Objective 7 Velocity of Blood Flow A The
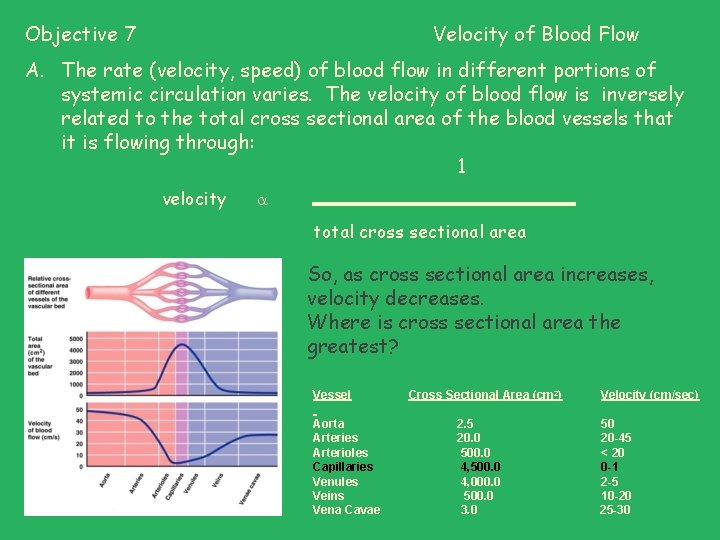
Objective 7 Velocity of Blood Flow A. The rate (velocity, speed) of blood flow in different portions of systemic circulation varies. The velocity of blood flow is inversely related to the total cross sectional area of the blood vessels that it is flowing through: 1 velocity total cross sectional area So, as cross sectional area increases, velocity decreases. Where is cross sectional area the greatest? Vessel Cross Sectional Area (cm 2) Velocity (cm/sec) Aorta 2. 5 50 Arteries 20. 0 20 -45 Arterioles 500. 0 < 20 Capillaries 4, 500. 0 0 -1 Venules 4, 000. 0 2 -5 Veins 500. 0 10 -20 Vena Cavae 3. 0 25 -30
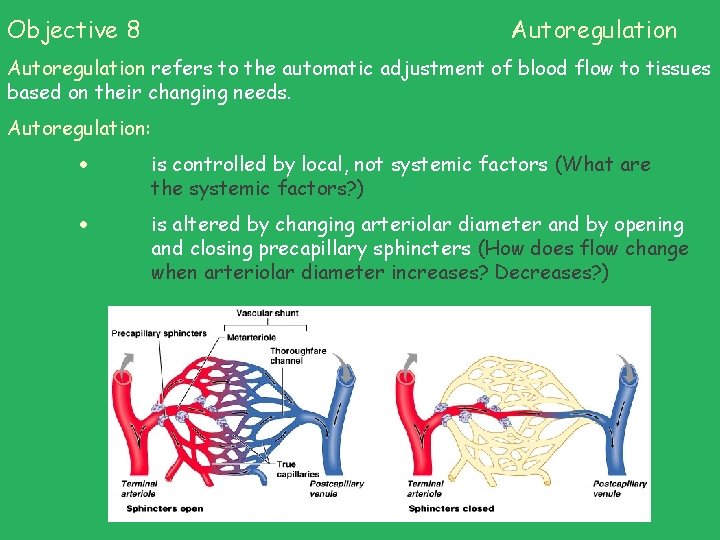
Objective 8 Autoregulation refers to the automatic adjustment of blood flow to tissues based on their changing needs. Autoregulation: is controlled by local, not systemic factors (What are the systemic factors? ) is altered by changing arteriolar diameter and by opening and closing precapillary sphincters (How does flow change when arteriolar diameter increases? Decreases? )
