Nutritional assessment in hospitalized patients Biochemical laboratory assessment

Nutritional assessment in hospitalized patients Biochemical, laboratory assessment
The possibilities of biochemical monitoring n On-line monitoring (cardiosurgery – p. H, minerals (K), the electrodes are localized on central cateter, possibility to check parameters on-line. n bed side monitoring (glycaemia, urine /protein, p. H, blood. . /, oximeter O 2 saturation, acidobasis, drugs /dg. strips) n Biochemical analysis
Biochemical parameters n Na, K, Cl, Ca, P, Mg, osmolality - blood, urine n Acidobasis, lactate n urea, creatinin clearence, Nitrogen balance n bilirubine, ALT, AST, LDH, amylase, lipase n cholesterol, triglycerides, glucose – blood, urine
Biochemical parameters n Total protein, albumine, prealbumine n CRP n TSH n Basic analysis are made at the first, must be done within 90 minutes
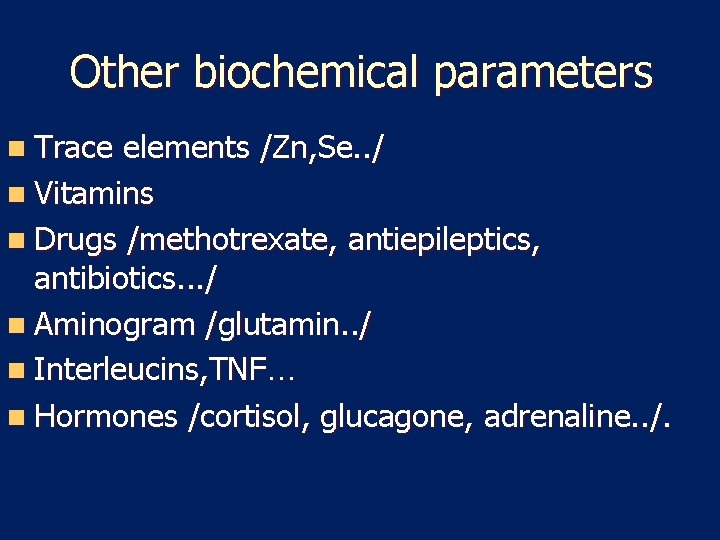
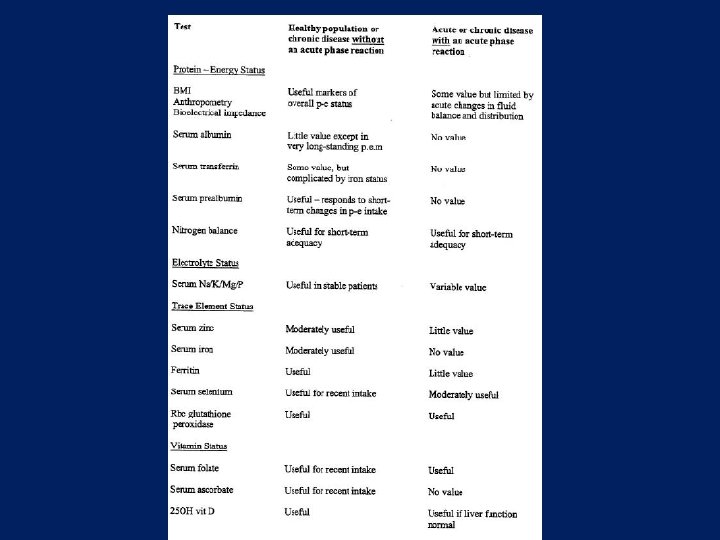
Other biochemical parameters n Trace elements /Zn, Se. . / n Vitamins n Drugs /methotrexate, antiepileptics, antibiotics. . . / n Aminogram /glutamin. . / n Interleucins, TNF… n Hormones /cortisol, glucagone, adrenaline. . /.
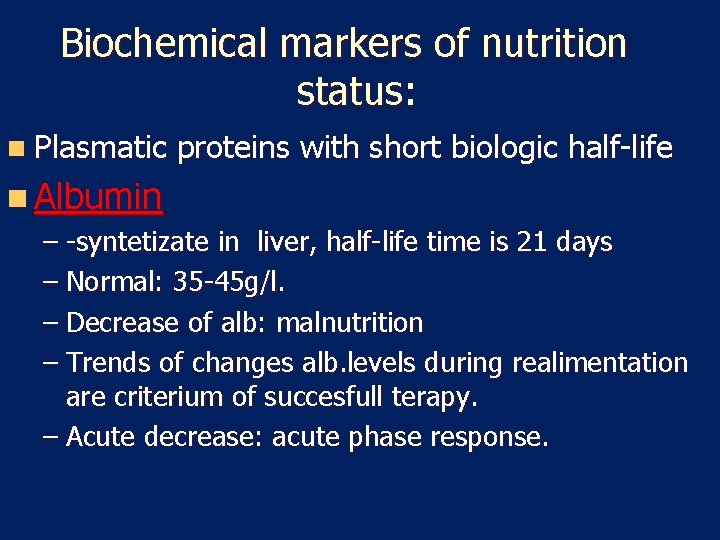
Biochemical markers of nutrition status: n Plasmatic proteins with short biologic half-life n Albumin – -syntetizate in liver, half-life time is 21 days – Normal: 35 -45 g/l. – Decrease of alb: malnutrition – Trends of changes alb. levels during realimentation are criterium of succesfull terapy. – Acute decrease: acute phase response.

