OBSTRUCTIVE AND RESTRICTIVE LUNG DISEASE JED WOLPAW MD
OBSTRUCTIVE AND RESTRICTIVE LUNG DISEASE JED WOLPAW MD, M. ED
OUTLINE • OBSTRUCTIVE DISEASE • UPPER AIRWAY • EXTRATHORACIC • INTRATHORACIC • LOWER AIRWAY/PARENCHYMAL • RESTRICTIVE DISEASE • NEUROLOGIC • MUSKULOSKELETAL • PARENCHYMAL • PLEURAL AND MEDIASTINAL • OTHER
OBSTRUCTIVE DISEASE: UPPER AIRWAY
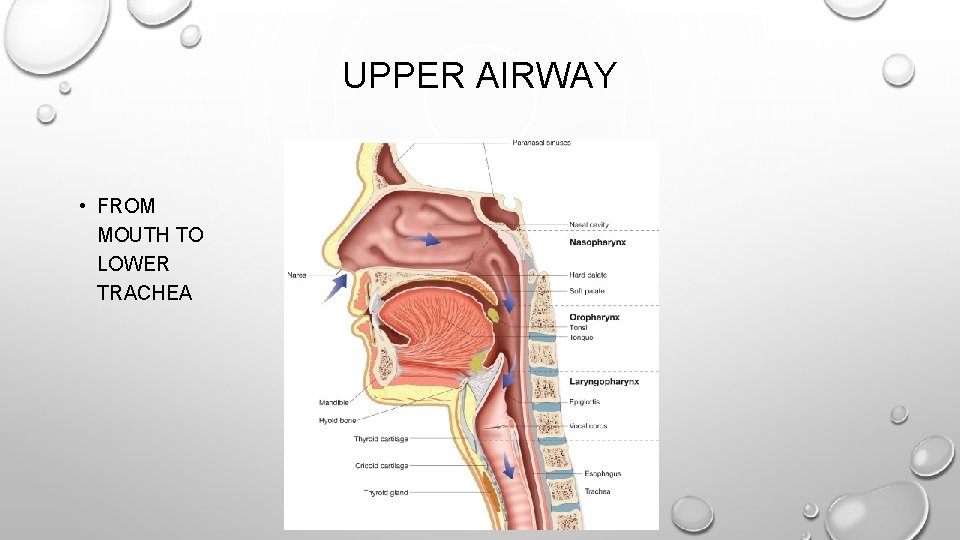
UPPER AIRWAY • FROM MOUTH TO LOWER TRACHEA
INTRA VS EXTRATHORACIC • WHICH LESION LIMITS INSPIRATORY FLOW THE MOST? • A: VARIABLE UPPER AIRWAY EXTRATHORACIC OBSTRUCTION • B: VARIABLE UPPER AIRWAY INTRATHORACIC OBSTRUCTION • C: COPD • D: ASTHMA
INTRA VS EXTRATHORACIC • WHICH LESION LIMITS INSPIRATORY FLOW THE MOST? • A: VARIABLE UPPER AIRWAY EXTRATHORACIC OBSTRUCTION • B: VARIABLE UPPER AIRWAY INTRATHORACIC OBSTRUCTION • C: COPD • D: ASTHMA
