Nutritional support Nutritional support includes the use of




- Slides: 61

Nutritional support
Nutritional support: includes: the use of artificial feeding methods such as tube feeding (Enteral feeding), total parenteral nutrition (TPN) and administration of intravenous fluids. Nutritional support means the provision of patient's dietary requirements
Critically ill patients are often unable to eat because of certain conditions: 1 -Endotracheal intubation. 2 -The need for mechanical ventilation. 3 -Altered level of consciousness as a result of severe trauma, major surgery or acute medical condition. Lack of nutrients may: 1 -Alter the structure and function of the gut. 2 -Increase the risk of entry and spread of intestinal bacteria.
Early nutritional support for critically ill patients has been advocated to: 1 -Promote the immune system recovery 2 -prevent as much as tissue breakdown 3 -avoid nutritional deficit as possible 4 -Improves patient outcomes. 5 -Enhances recovery from illness.
Enteral Nutrition • Enteral Nutrition or tube feeding is a way of providing nutrition support via the GIT for patients unable to otherwise meet nutrition requirements by the oral route. • Enteral feeding has several advantages over total parenteral nutrition: 1. EN has been shown to be easier, safer and cheaper than PN. 2. EF maintains the structure and functional integrity of the gastrointestinal tract by intraluminal delivery of nutrients and preventing atrophic changes.