Biochemical markers of nutrition status: n Transferin: syntesized in liver, – biolog HL: 8 days. Fysiolog. – Value 2 -4 g/l, – fe n RBP: syntesized in liver – Biolog half-life : 12 h. , – Normal value: 0, 03 -0, 006 g/l. – Acute phase reactant (negative) – Zn
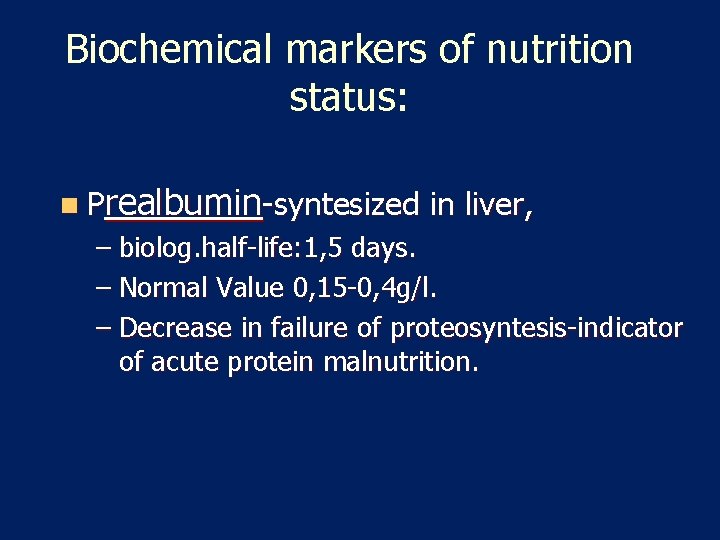
Biochemical markers of nutrition status: n Prealbumin-syntesized in liver, – biolog. half-life: 1, 5 days. – Normal Value 0, 15 -0, 4 g/l. – Decrease in failure of proteosyntesis-indicator of acute protein malnutrition.
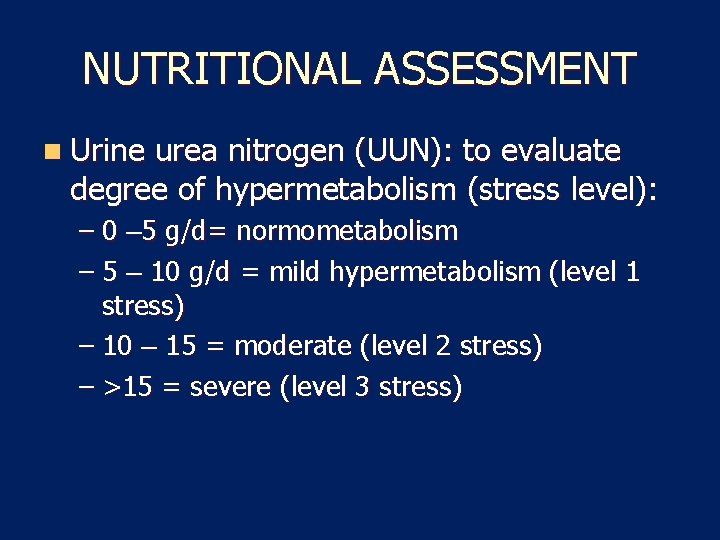
NUTRITIONAL ASSESSMENT n Urine urea nitrogen (UUN): to evaluate degree of hypermetabolism (stress level): – 0 – 5 g/d= normometabolism – 5 – 10 g/d = mild hypermetabolism (level 1 stress) – 10 – 15 = moderate (level 2 stress) – >15 = severe (level 3 stress)
Nutrition Monitoring and Evaluation n Monitor progress and determine if goals are met n Identifies patient/client outcomes relevant to the nutrition diagnosis and intervention plans and goals n Measure and compare to client’s previous status, nutrition goals, or reference standards
