Objective 20 Location Functions and Gross Anatomy of
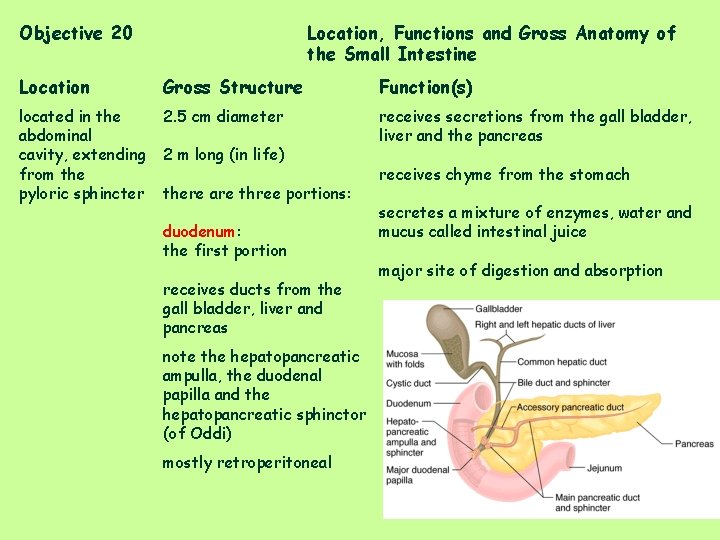
Objective 20 Location, Functions and Gross Anatomy of the Small Intestine Location Gross Structure Function(s) located in the abdominal cavity, extending from the pyloric sphincter 2. 5 cm diameter receives secretions from the gall bladder, liver and the pancreas 2 m long (in life) there are three portions: duodenum: the first portion receives ducts from the gall bladder, liver and pancreas note the hepatopancreatic ampulla, the duodenal papilla and the hepatopancreatic sphinctor (of Oddi) mostly retroperitoneal receives chyme from the stomach secretes a mixture of enzymes, water and mucus called intestinal juice major site of digestion and absorption
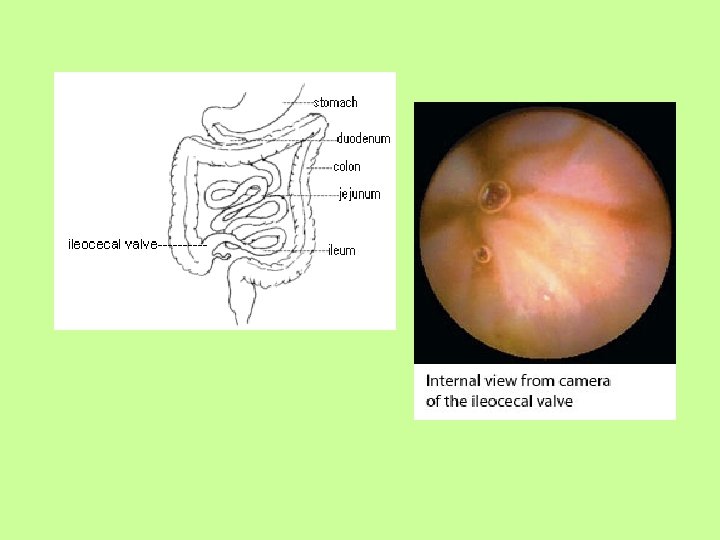
jejunum: second portion extends from the duodenum to the ileum is intraperitoneal supported by mesntery ileum: last portion extends from the jejunum to the cecum note the ileocecal valve is intraperitoneal supported by mesentery The nerve supply is parasympathetic (vagus) and sympathetic (thoracic nerves via the superior mesenteric and celiac plexus)
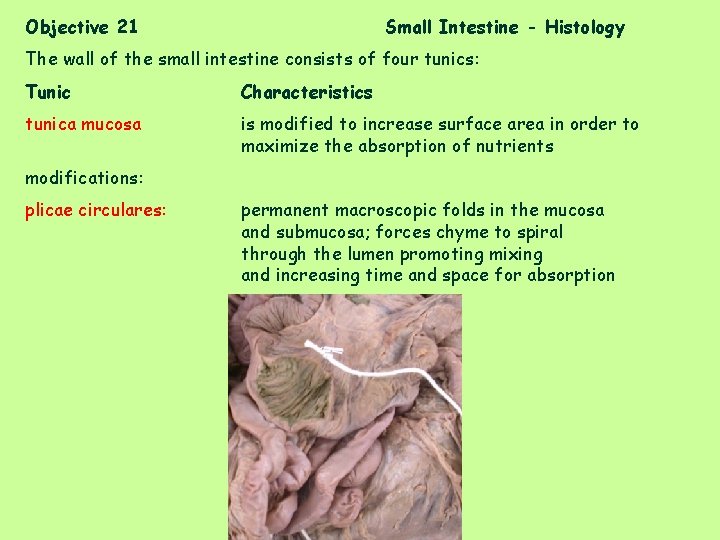
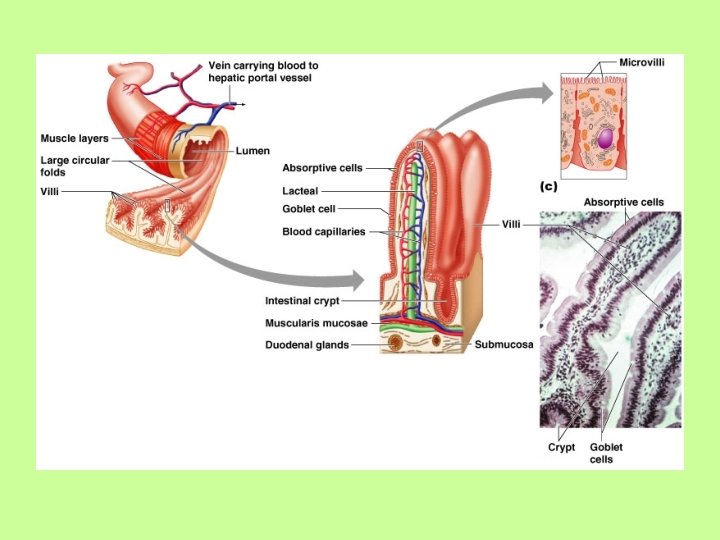
Objective 21 Small Intestine - Histology The wall of the small intestine consists of four tunics: Tunic Characteristics tunica mucosa is modified to increase surface area in order to maximize the absorption of nutrients modifications: plicae circulares: permanent macroscopic folds in the mucosa and submucosa; forces chyme to spiral through the lumen promoting mixing and increasing time and space for absorption
