toward bronchoconstrictor leukotrienes
Clinical Course - - An attack of asthma is characterized by severe dyspnea with wheezing; the chief difficulty lies in expiration. The victim labors to get air into the lungs and then cannot get it out, so that there is progressive hyperinflation of the lungs with air trapped distal to the bronchi, which are constricted and filled with mucus and debris.
- In the usual case, attacks last from 1 to several hours and subside either spontaneously or with therapy, usually bronchodilators and corticosteroids.
- Intervals between attacks are characteristically free from respiratory difficulty, but persistent, subtle respiratory deficits can be detected by spirometric methods.
- - Occasionally a severe paroxysm occurs that does not respond to therapy and persists for days and even weeks (status asthmaticus). The associated hypercapnia, acidosis, and severe hypoxia may be fatal, although in most cases the disease is more disabling than lethal
4. Bronchiectasis : - Bronchiectasis is the permanent dilation of bronchi and bronchioles caused by destruction of the muscle and elastic supporting tissue, resulting from or associated with chronic necrotizing infections. - It is not a primary disease but rather is secondary to persisting infection or obstruction caused by a variety of
- Once developed, it gives rise to a characteristic symptom complex dominated by cough and expectoration of copious amounts of purulent fetid sputum.
- - Diagnosis depends on an appropriate history along with radiographic demonstration of bronchial dilation. The conditions that most commonly predispose to bronchiectasis include the following:
1. - - Bronchial obstruction. Common causes are tumors, foreign bodies, and occasionally impaction of mucus. Under these conditions, the bronchiectasis is localized to the obstructed lung segment
Bronchiectasis can also complicate atopic asthma and chronic bronchitis. 2. Congenital or hereditary conditions. a. In cystic fibrosis, widespread severe bronchiectasis results from obstruction and infection caused by the secretion of abnormally mucus. - This is an important and serious -
b. In immunodeficiency states, particularly immunoglobulin deficiencies, bronchiectasis is likely to develop because of an increased susceptibility to repeated bacterial infections;
c. Kartagener syndrome, an autosomal recessive disorder, is frequently associated with bronchiectasis and with sterility in males. - Structural abnormalities of the cilia impair mucociliary clearance in the airways, leading to persistent infections, and reduce the mobility of spermatozoa.
3. Necrotizing, or suppurative, pneumonia, particularly with virulent organisms such as Staphylococcus aureus or Klebsiella spp. , may predispose to bronchiectasis.
n n The airways may be dilated to as much as four times their usual diameter and on gross examination of the lung can be followed almost to the pleural surfaces By contrast, in normal lungs, the bronchioles cannot be followed by ordinary gross examination beyond a point 2 -3 cm from the pleural surfaces.
Clinical Course - The clinical manifestations consist of severe, persistent cough with expectoration of mucopurulent, sometimes fetid, sputum. - The sputum may contain flecks of blood; frank hemoptysis can occur. - Symptoms are often episodic and are precipitated by upper respiratory tract infections or the introduction of new pathogenic agents.
- - In cases of severe, widespread bronchiectasis, significant obstructive ventilatory defects develop, with hypoxemia, hypercapnia, pulmonary hypertension, and (rarely) cor pulmonale (right-sided heart failure). Metastatic brain abscesses and reactive amyloidosis are other, less frequent complications
Restrictive lung diseases n Diffuse interstitial (restrictive) lung diseases are a heterogeneous group of disorders characterized predominantly by diffuse and usually chronic involvement of the pulmonary connective tissue, principally the most peripheral and delicate interstitium in the alveolar walls.
Many of the entities in this group are of unknown cause and pathogenesis; some have an intra-alveolar as well as an interstitial component, and there is frequent overlap in histologic features among the different conditions. n Nevertheless, the presence of similar clinical signs, symptoms, radiographic alterations, and pathophysiologic changes justifies their consideration as a group. n
I. Idiopathic Pulmonary Fibrosis - - - Idiopathic pulmonary fibrosis (IPF), also known as cryptogenic fibrosing alveolitis, refers to a pulmonary disorder of unknown etiology Characterized histologically by diffuse interstitial fibrosis, which in advanced cases results in severe hypoxemia and cyanosis. The inciting agent for recurrent alveolitis in IPF is unknown.
