Obstetric Triage Units Increasing Efficiency and Quality of
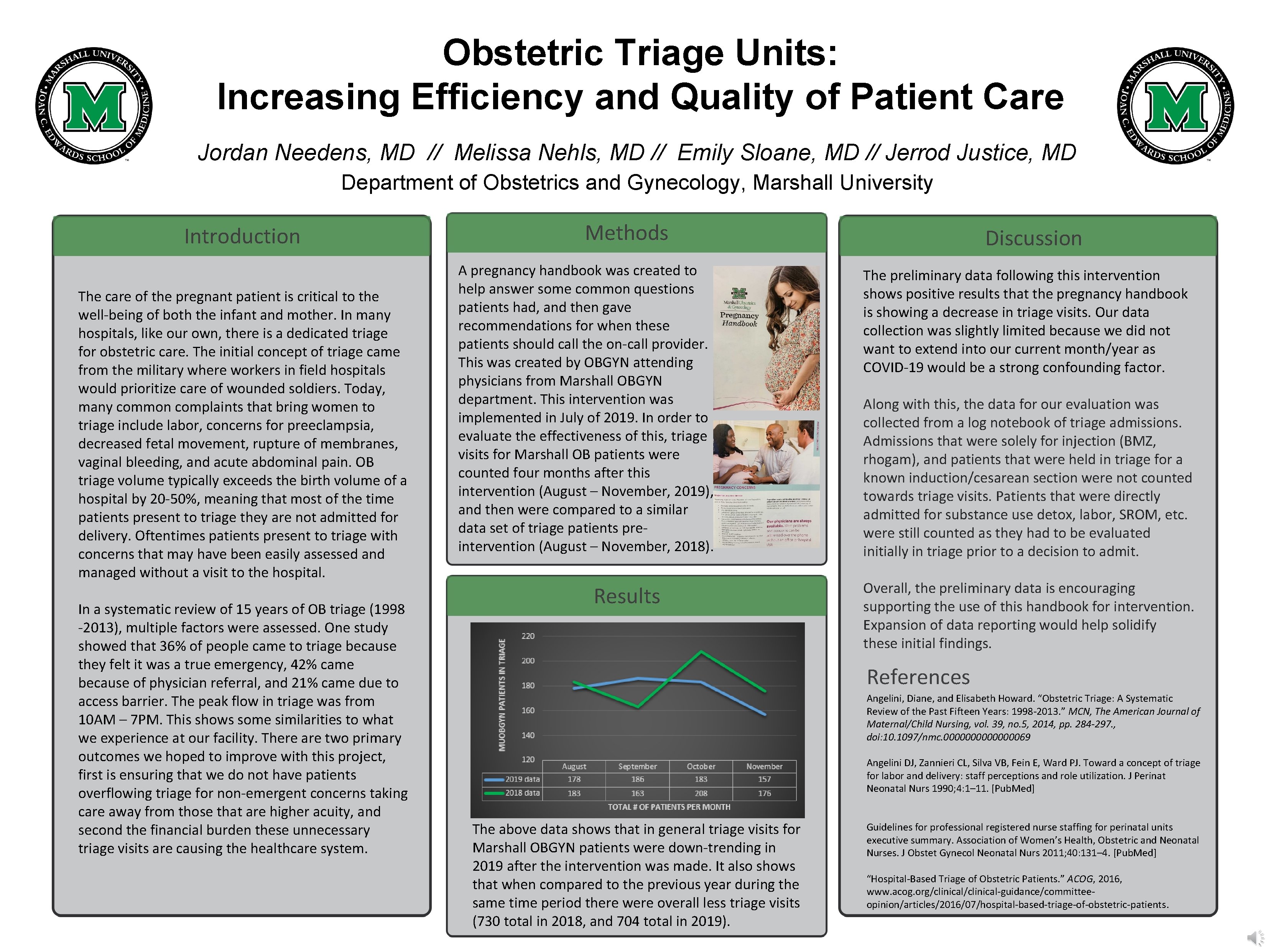
Obstetric Triage Units: Increasing Efficiency and Quality of Patient Care Jordan Needens, MD // Melissa Nehls, MD // Emily Sloane, MD // Jerrod Justice, MD Department of Obstetrics and Gynecology, Marshall University Introduction The care of the pregnant patient is critical to the well-being of both the infant and mother. In many hospitals, like our own, there is a dedicated triage for obstetric care. The initial concept of triage came from the military where workers in field hospitals would prioritize care of wounded soldiers. Today, many common complaints that bring women to triage include labor, concerns for preeclampsia, decreased fetal movement, rupture of membranes, vaginal bleeding, and acute abdominal pain. OB triage volume typically exceeds the birth volume of a hospital by 20 -50%, meaning that most of the time patients present to triage they are not admitted for delivery. Oftentimes patients present to triage with concerns that may have been easily assessed and managed without a visit to the hospital. In a systematic review of 15 years of OB triage (1998 -2013), multiple factors were assessed. One study showed that 36% of people came to triage because they felt it was a true emergency, 42% came because of physician referral, and 21% came due to access barrier. The peak flow in triage was from 10 AM – 7 PM. This shows some similarities to what we experience at our facility. There are two primary outcomes we hoped to improve with this project, first is ensuring that we do not have patients overflowing triage for non-emergent concerns taking care away from those that are higher acuity, and second the financial burden these unnecessary triage visits are causing the healthcare system. Methods Intervention A pregnancy handbook was created to help answer some common questions patients had, and then gave recommendations for when these patients should call the on-call provider. This was created by OBGYN attending physicians from Marshall OBGYN department. This intervention was implemented in July of 2019. In order to evaluate the effectiveness of this, triage visits for Marshall OB patients were counted four