Obstetrics 1 ANTENATAL PHASE 3 A Jonathan Borland
Obstetrics 1 – ANTENATAL PHASE 3 A Jonathan Borland & Rajiv Joshi The Peer Teaching Society is not liable for false or misleading information.
What we will cover tonight • • Antenatal screening – bloods, USS, Down’s syndrome etc Rhesus disease Infections Complications of pregnancy; – Miscarriages – Ectopic pregnancies – Molar pregnancies • Maternal disorders – especially pre-eclampsia and other hypertensive diseases • Obstetric shock – APH, disorders of the placenta, include PPH here

Antenatal Screening • Question 1: When is the first US scan performed and what does the obstetrician check for during this exam? • Question 2: What two tests are used to screen for the presence of Down’s syndrome?
Antenatal Screening • Question 1: Performed 11 -13 weeks. Checks for presence of foetus, number of foetuses, heartbeat, crown rump length, nuchal translucency, ovaries. • Question 2: Combined test and Quadruple test.
Antenatal Screening • Question 3: What are the 3 components of the combined test? • Question 4: What are the 4 components of the quadruple test?
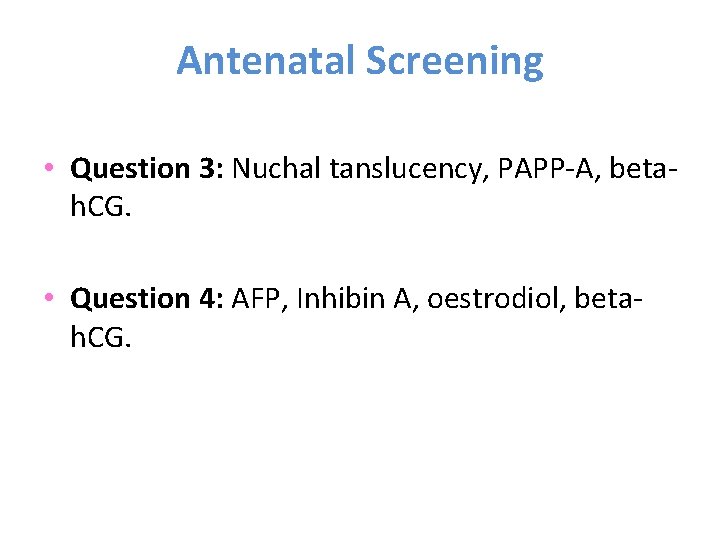
Antenatal Screening • Question 3: Nuchal tanslucency, PAPP-A, betah. CG. • Question 4: AFP, Inhibin A, oestrodiol, betah. CG.

Antenatal Screening • Question 5: If the test results of the combined / quadruple test come back as positive, what two invasive investigations can be used to definitively diagnose Down’s syndrome? • Question 6: What is the risk of miscarriage of each of these investigations?
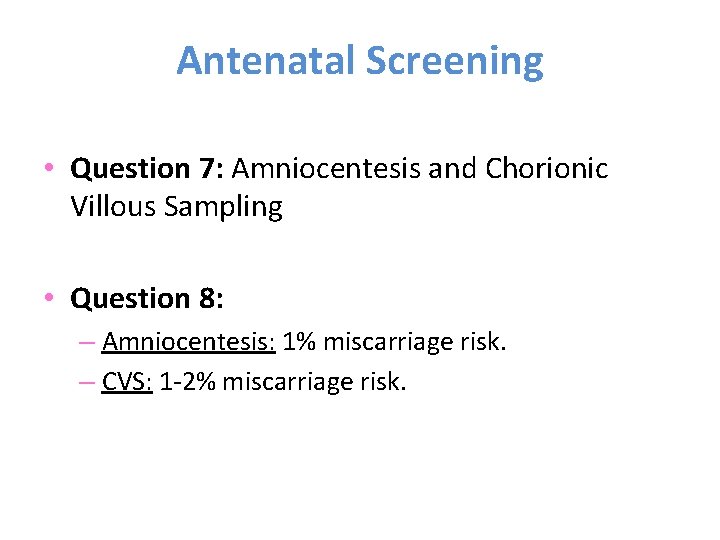
Antenatal Screening • Question 7: Amniocentesis and Chorionic Villous Sampling • Question 8: – Amniocentesis: 1% miscarriage risk. – CVS: 1 -2% miscarriage risk.
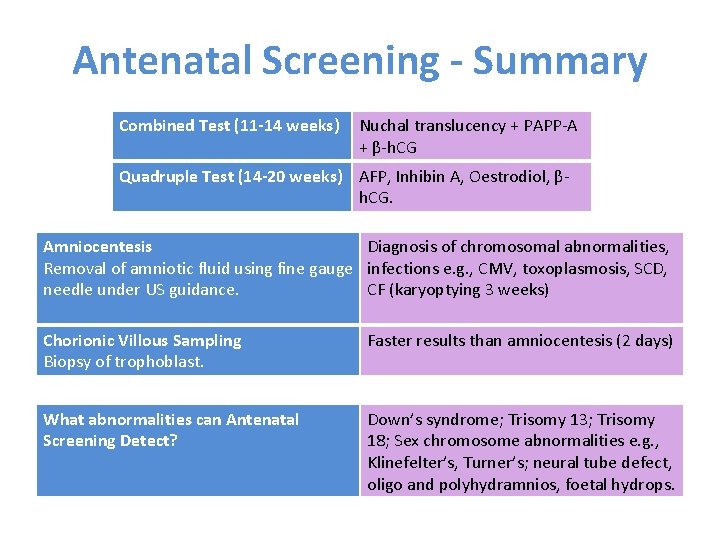
Antenatal Screening - Summary Combined Test (11 -14 weeks) Nuchal translucency + PAPP-A + β-h. CG Quadruple Test (14 -20 weeks) AFP, Inhibin A, Oestrodiol, βh. CG. Amniocentesis Diagnosis of chromosomal abnormalities, Removal of amniotic fluid using fine gauge infections e. g. , CMV, toxoplasmosis, SCD, needle under US guidance. CF (karyoptying 3 weeks) Chorionic Villous Sampling Biopsy of trophoblast. Faster results than amniocentesis (2 days) What abnormalities can Antenatal Screening Detect? Down’s syndrome; Trisomy 13; Trisomy 18; Sex chromosome abnormalities e. g. , Klinefelter’s, Turner’s; neural tube defect, oligo and polyhydramnios, foetal hydrops.