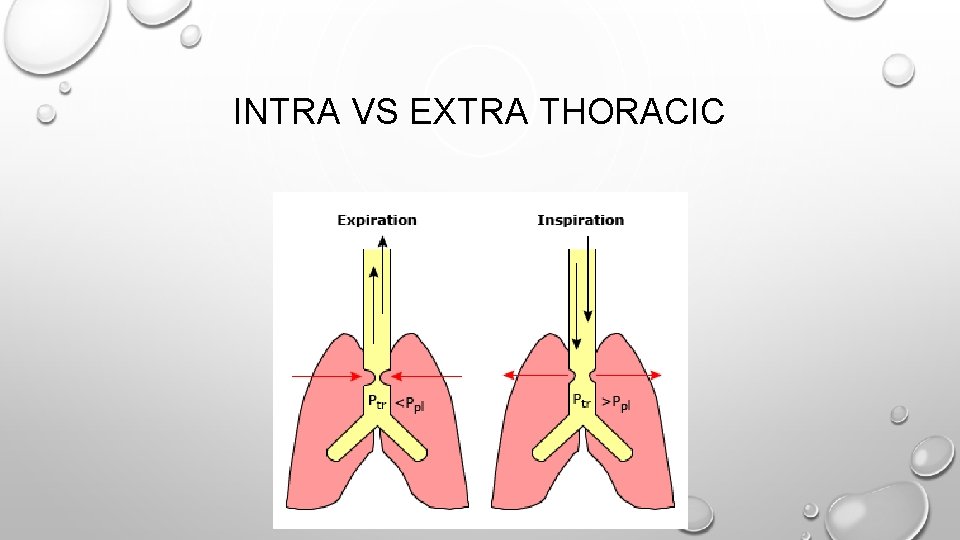
INTRA VS EXTRA THORACIC
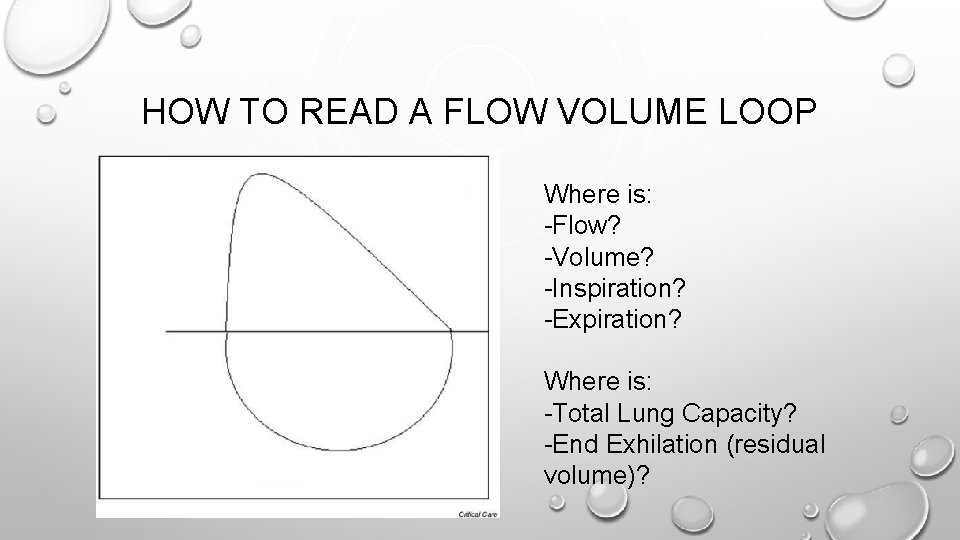
HOW TO READ A FLOW VOLUME LOOP Where is: -Flow? -Volume? -Inspiration? -Expiration? Where is: -Total Lung Capacity? -End Exhilation (residual volume)?
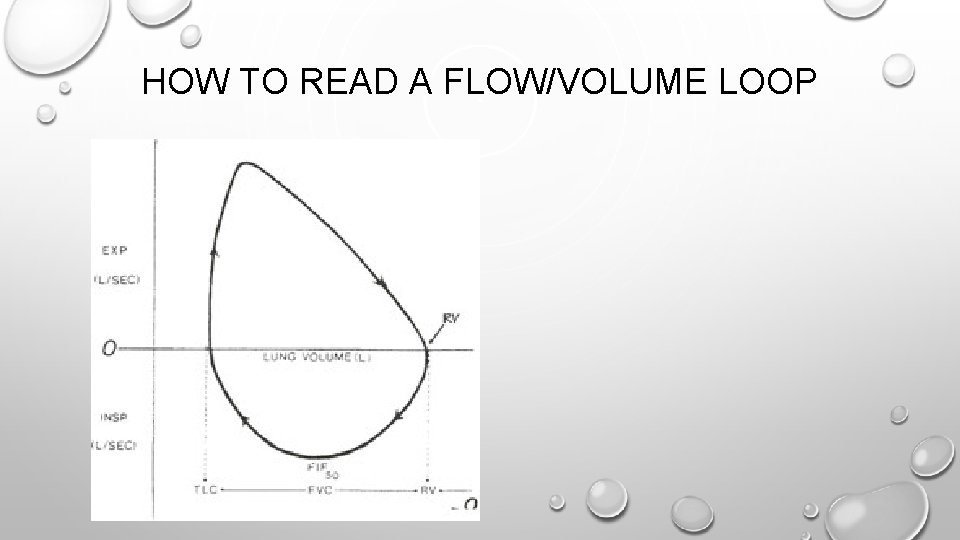
HOW TO READ A FLOW/VOLUME LOOP

NAME THAT OBSTRUCTION
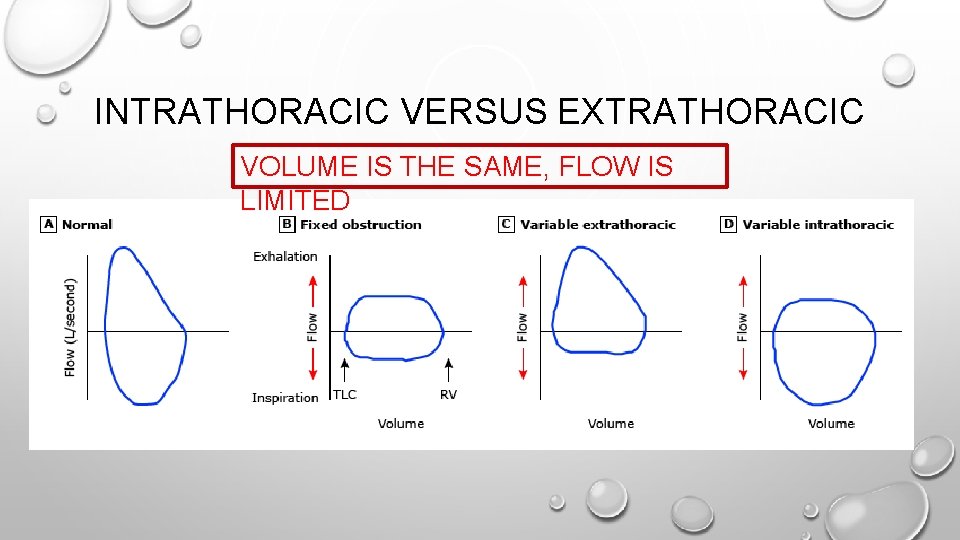
INTRATHORACIC VERSUS EXTRATHORACIC VOLUME IS THE SAME, FLOW IS LIMITED
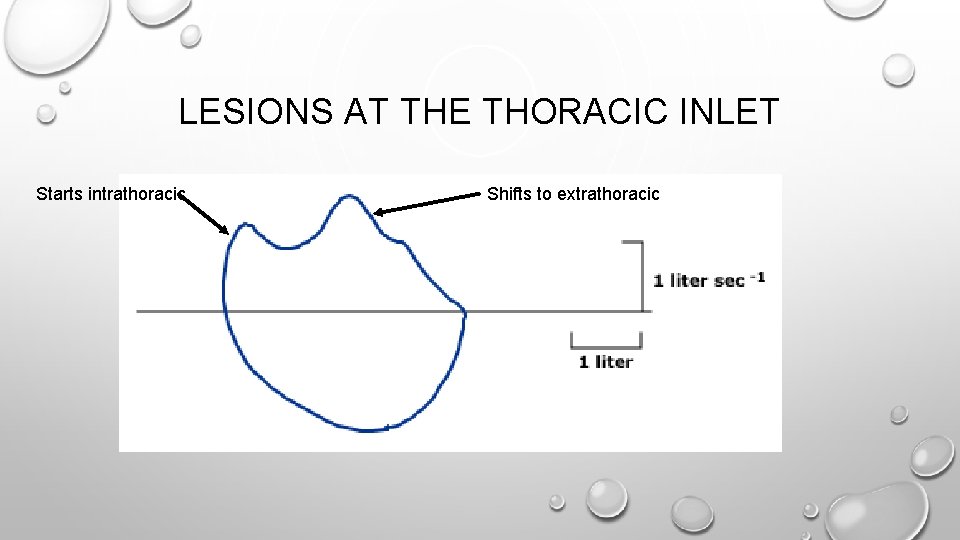
LESIONS AT THE THORACIC INLET Starts intrathoracic Shifts to extrathoracic
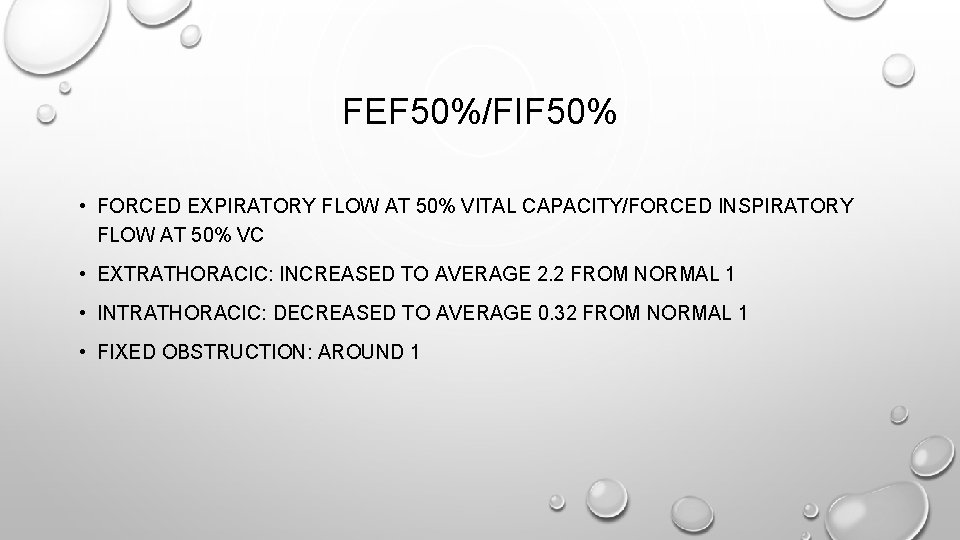
FEF 50%/FIF 50% • FORCED EXPIRATORY FLOW AT 50% VITAL CAPACITY/FORCED INSPIRATORY FLOW AT 50% VC • EXTRATHORACIC: INCREASED TO AVERAGE 2. 2 FROM NORMAL 1 • INTRATHORACIC: DECREASED TO AVERAGE 0. 32 FROM NORMAL 1 • FIXED OBSTRUCTION: AROUND 1