Other Outcomes Food and Nutrient Intake (FI) n Energy intake n Food and Beverage n Enteral and parenteral n Bioactive substances n Macronutrients n Micronutrients Physical Signs/Symptoms n Anthropometric n Biochemical and medical tests n Physical examination

Monitoring
Some Lab tests
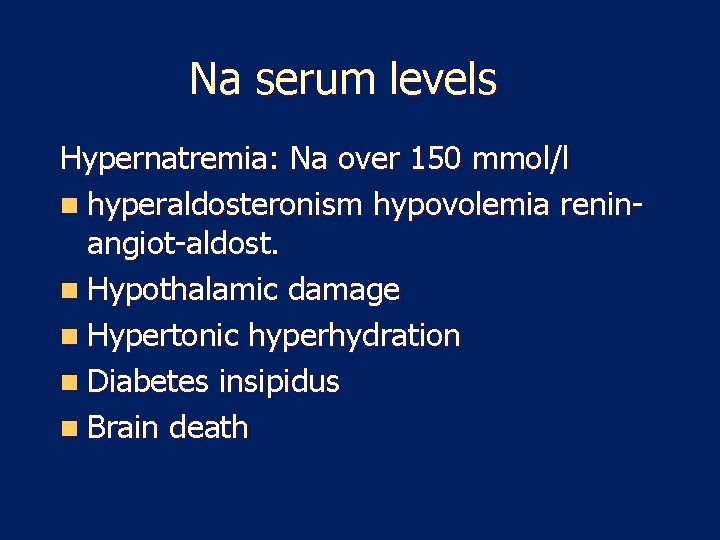
Na serum levels Hypernatremia: Na over 150 mmol/l n hyperaldosteronism hypovolemia reninangiot-aldost. n Hypothalamic damage n Hypertonic hyperhydration n Diabetes insipidus n Brain death
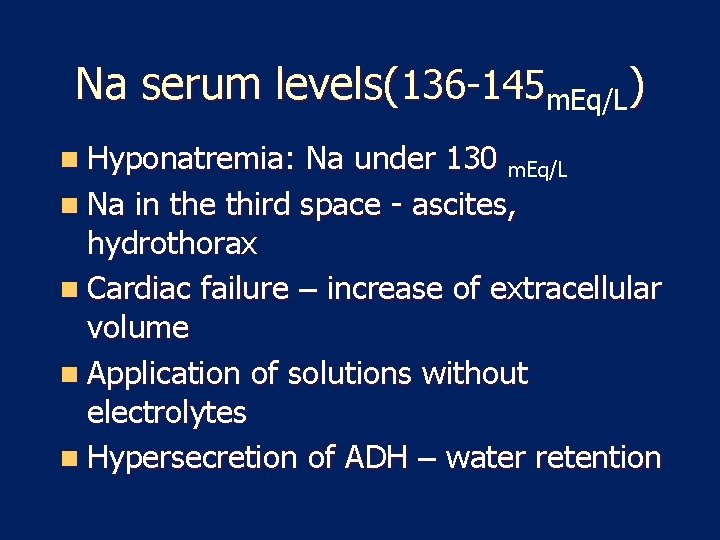
Na serum levels(136 -145 m. Eq/L) n Hyponatremia: Na under 130 m. Eq/L n Na in the third space - ascites, hydrothorax n Cardiac failure – increase of extracellular volume n Application of solutions without electrolytes n Hypersecretion of ADH – water retention
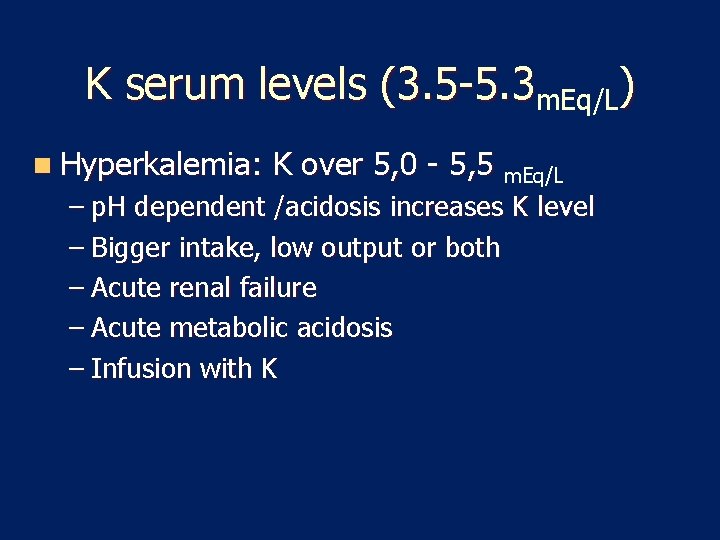
