OBSTETRICS EMERGENCY Fetal Shoulder dystocia Umbilical cord prolapse
OBSTETRICS EMERGENCY

Fetal • Shoulder dystocia • Umbilical cord prolapse • Vasa Previa Maternal • Eclampsia • PPH • Amniotic fluid embolism
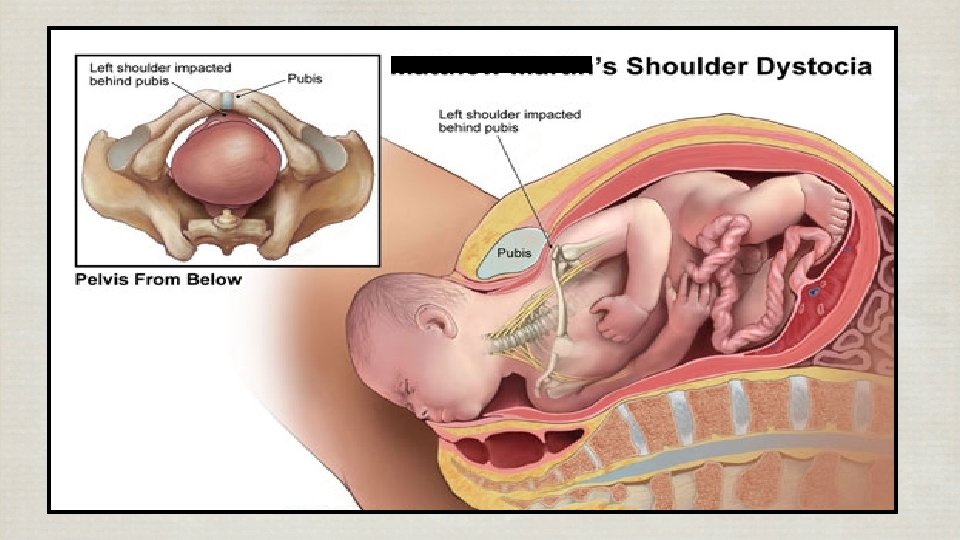
Shoulder dystocia • 0. 2 – 3. 0% of vaginal deliveries • Head – to – body times of more than 60 seconds • Unpredictable
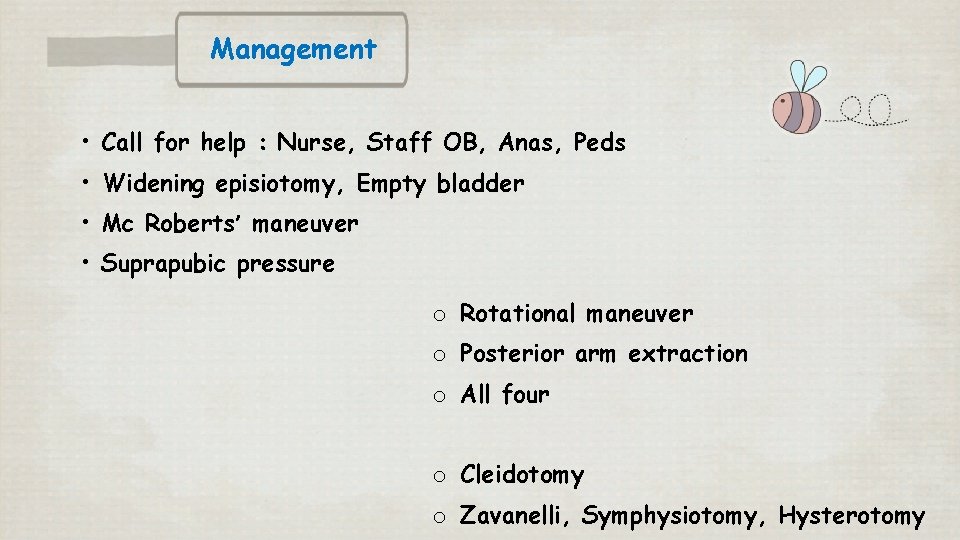
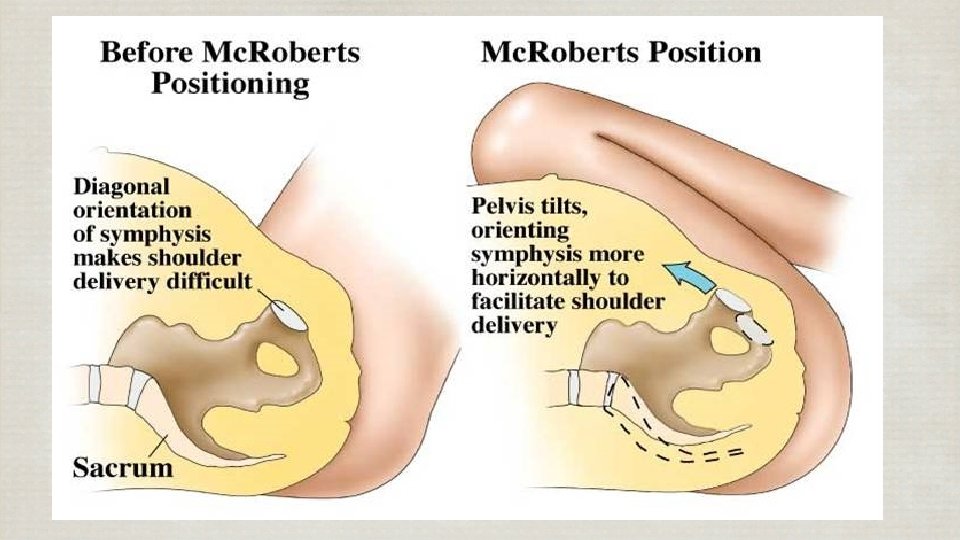
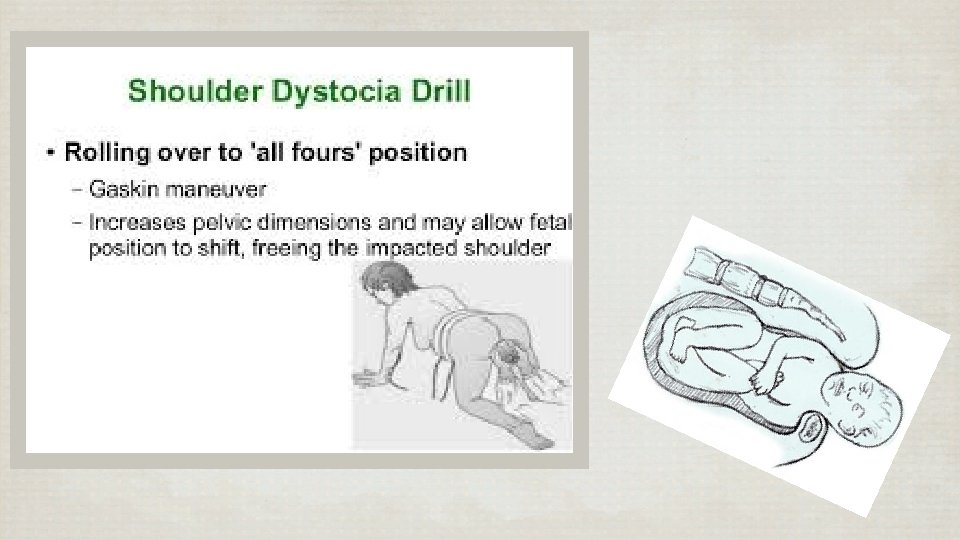
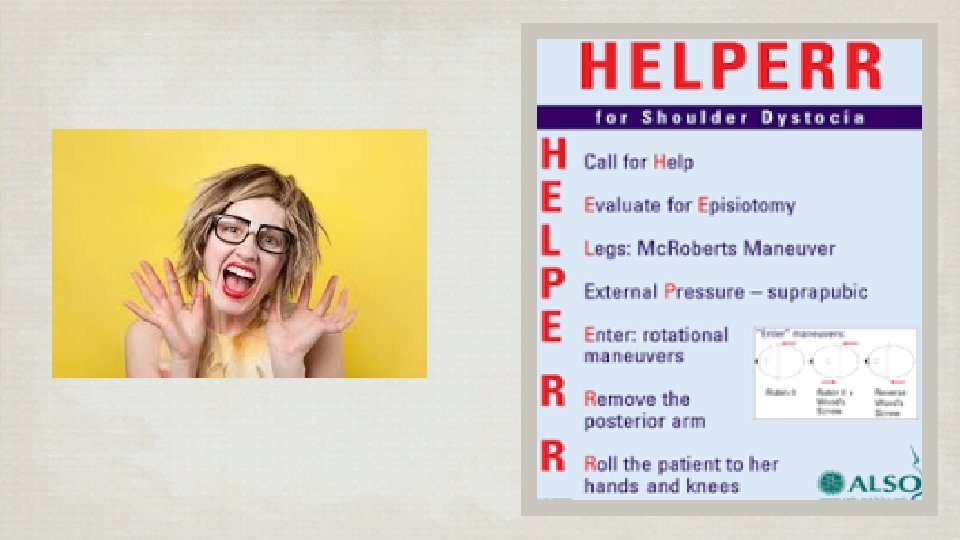
