NUTRITIONAL SUPPORT IN CRITICALLY ILL Prof Mehdi Hasan












- Slides: 102
NUTRITIONAL SUPPORT IN CRITICALLY ILL Prof. Mehdi Hasan Mumtaz
PRINCIPAL Support for those who q q q Should not eat. Will not eat. Can not eat.
AIMS q q q Detection and correction of pre-existing malnutrition. Prevention of progressive protein energy malnutrition. Optimization of metabolic rate. Reduction of morbidity. Reduction of time to convalescence.
NUTRITIONAL ASSESSMENT q q q Dietary history. Clinical examination. Lab. Investigations. – – Hypoalbuminaemia<35 G/L. Lymphocytopenia<1500/mm 3. Serum transferase<1. 5 G/L. Cell mediated immunity –ve.
NUTRITIONAL ASSESSMENT q q q Changes in body mass. Skin fold measurements. Sophisticated techniques. – – Neutron activation analysis. Dual X-ray absorptiometry. MRI. Bioimpedance methods.
NUTRITIONAL REQUIREMENT q q Nitrogen loss Urine urea Protein loss Plasma urea Nitrogen loss by pyrochemilumiscence. Portable calorimetery (bedside). – – Gas leak. FIO 2. Water vapours. Steady state achievement
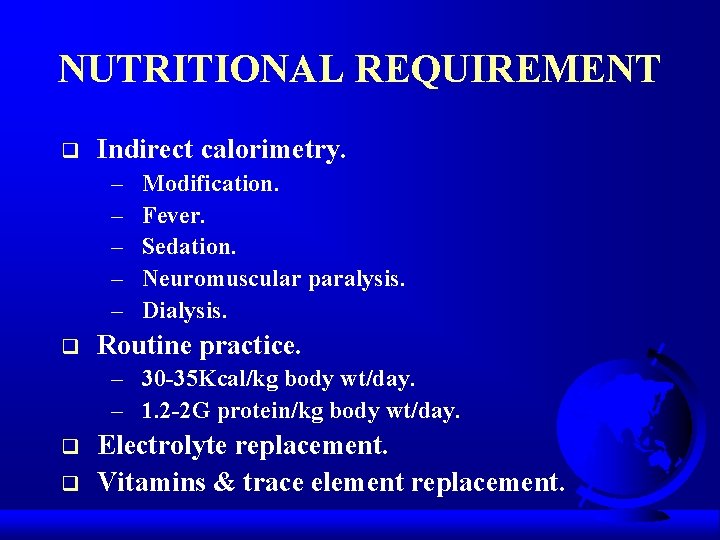
NUTRITIONAL REQUIREMENT q Indirect calorimetry. – – – q Modification. Fever. Sedation. Neuromuscular paralysis. Dialysis. Routine practice. – 30 -35 Kcal/kg body wt/day. – 1. 2 -2 G protein/kg body wt/day. q q Electrolyte replacement. Vitamins & trace element replacement.
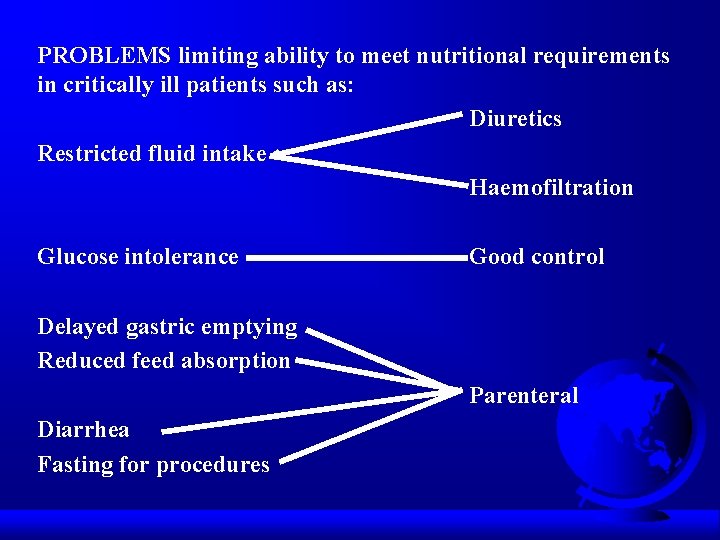
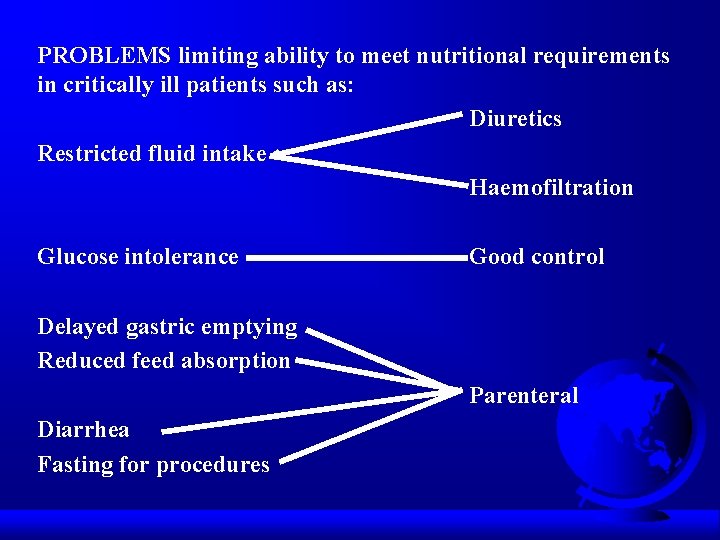
PROBLEMS limiting ability to meet nutritional requirements in critically ill patients such as: Diuretics Restricted fluid intake Haemofiltration Glucose intolerance Good control Delayed gastric emptying Reduced feed absorption Parenteral Diarrhea Fasting for procedures
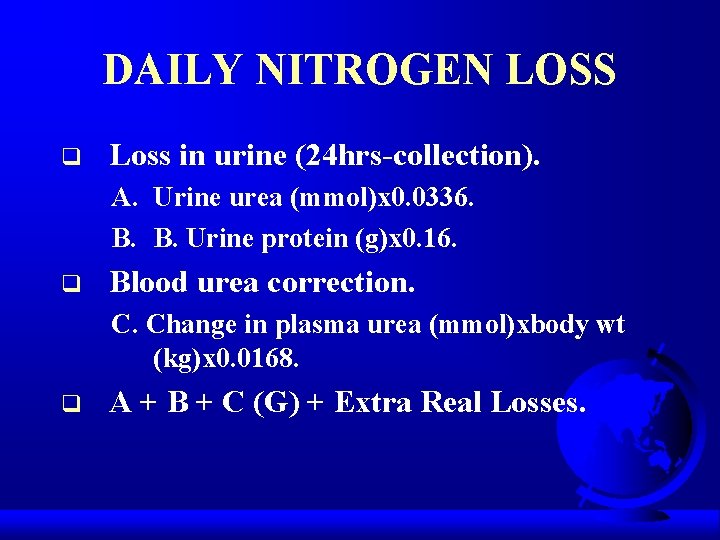
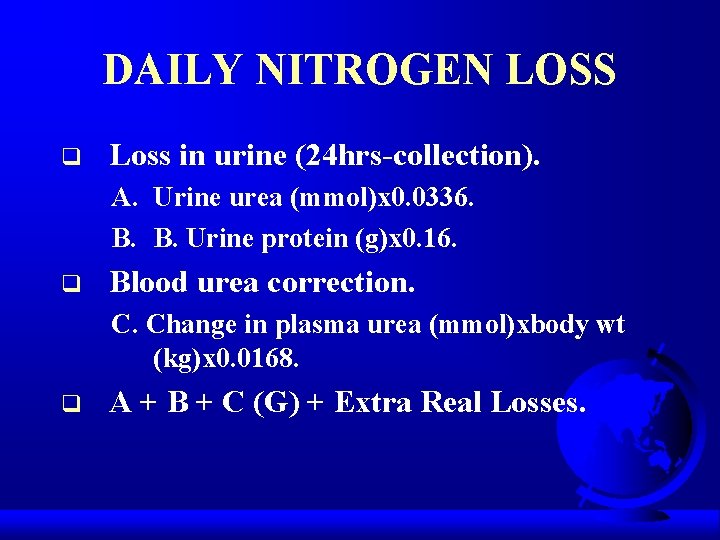
DAILY NITROGEN LOSS q Loss in urine (24 hrs-collection). A. Urine urea (mmol)x 0. 0336. B. B. Urine protein (g)x 0. 16. q Blood urea correction. C. Change in plasma urea (mmol)xbody wt (kg)x 0. 0168. q A + B + C (G) + Extra Real Losses.
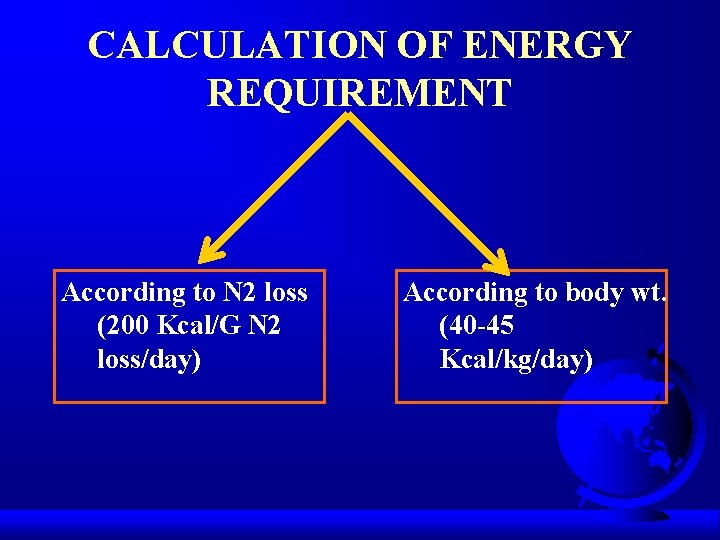
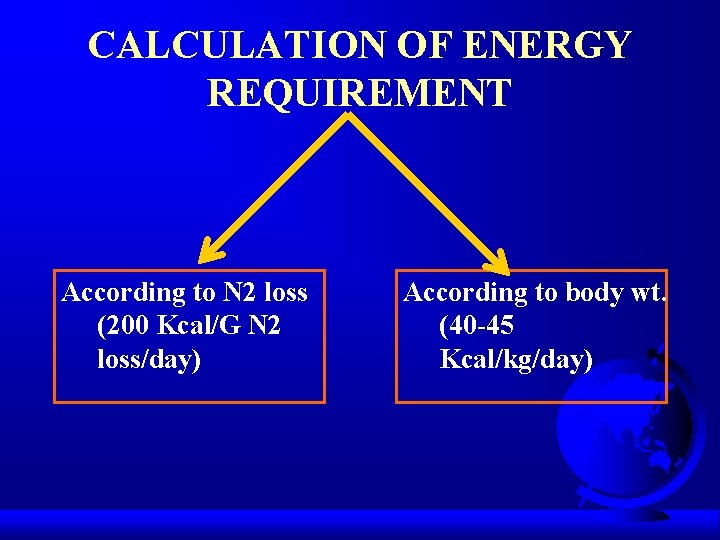
CALCULATION OF ENERGY REQUIREMENT According to N 2 loss (200 Kcal/G N 2 loss/day) According to body wt. (40 -45 Kcal/kg/day)
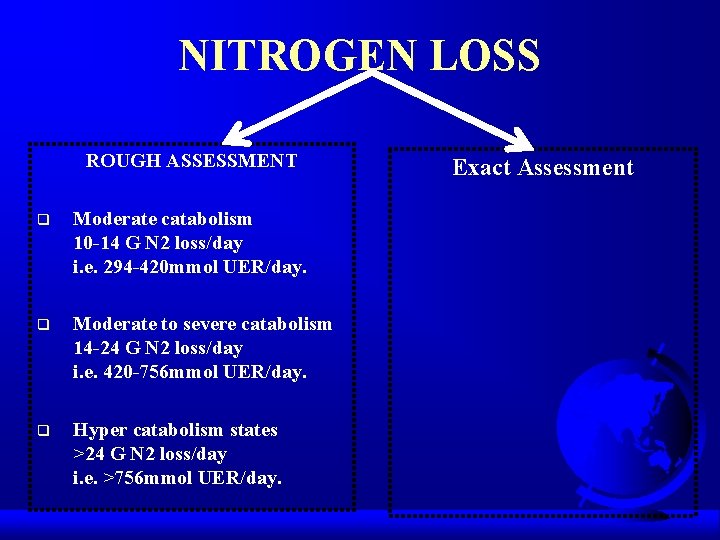
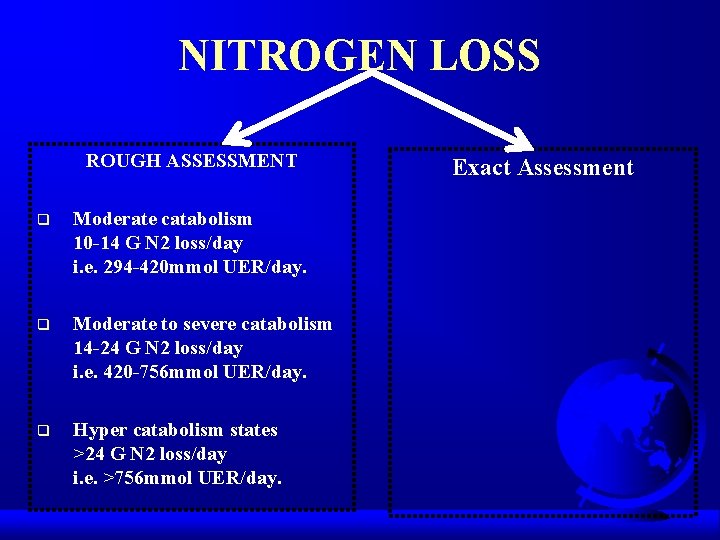
NITROGEN LOSS ROUGH ASSESSMENT q Moderate catabolism 10 -14 G N 2 loss/day i. e. 294 -420 mmol UER/day. q Moderate to severe catabolism 14 -24 G N 2 loss/day i. e. 420 -756 mmol UER/day. q Hyper catabolism states >24 G N 2 loss/day i. e. >756 mmol UER/day. Exact Assessment