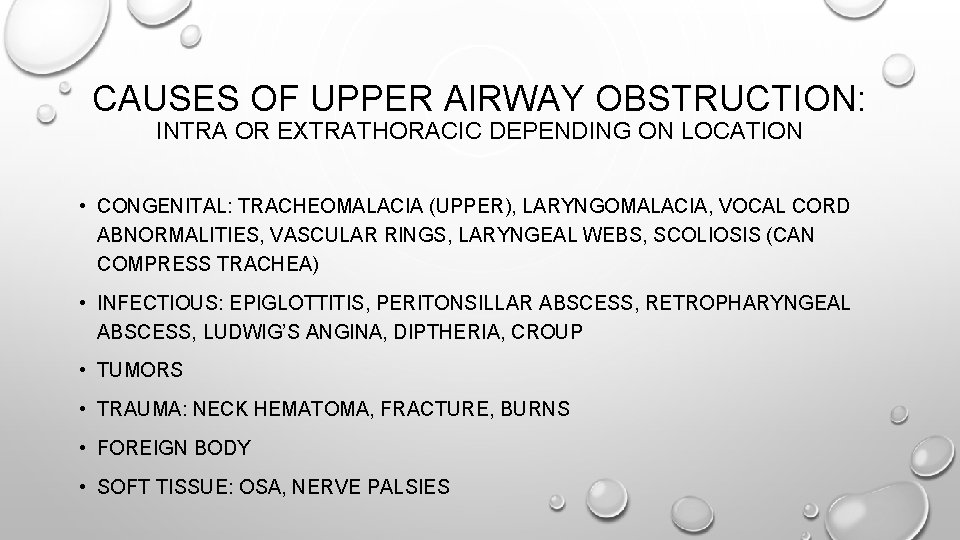
CAUSES OF UPPER AIRWAY OBSTRUCTION: INTRA OR EXTRATHORACIC DEPENDING ON LOCATION • CONGENITAL: TRACHEOMALACIA (UPPER), LARYNGOMALACIA, VOCAL CORD ABNORMALITIES, VASCULAR RINGS, LARYNGEAL WEBS, SCOLIOSIS (CAN COMPRESS TRACHEA) • INFECTIOUS: EPIGLOTTITIS, PERITONSILLAR ABSCESS, RETROPHARYNGEAL ABSCESS, LUDWIG’S ANGINA, DIPTHERIA, CROUP • TUMORS • TRAUMA: NECK HEMATOMA, FRACTURE, BURNS • FOREIGN BODY • SOFT TISSUE: OSA, NERVE PALSIES
OBSTRUCTIVE DISEASE: LOWER AIRWAY/PARENCHYMAL
LOWER AIRWAY/PARENCHYMAL OBSTRUCTIVE DISEASES • ASTHMA • EMPHYSEMA • BRONCHITIS • CF: BRONCHIECTASIS • MEDIASTINAL MASSES
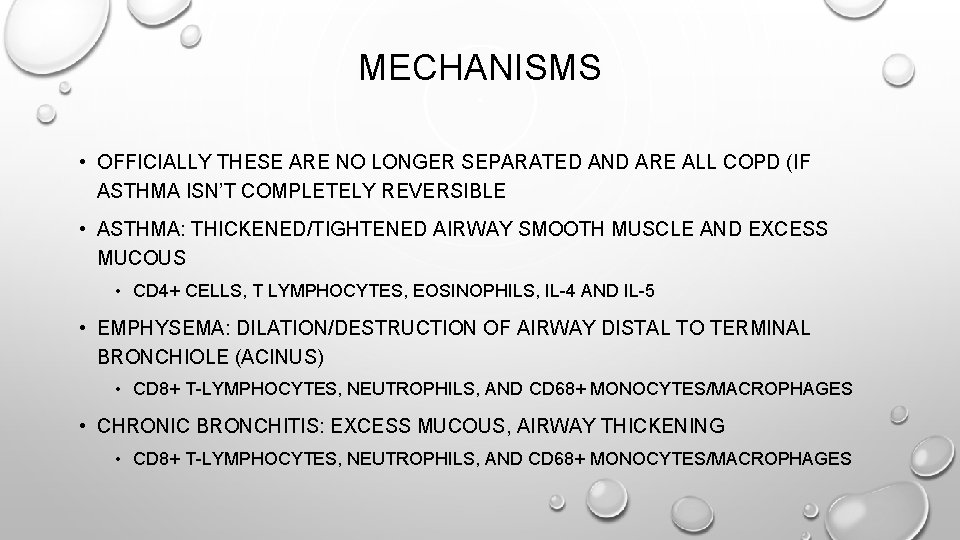