Management • Call for help : Nurse, Staff OB, Anas, Peds • Widening episiotomy, Empty bladder • Mc Roberts’ maneuver • Suprapubic pressure o Rotational maneuver o Posterior arm extraction o All four o Cleidotomy o Zavanelli, Symphysiotomy, Hysterotomy
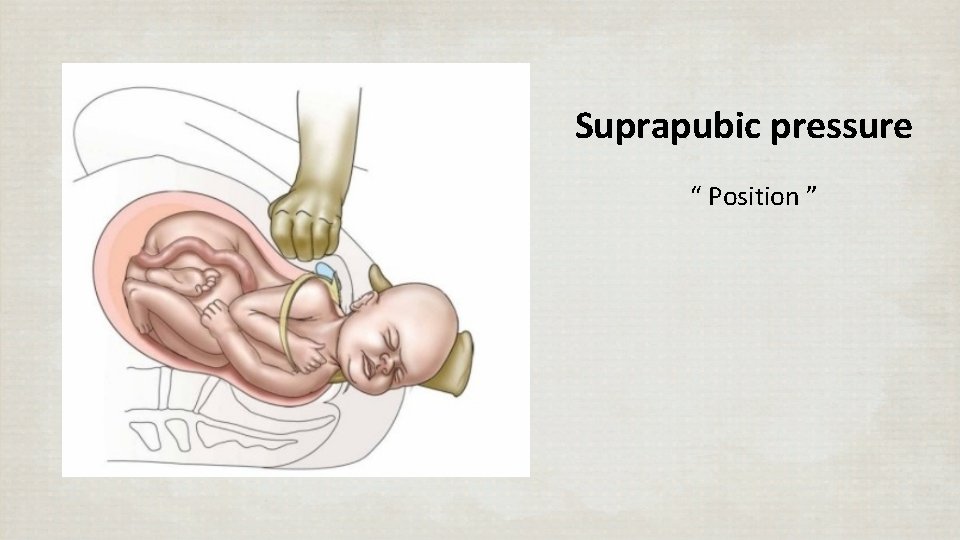
Suprapubic pressure “ Position ”
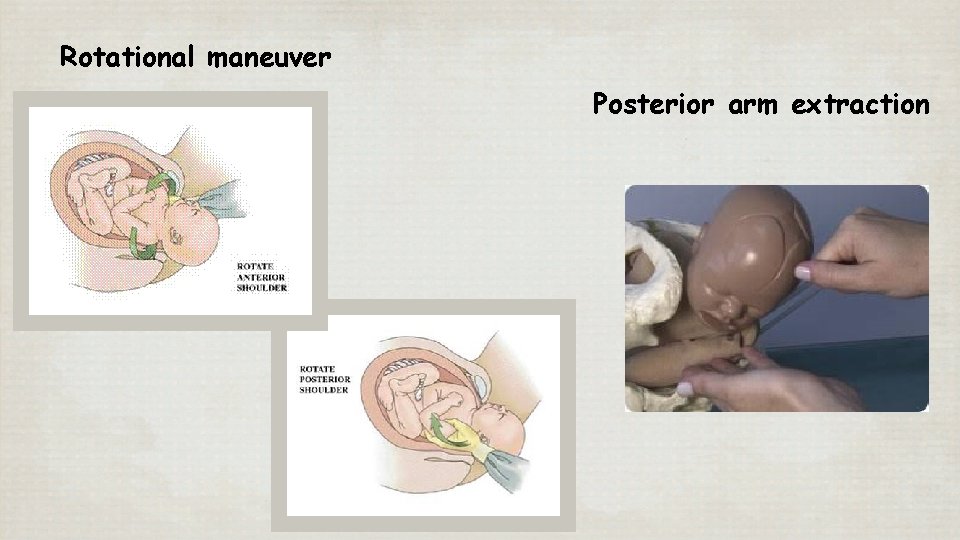
Rotational maneuver Posterior arm extraction
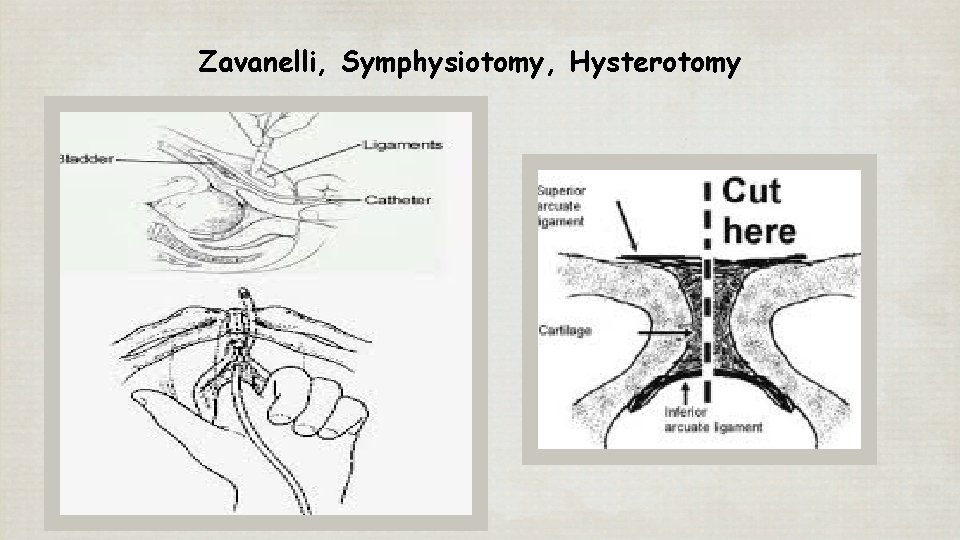
Zavanelli, Symphysiotomy, Hysterotomy
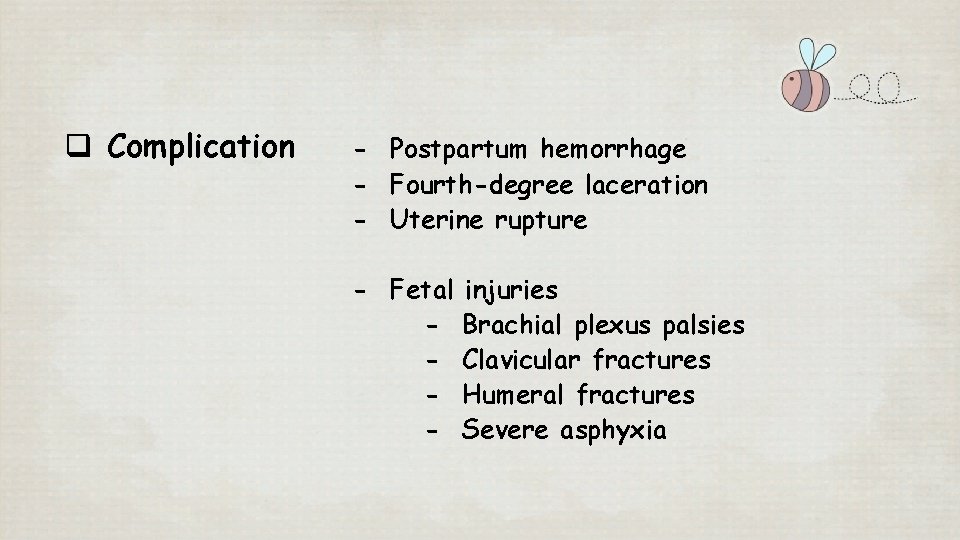
