Objectives for Lecture on Pharmacotherapy of Hypertension By
Objectives for Lecture on Pharmacotherapy of Hypertension • By the end of this class students will be able to: • Describe the epidemiology of essential hypertension and explain the goals and importance of blood pressure control • Classify the severity of hypertension • Match the recommended diet/lifestyle changes and pharmacotherapy to the severity of hypertension • Name the major drugs and drug classes used to reduce blood pressure • Describe the actions in the body of each drug, explain the mechanism by which it produces those actions and explain why the drug is useful in treating hypertension
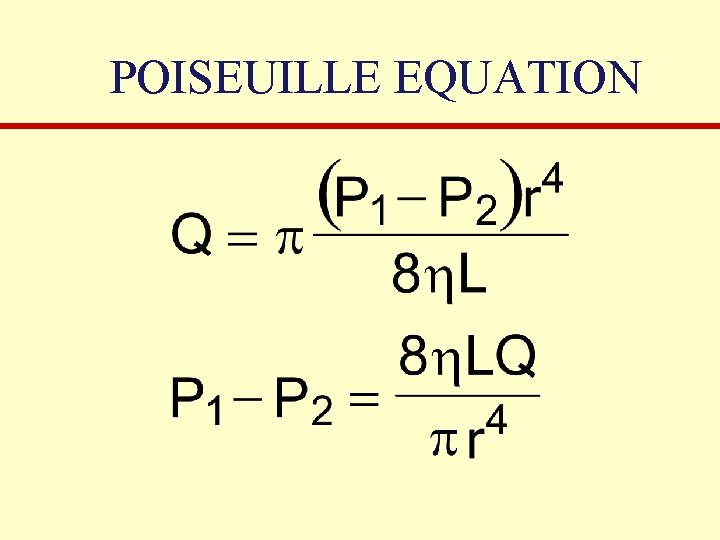
POISEUILLE EQUATION
Blood Pressure Variables • P 1 – Mean arterial pressure • P 2 – Central venous pressure (relatively low and essentially constant) • Q – Cardiac output • η – Viscosity • L – Length of the vasculature • R – Radius of the arterioles • Large effect on blood pressure with little change in r
Key References for Antihypertensive Therapy • 7 th report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). JAMA, 289, 2560 -2571 (2003). • 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults (JNC 8). JAMA, 311, 507 -520 (2014). • An Effective Approach to High Blood Pressure Control: A Science Advisory From the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension, 63, 878 -885 (2014). • Clinical practice guidelines for the management of hypertension in the community. J. Clin. Hypertens. , 32, 3 -15 (2014).
Essential Hypertension • Arbitrarily defined as a blood pressure >140/90 mm Hg. • Hypertension is a symptom, not a disease. The underlying disease is a cardiovascular abnormality that leads to morbid events. • Many causes, all thought to be genetic in origin. • Environmental and psychosocial factors interact with the genetic background to produce the hypertensive phenotype.
Major Risk Factors • • Cigarette smoking Obesity (BMI 30) Physical inactivity Dyslipidemia Diabetes mellitus Microalbuminemia or GFR <60 m. L/min Age (>55 yr for men, >65 yr for women) Family history of premature cardiovascular disease (<55 yr for men, <65 yr for women)
Secondary Hypertension • Examination should seek to exclude this possibility • Physical findings suggestive of secondary hypertension: • Abdominal or flank masses (polycystic kidneys) • Abdominal bruits (renovascular disease) • Delayed or absent femoral arterial pulses or BP in lower extremities (aortic coarctation) • Truncal obesity with pigmented striae (Cushing’s syndrome) • Tachycardia, orthostatic hypotension, sweating, pallor (pheochromocytoma)
