Obesity and Life expectancy January 2003 Life Table
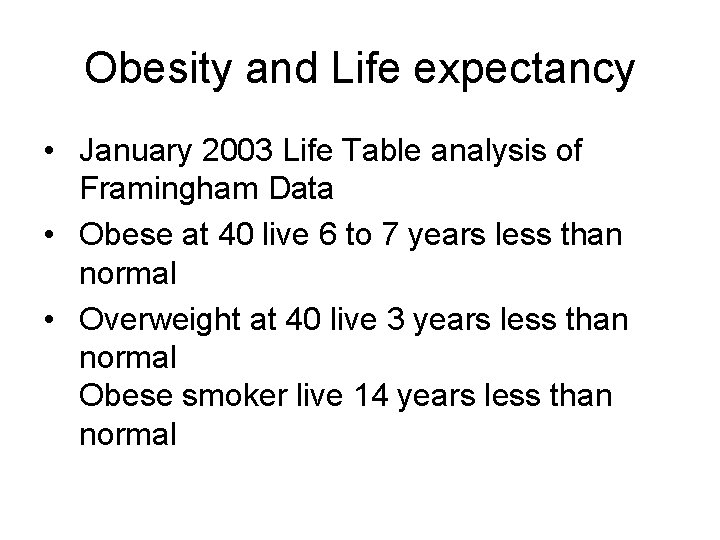
Obesity and Life expectancy • January 2003 Life Table analysis of Framingham Data • Obese at 40 live 6 to 7 years less than normal • Overweight at 40 live 3 years less than normal Obese smoker live 14 years less than normal
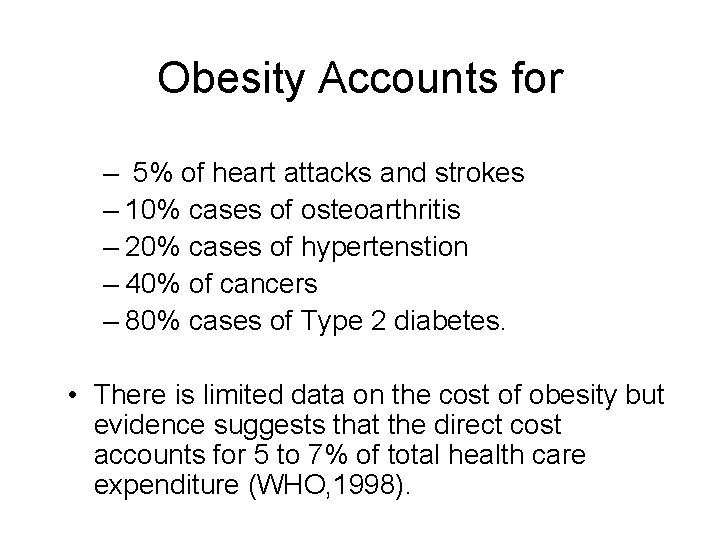
Obesity Accounts for – 5% of heart attacks and strokes – 10% cases of osteoarthritis – 20% cases of hypertenstion – 40% of cancers – 80% cases of Type 2 diabetes. • There is limited data on the cost of obesity but evidence suggests that the direct cost accounts for 5 to 7% of total health care expenditure (WHO, 1998).
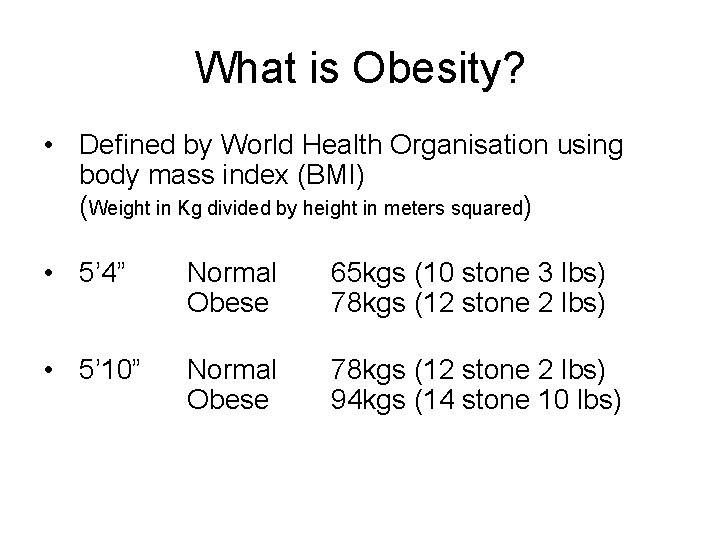
What is Obesity? • Defined by World Health Organisation using body mass index (BMI) (Weight in Kg divided by height in meters squared) • 5’ 4” Normal Obese 65 kgs (10 stone 3 lbs) 78 kgs (12 stone 2 lbs) • 5’ 10” Normal Obese 78 kgs (12 stone 2 lbs) 94 kgs (14 stone 10 lbs)
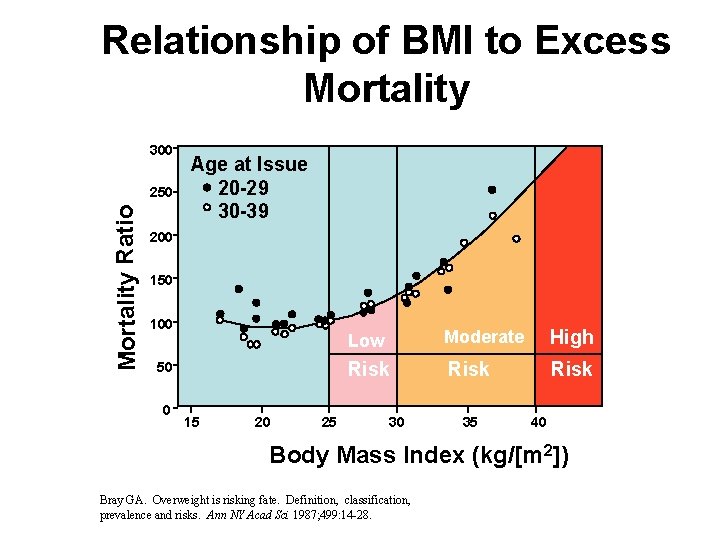
Relationship of BMI to Excess Mortality 300 Mortality Ratio 250 Age at Issue 20 -29 30 -39 200 150 100 50 0 15 20 25 Low Moderate High Risk 30 35 40 Body Mass Index (kg/[m 2]) Bray GA. Overweight is risking fate. Definition, classification, prevalence and risks. Ann NY Acad Sci 1987; 499: 14 -28.