q Complication - Postpartum hemorrhage - Fourth-degree laceration - Uterine rupture - Fetal - injuries Brachial plexus palsies Clavicular fractures Humeral fractures Severe asphyxia
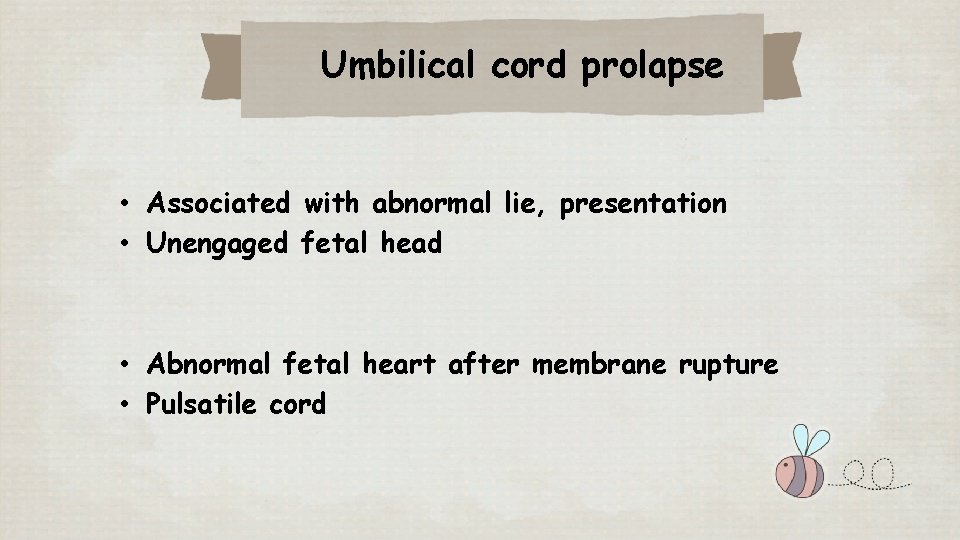
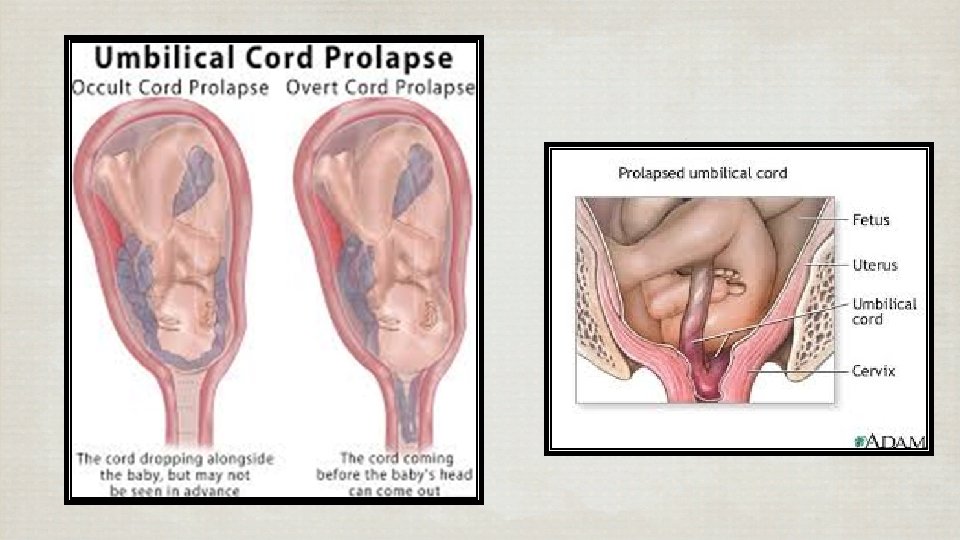
Umbilical cord prolapse • Associated with abnormal lie, presentation • Unengaged fetal head • Abnormal fetal heart after membrane rupture • Pulsatile cord
Management • Call for help : Nurse, Staff OB, Anas, Peds • Emergency Cesarean section for alive fetus • Counselling
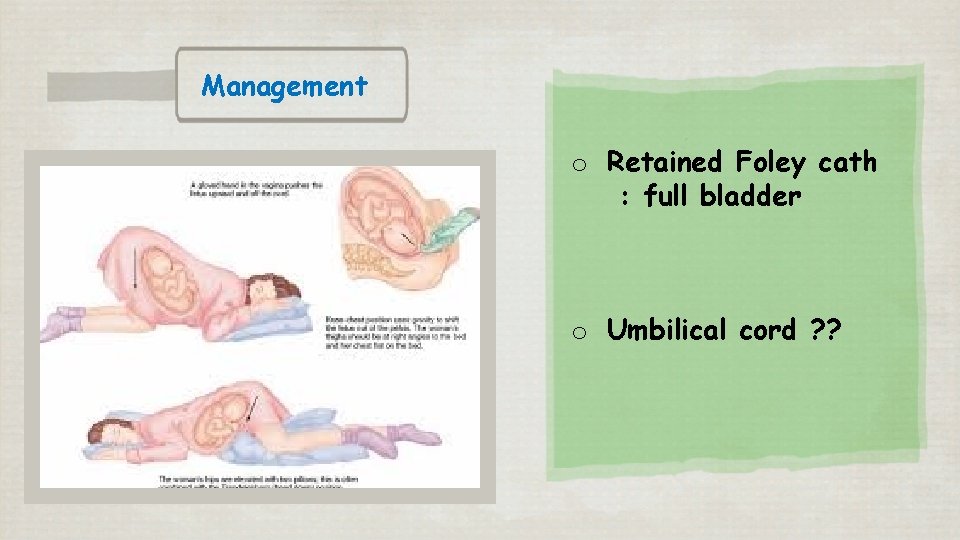
Management o Retained Foley cath : full bladder o Umbilical cord ? ?