MECHANISMS • OFFICIALLY THESE ARE NO LONGER SEPARATED AND ARE ALL COPD (IF ASTHMA ISN’T COMPLETELY REVERSIBLE • ASTHMA: THICKENED/TIGHTENED AIRWAY SMOOTH MUSCLE AND EXCESS MUCOUS • CD 4+ CELLS, T LYMPHOCYTES, EOSINOPHILS, IL-4 AND IL-5 • EMPHYSEMA: DILATION/DESTRUCTION OF AIRWAY DISTAL TO TERMINAL BRONCHIOLE (ACINUS) • CD 8+ T-LYMPHOCYTES, NEUTROPHILS, AND CD 68+ MONOCYTES/MACROPHAGES • CHRONIC BRONCHITIS: EXCESS MUCOUS, AIRWAY THICKENING • CD 8+ T-LYMPHOCYTES, NEUTROPHILS, AND CD 68+ MONOCYTES/MACROPHAGES
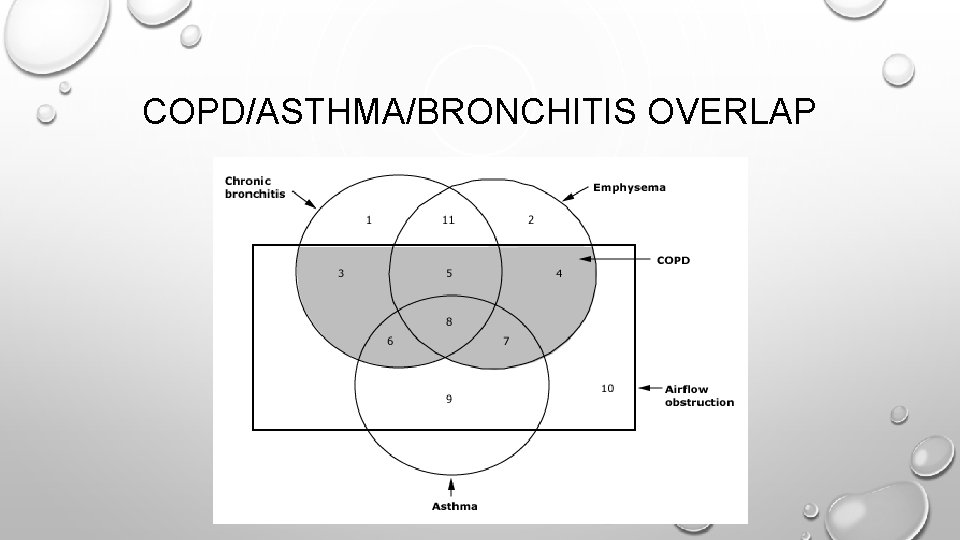
COPD/ASTHMA/BRONCHITIS OVERLAP
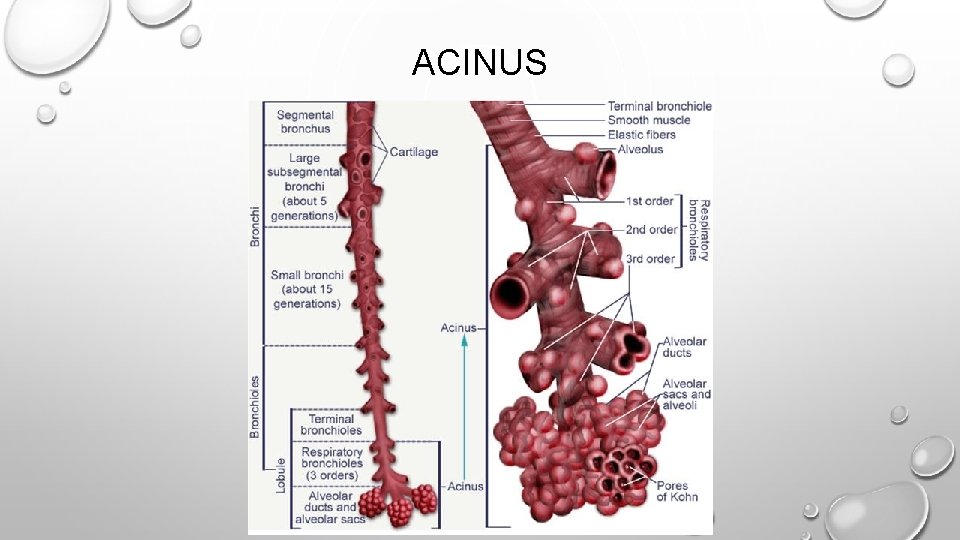
ACINUS
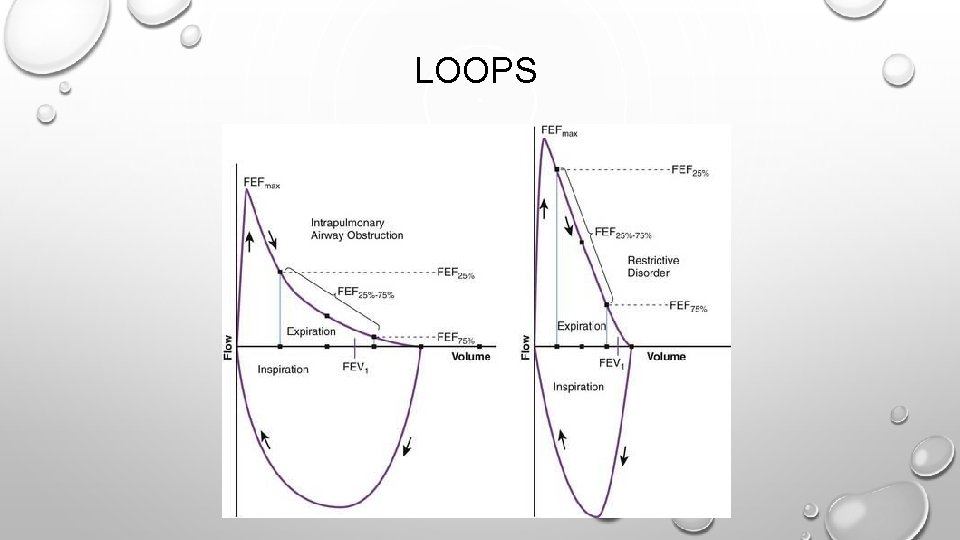
LOOPS
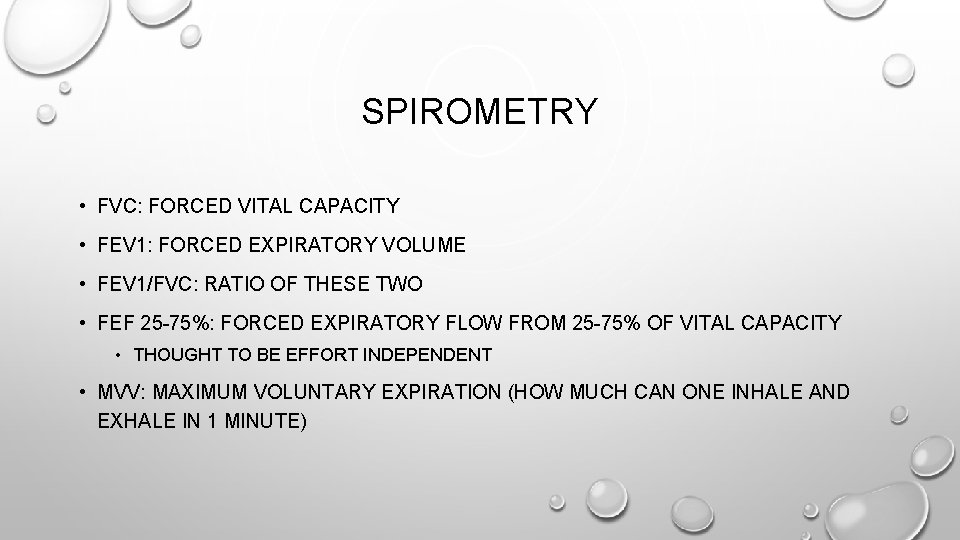