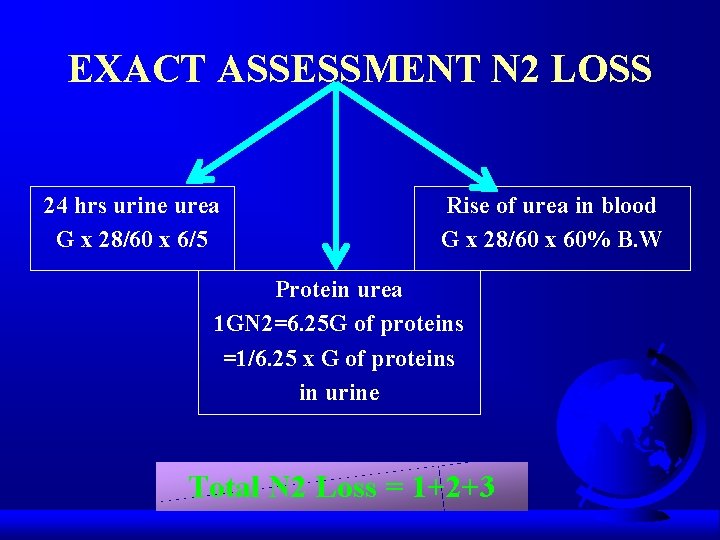
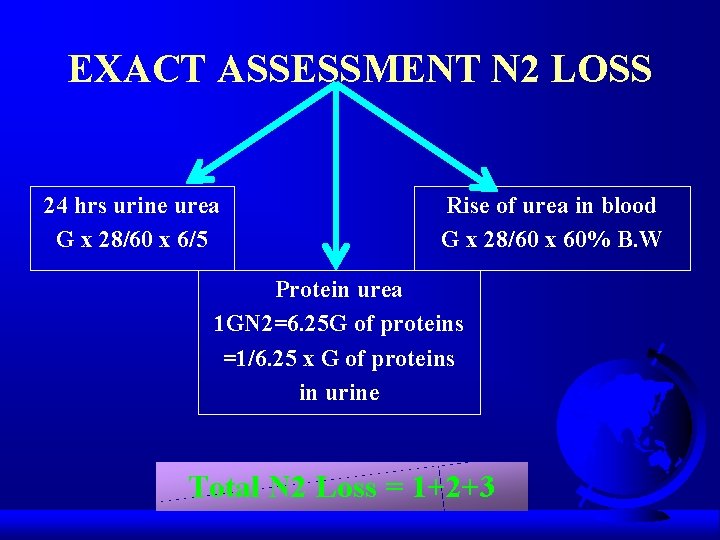
EXACT ASSESSMENT N 2 LOSS 24 hrs urine urea G x 28/60 x 6/5 Rise of urea in blood G x 28/60 x 60% B. W Protein urea 1 GN 2=6. 25 G of proteins =1/6. 25 x G of proteins in urine Total N 2 Loss = 1+2+3
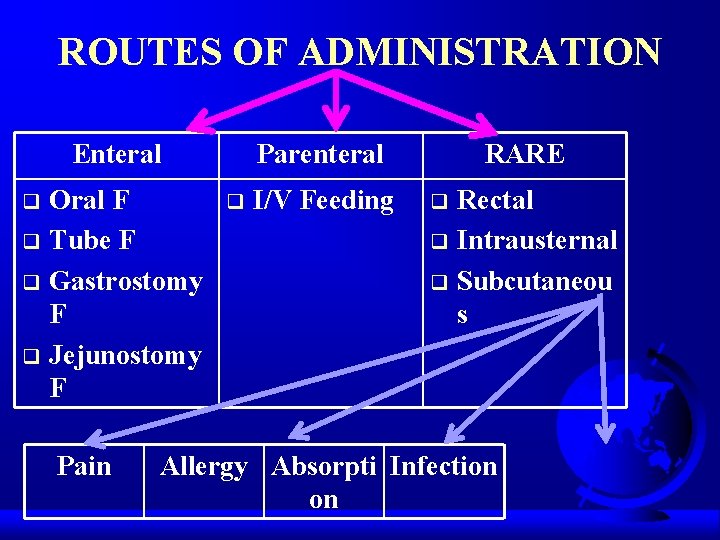
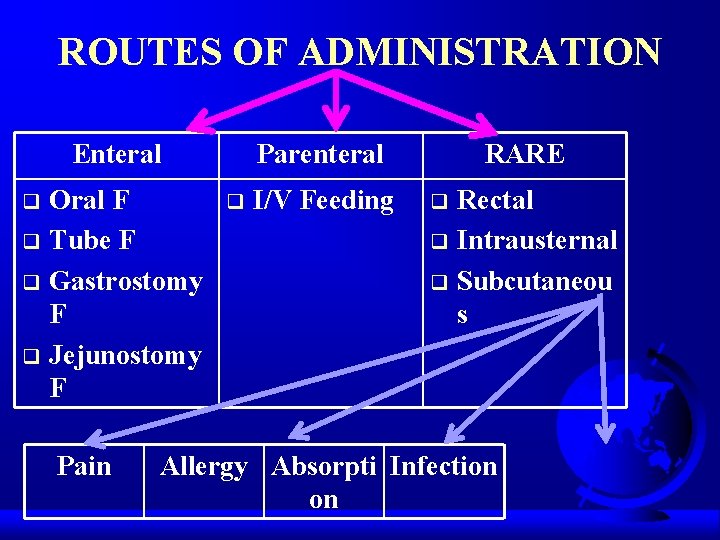
ROUTES OF ADMINISTRATION Enteral Oral F q Tube F q Gastrostomy F q Jejunostomy F q Pain Parenteral q I/V Feeding RARE Rectal q Intrausternal q Subcutaneou s q Allergy Absorpti Infection on
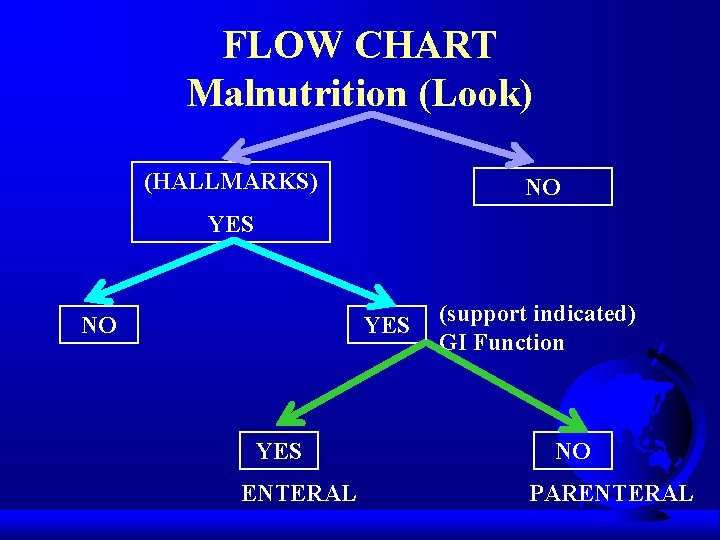
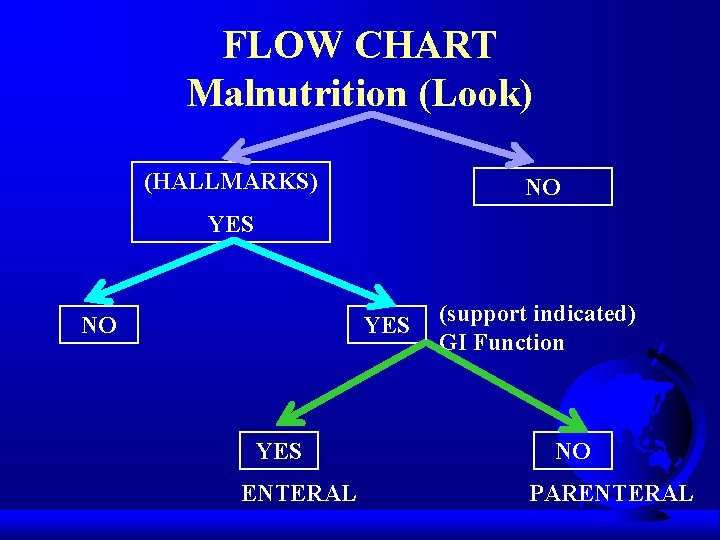
FLOW CHART Malnutrition (Look) (HALLMARKS) NO YES YES ENTERAL (support indicated) GI Function NO PARENTERAL
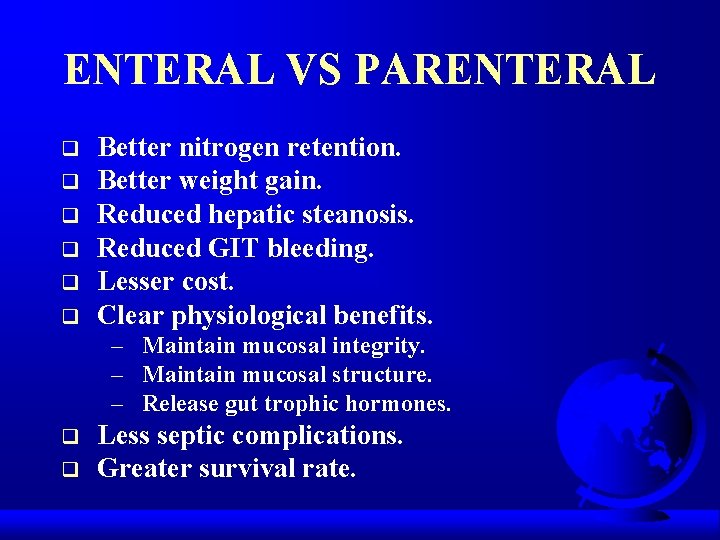
ENTERAL VS PARENTERAL q q q Better nitrogen retention. Better weight gain. Reduced hepatic steanosis. Reduced GIT bleeding. Lesser cost. Clear physiological benefits. – Maintain mucosal integrity. – Maintain mucosal structure. – Release gut trophic hormones. q q Less septic complications. Greater survival rate.
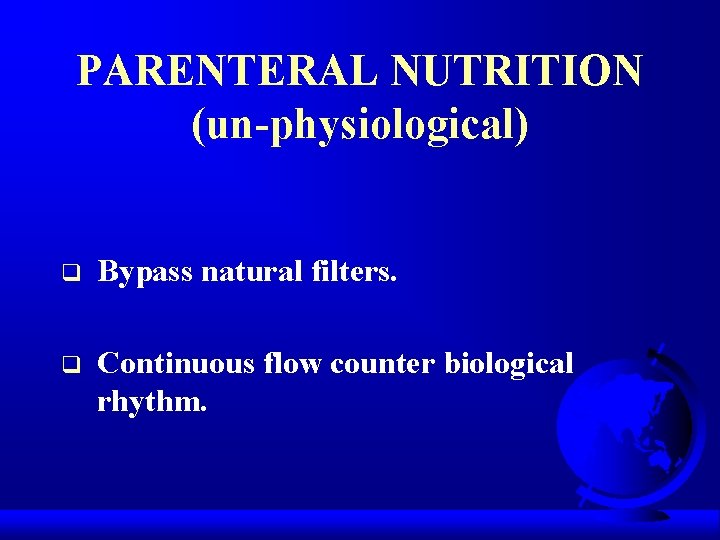
PARENTERAL NUTRITION (un-physiological) q Bypass natural filters. q Continuous flow counter biological rhythm.
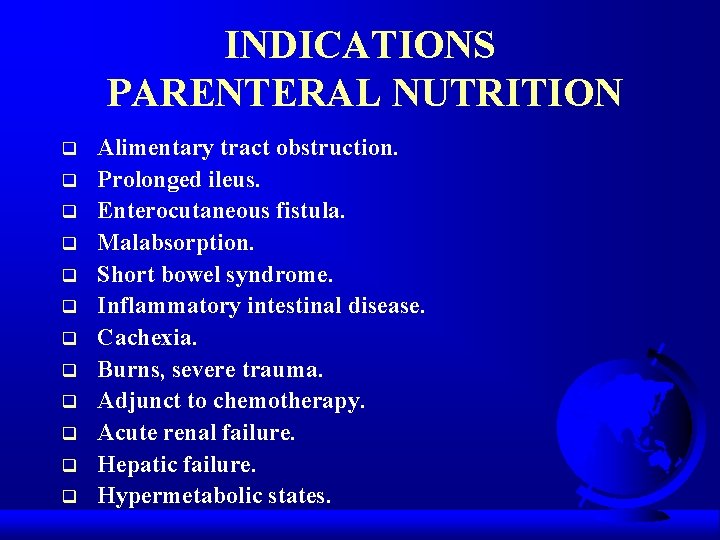
INDICATIONS PARENTERAL NUTRITION q q q Alimentary tract obstruction. Prolonged ileus. Enterocutaneous fistula. Malabsorption. Short bowel syndrome. Inflammatory intestinal disease. Cachexia. Burns, severe trauma. Adjunct to chemotherapy. Acute renal failure. Hepatic failure. Hypermetabolic states.
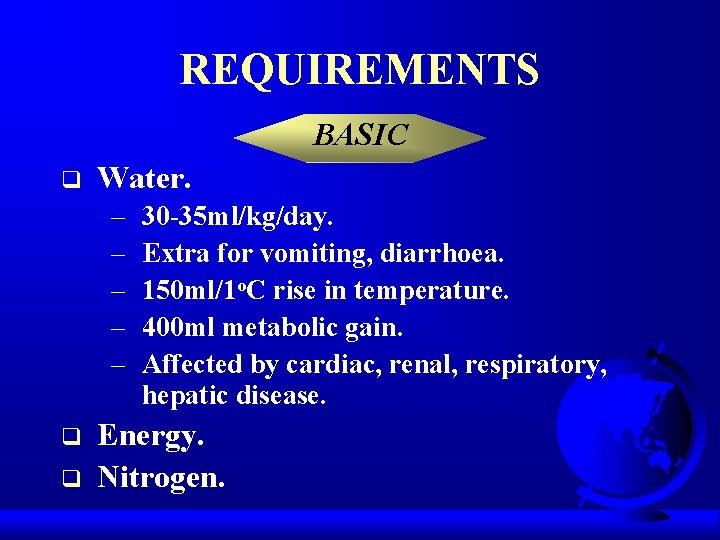
REQUIREMENTS BASIC q Water. – – – q q 30 -35 ml/kg/day. Extra for vomiting, diarrhoea. 150 ml/1 o. C rise in temperature. 400 ml metabolic gain. Affected by cardiac, renal, respiratory, hepatic disease. Energy. Nitrogen.

REQUIREMENTS ADDITIONAL q q Electrolytes. Vitamins. Trace-elements. Additives.
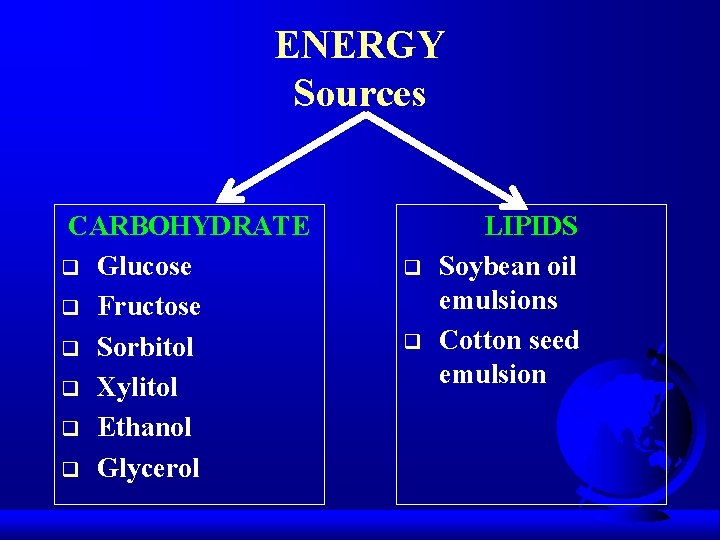
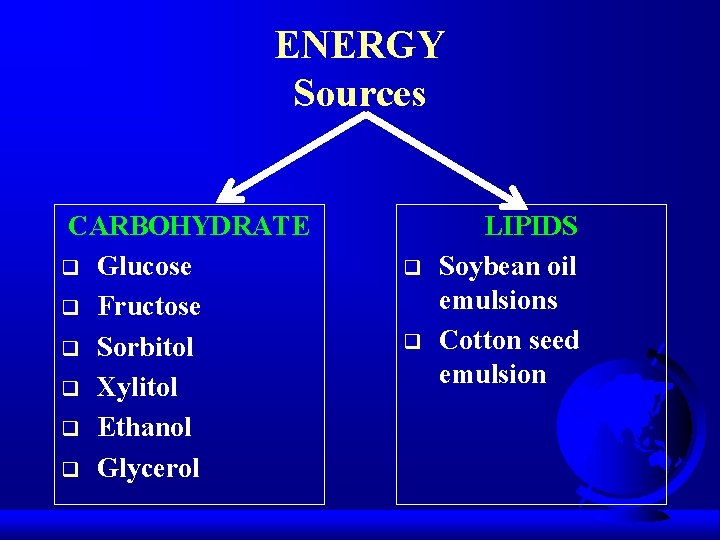
ENERGY Sources CARBOHYDRATE q Glucose q Fructose q Sorbitol q Xylitol q Ethanol q Glycerol q q LIPIDS Soybean oil emulsions Cotton seed emulsion
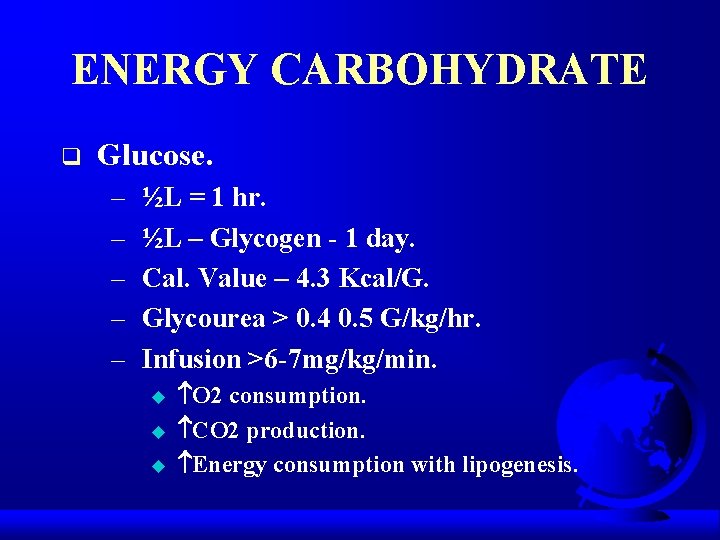
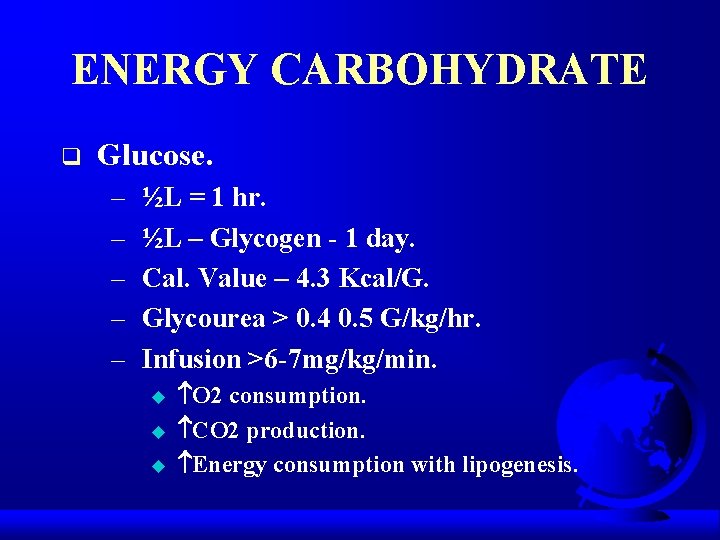
ENERGY CARBOHYDRATE q Glucose. – – – ½L = 1 hr. ½L – Glycogen - 1 day. Cal. Value – 4. 3 Kcal/G. Glycourea > 0. 4 0. 5 G/kg/hr. Infusion >6 -7 mg/kg/min. u u u O 2 consumption. CO 2 production. Energy consumption with lipogenesis.