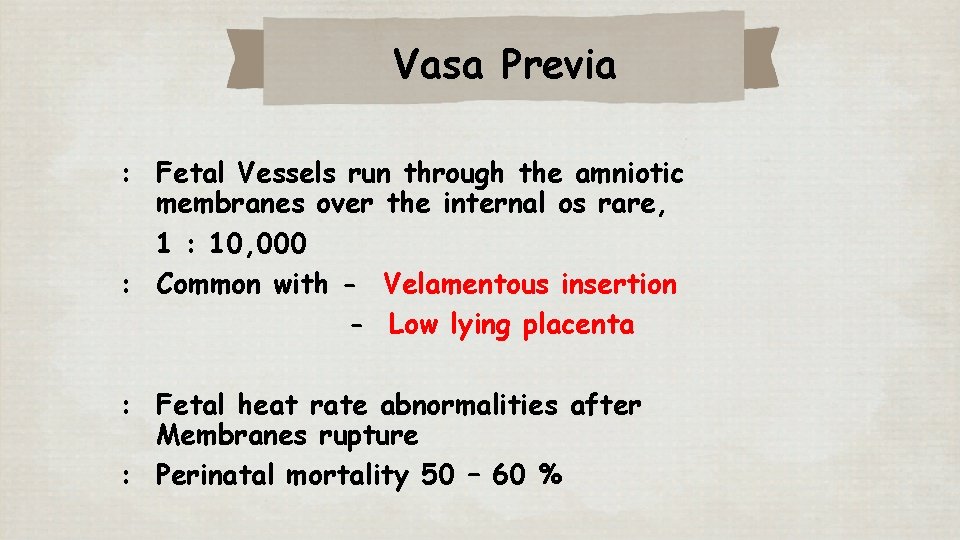
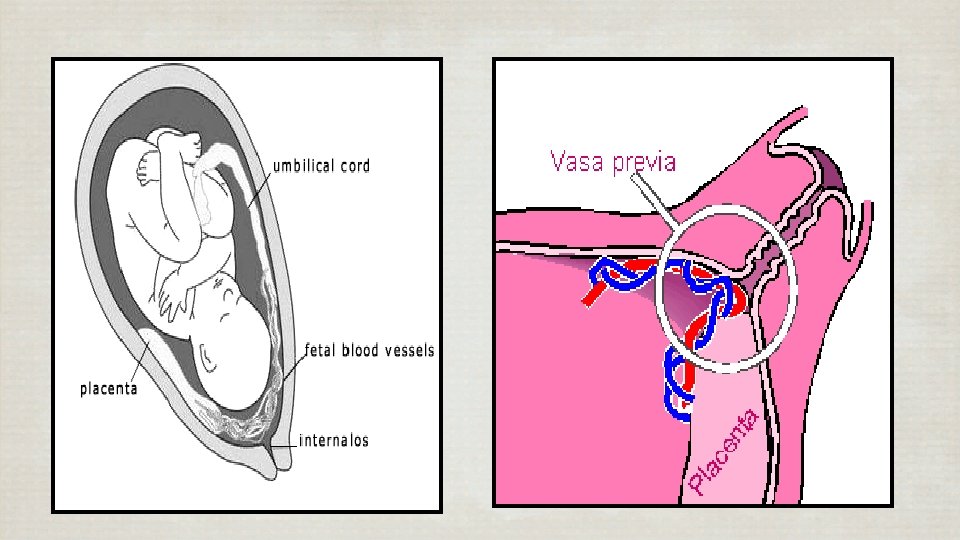
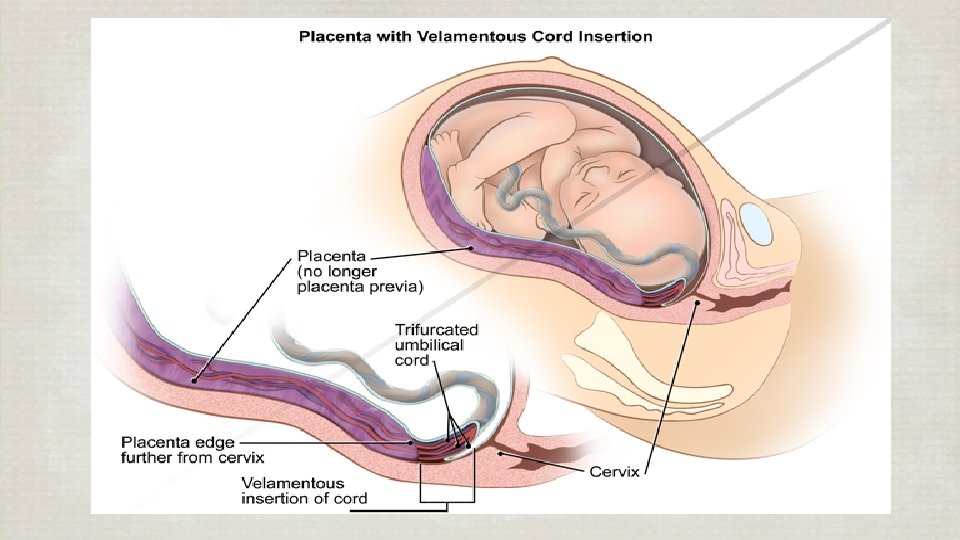
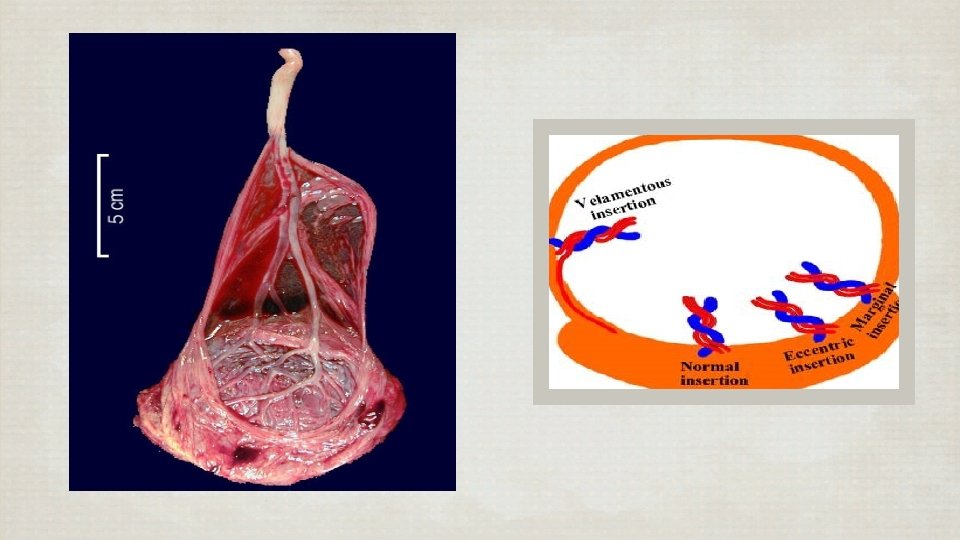
Vasa Previa : Fetal Vessels run through the amniotic membranes over the internal os rare, 1 : 10, 000 : Common with - Velamentous insertion - Low lying placenta : Fetal heat rate abnormalities after Membranes rupture : Perinatal mortality 50 – 60 %
Management v Early detection v In viable fetus - Emergency Cesarean section - Short second stage v G/M PCR group O low-titer
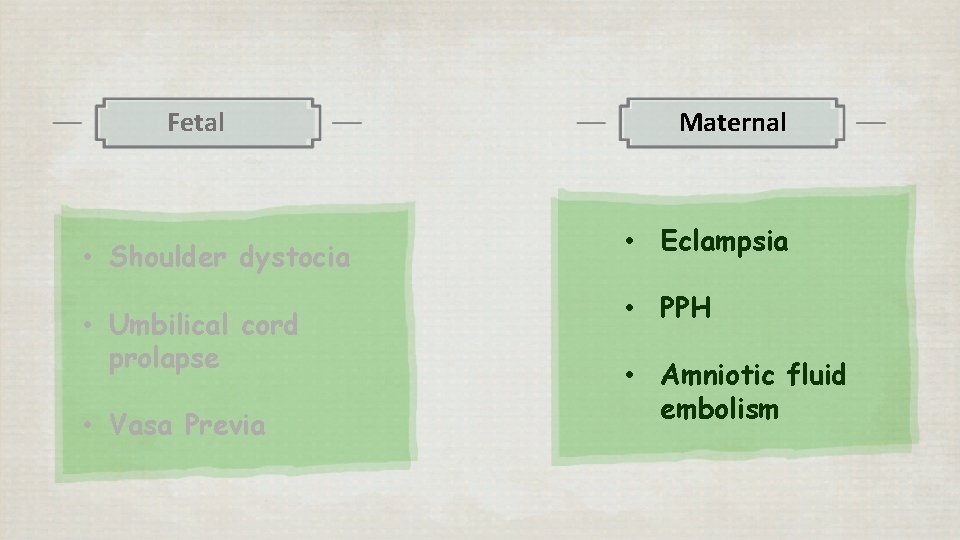
Fetal • Shoulder dystocia • Umbilical cord prolapse • Vasa Previa Maternal • Eclampsia • PPH • Amniotic fluid embolism