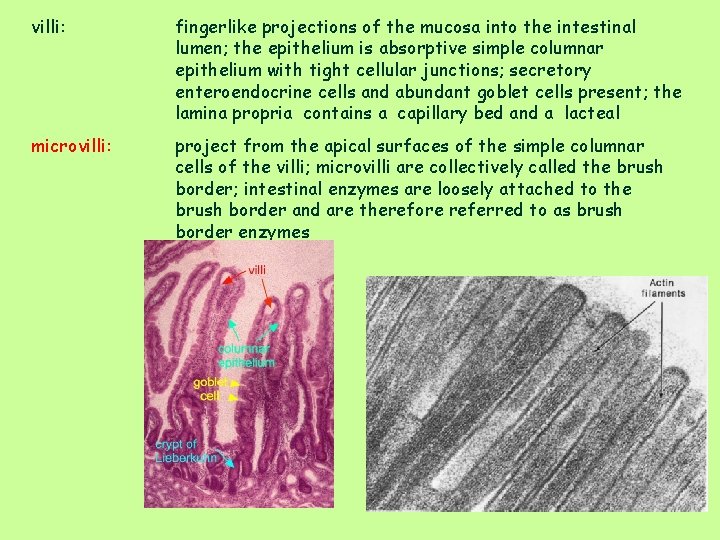
villi: fingerlike projections of the mucosa into the intestinal lumen; the epithelium is absorptive simple columnar epithelium with tight cellular junctions; secretory enteroendocrine cells and abundant goblet cells present; the lamina propria contains a capillary bed and a lacteal microvilli: project from the apical surfaces of the simple columnar cells of the villi; microvilli are collectively called the brush border; intestinal enzymes are loosely attached to the brush border and are therefore referred to as brush border enzymes

intestinal crypts: are depressions in the mucosa; cells secrete intestinal juice (enzymes, mucus) and paneth cells secrete lysozyme Goblet cells: secrete mucous Enteroendocrine cells: produce enterogastrones
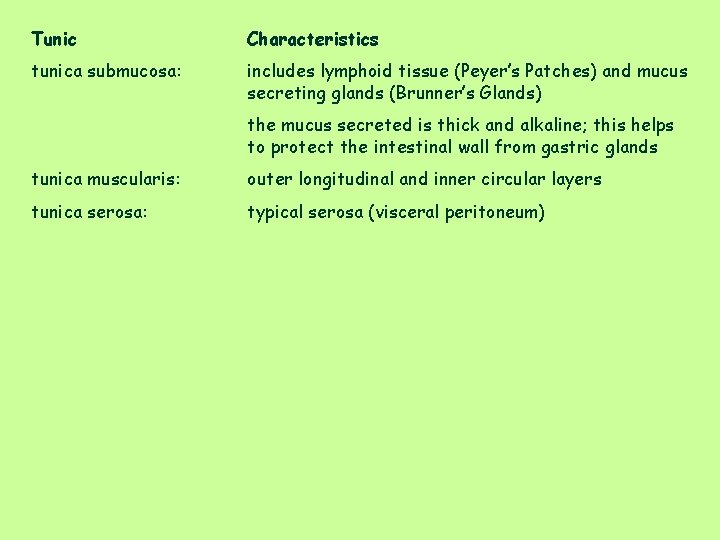
Tunic Characteristics tunica submucosa: includes lymphoid tissue (Peyer’s Patches) and mucus secreting glands (Brunner’s Glands) the mucus secreted is thick and alkaline; this helps to protect the intestinal wall from gastric glands tunica muscularis: outer longitudinal and inner circular layers tunica serosa: typical serosa (visceral peritoneum)
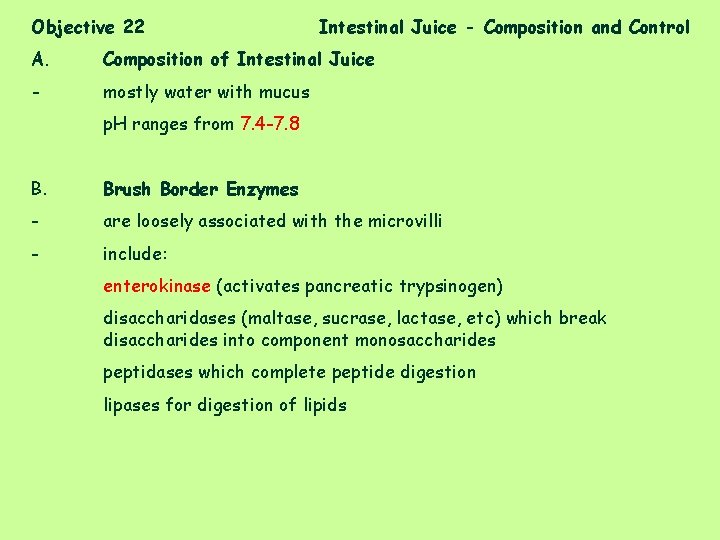