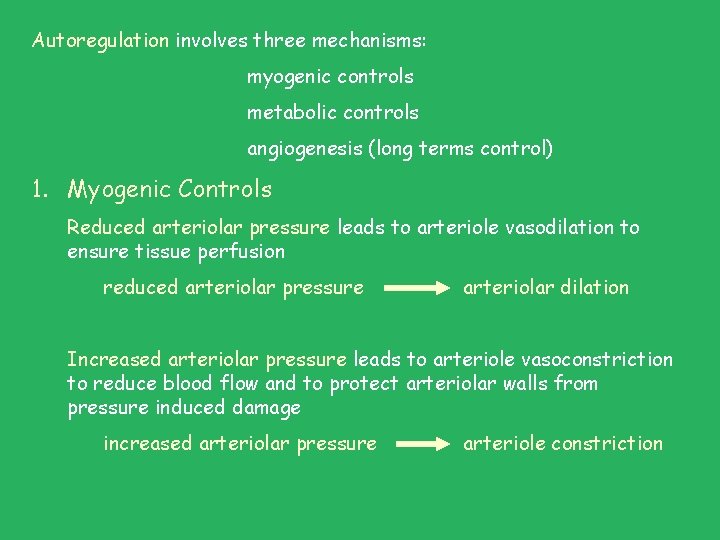
Autoregulation involves three mechanisms: myogenic controls metabolic controls angiogenesis (long terms control) 1. Myogenic Controls Reduced arteriolar pressure leads to arteriole vasodilation to ensure tissue perfusion reduced arteriolar pressure arteriolar dilation Increased arteriolar pressure leads to arteriole vasoconstriction to reduce blood flow and to protect arteriolar walls from pressure induced damage increased arteriolar pressure arteriole constriction
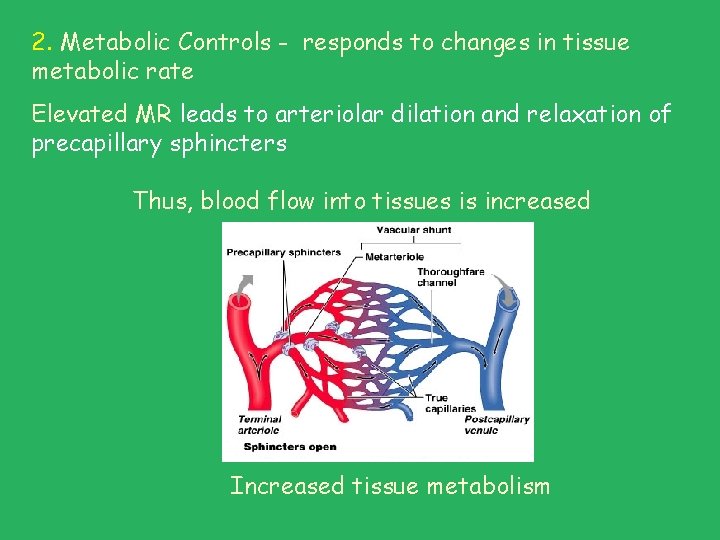
2. Metabolic Controls - responds to changes in tissue metabolic rate Elevated MR leads to arteriolar dilation and relaxation of precapillary sphincters Thus, blood flow into tissues is increased Increased tissue metabolism
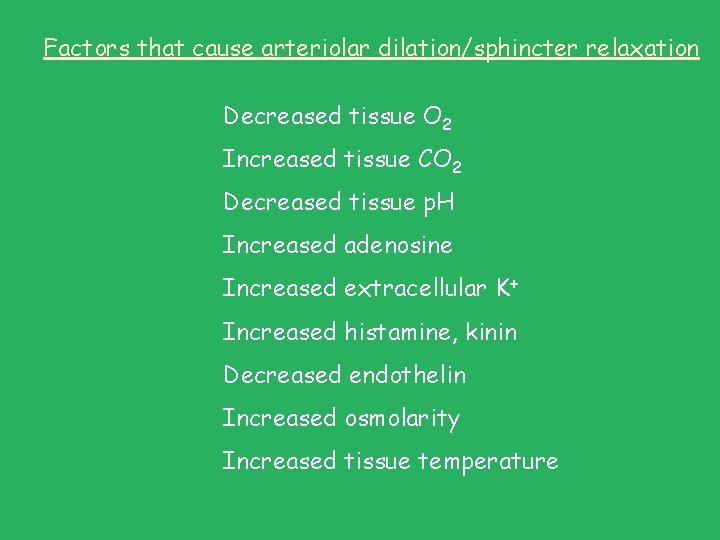