SPIROMETRY • FVC: FORCED VITAL CAPACITY • FEV 1: FORCED EXPIRATORY VOLUME • FEV 1/FVC: RATIO OF THESE TWO • FEF 25 -75%: FORCED EXPIRATORY FLOW FROM 25 -75% OF VITAL CAPACITY • THOUGHT TO BE EFFORT INDEPENDENT • MVV: MAXIMUM VOLUNTARY EXPIRATION (HOW MUCH CAN ONE INHALE AND EXHALE IN 1 MINUTE)

SPIROMETRY
DLCO (DIFFUSION CAPACITY FOR CARBON MONOXIDE) • MEASURES THE ABILITY OF THE LUNGS TO TRANSFER O 2 TO THE BLOOD • OBSTRUCTIVE DISEASE • CORRELATES WITH DEGREE OF EMPHYSEMA • SMOKERS WITH AIRWAY OBSTRUCTION BUT NORMAL DLCO HAVE BRONCHITIS BUT NOT EMPHYSEMA • ASTHMATICS HAVE NORMAL OR HIGH DLCO • CYSTIC FIBROSIS: NORMAL UNTIL VERY LATE IN DISEASE
CYSTIC FIBROSIS • MUTATION IN CFTR LEADING TO INABILITY TO TRANSPORT CHLORIDE AND SODIUM • AUTOSOMAL RECESSIVE • MULTIPLE ORGAN SYSTEMS EFFECTED, WE WILL FOCUS ON RESPIRATORY • LIFE EXPECTANCY AVERAGE 39 YEARS