Diagnosis • Based on two or more blood pressure measurements with the patient seated. Average of the readings should be used. • Confirmed with measurements taken during two or more office visits. • Verification in the contralateral arm. • At home monitoring recommended in Europe to avoid the phenomenon of “white coat hypertension”
Hypertension Contributes to or Exacerbates: • • Atherosclerosis Coronary artery disease Congestive heart failure* Diabetes Stroke* Renal failure* Retinal disease
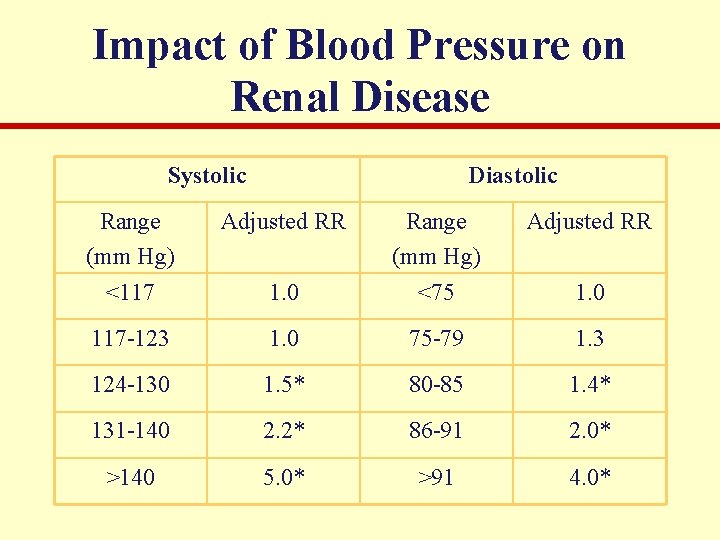
Impact of Blood Pressure on Renal Disease Systolic Diastolic Range (mm Hg) <117 Adjusted RR 1. 0 Range (mm Hg) <75 117 -123 1. 0 75 -79 1. 3 124 -130 1. 5* 80 -85 1. 4* 131 -140 2. 2* 86 -91 2. 0* >140 5. 0* >91 4. 0* 1. 0
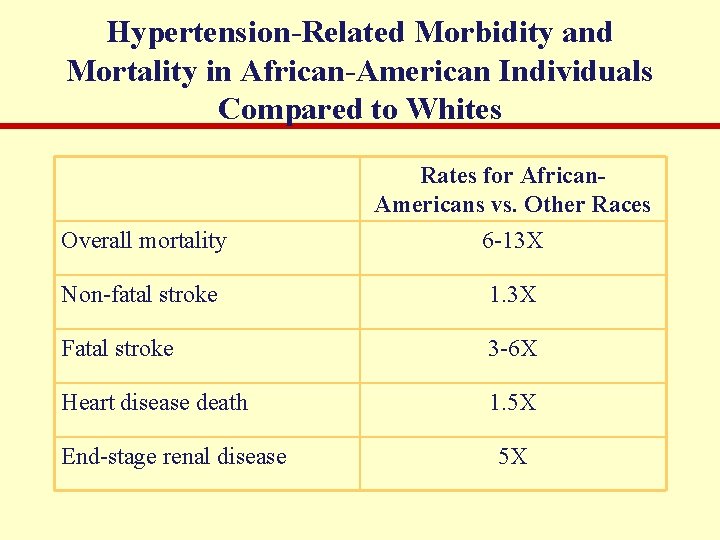
Hypertension-Related Morbidity and Mortality in African-American Individuals Compared to Whites Overall mortality Rates for African. Americans vs. Other Races 6 -13 X Non-fatal stroke 1. 3 X Fatal stroke 3 -6 X Heart disease death 1. 5 X End-stage renal disease 5 X
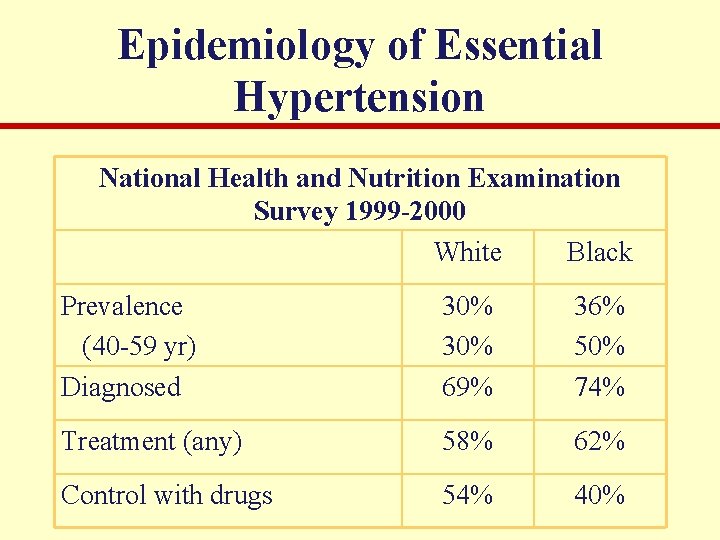
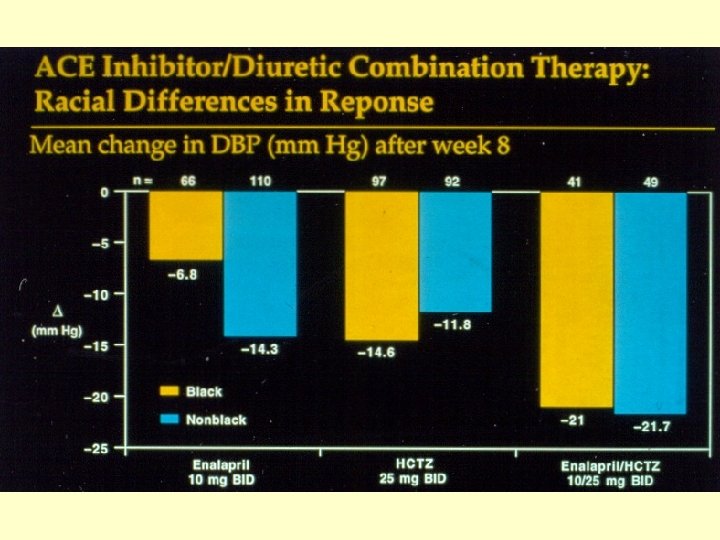
Epidemiology of Essential Hypertension National Health and Nutrition Examination Survey 1999 -2000 White Black Prevalence (40 -59 yr) Diagnosed 30% 69% 36% 50% 74% Treatment (any) 58% 62% Control with drugs 54% 40%
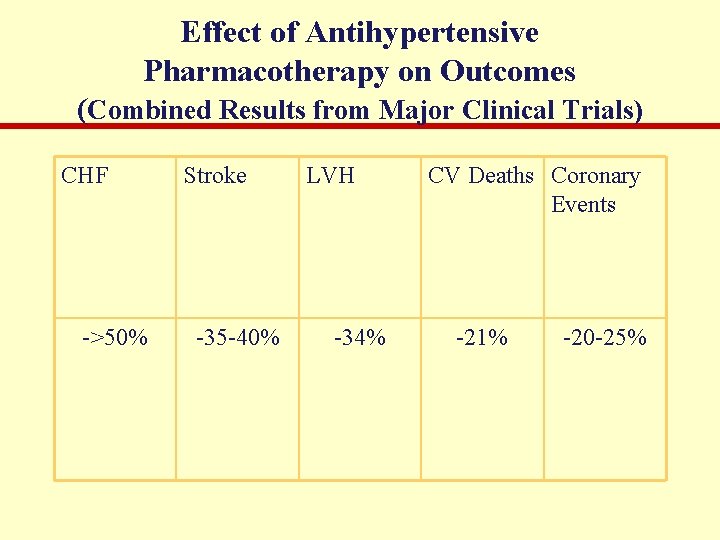
Effect of Antihypertensive Pharmacotherapy on Outcomes (Combined Results from Major Clinical Trials) CHF ->50% Stroke -35 -40% LVH -34% CV Deaths Coronary Events -21% -20 -25%
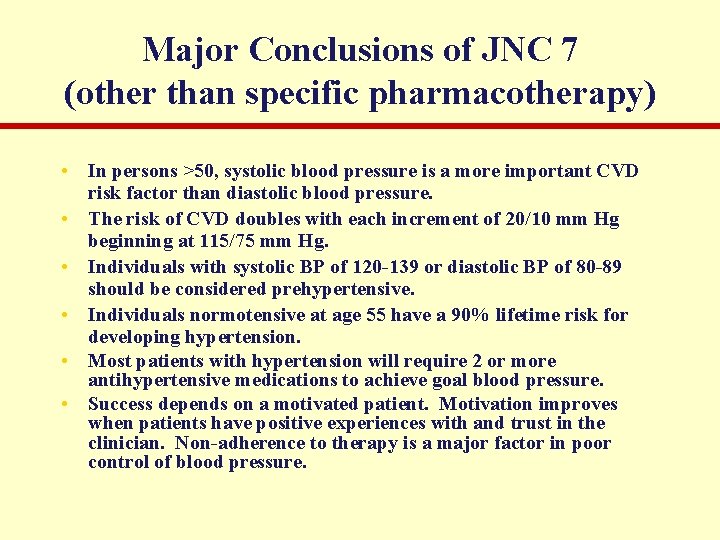
Major Conclusions of JNC 7 (other than specific pharmacotherapy) • In persons >50, systolic blood pressure is a more important CVD risk factor than diastolic blood pressure. • The risk of CVD doubles with each increment of 20/10 mm Hg beginning at 115/75 mm Hg. • Individuals with systolic BP of 120 -139 or diastolic BP of 80 -89 should be considered prehypertensive. • Individuals normotensive at age 55 have a 90% lifetime risk for developing hypertension. • Most patients with hypertension will require 2 or more antihypertensive medications to achieve goal blood pressure. • Success depends on a motivated patient. Motivation improves when patients have positive experiences with and trust in the clinician. Non-adherence to therapy is a major factor in poor control of blood pressure.