Factors that cause arteriolar dilation/sphincter relaxation Decreased tissue O 2 Increased tissue CO 2 Decreased tissue p. H Increased adenosine Increased extracellular K+ Increased histamine, kinin Decreased endothelin Increased osmolarity Increased tissue temperature
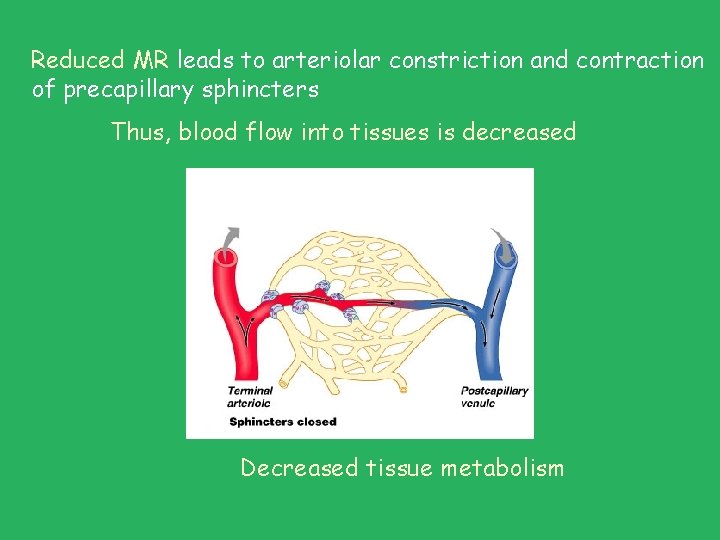
Reduced MR leads to arteriolar constriction and contraction of precapillary sphincters Thus, blood flow into tissues is decreased Decreased tissue metabolism
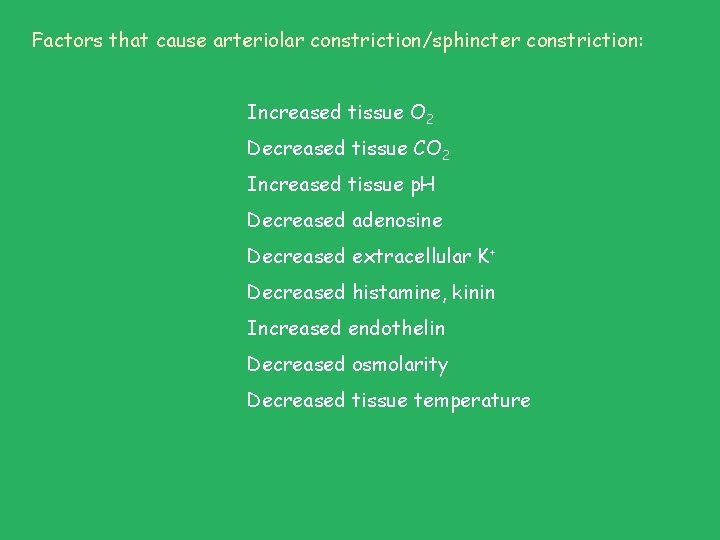
Factors that cause arteriolar constriction/sphincter constriction: Increased tissue O 2 Decreased tissue CO 2 Increased tissue p. H Decreased adenosine Decreased extracellular K+ Decreased histamine, kinin Increased endothelin Decreased osmolarity Decreased tissue temperature
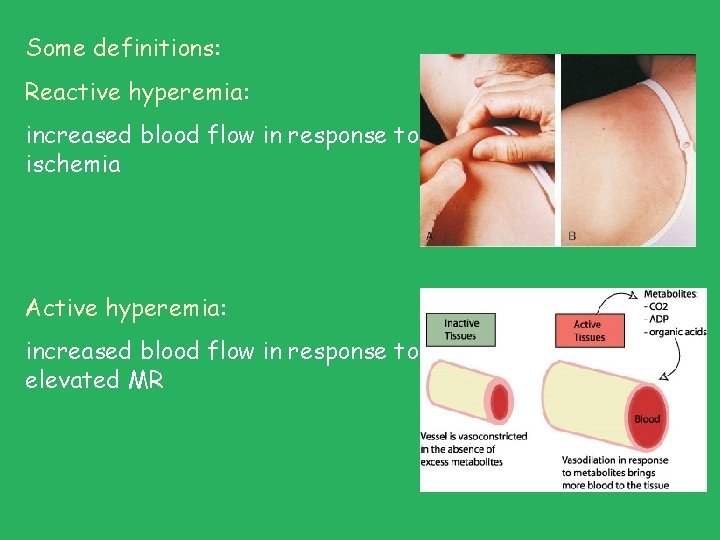
Some definitions: Reactive hyperemia: increased blood flow in response to ischemia Active hyperemia: increased blood flow in response to elevated MR
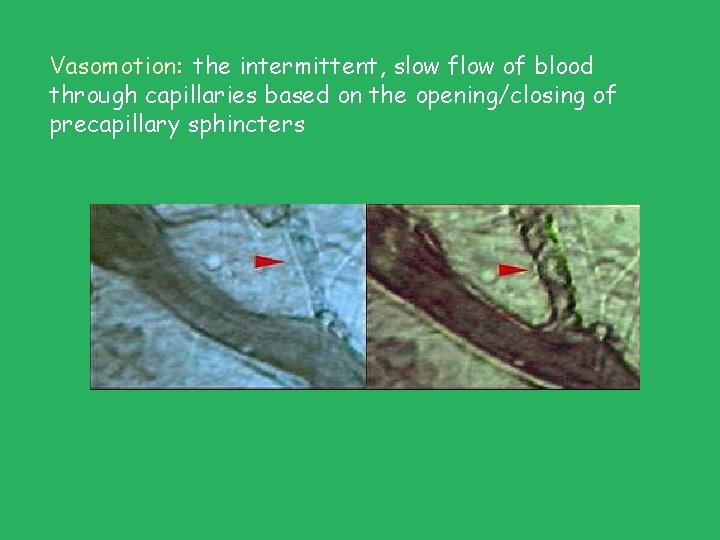
Vasomotion: the intermittent, slow flow of blood through capillaries based on the opening/closing of precapillary sphincters
