OBSTRUCTIVE AIRWAY DISEASE Airways obstructive disease Lungs restrictive
OBSTRUCTIVE AIRWAY DISEASE • Airways - obstructive disease Lungs - restrictive disease • Obstructive airway syndrome Asthma Chronic bronchitis Emphysema
OBSTRUCTIVE AIRWAY DISEASE Terminology • Early onset / late onset • Atopic / non-atopic • Extrinsic / Intrinsic
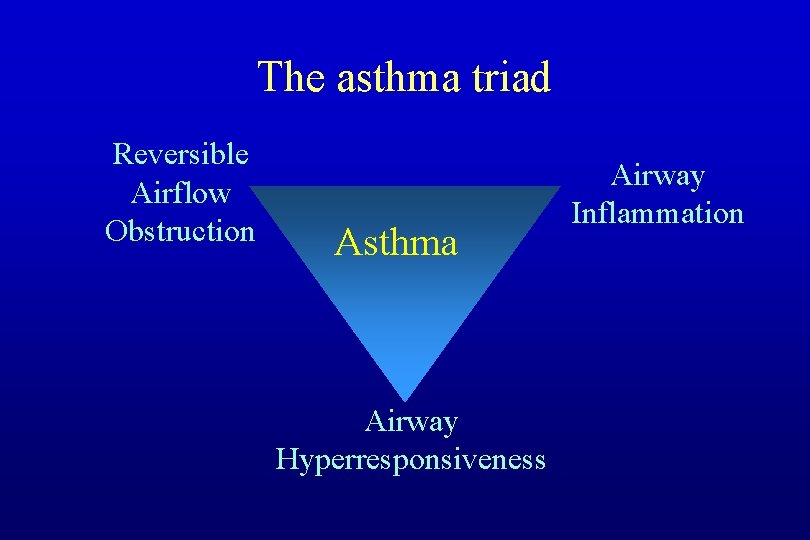
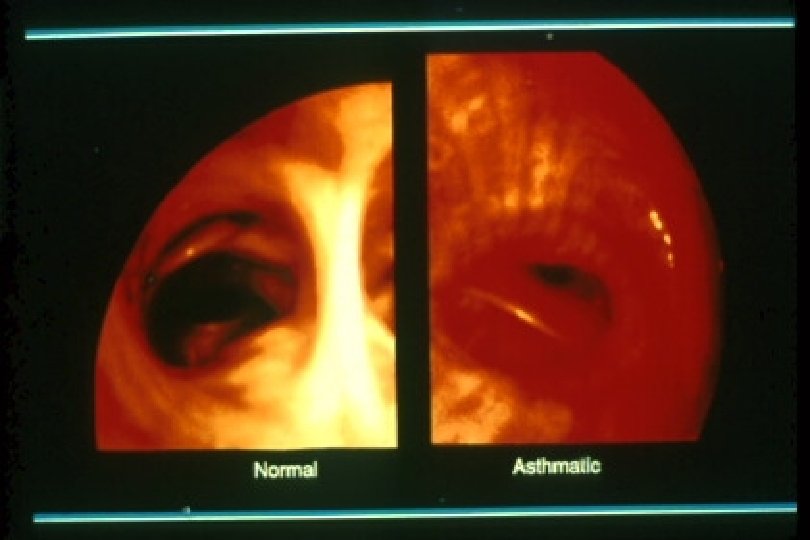
The asthma triad Reversible Airflow Obstruction Asthma Airway Hyperresponsiveness Airway Inflammation
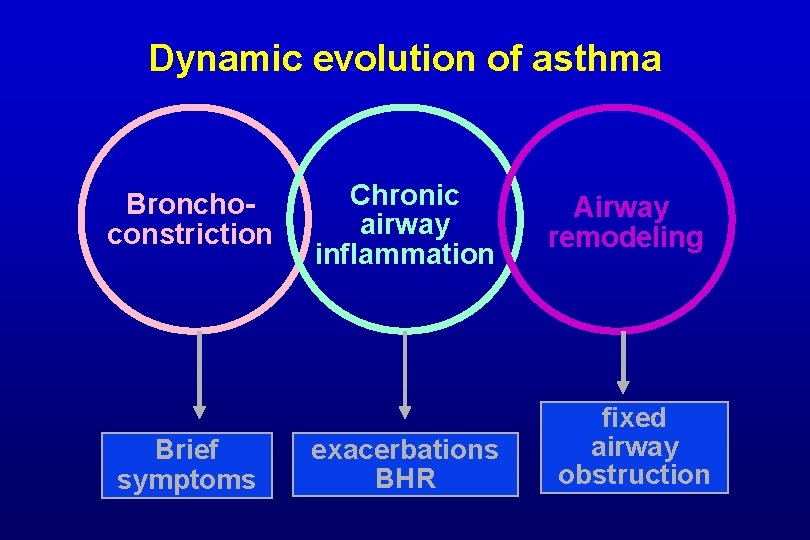
Dynamic evolution of asthma Bronchoconstriction Brief symptoms Chronic airway inflammation exacerbations BHR Airway remodeling fixed airway obstruction