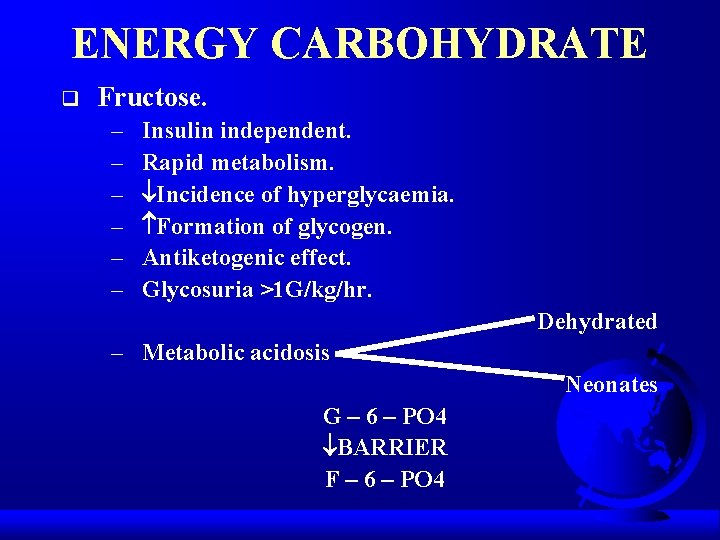
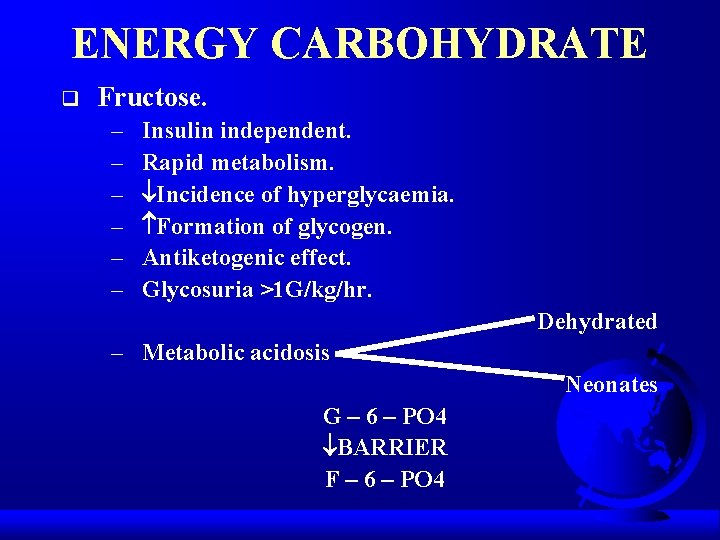
ENERGY CARBOHYDRATE q Fructose. – – – Insulin independent. Rapid metabolism. Incidence of hyperglycaemia. Formation of glycogen. Antiketogenic effect. Glycosuria >1 G/kg/hr. Dehydrated – Metabolic acidosis Neonates G – 6 – PO 4 BARRIER F – 6 – PO 4
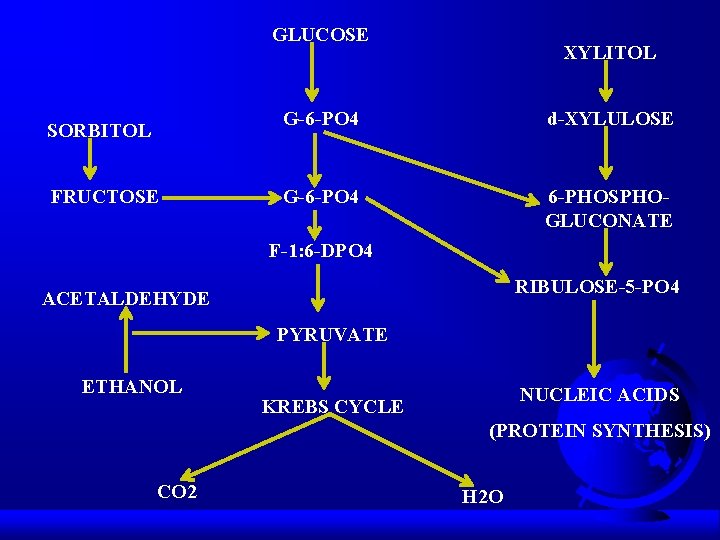
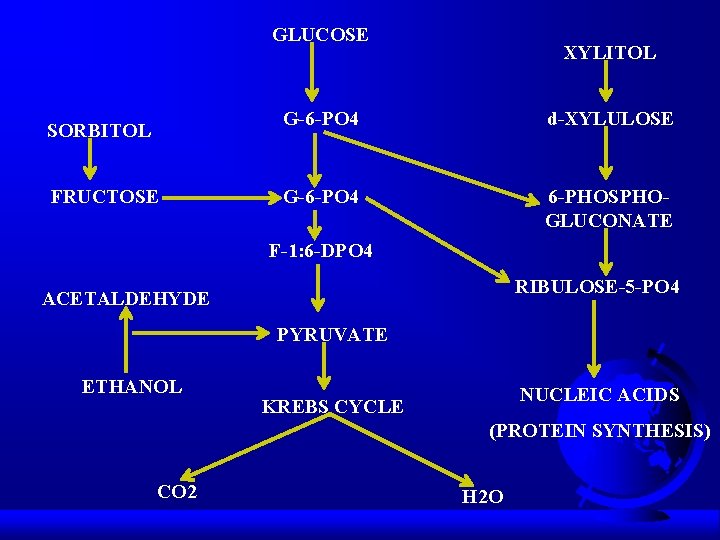
GLUCOSE SORBITOL FRUCTOSE XYLITOL G-6 -PO 4 d-XYLULOSE G-6 -PO 4 6 -PHOSPHOGLUCONATE F-1: 6 -DPO 4 RIBULOSE-5 -PO 4 ACETALDEHYDE PYRUVATE ETHANOL NUCLEIC ACIDS KREBS CYCLE (PROTEIN SYNTHESIS) CO 2 H 2 O
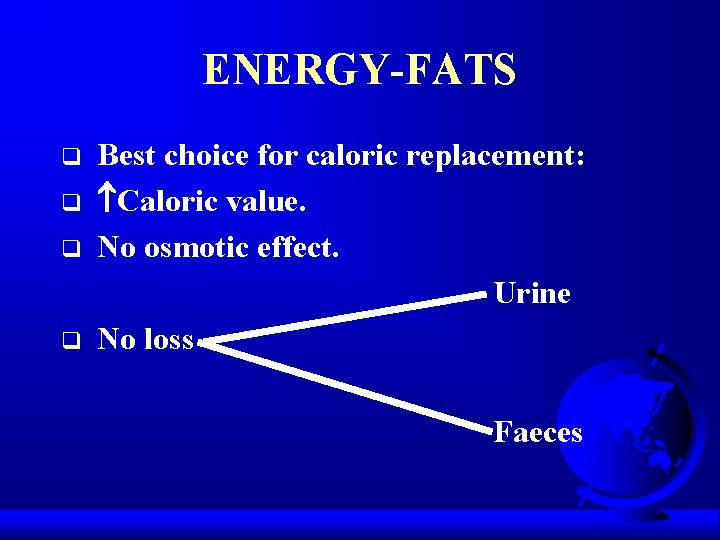
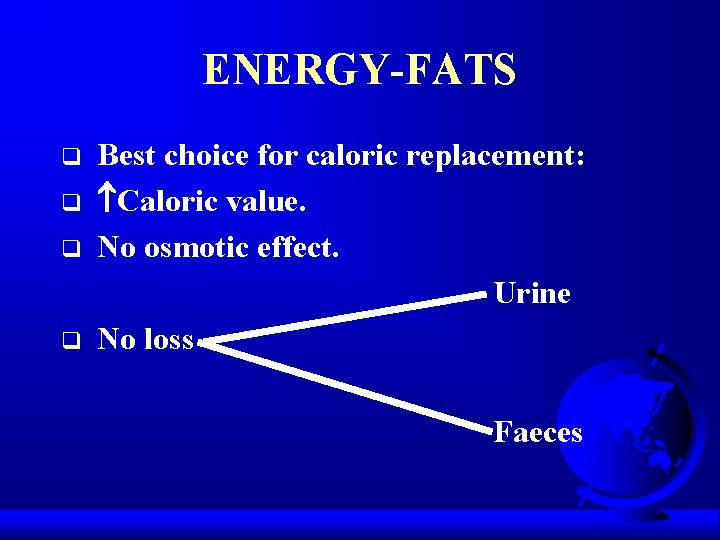
ENERGY-FATS q q Best choice for caloric replacement: Caloric value. No osmotic effect. Urine No loss Faeces
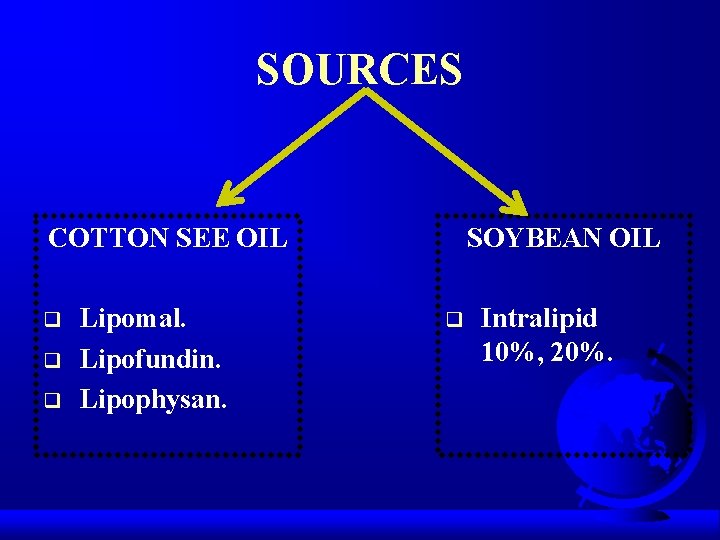
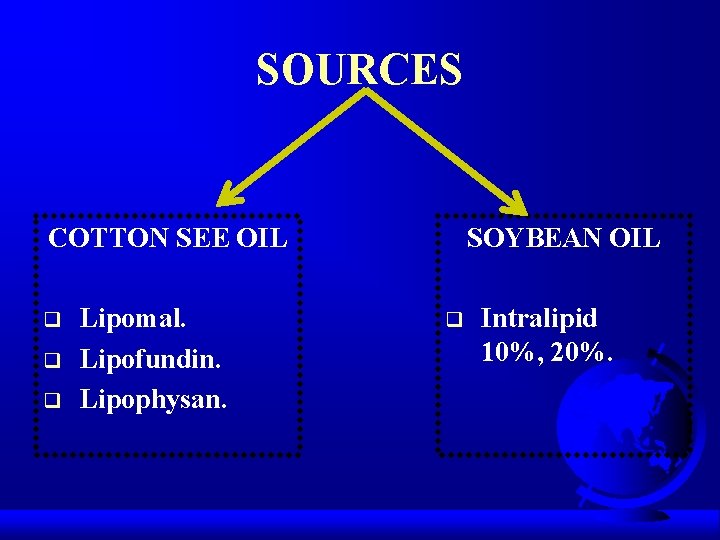
SOURCES COTTON SEE OIL q q q Lipomal. Lipofundin. Lipophysan. SOYBEAN OIL q Intralipid 10%, 20%.
IDEAL FAT EMULSION q Size <4. q Component of utmost purity. q Should be isotonic. q Should have no effect on BP or respiratory system. q Chronic toxicity – low.
INDICATIONS q Serious malabsorption (fistula, eneritis, colitis). q Cachexia. q Burns. q Prolonged unconsciousness. q High calorific deficiency.
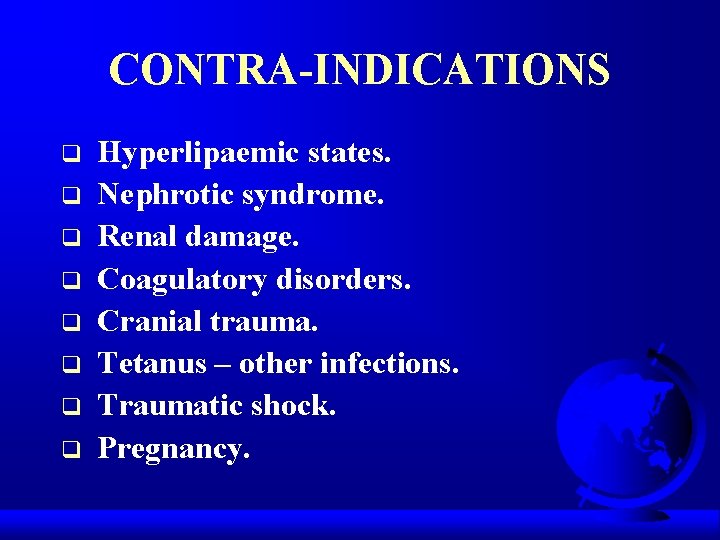
CONTRA-INDICATIONS q q q q Hyperlipaemic states. Nephrotic syndrome. Renal damage. Coagulatory disorders. Cranial trauma. Tetanus – other infections. Traumatic shock. Pregnancy.
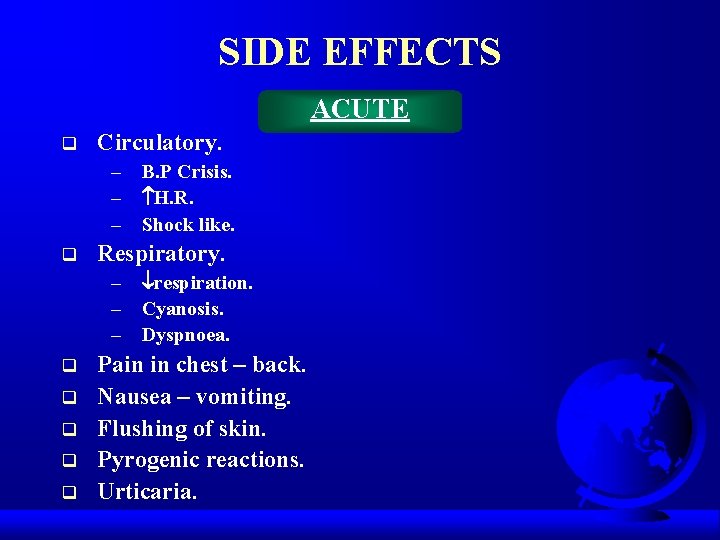
SIDE EFFECTS ACUTE q Circulatory. – B. P Crisis. – H. R. – Shock like. q Respiratory. – respiration. – Cyanosis. – Dyspnoea. q q q Pain in chest – back. Nausea – vomiting. Flushing of skin. Pyrogenic reactions. Urticaria.
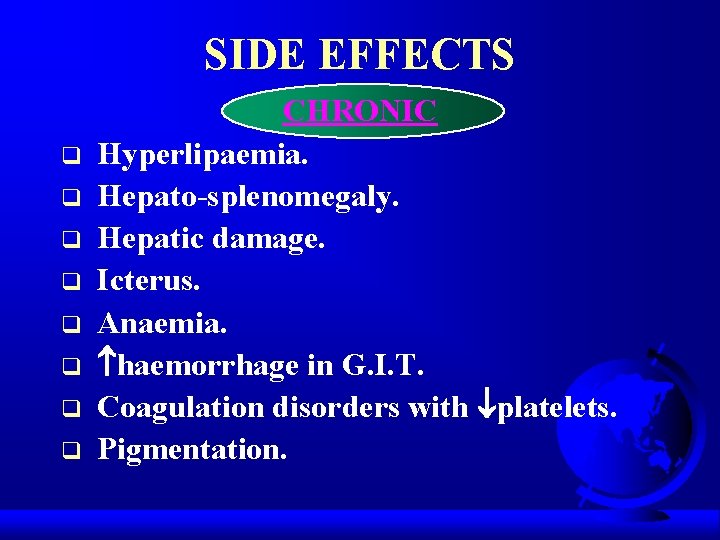
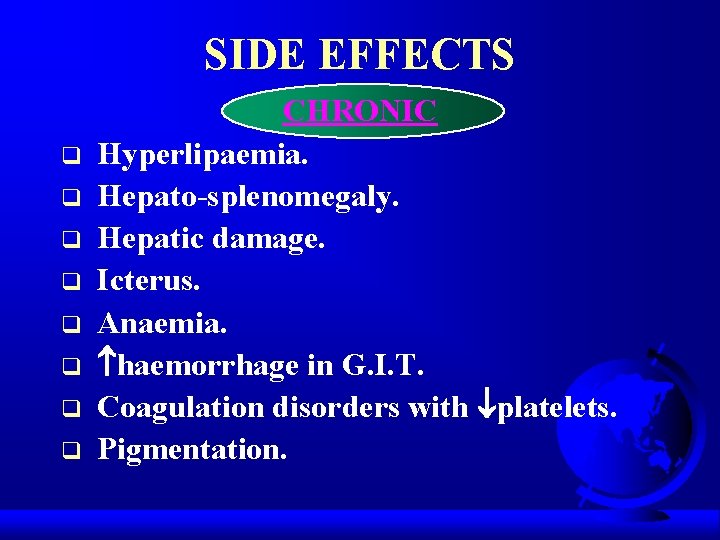
SIDE EFFECTS q q q q CHRONIC Hyperlipaemia. Hepato-splenomegaly. Hepatic damage. Icterus. Anaemia. haemorrhage in G. I. T. Coagulation disorders with platelets. Pigmentation.
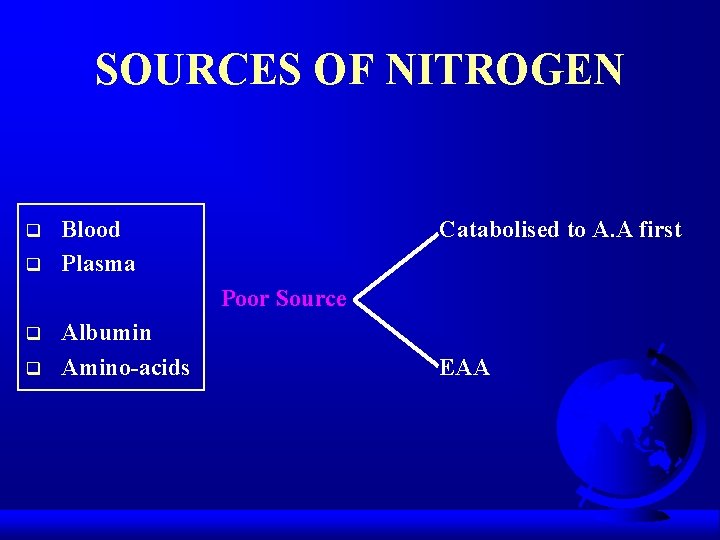
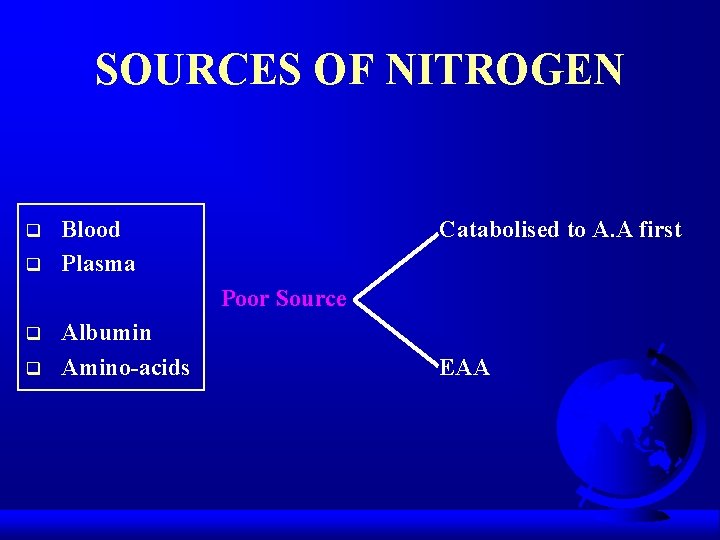
SOURCES OF NITROGEN q q Blood Plasma Catabolised to A. A first Poor Source q q Albumin Amino-acids EAA
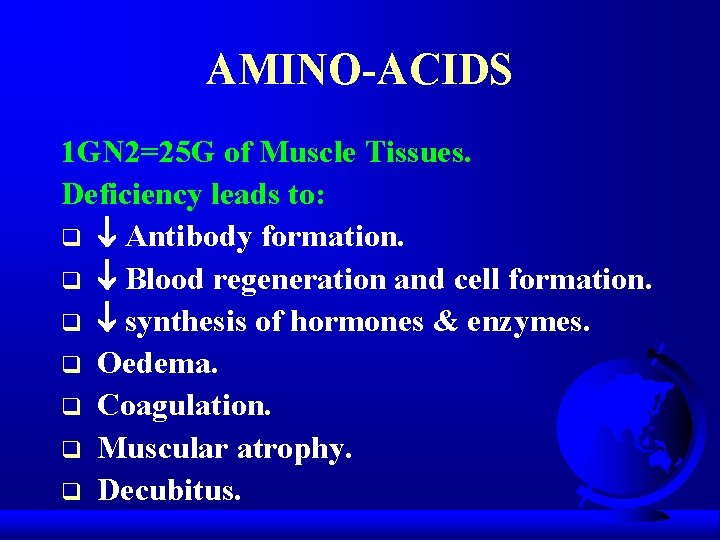
AMINO-ACIDS 1 GN 2=25 G of Muscle Tissues. Deficiency leads to: q Antibody formation. q Blood regeneration and cell formation. q synthesis of hormones & enzymes. q Oedema. q Coagulation. q Muscular atrophy. q Decubitus.