3. EF preserves the normal sequence of intestinal and hepatic metabolism, fat metabolism, lipoprotein synthesis and prevents cholestasis by stimulating bile flow. 4. Maintains normal insulin / glucagon ratio. 5. Reduction in septic complications with EF compared with PN. 6. EF improves systemic immunity and lower infection risk. 7. Prevents translocation of bacteria into the systemic circulation and reduce the incidence of sepsis.
• On the other hand, intragastric EN often is complicated by intolerance, as indicated by elevated volumes of aspirated gastric residual. High gastric residual is a return of at least half of the hourly feeding rate. • It is commonly accepted that high gastric residual volume enhances regurgitation and increases the risk for aspiration pneumonia.
• Gastric residual is the amount of previous feeding remaining in the stomach. • This fluids commonly accumulate in the gastrointestinal tract of a tube fed patient include the • 1 -Feeding formula • 2 -Swallowed saliva (> 0. 8 L/ day), • 3 -Gastric secretion (1. 5 L/ day), • 4 -Small bowel secretion regurgitated into the stomach (2. 7 – 3 L/ day).
• Micro aspiration – Aspiration of small volume that is usually asymptomatic and clinically undetected. • Macro aspiration – Aspiration of large volume that is usually detected by clinical observation. • Silent aspiration – Aspiration occurring in the absence of acute symptoms. • Symptomatic aspiration – Aspiration accompanied by acute clinical symptoms of coughing, choking, dyspnea, or respiratory distress.
• Patients receiving isotonic formulas who are given too much fluid may show signs of fluid excess such as weight gain, edema and may develop dilutional hyponatremia.