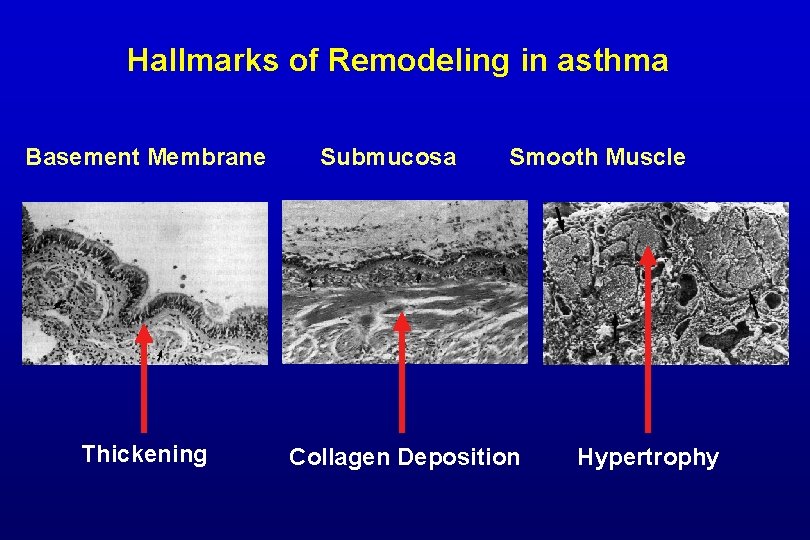
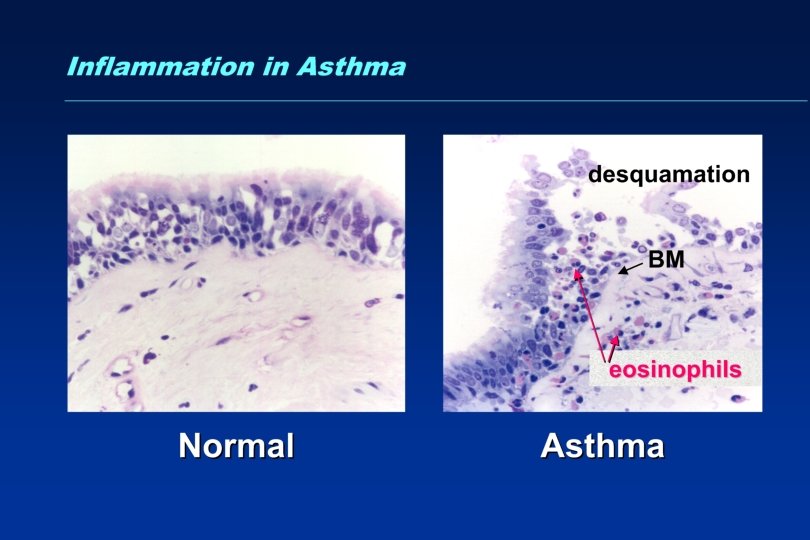
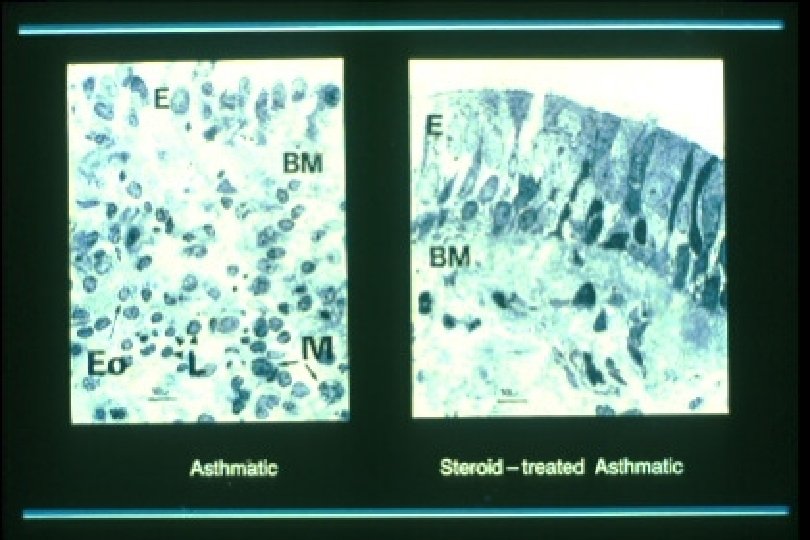
Hallmarks of Remodeling in asthma Basement Membrane Thickening Submucosa Smooth Muscle Collagen Deposition Hypertrophy
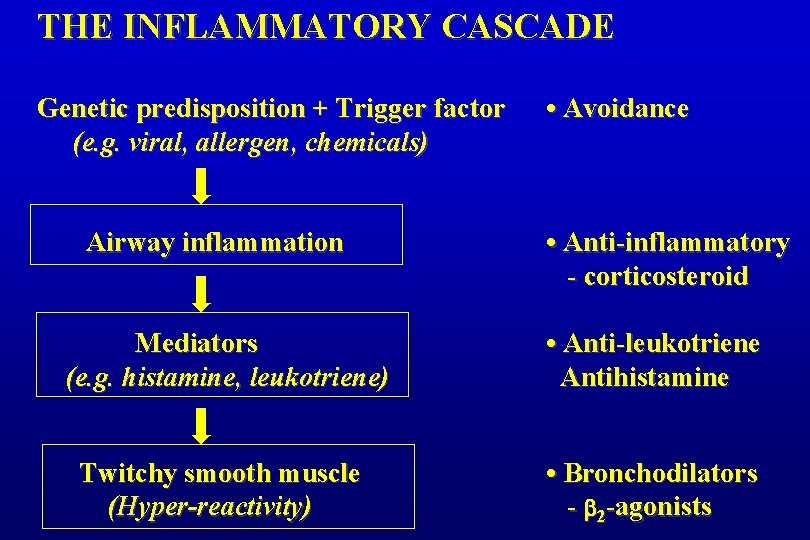
THE INFLAMMATORY CASCADE Genetic predisposition + Trigger factor (e. g. viral, allergen, chemicals) Airway inflammation • Avoidance • Anti-inflammatory - corticosteroid Mediators (e. g. histamine, leukotriene) • Anti-leukotriene Antihistamine Twitchy smooth muscle (Hyper-reactivity) • Bronchodilators - 2 -agonists
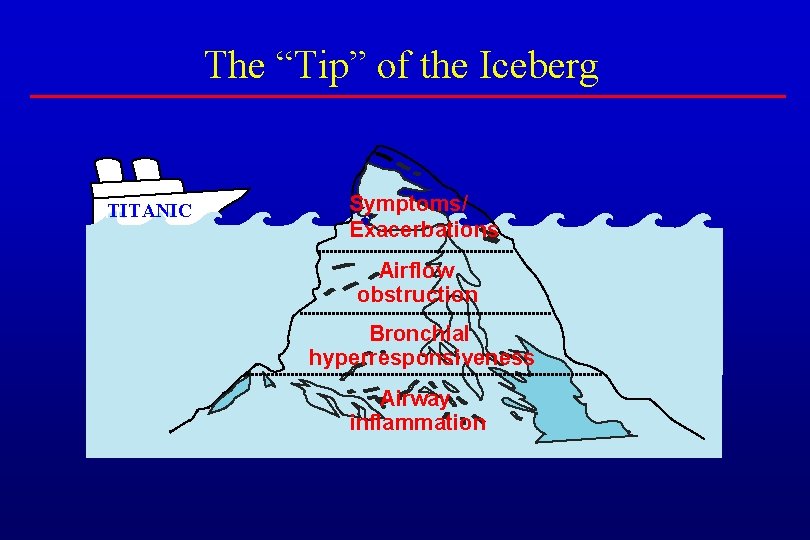