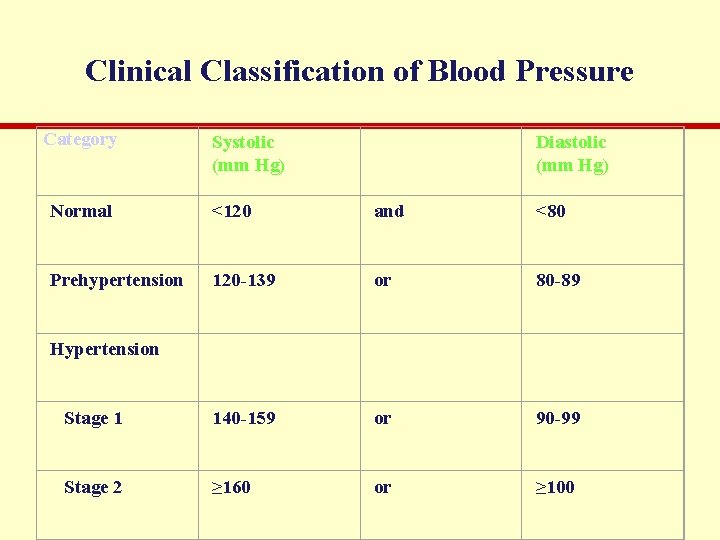
Clinical Classification of Blood Pressure Category Systolic (mm Hg) Diastolic (mm Hg) Normal <120 and <80 Prehypertension 120 -139 or 80 -89 Stage 1 140 -159 or 90 -99 Stage 2 ≥ 160 or ≥ 100 Hypertension
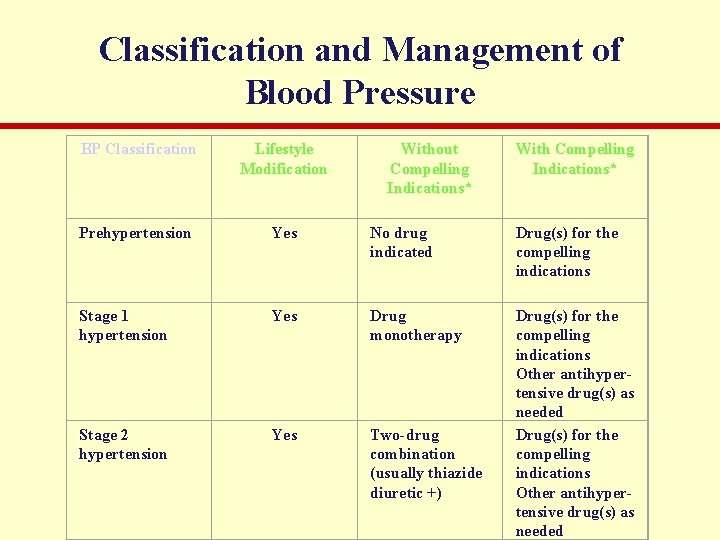
Classification and Management of Blood Pressure BP Classification Lifestyle Modification Without Compelling Indications* With Compelling Indications* Prehypertension Yes No drug indicated Drug(s) for the compelling indications Stage 1 hypertension Yes Drug monotherapy Stage 2 hypertension Yes Two-drug combination (usually thiazide diuretic +) Drug(s) for the compelling indications Other antihypertensive drug(s) as needed
![Compelling Indications • Congestive heart failure (diuretic, beta blocker, ACE inhibitor [or ARB], aldosterone Compelling Indications • Congestive heart failure (diuretic, beta blocker, ACE inhibitor [or ARB], aldosterone](http://slidetodoc.com/presentation_image_h2/4c59449f9fab09d671a980aa6b17413b/image-18.jpg)
Compelling Indications • Congestive heart failure (diuretic, beta blocker, ACE inhibitor [or ARB], aldosterone antagonist) • Post-myocardial infarction (beta blocker, ACE inhibitor [or ARB], aldosterone antagonist) • High coronary disease risk (diuretic, beta blocker, ACE inhibitor [or ARB], calcium channel blocker) • Recurrent stroke prevention (diuretic, ACE inhibitor [or ARB]) • Note that ACE inhibitor/ARB should be the first or second drug used to treat hypertension in the presence of diabetes, post-MI, or chronic kidney disease.
