Obstetric Anaesthesia Physiological changes in pregnancy Mechanical Hormonal
Obstetric Anaesthesia
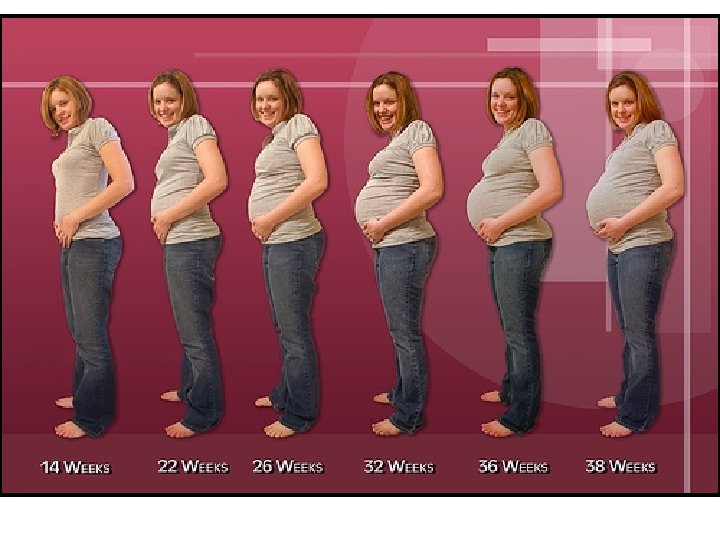
Physiological changes in pregnancy Mechanical Hormonal Increased metabolic demands Fetoplacental circulation
Respiratory changes n n n FRC decreased 20% Ventilation increased (progesterone) At term minute ventilation increased 50% O 2 consumption increases 40 – 60% and 100% in labour Blood gas: compensated resp alkalosis O 2 dissociation curve shifted to right
Consequences n Greater risk of hypoxaemia n n Decreased O 2 stores Increased O 2 demand
CVS Changes n n n Blood volume increases 30 – 40% CO increased 43% SVR decreased 21% During labour CO increases a further 43% (Pain) Aortocaval compression Delivery – autotransfusion < 500 ml
Blood Constituents n n n Plasma protein concentration decreases Decreased A/G ratio COP decreases 13% n n Pulmonary oedema Hypercoagulable state
Consequences n Airway difficulties n n Oedema Worse Malampatti Score

GIT Function n n n Increased gastric acid Delayed gastric emptying Decreased lower oesophageal sphincter tone Increased risk of G-O reflux Increased aspiration risk Prophylactic measures mandatory
Placenta n n Not autoregulated Hypotension can lead to severe uteroplacental insufficiency and fetal distress
GA vs Regional for C/S?
Regional Anaesthesia is SAFER But……… Mortality with both
National Committee on Confidential Enquiries into Maternal Death of SA 1999 – 2001 25 deaths under Spinal
Advantages of Regional n Improved safety n Risk of Intubation averted n n n Hypoxia Aspiration Bonding between mother & baby
Regional Techniques n n n Spinal Anaesthesia Epidural Anaesthesia Combined Spinal - Epidural
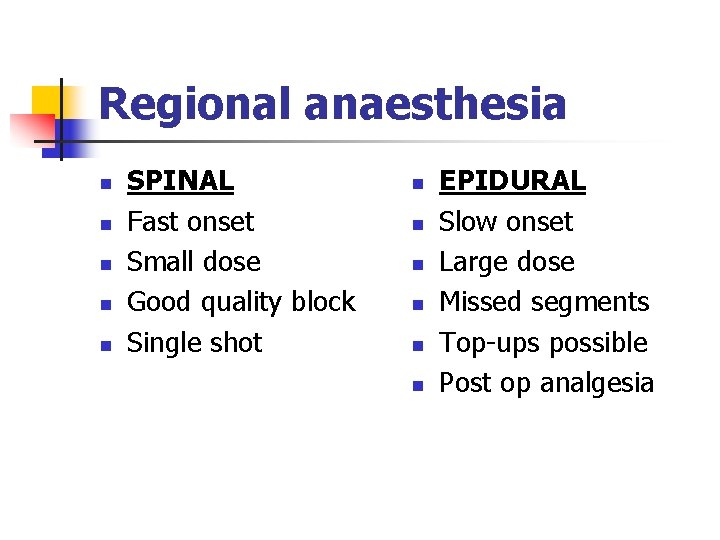
Regional anaesthesia n n n SPINAL Fast onset Small dose Good quality block Single shot n n n EPIDURAL Slow onset Large dose Missed segments Top-ups possible Post op analgesia
Contraindications to Regional n n n Patient refusal Operator inexperience Absent resuscitation equipment However…… The above applies to any procedure!!