Miscarriage • Question 7: What is the definition of a miscarriage? • Question 8: Before what week do the majority of miscarriages occur? • Question 9: List the 6 types of miscarriage.
Miscarriage • Question 7: Foetus dies or delivers dead before 24 weeks. • Question 8: Majority occur before 12 weeks. • Question 9: Threatened, inevitable, incomplete, septic, missed.
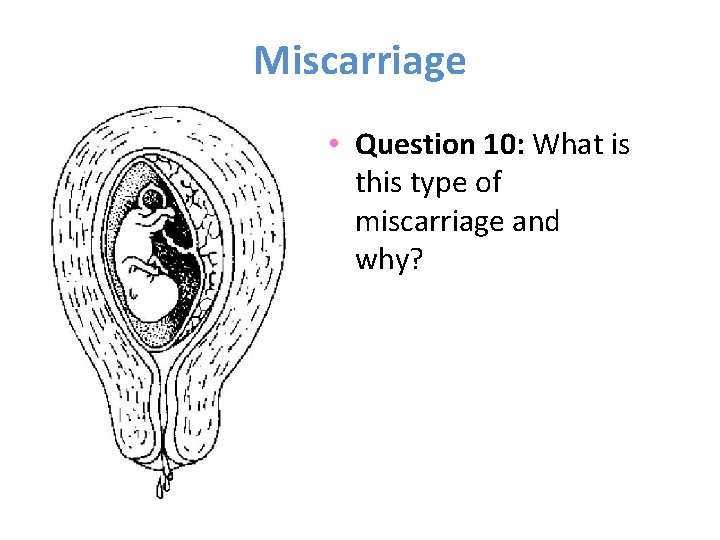
Miscarriage • Question 10: What is this type of miscarriage and why?
Miscarriage • Question 10: THREATENED. – PV Bleeding – Foetus still alive – Uterus is the size expected from the dates. – Os is closed. – 25% miscarry.
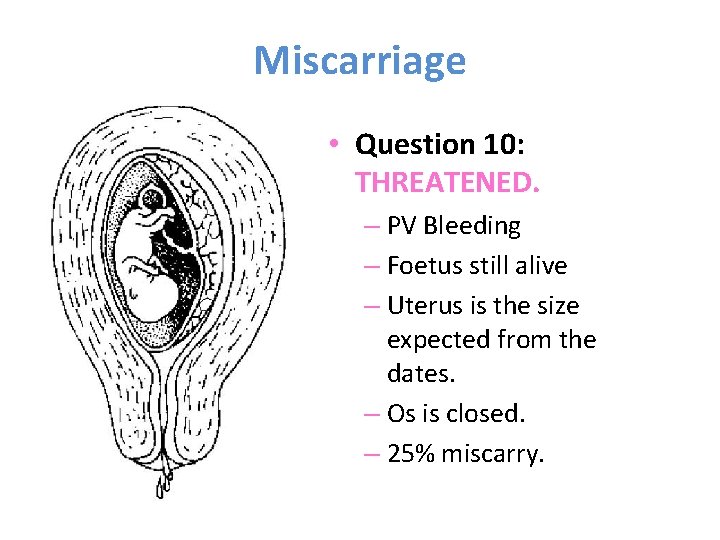
Miscarriage • Question 11: What is this type of miscarriage and why?
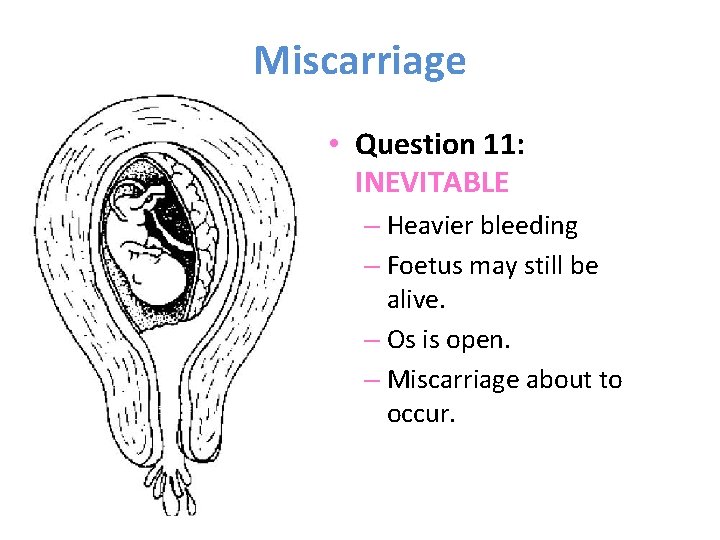
Miscarriage • Question 11: INEVITABLE – Heavier bleeding – Foetus may still be alive. – Os is open. – Miscarriage about to occur.
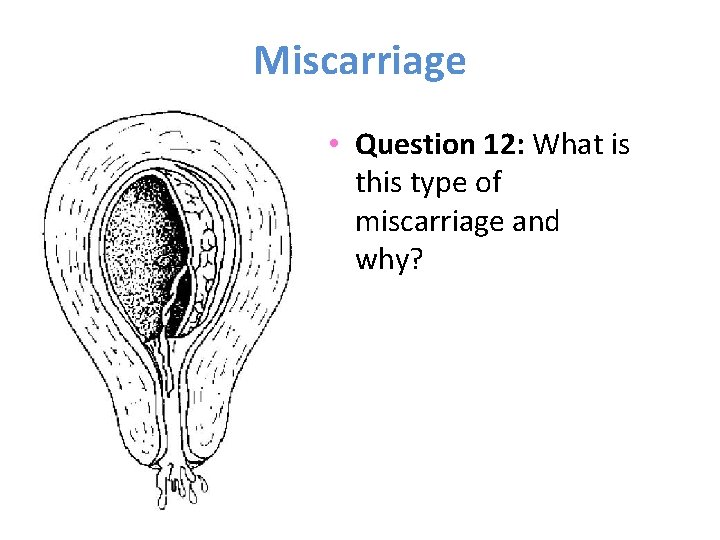
Miscarriage • Question 12: What is this type of miscarriage and why?