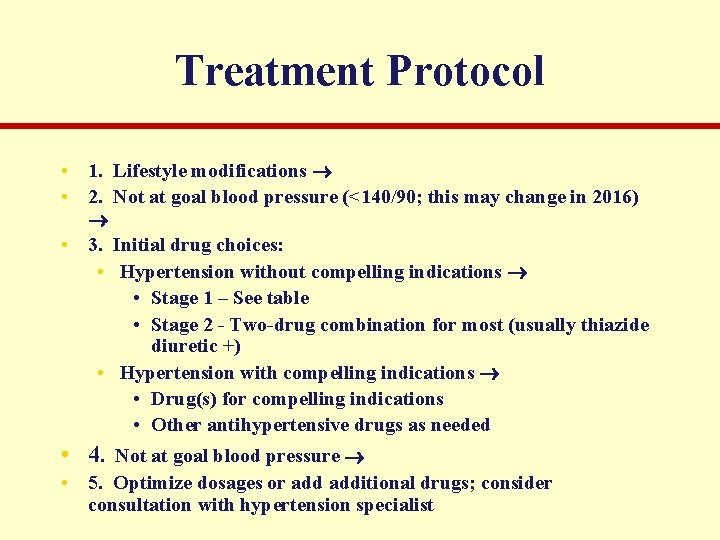
Treatment Protocol • 1. Lifestyle modifications • 2. Not at goal blood pressure (<140/90; this may change in 2016) • 3. Initial drug choices: • Hypertension without compelling indications • Stage 1 – See table • Stage 2 - Two-drug combination for most (usually thiazide diuretic +) • Hypertension with compelling indications • Drug(s) for compelling indications • Other antihypertensive drugs as needed • 4. Not at goal blood pressure • 5. Optimize dosages or additional drugs; consider consultation with hypertension specialist
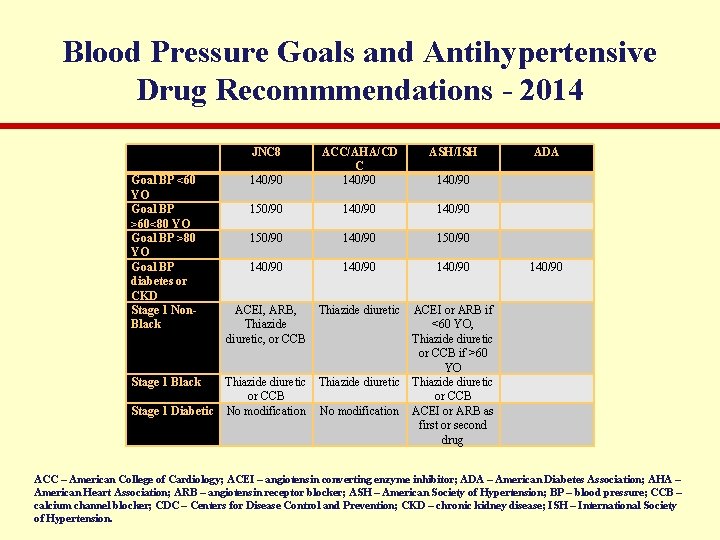
Blood Pressure Goals and Antihypertensive Drug Recommmendations - 2014 JNC 8 Goal BP <60 YO Goal BP >60<80 YO Goal BP >80 YO Goal BP diabetes or CKD Stage 1 Non. Black ASH/ISH 140/90 ACC/AHA/CD C 140/90 150/90 140/90 ACEI, ARB, Thiazide diuretic, or CCB Thiazide diuretic ADA 140/90 ACEI or ARB if <60 YO, Thiazide diuretic or CCB if >60 YO Stage 1 Black Thiazide diuretic or CCB Stage 1 Diabetic No modification ACEI or ARB as first or second drug ACC – American College of Cardiology; ACEI – angiotensin converting enzyme inhibitor; ADA – American Diabetes Association; AHA – American Heart Association; ARB – angiotensin receptor blocker; ASH – American Society of Hypertension; BP – blood pressure; CCB – calcium channel blocker; CDC – Centers for Disease Control and Prevention; CKD – chronic kidney disease; ISH – International Society of Hypertension.
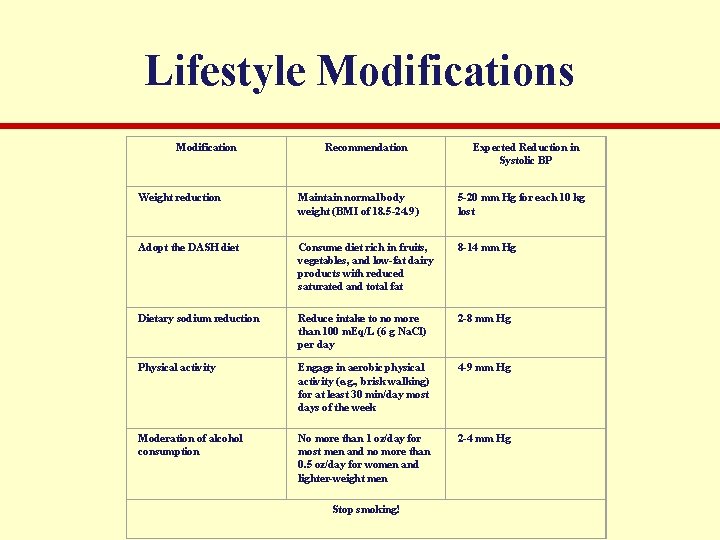
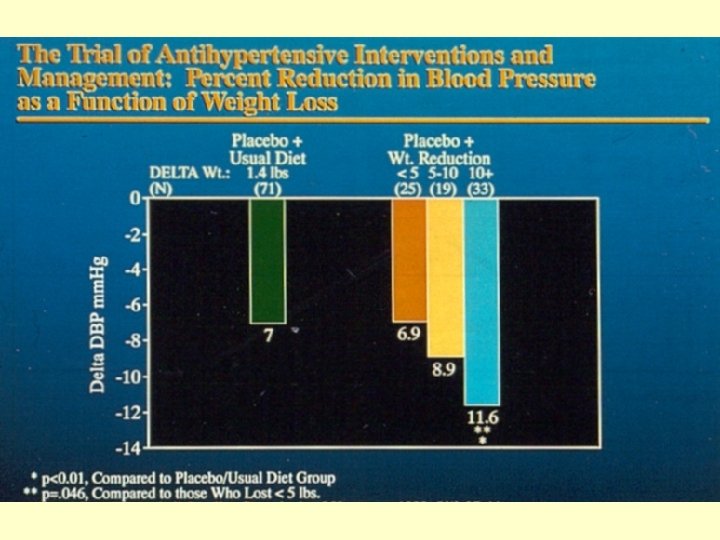
Lifestyle Modifications Modification Recommendation Expected Reduction in Systolic BP Weight reduction Maintain normal body weight (BMI of 18. 5 -24. 9) 5 -20 mm Hg for each 10 kg lost Adopt the DASH diet Consume diet rich in fruits, vegetables, and low-fat dairy products with reduced saturated and total fat 8 -14 mm Hg Dietary sodium reduction Reduce intake to no more than 100 m. Eq/L (6 g Na. Cl) per day 2 -8 mm Hg Physical activity Engage in aerobic physical activity (e. g. , brisk walking) for at least 30 min/day most days of the week 4 -9 mm Hg Moderation of alcohol consumption No more than 1 oz/day for most men and no more than 0. 5 oz/day for women and lighter-weight men 2 -4 mm Hg Stop smoking!
