Observing the Application of the 4 Ms in
Observing the Application of the 4 Ms in Nursing Care of Older Adults Age-Friendly Health Systems
Older Adults • Approximately 56. 4 million people 65+ • 10, 000 people turn 65 every day • By 2060, older adults will comprise 25% of the U. S. population • Growing more racially, ethnically and culturally diverse • Burden of disease • Care more complex • Chronic health condition: • • • HTN (58%) Hyperlipidemia (48%) Arthritis (31%) Ischemic Heart Disease (28%) Diabetes (27%)
Older Adults • Routinely receive unwanted care and treatment • Routinely do not receive necessary and evidence-based care • Needless harmed by inappropriate medications • Experience functional decline when mobility is not encouraged • Experience avoidable delirium and cognitive decline • Disproportionately experience needless harms and death
“Avoidable Harm” Priorities • Adverse Drug Events • Catheter Associated Urinary Tract Infections (CAUTI) • Central Line Associated Bloodstream Infections (CLABSI) • Injuries from Falls and Immobility • Pressure Ulcers • Surgical Site Infections • Venous Thromboembolism • Ventilator Associated Events • Readmissions
Age-Friendly Health Systems • “The 4 Ms are implemented together as a set of evidence-based interrelated-high quality care practices interprofessional teams can implement to improve care for older adults” (IHI, 2019) • Causes no harm to older adults • Aligns with older adult’s goals and preferences
Potential Benefits of Age-Friendly Care • Reduce ED visits, hospitalizations and hospital readmissions • Improve patient satisfaction • Reduce number of adverse drug events • Detect cognitive impairment and depression • Improve mobility and reduce falls
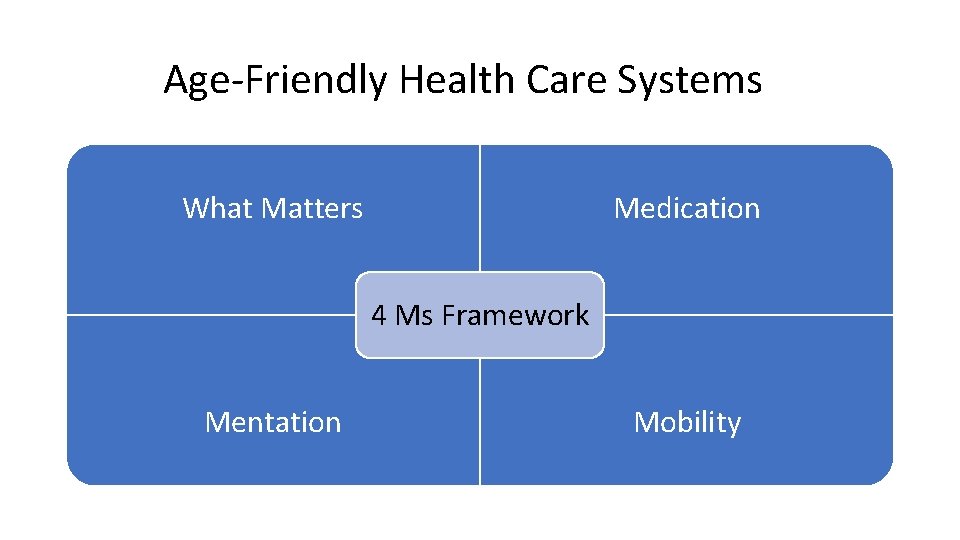
Age-Friendly Health Care Systems What Matters Medication 4 Ms Framework Mentation Mobility

4 Ms Framework • Four evidence-based interventions/barriers to age-friendly care: • What Matters- • Shared decision making (Nothing about me, without me) • Knowing and aligning care with older adult’s health outcome goals and care preferences • Medication- • Commission and omission of pharmacologic interventions • Reviewing when medications are necessary, prescribing only age-friendly medications, and only using medications that do not negatively impact what matters, mobility or mentation • Mentation- • Cognitive and affective changes that are age associated • Prevention, identification, treatment and management of dementia, delirium and depression • Mobility- • Importance of function to health and quality of life • Keeping older adult moving safely to maintain function and do what matter