• On the other hand, patients receiving hypertonic, high-protein feedings who do not ingest enough fluid are at risk for life-threatening condition called tube-feeding syndrome, characterized by fluidvolume deficit, hypernatremia, hyperchloremia and azotemia.

• So it is very important to monitor and assess fluid intake and output such as 1 - body weight, 2 - edema and respiratory rate, 3 - blood urea nitrogen and other electrolytes.
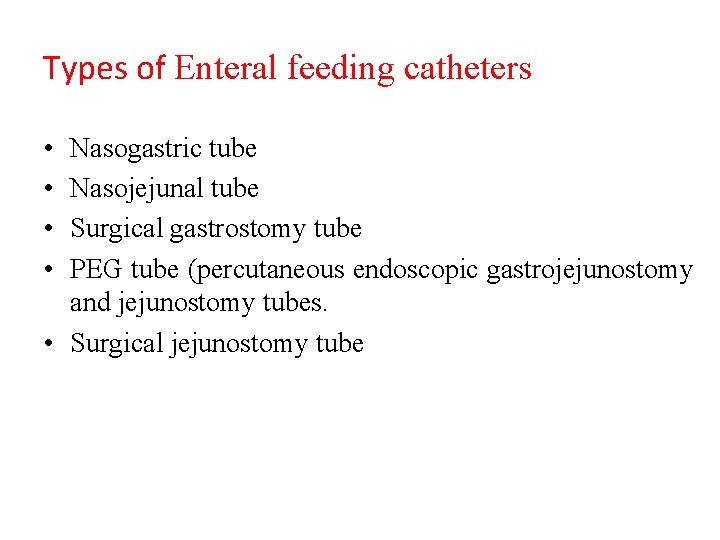
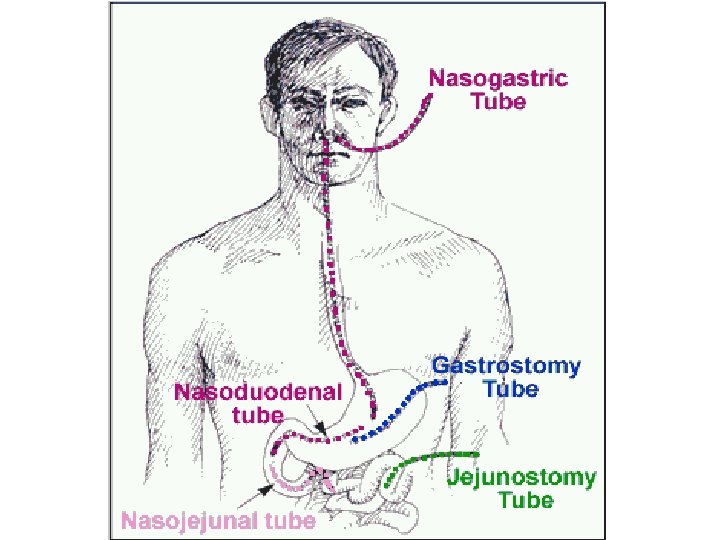
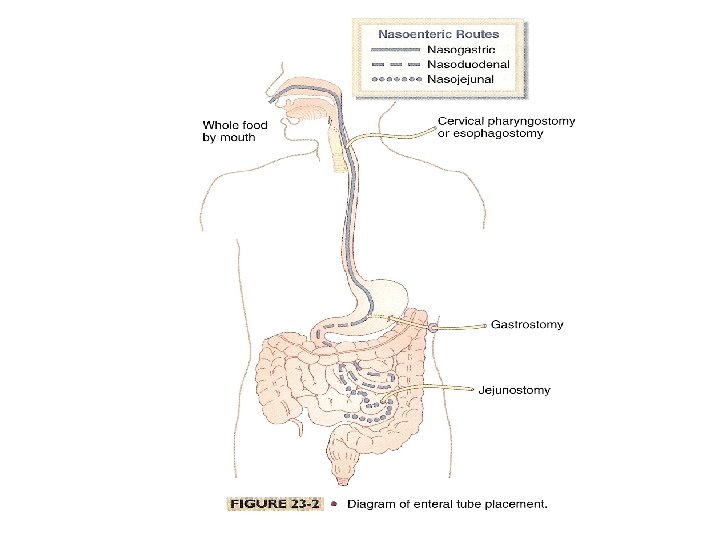
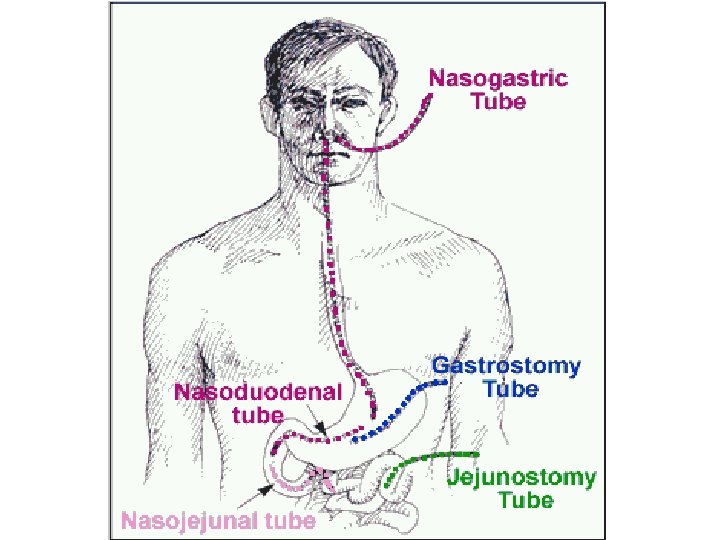
Types of Enteral feeding catheters • • Nasogastric tube Nasojejunal tube Surgical gastrostomy tube PEG tube (percutaneous endoscopic gastrojejunostomy and jejunostomy tubes. • Surgical jejunostomy tube
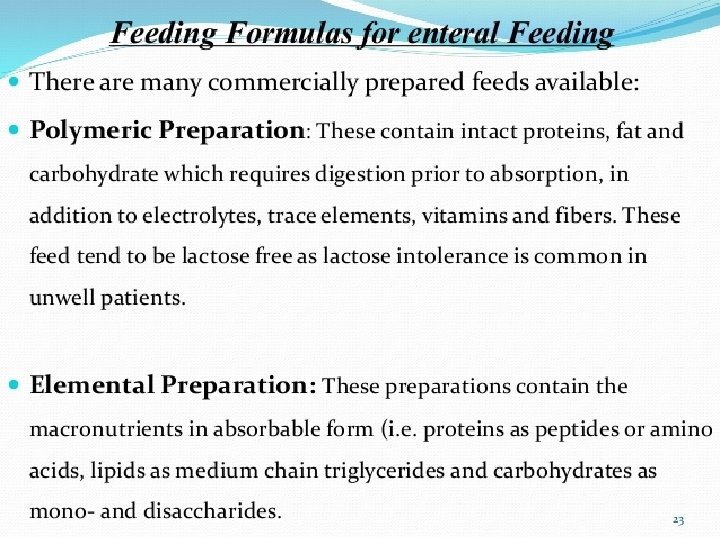
Tube feeding formulations • Standard polymeric • Elemental or small peptide • Disease specific
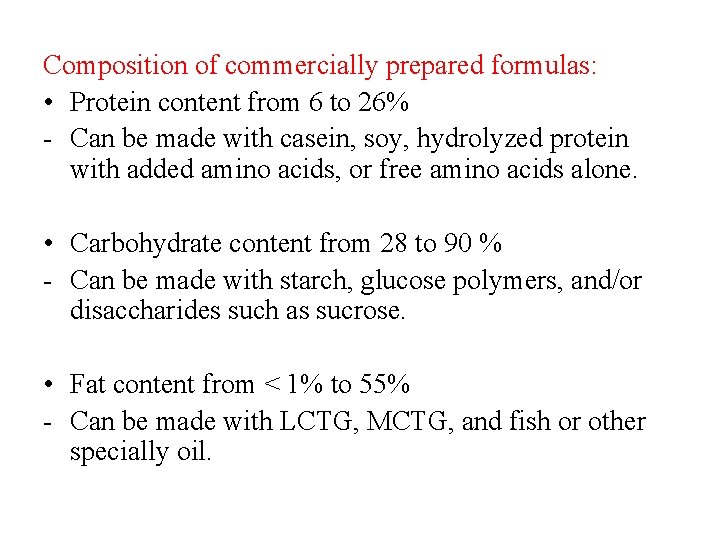
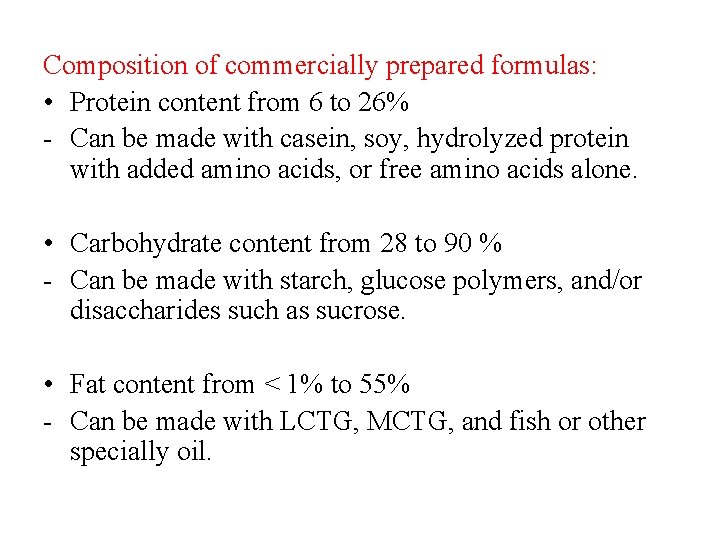
Composition of commercially prepared formulas: • Protein content from 6 to 26% - Can be made with casein, soy, hydrolyzed protein with added amino acids, or free amino acids alone. • Carbohydrate content from 28 to 90 % - Can be made with starch, glucose polymers, and/or disaccharides such as sucrose. • Fat content from < 1% to 55% - Can be made with LCTG, MCTG, and fish or other specially oil.
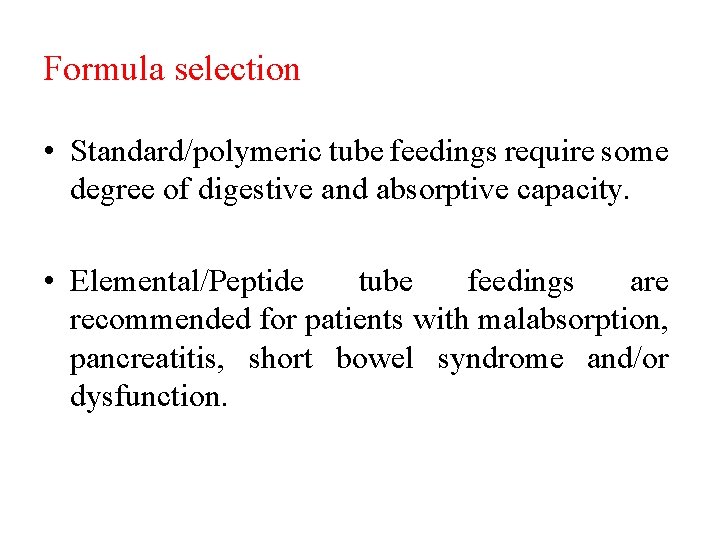
Formula selection • Standard/polymeric tube feedings require some degree of digestive and absorptive capacity. • Elemental/Peptide tube feedings are recommended for patients with malabsorption, pancreatitis, short bowel syndrome and/or dysfunction.
