Obstructed Labor Obstructed labour Definition defined as labor
Obstructed Labor
Obstructed labour ►Definition : defined as labor where there is poor or no progress of labor in spite of good uterine contraction! ►Incidence : - 1 -2% of cases in developing country
Causes ►Maternal condition (fault in the passage): 1. Contracted pelvis 2. Abnormal pelvis: android, anthropoid 3. Pelvic tumor: fibroid, ovarian tumor 4. Tumor of rectum, bladder or pelvic bone 5. Abnormality in uterus & vagina: scarring in cervix, vaginal septum, rigid perineum
fetal causes Big baby Big head, hydrocephalus Deflexed head, brow and face mentoposterior. Oblique or transverse lie
Diagnosis ►Partogram will recognize impending obstruction of labor ►Careful general, abdominal and vaginal examination can detect if labor is slow or no progress
General examination: Features of maternal distress Dehydration Tachycardia >100/m Raise temperature Scanty urine
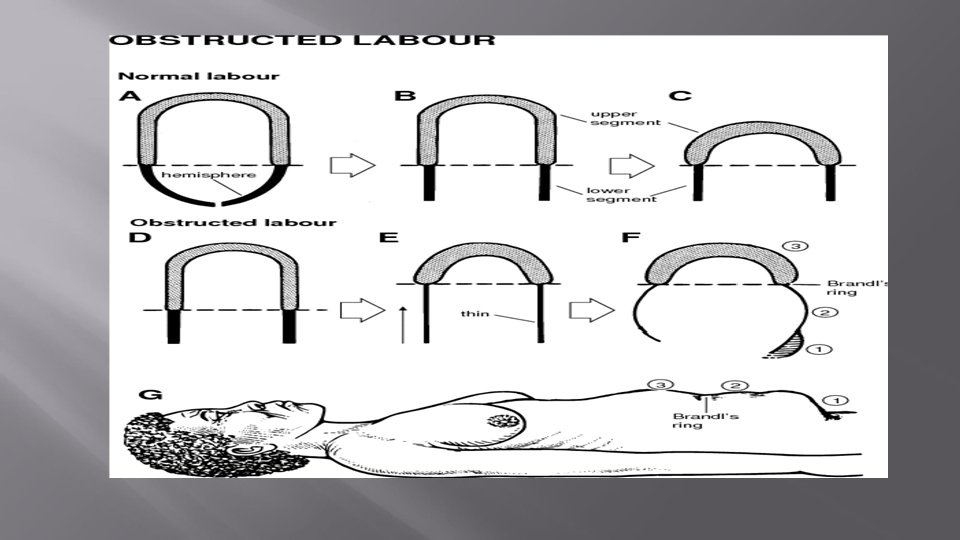
Abdominal examination : -The retraction ring might appear and felt between the tonic contracted upper segment of the uterus and the distended lower segment - Distended urinary bladder
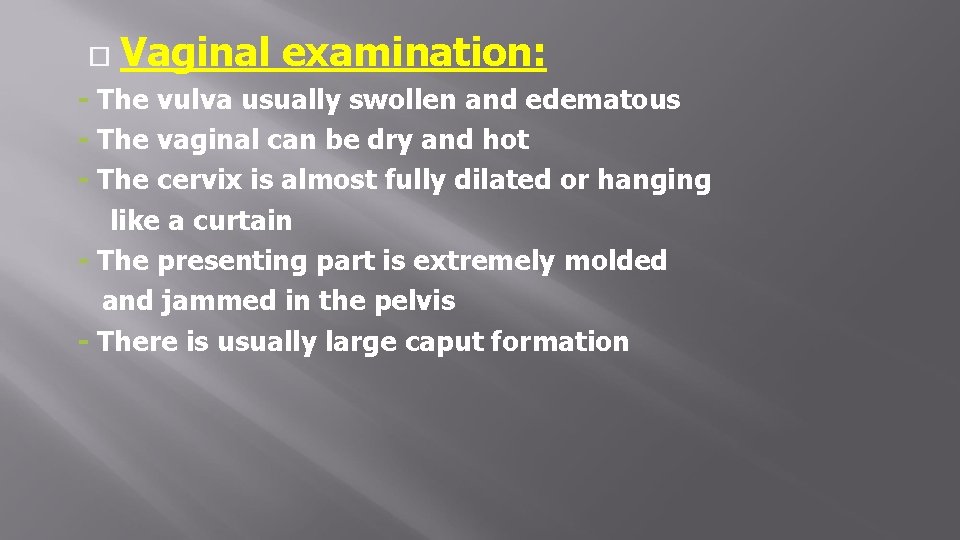
Vaginal examination: - The vulva usually swollen and edematous - The vaginal can be dry and hot - The cervix is almost fully dilated or hanging like a curtain - The presenting part is extremely molded and jammed in the pelvis - There is usually large caput formation
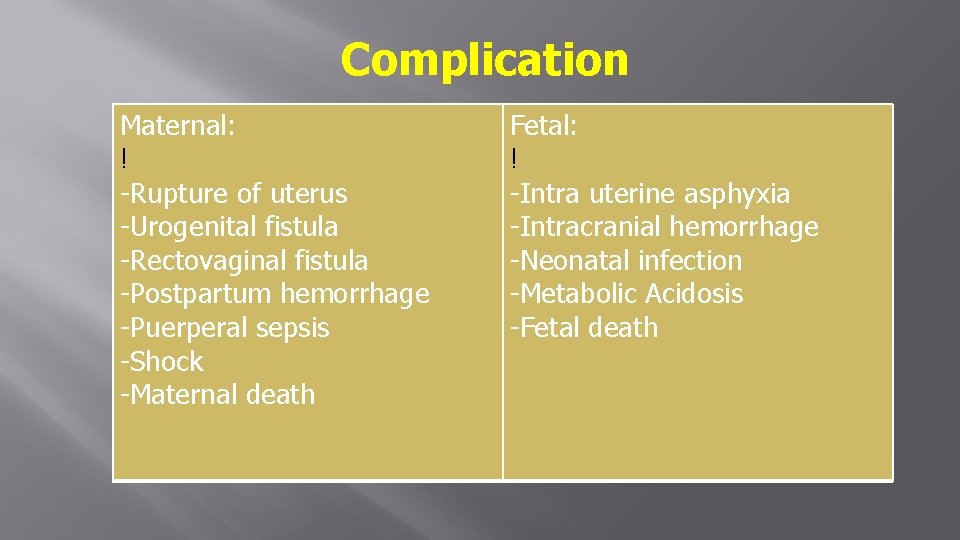
Complication Maternal: ! -Rupture of uterus -Urogenital fistula -Rectovaginal fistula -Postpartum hemorrhage -Puerperal sepsis -Shock -Maternal death Fetal: ! -Intra uterine asphyxia -Intracranial hemorrhage -Neonatal infection -Metabolic Acidosis -Fetal death
Management ►Preventive: - Proper assessment of pregnant woman during ANC - Regular ANC visit - Proper assessment in early labor to - Use of Partogram - Prompt and appropriate treatment
Obstetric Management 1. Delivery of fetus: a. Vaginal delivery: if head is low and vaginal delivery is not risky, forceps extraction may be done b. Caesarean section: 2. Active management of 3 rd stage of labor 3. Continuous bladder drainage for 2 -3 days to prevent any urogenital fistula
- Slides: 12