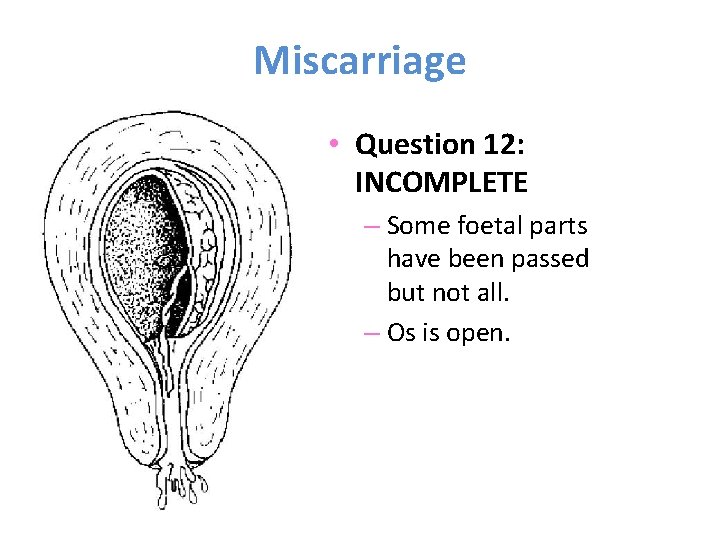
Miscarriage • Question 12: INCOMPLETE – Some foetal parts have been passed but not all. – Os is open.
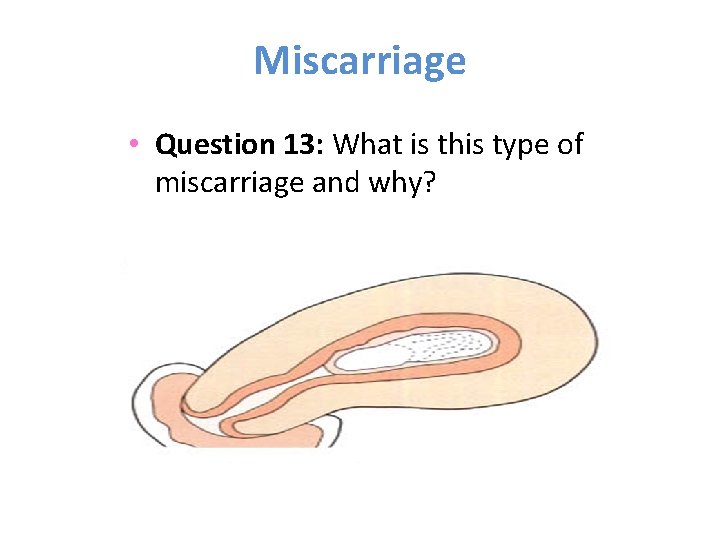
Miscarriage • Question 13: What is this type of miscarriage and why?
Miscarriage • Question 13: MISSED – Foetus has died in utero and this has not been recognised until scan is performed. – Uterus is smaller than expected for dates – Os is closed.
Miscarriage • Question 14: What is this type of miscarriage and why?
Miscarriage • Question 14: COMPLETE – All foetal tissue has been passed – Bleeding diminished – Uterus no longer enlarged – Cervical os is closed
Miscarriage • Question 15: Describe the features of a septic miscarriage. • Question 16: In what three ways can a miscarriage be managed?
Miscarriage • Question 15: Contents of the uterus are infected leading to endometritis, vaginal discharge is offensive, uterus is tender, fever may be absent and may progress to peritonism. • Question 16: expectant, medical or surgical.
Miscarriage • Question 17: What is the expectant management of a non-viable pregnancy? • Question 18: What drug is used in the medical management of a non-viable pregnancy and how is the surgical management carried out?
Miscarriage • Question 17: Can be continued as long as woman is willing. Must be no signs of infection. • Question 18: Medical management is via misoprostol (prostaglandin) sometimes preceded by the oral anti-progesterone mifepristone and surgical is via ERPC. And obviously patient support, education and reassurance. Anti-D given to women who are rhesus negative.
Miscarriage • Question 19: What is the definition of a recurrent miscarriage? • Question 20: What are two causes of late miscarriages (i. e. , those occurring beyond 16 weeks)?
Miscarriage • Question 19: 3 or more miscarriages occurring in succession. • Question 20: Cervical incompetence and infection (often bacterial vaginosis).
Miscarriage • Question 21: List 4 other causes of miscarriage.
Miscarriage • Question 21: Antiphospholipid syndrome, chromosomal abnormalities, anatomical factors (bicornuate uterus), infection, obesity, PCOS, older maternal age.
Maternal Infections • Question 22: What mnemonic is used to remember the perinatal infections that account for 2 -3% of all congenital anomalies?
Maternal Infections • Question 22: TORCH – Toxoplasmosis – Other (syphilis, VCZ, parovirus B 19) – Rubella – CMV – Herpes Infections
Maternal Infections • Question 23: What is the name of the protozoan responsible for toxoplasmosis? • Question 24: What is the text-book source of the toxoplasmosis protozoan?
Maternal Infections • Question 23: Toxoplasma gondii • Question 24: Cat faeces (also raw meat).
Maternal Infections • Question 25: What are the foetal effects of a perinatal toxoplasmosis infection? • Question 26 (PAEDS QUESTION): List 3 other names for parvovirus B 19 infection.
Maternal Infections • Question 25: Mental retardation, convulsions, spasticities, visual impairment – affects the brain. • Question 26: Slapped check syndrome, fifth disease, erythema infectiosum.
Maternal Infections • Question 27: What is the foetal effect of a perinatal parvovirus B 19 infection and how might you detect any complications of such an infection during pregnancy? • Question 28: What percentage of parvovirus B 19 infections result in foetal death?