Objective 22 Intestinal Juice - Composition and Control A. Composition of Intestinal Juice - mostly water with mucus p. H ranges from 7. 4 -7. 8 B. Brush Border Enzymes - are loosely associated with the microvilli - include: enterokinase (activates pancreatic trypsinogen) disaccharidases (maltase, sucrase, lactase, etc) which break disaccharides into component monosaccharides peptidases which complete peptide digestion lipases for digestion of lipids
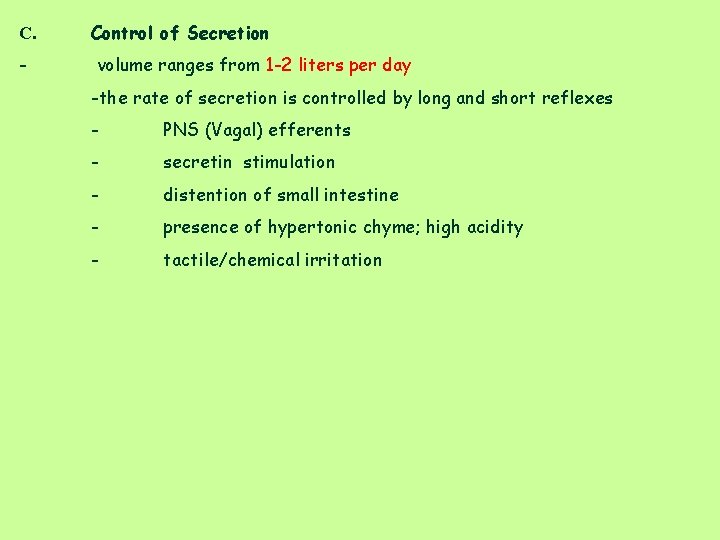
C. Control of Secretion - volume ranges from 1 -2 liters per day -the rate of secretion is controlled by long and short reflexes - PNS (Vagal) efferents - secretin stimulation - distention of small intestine - presence of hypertonic chyme; high acidity - tactile/chemical irritation
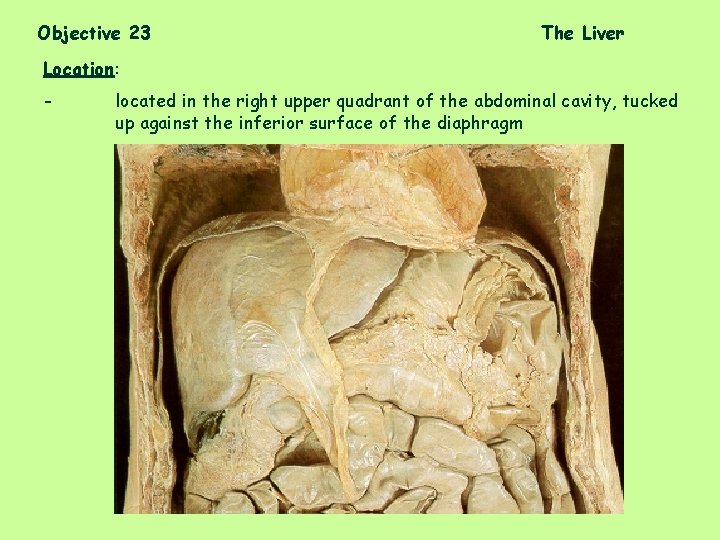
Objective 23 The Liver Location: - located in the right upper quadrant of the abdominal cavity, tucked up against the inferior surface of the diaphragm
-is the largest glandular organ, weighs about 1. 4 kg -there are four lobes: right lobe left lobe caudate lobe quadrate lobe -the falciform ligament separates the right lobe and the left lobe -blood is supplied by the hepatic artery and the portal vein; blood is removed by the right and left hepatic veins which join the inferior vena cava -the liver is intraperitoneal -bile carried by right and left hepatic duct, to common hepatic duct which joins the cystic duct to form the common bile duct
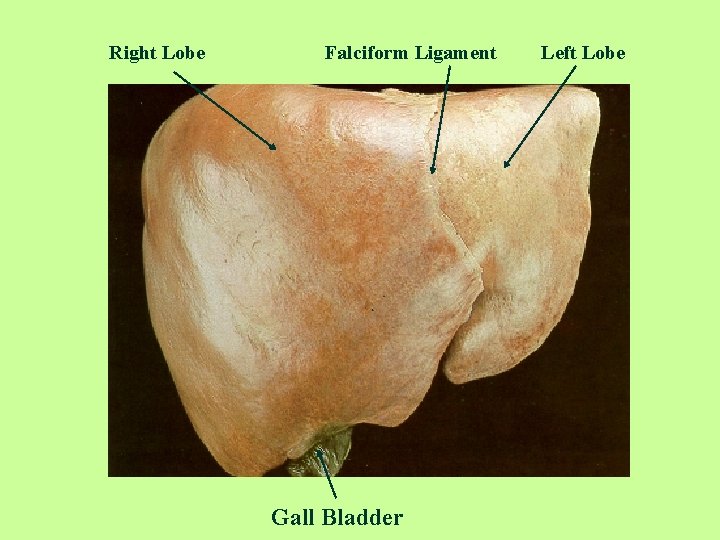