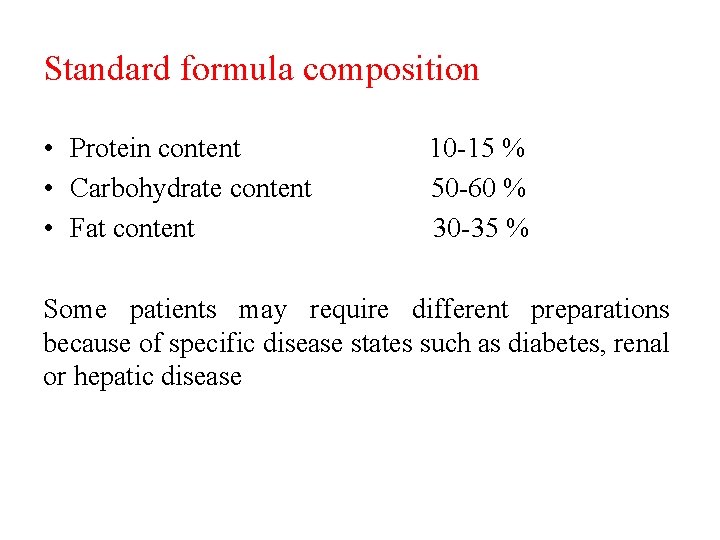
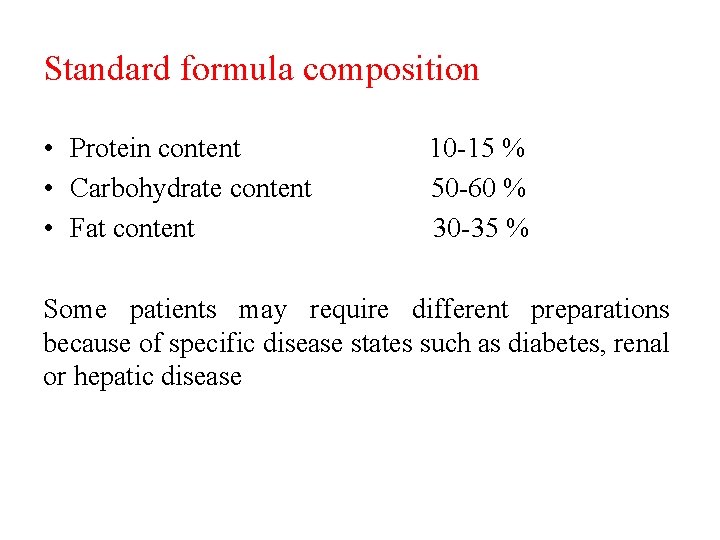
Standard formula composition • Protein content • Carbohydrate content • Fat content 10 -15 % 50 -60 % 30 -35 % Some patients may require different preparations because of specific disease states such as diabetes, renal or hepatic disease
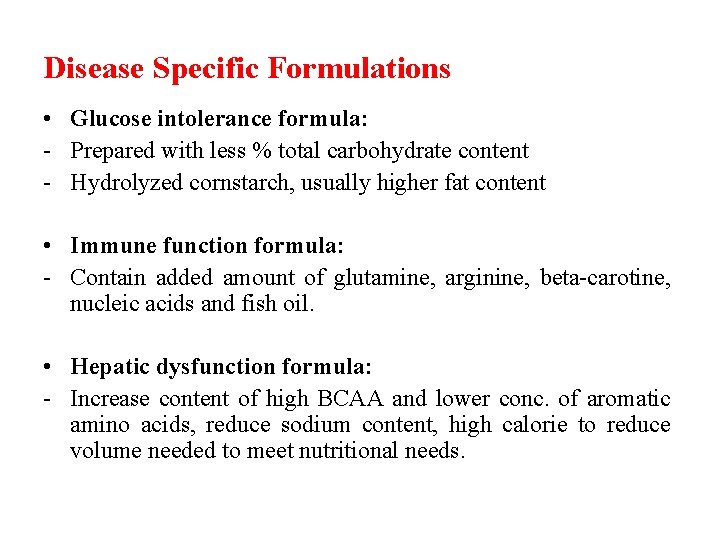
Disease Specific Formulations • Glucose intolerance formula: - Prepared with less % total carbohydrate content - Hydrolyzed cornstarch, usually higher fat content • Immune function formula: - Contain added amount of glutamine, arginine, beta-carotine, nucleic acids and fish oil. • Hepatic dysfunction formula: - Increase content of high BCAA and lower conc. of aromatic amino acids, reduce sodium content, high calorie to reduce volume needed to meet nutritional needs.
Disease Specific Formulations • Renal dysfunction formula: - High calorie, high protein, modified level of electrolytes and specific alterations in vitamin and mineral content. • Trauma formulation: - High protein, high calorie, some with increased BCAA content, some with added glutamine, arginine, special fat blends, increased levels of copper and zinc. • Wound healing formulation: - High protein and high content of vitamin A, vitamin C and zinc.
Monitoring tube feeding tolerance • Gastric residuals: volume aspirated from a feeding tube placed in the stomach should not exceed 250 ml volume. • Abdominal distension. • Diarrhea. • Constipation.