Maternal Infections • Question 27: Suppresses foetal erythropoiesis causing anaemia (can be detected on USS hydrops). • Question 28: Foetal death in 10% of cases; usually before 20 weeks.
Maternal Infections • Question 29: What would be revealed in a USS in a foetus with CMV infection? • Question 30: How does foetal CMV infection typically present?
Maternal Infections • Question 29: USS show hepatic / cranial calcification. • Question 30: IUGR; pneumonia; thrombocytopenia; hearing, visual and mental impairment.
Maternal Infections • Question 31: A maternal infection with herpes zoster how many weeks before delivery is associated with severe neonatal infection? • Question 32: What is the name of the spirochaete responsible for syphilis infection?
Maternal Infections • Question 31: 4 weeks. • Question 32: Treponema pallidum.
Maternal Infections • Question 33: What are the foetal consequences of maternal syphilis infection during pregnancy? • Question 34: What is the recommended mode of delivery in a foetus seen in herpes simplex infection?
Maternal Infections • Question 33: Causes miscarriage, severe congenital disease or still birth. • Question 34: Herpes simplex infection is not teratogenic. Transmission during birth with high mortality if neonate becomes infected. Csection recommended if delivering within 6 weeks of primary attack.
Maternal Infections • Question 35: Why can’t a pregnant woman eat the following foods during pregnancy? Name the responsible pathogen.
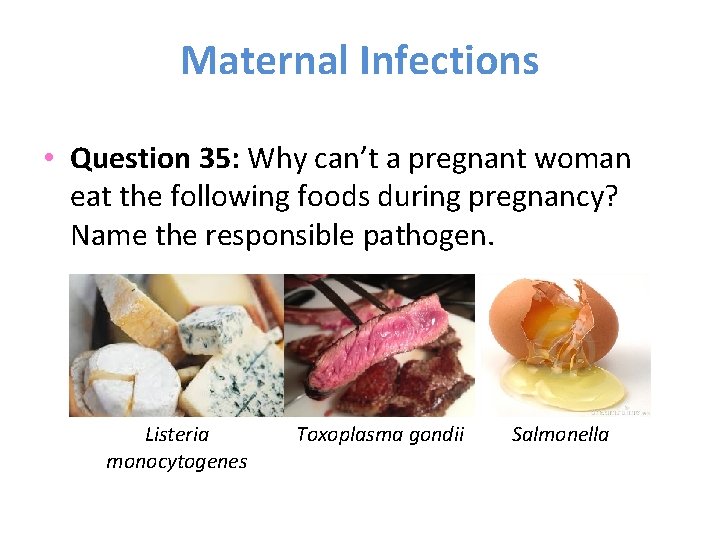
Maternal Infections • Question 35: Why can’t a pregnant woman eat the following foods during pregnancy? Name the responsible pathogen. Listeria monocytogenes Toxoplasma gondii Salmonella
Rhesus Disease • Question 36: What is red blood cell isoimmunisation and when does it happen? • Question 37: Why is anti-D called anti-D?
Rhesus Disease • Question 36: When the mother mounts an immune response against antigens on foetal red cells that enter her circulation. The resulting antibodies then cross the placenta and cause foetal red cell destruction.

Rhesus Disease • Question 37: What is the D refer to in anti-D?
Rhesus Disease • Question 37: The rhesus system consists of 3 linked gene pairs; one allele of each pair is dominant (C/c, D/d, E/e). One allele of each pair is inherited (Mendelian inheritance). The important one is the D gene. Only those who are DD or Dd express the D antigen and a ‘D rhesus positive’. Those who are dd are rhesus negative and will immunological recognise th D antigen as foreign if exposed.
Rhesus Disease • Question 38: What percetange of Caucasian women are rhesus negative and what percentage of these will mount an anti-D response? • Question 39: If an anti-D response is mounted, what symptoms, signs and complications might you observe?
Rhesus Disease • Question 38: 15% of Caucasian women are rhesus negative and 1. 7% of these will mount an anti-D response. • Question 39: Haemolysis causes anaemia. Neonatal jaundice with or without anaemia if less severe but hydrops and foetal death if severe.
Rhesus Disease • Question 40: How is rhesus disease identified? • Question 41: How is the severity of rhesus disease assessed?
Rhesus Disease • Question 40: Unsensitised women are screened for antibodies at booking and at 28 weeks’ gestation. • Question 41: Pregnancies at risk of foetal anaemia are assessed using US. Doppler of foetal middle cerebral artery, foetal blood sampling to confirm.
Rhesus Disease • Question 42: How is rhesus disease treated? • Question 43: In all neoantes bron to rhesusnegative women, what blood tests should be performed?
Rhesus Disease • Question 42: in utero transfusion if foetus is anaemia, and deliver if < 36 weeks. • Question 43: Should have blood group checked, FBC, blood film and bilirubin. A coomb’s test is no longer advised.
Complications of pregnancies • Ectopic pregnancies • Maternal disorders – especially pre-eclampsia and other hypertensive diseases • Obstetric shock – APH

Ectopic Pregnancy • • • This came up as a SAQ in 2013 What is EP? How common is EP as a % of all pregnancies? Mortality rate (/100, 000)? Commonest gestational age to present?