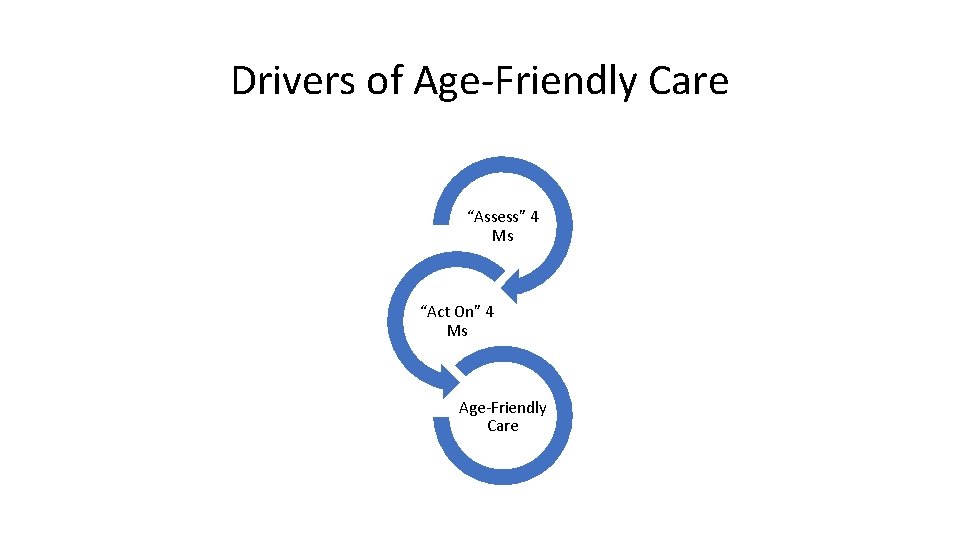
Drivers of Age-Friendly Care “Assess” 4 Ms “Act On” 4 Ms Age-Friendly Care
Assess What Matters • Know and align care plan with specific outcomes goals and care preferences • Including but not limited to end-of-life
Act on What Matters • Ask what matters most and document • Align care plan with what matters most
Assess Medications • Medications to screen for regularly • • Benzodiazepines Opioids Muscle Relaxants Tricyclic Antidepressants Antipsychotics Highly-Anticholinergic Medications (e. g. diphenhydramine (Benadryl) Prescription and over-the-counter (OTC) sedative and sleep medications Other
Act on Medications • Review high risk medications and document • Deprescribe or avoid high-risk medications and document/communicate changes • Pharmacy consult
Assess Mentation • Screen for delirium at least every 12 hours and document • CAM (Confusion Assessment Method) • UB-2 (Ultra-Brief 2 -Item Screener) • Psych referral
Act on Mentation • Ensure sufficient oral hydration • Orient to time, place, and situation every shift • Ensure personal adaptive equipment (e. g. glasses, hearing aids, dentures, walkers, canes) • Prevent sleep interruptions • Use non-pharmacological interventions to support sleep • Avoid-high-risk medications
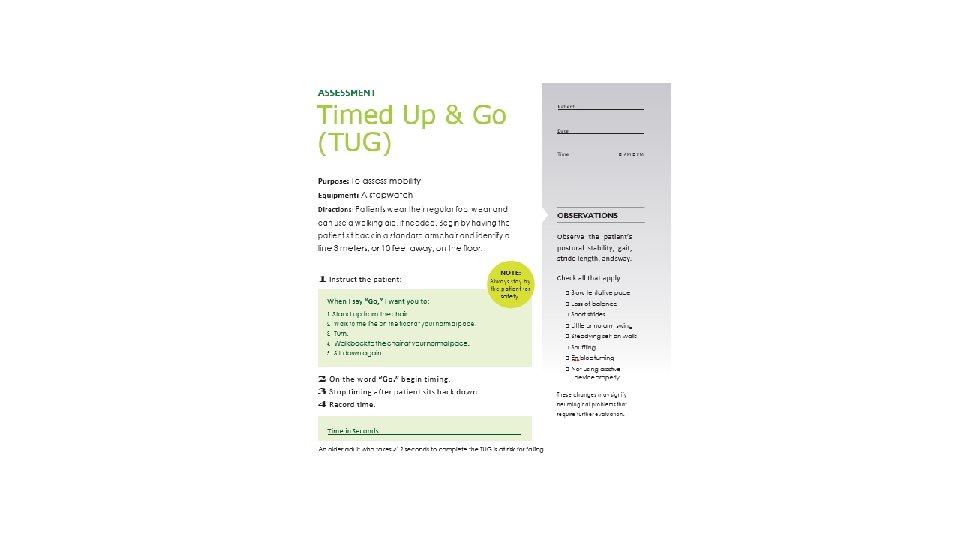
Assess Mobility • Screen for mobility and document • TUG • Get Up and Go • PT referral • Ensure early, frequent, and safe mobility
Act on Mobility • Ambulate 3 times a day • Out of bed or leave room for meals • PT (balance, gait, strength, gate training, exercise program) • Avoid restraints • Remove catheters and other tethering devices • Avoid high-risk medications
Clinical Exercise Complete the “Find the Application of the 4 Ms in Your Clinical Setting” handout during clinical today Be prepared to discuss your findings in post-conference including screenings and interpretations
References • Cacchione, P. Z. (2020). Age-Friendly Health Systems: The 4 Ms Framework. Clinical Nursing Research 29(3) 139 -140. • Institute for Healthcare Improvement. (2020). Age-Friendly Health Systems Action Community: Getting Started Checklist. • Institute for Healthcare Improvement. (2019). Age-Friendly Health Systems: Guide to Using the 4 Ms in the Care of Older Adults. • O’Neill, D. et al. , (2020). Primary prevention statins in older adults: personalized care for a heterogeneous population. Journal of the American Geriatrics Society, https: //doi. org. /10. 1111/jgs. 16330. • Pettis, J. (2020). Nurses leading the way to age-friendly care using the 4 Ms model. Geriatric Nursing, https: //doi. org/10. 1016/j. gerinurse. 2020. 03. 010
- Slides: 20