Contraindications for EN • • • Severe acute pancreatitis High output proximal fistula Inability to gain access Intractable vomiting or diarrhea Aggressive therapy not warranted
Contraindications for EN • Inadequate resuscitation or hypotension; hemodynamic instability • Ileus disease • Intestinal obstruction • Severe G. I. Bleed
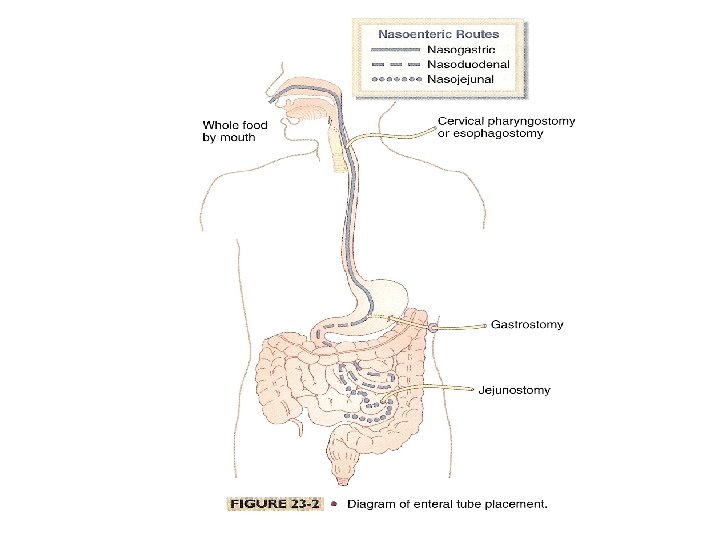
Nasogastric Tubes • A tube inserted through the nasal passage into the stomach Indications: • Short term feedings required • Intact gag reflex • Gastric function not compromised • Low risk for aspiration
Nasogastric Tubes Advantages: • Ease of tube placement • Surgery not required • Easy to check gastric residuals • Accommodates various administration techniques Disadvantages: • Increases risk of aspiration (may be) • Not suitable for patients with compromised gastric function • May promote nasal necrosis and esophagitis • Impacts patient quality of life
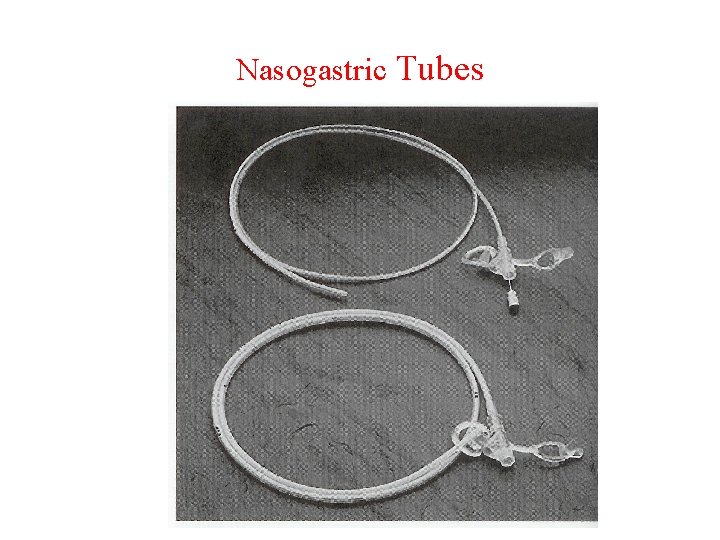
Nasogastric Tubes
Nasoduodenal/Jejunal • A tube inserted through the nasal passage through the stomach into the duodenum or jejunum Indications: • High risk of aspiration • Gastric function compromised Advantages: • Allows for initiation of early enteral feeding • May decrease risk of aspiration • Surgery not required