K serum levels (3. 5 -5. 3 m. Eq/L) n Hyperkalemia: K over 5, 0 - 5, 5 m. Eq/L – p. H dependent /acidosis increases K level – Bigger intake, low output or both – Acute renal failure – Acute metabolic acidosis – Infusion with K
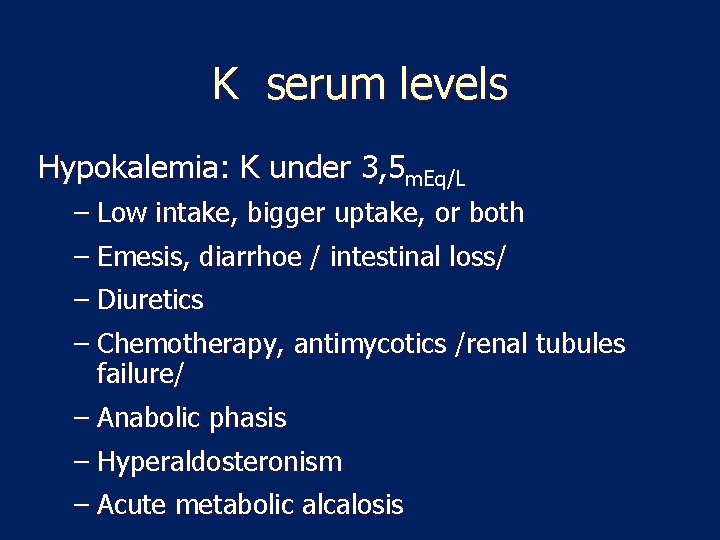
K serum levels Hypokalemia: K under 3, 5 m. Eq/L – Low intake, bigger uptake, or both – Emesis, diarrhoe / intestinal loss/ – Diuretics – Chemotherapy, antimycotics /renal tubules failure/ – Anabolic phasis – Hyperaldosteronism – Acute metabolic alcalosis
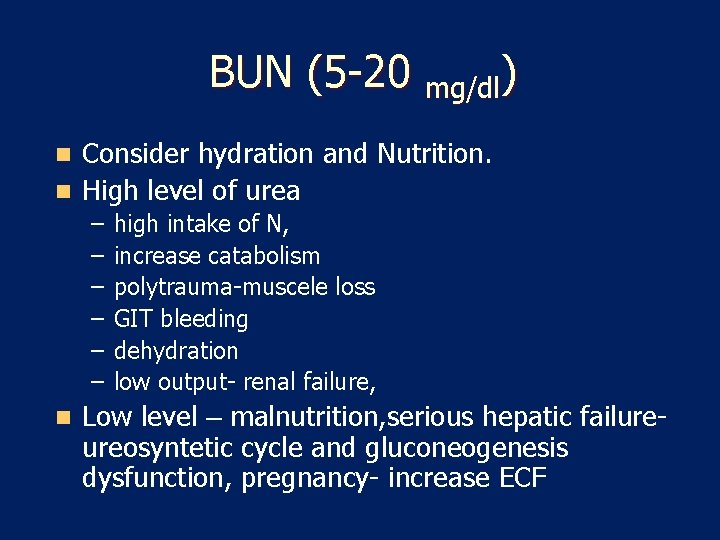
BUN (5 -20 mg/dl) Consider hydration and Nutrition. n High level of urea n – – – n high intake of N, increase catabolism polytrauma-muscele loss GIT bleeding dehydration low output- renal failure, Low level – malnutrition, serious hepatic failureureosyntetic cycle and gluconeogenesis dysfunction, pregnancy- increase ECF

BUN (5 -20 mg/dl) n Low level – – malnutrition, – serious hepatic failure– ureosyntetic cycle and gluconeogenesis dysfunction, – pregnancy– increase ECF