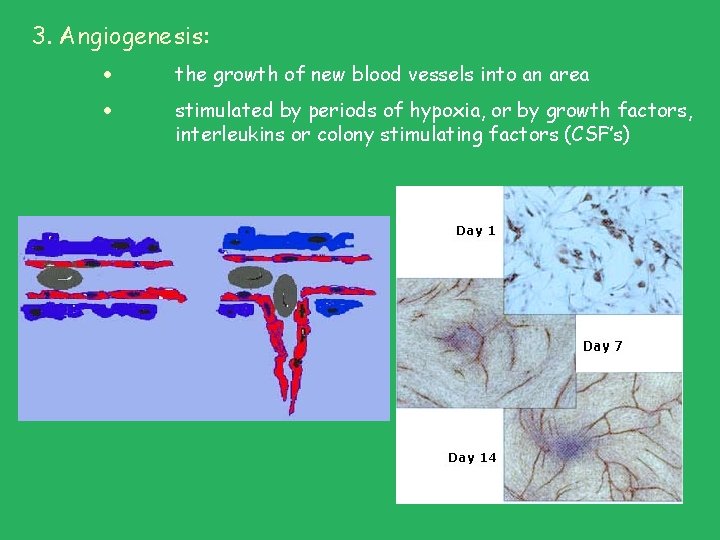
3. Angiogenesis: the growth of new blood vessels into an area stimulated by periods of hypoxia, or by growth factors, interleukins or colony stimulating factors (CSF’s)
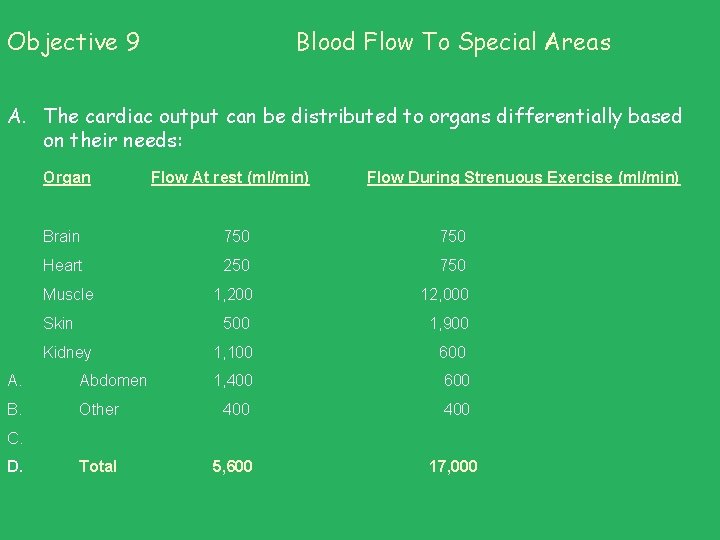
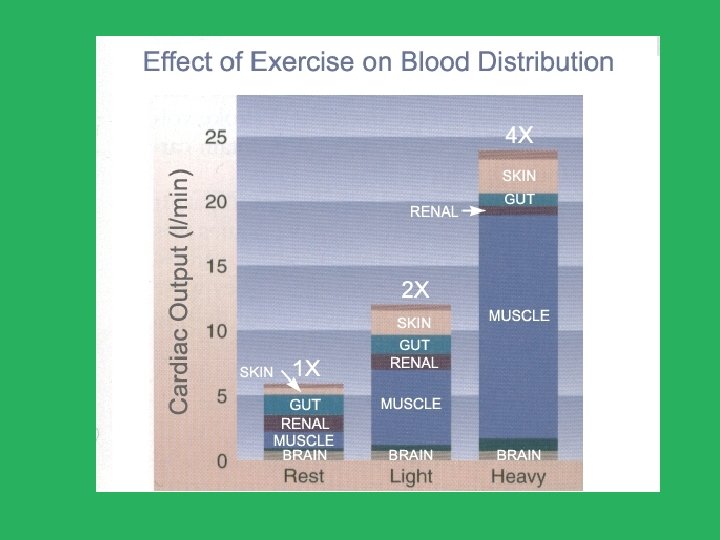
Objective 9 Blood Flow To Special Areas A. The cardiac output can be distributed to organs differentially based on their needs: Organ Flow At rest (ml/min) Flow During Strenuous Exercise (ml/min) Brain 750 Heart 250 750 1, 200 12, 000 500 1, 900 Muscle Skin Kidney 1, 100 600 A. Abdomen 1, 400 600 B. Other 400 Total 5, 600 C. D. 17, 000
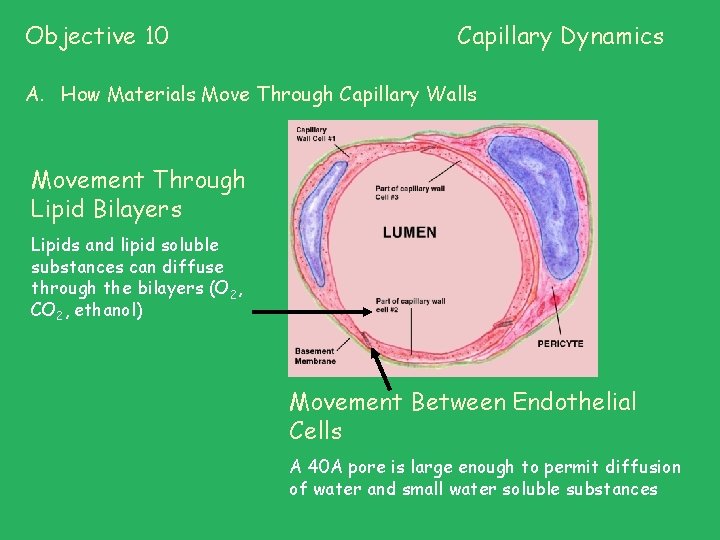
Objective 10 Capillary Dynamics A. How Materials Move Through Capillary Walls Movement Through Lipid Bilayers Lipids and lipid soluble substances can diffuse through the bilayers (O 2, CO 2, ethanol) Movement Between Endothelial Cells A 40 A pore is large enough to permit diffusion of water and small water soluble substances