Nasoduodenal/Jejunal Disadvantages: • Transpyloric tube placement may be difficult • Limited to continuous infusion • May promote nasal necrosis and esophagitis • Impacts patient quality of life
Orogastric • Tube is placed through mouth and into stomach • Often used in premature and small infants as they are nasal breathers • Not tolerated by alert patients; tubes may be damaged by teeth
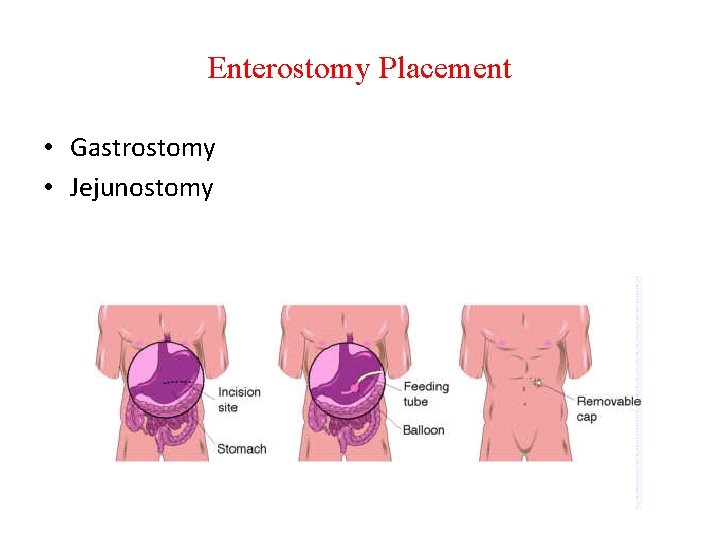
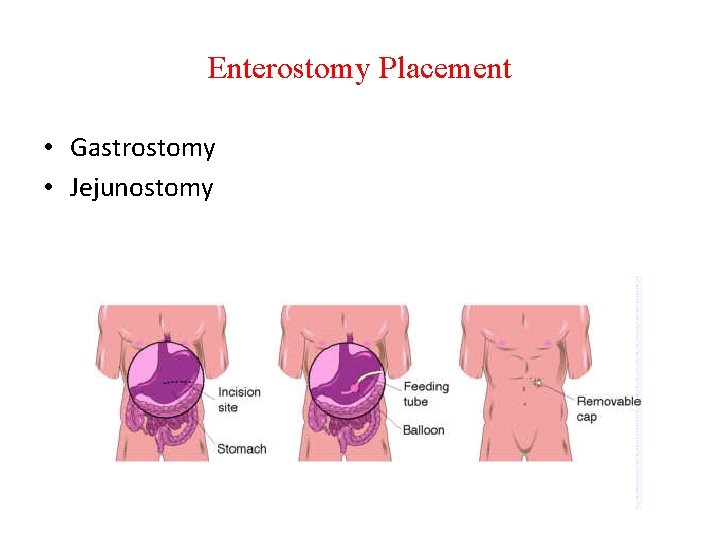
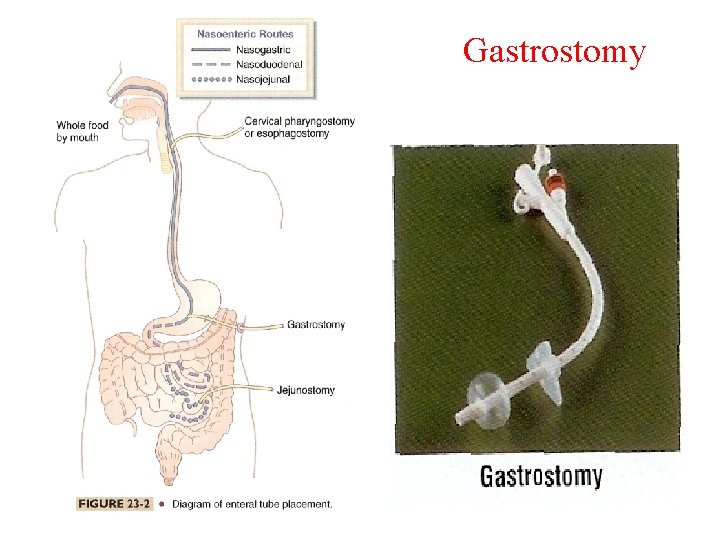
Enterostomy Placement • Gastrostomy • Jejunostomy
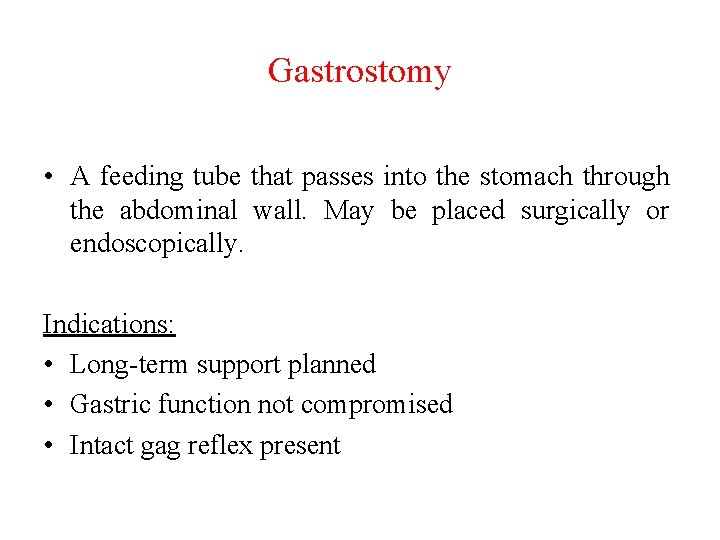
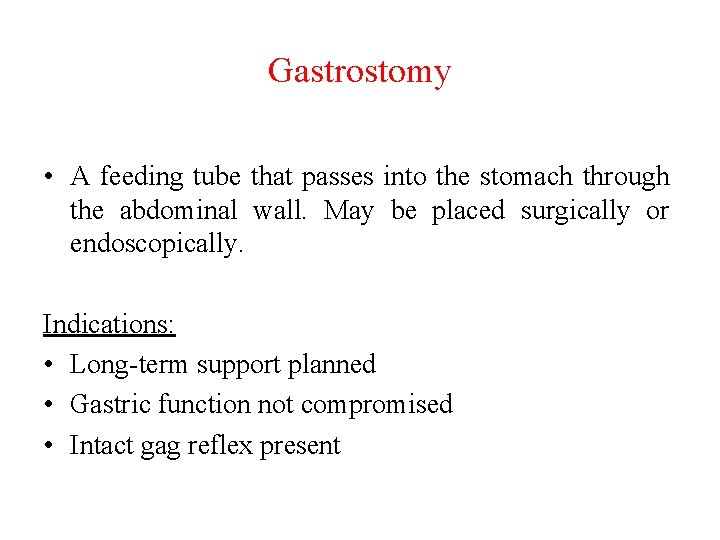
Gastrostomy • A feeding tube that passes into the stomach through the abdominal wall. May be placed surgically or endoscopically. Indications: • Long-term support planned • Gastric function not compromised • Intact gag reflex present
Gastrostomy Disadvantages: • May require surgery • Stoma care required • Potential problems for leakage or tube dislodgment
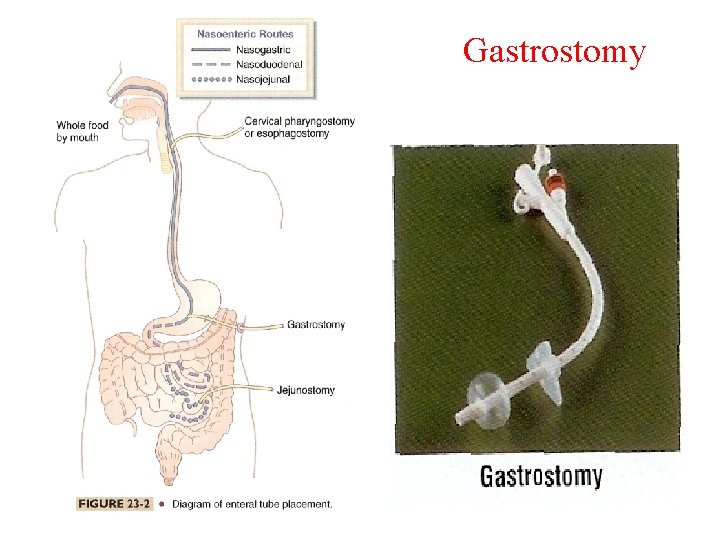
Gastrostomy
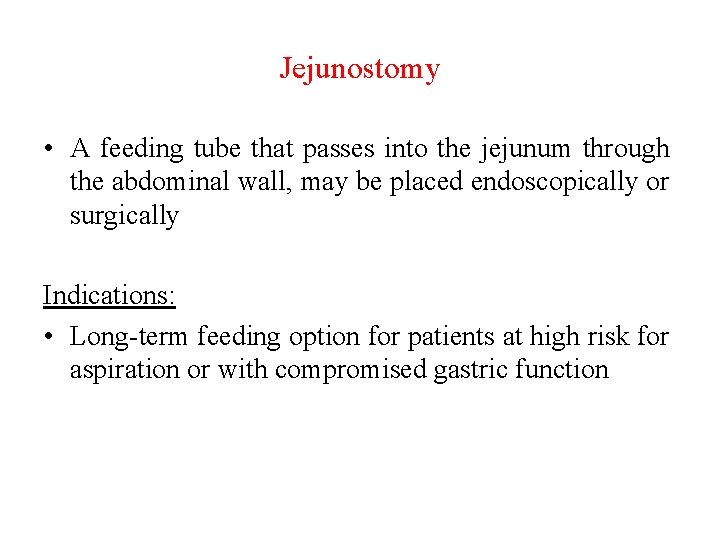
Jejunostomy • A feeding tube that passes into the jejunum through the abdominal wall, may be placed endoscopically or surgically Indications: • Long-term feeding option for patients at high risk for aspiration or with compromised gastric function
Jejunostomy Advantages: • Post-op feedings may be initiated immediately • Decreased risk of aspiration • Suitable option for patients with compromised gastric function • Stable patients can tolerate intermittent feedings
Jejunostomy Disadvantages: • Requires stoma care • Potential problems related to leakage or tube dislodgement/clogging may arise • May restrict ambulation • Bolus feedings inappropriate (stable patients may tolerate intermittent feedings)
Determining Method of Administration • • • Feeding site Clinical status of patient Type of formula used Availability of pump Mobility of patient
Enteral Feeding Complications • • Mechanical Gastrointestinal Metabolic Infectious
Mechanical complication • Aspiration • Tube obstruction • Tube displacement
• Aspiration is the most dangerous mechanical complication associated with EF. • Pulmonary aspiration of EF with subsequent pneumonia is a frequent and serious complication of enteral nutrition in critically ill adults despite the presence of cuffed and properly inflated endotracheal tubes.
• Aspiration pneumonia develops in 43% of patients on nasogastric tube feeding and in 56% of patients with a gastrostomy.