Contraindications to Regional Specific n n n n Hypovolaemia Coagulation abnormalities Thrombocytopaenia (<75 x 109/L) Local sepsis CVS co-morbidity – MS, AS Raised intracranial pressure Allergy
Spinal Anaesthesia n n n History / examination / explanation / consent Antacid prophylaxis IV access and crystalloid at the time of block n n n 10 - 20 ml Kg-1 (co-loading) Spinal at L 3/4: 25 G pencil point needle 2 ml 0, 5% Bupivacaine (10 mg), plus 10 g Fentanyl (0, 2 ml) T 4 block in most cases Position supine with 150 L lateral wedge/tilt i. e. L side down
Spinal (continued) n n Facemask oxygen Rx hypotension n n Ephedrine / Phenylephrine Increase L uterine displacement Fluid At delivery n n Oxytocin 2, 5 iu over 30 seconds Oxytocin infusion 10 iu in 1000 ml
Inadequate block n n Pre – Sx Intra-operatively n n n Inhaled nitrous oxide Alfentanil 250 μg or Fentanyl 50 μg BZD small dose (Midazolam 1 - 2 mg) n n n NB Amnesia and respiratory depression LA Convert to GA
Complications of Spinal n Hypotension n n n Sympathetic block Bradycardia Aorto-caval compression Occult haemorrhage High motor blockade Failed block Headache

Spinals and Epidurals
Spinal Anaesthesia
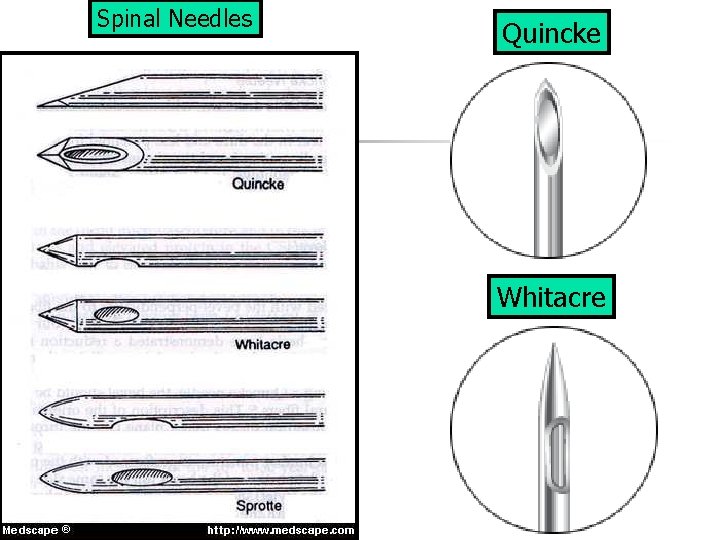
Spinal Needles Quincke Whitacre
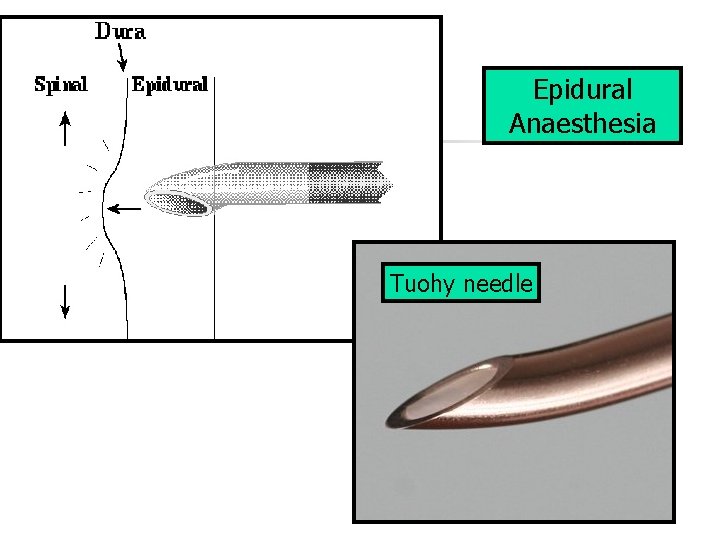
Epidural Anaesthesia Tuohy needle
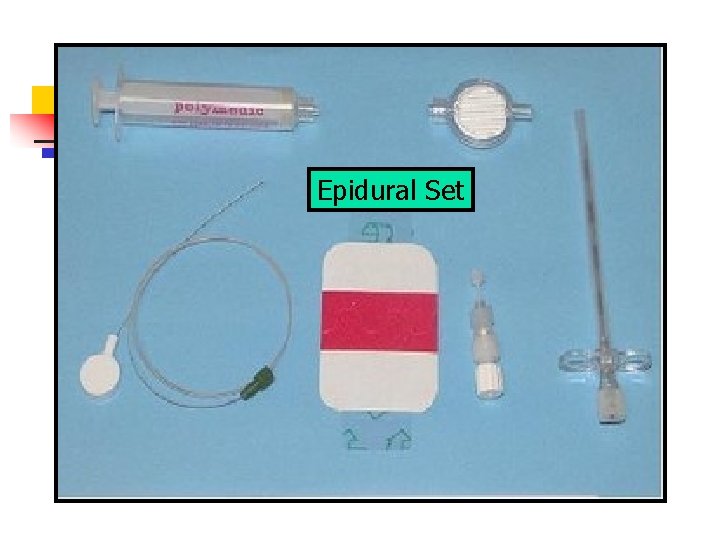
Epidural Set
General Anaesthesia for C/S Two patients with differing requirements
Indications for GA n n Maternal request Urgent surgery Regional anaesthesia contraindicated Failed regional anaesthesia

Technique n n n History / examination Antacid prophylaxis Monitoring L lateral tilt Preoxygenate Rapid Sequence Induction / Intubation (RSI or “Crash Induction”) with Thiopentone / Suxamethonium