WHAT IS BRONCHIECTASIS • A: CHRONIC AIRWAY INFECTION • B: RECURRENT PNEUMONIA IN CYSTIC FIBROSIS • C: DILATION OF AIRWAYS DUE TO WALL DESTRUCTION • D: BEING THE SUBJECT OF EXCESS BRONCHOSCOPIES
WHAT IS BRONCHIECTASIS • A: CHRONIC AIRWAY INFECTION • B: RECURRENT PNEUMONIA IN CYSTIC FIBROSIS • C: DILATION OF AIRWAYS DUE TO WALL DESTRUCTION • D: BEING THE SUBJECT OF EXCESS BRONCHOSCOPIES
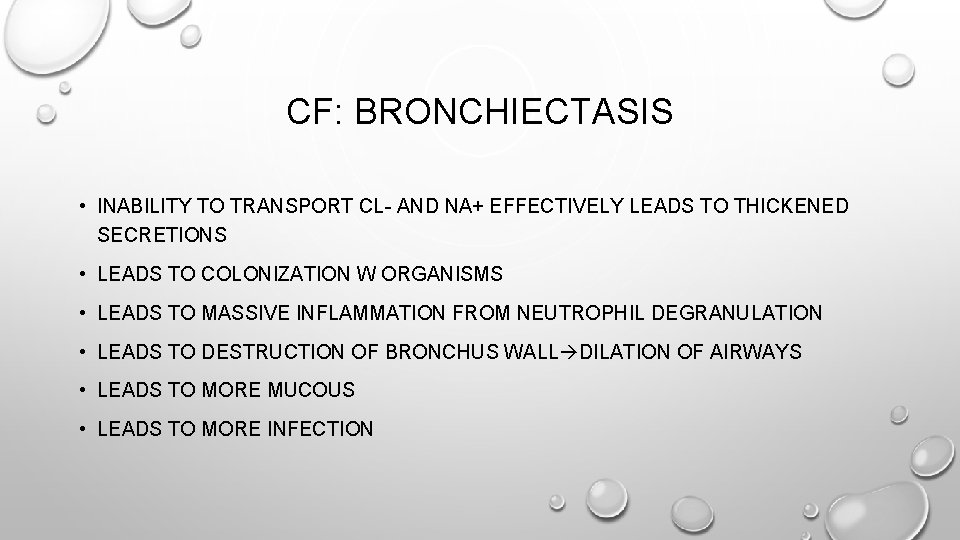
CF: BRONCHIECTASIS • INABILITY TO TRANSPORT CL- AND NA+ EFFECTIVELY LEADS TO THICKENED SECRETIONS • LEADS TO COLONIZATION W ORGANISMS • LEADS TO MASSIVE INFLAMMATION FROM NEUTROPHIL DEGRANULATION • LEADS TO DESTRUCTION OF BRONCHUS WALL DILATION OF AIRWAYS • LEADS TO MORE MUCOUS • LEADS TO MORE INFECTION
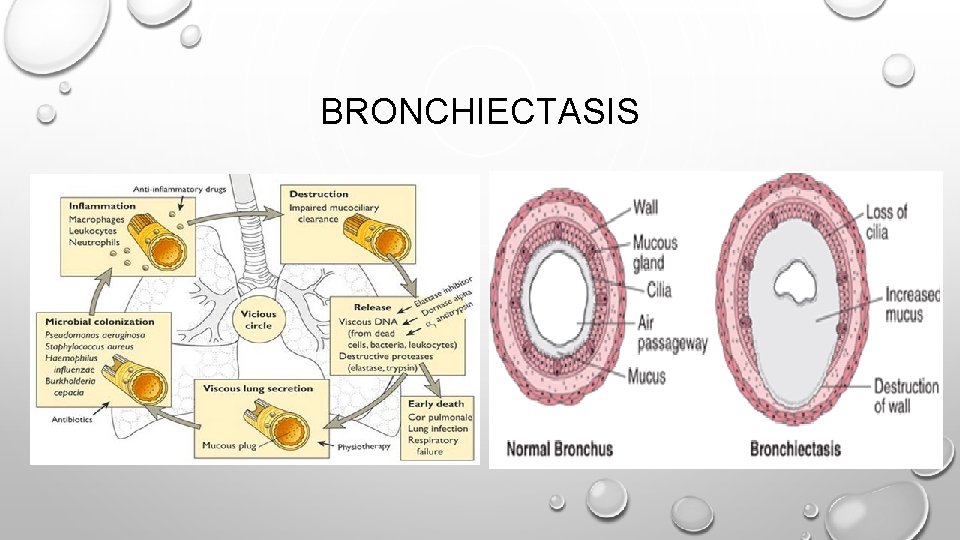
BRONCHIECTASIS