The “Tip” of the Iceberg TITANIC Symptoms/ Exacerbations Airflow obstruction Bronchial hyperresponsiveness Airway inflammation
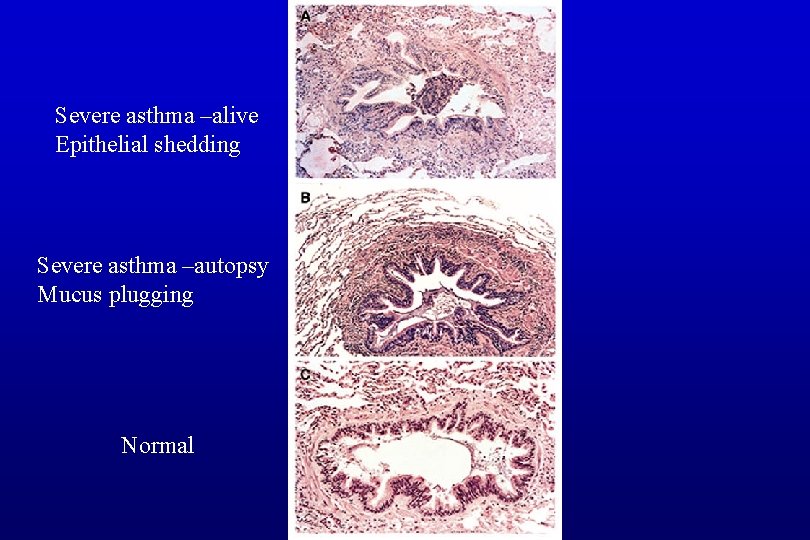
Severe asthma –alive Epithelial shedding Severe asthma –autopsy Mucus plugging Normal
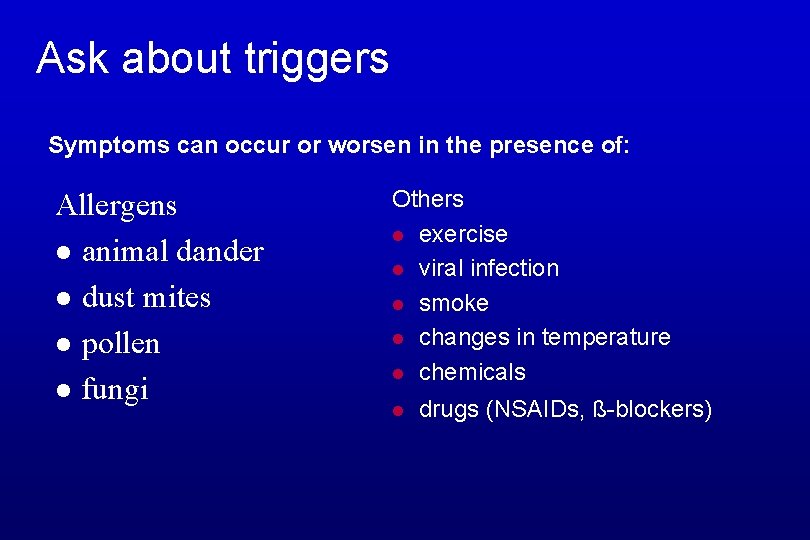
Ask about triggers Symptoms can occur or worsen in the presence of: Allergens l animal dander l dust mites l pollen l fungi Others l exercise l viral infection l smoke l changes in temperature l chemicals l drugs (NSAIDs, ß-blockers)
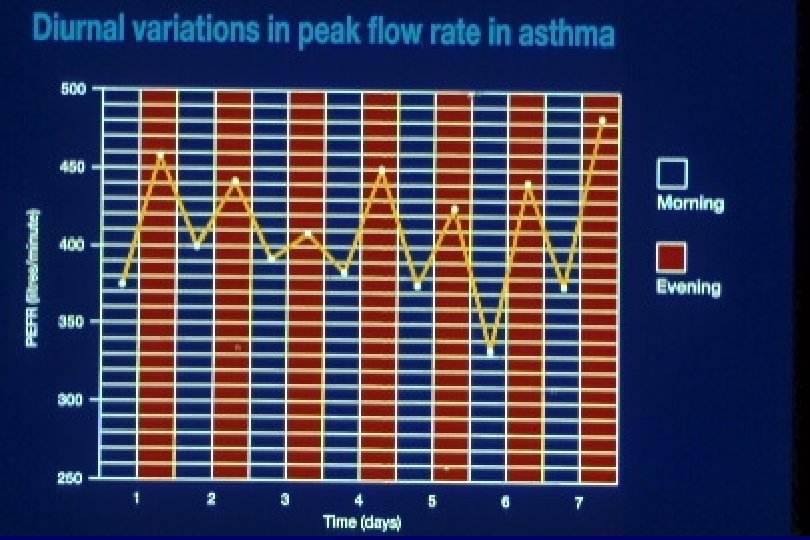
ASTHMA - THE CLINICAL SYNDROME • • Episodic symptoms and signs Diurinal variability – nocturnal/early morning Non-productive cough, wheeze