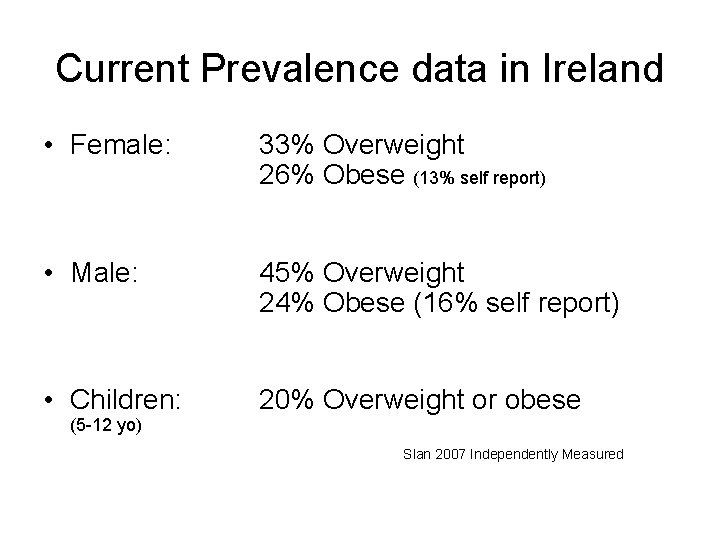
Current Prevalence data in Ireland • Female: 33% Overweight 26% Obese (13% self report) • Male: 45% Overweight 24% Obese (16% self report) • Children: 20% Overweight or obese (5 -12 yo) Slan 2007 Independently Measured
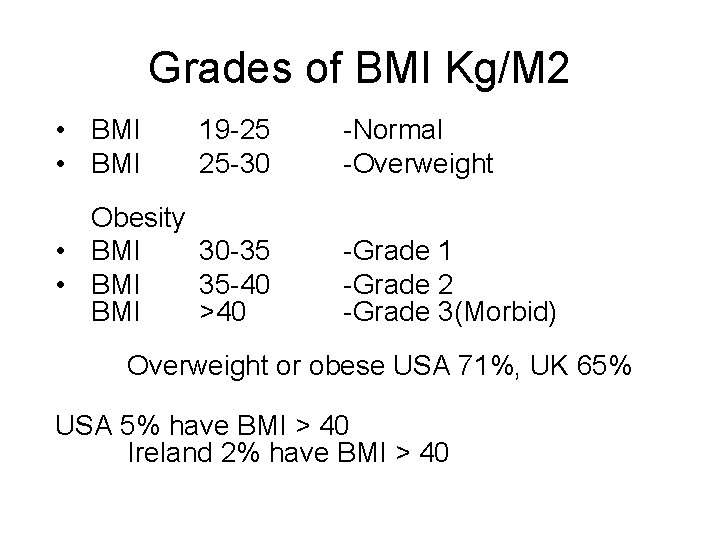
Grades of BMI Kg/M 2 • BMI 19 -25 25 -30 Obesity • BMI 30 -35 • BMI 35 -40 BMI >40 -Normal -Overweight -Grade 1 -Grade 2 -Grade 3(Morbid) Overweight or obese USA 71%, UK 65% USA 5% have BMI > 40 Ireland 2% have BMI > 40
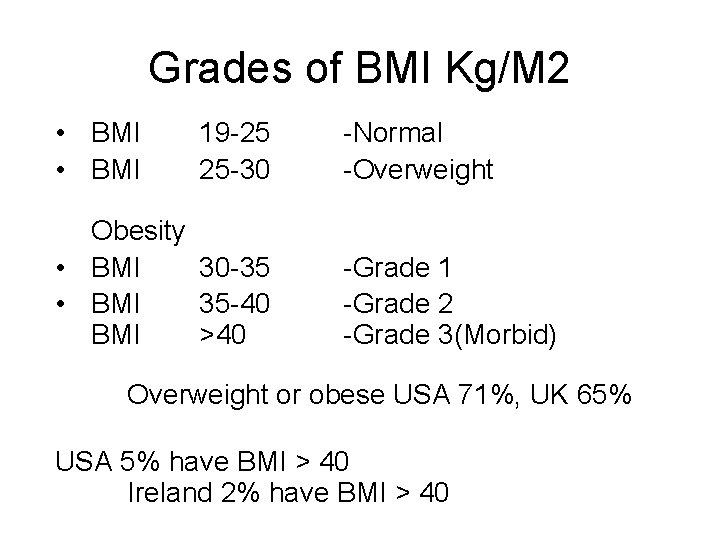
Grades of BMI Kg/M 2 • BMI 19 -25 25 -30 Obesity • BMI 30 -35 • BMI 35 -40 BMI >40 -Normal -Overweight -Grade 1 -Grade 2 -Grade 3(Morbid) Overweight or obese USA 71%, UK 65% USA 5% have BMI > 40 Ireland 2% have BMI > 40
BMI and weight
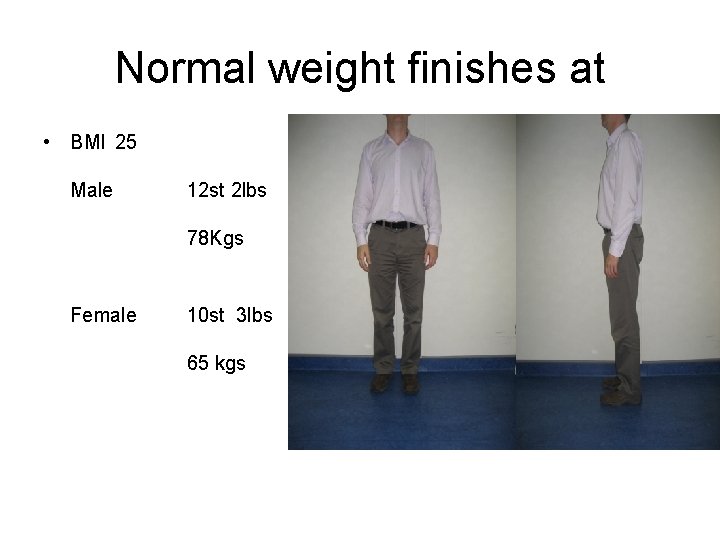
Normal weight finishes at • BMI 25 Male 12 st 2 lbs 78 Kgs Female 10 st 3 lbs 65 kgs
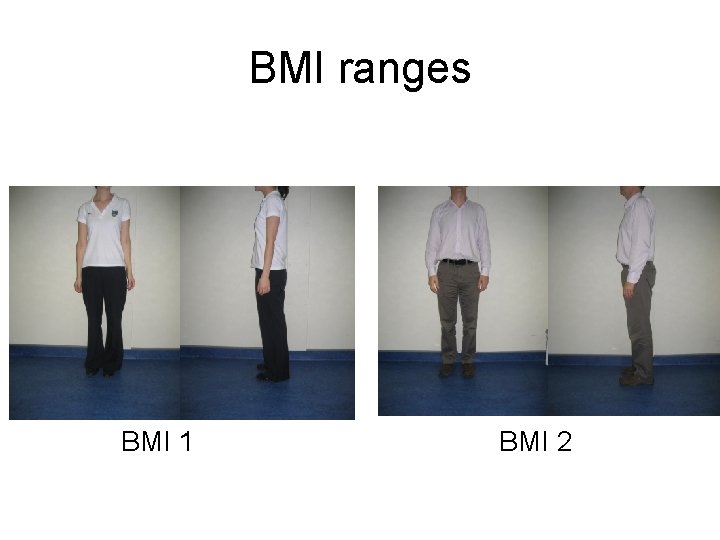
BMI ranges BMI 1 BMI 2
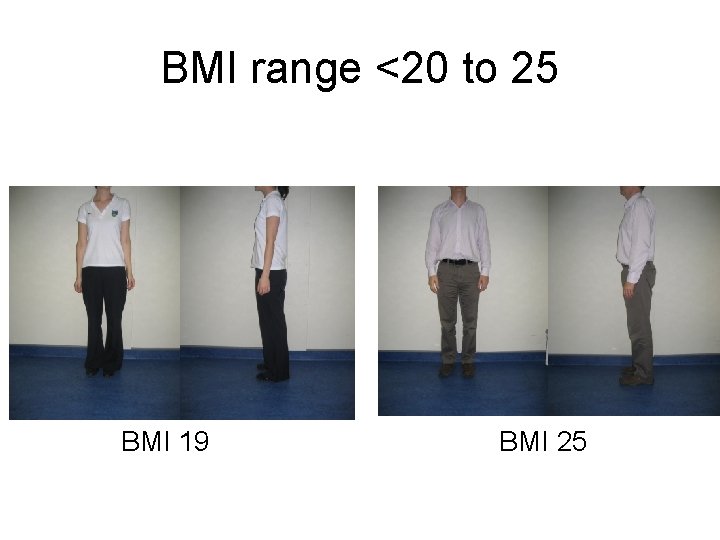
BMI range <20 to 25 BMI 19 BMI 25
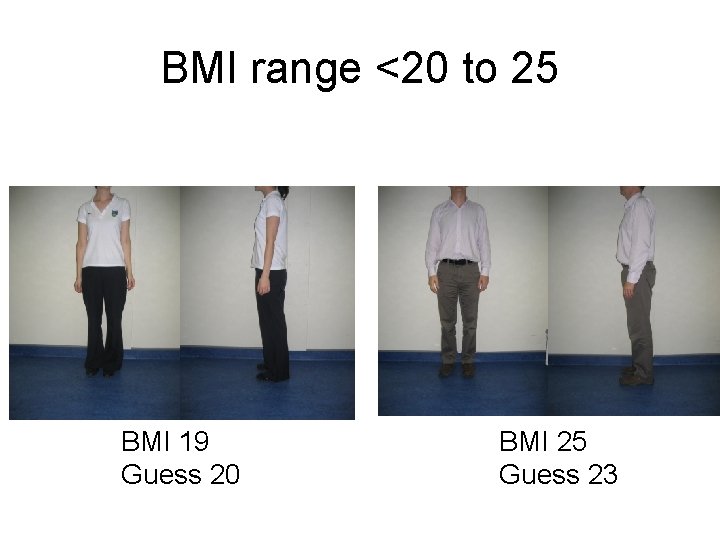
BMI range <20 to 25 BMI 19 Guess 20 BMI 25 Guess 23
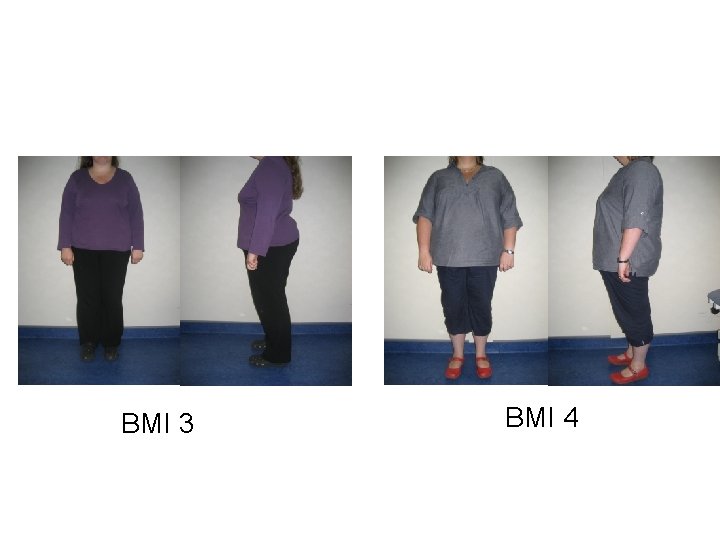
BMI 3 BMI 4
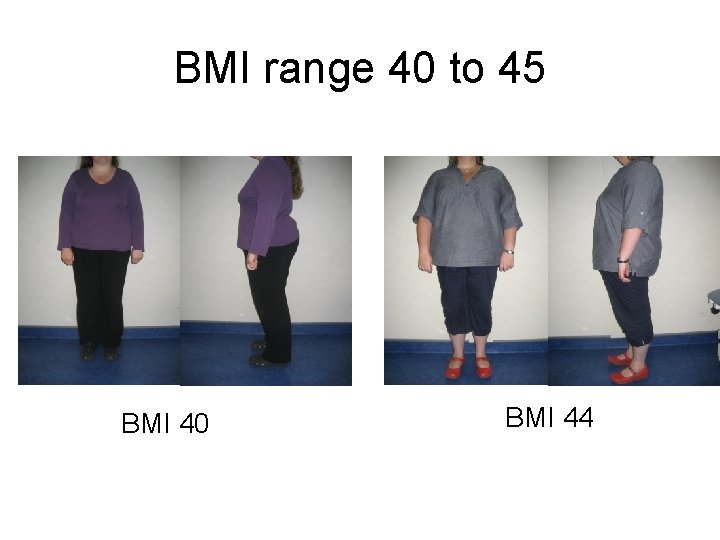
BMI range 40 to 45 BMI 40 BMI 44
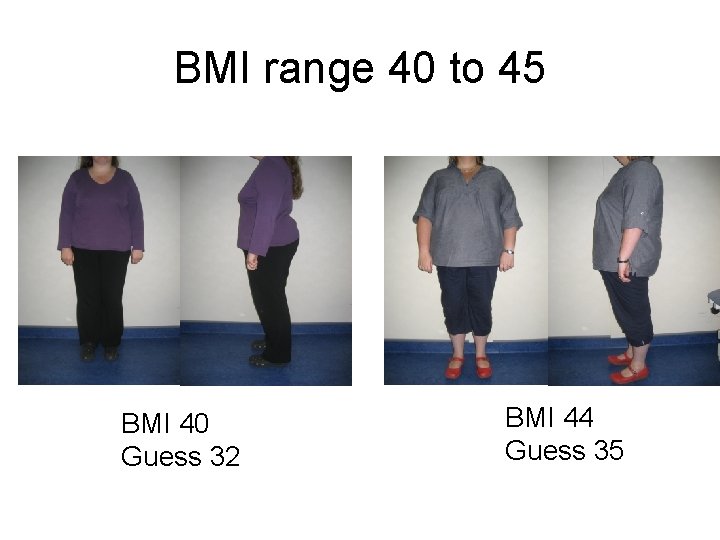