- - - Males are affected more often than are females, and approximately two-thirds of patients are older than 60 years of age at presentation. The histologic pattern of fibrosis is referred to as usual interstitial pneumonia (UIP), which is required for the diagnosis of IPF.
n It should be noted, however, that similar pathologic findings in the lung may be seen with well-defined entities such as asbestosis, the collagen-vascular diseases. Therefore, known causes must be ruled out before the term of "idiopathic" is used
n - - Morphology The histologic hallmark of UIP is patchy interstitial fibrosis, which varies in intensity and with time. The earliest lesions contain exuberant fibroblastic proliferation and appear as fibroblastic foci With time these areas become more collagenous and less cellular.
- - Quite typical is the existence of both early and late lesions (temporal heterogeneity). The dense fibrosis causes collapse of alveolar walls and formation of cystic spaces lined by hyperplastic type II pneumocytes or bronchiolar epithelium (honeycomb fibrosis)
- - The interstitial inflammation is usually patchy and consists of an alveolar septal infiltrate of mostly lymphocytes and occasional plasma cells, mast cells, and eosinophils. Secondary pulmonary hypertensive changes (intimal fibrosis and medial thickening of pulmonary arteries) are often
Clinical Course - IPF usually presents insidiously, with the gradual onset of a nonproductive cough and progressive dyspnea. - On physical examination, most individuals with IPF have characteristic "dry" crackles during inspiration.
- Cyanosis, cor pulmonale, and peripheral edema may develop in the later stages of the disease. Surgical lung biopsy remains the gold standard for diagnosing IPF and for excluding other causes of pulmonary fibrosis. Unfortunately, the progress of IPF is relentless despite therapy, and the mean
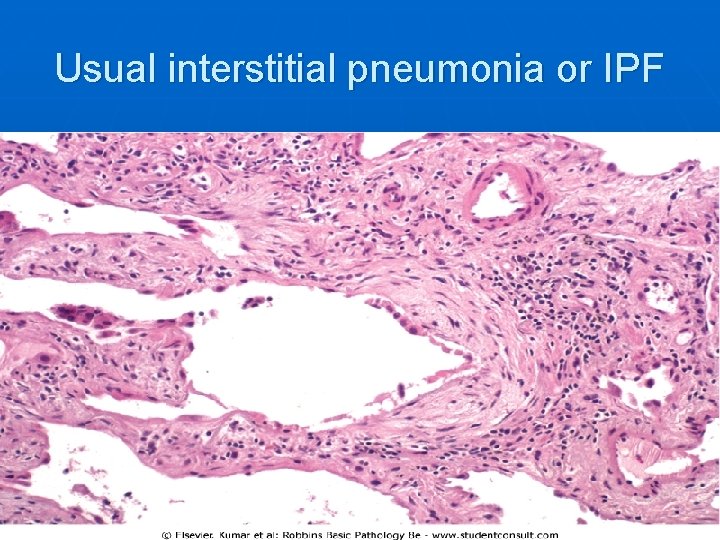
Usual interstitial pneumonia or IPF
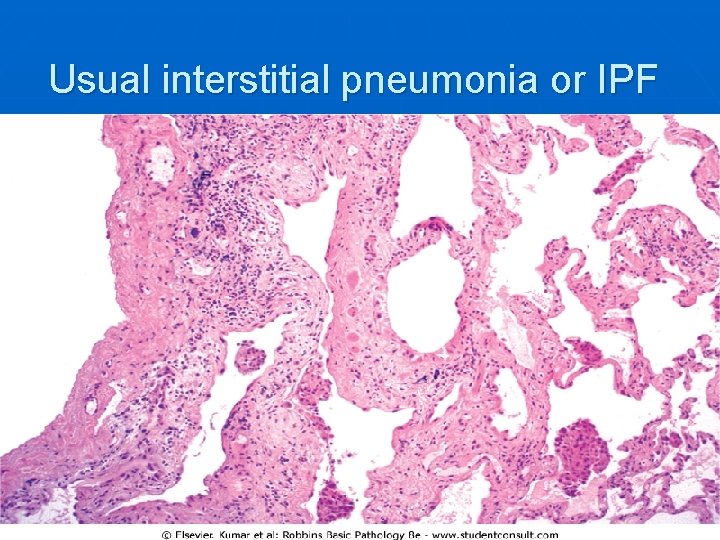
Usual interstitial pneumonia or IPF

Honeycomb lung

Other interstitial lung disease II. Coal worker pneumoconiosis III. Silicosis IV. Asbestosis a. Diffuse lung fibrosis b. Fibrous plaques in pleura (most common) c. Pleural effusion d. Lung carcinoma e. Mesothelioma
Diseases of vascular origin Diffuse Alveolar Hemorrhage Syndromes -While there may be several "secondary" causes of pulmonary hemorrhage (necrotizing bacterial pneumonia, passive venous congestion, bleeding diathesis), - The diffuse alveolar hemorrhage syndromes are a group of "primary" immune-mediated diseases that present as the triad of hemoptysis, anemia, and diffuse pulmonary infiltrates n