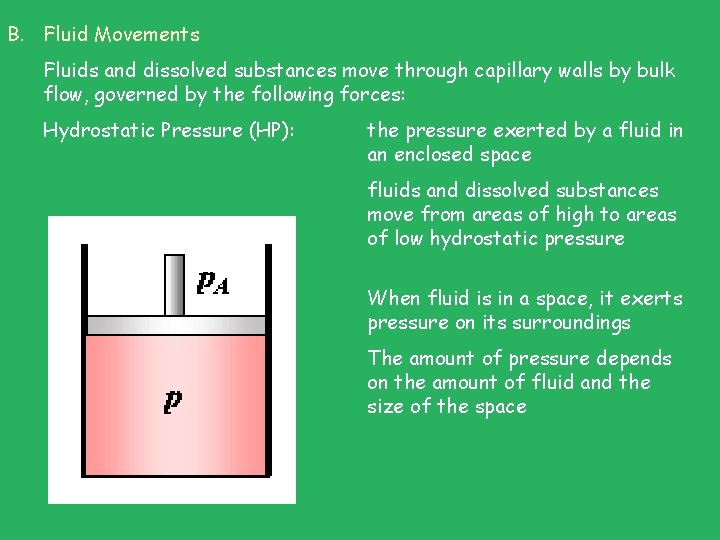
B. Fluid Movements Fluids and dissolved substances move through capillary walls by bulk flow, governed by the following forces: Hydrostatic Pressure (HP): the pressure exerted by a fluid in an enclosed space fluids and dissolved substances move from areas of high to areas of low hydrostatic pressure When fluid is in a space, it exerts pressure on its surroundings The amount of pressure depends on the amount of fluid and the size of the space
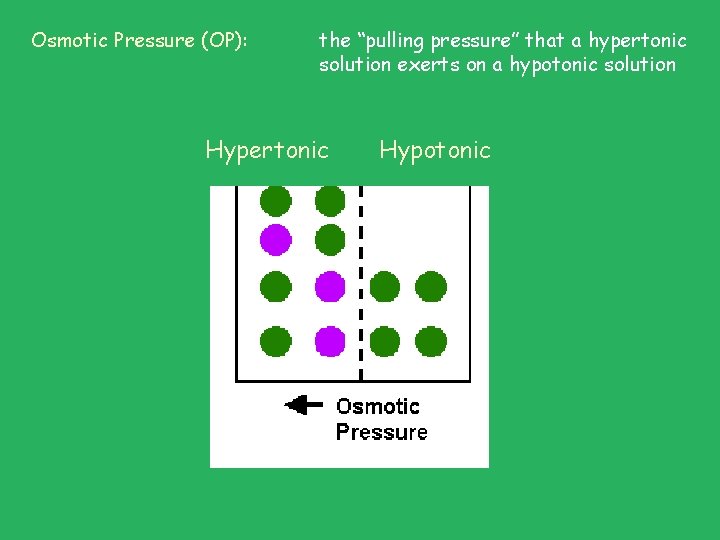
Osmotic Pressure (OP): the “pulling pressure” that a hypertonic solution exerts on a hypotonic solution Hypertonic Hypotonic
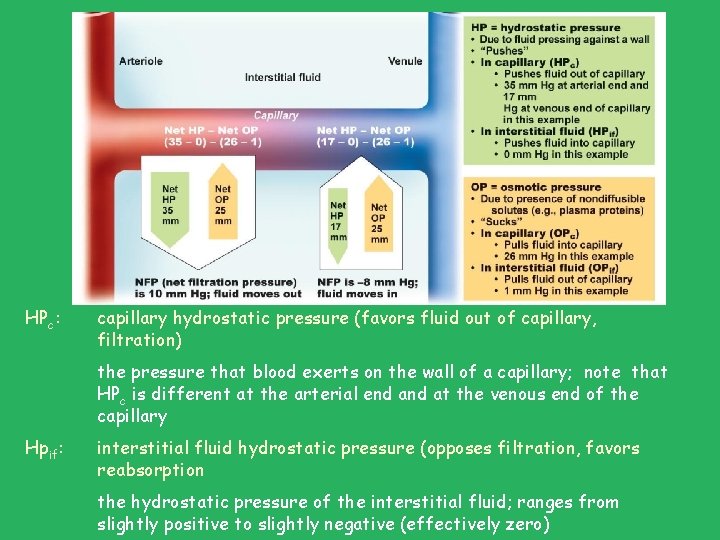
HPc: capillary hydrostatic pressure (favors fluid out of capillary, filtration) the pressure that blood exerts on the wall of a capillary; note that HPc is different at the arterial end at the venous end of the capillary Hpif: interstitial fluid hydrostatic pressure (opposes filtration, favors reabsorption the hydrostatic pressure of the interstitial fluid; ranges from slightly positive to slightly negative (effectively zero)