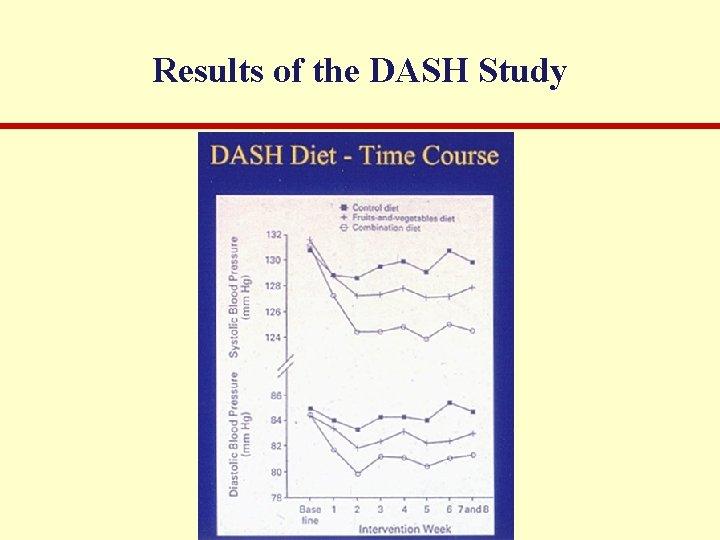
Results of the DASH Study
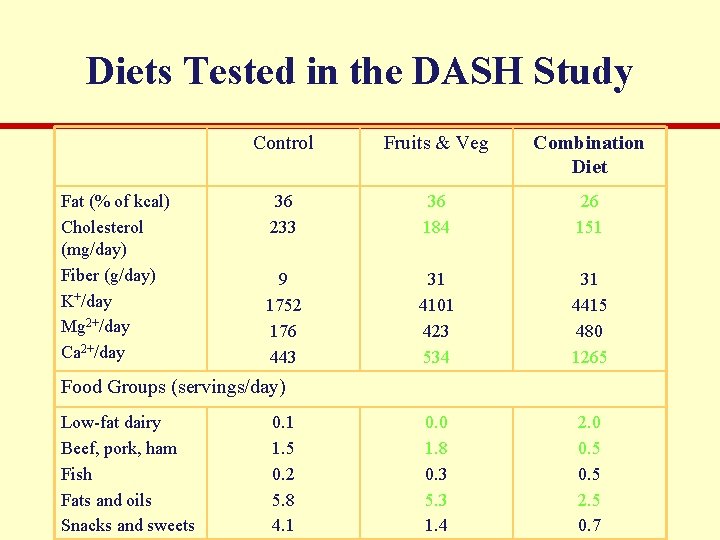
Diets Tested in the DASH Study Fat (% of kcal) Cholesterol (mg/day) Fiber (g/day) K+/day Mg 2+/day Ca 2+/day Control Fruits & Veg Combination Diet 36 233 36 184 26 151 9 1752 176 443 31 4101 423 534 31 4415 480 1265 0. 0 1. 8 0. 3 5. 3 1. 4 2. 0 0. 5 2. 5 0. 7 Food Groups (servings/day) Low-fat dairy Beef, pork, ham Fish Fats and oils Snacks and sweets 0. 1 1. 5 0. 2 5. 8 4. 1
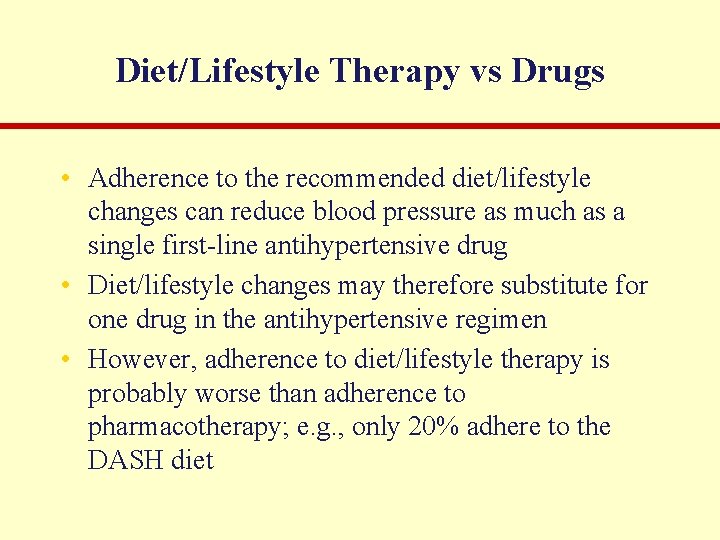
Diet/Lifestyle Therapy vs Drugs • Adherence to the recommended diet/lifestyle changes can reduce blood pressure as much as a single first-line antihypertensive drug • Diet/lifestyle changes may therefore substitute for one drug in the antihypertensive regimen • However, adherence to diet/lifestyle therapy is probably worse than adherence to pharmacotherapy; e. g. , only 20% adhere to the DASH diet
Antihypertensive Drugs • First-line; shown to reduce morbidity and mortality • Thiazide diuretics (chlorthalidone, hydrochlorothiazide) • ACE inhibitors (lisinopril) • AT 1 receptor antagonists (ARBs; candesartan) • Ca 2+ channel blockers (amlodipine) • Second-line • Beta blockers (atenolol, metoprolol, carvedilol, nebivolol) • Alpha blockers ( 1 -selective; prazosin) • Third line (for your reference only) • Sympatholytic agents (clonidine, reserpine, guanethidine) • Direct-acting vasodilators (hydralazine, minoxidil)
First-Line Antihypertensive Drugs Combat Cardiovascular Remodeling • Remodeling (resulting in arteriosclerosis and/or congestive heart failure) may include oxidative damage, overgrowth of smooth muscle or cardiac muscle, fibrosis, apoptosis of cardiac muscle, overgrowth of connective tissue, endothelial damage, etc. • Factors that promote remodeling include (among others) excess sodium, glucose, angiotensin II, catecholamines, aldosterone. NO inhibits remodeling. • First-line antihypertensive drugs reduce cardiovascular morbidity and mortality even if they little reduce blood pressure. This additional benefit, beyond that provided by blood pressure reduction, may be explained by inhibition or reversal of remodeling.