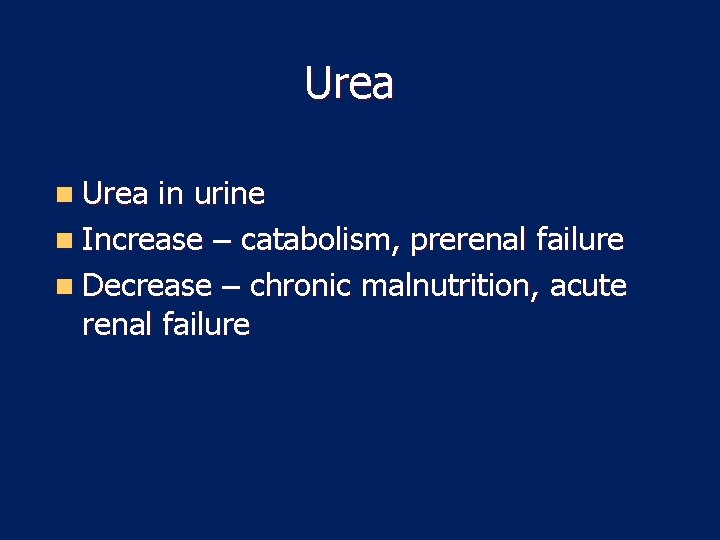
Urea n Urea in urine n Increase – catabolism, prerenal failure n Decrease – chronic malnutrition, acute renal failure
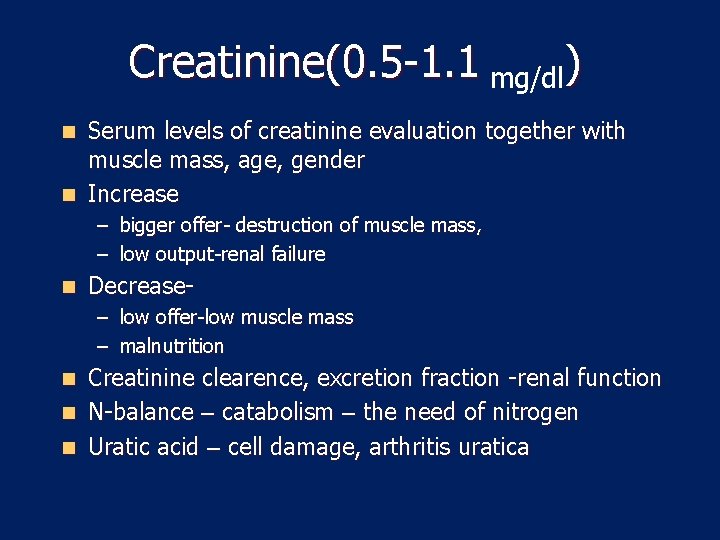
Creatinine(0. 5 -1. 1 mg/dl) Serum levels of creatinine evaluation together with muscle mass, age, gender n Increase n – bigger offer- destruction of muscle mass, – low output-renal failure n Decrease– low offer-low muscle mass – malnutrition Creatinine clearence, excretion fraction -renal function n N-balance – catabolism – the need of nitrogen n Uratic acid – cell damage, arthritis uratica n
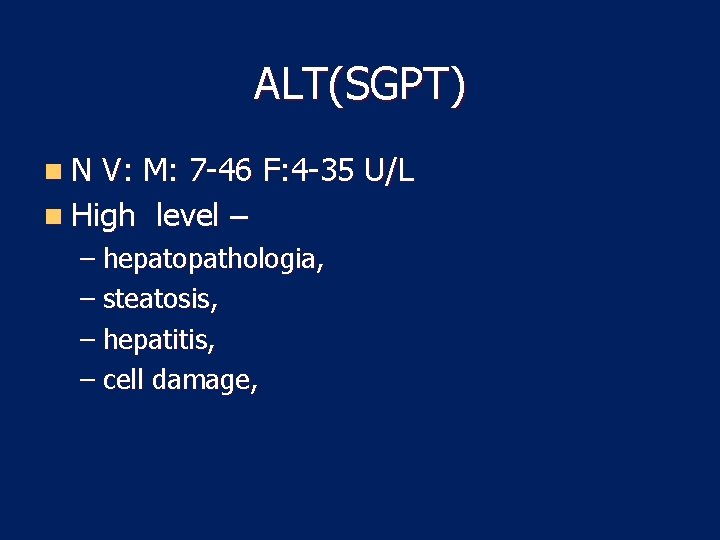
ALT(SGPT) n. N V: M: 7 -46 F: 4 -35 U/L n High level – – hepatopathologia, – steatosis, – hepatitis, – cell damage,
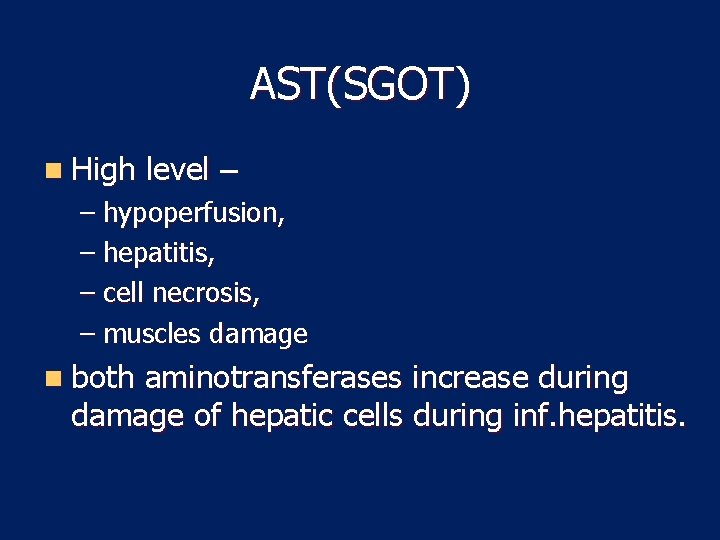
AST(SGOT) n High level – – hypoperfusion, – hepatitis, – cell necrosis, – muscles damage n both aminotransferases increase during damage of hepatic cells during inf. hepatitis.