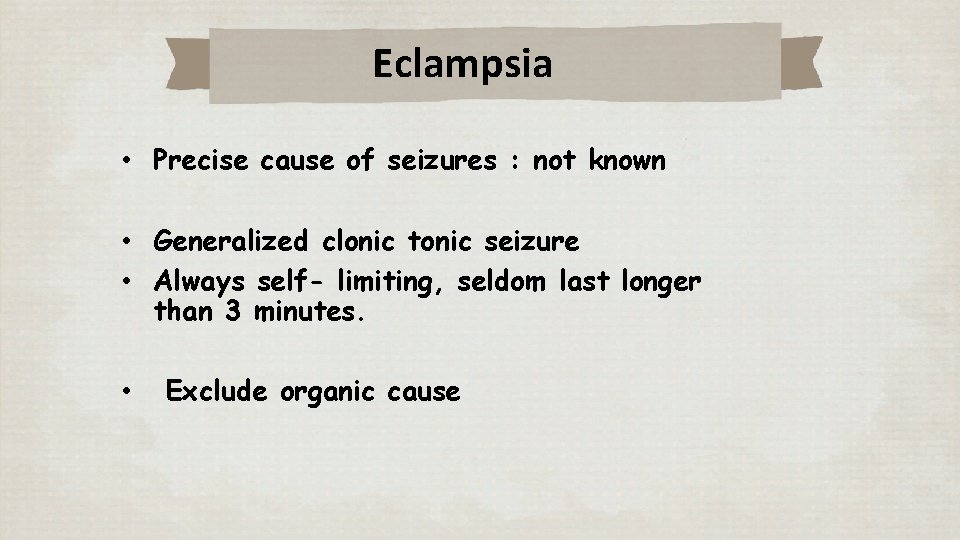
Eclampsia • Precise cause of seizures : not known • Generalized clonic tonic seizure • Always self- limiting, seldom last longer than 3 minutes. • Exclude organic cause
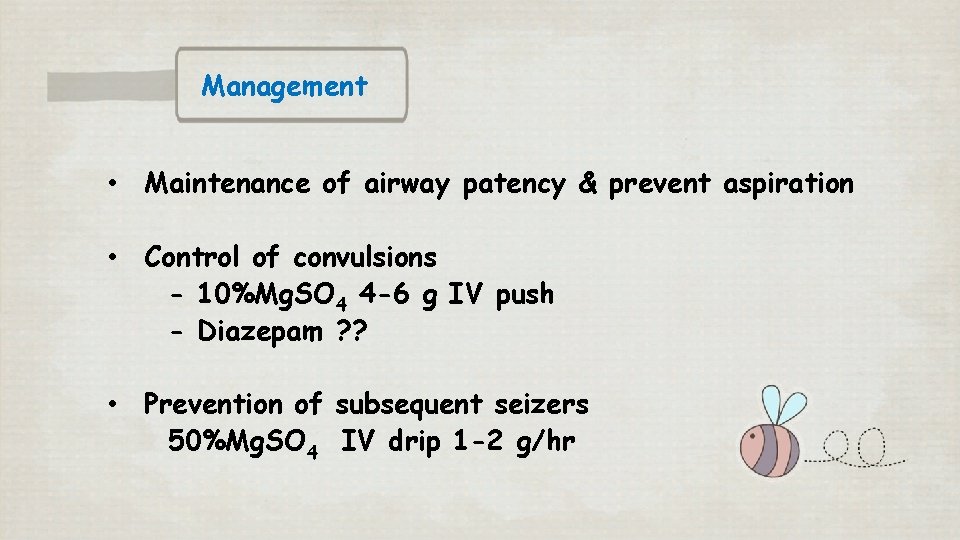
Management • Maintenance of airway patency & prevent aspiration • Control of convulsions - 10%Mg. SO 4 4 -6 g IV push - Diazepam ? ? • Prevention of subsequent seizers 50%Mg. SO 4 IV drip 1 -2 g/hr
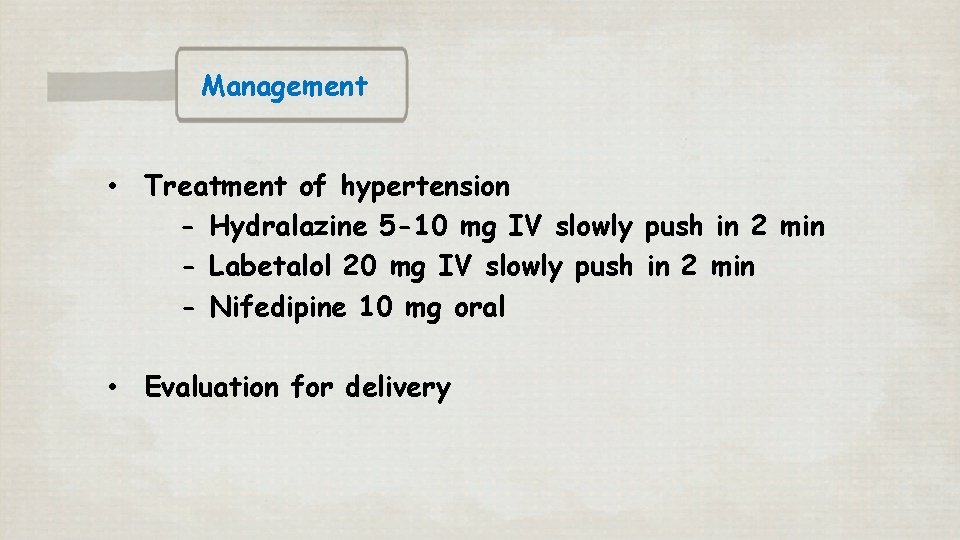
Management • Treatment of hypertension - Hydralazine 5 -10 mg IV slowly push in 2 min - Labetalol 20 mg IV slowly push in 2 min - Nifedipine 10 mg oral • Evaluation for delivery