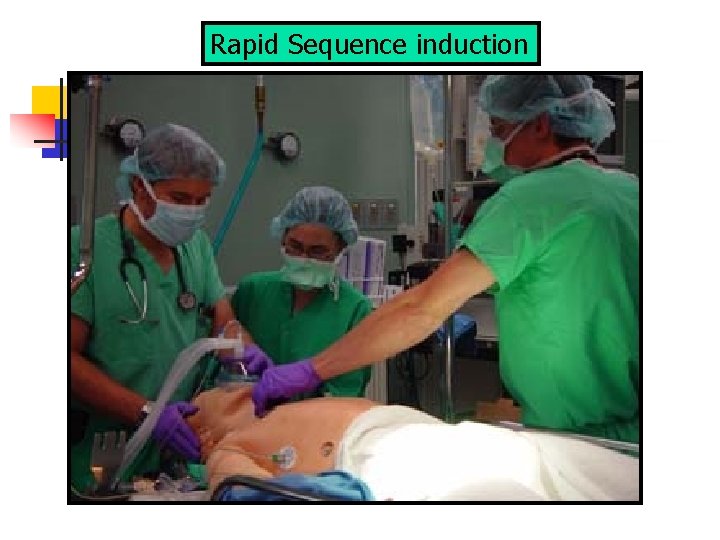
Rapid Sequence induction
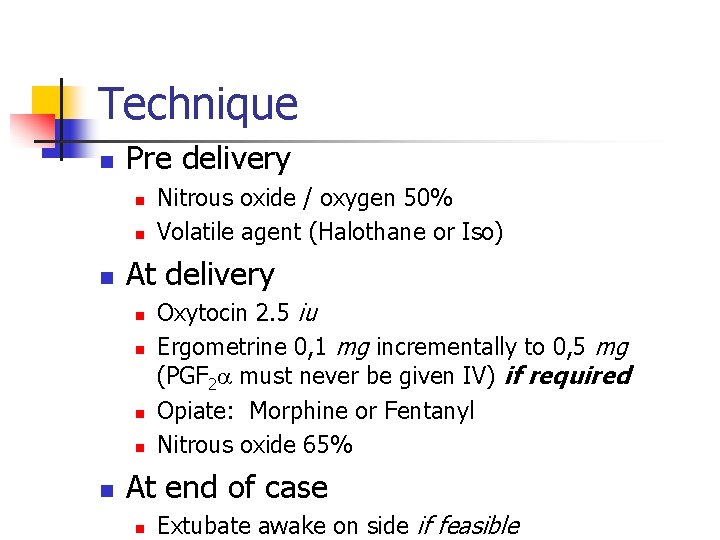
Technique n Pre delivery n n n At delivery n n n Nitrous oxide / oxygen 50% Volatile agent (Halothane or Iso) Oxytocin 2. 5 iu Ergometrine 0, 1 mg incrementally to 0, 5 mg (PGF 2 must never be given IV) if required Opiate: Morphine or Fentanyl Nitrous oxide 65% At end of case n Extubate awake on side if feasible

Malampatti Score
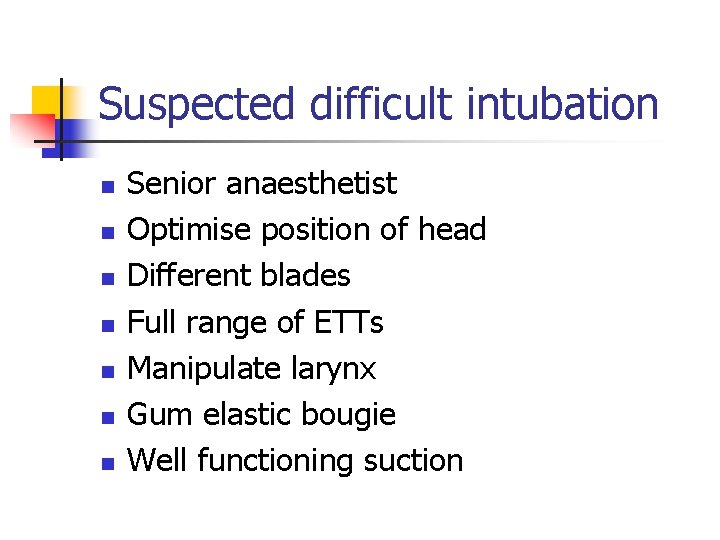
Suspected difficult intubation n n n Senior anaesthetist Optimise position of head Different blades Full range of ETTs Manipulate larynx Gum elastic bougie Well functioning suction
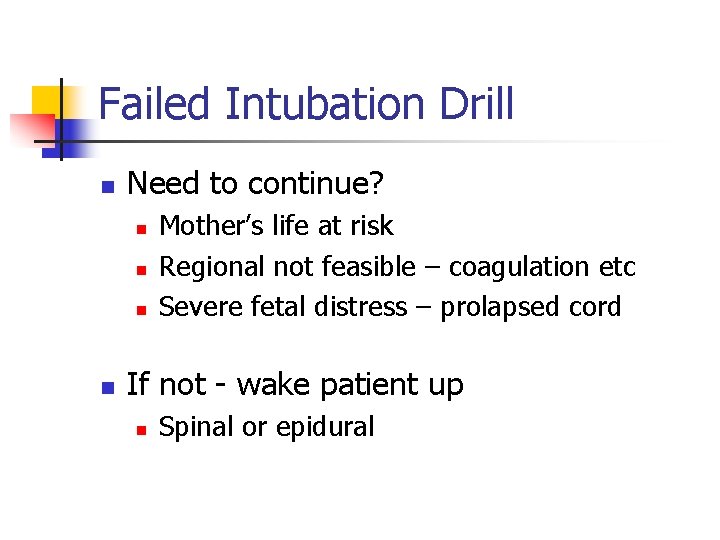
Failed Intubation Drill n Need to continue? n n Mother’s life at risk Regional not feasible – coagulation etc Severe fetal distress – prolapsed cord If not - wake patient up n Spinal or epidural