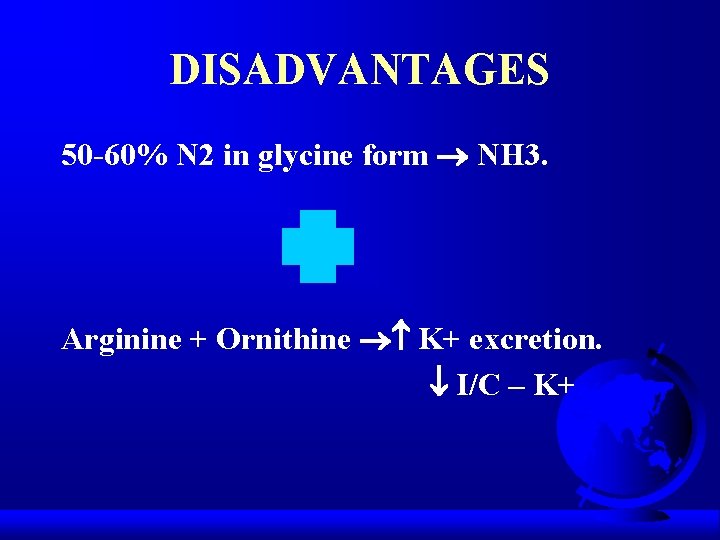
DISADVANTAGES 50 -60% N 2 in glycine form NH 3. Arginine + Ornithine K+ excretion. I/C – K+
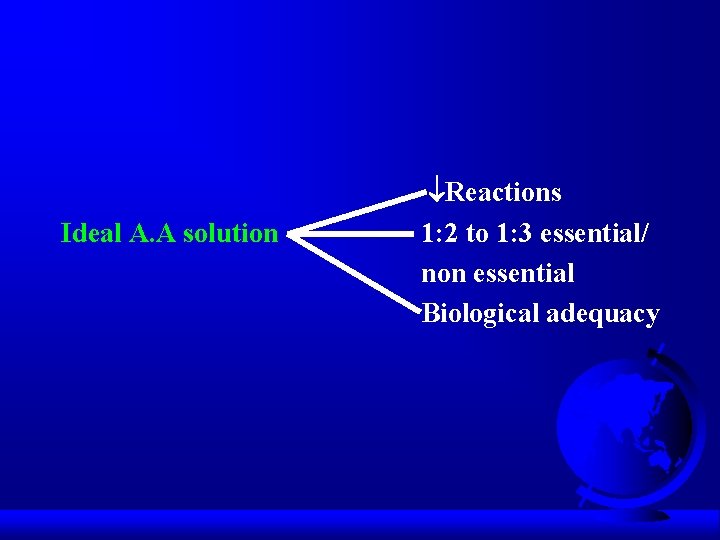
Ideal A. A solution Reactions 1: 2 to 1: 3 essential/ non essential Biological adequacy
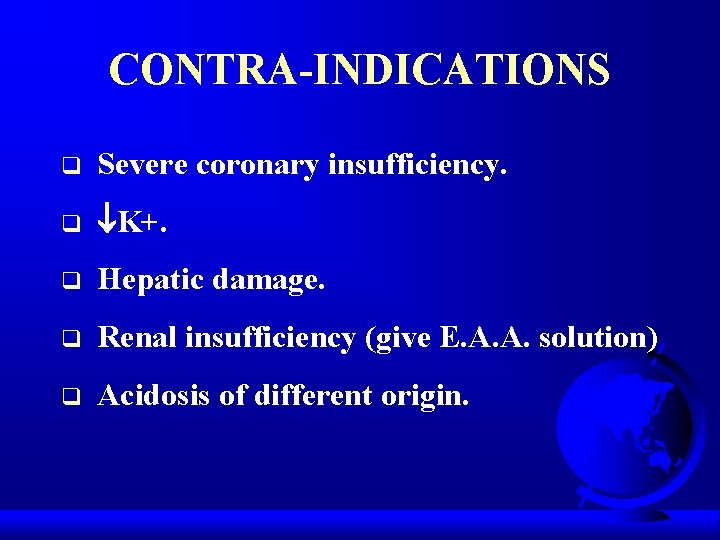
CONTRA-INDICATIONS q Severe coronary insufficiency. q K+. q Hepatic damage. q Renal insufficiency (give E. A. A. solution) q Acidosis of different origin.
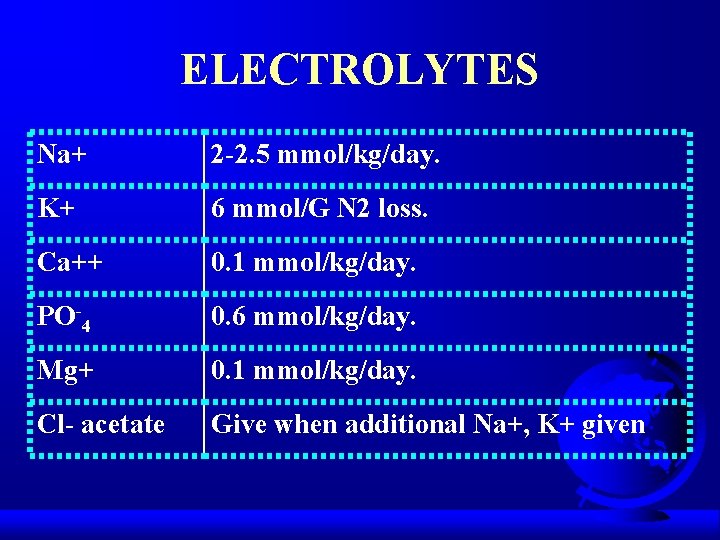
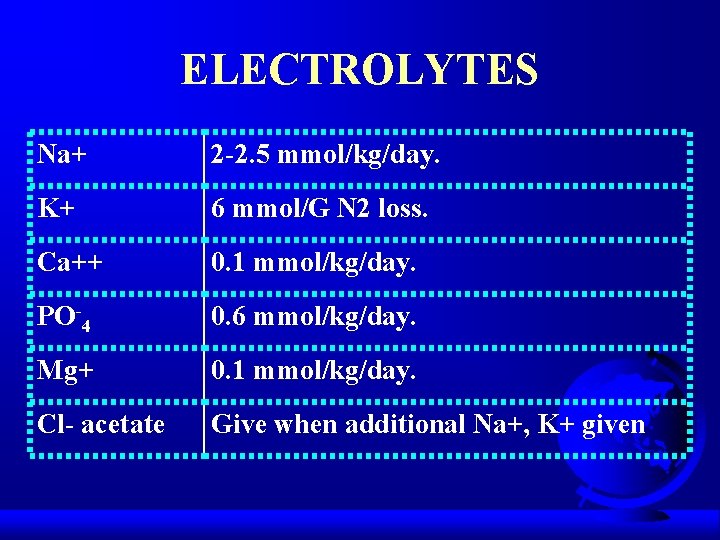
ELECTROLYTES Na+ 2 -2. 5 mmol/kg/day. K+ 6 mmol/G N 2 loss. Ca++ 0. 1 mmol/kg/day. PO-4 0. 6 mmol/kg/day. Mg+ 0. 1 mmol/kg/day. Cl- acetate Give when additional Na+, K+ given
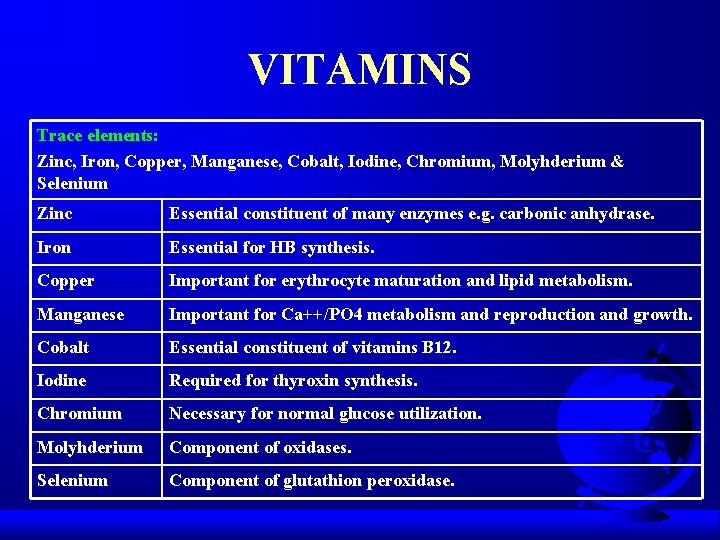
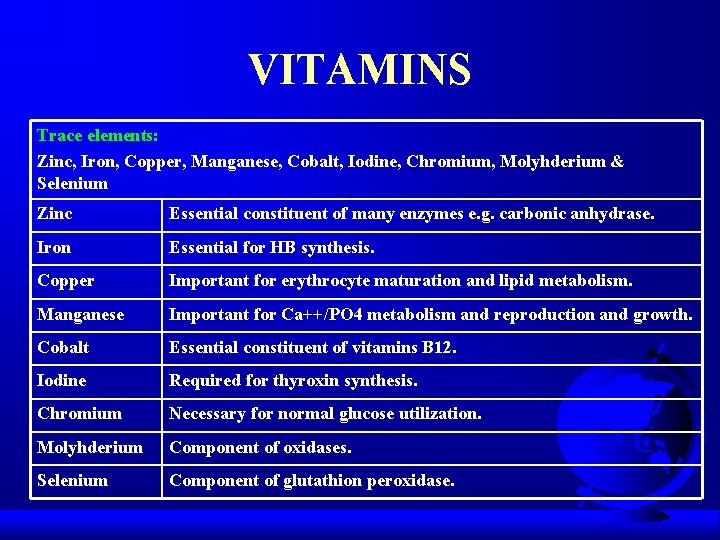
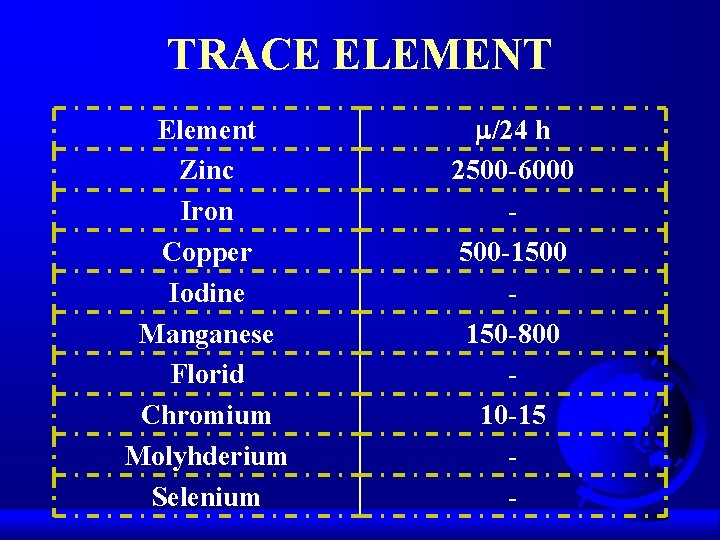
VITAMINS Trace elements: Zinc, Iron, Copper, Manganese, Cobalt, Iodine, Chromium, Molyhderium & Selenium Zinc Essential constituent of many enzymes e. g. carbonic anhydrase. Iron Essential for HB synthesis. Copper Important for erythrocyte maturation and lipid metabolism. Manganese Important for Ca++/PO 4 metabolism and reproduction and growth. Cobalt Essential constituent of vitamins B 12. Iodine Required for thyroxin synthesis. Chromium Necessary for normal glucose utilization. Molyhderium Component of oxidases. Selenium Component of glutathion peroxidase.
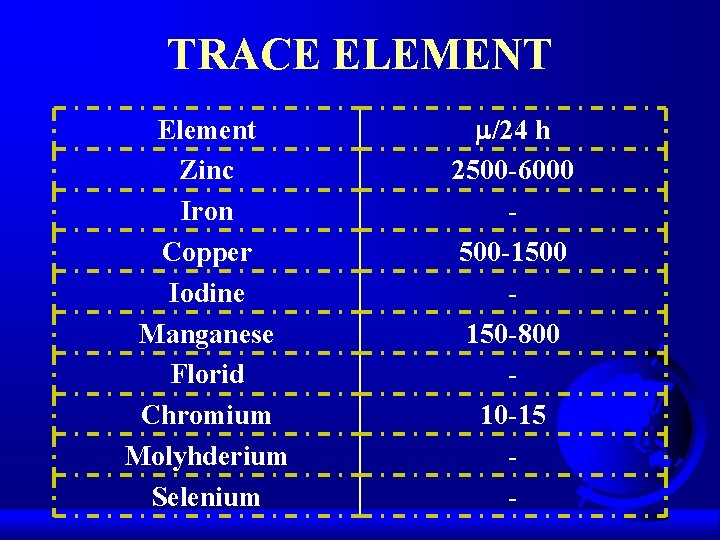
TRACE ELEMENT Element Zinc Iron Copper Iodine Manganese Florid Chromium Molyhderium Selenium /24 h 2500 -6000 500 -1500 150 -800 10 -15 -

ADDITIVES q Insulin. q Heparin. q Anabolic steroids.
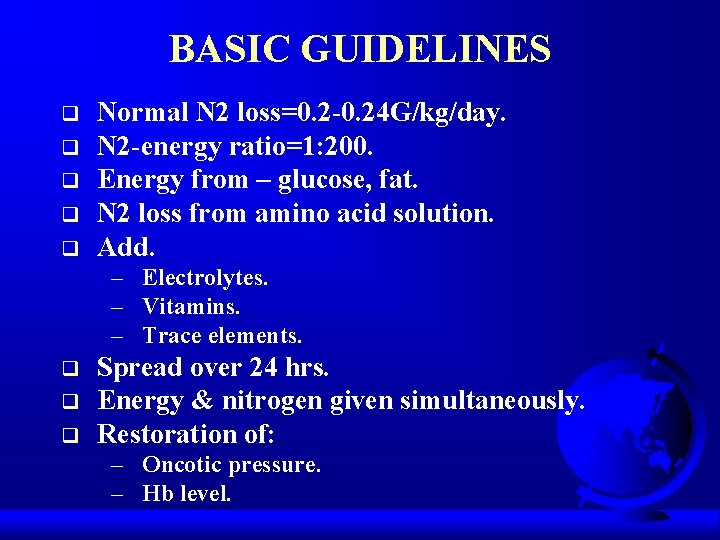
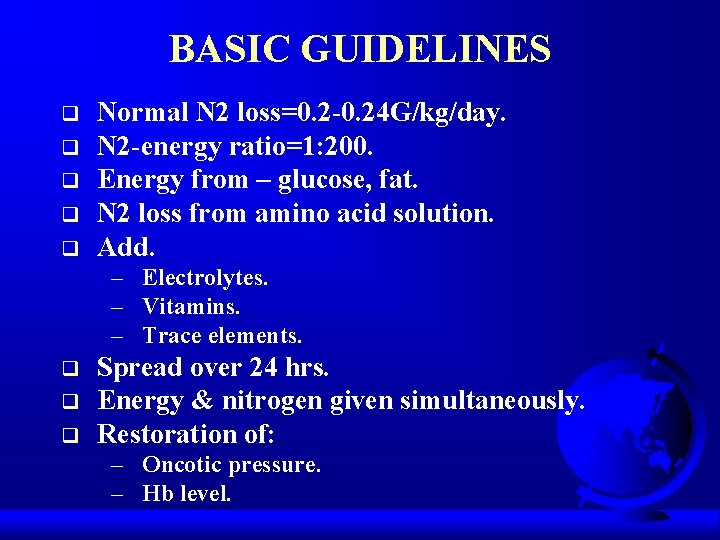
BASIC GUIDELINES q q q Normal N 2 loss=0. 2 -0. 24 G/kg/day. N 2 -energy ratio=1: 200. Energy from – glucose, fat. N 2 loss from amino acid solution. Add. – Electrolytes. – Vitamins. – Trace elements. q q q Spread over 24 hrs. Energy & nitrogen given simultaneously. Restoration of: – Oncotic pressure. – Hb level.

MONITORING q Biochemical. q Physiological. q Haematological. q Mechanical. q Bacteriological. q Radiological.
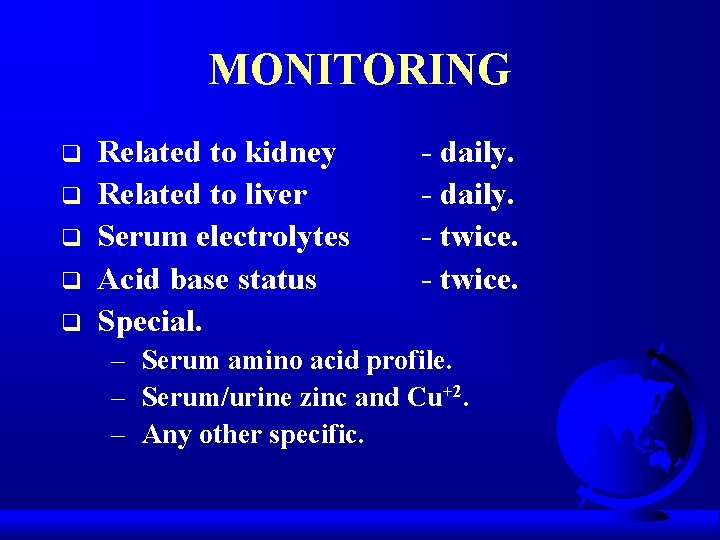
MONITORING q q q Related to kidney Related to liver Serum electrolytes Acid base status Special. - daily. - twice. – Serum amino acid profile. – Serum/urine zinc and Cu+2. – Any other specific.