Right Lobe Falciform Ligament Gall Bladder Left Lobe
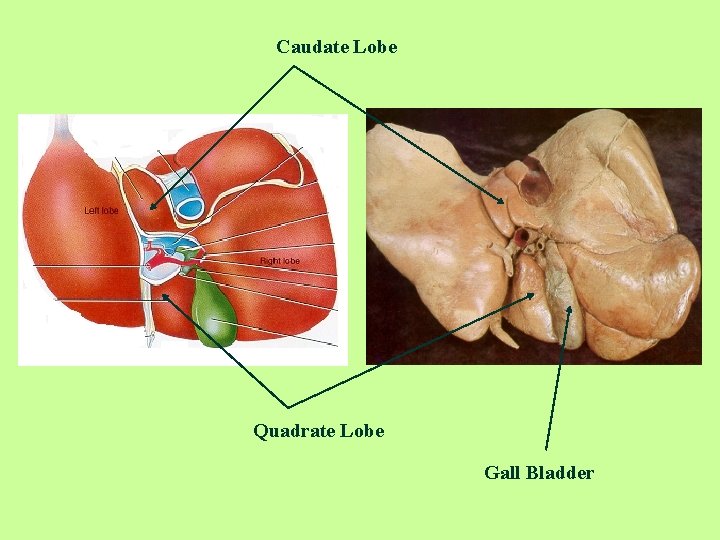
Caudate Lobe Quadrate Lobe Gall Bladder
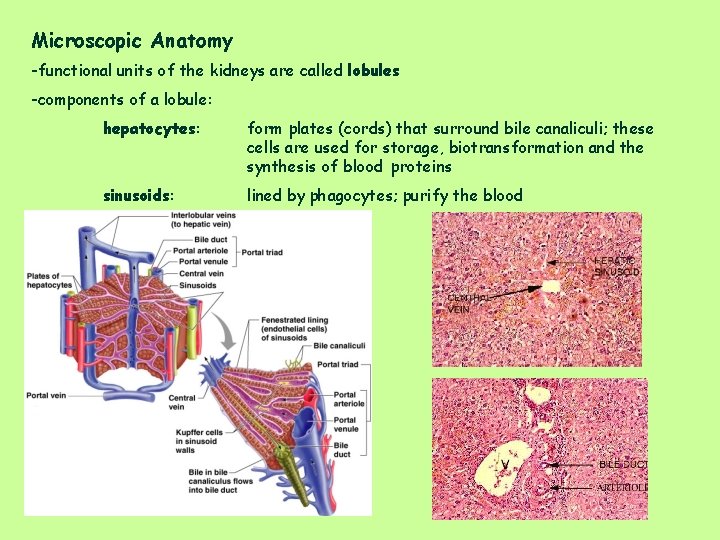
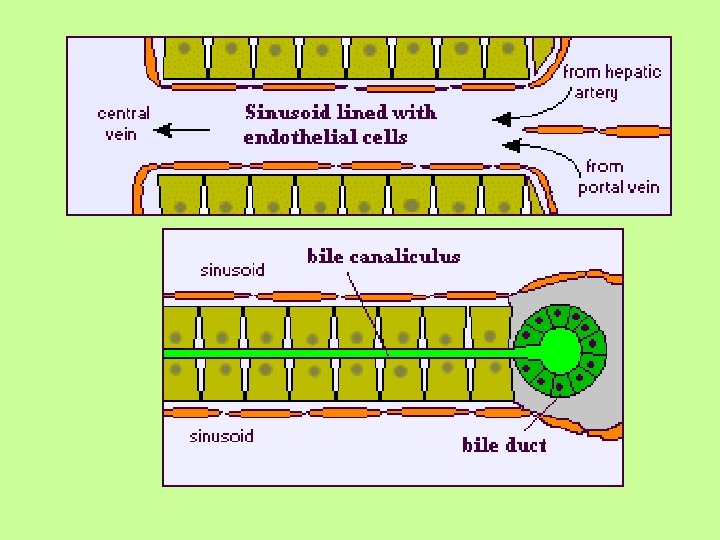
Microscopic Anatomy -functional units of the kidneys are called lobules -components of a lobule: hepatocytes: form plates (cords) that surround bile canaliculi; these cells are used for storage, biotransformation and the synthesis of blood proteins sinusoids: lined by phagocytes; purify the blood
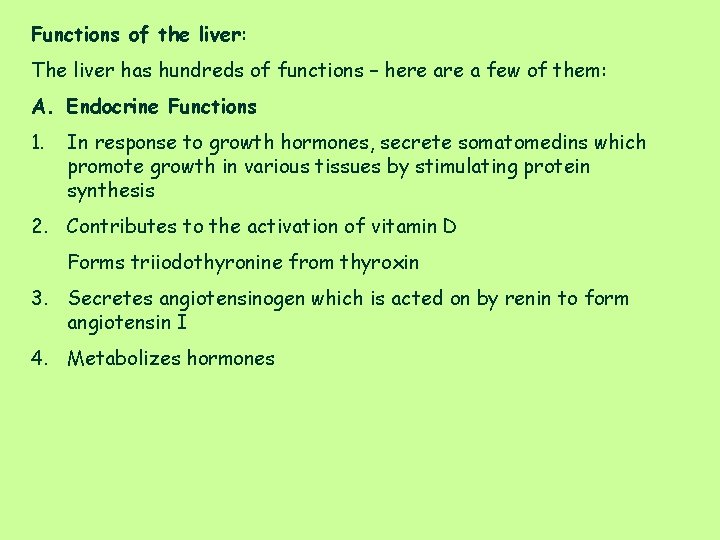
Functions of the liver: The liver has hundreds of functions – here a few of them: A. Endocrine Functions 1. In response to growth hormones, secrete somatomedins which promote growth in various tissues by stimulating protein synthesis 2. Contributes to the activation of vitamin D Forms triiodothyronine from thyroxin 3. Secretes angiotensinogen which is acted on by renin to form angiotensin I 4. Metabolizes hormones
B. Clotting Functions 1. Produces many of the plasma clotting factors, including prothrombin and fibrinogen 2. Produces bile salts which are needed for the absorption of vitamin K; vitamin K is needed for the synthesis of clotting factors C. Plasma Proteins 1. Synthesizes and secretes albumen, binding proteins for steroid hormones, trace elements and lipoproteins D. Digestive Functions 1. Synthesizes and secretes bile salts which are necessary for the digestion and absorption of fats