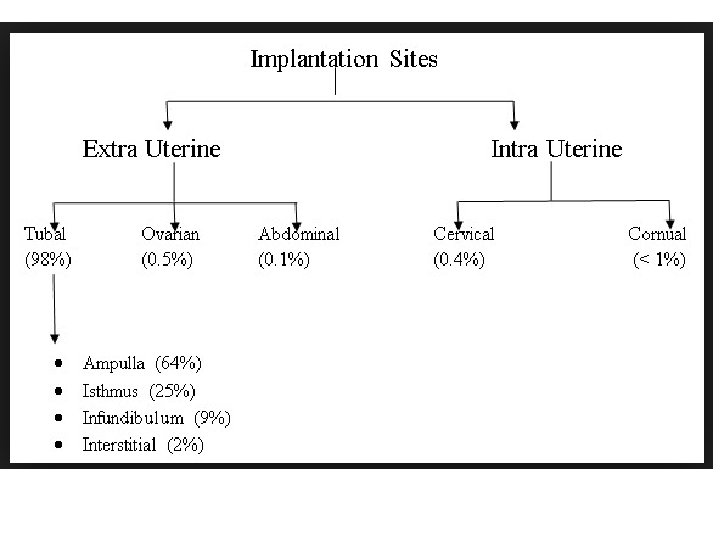
• EP is when the embryo implants outside the uterine cavity* • 1 -2% (1 in 60 -100) • 17/100, 000 • 8 weeks *Not strictly true, see next slide
Ectopic Pregnancy • What is the commonest site for ectopic pregnancy? • Name 2 other sites for EP
EP • Why is it a problem if an embryo implants into the fallopian tube? Won’t it just grow there happily?
EP • The fallopian tube is thin walled therefore trophoblastic invasion can lead to bleeding into the lumen or may rupture which can cause catastrophic blood loss
EP risk factors • What are they?
• • • PID Assisted conception Pelvic (especially tubal) surgery Previous ectopic Smoking Copper coil
EP • Abnormal vaginal bleeding, abdominal pain or collapse in a woman of reproductive age? Always rule out ectopic! • The classical presentation is collapse with abdominal pain – although this occurs <¼ of the time
Symptoms of an Ectopic Pregnancy Light vaginal bleeding (scanty, dark bleeding) Nausea and vomiting with pain. Lower abdominal pain. Sharp abdominal cramps. Pain on one side of your body (differential is appendicitis) • Dizziness or weakness. • Pain in your shoulder, neck, or rectum. • If the fallopian tube ruptures, the pain and bleeding could be severe enough to cause fainting. • • •
• Examination findings?
EP • Tachycardia (blood loss) – although hypotension and collapse only occurs in severe blood loss • Abdominal and rebound tenderness • Cervical excitation (pain on manipulation of uterus) • Adnexal tenderness • Small uterus for gestational age • Cervical os closed
EP • Investigations?
EP • PREGNANCY TEST! (Any woman of reproductive age with collapse, abdo pain or bleeding) • TVUSS (can see intrauterine pregnancies) • A h. CG level that is rising by less than 66% over 48 hours means it is likely, but not a certainty, that the pregnancy is ectopic • Laproscopy
EP • Management for EP varies depending on the patient • Acute presentations (patient is haemodynamically unstable) and subacute presentations • Name 3 TREATMENT options Management: Pregnancy test, IV access, FBC and cross match, USS, nil by mouth, laproscopy or medical management
• Salpingectomy (removal of whole tube) • Salpingostomy (removal of ectopic from tube) • Methotrexate (25% need another dose or surgery) • Note that to use methotrexate (medical management) 3 criteria are required: Unruptured ectopic No cardiac activity h. CG <3000 IU/m. L
EP • Risk of another EP? • Chance of subsequent successful pregnancy?
Summary EP • Embryo implants where is shouldn’t • Common (1 -2%) • Abdo pain, bleeding and collapse required pregnancy test! • Key invs: h. CG, TVUSS, laproscopy • Treatment: salpingectomy, salpinostomy, methotrexate
Molar pregnancies • Decided not to cover because of time • Gestational trophoblastic disease is RARE but Sheffield is a key centre so you never know what might come up in the exam… Might be worth a look • Buzzword: “Snowstorm” appearance on ultrasound scan!
Hypertensive Disorders in Pregnancy • What is pregnancy induced hypertension? • What is chronic/pre-existing HTN? • What is pre-eclampsia?
• BP rises above 140/90 AFTER 20 weeks • BP above 140/90 BEFORE 20 weeks or is on antihypertensive medication • Hypertension (pregnancy-induced) and proteinuria (>0. 3 g/24 h) in 2 nd half of pregnancy
Pre-eclampsia • Mild: proteinuria with mild/moderate HTN • Moderate: proteinuria with severe HTN • Severe: proteinuria with HTN <34 w or with maternal complications • N. B. Mild HTN 140/90 – 149 -99; moderate 150/100 -159/109 and severe >160/110
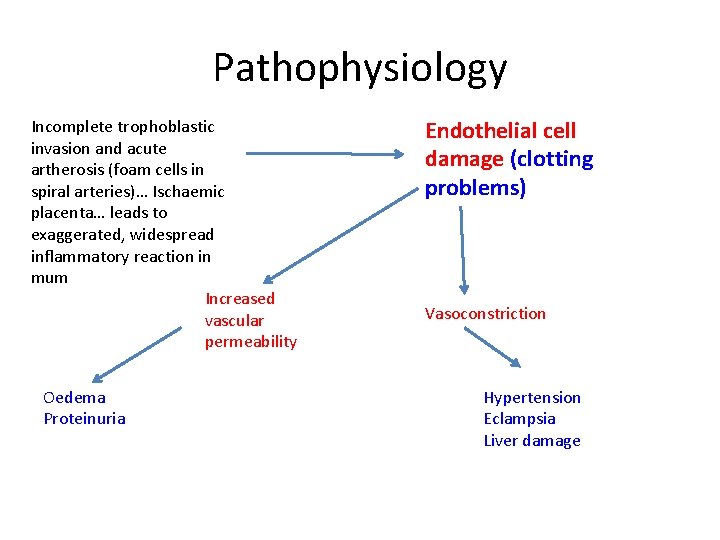
Pathophysiology Incomplete trophoblastic invasion and acute artherosis (foam cells in spiral arteries)… Ischaemic placenta… leads to exaggerated, widespread inflammatory reaction in mum Increased vascular permeability Oedema Proteinuria Endothelial cell damage (clotting problems) Vasoconstriction Hypertension Eclampsia Liver damage
Pre-E • What are the risk factors for pre-eclampsia?