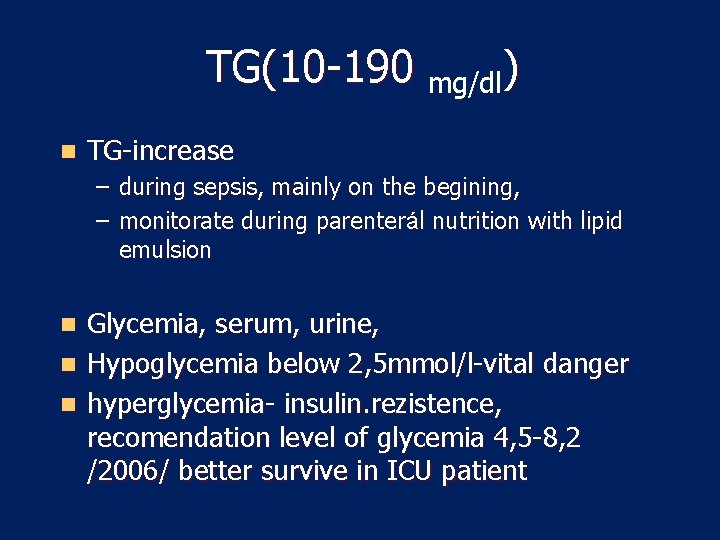
TG(10 -190 mg/dl) n TG-increase – during sepsis, mainly on the begining, – monitorate during parenterál nutrition with lipid emulsion Glycemia, serum, urine, n Hypoglycemia below 2, 5 mmol/l-vital danger n hyperglycemia- insulin. rezistence, recomendation level of glycemia 4, 5 -8, 2 /2006/ better survive in ICU patient n
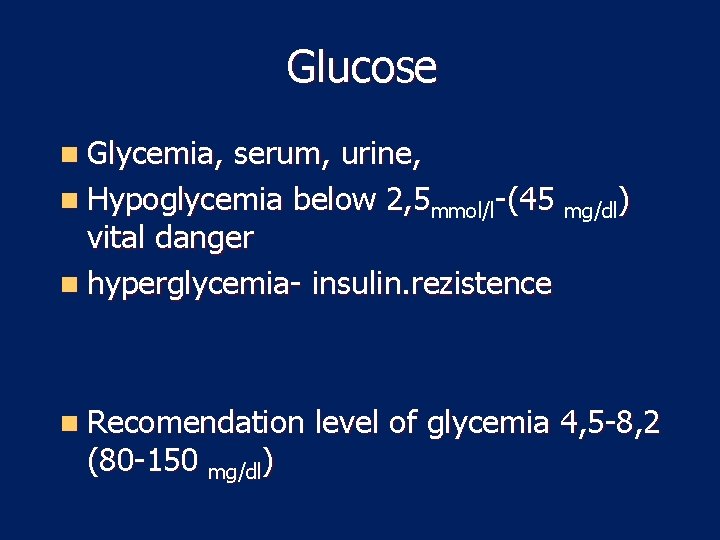
Glucose n Glycemia, serum, urine, n Hypoglycemia below 2, 5 mmol/l-(45 mg/dl) vital danger n hyperglycemia- insulin. rezistence n Recomendation (80 -150 mg/dl) level of glycemia 4, 5 -8, 2
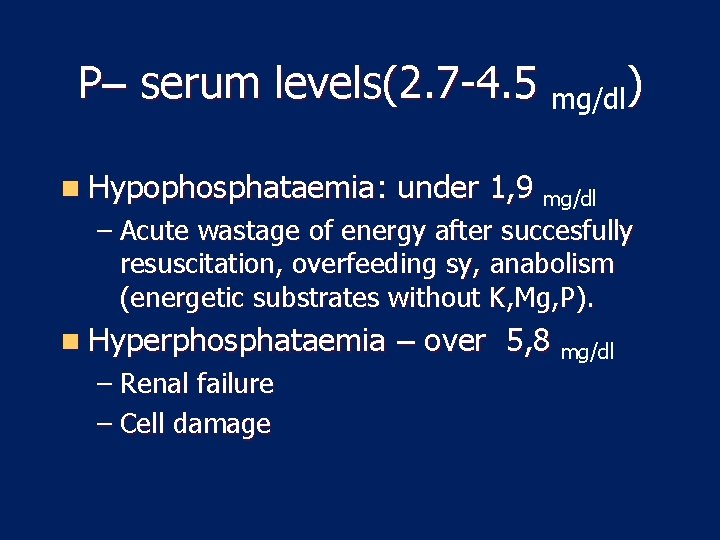
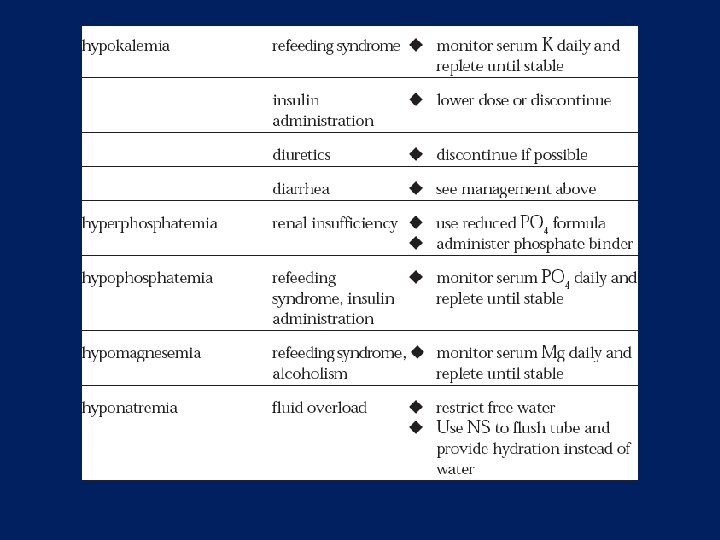
P– serum levels(2. 7 -4. 5 mg/dl) n Hypophosphataemia: under 1, 9 mg/dl – Acute wastage of energy after succesfully resuscitation, overfeeding sy, anabolism (energetic substrates without K, Mg, P). n Hyperphosphataemia – Renal failure – Cell damage – over 5, 8 mg/dl
Mg – serum levels (1, 3 -2, 5 m. Eq/L) n Mg – together with potassium n Hypomagnesaemia – under 1, 2 m. Eq/L / – renal failure – low intake.