BMI range 40 to 45 BMI 40 Guess 32 BMI 44 Guess 35
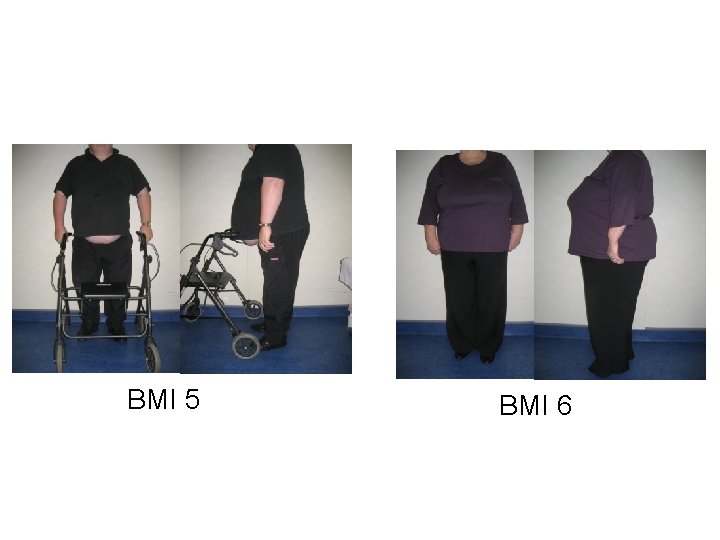
BMI 5 BMI 6

BMI range 50 to 55 BMI 51 BMI 52

BMI range 50 to 55 BMI 51 Guess 43 BMI 52 Guess 42
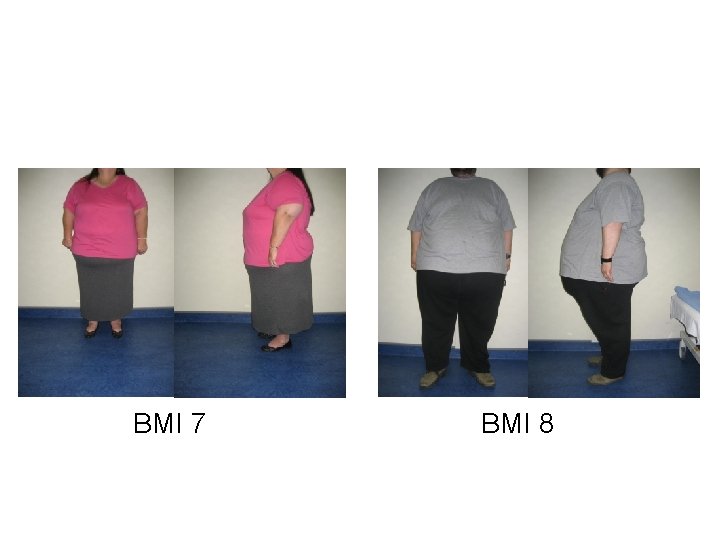
BMI 7 BMI 8
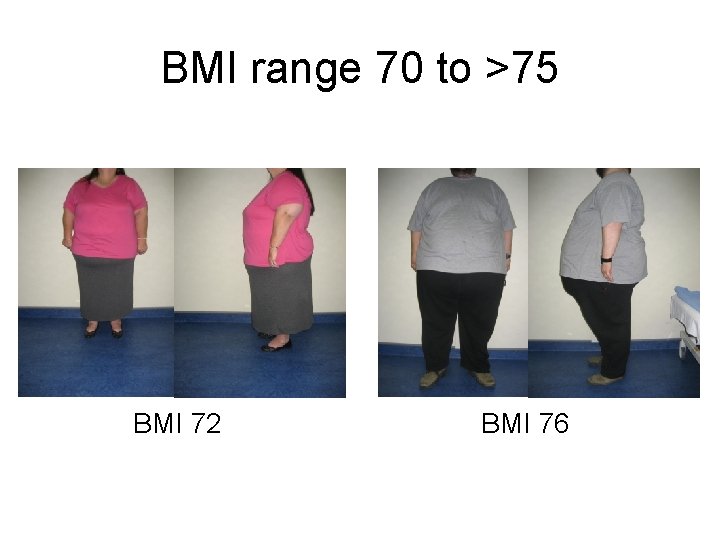
BMI range 70 to >75 BMI 72 BMI 76
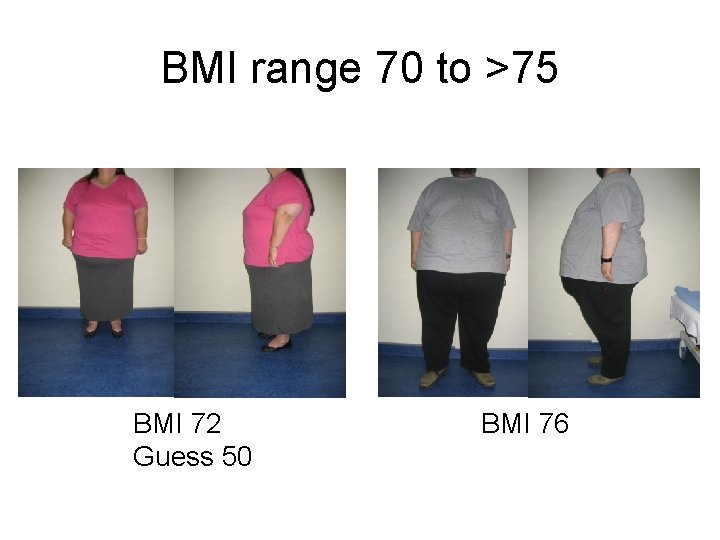
BMI range 70 to >75 BMI 72 Guess 50 BMI 76
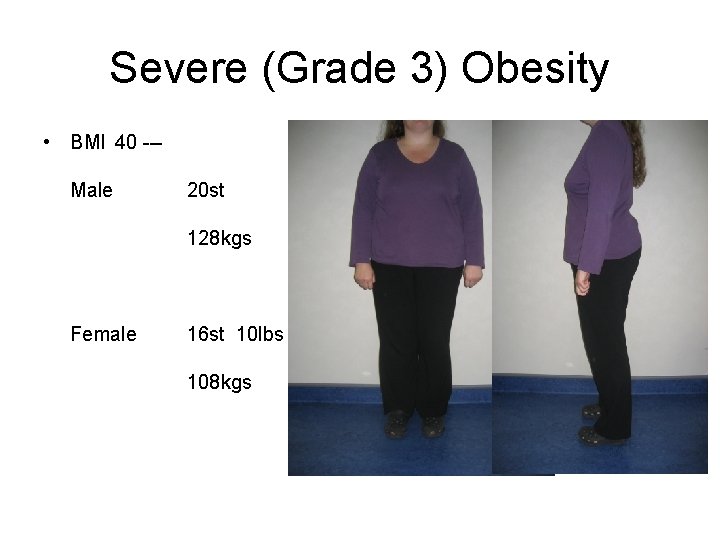
Severe (Grade 3) Obesity • BMI 40 --Male 20 st 128 kgs Female 16 st 10 lbs 108 kgs
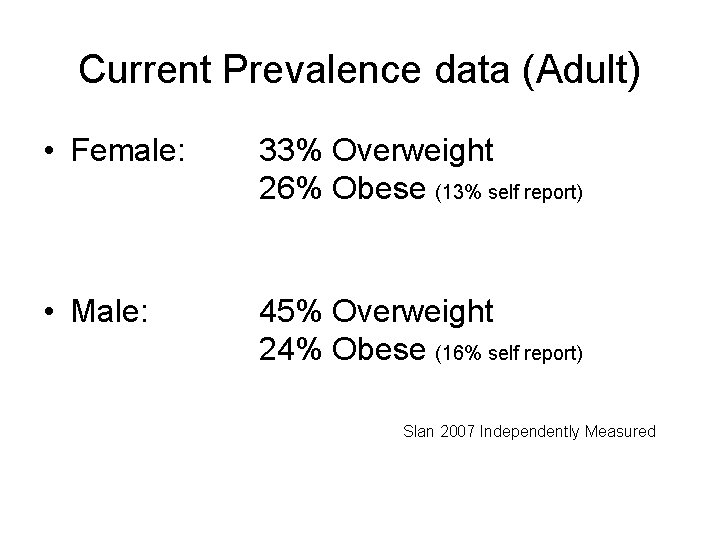
Current Prevalence data (Adult) • Female: 33% Overweight 26% Obese (13% self report) • Male: 45% Overweight 24% Obese (16% self report) Slan 2007 Independently Measured
Obesity is associated with • • • Diabetes Cancer Sleep Apnoea Osteoarthritis Fatty liver disease Psoriasis Dementia Cardiovascular Disease Death from H 1 N 1 (Swine Flu)
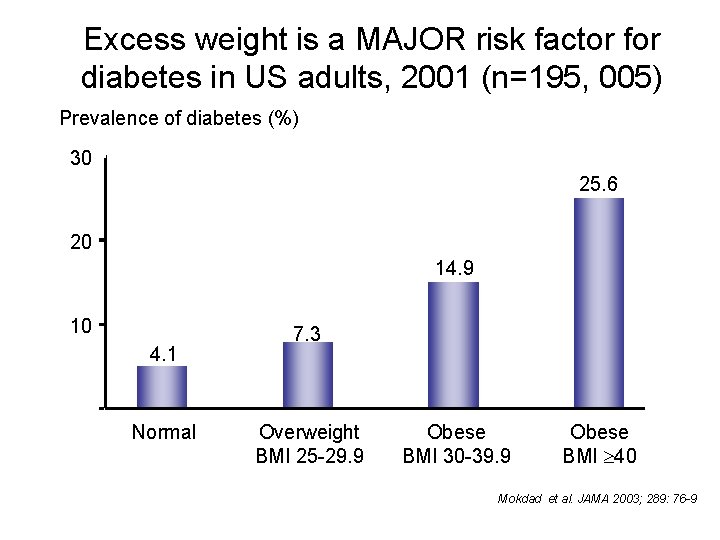
Excess weight is a MAJOR risk factor for diabetes in US adults, 2001 (n=195, 005) Prevalence of diabetes (%) 30 25. 6 20 14. 9 10 4. 1 0 Normal 7. 3 Overweight BMI 25 -29. 9 Obese BMI 30 -39. 9 Obese BMI 40 Mokdad et al. JAMA 2003; 289: 76 -9
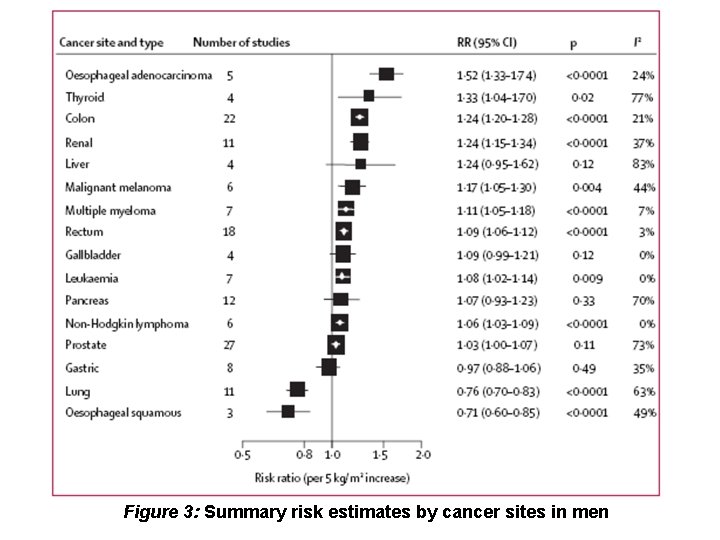
Figure 3: Summary risk estimates by cancer sites in men
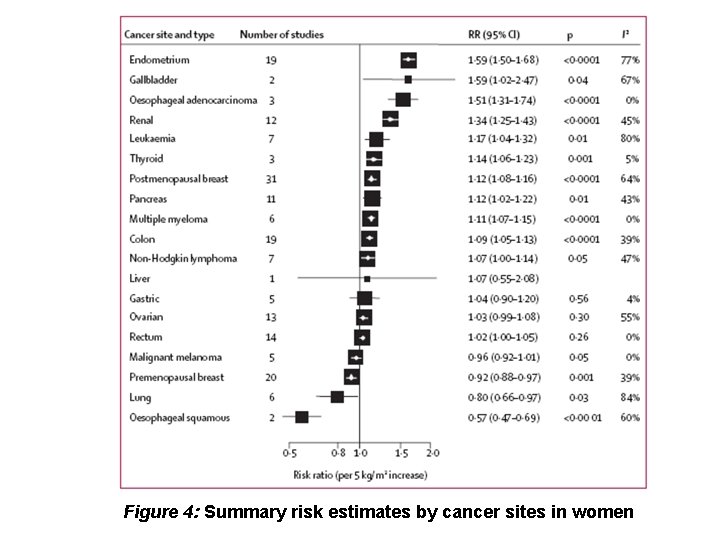