E. Organic Metabolism 1. Converts plasma glucose to glycogen and triacylglycerols 2. Converts plasma amino acids to fatty acids 3. Produces glucose from glycogen and other sources 4. Converts fatty acids to ketones during fasting 5. Produces urea, the major end product of amino acid catabolism and releases it into the blood F. Cholesterol Metabolism 1. Synthesizes cholesterol and releases it into the blood 2. Secretes plasma cholesterol into bile 3. Converts plasma cholesterol into amino acids
G. Excretory and Degradation Functions 1. Secretes bilirubin and many other bile pigments into the bile 2. Excretes via the bile, many endogenous and foreign organic molecules as well as trace elements 3. Transforms many endogenous and foreign molecules 4. Destroys aged, damaged, or defective erythrocytes
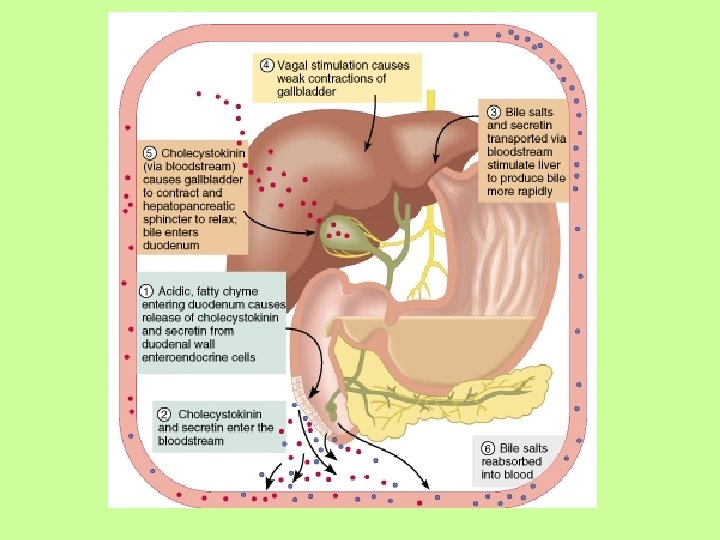
Objective 24 Bile – Composition and Control of Secretion A. Composition of Bile - alkaline solution containing water - other components include: bicarbonate bile salts (cholic acid, chenodeoxycholic acid) bile pigments (mostly bilirubin) cholesterol neutral fats phospholipids electrolytes lecithin B. Function: - the digestive function of bile salts is to emulsify fats C. Control of Secretion - 500 to 100 ml average daily volume - production is constant throughout the day, but will be increased if fatty chyme is present in the duodenum (secretin) and if there are bile salts ion the plasma