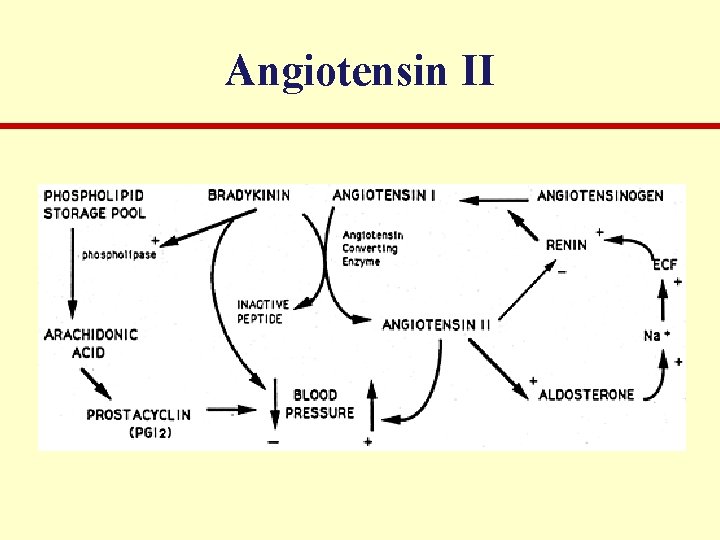
Angiotensin II
ACE Inhibitors • Molecular Mechanism • Competitive inhibition of angiotensin converting enzyme (kininase II)* • Physiological Mechanisms • Block of angiotensin II-mediated vasoconstriction* • norepinephrine release by block of angiotensin IImediated enhancement • sympathetic outflow from the brain stem • bradykinin-mediated vasodilation • aldosterone secretion (reverses in many cases)* • Block of angiotensin II-mediated arterial and left ventricular remodeling*
ACE Inhibitors • Other Actions • Dry cough (partly caused by bradykinin)* • Rapid swelling of nose, throat, mouth, tongue (angioedema; partly caused by bradykinin)* • Teratogenesis in the second and third trimesters* • Hyperkalemia (in the absence of diuretic)*
AT 1 Receptor Blockers (ARBs) • Molecular Mechanism • Competitive antagonism of angiotensin II at the AT 1 receptor* • Physiological Mechanisms • Block of angiotensin II-mediated vasoconstriction* • norepinephrine release by block of angiotensin IImediated enhancement • sympathetic outflow from the brain stem • aldosterone secretion (reverses in many cases)* • Block of angiotensin II-mediated left ventricular remodeling*
AT 1 Receptor Blockers • No change in bradykinin levels • Much lower risk of dry cough than with ACE inhibitors* • Much lower risk of angioedema than with ACE inhibitors* • As teratogenic as ACE inhibitors* • Hyperkalemia (in the absence of diuretic)* • No benefit to combining ACE inhibitor and ARB
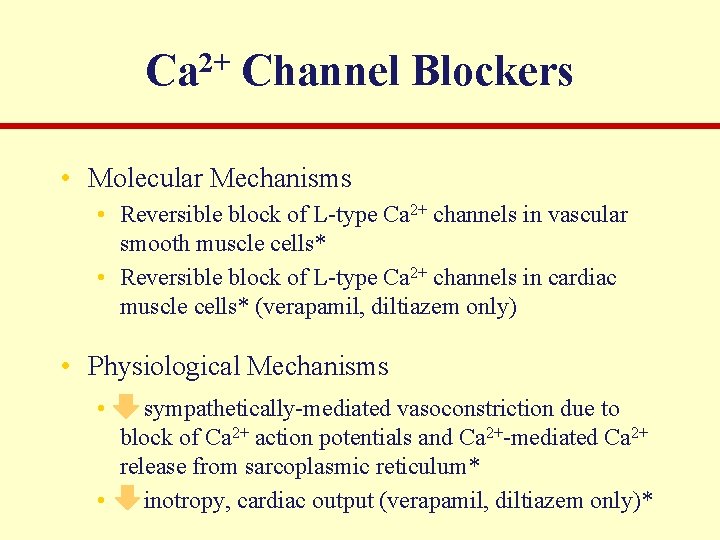
2+ Ca Channel Blockers • Molecular Mechanisms • Reversible block of L-type Ca 2+ channels in vascular smooth muscle cells* • Reversible block of L-type Ca 2+ channels in cardiac muscle cells* (verapamil, diltiazem only) • Physiological Mechanisms • sympathetically-mediated vasoconstriction due to block of Ca 2+ action potentials and Ca 2+-mediated Ca 2+ release from sarcoplasmic reticulum* • inotropy, cardiac output (verapamil, diltiazem only)*
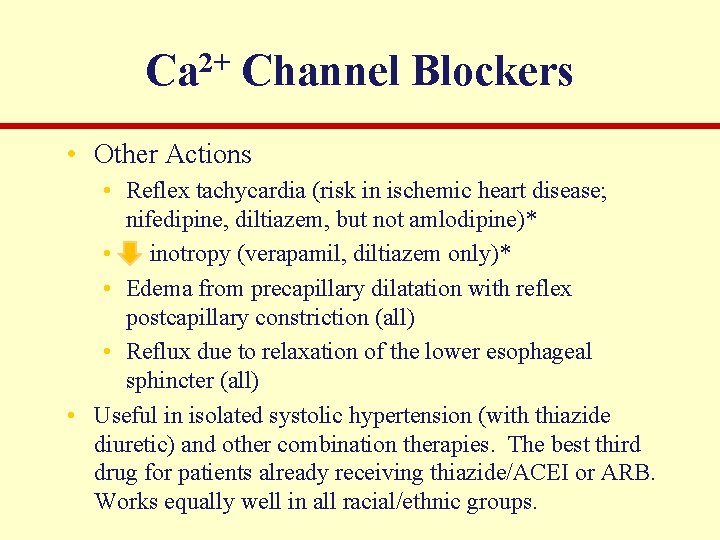
2+ Ca Channel Blockers • Other Actions • Reflex tachycardia (risk in ischemic heart disease; nifedipine, diltiazem, but not amlodipine)* • inotropy (verapamil, diltiazem only)* • Edema from precapillary dilatation with reflex postcapillary constriction (all) • Reflux due to relaxation of the lower esophageal sphincter (all) • Useful in isolated systolic hypertension (with thiazide diuretic) and other combination therapies. The best third drug for patients already receiving thiazide/ACEI or ARB. Works equally well in all racial/ethnic groups.