MONITORING PHYSIOLOGICAL q Haemodynamics. q C. V. P. q Weight. q Fluid balance.
MONITORING HAEMATOLOGICAL q q q Haemodynamics. While cell count. Differential count. Serum protein. Folate level.
MONITORING MECHANICAL INSEPCTION OF: q I/V lines. q Flow rate. q Catheter insertion point. q Infusion pumps. q Monitoring equipment.
MONITORING BACTERIOLOGICAL q Blood culture – weekly. q Viral agglutination titres.
MONITORING RADIOLOGICAL X-RAY CHEST Lung Fields CVP Catheter
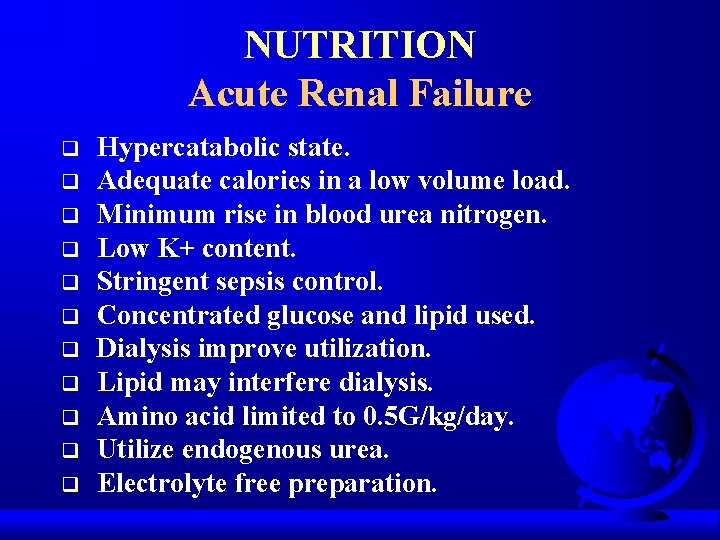
NUTRITION Acute Renal Failure q q q Hypercatabolic state. Adequate calories in a low volume load. Minimum rise in blood urea nitrogen. Low K+ content. Stringent sepsis control. Concentrated glucose and lipid used. Dialysis improve utilization. Lipid may interfere dialysis. Amino acid limited to 0. 5 G/kg/day. Utilize endogenous urea. Electrolyte free preparation.
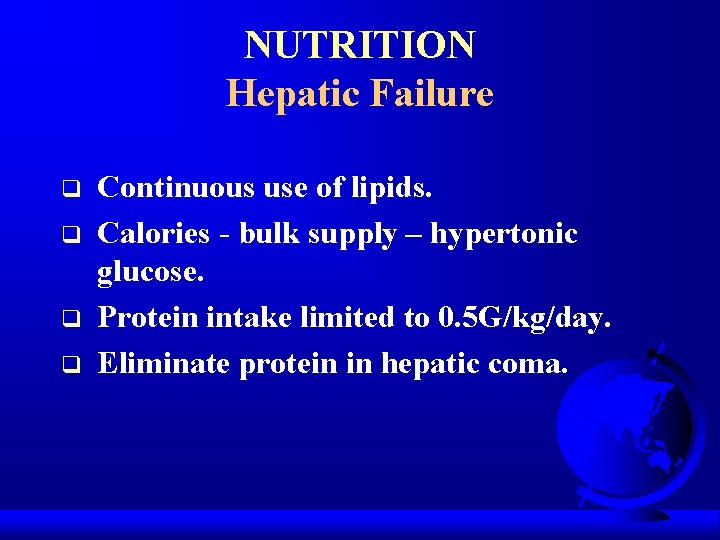
NUTRITION Hepatic Failure q q Continuous use of lipids. Calories - bulk supply – hypertonic glucose. Protein intake limited to 0. 5 G/kg/day. Eliminate protein in hepatic coma.
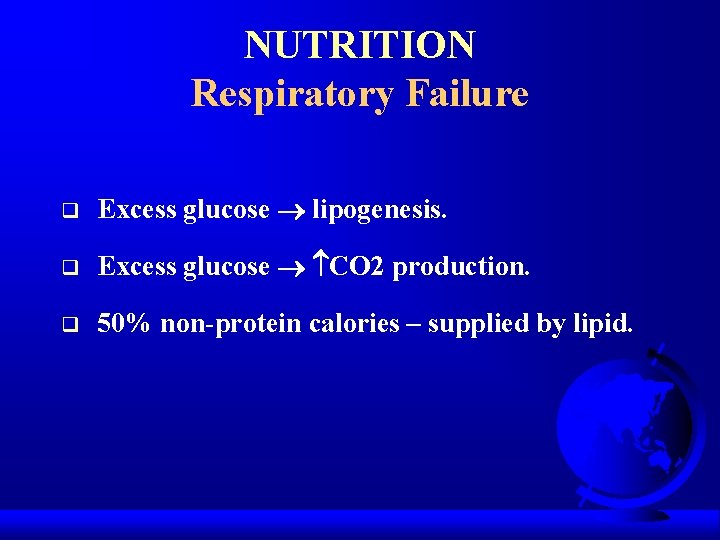
NUTRITION Respiratory Failure q Excess glucose lipogenesis. q Excess glucose CO 2 production. q 50% non-protein calories – supplied by lipid.
STRESS ON 1. 2. Specialised Nutrition Support In Critically Ill Patients. Glutamine and Acute Illness. PRESENT & FUTURE

SIGNIFICANCE OF GIT IN CRITICALLY ILL
ANATOMY & HISTORY OF GUT
FUNCTIONS Barrier Transport Endocrine
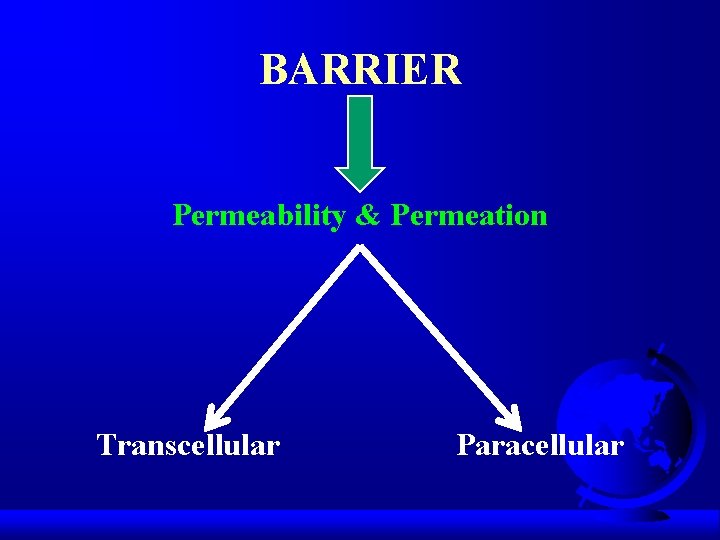
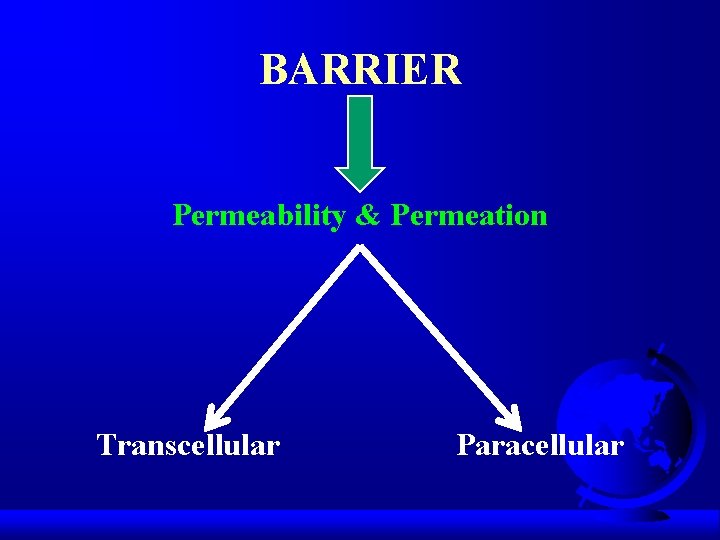
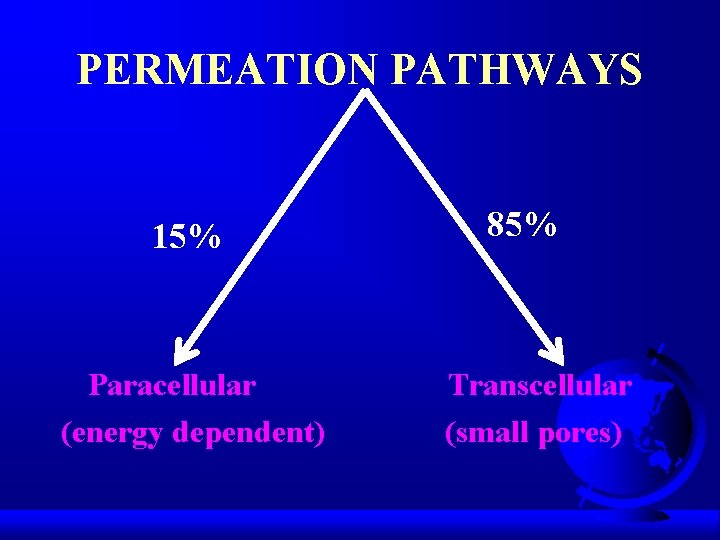
BARRIER Permeability & Permeation Transcellular Paracellular
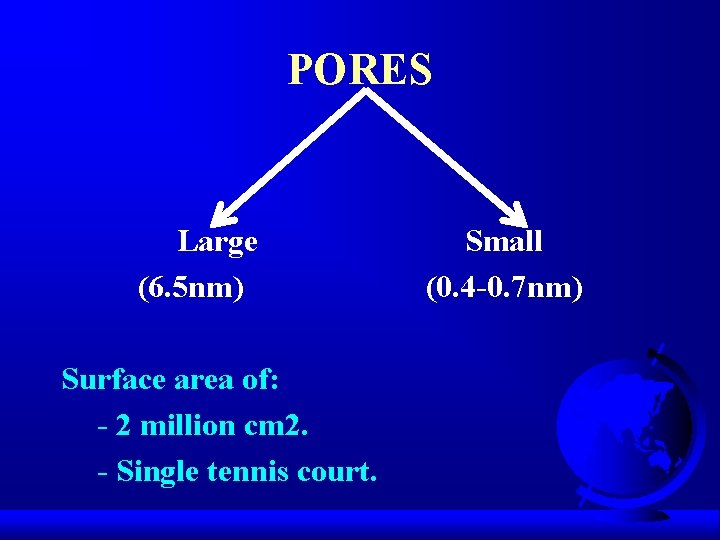
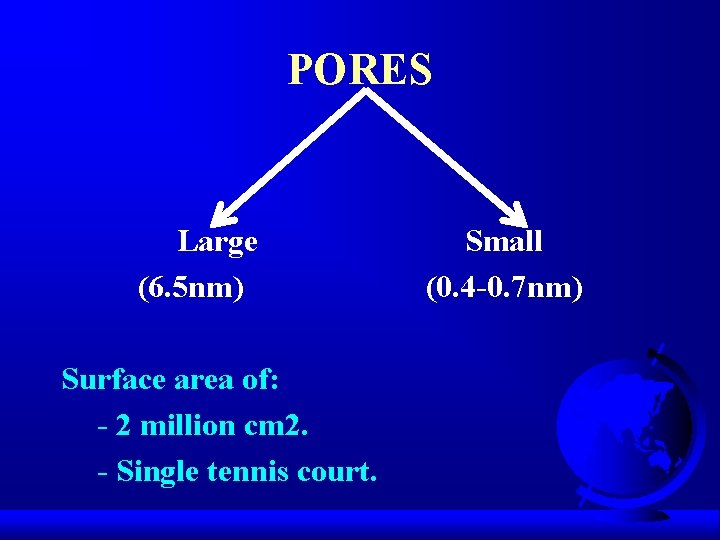
PORES Large (6. 5 nm) Surface area of: - 2 million cm 2. - Single tennis court. Small (0. 4 -0. 7 nm)
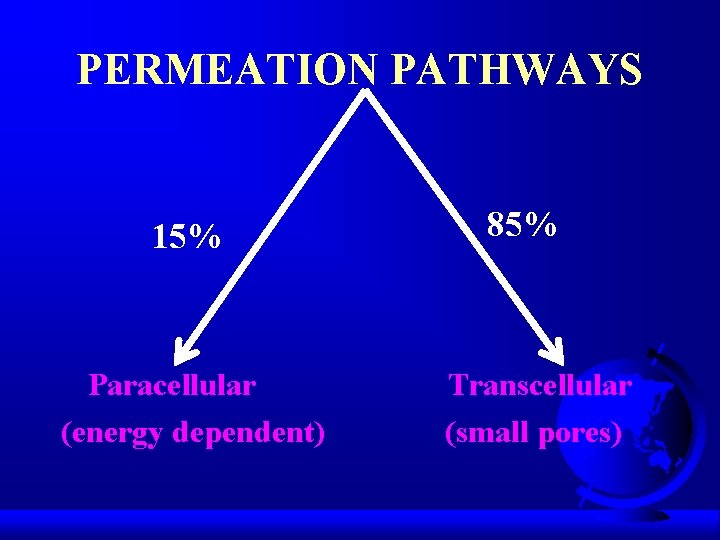
PERMEATION PATHWAYS 15% Paracellular (energy dependent) 85% Transcellular (small pores)
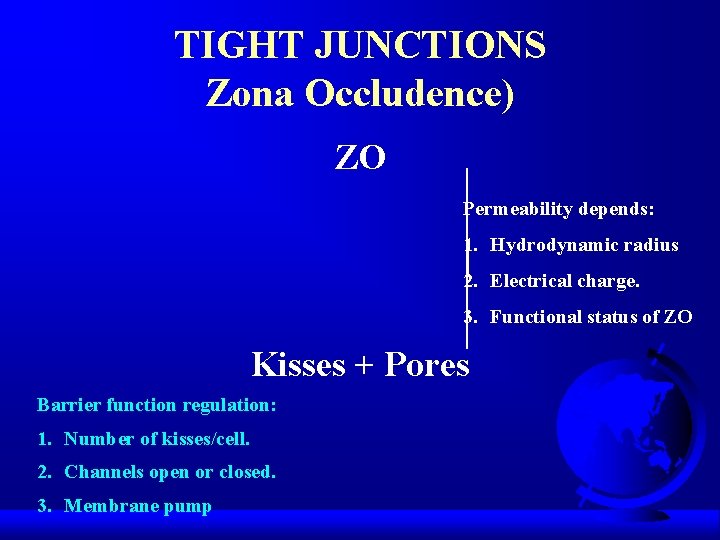
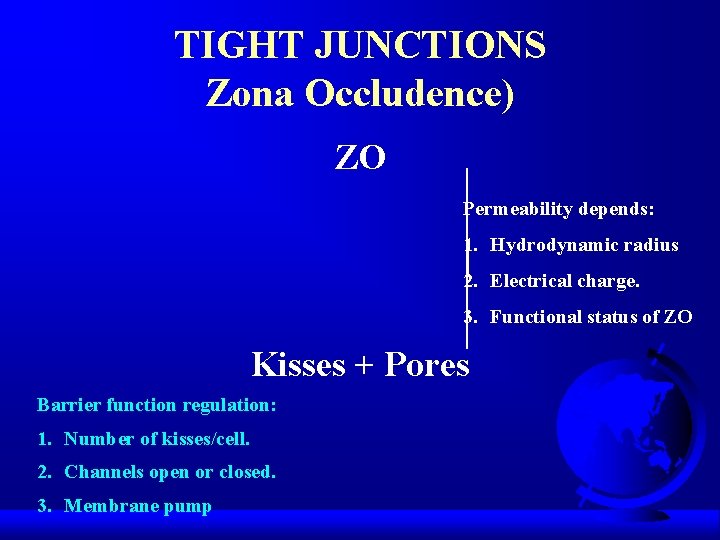
TIGHT JUNCTIONS Zona Occludence) ZO Permeability depends: 1. Hydrodynamic radius 2. Electrical charge. 3. Functional status of ZO Kisses + Pores Barrier function regulation: 1. Number of kisses/cell. 2. Channels open or closed. 3. Membrane pump
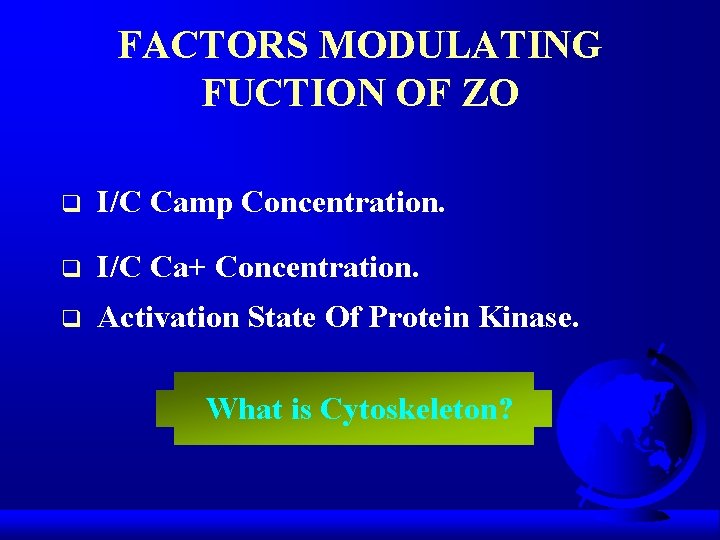
FACTORS MODULATING FUCTION OF ZO q I/C Camp Concentration. q I/C Ca+ Concentration. q Activation State Of Protein Kinase. What is Cytoskeleton?
TRANSLOCATION DEFINITION

CAUSES q q q q Non Occlusive Intestinal Gangrene. Neutropenia. Colon Cancer. Penumatosis Intestinals. Necrtising Enterocolitis. Ionizing Radiation. Cytotoxic Drugs.