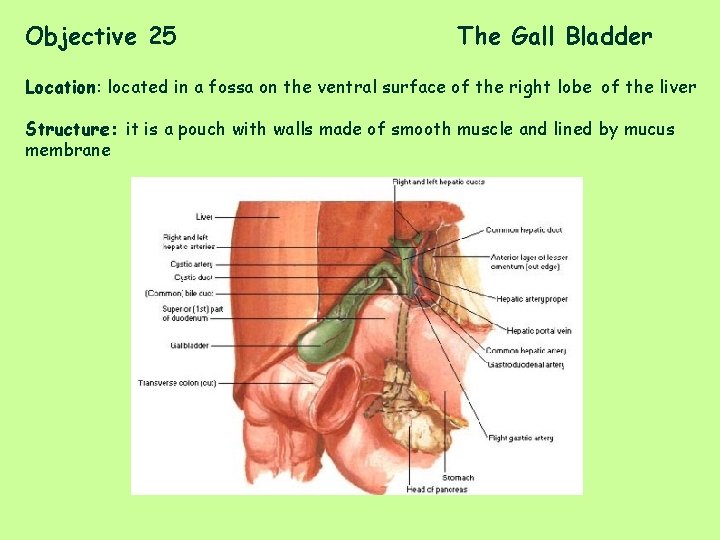
Objective 25 The Gall Bladder Location: located in a fossa on the ventral surface of the right lobe of the liver Structure: it is a pouch with walls made of smooth muscle and lined by mucus membrane
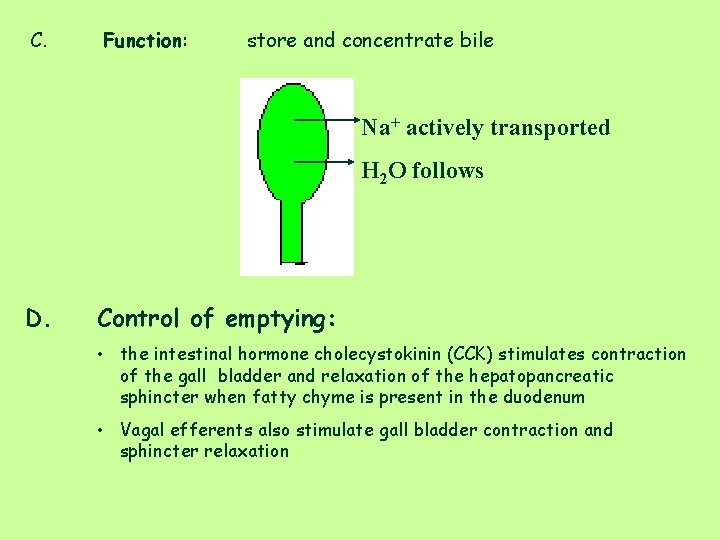
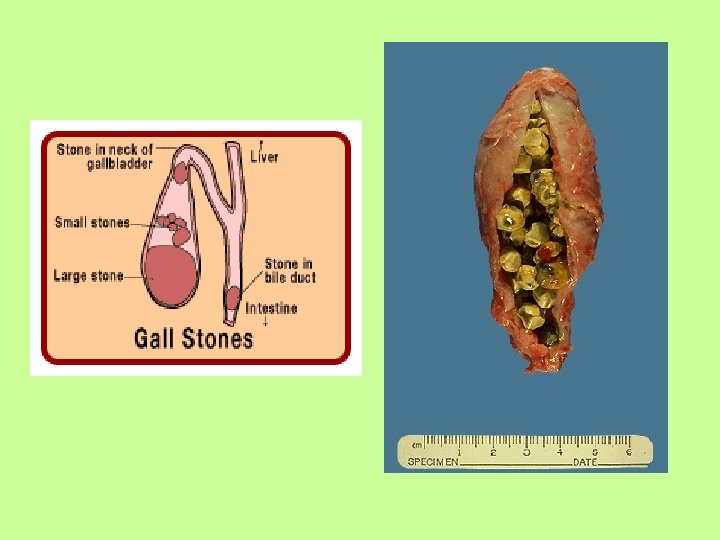
C. Function: store and concentrate bile Na+ actively transported H 2 O follows D. Control of emptying: • the intestinal hormone cholecystokinin (CCK) stimulates contraction of the gall bladder and relaxation of the hepatopancreatic sphincter when fatty chyme is present in the duodenum • Vagal efferents also stimulate gall bladder contraction and sphincter relaxation
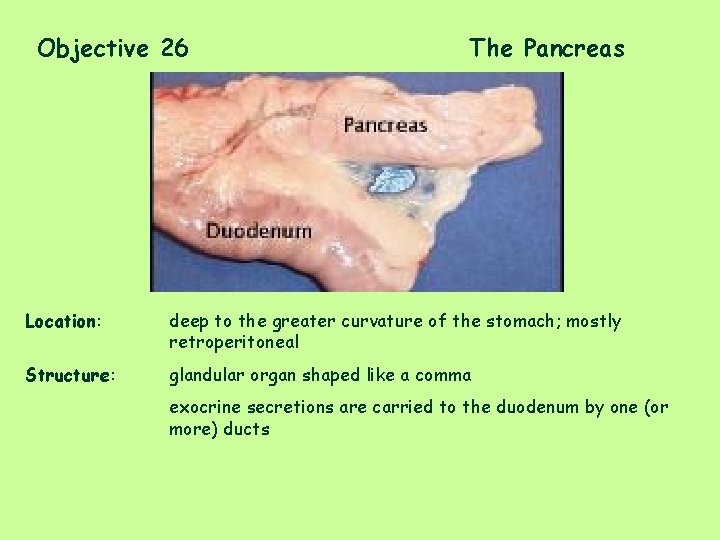
Objective 26 The Pancreas Location: deep to the greater curvature of the stomach; mostly retroperitoneal Structure: glandular organ shaped like a comma exocrine secretions are carried to the duodenum by one (or more) ducts
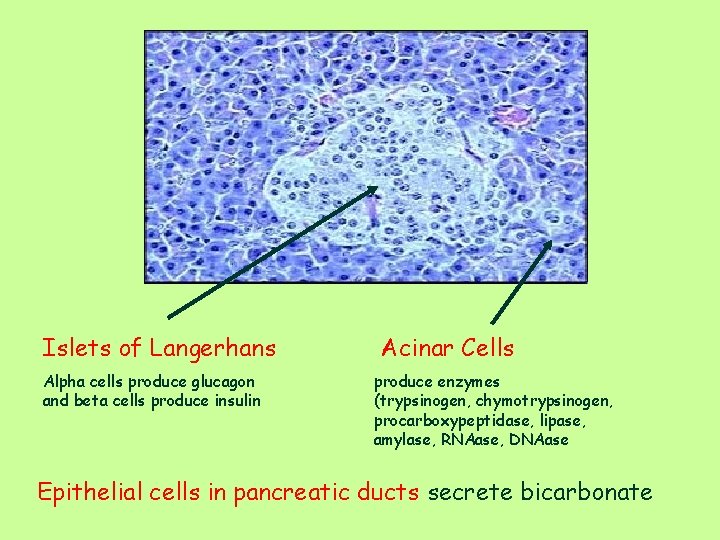
Islets of Langerhans Alpha cells produce glucagon and beta cells produce insulin Acinar Cells produce enzymes (trypsinogen, chymotrypsinogen, procarboxypeptidase, lipase, amylase, RNAase, DNAase Epithelial cells in pancreatic ducts secrete bicarbonate
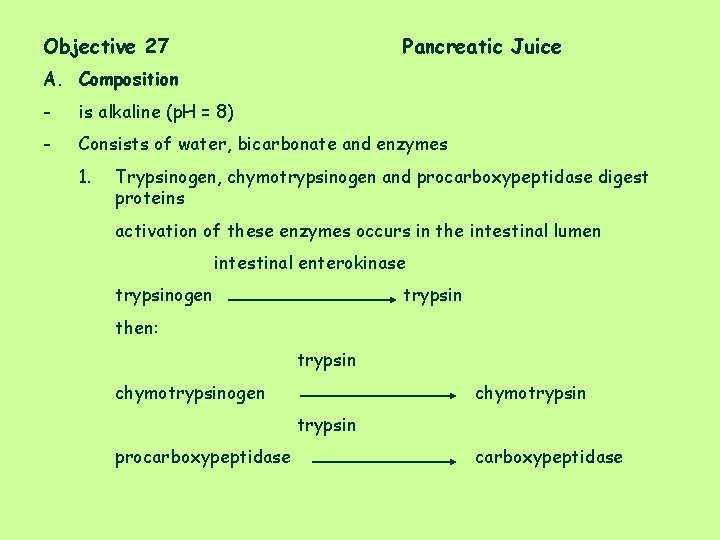