Monitoring of EN n For formula intolerance, n Hydration status, n Electrolyte status, n Nutritional status,
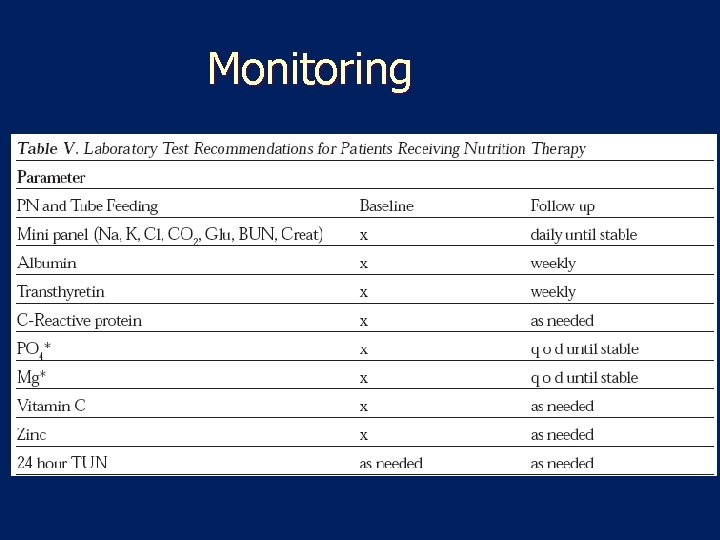
Monitoring

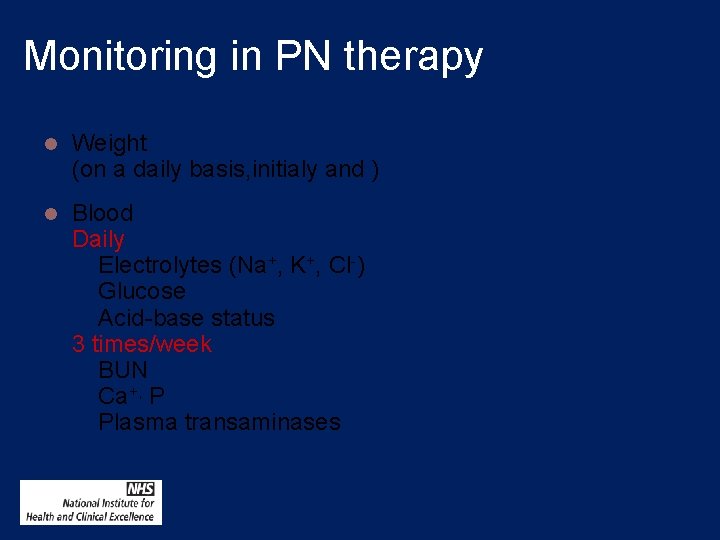
Monitoring in PN therapy l Weight (on a daily basis, initialy and ) l Blood Daily Electrolytes (Na+, K+, Cl-) Glucose Acid-base status 3 times/week BUN Ca+, P Plasma transaminases
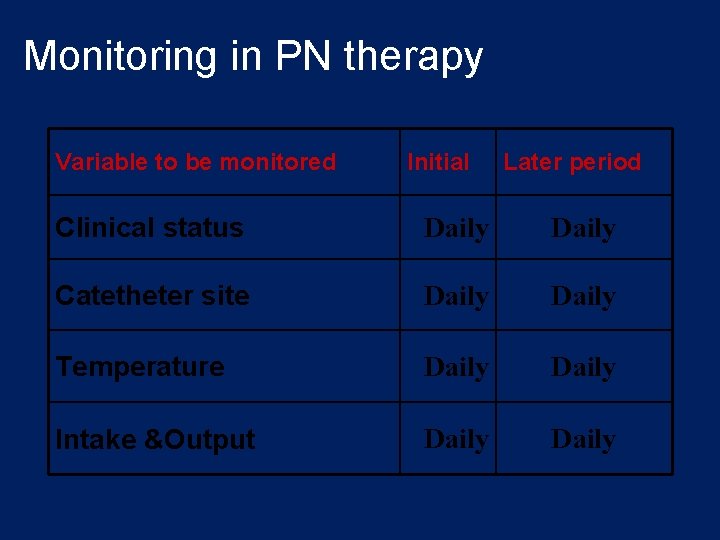
Monitoring in PN therapy Variable to be monitored Initial Later period Clinical status Daily Catetheter site Daily Temperature Daily Intake &Output Daily