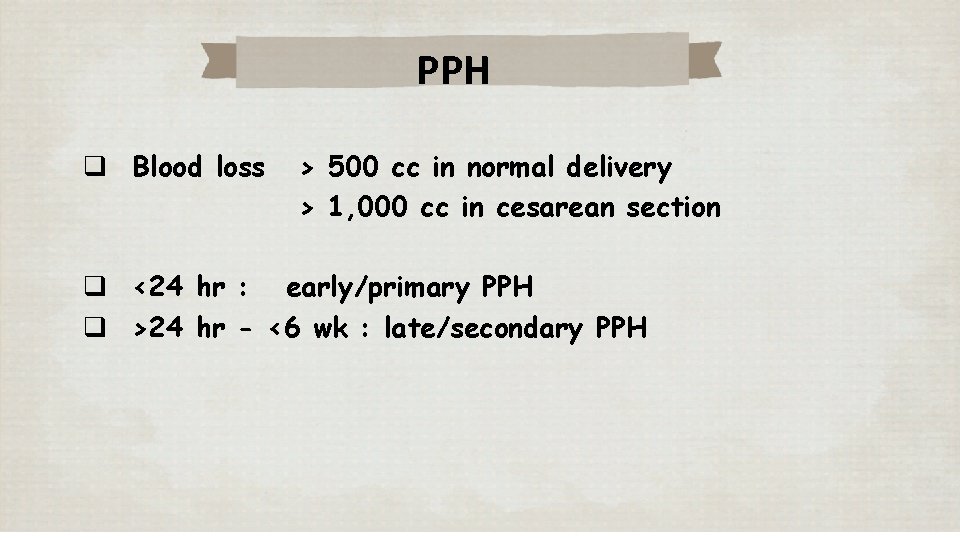
PPH q Blood loss > 500 cc in normal delivery > 1, 000 cc in cesarean section q <24 hr : early/primary PPH q >24 hr - <6 wk : late/secondary PPH
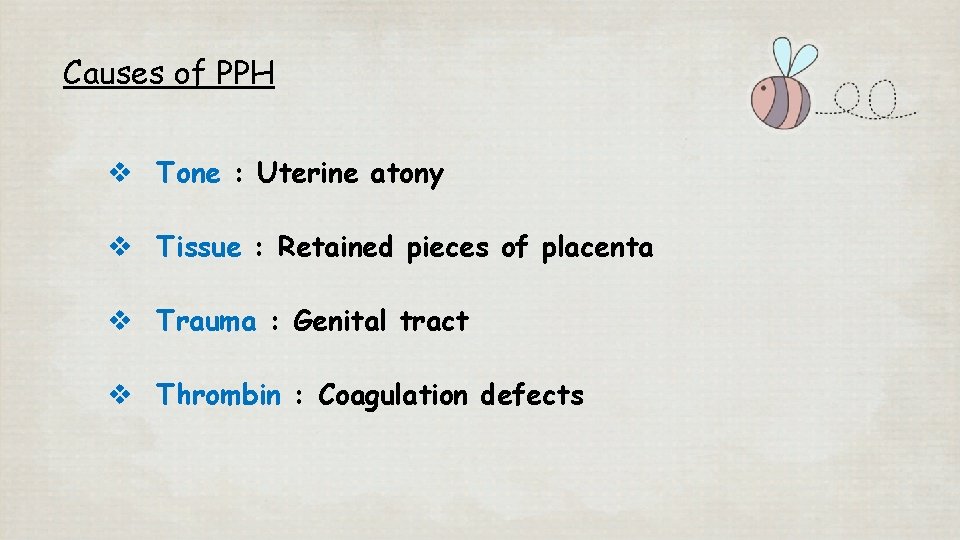
Causes of PPH v Tone : Uterine atony v Tissue : Retained pieces of placenta v Trauma : Genital tract v Thrombin : Coagulation defects
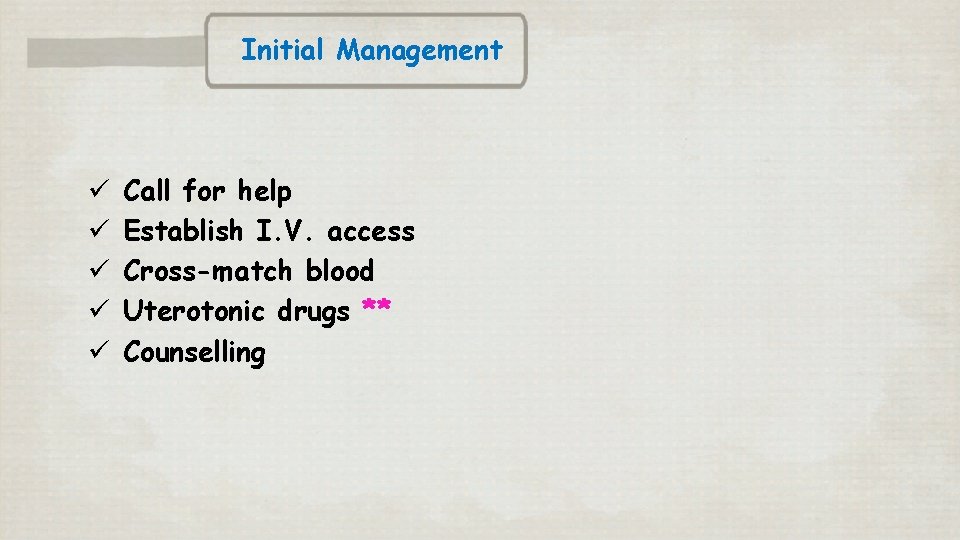
Initial Management ü ü ü Call for help Establish I. V. access Cross-match blood Uterotonic drugs ** Counselling
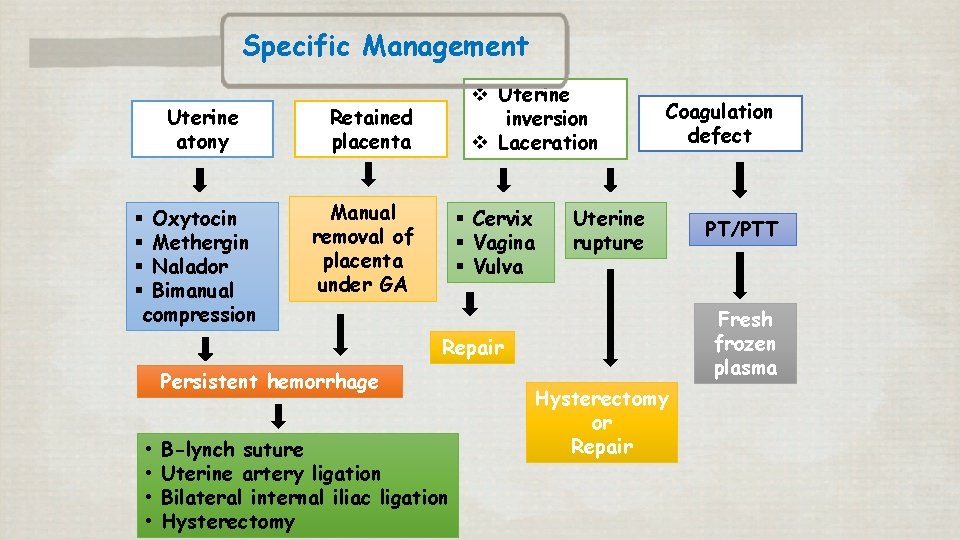
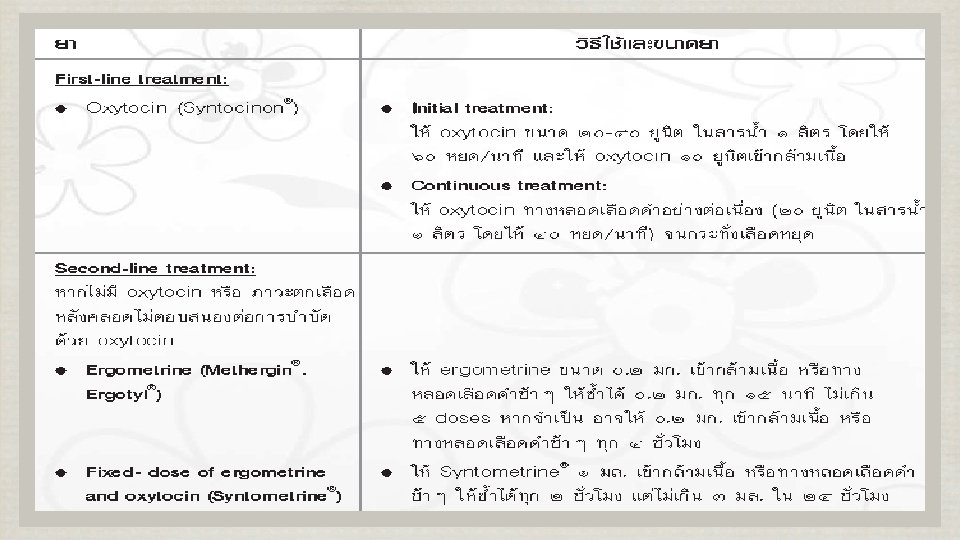