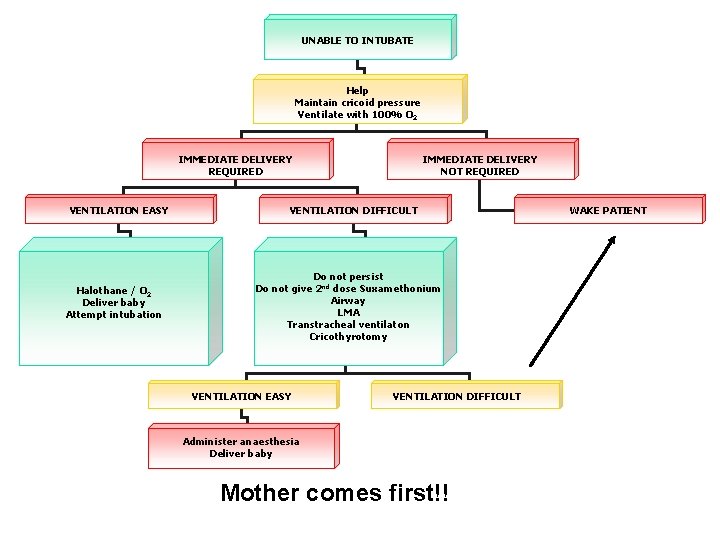
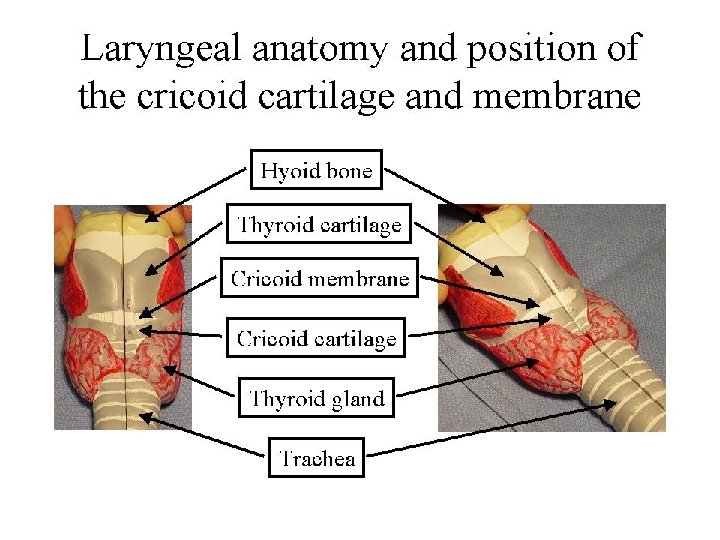
UNABLE TO INTUBATE Help Maintain cricoid pressure Ventilate with 100% O 2 IMMEDIATE DELIVERY REQUIRED VENTILATION EASY Halothane / O 2 Deliver baby Attempt intubation IMMEDIATE DELIVERY NOT REQUIRED VENTILATION DIFFICULT Do not persist Do not give 2 nd dose Suxamethonium Airway LMA Transtracheal ventilaton Cricothyrotomy VENTILATION EASY VENTILATION DIFFICULT Administer anaesthesia Deliver baby Mother comes first!! WAKE PATIENT
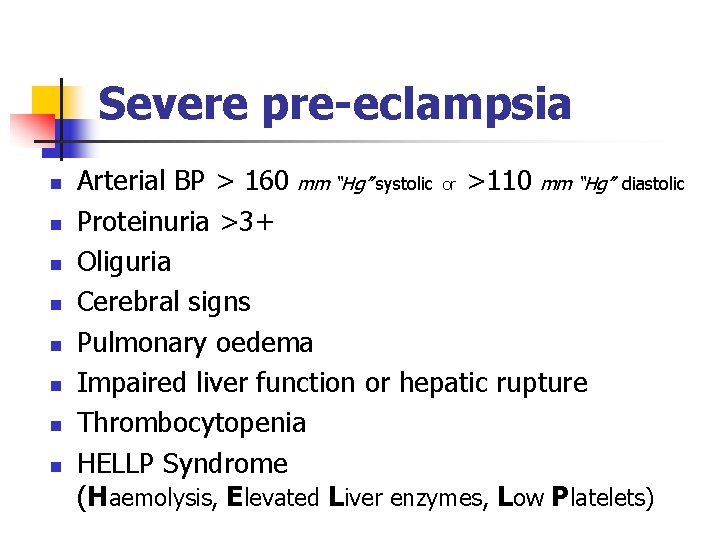
Severe pre-eclampsia n n n n Arterial BP > 160 mm “Hg” systolic or >110 mm “Hg” diastolic Proteinuria >3+ Oliguria Cerebral signs Pulmonary oedema Impaired liver function or hepatic rupture Thrombocytopenia HELLP Syndrome (Haemolysis, Elevated Liver enzymes, Low Platelets)