Figure 4: Summary risk estimates by cancer sites in women
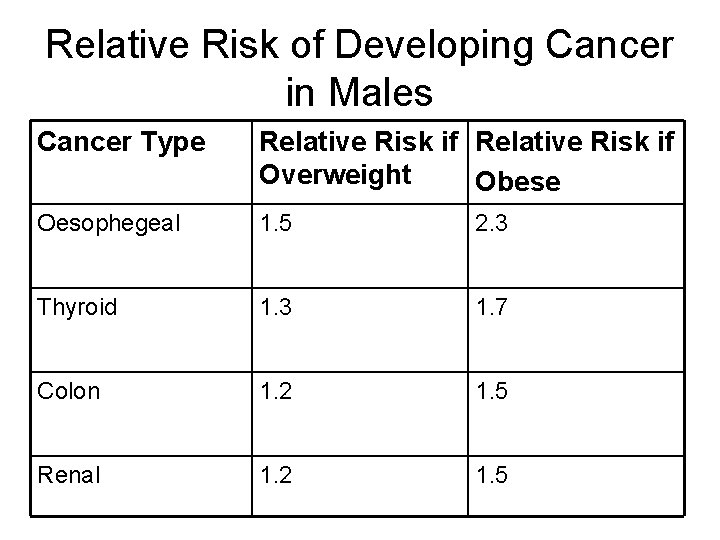
Relative Risk of Developing Cancer in Males Cancer Type Relative Risk if Overweight Obese Oesophegeal 1. 5 2. 3 Thyroid 1. 3 1. 7 Colon 1. 2 1. 5 Renal 1. 2 1. 5
Obesity also reduces survival in certain cancers • • • Colon Breast Endometrium Prostate Ovary
Increased risk of dementia • BMI and increased risk of dementia – analysis of prospective cohort study (Whitmer et al. 2005) – Increased risk of dimentia in later years for those overweight / obese in mid-life – Increased risk for • Males • Females
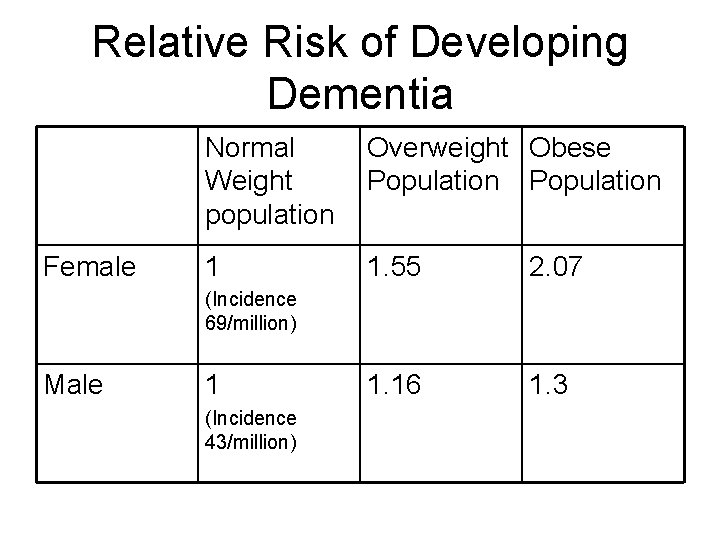
Relative Risk of Developing Dementia Female Normal Weight population Overweight Obese Population 1 1. 55 2. 07 1. 16 1. 3 (Incidence 69/million) Male 1 (Incidence 43/million)
Obese patient with Acute abdomen • 30% chance of atelecasis/pneumonia • 2. 8 times more likely than non obese
Overweight and obesity following Road Accidents • Study of 1, 615 Crashes Crash factor adjusted odds for dying 2. 08 for overweight 3. 17 for obese Injury severity adjusted odds for dying 1. 87 for overweight 3. 89 for obese Ryb J. Trauma 2008(64)406 -411 CIREN study
Role of weight and seatbelts • Seatbelts decrease risk of death and intraabdominal injury in obese and non obese Lack of seatbelt increases risk of death 9. 7 fold in obese 5. 2 fold in non obese Zarzaur & Marshall J Trauma 2008(64)412 -417