CF: WHY PSEUDOMONAS? • INCREASED O 2 UTILIZATION BY LUNG EPITHELIAL CELLS CAUSES LOCAL HYPOXIA • THIS CAUSES PSEUDOMONAS TO GAIN THE ABILITY TO MAKE BIOFILMS • ALMOST IMPOSSIBLE TO ERADICATE AT THAT POINT
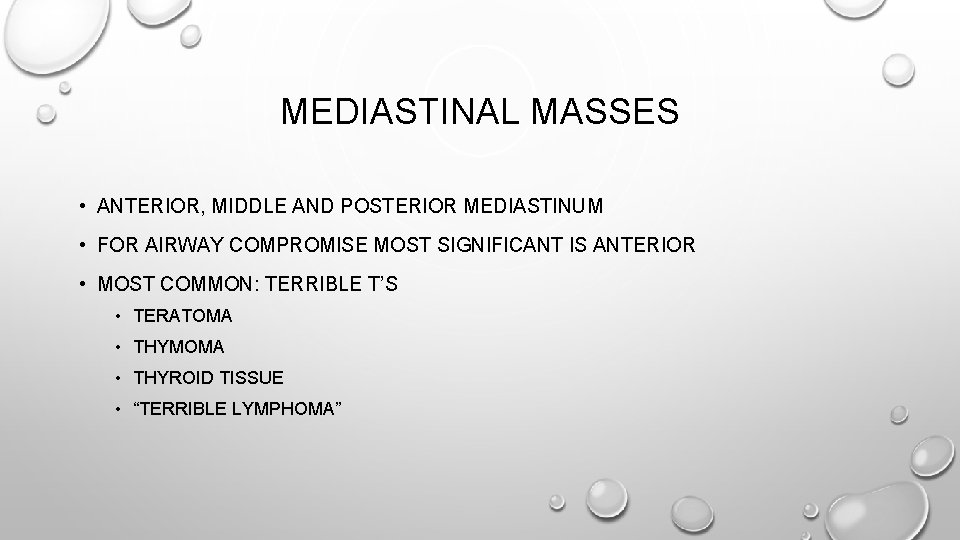
MEDIASTINAL MASSES • ANTERIOR, MIDDLE AND POSTERIOR MEDIASTINUM • FOR AIRWAY COMPROMISE MOST SIGNIFICANT IS ANTERIOR • MOST COMMON: TERRIBLE T’S • TERATOMA • THYMOMA • THYROID TISSUE • “TERRIBLE LYMPHOMA”
WHAT IS THE SAFEST WAY TO INDUCE A PATIENT WITH AN ANTERIOR MEDIASTINAL MASS COMPRESSING THE AIRWAY? • A: RSI WITH SUX AND ETOMIDATE • B: ASLEEP FIBER • C: AWAKE FIBER WITH SURGEON STANDING BY READY TO PERFORM TRACHEOSTOMY • D: AWAKE FIBER AFTER CANNULATING GROIN VESSELS FOR ECMO