Triggers Associated atopy ( rhinitis , conjunctivitis, eczema) Family history of asthma Wheezing due to turbulent airflow
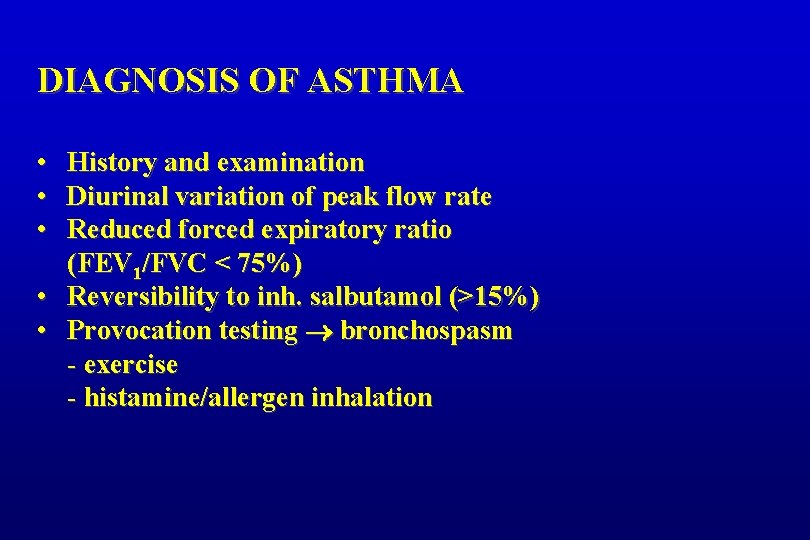
DIAGNOSIS OF ASTHMA • • • History and examination Diurinal variation of peak flow rate Reduced forced expiratory ratio (FEV 1/FVC < 75%) • Reversibility to inh. salbutamol (>15%) • Provocation testing bronchospasm - exercise - histamine/allergen inhalation
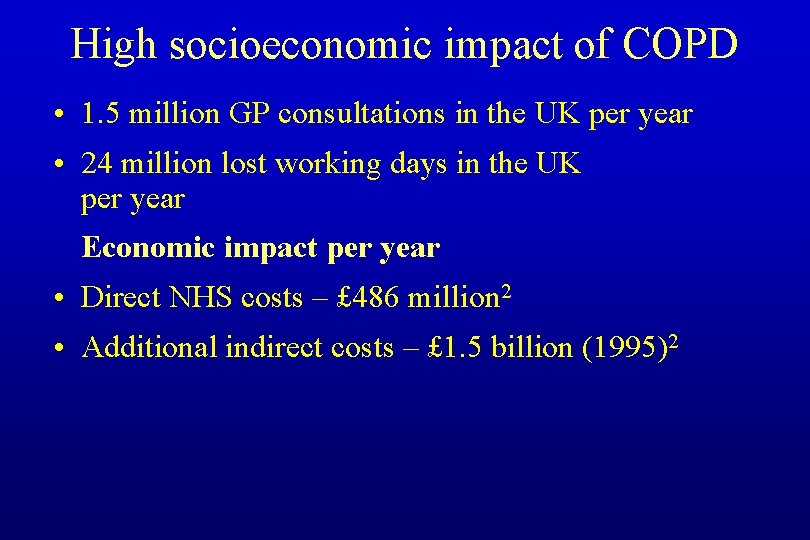
High socioeconomic impact of COPD • 1. 5 million GP consultations in the UK per year • 24 million lost working days in the UK per year Economic impact per year • Direct NHS costs – £ 486 million 2 • Additional indirect costs – £ 1. 5 billion (1995)2