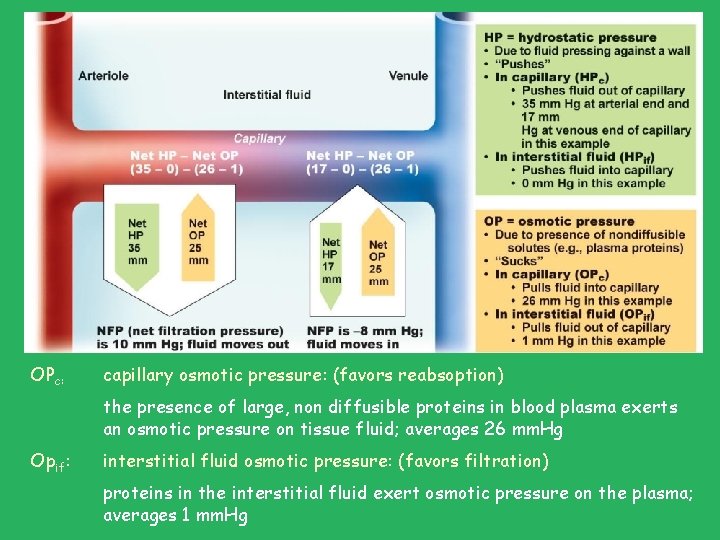
OPc: capillary osmotic pressure: (favors reabsoption) the presence of large, non diffusible proteins in blood plasma exerts an osmotic pressure on tissue fluid; averages 26 mm. Hg Opif: interstitial fluid osmotic pressure: (favors filtration) proteins in the interstitial fluid exert osmotic pressure on the plasma; averages 1 mm. Hg
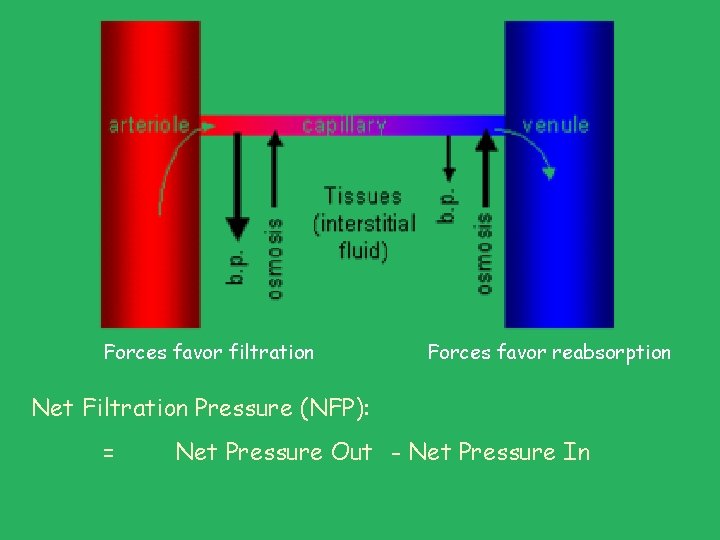
Forces favor filtration Forces favor reabsorption Net Filtration Pressure (NFP): = Net Pressure Out - Net Pressure In
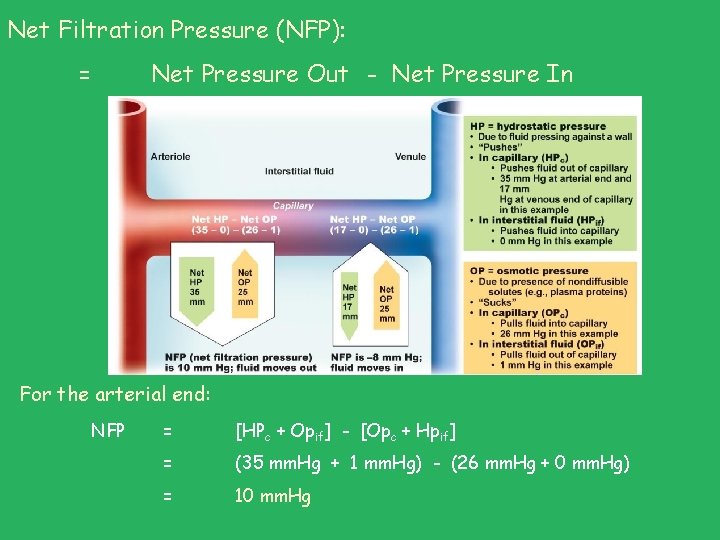
Net Filtration Pressure (NFP): = Net Pressure Out - Net Pressure In For the arterial end: NFP = [HPc + Opif] - [Opc + Hpif] = (35 mm. Hg + 1 mm. Hg) - (26 mm. Hg + 0 mm. Hg) = 10 mm. Hg
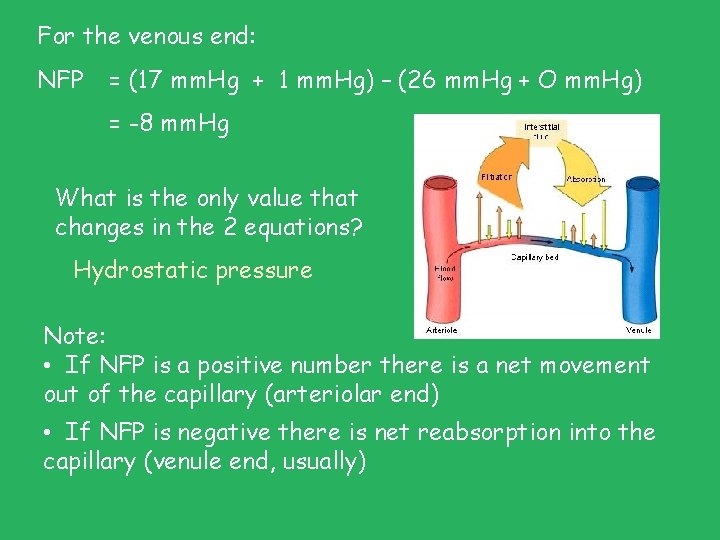