WHAT IS THE SAFEST WAY TO INDUCE A PATIENT WITH AN ANTERIOR MEDIASTINAL MASS COMPRESSING THE AIRWAY? • A: RSI WITH SUX AND ETOMIDATE • B: ASLEEP FIBER • C: AWAKE FIBER WITH SURGEON STANDING BY READY TO PERFORM TRACHEOSTOMY • D: AWAKE FIBER AFTER CANNULATING GROIN VESSELS FOR ECMO
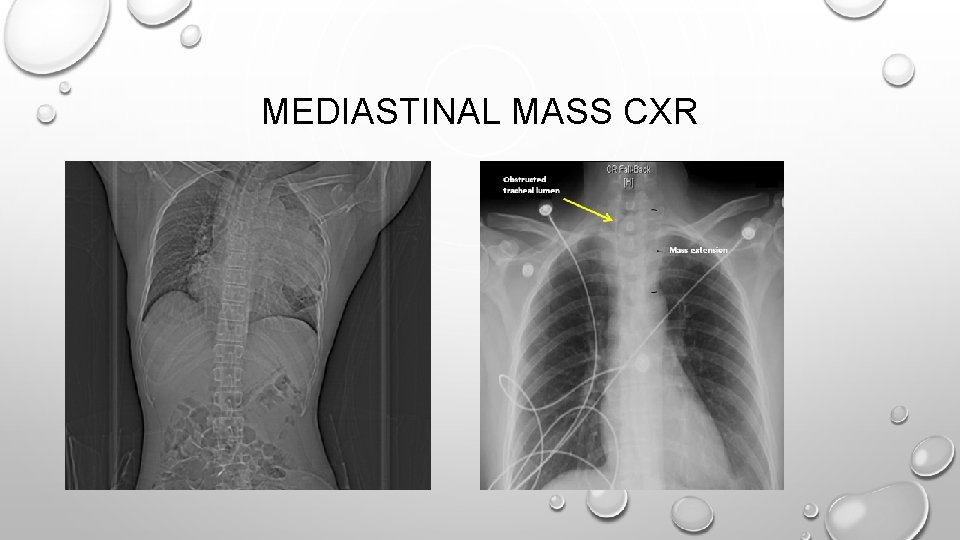
MEDIASTINAL MASS CXR
MEDIASTINAL MASS • CAN CAUSE BOTH OBSTRUCTIVE (COMPRESSING TRACHEA) OR RESTRICTIVE (REDUCING COMPLIANCE OF LUNGS) PATHOLOGY • CAN COMPRESS: • AIRWAYS • VESSELS (SVC) • HEART
MEDIASTINAL MASS • PREPARATION • GROIN LINE IN CASE OF SVC OBSTRUCTION • AWAKE INTUBATION WITH SPONTANEOUS VENTILATION IN CASE OF AIRWAY OBSTRUCTION • AVOID NEUROMUSCULAR BLOCKADE IF POSSIBLE • IF IMAGING/SYMPTOMS VERY CONCERNING CANNULATE FOR ECMO/BYPASS FIRST • CRICHOTHYROTOMY WILL NOT HELP HERE
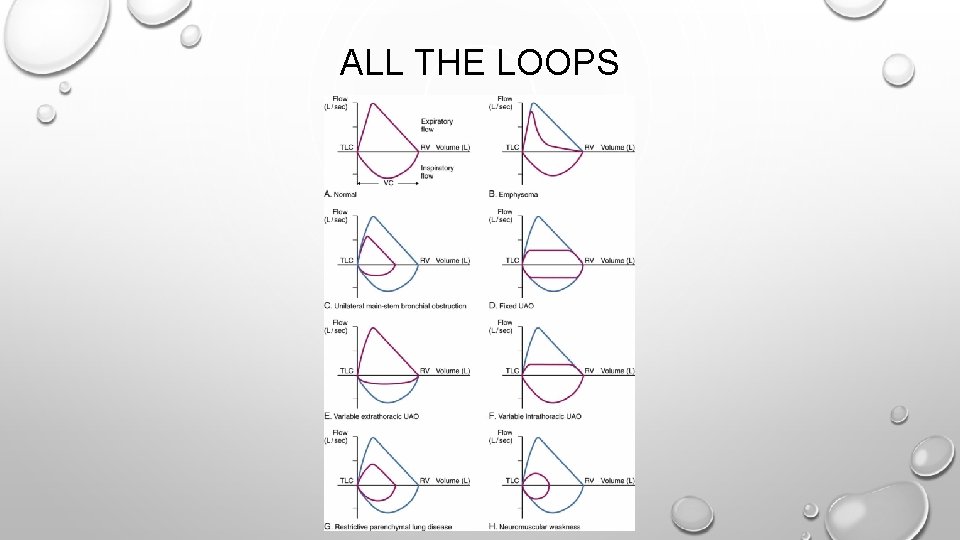
ALL THE LOOPS
- Slides: 36