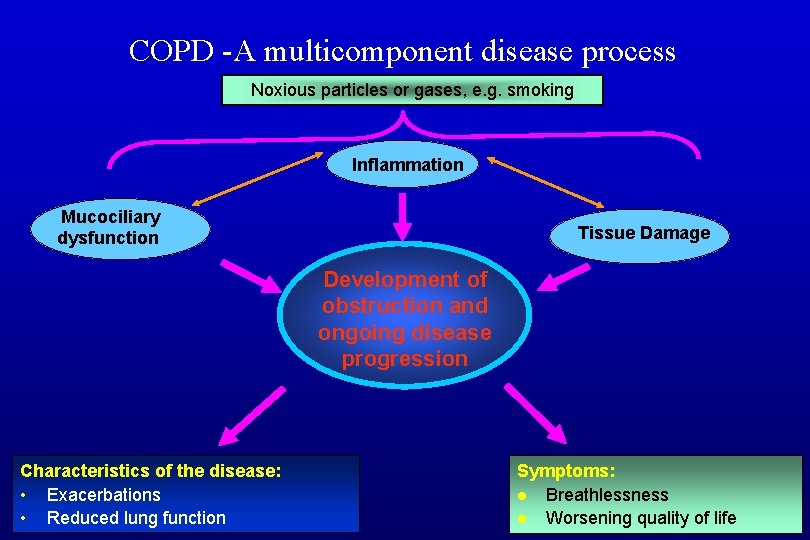
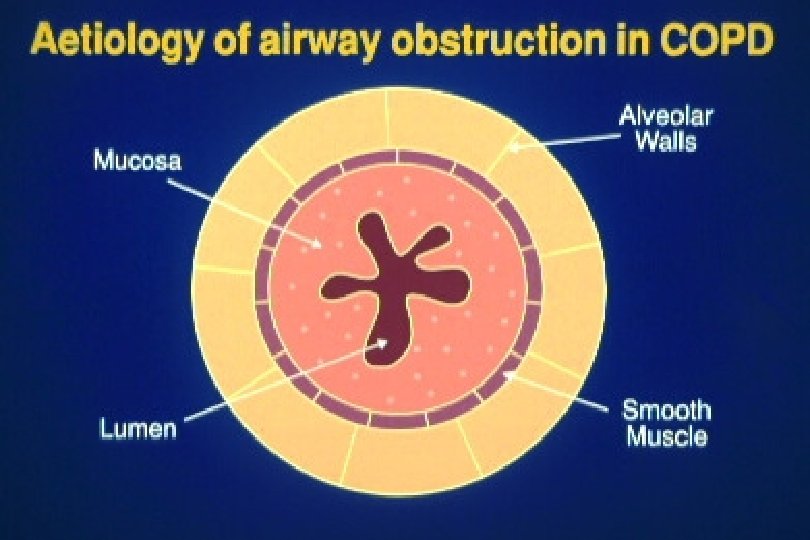
COPD -A multicomponent disease process Noxious particles or gases, e. g. smoking Inflammation Mucociliary dysfunction Tissue Damage Development of obstruction and ongoing disease progression Characteristics of the disease: • Exacerbations • Reduced lung function Symptoms: l Breathlessness l Worsening quality of life
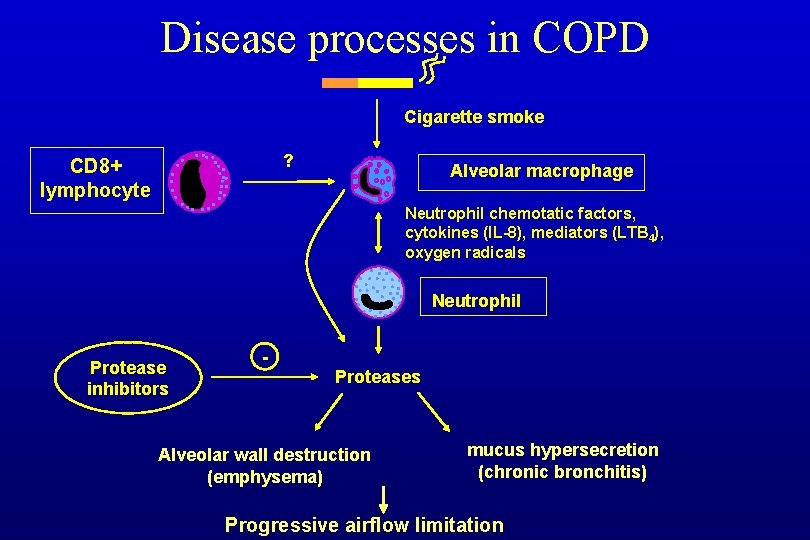
Disease processes in COPD Cigarette smoke ? CD 8+ lymphocyte Alveolar macrophage Neutrophil chemotatic factors, cytokines (IL-8), mediators (LTB 4), oxygen radicals Neutrophil Protease inhibitors - Proteases Alveolar wall destruction (emphysema) mucus hypersecretion (chronic bronchitis) Progressive airflow limitation