months after this intervention (August – November, 2019), and then were compared to a similar data set of triage patients preintervention (August – November, 2018). Results Discussion The preliminary data following this intervention shows positive results that the pregnancy handbook is showing a decrease in triage visits. Our data collection was slightly limited because we did not want to extend into our current month/year as COVID-19 would be a strong confounding factor. Along with this, the data for our evaluation was collected from a log notebook of triage admissions. Admissions that were solely for injection (BMZ, rhogam), and patients that were held in triage for a known induction/cesarean section were not counted towards triage visits. Patients that were directly admitted for substance use detox, labor, SROM, etc. were still counted as they had to be evaluated initially in triage prior to a decision to admit. Overall, the preliminary data is encouraging supporting the use of this handbook for intervention. Expansion of data reporting would help solidify these initial findings. References Angelini, Diane, and Elisabeth Howard. “Obstetric Triage: A Systematic Review of the Past Fifteen Years: 1998 -2013. ” MCN, The American Journal of Maternal/Child Nursing, vol. 39, no. 5, 2014, pp. 284 -297. , doi: 10. 1097/nmc. 000000069 Angelini DJ, Zannieri CL, Silva VB, Fein E, Ward PJ. Toward a concept of triage for labor and delivery: staff perceptions and role utilization. J Perinat Neonatal Nurs 1990; 4: 1– 11. [Pub. Med] The above data shows that in general triage visits for Marshall OBGYN patients were down-trending in 2019 after the intervention was made. It also shows that when compared to the previous year during the same time period there were overall less triage visits (730 total in 2018, and 704 total in 2019). Guidelines for professional registered nurse staffing for perinatal units executive summary. Association of Women’s Health, Obstetric and Neonatal Nurses. J Obstet Gynecol Neonatal Nurs 2011; 40: 131– 4. [Pub. Med] “Hospital-Based Triage of Obstetric Patients. ” ACOG, 2016, www. acog. org/clinical-guidance/committeeopinion/articles/2016/07/hospital-based-triage-of-obstetric-patients.
- Slides: 1