Crash Dummy Research

Equipment Needs
A lot of equipment • Has upper weight limit of ~ 150 kgs Trolleys Beds Theatre Tables Radiology – equipment and quality
Radiology Equipment in Ireland • Audit of 40 hospitals • CT, MRI, Fluoroscopy • Weight Limit • Aperture Diameter

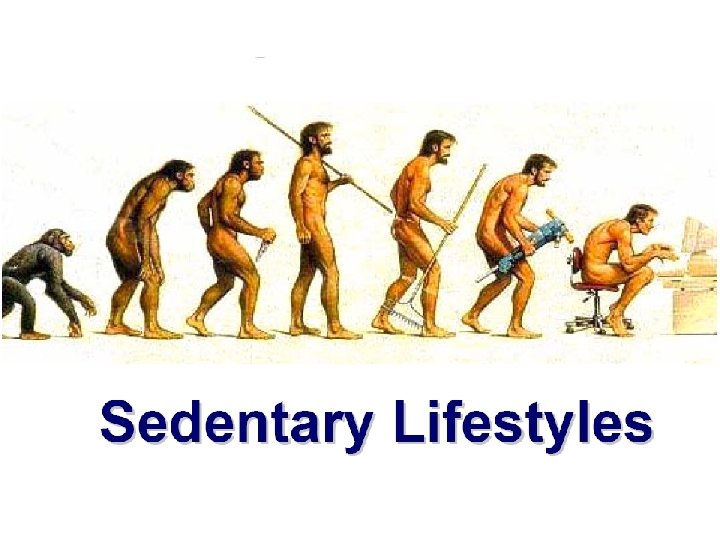
Toxic environment we live in…
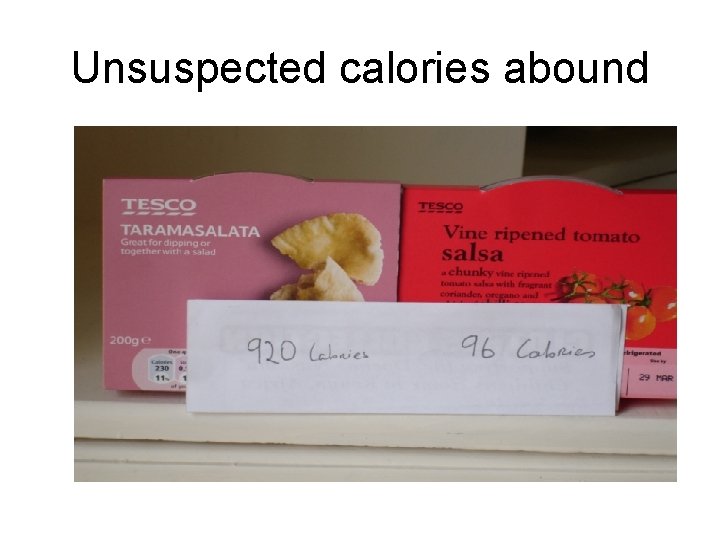
Unsuspected calories abound
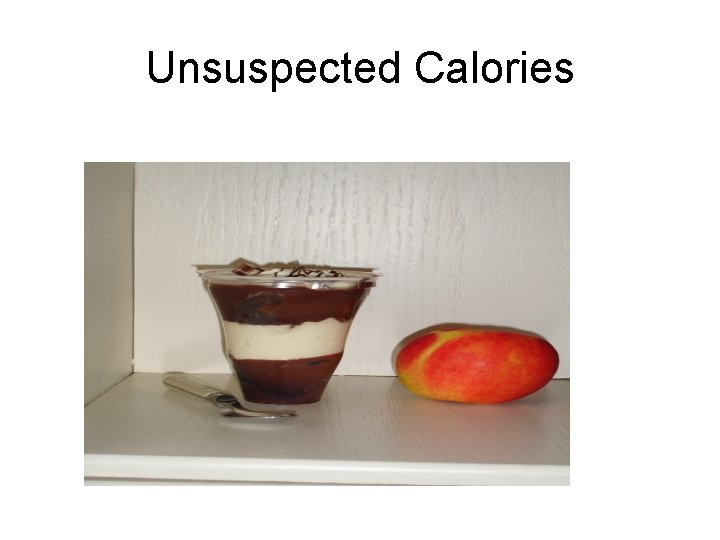
Unsuspected Calories
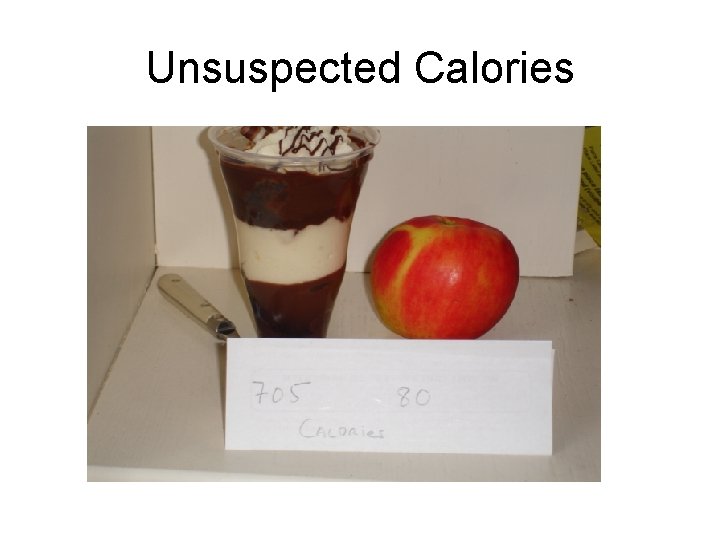
Unsuspected Calories
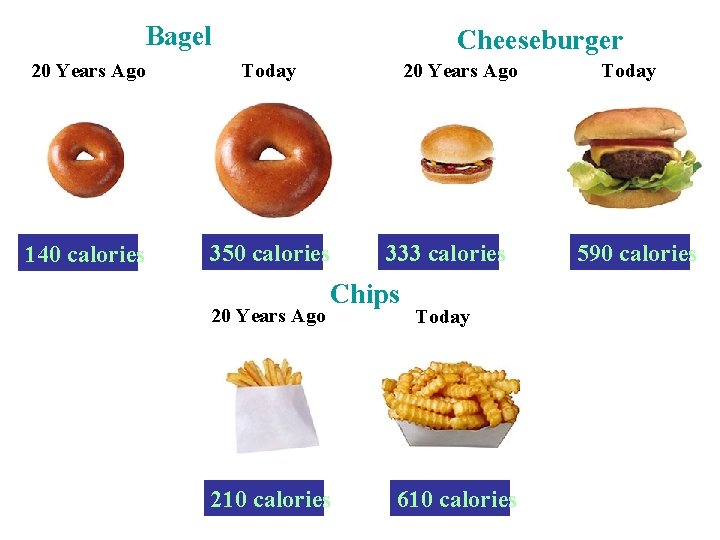
Bagel Cheeseburger 20 Years Ago Today 140 calories 350 calories 20 Years Ago 333 calories Chips 210 calories Today 610 calories Today 590 calories
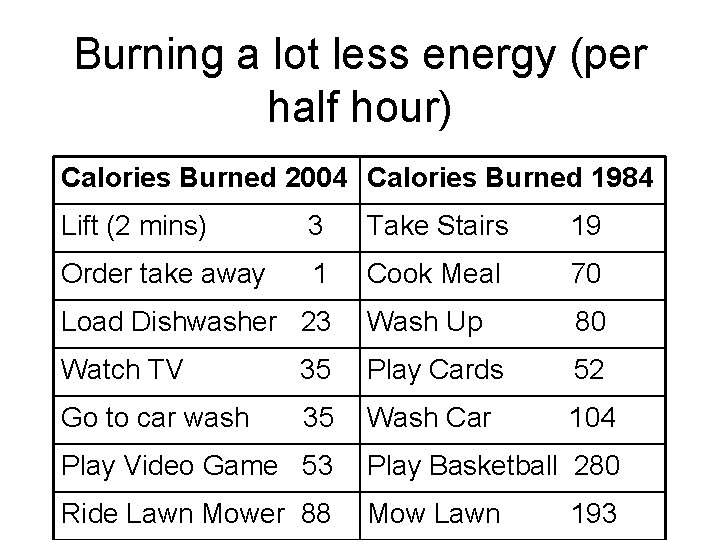
Burning a lot less energy (per half hour) Calories Burned 2004 Calories Burned 1984 Lift (2 mins) 3 Take Stairs 19 Order take away 1 Cook Meal 70 Load Dishwasher 23 Wash Up 80 Watch TV 35 Play Cards 52 Go to car wash 35 Wash Car 104 Play Video Game 53 Play Basketball 280 Ride Lawn Mower 88 Mow Lawn 193

What about children?
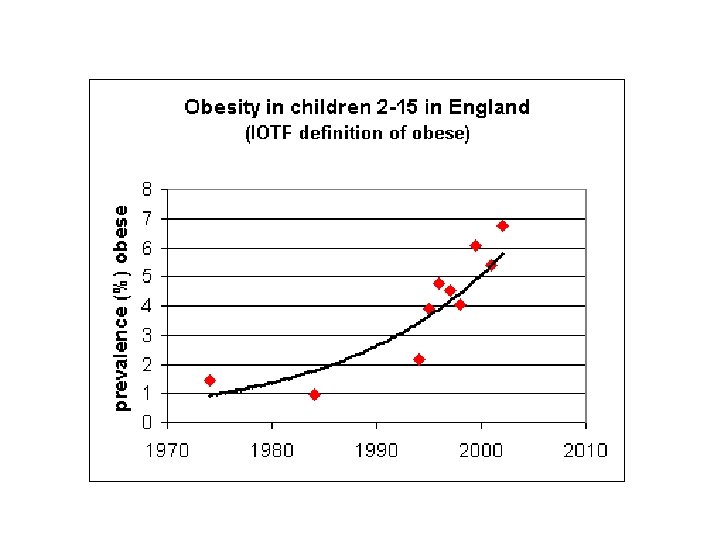
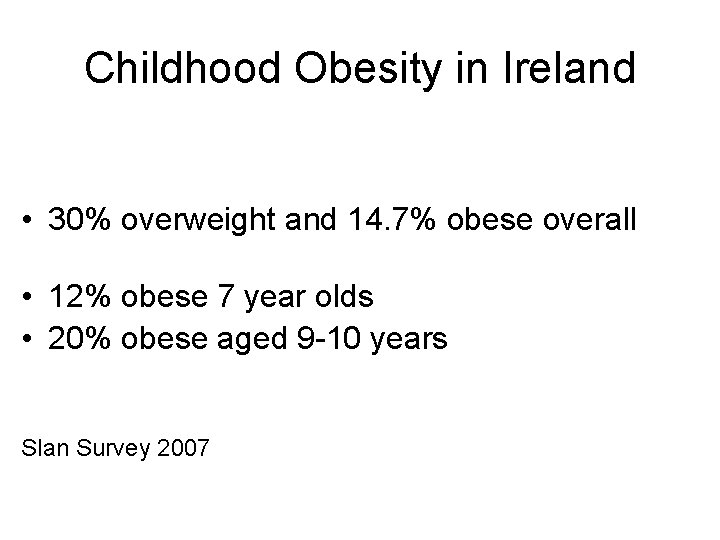