Pre-eclampsia
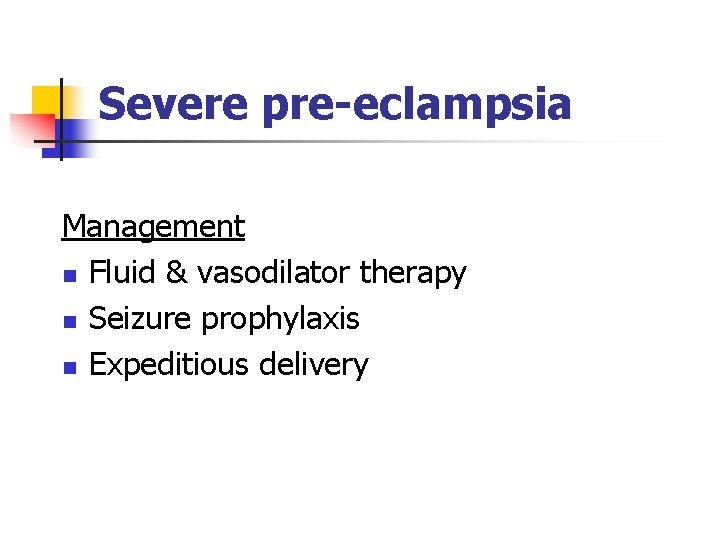
Severe pre-eclampsia Management n Fluid & vasodilator therapy n Seizure prophylaxis n Expeditious delivery
Severe pre-eclampsia n n n Spinal anaesthesia method of choice if no contraindications even if NRFHT Platelet count > 75 x 109 l-1 Fetal bradycardia is an indication for GA Use normal doses for spinal anaesthesia Similar doses of vasopressors
Major anaesthetic problems n Airway management n n Intubation response n n Pre O 2, range of ETTs, bougie, LMA Mg. SO 4, Alfentanil Neuromuscular blockade n Mg. SO 4 prolongs NDMRs
Eclampsia n n GA favoured Postoperative ventilation, depending on presence of cerebral oedema
References n n Prevention & Rx of CVS instability during spinal anaesthesia for C/S Dyer et al. SAMJ 94; 3: 367 -372 Oxford Handbook of Anaesthesia Allman & Wilson
- Slides: 44