CAUSES q q q q Cytokine Release Syndrome. Crohns Disease. Ulcerative Colitis. Haemorrhagic Shock. Severe Trauma Burn Injury. Leukaemia.
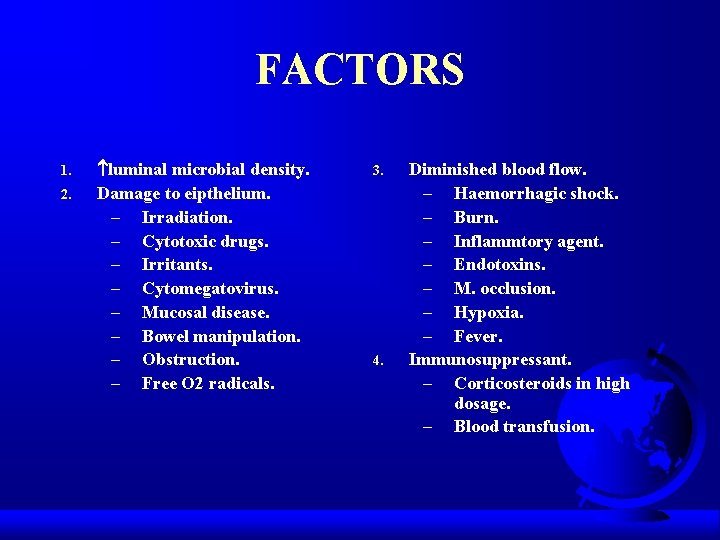
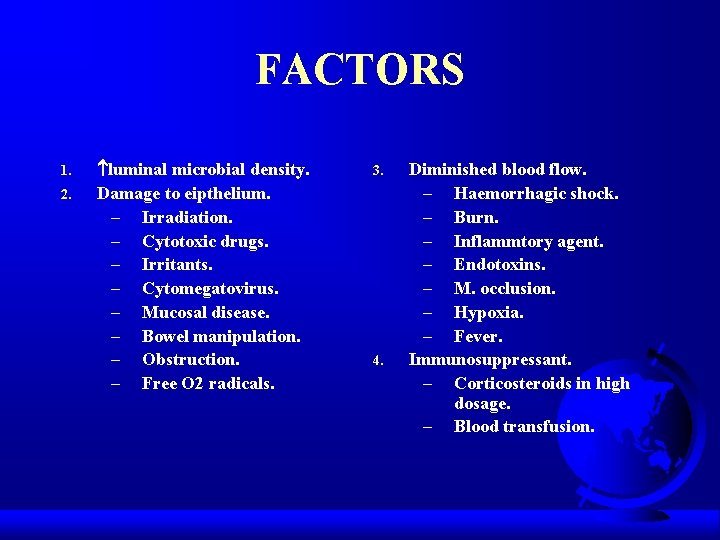
FACTORS 1. 2. luminal microbial density. Damage to eipthelium. – Irradiation. – Cytotoxic drugs. – Irritants. – Cytomegatovirus. – Mucosal disease. – Bowel manipulation. – Obstruction. – Free O 2 radicals. 3. 4. Diminished blood flow. – Haemorrhagic shock. – Burn. – Inflammtory agent. – Endotoxins. – M. occlusion. – Hypoxia. – Fever. Immunosuppressant. – Corticosteroids in high dosage. – Blood transfusion.
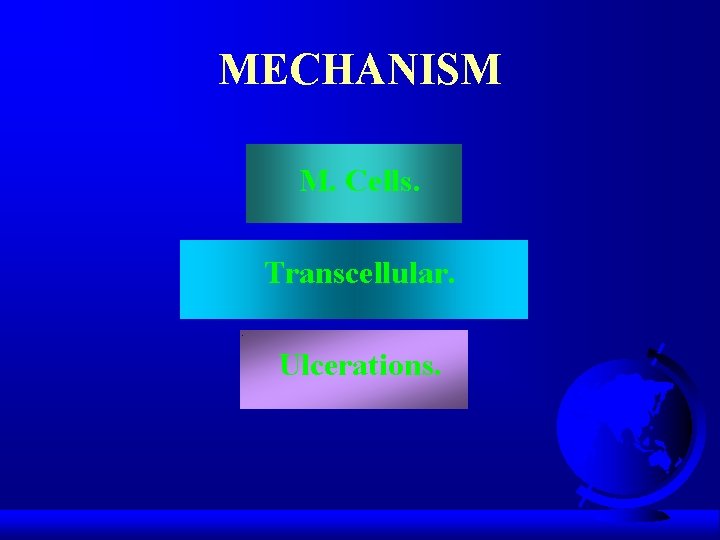
MECHANISM M. Cells. Transcellular. Ulcerations.
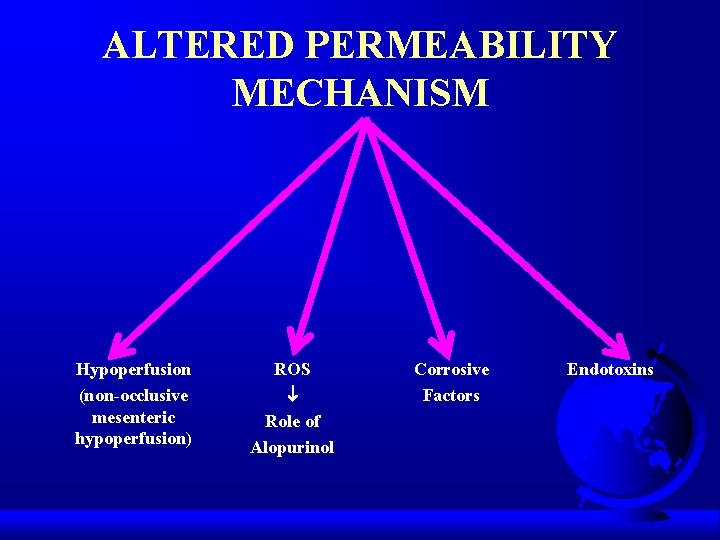
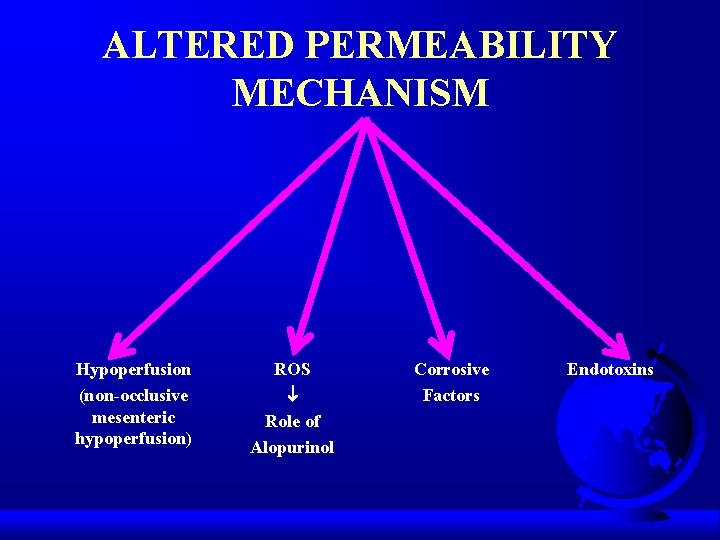
ALTERED PERMEABILITY MECHANISM Hypoperfusion (non-occlusive mesenteric hypoperfusion) ROS Role of Alopurinol Corrosive Factors Endotoxins
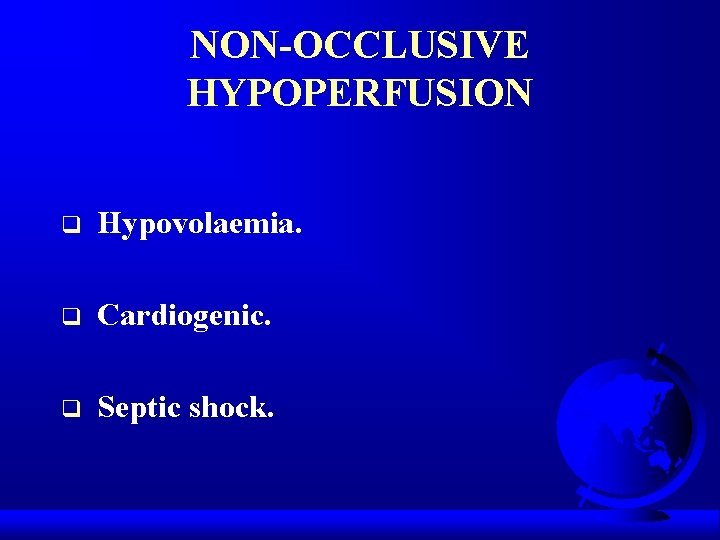
NON-OCCLUSIVE HYPOPERFUSION q Hypovolaemia. q Cardiogenic. q Septic shock.
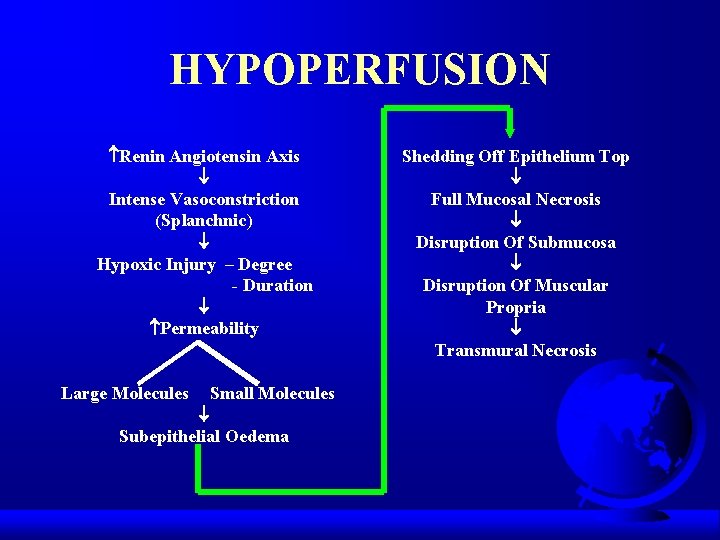
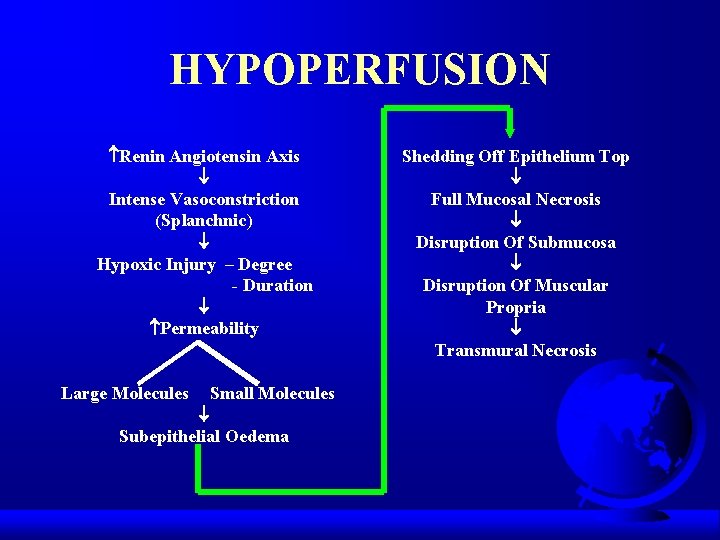
HYPOPERFUSION Renin Angiotensin Axis Intense Vasoconstriction (Splanchnic) Hypoxic Injury – Degree - Duration Permeability Large Molecules Small Molecules Subepithelial Oedema Shedding Off Epithelium Top Full Mucosal Necrosis Disruption Of Submucosa Disruption Of Muscular Propria Transmural Necrosis
ROS Role of Allopurinal

CORROSIVE FACTORS q q q Hydrochloric acid. Bile salts. Bacterial toxins. Proteases. Digestive enzymes.
ENDOTOXINS q Ischaemia. q Direct injury. q metabolic demand of GUT. q Alteration of micro-circulation.
MEASUREMENT OF GUT PERMEABILITY q Isotope tests. q PEG tests. q Dual sacharide tests. – Lactulose/Rhamnose. – Lactulose/Mannitol.

NON MUCOSAL FACTORS q Gastric Emptying. q Intestinal Transit. q Dilution By Secretion. q Surface Area Available. q Altered Renal Clearance.
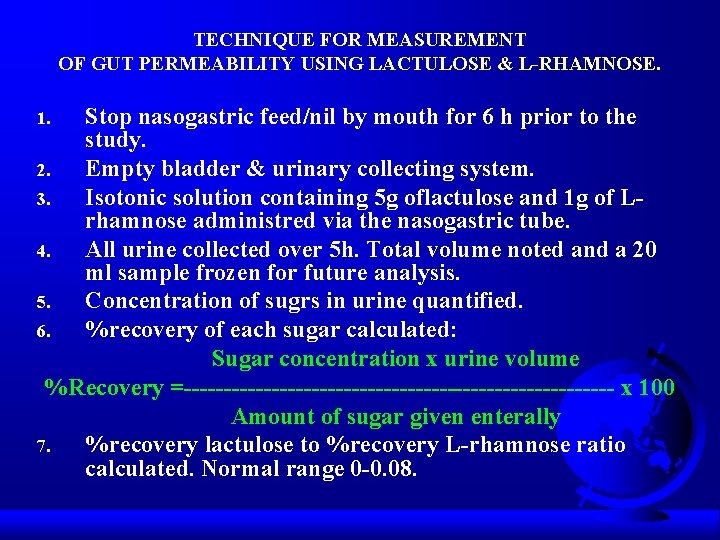
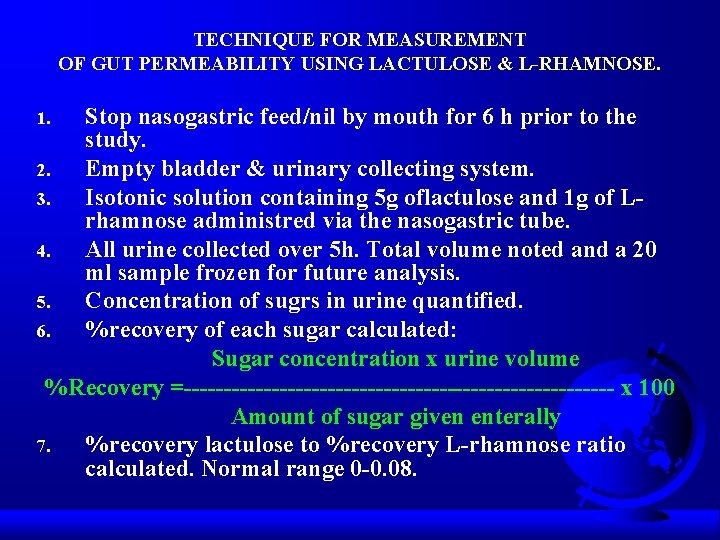
TECHNIQUE FOR MEASUREMENT OF GUT PERMEABILITY USING LACTULOSE & L-RHAMNOSE. Stop nasogastric feed/nil by mouth for 6 h prior to the study. 2. Empty bladder & urinary collecting system. 3. Isotonic solution containing 5 g oflactulose and 1 g of Lrhamnose administred via the nasogastric tube. 4. All urine collected over 5 h. Total volume noted and a 20 ml sample frozen for future analysis. 5. Concentration of sugrs in urine quantified. 6. %recovery of each sugar calculated: Sugar concentration x urine volume %Recovery =--------------------------- x 100 Amount of sugar given enterally 7. %recovery lactulose to %recovery L-rhamnose ratio calculated. Normal range 0 -0. 08. 1.
IMMUNONUTRTION (Nutritional Paharmacology) Why Name Immunonutrition? q q Lipids -3, -6 Aminoacids – Arginine – Glutamine q q Ribonucleic acid Vitamins, E, C and A
LIPIDS q q q q q Production of free radicals. Inflammatory response. Ulcer formation. Hypersensitivity response. Altered renal vascular flow. Uterine contraction. Incidence of atherosclerosis. Incidence of heart attacks. Bleeding tendency. Haemorrhagic strokes.
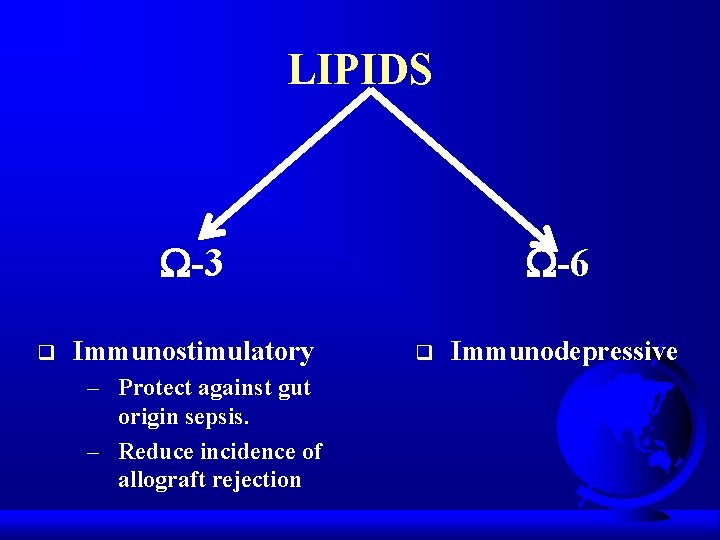
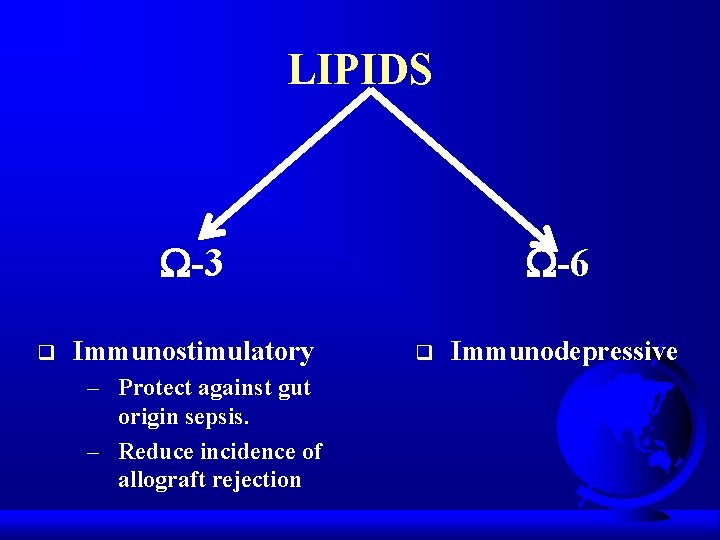
LIPIDS -3 q Immunostimulatory – Protect against gut origin sepsis. – Reduce incidence of allograft rejection -6 q Immunodepressive
VITAMINS, E, C, A q Control lipid peroxidation. q Regulate RO intermediates (macrophages).