Childhood Obesity in Ireland • 30% overweight and 14. 7% obese overall • 12% obese 7 year olds • 20% obese aged 9 -10 years Slan Survey 2007
Do obese children become obese adults? • 30% of adult obesity begins in childhood so many adults were not obese children and not all obese children will stay obese • 1/3 obese preschoolers = obese adults (26 -41%) • All ages risk twice as high for obese as non-obese (range 26. 5 fold risk) Serdula, Preventative Medicine 1993: 22; 167 -177 • Parental obesity > doubles the risk of adult obesity in both obese and non-obese children < 10 years Whittaker NEJM 1997; 337(13): 869 -73
Just say no…… •
Treatment Options for Obesity • Diet & Lifestyle changes • Pharmacotherapy • Surgery
Nothing works without diet/lifestyle change • Diet – 500 kcalorie deficit/day healthy eating priciples • Activity - No consensus 1 hour daily every day • No treatment works without this
Who would you rather be? • Man on Left = Driver • Man on Right = Conductor
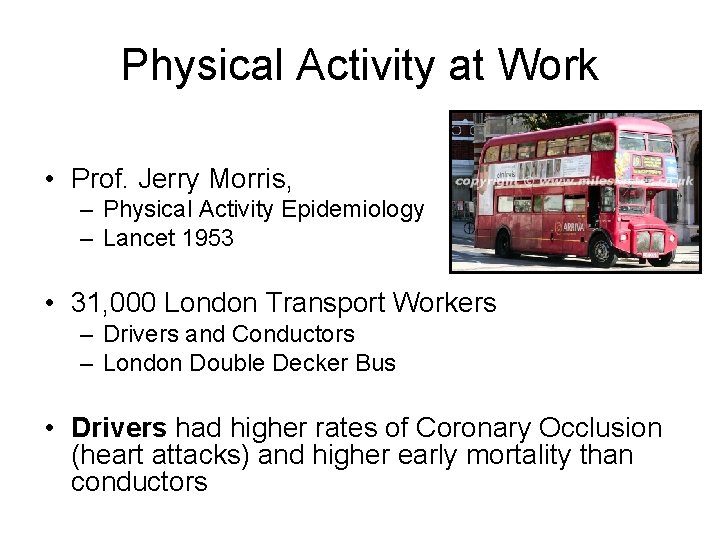
Physical Activity at Work • Prof. Jerry Morris, – Physical Activity Epidemiology – Lancet 1953 • 31, 000 London Transport Workers – Drivers and Conductors – London Double Decker Bus • Drivers had higher rates of Coronary Occlusion (heart attacks) and higher early mortality than conductors
Does type of exercise matter?
Does type of exercise matter?