Specific Management Uterine atony § Oxytocin § Methergin § Nalador § Bimanual compression v Uterine inversion v Laceration Retained placenta Manual removal of placenta under GA § Cervix § Vagina § Vulva Coagulation defect Uterine rupture Fresh frozen plasma Repair Persistent hemorrhage • • B-lynch suture Uterine artery ligation Bilateral internal iliac ligation Hysterectomy PT/PTT Hysterectomy or Repair
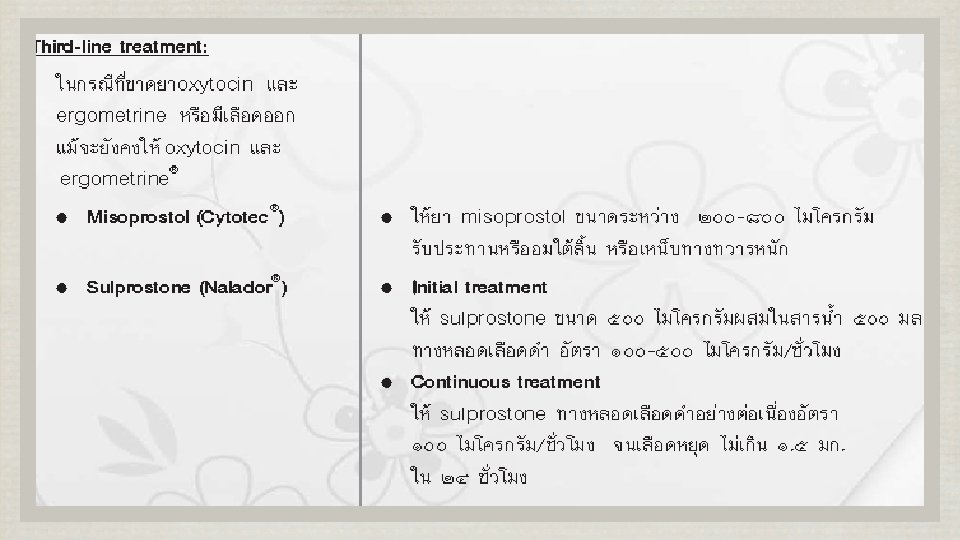
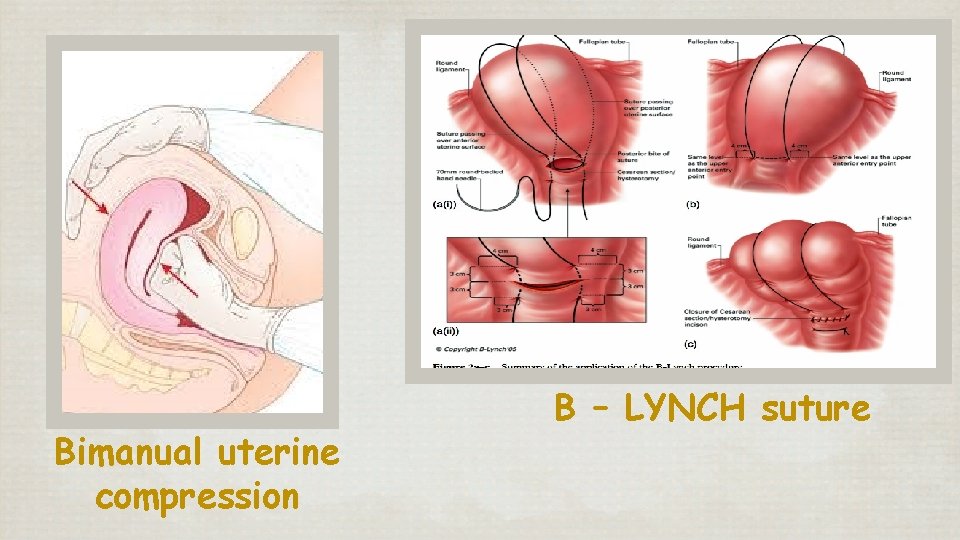
Bimanual uterine compression B – LYNCH suture
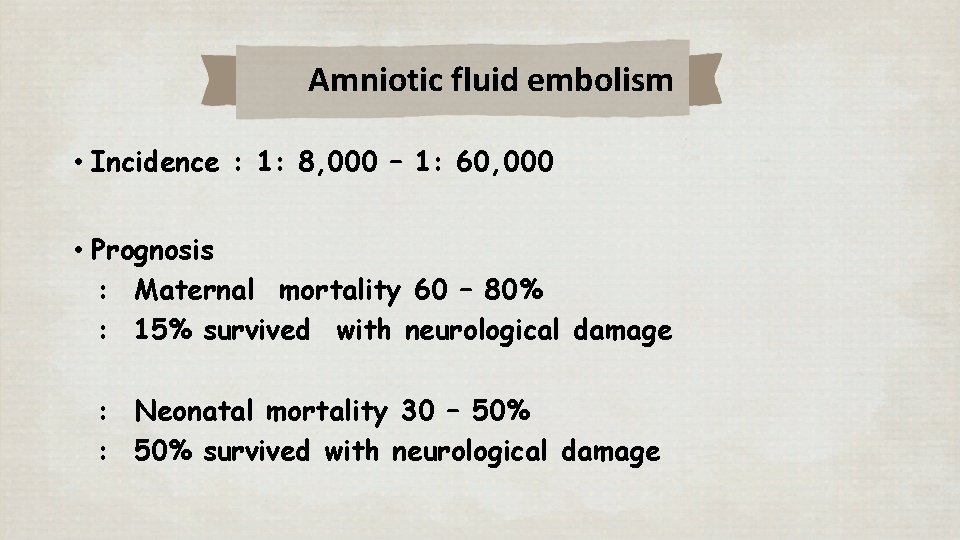
Amniotic fluid embolism • Incidence : 1: 8, 000 – 1: 60, 000 • Prognosis : Maternal mortality 60 – 80% : 15% survived with neurological damage : Neonatal mortality 30 – 50% : 50% survived with neurological damage