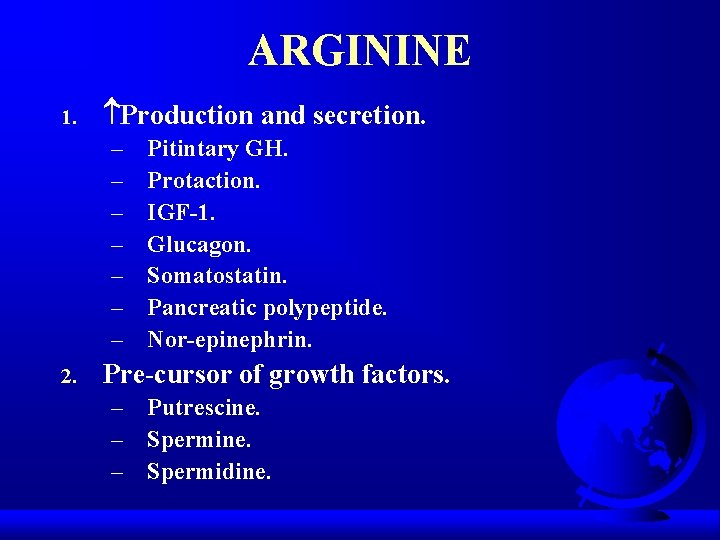
ARGININE 1. Production and secretion. – – – – 2. Pitintary GH. Protaction. IGF-1. Glucagon. Somatostatin. Pancreatic polypeptide. Nor-epinephrin. Pre-cursor of growth factors. – Putrescine. – Spermidine.
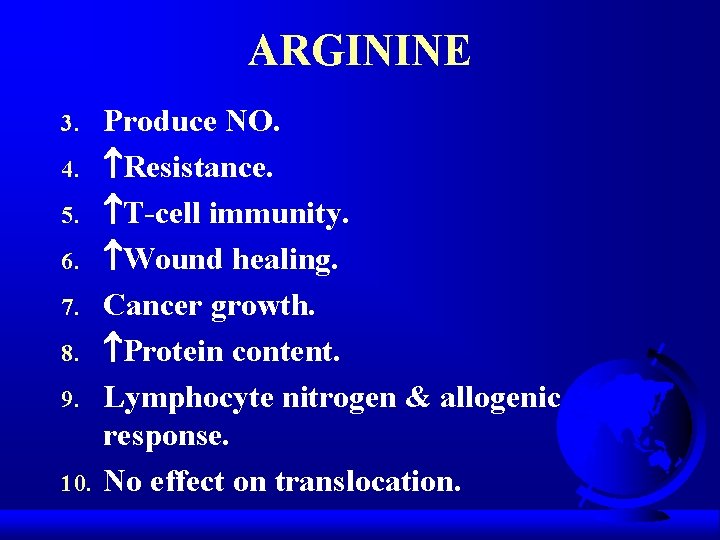
ARGININE 3. 4. 5. 6. 7. 8. 9. 10. Produce NO. Resistance. T-cell immunity. Wound healing. Cancer growth. Protein content. Lymphocyte nitrogen & allogenic response. No effect on translocation.
GLUTANINE q Barrier Function. q T-cell Function. q Neutrophil Function. q Kills Translocated Bacteria. q Hospital Stay.
NUCLEOTIDES q Resistance. q Immune response.
EFFECT OF CRITICAL ILLNESS ON GIT q q q Starvation & Bowel rest. Metabolic stress. Entral/Parenteral nutrition. Sepsis. Shock.
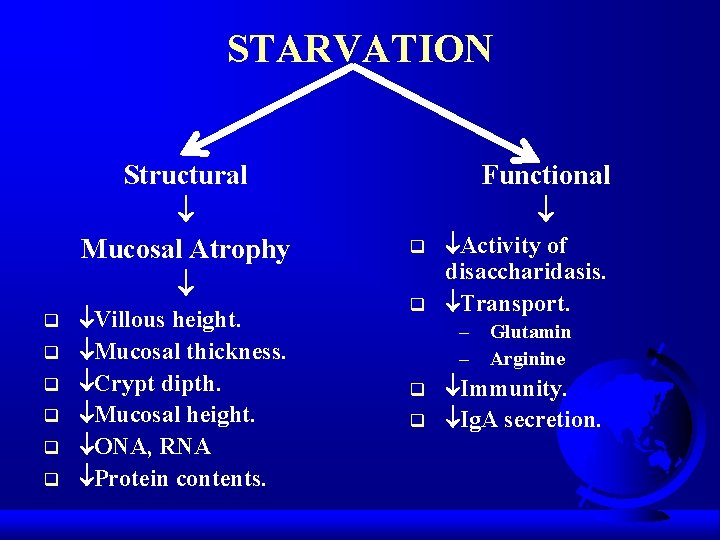
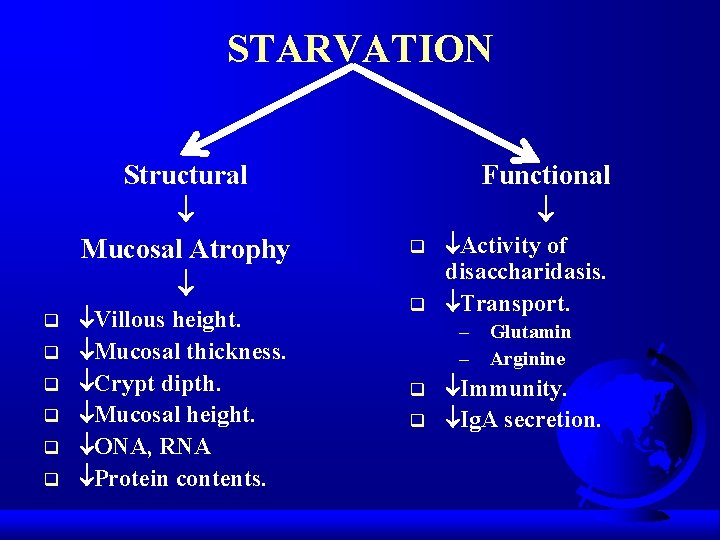
STARVATION Structural Mucosal Atrophy q q q Villous height. Mucosal thickness. Crypt dipth. Mucosal height. ONA, RNA Protein contents. Functional q q Activity of disaccharidasis. Transport. – Glutamin – Arginine q q Immunity. Ig. A secretion.
GIT IMMUNOLOGIC DEFENCE q q Ig. A. Lymphocyte macrophages & neutrophils. Lymph nodes. Kupffer cells in liver.
BOWEL REST q q q G. I. Mass. Small bowel mucosal weight. DNA content. Protein content. Villous height. Enzyme activity. Even if nitrogen balance is maintained & on TPN
PRESENCE OF LUMINAL NUTRIENTS NECESSARY FOR NORMAL GUT GROWTH & FUNCTION
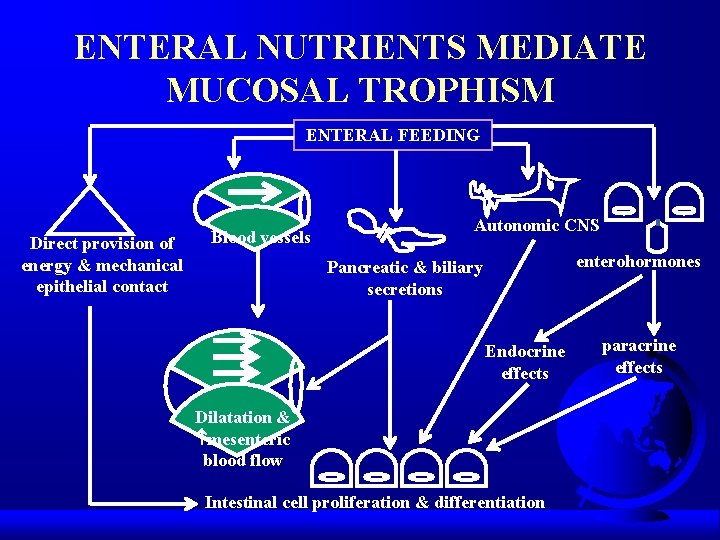
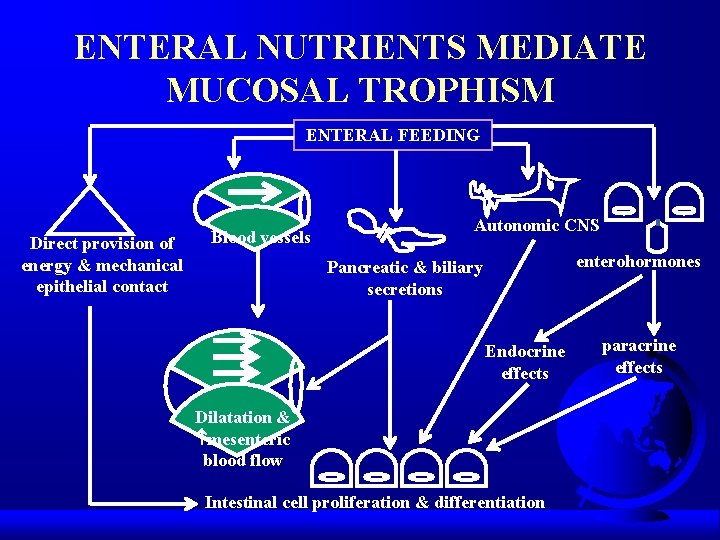
ENTERAL NUTRIENTS MEDIATE MUCOSAL TROPHISM ENTERAL FEEDING Direct provision of energy & mechanical epithelial contact Blood vessels Autonomic CNS enterohormones Pancreatic & biliary secretions Endocrine effects Dilatation & mesenteric blood flow Intestinal cell proliferation & differentiation paracrine effects
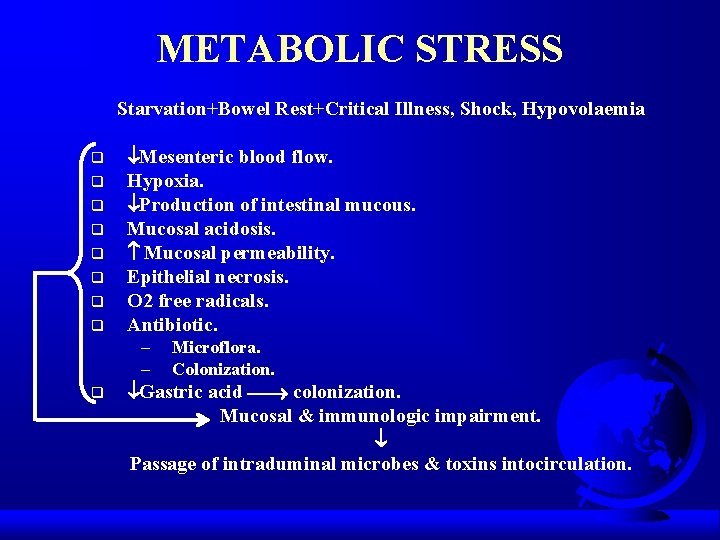
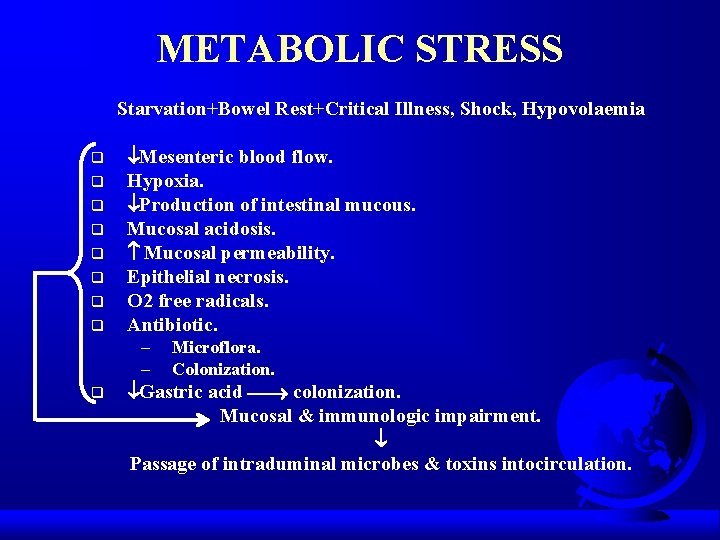
METABOLIC STRESS Starvation+Bowel Rest+Critical Illness, Shock, Hypovolaemia q q q q Mesenteric blood flow. Hypoxia. Production of intestinal mucous. Mucosal acidosis. Mucosal permeability. Epithelial necrosis. O 2 free radicals. Antibiotic. – – q Microflora. Colonization. Gastric acid colonization. Mucosal & immunologic impairment. Passage of intraduminal microbes & toxins intocirculation.
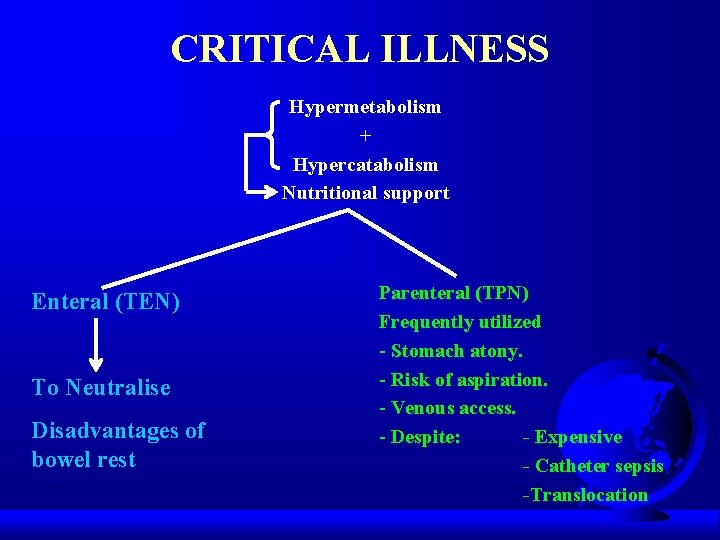
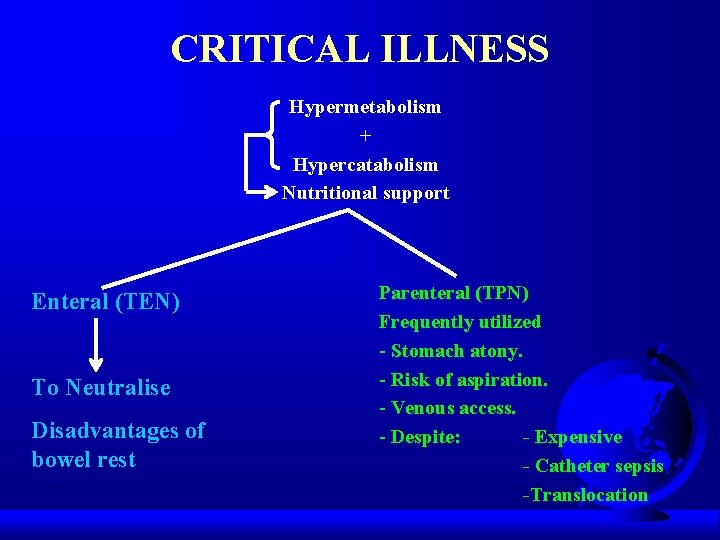
CRITICAL ILLNESS Hypermetabolism + Hypercatabolism Nutritional support Enteral (TEN) To Neutralise Disadvantages of bowel rest Parenteral (TPN) Frequently utilized - Stomach atony. - Risk of aspiration. - Venous access. - Despite: - Expensive - Catheter sepsis -Translocation
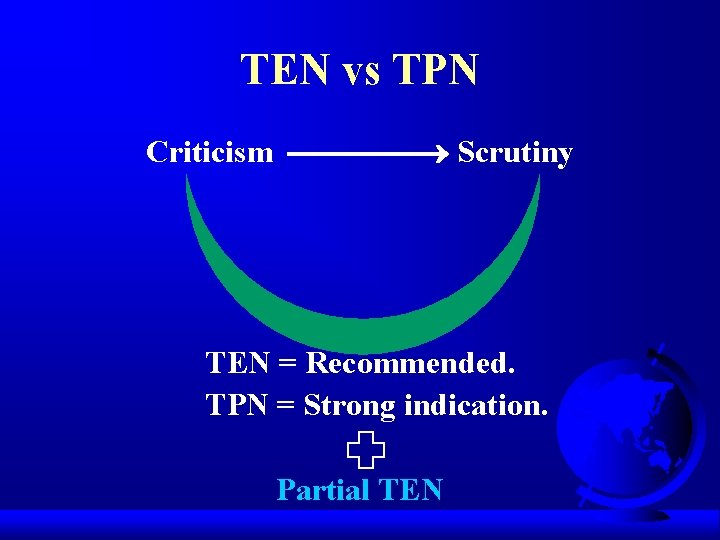
TEN vs TPN Criticism Scrutiny TEN = Recommended. TPN = Strong indication. Partial TEN
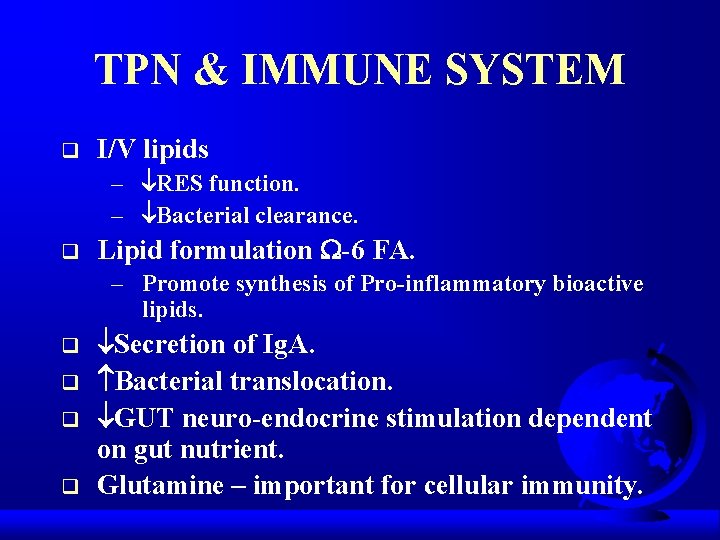
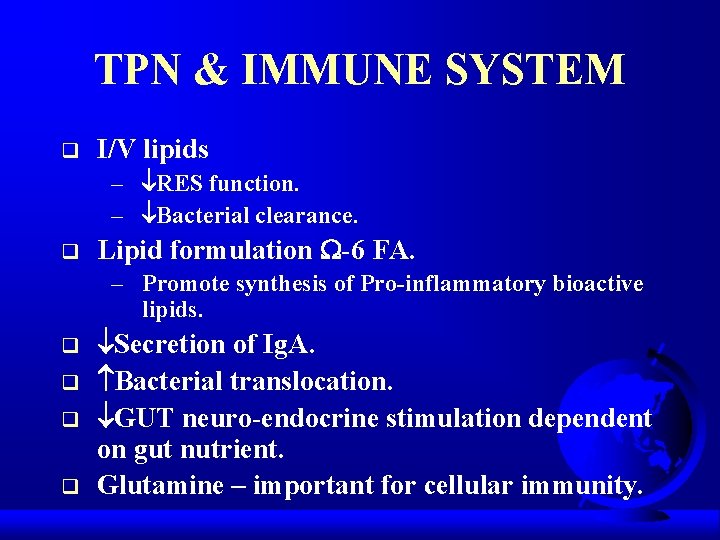
TPN & IMMUNE SYSTEM q I/V lipids – RES function. – Bacterial clearance. q Lipid formulation -6 FA. – Promote synthesis of Pro-inflammatory bioactive lipids. q q Secretion of Ig. A. Bacterial translocation. GUT neuro-endocrine stimulation dependent on gut nutrient. Glutamine – important for cellular immunity.