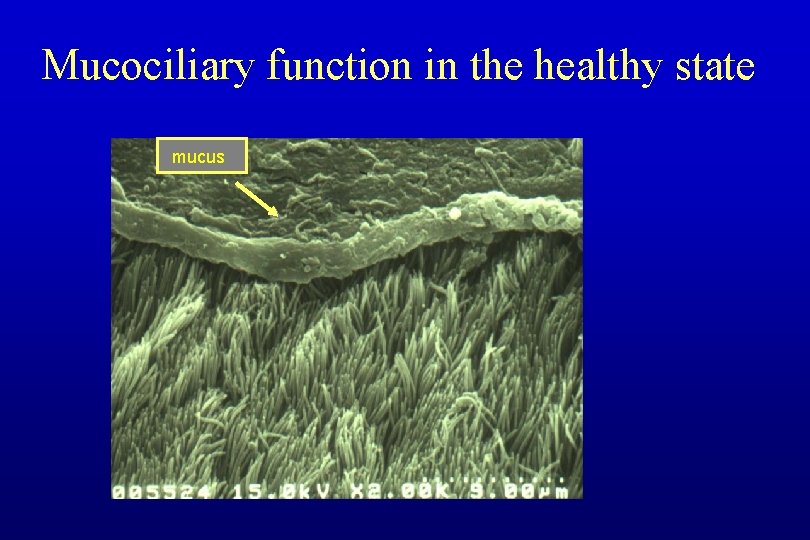
Mucociliary function in the healthy state mucus
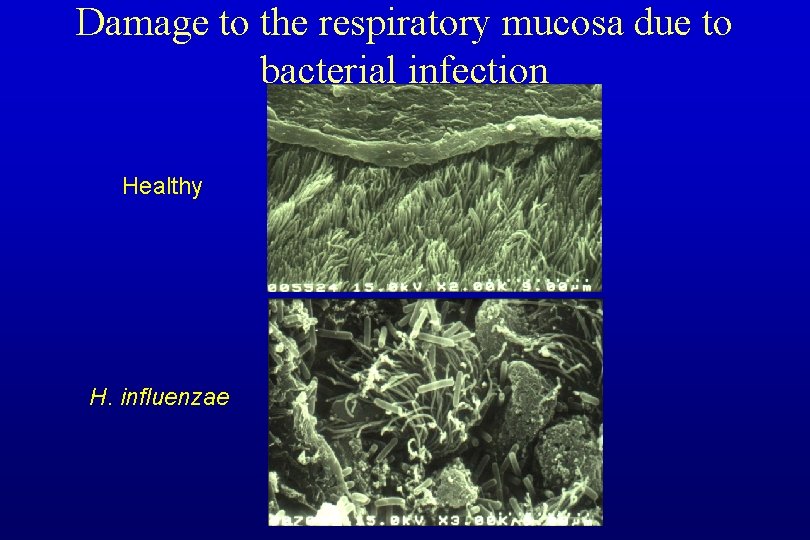
Damage to the respiratory mucosa due to bacterial infection Healthy H. influenzae
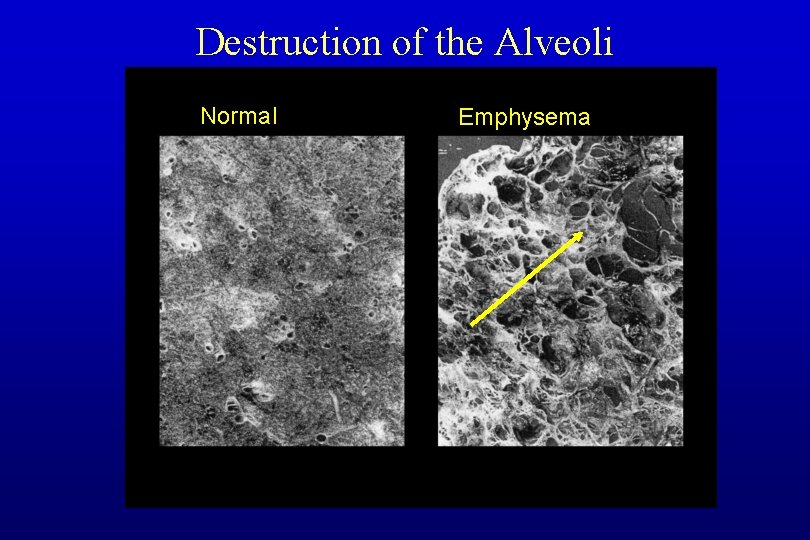
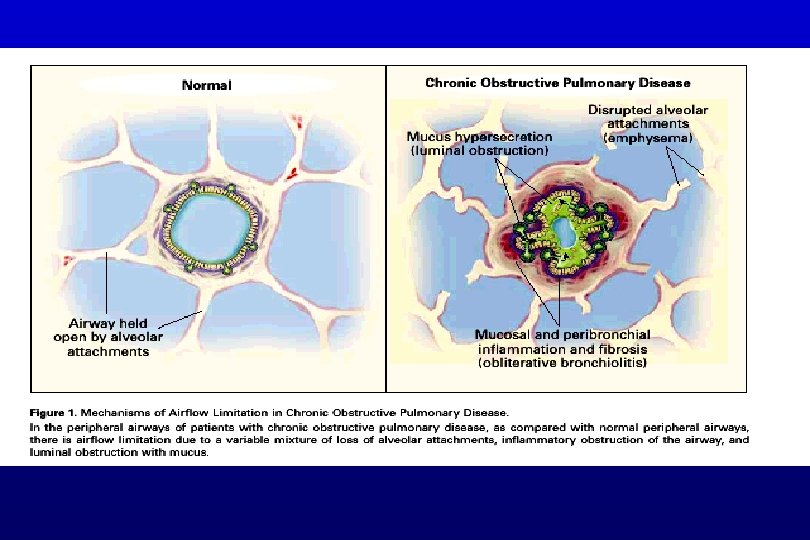
Destruction of the Alveoli Normal Emphysema
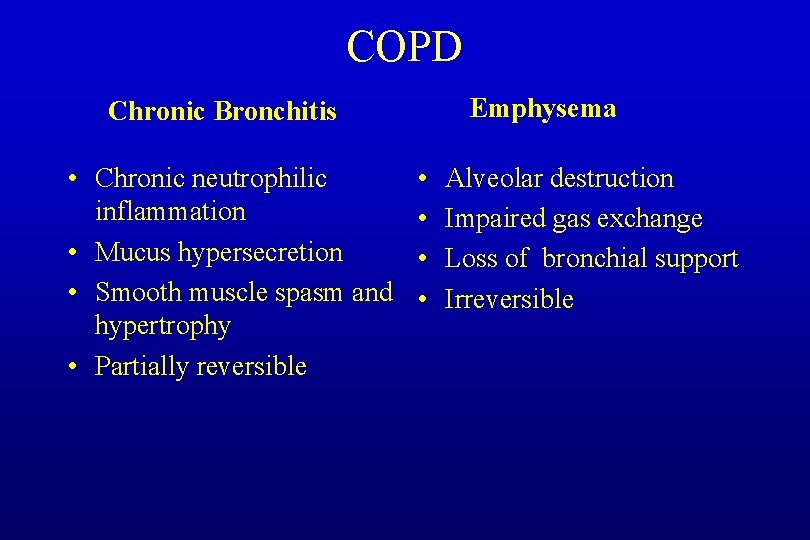
COPD Emphysema Chronic Bronchitis • Chronic neutrophilic inflammation • Mucus hypersecretion • Smooth muscle spasm and hypertrophy • Partially reversible • • Alveolar destruction Impaired gas exchange Loss of bronchial support Irreversible