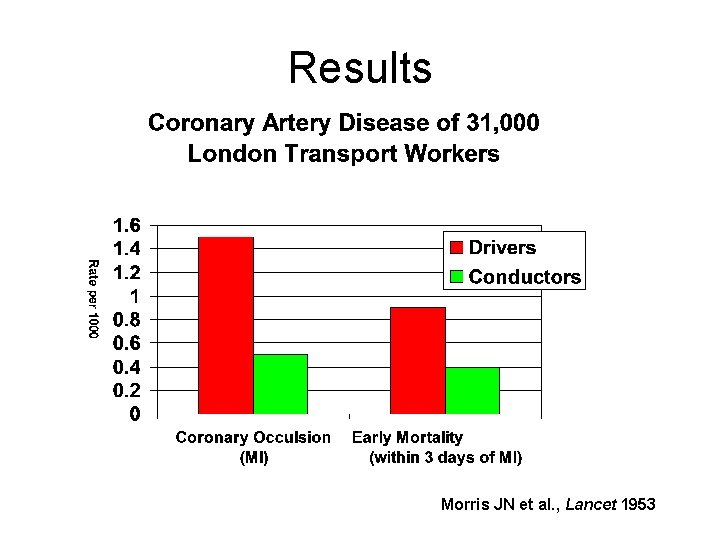
Results Morris JN et al. , Lancet 1953
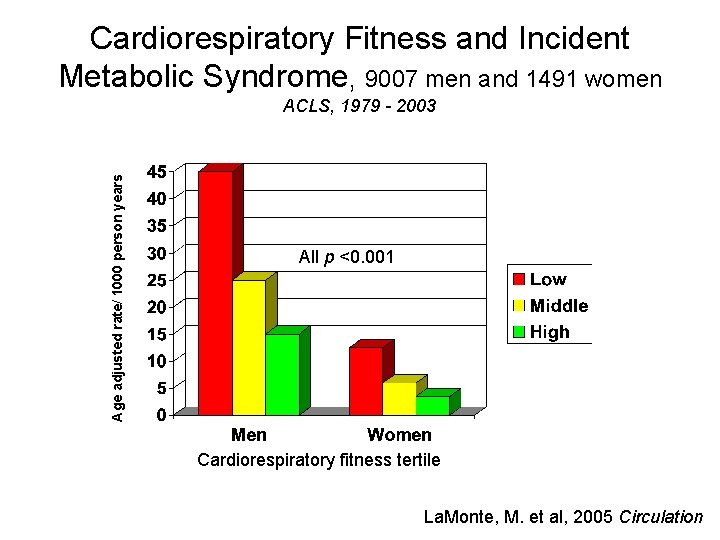
Cardiorespiratory Fitness and Incident Metabolic Syndrome, 9007 men and 1491 women Age adjusted rate/ 1000 person years ACLS, 1979 - 2003 All p <0. 001 Cardiorespiratory fitness tertile La. Monte, M. et al, 2005 Circulation

Need environment conducive to exercise
Obesity • Pandemic in Adults and Children • Tracks to adulthood strongly from kids • Is preventable • Is treatable
Malnutrition in Hospital
Malnutrition in Hospitals “Food is your medicine - hence let your medicine be your food” Hippocrates, circa 400 BC
Malnutrition in Hospitals • Malnutrition risk has been identified in 20% - 60% of hospital admissions to medical, surgical, elderly and orthopaedic wards. • Further, hospitalization with surgery or other medical treatments often result in additional weight loss. • It has been reported as undiagnosed in up to 70% of cases.
Malnutrition in Hospitals • Under-nutrition is associated with – Impairment of body systems including muscle weakness, immune system and gut function – Delayed wound healing – Apathy and depression – Reduction of appetite and ability to eat – Increased mortality rates
Which patients are at risk? • • Elderly Cancer Trauma/ sepsis Chronic disease states Pre and post operative Obese as well as normal weight Alcohol dependent
Malnutrition in Hospitals • There are many cost benefits in treating and preventing under-nutrition including – Reduced length of stay as inpatient – Reduced costs per stay – Reduced mortality • Benefits are seen the earlier undernutrition is recognised and treated
MUST • ‘Malnutrition Universal Screening Tool’ • Allows health care professionals to easily identify those at risk of malnutrition in a rapid and consistent manner. • This best targets appropriate nutrition therapy.
MUST • A screening tool should be used within the hospital to identify patients at risk of malnutrition • Within 48 hours of admission • Once weekly thereafter • Need to act on results of the screening tool • Should be included in nursing handover
MUST • • • Quick and easy to complete Universal- suitable for all patients Facilitates continuity of care Evidence- based Precedes nutritional assessment Ensures appropriate referrals
MUST Take a look at the format of the MUST screening tool………. .
The 5 steps of ‘MUST’ • Steps 1 -3: Take 3 measurements and score them against the scale provided • BMI • Weight loss • Acute disease effect • Step 4: Add scores together to identify overall risk of malnutrition • Step 5: Form appropriate care plan in line with local policy
What do you need to measure? • Weight: – Only 25% of patients are weighed on admission. (Mc. Whirter & Pennington, 1994) – Very difficult to assess nutritional status without weight • Height: – Measure with stadometer (height measure) – Self reported or Ulna Length • BMI: Weight / Height 2 – Normal range = 20 -25 kg/m 2 – Below 20 kg/m 2 possible malnutrition – Below 18. 5 kg/m 2 likely malnutrition NB. A word of warning Obese patients can still be at risk of malnutrition if they lose weight rapidly i. e. lose lean body mass
Step 1 • Weigh the patient
Step 1 • Measure the patients height using the stadometer – height measure
Step 1 – if you can’t measure height…. Estimated height from ulna length
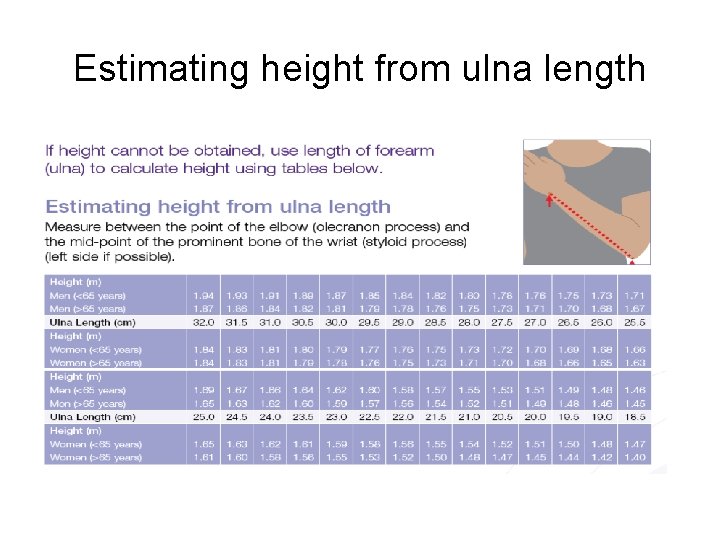
Estimating height from ulna length