Objective 27 Pancreatic Juice A. Composition - is alkaline (p. H = 8) - Consists of water, bicarbonate and enzymes 1. Trypsinogen, chymotrypsinogen and procarboxypeptidase digest proteins activation of these enzymes occurs in the intestinal lumen intestinal enterokinase trypsinogen trypsin then: trypsin chymotrypsinogen chymotrypsin procarboxypeptidase
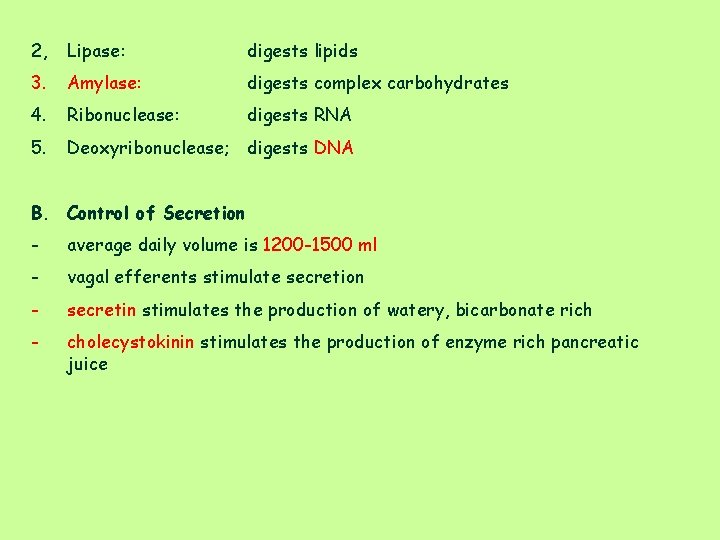
2, Lipase: digests lipids 3. Amylase: digests complex carbohydrates 4. Ribonuclease: digests RNA 5. Deoxyribonuclease; digests DNA B. Control of Secretion - average daily volume is 1200 -1500 ml - vagal efferents stimulate secretion - secretin stimulates the production of watery, bicarbonate rich - cholecystokinin stimulates the production of enzyme rich pancreatic juice
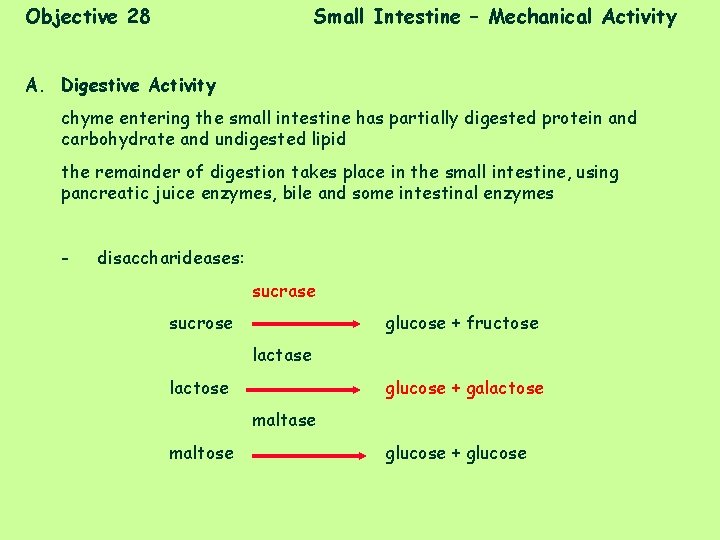
Objective 28 Small Intestine – Mechanical Activity A. Digestive Activity chyme entering the small intestine has partially digested protein and carbohydrate and undigested lipid the remainder of digestion takes place in the small intestine, using pancreatic juice enzymes, bile and some intestinal enzymes - disaccharideases: sucrase sucrose glucose + fructose lactase lactose glucose + galactose maltase maltose glucose + glucose
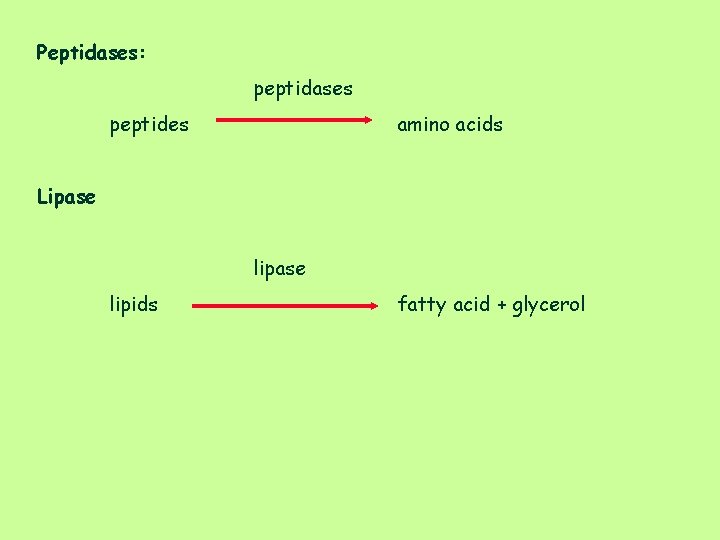
Peptidases: peptidases peptides amino acids Lipase lipids fatty acid + glycerol
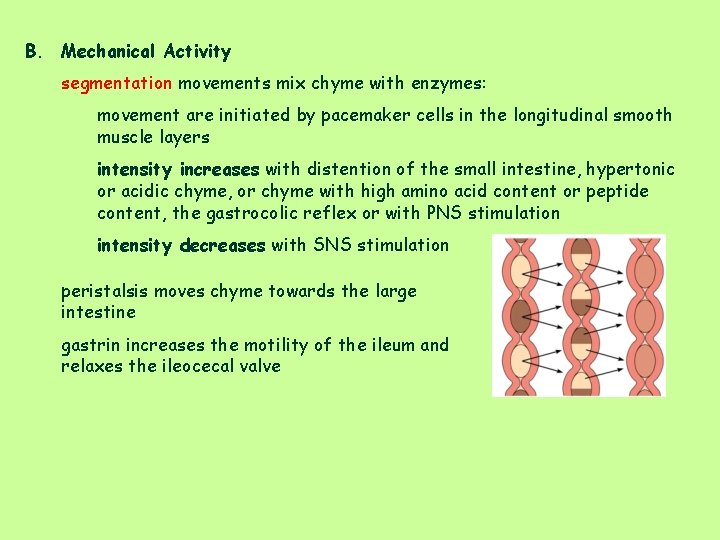
B. Mechanical Activity segmentation movements mix chyme with enzymes: movement are initiated by pacemaker cells in the longitudinal smooth muscle layers intensity increases with distention of the small intestine, hypertonic or