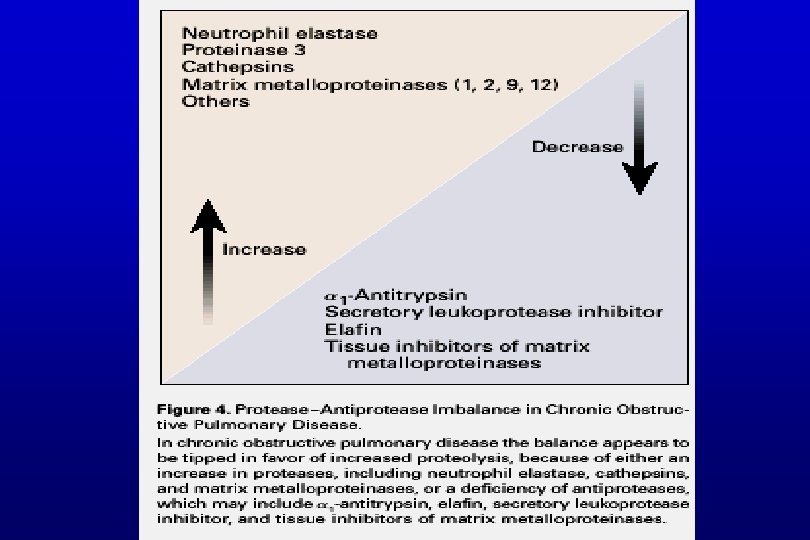
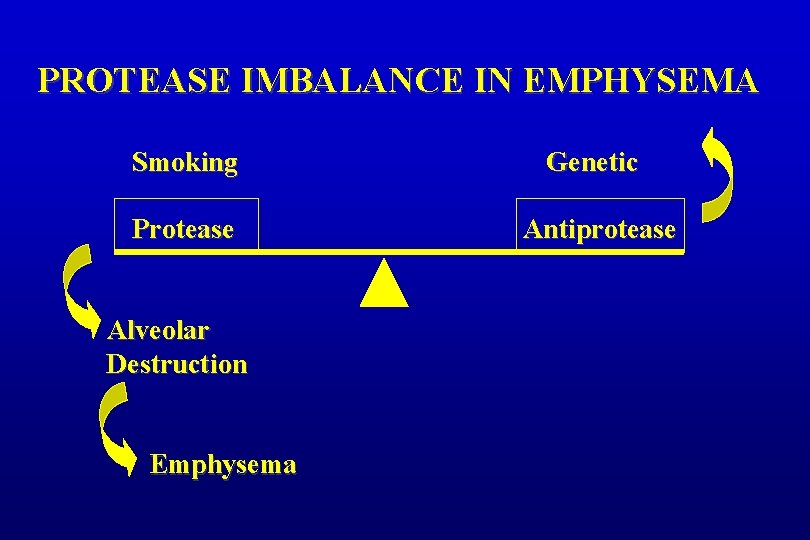
PROTEASE IMBALANCE IN EMPHYSEMA Smoking Genetic Protease Antiprotease Alveolar Destruction Emphysema
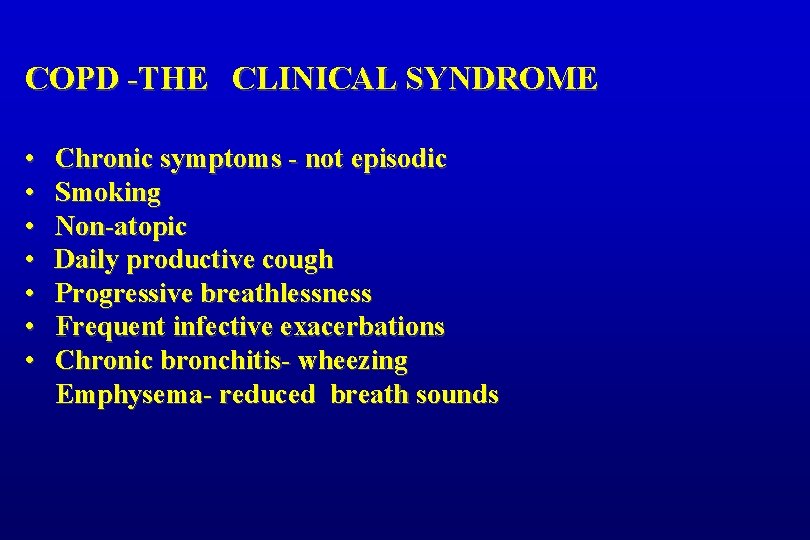
COPD -THE CLINICAL SYNDROME • • Chronic symptoms - not episodic Smoking Non-atopic Daily productive cough Progressive breathlessness Frequent infective exacerbations Chronic bronchitis- wheezing Emphysema- reduced breath sounds
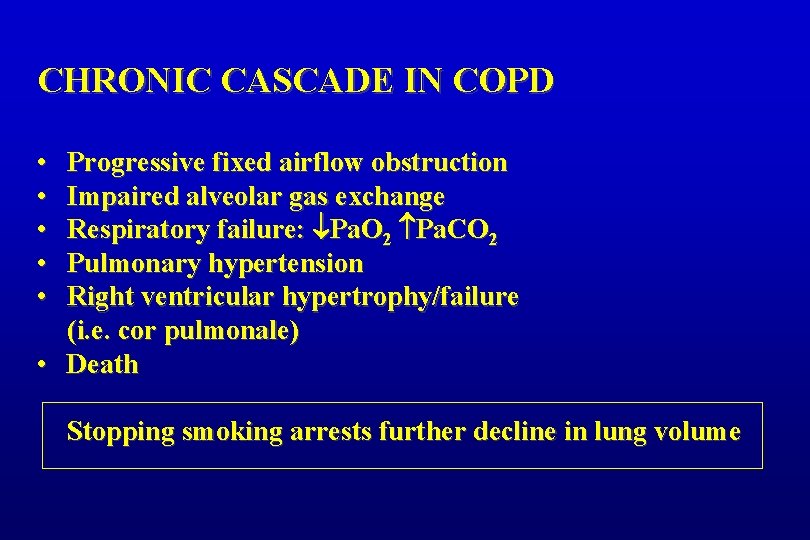
CHRONIC CASCADE IN COPD • • • Progressive fixed airflow obstruction Impaired alveolar gas exchange Respiratory failure: Pa. O 2 Pa. CO 2 Pulmonary hypertension