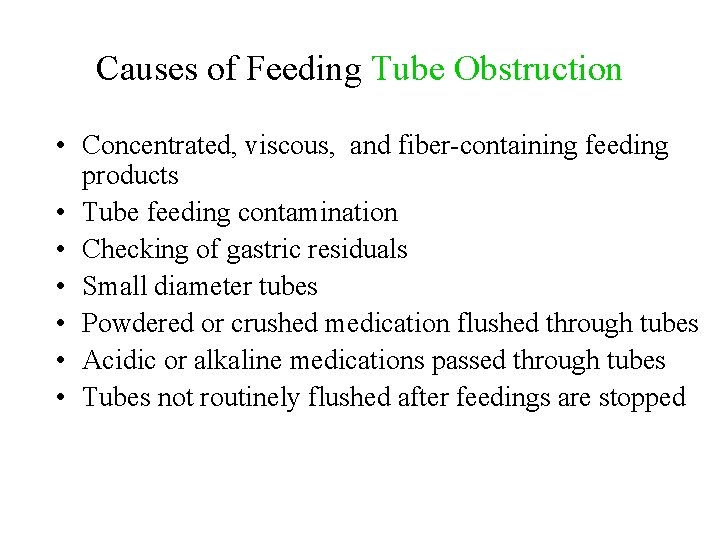
Causes of Feeding Tube Obstruction • Concentrated, viscous, and fiber-containing feeding products • Tube feeding contamination • Checking of gastric residuals • Small diameter tubes • Powdered or crushed medication flushed through tubes • Acidic or alkaline medications passed through tubes • Tubes not routinely flushed after feedings are stopped
Treatment of Feeding Tube Obstruction • Declog with irrigants (warm water) or sodium bicarbonate/pancrealipase mixture or by mechanical means • Cola beverages, cranberry juice, and tea not recommended
Gastrointestinal Complications • • • Diarrhea Constipation Gastric distention/bloating Gastric residuals/delayed gastric emptying Nausea/vomiting
Diarrhea • Definition: >500 ml every 8 hours or more than 3 stools a day for at least two consecutive days. Relates more to stool consistency than frequency • Diarrhea was a common consequence of enteral feedings when hyperosmolar feedings were routinely delivered via syringe • Occurs in 2 to 63% of enterally-fed pts depending on how defined
Causes of Diarrhea • Intestinal atrophy due to malnutrition. • Use an infusion pump to regulate flow. • Bacterial overgrowth of intestinal tract or contamination of the enteral feeding. • Steatorrhea: characterized by frothy, odiferous stools that float on water; caused by fat intolerance. • Lactose intolerance (lactose free & eliminate milk and dairy products).
Causes of Diarrhea • Drug-induced diarrhea – Meds may cause up to 61% of diarrhea in tube fed patients due to hypertonicity or direct laxative action (magnesium, sorbitol, potassium), and it is common with antibiotics. • GI disease: such as IBS, short gut, celiac disease, AIDS – May require PN or specially formulated EN
Nausea/Vomiting • 20% of patients on EN report nausea/vomiting • Often related to delayed gastric emptying caused by hypotension, sepsis, stress, anesthesia, medications (analgesics and anticholinergics), surgery.
Nausea/Vomiting Treatment • Consider reducing/discontinuing narcotic medications • Switch to a lowf at formula • Administer feeding solution at room temperature • Reduce rate of infusion by 20 -25 ml/hr • Administer prokinetic agent (metoclopramide, erythromycin, domperidone, bethanechol) • Check gastric residuals • Consider antiemetics
Metabolic • • Fluid and Electrolyte abnormalities Glucose intolerance Ca++, Mg++, PO 4 abnormalities Other
Fluid and Electrolyte Disturbances • May result from long term nutrition deficits, acute stress, medications, medical conditions, improper nutrient prescription • Electrolytes lost via stool, urine, ostomy or fistula drainage • Dehydration most common complication (tube feeding syndrome) especially with high protein feeding and insufficient fluid
• Hyperglycemia: complication that can be caused by high carbohydrate formula and Hyperosmolar feeding of fluid overload. • Hyperglycemia can be prevented by: 1 - Monitoring for fluid balance, urine and blood for glucose. 2 - Administering insulin on a sliding scale if necessary 3 - Changing the formula to lower calorie content and observing for hypercapnea.
• Hypoglycemia, caused by: • Sudden cessation of feeding can be prevented by frequent monitoring of blood sugar if feeding is interrupted.
• Dehydration caused by: 1 -High osmolality formula. 2 -Diarrhea and excessive protein intake with inadequate fluid intake. 3 -Large amount of fluid that can be lost during prolonged uncorrected vomiting and diarrhea without adequate replacement of fluid and electrolytes. 4 - gastric and intestinal suctioning occur without the proper monitoring
• Overhydration, can be caused by: 1 -Fluid overload, 2 -When the metabolic demands are high and the organ function is impaired namely cardiac, renal or hepatic. Management of Overhydration: 1 -Restricting free water intake 2 -Changing to concentrated formula 3 -Administering diuretics 4 -Decrease the delivery rate.
Refeeding Syndrome • At risk: when refeeding those with marginal body nutrient stores, stressed, depleted patients, those who have been unfed for 7 -10 days, persons with anorexia nervosa, chronic alcoholism, weight loss • Symptoms: Hypokalemia, hypophosphatemia and hypomagnesemia; cardiac arrhythmias, heart failure; acute respiratory failure
Refeeding Syndrome • Correct electrolyte abnormalities (via oral, enteral, parenteral route) before initiating nutrition support • Administer volume and energy slowly • Monitor pulse rate, intake and output, and electrolyte levels • Provide appropriate vitamin supplementation • Avoid overfeeding
Infectious Complications • Formula contamination • Unsanitary equipment • Failure to follow appropriate protocols re handling of enteral feedings/changing of bags and tubing
Monitoring of Patients on EN • • • Electrolytes BUN/Cr Albumin/prealbumin Ca++, PO 4, Mg++ Weight Input/output Vital signs Stool frequency/consistency Abdominal examination