V. Hypersensitivity pneumonitis - Hypersensitivity reaction at the level of alveoli - Characterized early by granuloma replaced by fibrosis in the late reaction
VI. Sarcoidosis - Is a systemic granulomatous disease - Involve many organ but the main involvement is in the form of bilateral hilar lymph node enlargement and or lung involvement
Vascular diseases of lung 1. Goodpasture Syndrome - Goodpasture syndrome, the prototype disorder of this group, is an uncommon condition that is characterized by a proliferative, usually rapidly progressive, glomerulonephritis and hemorrhagic interstitial pneumonitis. -.
- - Both the renal and the pulmonary lesions are caused by antibodies targeted against the noncollagenous domain of the α 3 chain of collagen IV. These antibodies can be detected in the serum of more than 90% of persons with Goodpasture syndrome
n - - a. b. Morphology In the classic case of diffuse alveolar hemorrhage, the lungs are heavy, with areas of red-brown consolidation. Microscopic examination of the lungs demonstrates: Focal necrosis of alveolar walls Intra-alveolar hemorrhages,
c. Fibrous thickening of the septa, and d. The presence of hemosiderin, either within macrophages or extracellularly, is characteristically seen for a few days after an acute presentation. The characteristic linear pattern of immunoglobulin deposition (usually Ig. G, sometimes Ig. A or Ig. M) is the most important diagnostic feature in renal biopsy specimens is also seen along the alveolar septa.
Plasmapheresis and immunosuppressive therapy have markedly improved the once dismal prognosis for this disease. n Plasma exchange removes offending antibodies, and immunosuppressive drugs inhibit antibody production. n With severe renal disease, renal transplantation is eventually required. n
Idiopathic Pulmonary Hemosiderosis Idiopathic pulmonary hemosiderosis is a disease of uncertain etiology that has pulmonary manifestations and histology similar to those of Goodpasture syndrome, but there is no associated renal disease or circulating anti-basement membrane antibody. 2. -
- - Clinically, the course is usually mild to moderate, with periods of activity followed by prolonged, often spontaneous, remissions. Most cases occur in children, although the disease is reported in adults as well.
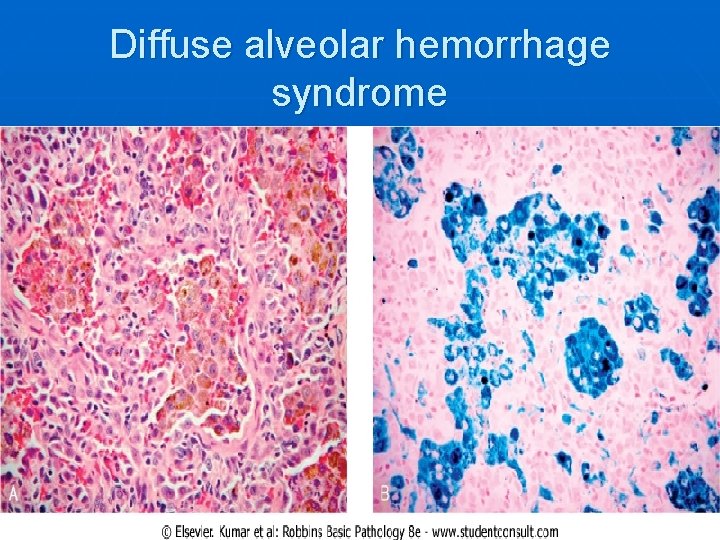
Diffuse alveolar hemorrhage syndrome
- Slides: 78