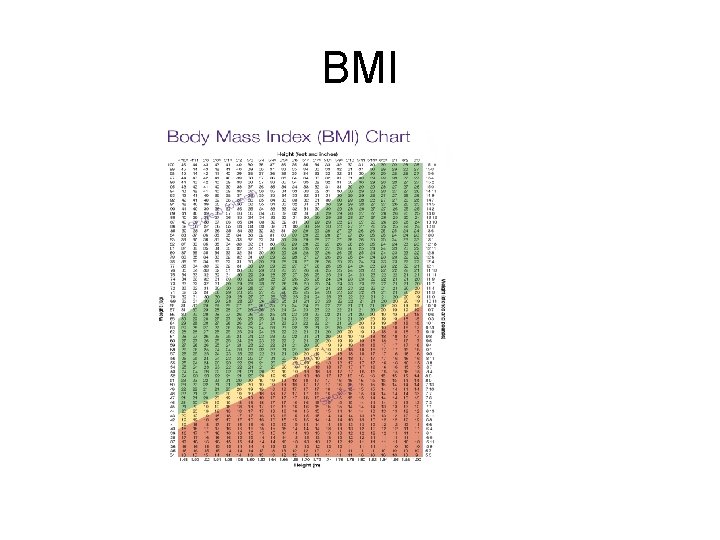
BMI
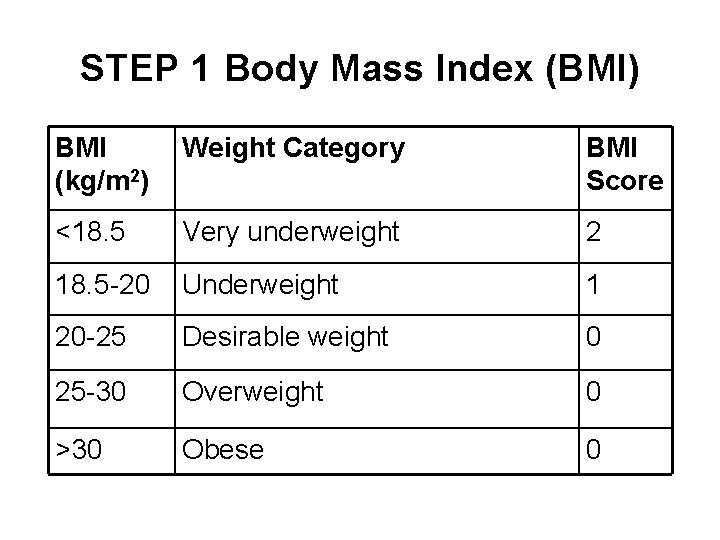
STEP 1 Body Mass Index (BMI) BMI (kg/m 2) Weight Category BMI Score <18. 5 Very underweight 2 18. 5 -20 Underweight 1 20 -25 Desirable weight 0 25 -30 Overweight 0 >30 Obese 0
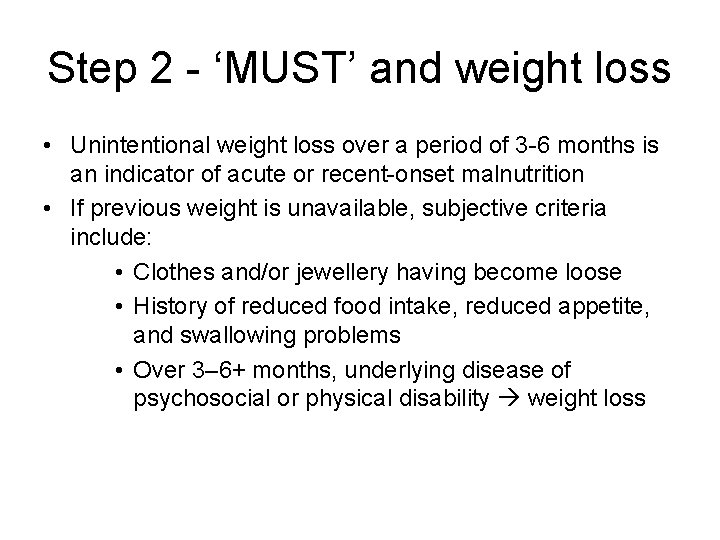
Step 2 - ‘MUST’ and weight loss • Unintentional weight loss over a period of 3 -6 months is an indicator of acute or recent-onset malnutrition • If previous weight is unavailable, subjective criteria include: • Clothes and/or jewellery having become loose • History of reduced food intake, reduced appetite, and swallowing problems • Over 3– 6+ months, underlying disease of psychosocial or physical disability weight loss
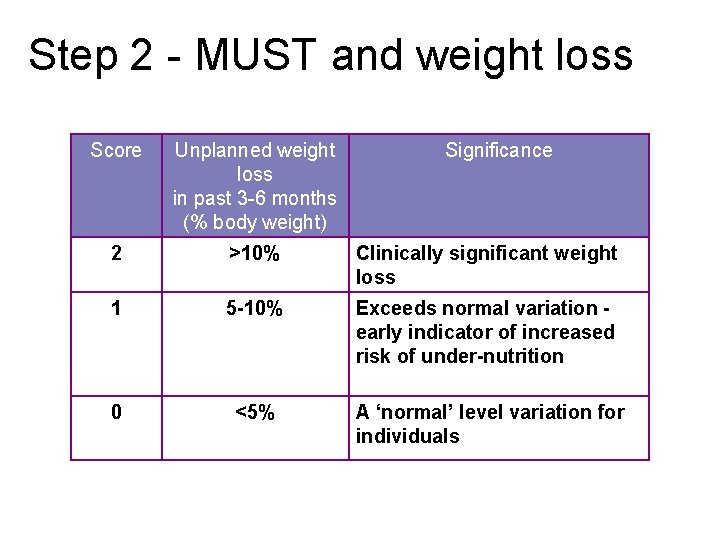
Step 2 - MUST and weight loss Score Unplanned weight loss in past 3 -6 months (% body weight) Significance 2 >10% Clinically significant weight loss 1 5 -10% Exceeds normal variation early indicator of increased risk of under-nutrition 0 <5% A ‘normal’ level variation for individuals
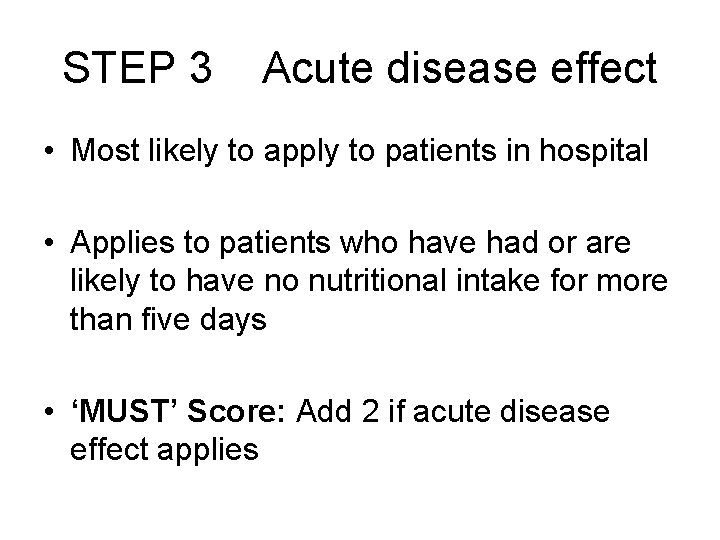
STEP 3 Acute disease effect • Most likely to apply to patients in hospital • Applies to patients who have had or are likely to have no nutritional intake for more than five days • ‘MUST’ Score: Add 2 if acute disease effect applies
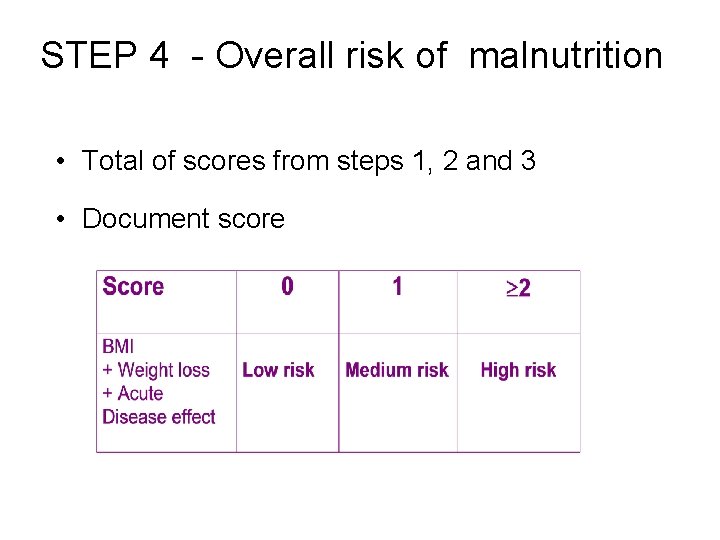
STEP 4 - Overall risk of malnutrition • Total of scores from steps 1, 2 and 3 • Document score
STEP 5 Nutrition Care Plan • Low risk of malnutrition – Repeat screening weekly • Medium and high risk of malnutrition – Nutritional intervention – refer to dietitian – Repeat screening weekly
Need to • Screen in all healthcare institutions • Get the surgeons on board • Manage obesity in hopsital – huge missed opportunity
10 Key Characteristics of good nutritional care in hospitals • All patients are screened on admission to identify the patients who are malnourished or at of becoming malnourished. All patients are re-screened weekly. • All patients have a care plan which identifies their nutritional care needs and how they are to be met.

10 Key Characteristics of good nutritional care in hospitals • The hospital includes specific guidance on food services and nutritional care in its Clinical Paths • Patients are involved in the planning and monitoring arrangements for food service provision. • The ward implements Protected Mealtimes to provide an environment conducive to patients enjoying and being able to eat their food.
10 Key Characteristics of good nutritional care in hospitals • All staff have the appropriate skills and competencies needed to ensure that patient’s nutritional needs are met. • All staff receive regular training on nutritional care and management. • Hospital facilities are designed to be flexible and patient centred with the aim of providing and delivering an excellent experience of food service and nutritional care 24 hours a day, every day.

10 Key Characteristics of good nutritional care in hospitals • The hospital has a policy for food service and nutritional care which is patient centred and performance managed in line with home country governance frameworks. • Food service and nutritional care is delivered to the patient safely. • The hospital supports a multi-disciplinary approach to nutritional care and values the contribution of all staff groups working in partnership with patients and users.
Thank you.
- Slides: 94