• Presentation usually sudden during labor or immediately postpartum • • • Acute dyspnea Shock Cyanosis Bleeding from DIC Tonic-clonic seizure Cardiac arrest
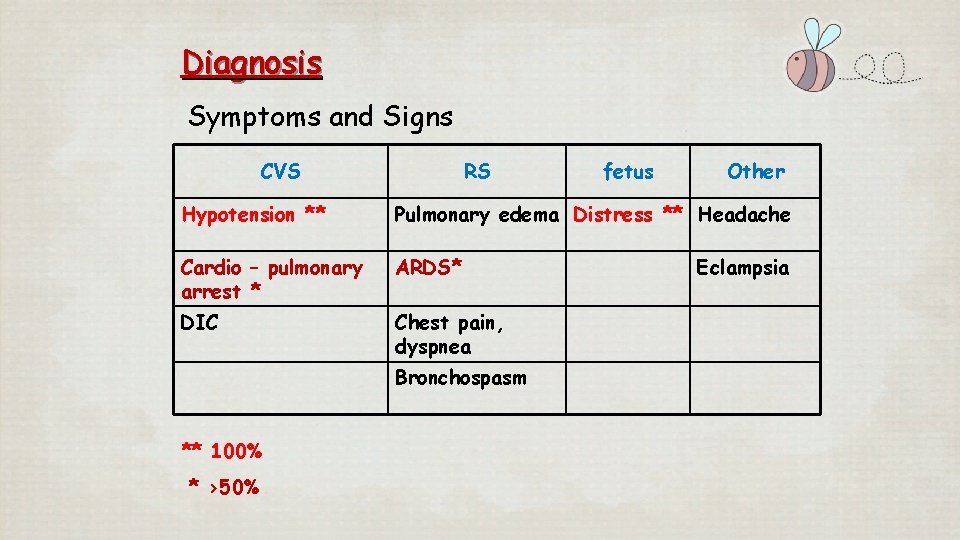
Diagnosis Symptoms and Signs CVS RS fetus Other Hypotension ** Pulmonary edema Distress ** Headache Cardio – pulmonary arrest * ARDS* DIC Chest pain, dyspnea Bronchospasm ** 100% * >50% Eclampsia
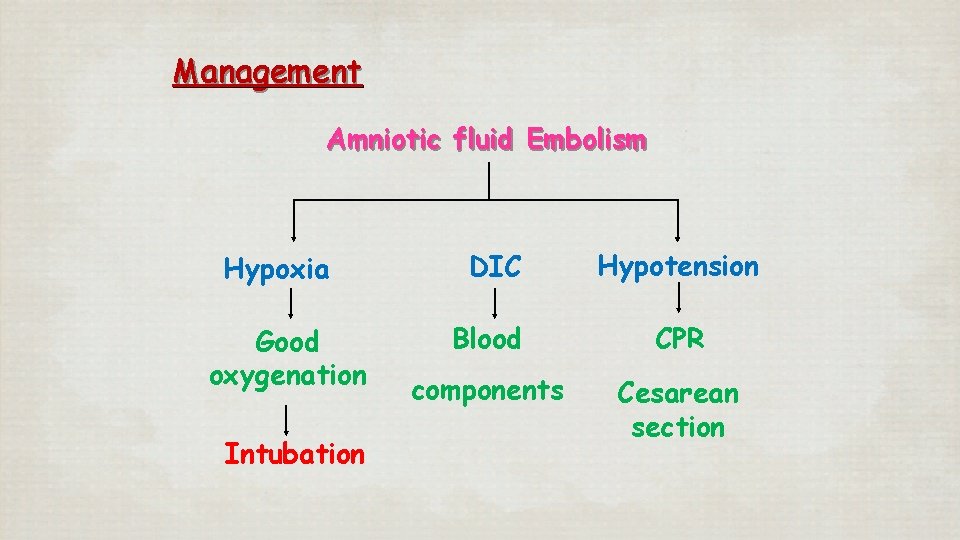
Management Amniotic fluid Embolism Hypoxia Good oxygenation Intubation DIC Hypotension Blood CPR components Cesarean section

- Slides: 37