For the venous end: NFP = (17 mm. Hg + 1 mm. Hg) – (26 mm. Hg + O mm. Hg) = -8 mm. Hg What is the only value that changes in the 2 equations? Hydrostatic pressure Note: • If NFP is a positive number there is a net movement out of the capillary (arteriolar end) • If NFP is negative there is net reabsorption into the capillary (venule end, usually)
Lets try these: Your patient suffers from hypertension. Based on the following values predict the outcome at the capillary end of things. Here are the values: Arterial end: Venous end: • HPc = 45 mm. Hg HPc = 20 mm. Hg • Opif = 1 mm. Hg • Opc = 26 mm. Hg • Hpif = 0 mm. Hg
Your patient suffers from liver disease. Based on the following values predict the outcome at the capillary end of things. Here are the values: Arterial end: • HPc = 35 mm. Hg • Opif = 1 mm. Hg • Opc = 10 mm. Hg • Hpif = 0 mm. Hg Venous end: HPc = 17 mm. Hg Opif = 1 mm. Hg Opc = 10 mm. Hg Hpif = 0 mm. Hg
Your patient suffers from severe dehydration. Based on the following values predict the outcome at the capillary end of things. Here are the values: Arterial end: • HPc = 35 mm. Hg • Opif = 1 mm. Hg • Opc = 37 mm. Hg • Hpif = 0 mm. Hg Venous end: HPc = 17 mm. Hg Opif = 1 mm. Hg Opc = 37 mm. Hg Hpif = 0 mm. Hg