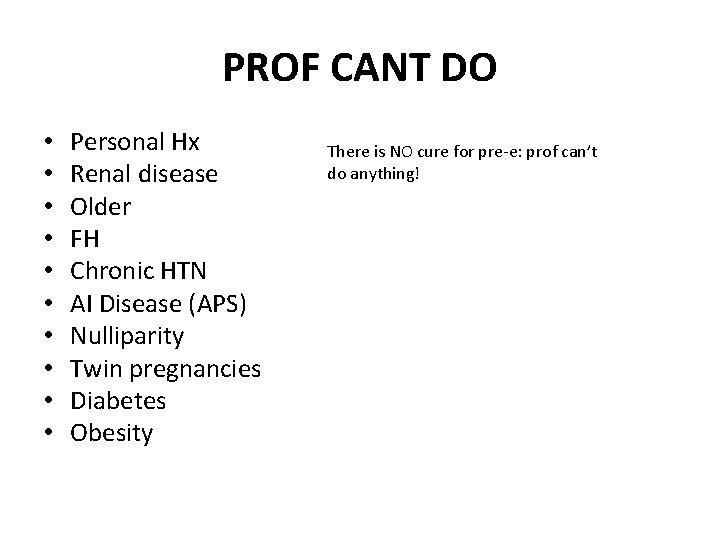
PROF CANT DO • • • Personal Hx Renal disease Older FH Chronic HTN AI Disease (APS) Nulliparity Twin pregnancies Diabetes Obesity There is NO cure for pre-e: prof can’t do anything!
• How do you assess urinary protein?
• Protein: creatinine ratio (PCR) - >30 mg/nmol • Dipstick • 24 hour collection
History from mum • Patient is usually asymptomatic apart from at a late stage: • Headaches, drowsiness, visual disturbances • Nausea, vomiting, epigastic pain • Swelling due to oedema
• What are the maternal complications of preeclampsia?
• • • DEATH Eclampsia CVA HELLP Syndrome DIC Liver failure Renal failure Pulmonary oedema (Tx oxygen and furosemide)
• What is HELLP Syndrome? • What types of seizures do you get in eclampsia and what is the treatment?
• H: haemolysis (dark urine, raised LDH, anaemia) • EL: elevated liver enzymes (epigastric pain [bad sign!], liver failure, abnormal clotting) • LP: low platelets (self-limiting) • Might also get DIC, liver failure or liver rupture
Tx of Eclampsia • Generalized tonic-clonic • This is thought to be due to cerebrovascular vasospam • Magnesium sulphate – not an anticonvulsant but it increases cerebral blood flow • Most epilepsy medication is related to fetal complications
• What are the fetal complications of preeclampsia?
Fetal complications of Pre-E • • • DEATH (5% of still births attributable to Pre-E) IUGR Pre-term birth (10% accounted for by Pre-E) Placental abruption Hypoxia
Investigations • Urinary protein (exclude infection if raised) • Blood tests – low platelets (get help as HELLP is on the way!) • LDH – up in heamolysis and liver disease • LFT – high ALT suggests HELLP or liver disease • Umbilical artery doppler to observe fetal blood flow
• Starting treatment with what at <16 w is recommended by NICE for high risk women?
• Aspirin 75 mg
Management • Admission to hospital is required for severe HTN or proteinuria • Anti-hypertensives are started if BP reaches 150/100 and started urgently if BP is >160/110 • If BP is >150/100 but <160/100 – what is the drug used to treated this and what class of drug is it? • If HTN is severe, what are the 2 treatments required? • Also if patient is diagnosed <34 weeks – give steroids
• Labetalol, beta-blocker • Oral nefidipine – 1 st (dihydropyridine calcium channel blocker) then consider IV labetalol
When to deliver if: • Mild pre-e • Moderate pre-e • Severe pre-e with maternal complications or fetal distress
• • • By 37 weeks 34 -36 NOW regardless of gestation Before 34 weeks c/s – after the mother can be induced using prostaglandins
Antepartum haemorrhage • Definition? • Causes?
• Bleeding from the genital tract after 24 weeks gestation • Common: undetermined origin, placenta praevia, placental abruption • Uncommon: incidental pathology, uterine rupute, vasa praevia
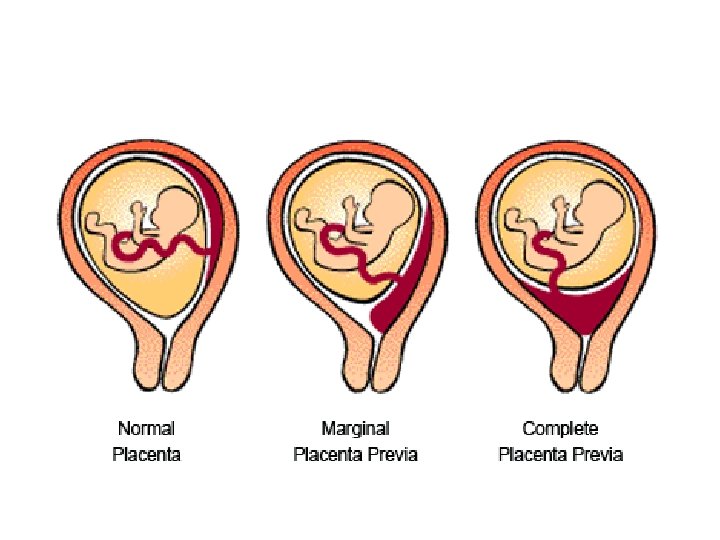
Placenta Praevia • What is it? • How common is it at term? • Types of PP?
• Placenta is implanted into the lower segment of the uterus • 0. 4% of pregnancies at term • Marginal – low lying by not covering os • Major – placenta covers some or all of os
• Risk factors?
• Previous caesarian section (placenta implants into c/s scar) • Twins • High parity • Older
• Complications?
• Placenta accreta, placenta increta, placenta percreta • Massive haemorrhage so large mother may need hysterectomy • C/s • Transverse lie, breech presentation
Clinical features • What might the mother give as a hx? • What examination should NEVER BE PERFORMED?
• Intermittent, painless bleeds which increase in frequency and intensity over several weeks • However, 1/3 experience no bleeding before birth • Vaginal examination
• How is the diagnosis made?