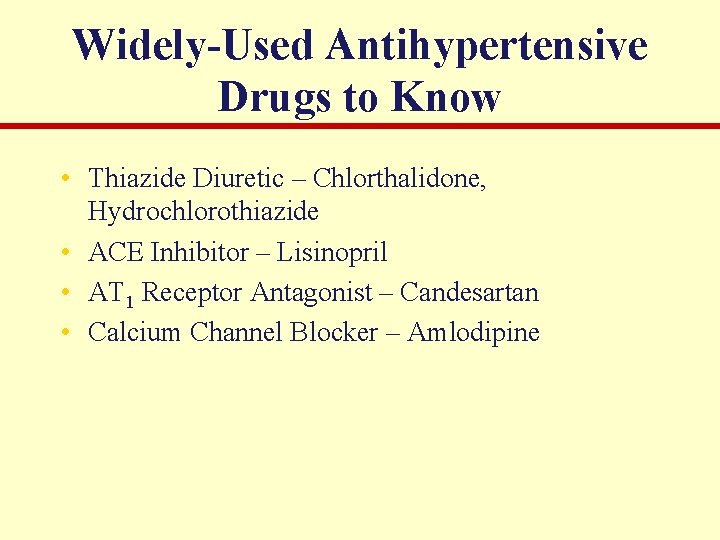
Widely-Used Antihypertensive Drugs to Know • Thiazide Diuretic – Chlorthalidone, Hydrochlorothiazide • ACE Inhibitor – Lisinopril • AT 1 Receptor Antagonist – Candesartan • Calcium Channel Blocker – Amlodipine
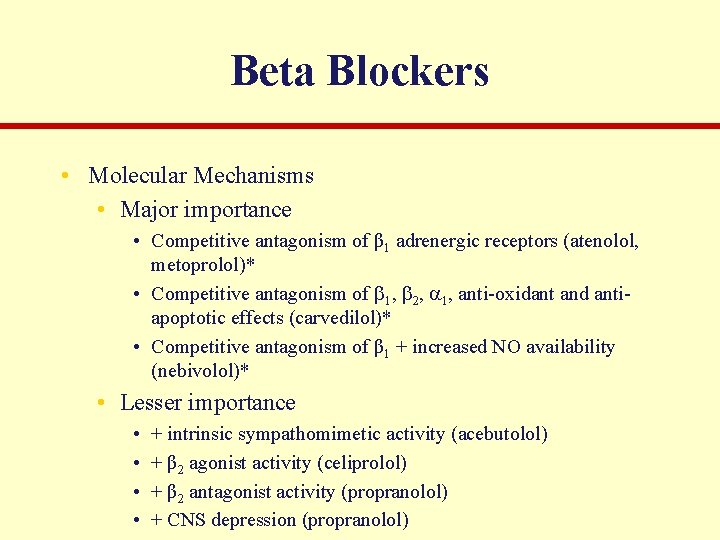
Beta Blockers • Molecular Mechanisms • Major importance • Competitive antagonism of β 1 adrenergic receptors (atenolol, metoprolol)* • Competitive antagonism of 1, 2, 1, anti-oxidant and antiapoptotic effects (carvedilol)* • Competitive antagonism of β 1 + increased NO availability (nebivolol)* • Lesser importance • • + intrinsic sympathomimetic activity (acebutolol) + β 2 agonist activity (celiprolol) + β 2 antagonist activity (propranolol) + CNS depression (propranolol)
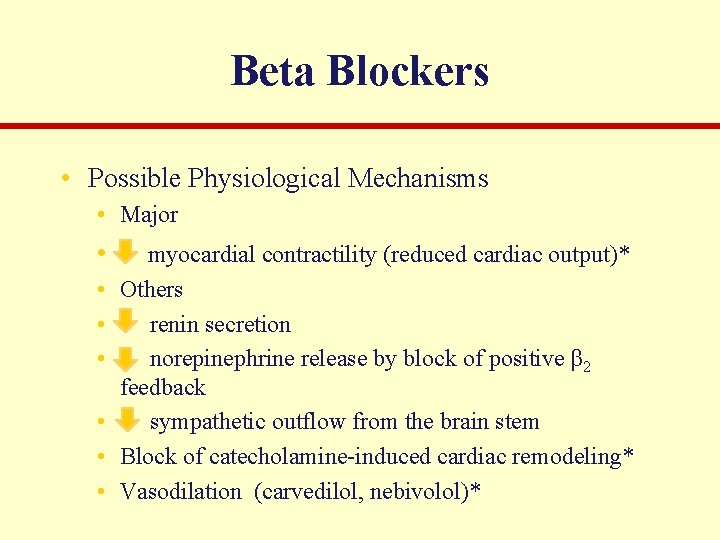
Beta Blockers • Possible Physiological Mechanisms • Major • • myocardial contractility (reduced cardiac output)* Others renin secretion norepinephrine release by block of positive β 2 feedback sympathetic outflow from the brain stem Block of catecholamine-induced cardiac remodeling* Vasodilation (carvedilol, nebivolol)*
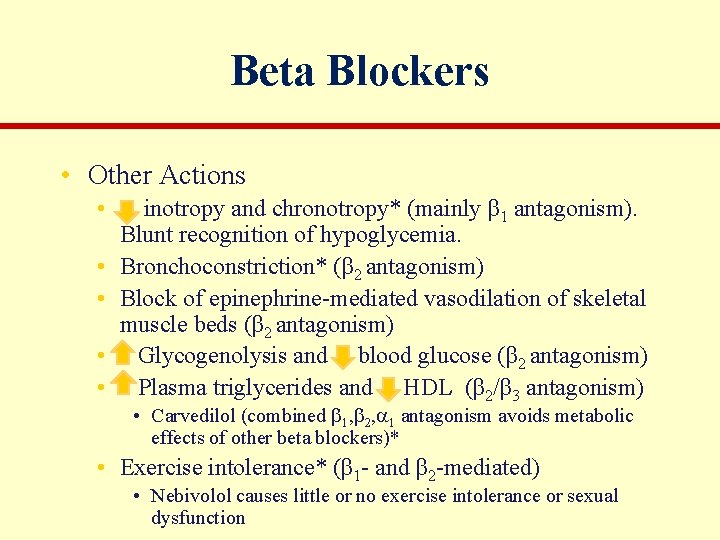