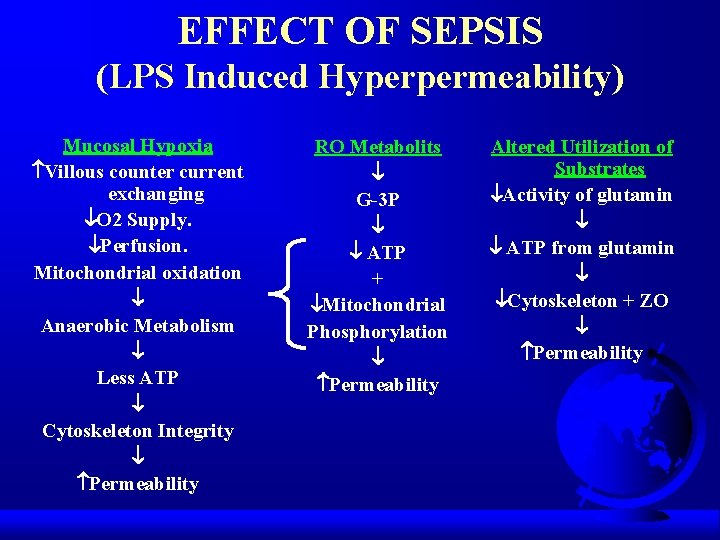
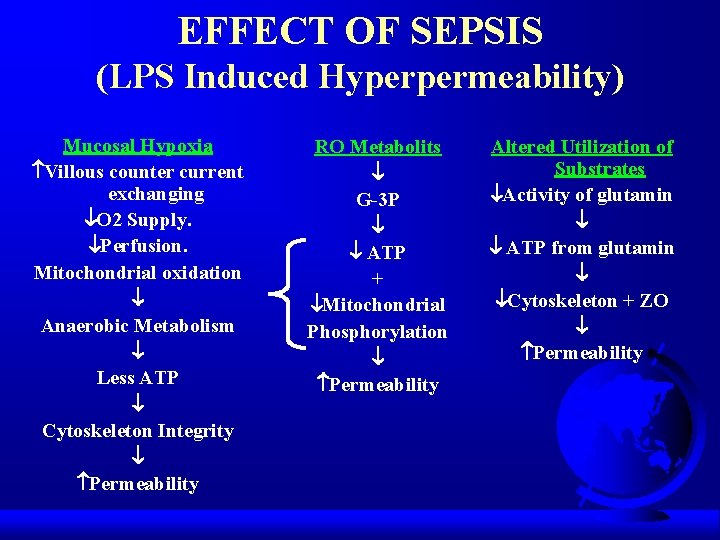
EFFECT OF SEPSIS (LPS Induced Hyperpermeability) Mucosal Hypoxia Villous counter current exchanging O 2 Supply. Perfusion. Mitochondrial oxidation Anaerobic Metabolism Less ATP Cytoskeleton Integrity Permeability RO Metabolits G-3 P ATP + Mitochondrial Phosphorylation Permeability Altered Utilization of Substrates Activity of glutamin ATP from glutamin Cytoskeleton + ZO Permeability
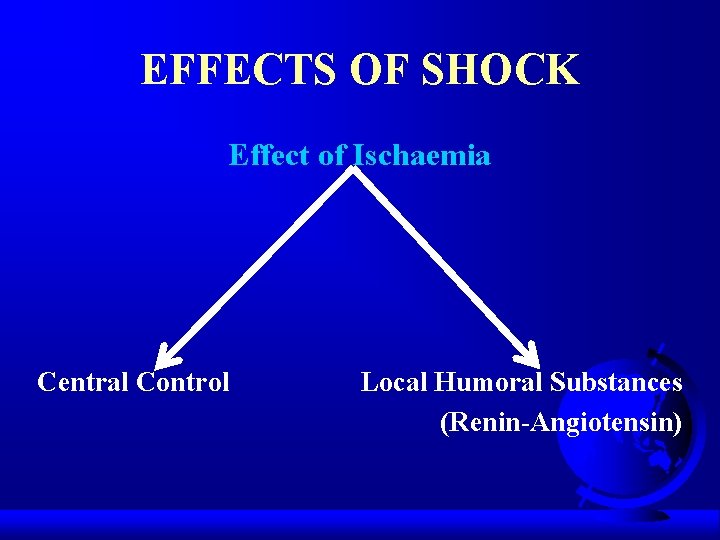
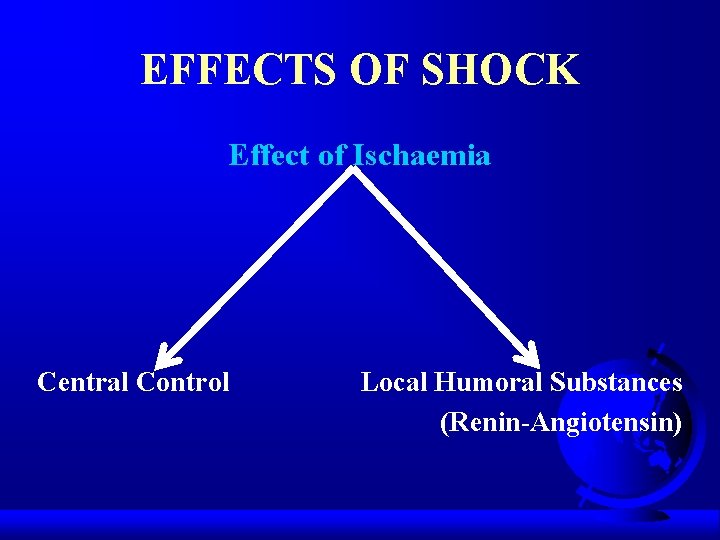
EFFECTS OF SHOCK Effect of Ischaemia Central Control Local Humoral Substances (Renin-Angiotensin)

THE CONTINUUM OF INTESTINAL ISCHAEMIC INJURY Normal Mucosa Capillar Permeability Mucosal Permeability Superficial Mucosal Injury Transmural Injury
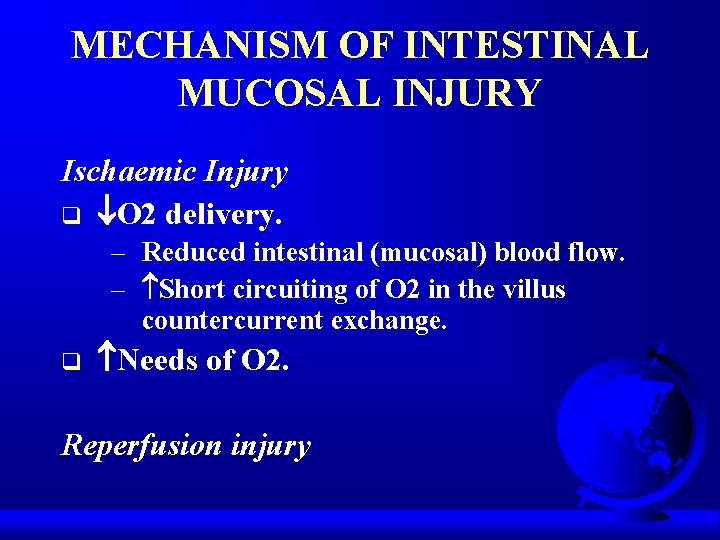
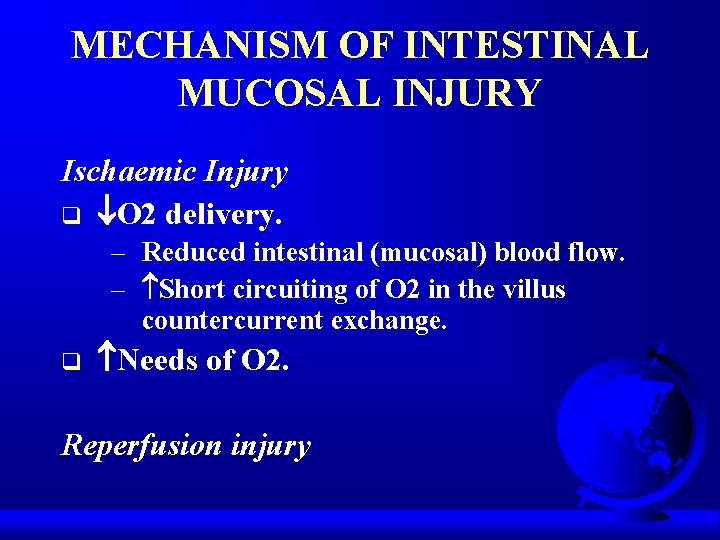
MECHANISM OF INTESTINAL MUCOSAL INJURY Ischaemic Injury q O 2 delivery. – Reduced intestinal (mucosal) blood flow. – Short circuiting of O 2 in the villus countercurrent exchange. q Needs of O 2. Reperfusion injury

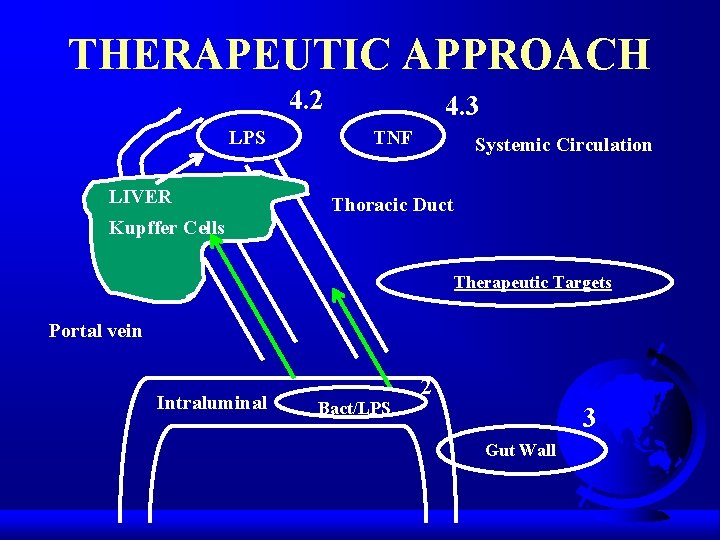
THERAPEUTIC APPROACH q Intraluminal therapeutic approach. q Maintenance of Gut Wall. q Intravasal therapeutic measures.

INTRALUMINAL THERAPEUTIC APPROACH q Peristaltic movement. – Fibre application. q q Bacterial adherence. Bacterial elimination. – SDD. q LPS Neutralization. – Bile acids. – Lactoferin. – Lactulose.
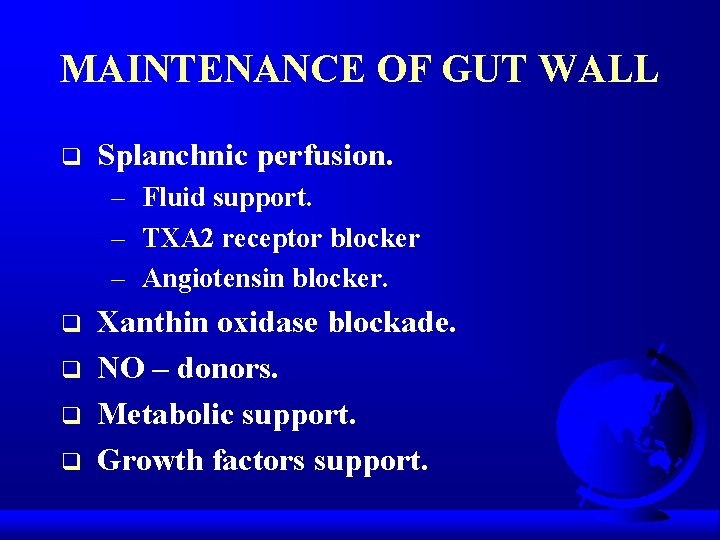
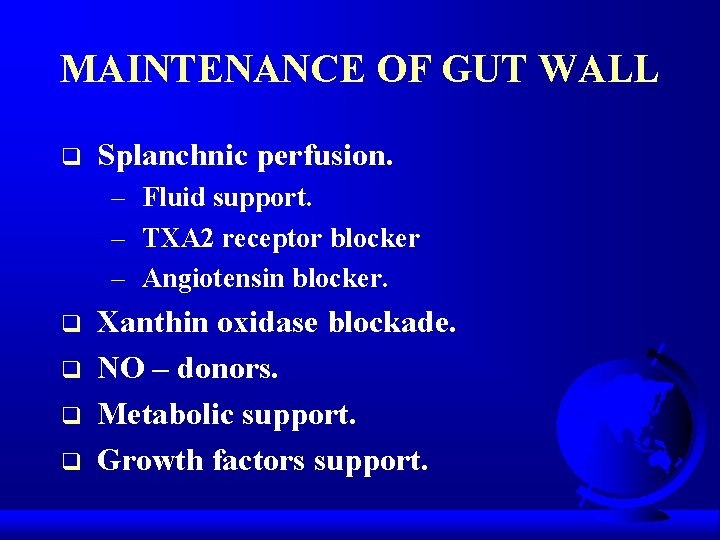
MAINTENANCE OF GUT WALL q Splanchnic perfusion. – Fluid support. – TXA 2 receptor blocker – Angiotensin blocker. q q Xanthin oxidase blockade. NO – donors. Metabolic support. Growth factors support.
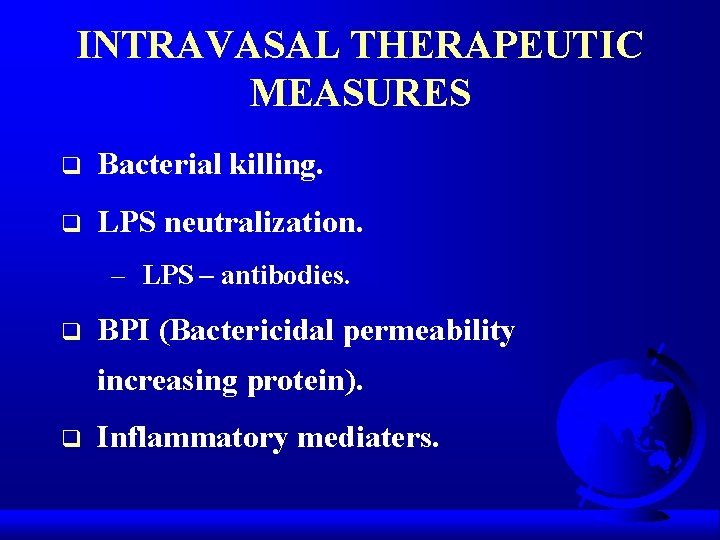
INTRAVASAL THERAPEUTIC MEASURES q Bacterial killing. q LPS neutralization. – LPS – antibodies. q BPI (Bactericidal permeability increasing protein). q Inflammatory mediaters.
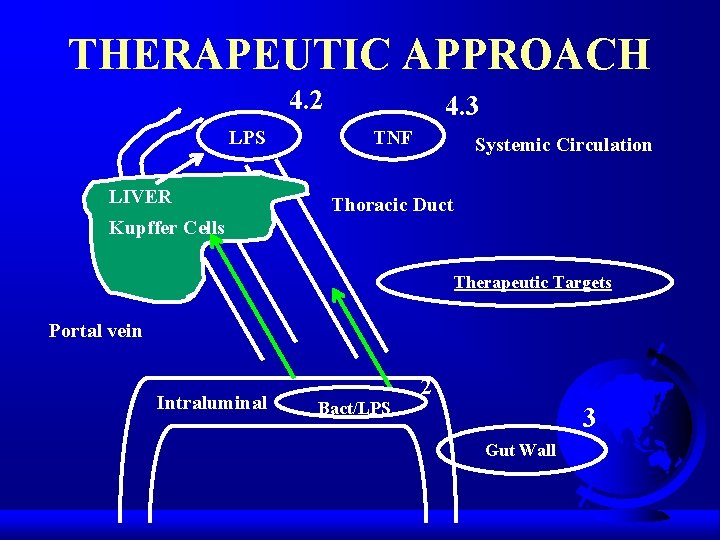
THERAPEUTIC APPROACH 4. 2 LPS LIVER 4. 3 TNF Systemic Circulation Thoracic Duct Kupffer Cells Therapeutic Targets Portal vein Intraluminal Bact/LPS 2 3 Gut Wall

NEW & FUTURE THERAPIES q Metabolic intestinal fuels. – Glutamine. – Shot-chain fatty acids (SCFA). q q Intestinal growth factors. Immunomodulation. – Arginine. – -3 fatty acids. q Antioxidants.

SELECTIVE DECONTAMINATI ON OF DIGESTIVE TRACT