• USS • Before 20 weeks placenta can be ‘low-lying’ but 90% of these do not develop in placenta praevia • If a low-lying placenta is seen at the 20 week USS, a repeat USS is done at 32 weeks. If it’s within 2 cm of the os, it’s likely to be PP at term • Anterior placentas seen at 20 weeks can be scanned using a 3 D power USS to check for placenta accreta
• When to admit: • Any pregnant woman with bleeding should be admitted – if PP found, they stay in hospital until delivery as there’s a risk of massive haemorrhage • Bloods, IV access, anti-D to rh-ve women, steroids <34 w • PP and asymptomatic? Mum can stay at home until 37 weeks providing they can get into hospital easily
• When to deliver?
• 39 weeks by most senior person available • Be prepared for placenta accreta or percreta! • Be prepared to PPH
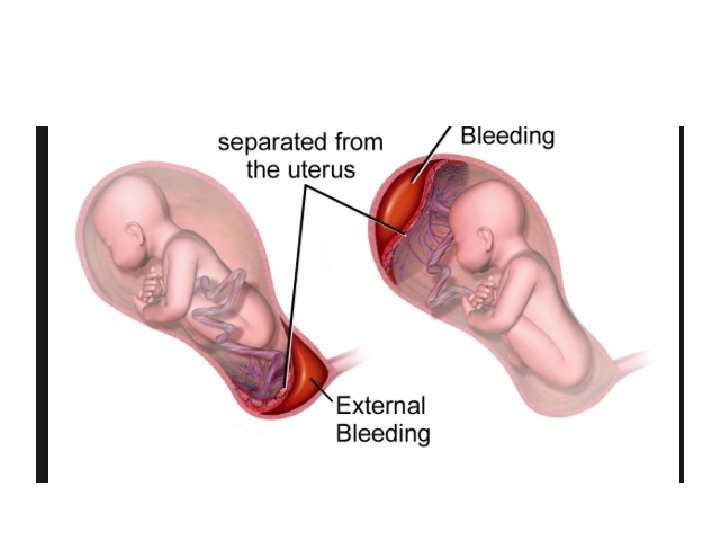
Placental abruption • What is it? • How common is it?
• It’s when the placenta separates before the delivery of the fetus • 1% • When the placenta separates, there can be significant maternal bleeding behind it
• Blood can track between the membranes and myometrium to reveal APH • Or blood can go directly into the myometrium (‘concealed’) • Visible haemorrhage is absent in 20% of cases!
• Complications?
• • Fetal death (30%!) Maternal death (rare) Haemorrhage transfusion required Haemorrhage DIC and renal failure
• Risk factors?
• • • Previous PA IUGR Pre-eclampsia Pre-existing HTN Smoking Cocaine AI disease Multiple pregnancy High maternal parity And more….
• Clinical features?
Symptoms • Pain • Bleeding (dark) • Pain can occur alone with concealed blood loss • Visible bleeding does not equate to severity of abruption
Signs Buzzword: woody hard uterus on examination Tender, contracting uterus Tachycardia Hypotension with severe loss of blood – this can lead to maternal collapse • Fetal heart tones abnormal or absent • Poor urine output • Renal failure • •
• A woman, 32 weeks pregnant, comes into A+E with pain and uterine tenderness but no bleeding • What should you do?
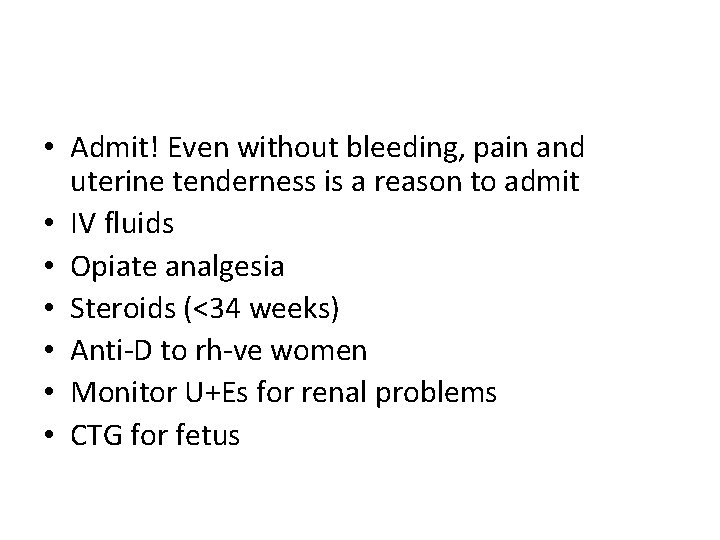
• Admit! Even without bleeding, pain and uterine tenderness is a reason to admit • IV fluids • Opiate analgesia • Steroids (<34 weeks) • Anti-D to rh-ve women • Monitor U+Es for renal problems • CTG for fetus
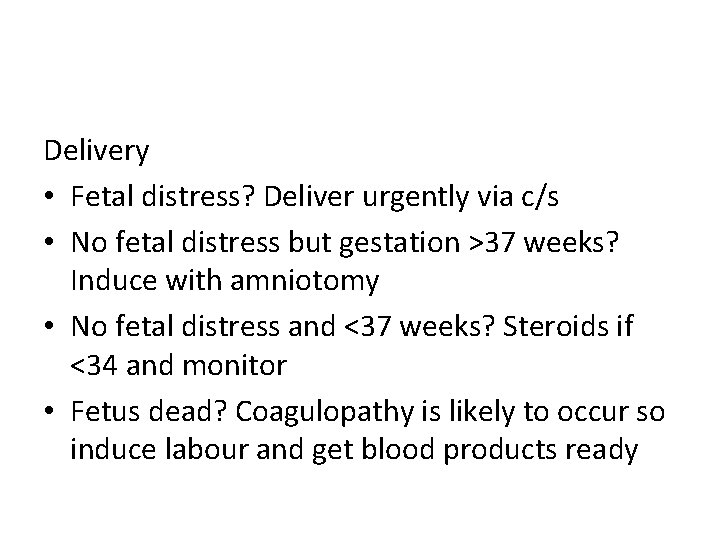
Delivery • Fetal distress? Deliver urgently via c/s • No fetal distress but gestation >37 weeks? Induce with amniotomy • No fetal distress and <37 weeks? Steroids if <34 and monitor • Fetus dead? Coagulopathy is likely to occur so induce labour and get blood products ready
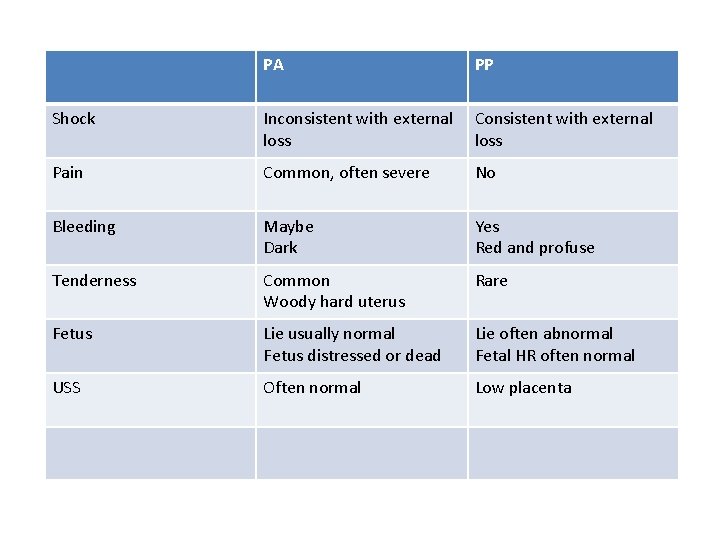
PA PP Shock Inconsistent with external loss Consistent with external loss Pain Common, often severe No Bleeding Maybe Dark Yes Red and profuse Tenderness Common Woody hard uterus Rare Fetus Lie usually normal Fetus distressed or dead Lie often abnormal Fetal HR often normal USS Often normal Low placenta
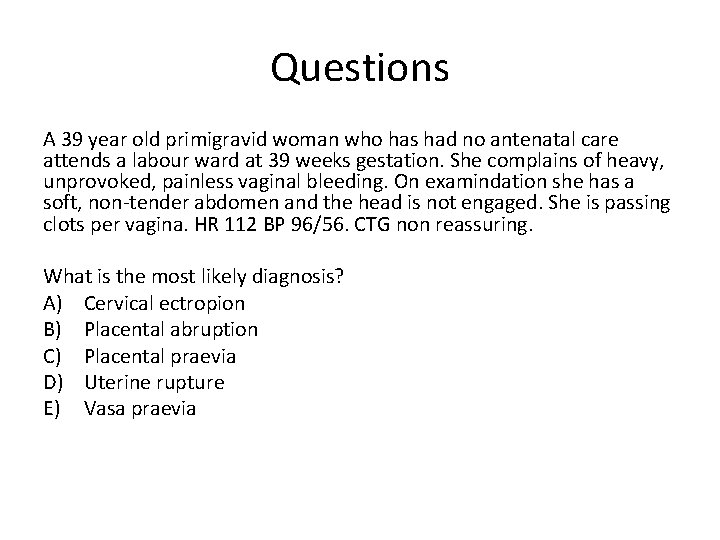