Beta Blockers • Other Actions • • • inotropy and chronotropy* (mainly β 1 antagonism). Blunt recognition of hypoglycemia. Bronchoconstriction* (β 2 antagonism) Block of epinephrine-mediated vasodilation of skeletal muscle beds (β 2 antagonism) Glycogenolysis and blood glucose (β 2 antagonism) Plasma triglycerides and HDL (β 2/β 3 antagonism) • Carvedilol (combined 1, 2, 1 antagonism avoids metabolic effects of other beta blockers)* • Exercise intolerance* (β 1 - and β 2 -mediated) • Nebivolol causes little or no exercise intolerance or sexual dysfunction
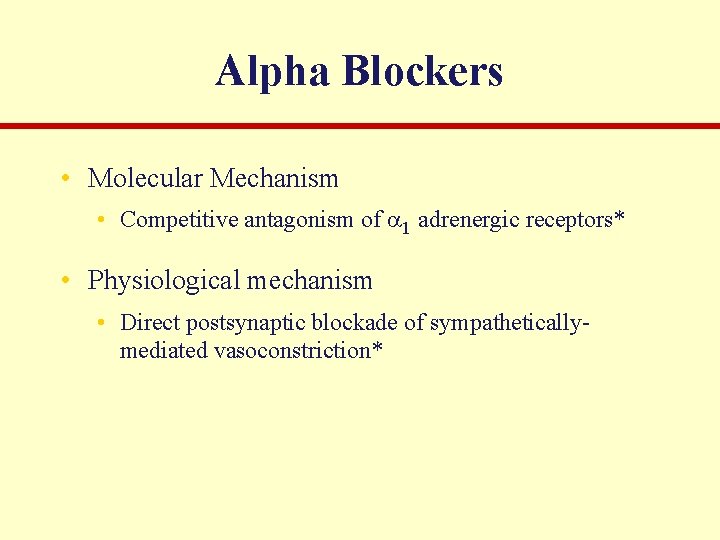
Alpha Blockers • Molecular Mechanism • Competitive antagonism of 1 adrenergic receptors* • Physiological mechanism • Direct postsynaptic blockade of sympatheticallymediated vasoconstriction*
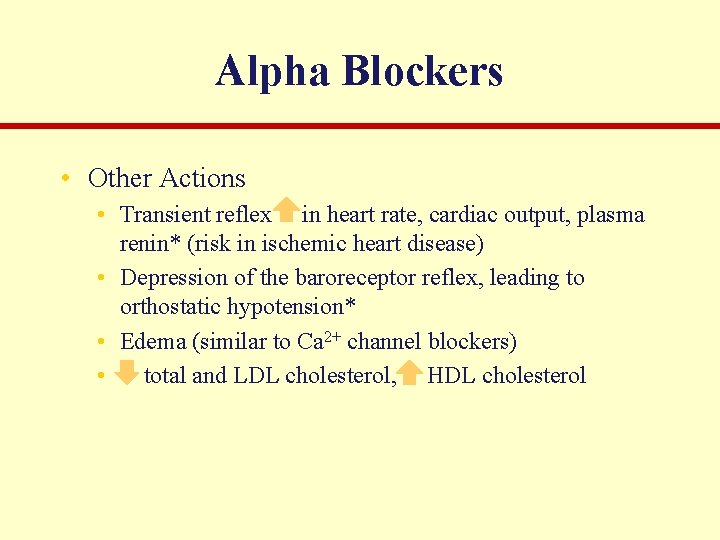
Alpha Blockers • Other Actions • Transient reflex in heart rate, cardiac output, plasma renin* (risk in ischemic heart disease) • Depression of the baroreceptor reflex, leading to orthostatic hypotension* • Edema (similar to Ca 2+ channel blockers) • total and LDL cholesterol, HDL cholesterol
Renin Antagonist • Aliskerin • Inhibits the renin-mediated conversion of angiotensinogen to angiotensin I • Appears to be as efficacious as ACE inhibitors with lower incidence of side effects • Counteracts the up regulation of renin by diuretics • Being used in combination therapies
- Slides: 42