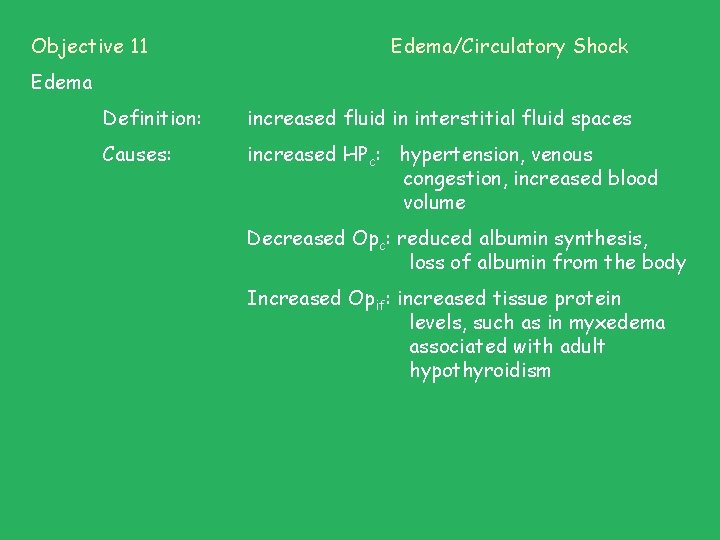
Objective 11 Edema/Circulatory Shock Edema Definition: increased fluid in interstitial fluid spaces Causes: increased HPc: hypertension, venous congestion, increased blood volume Decreased Opc: reduced albumin synthesis, loss of albumin from the body Increased Opif: increased tissue protein levels, such as in myxedema associated with adult hypothyroidism

Lymphatic Obstruction Lymphedema, left leg Myxedema, reversible with thyroid hormone Filariasis
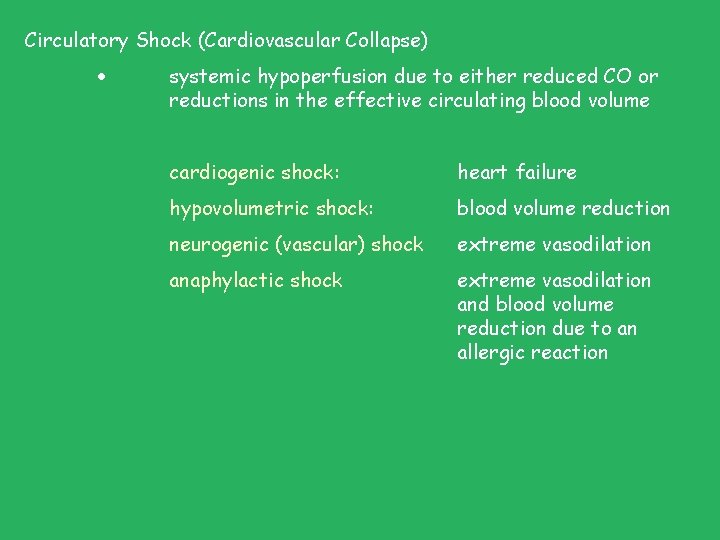
Circulatory Shock (Cardiovascular Collapse) systemic hypoperfusion due to either reduced CO or reductions in the effective circulating blood volume cardiogenic shock: heart failure hypovolumetric shock: blood volume reduction neurogenic (vascular) shock extreme vasodilation anaphylactic shock extreme vasodilation and blood volume reduction due to an allergic reaction
- Slides: 26