Questions A 39 year old primigravid woman who has had no antenatal care attends a labour ward at 39 weeks gestation. She complains of heavy, unprovoked, painless vaginal bleeding. On examindation she has a soft, non-tender abdomen and the head is not engaged. She is passing clots per vagina. HR 112 BP 96/56. CTG non reassuring. What is the most likely diagnosis? A) Cervical ectropion B) Placental abruption C) Placental praevia D) Uterine rupture E) Vasa praevia
B – placenta praevia
A 31 year old woman, who has recently had a postive pregnancy test, has an early TVUSS which showed no intrauterine pregnancy. She subsequently has two beta h. CG samples taken, the first one the day of the scan and the second 48 hours later. The first test result was 578 iu and the second 1126 iu. What is the most likely diagnosis? A) B) C) D) E) Ectopic pregnancy Early intrauterine pregnancy Inevitable miscarriage Missed miscarriage Threatened miscarriage?
Answer – B: early intrauterine pregnancy • The fact that beta h. CG was less than 1000 iu on the day of the scan explains why no pregnancy was seen. >1000 iu usually means the gestational sac can be seen. • If the repeat h. CG is static or only reducing slowly, an ectopic must be ruled out and further management considered. • A SIGNIFICANT fall in b. HCG is caused by a miscarriage • An empty uterus means 3 things: ectopic pregnancy, early intrauterine pregnancy or missed miscarriage.
• A 25 year old woman is brought into the resus area having collapsed. She is maintaining her airway and is breathing via a non-rebreathe bag. She has a week pulse, HR 123, BP 86/48, o 2 98%, temp 37. 2. After fluid resuscitation the patient is responsive enough to tell you she had some lower, right sided abdominal pain earlier in the day but cannot remember anything else. She uses the copper coil for contraception. On examination, she is tender with guarding in the right iliac fossa. On speculum examination there is brown discharge seen in the vagina. Threads for the coil are seen and cervical excitation is present. A urine result is awaited. What is the most likely diagnosis? A) B) C) D) E) Appendicitis Dislodged coil to the cervical location Ectopic pregnancy Ovarian cyst torsion PID
C – ectopic pregnancy • This is the most likely to be an ectopic pregnancy which may have ruptured into the abdominal cavity leading to the patient become clinically shocked.
• A 30 year old primigravid woman who is 34 weeks pregnant attends the antenatal clinic. She has persistent hypertension of 164/112 mm. Hg and some protein in her urine on dipstick testing. She has no visual disturbance, no epigastric pain and complains of mild headaches which are generally relieved by paracetamol. On examination her abdomen is soft non-tender, she has mild petal oedema, normal reflexes and one beat of clonus. Her bloods are normal. She has asthma for which she takes a salbutamol inhaler when required. What hypertensive should you use to manage her? • • • A) furosemide B) labetalol C) magnesium sulphate D) nefidipine E) rampril
D - nefidipine
- Slides: 139