Right ventricular hypertrophy/failure (i. e. cor pulmonale) • Death Stopping smoking arrests further decline in lung volume
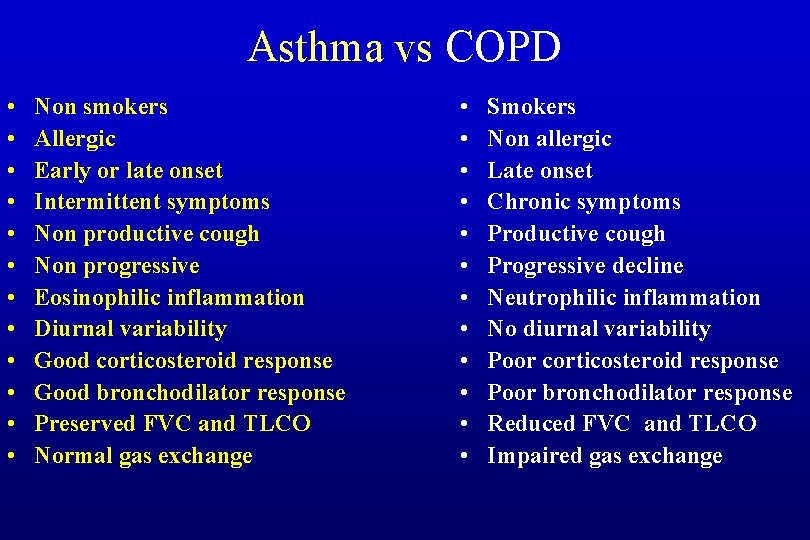
Asthma vs COPD • • • Non smokers Allergic Early or late onset Intermittent symptoms Non productive cough Non progressive Eosinophilic inflammation Diurnal variability Good corticosteroid response Good bronchodilator response Preserved FVC and TLCO Normal gas exchange • • • Smokers Non allergic Late onset Chronic symptoms Productive cough Progressive decline Neutrophilic inflammation No diurnal variability Poor corticosteroid response Poor bronchodilator response Reduced FVC and TLCO Impaired gas exchange
- Slides: 29