acidic chyme, or chyme with high amino acid content or peptide content, the gastrocolic reflex or with PNS stimulation intensity decreases with SNS stimulation peristalsis moves chyme towards the large intestine gastrin increases the motility of the ileum and relaxes the ileocecal valve
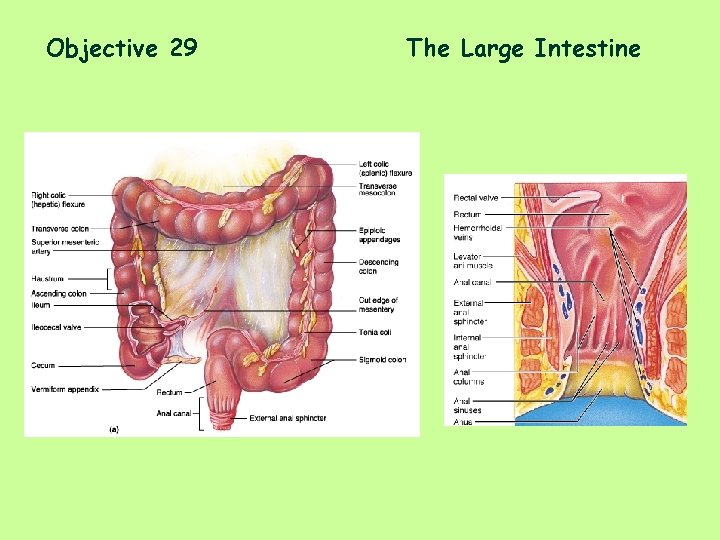
Objective 29 The Large Intestine
C. Functions of the Large Intestine - temporarily stores unabsorbed material - Bacterial actions - produce vitamins (B complex and K) - ferment carbohydrates and produce gas and acid - convert amino acids to indolel, skatole, mercaptens - convert bile pigments to urobilogen - reabsorb water from chyme - Absorb Na+ and Cl- into the blood - Secrete bicarbonate, K+ - feces formation - Defecation
D. Movements Haustral contractions: - haustra are created by slow segmentations which help to mix the contents of the large intestine and aid in water reabsorption - are somewhat propulsive Mass Movements - long, slow powerful contractions that occur 3 -4 times/day - move feces towards the rectum - occurs as part of the gastrocolic reflex
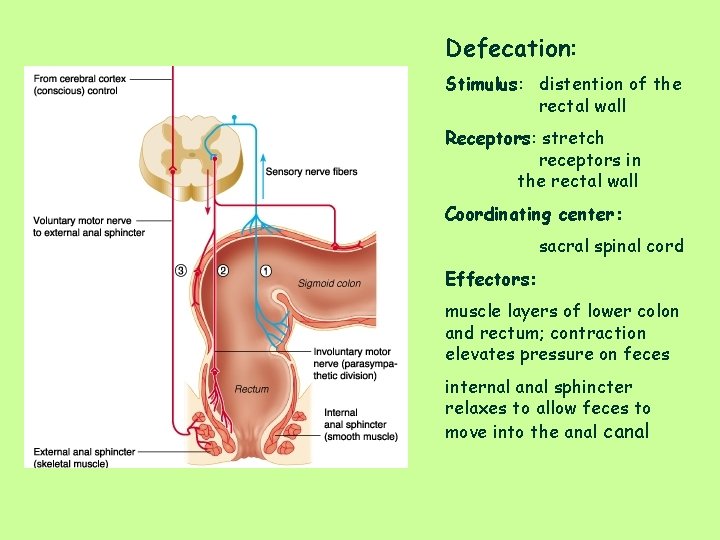
Defecation: Stimulus: distention of the rectal wall Receptors: stretch receptors in the rectal wall Coordinating center: sacral spinal cord Effectors: muscle layers of lower colon and rectum; contraction elevates pressure on feces internal anal sphincter relaxes to allow feces to move into the anal canal
- Slides: 36