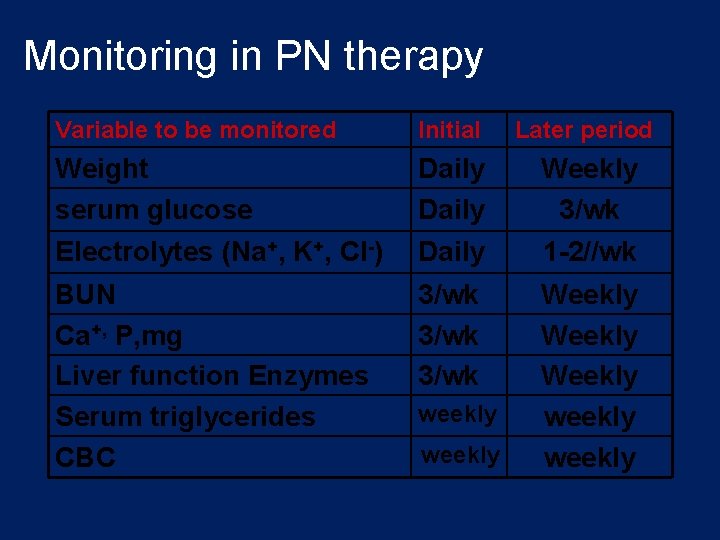
Monitoring in PN therapy Variable to be monitored Initial Later period Weight serum glucose Daily Weekly 3/wk Electrolytes (Na+, K+, Cl-) Daily 1 -2//wk BUN Ca+, P, mg Liver function Enzymes Serum triglycerides CBC 3/wk Weekly weekly
Problems 1. Catheter sepsis 2. Placement problems 3. Metabolic complications
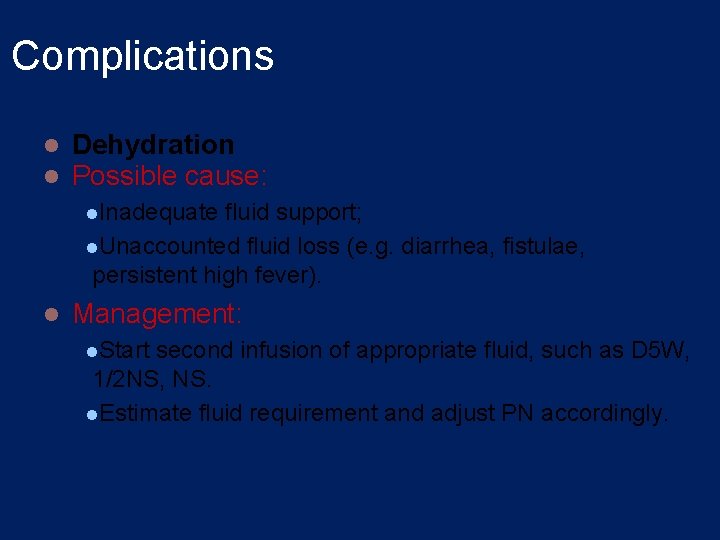
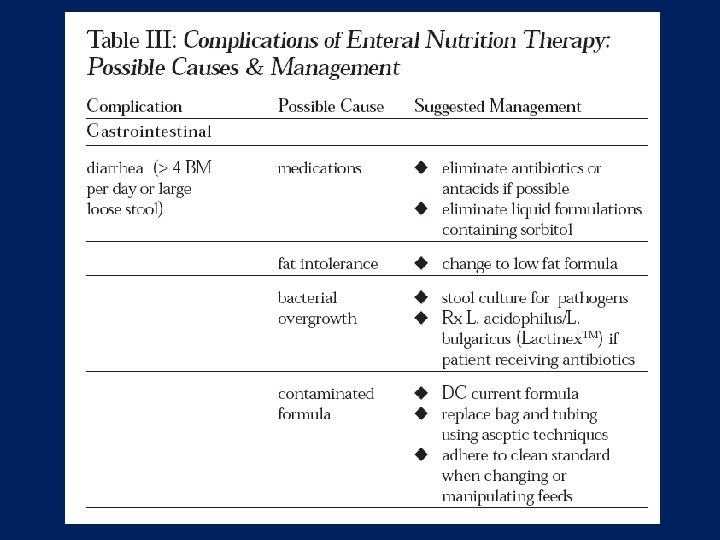
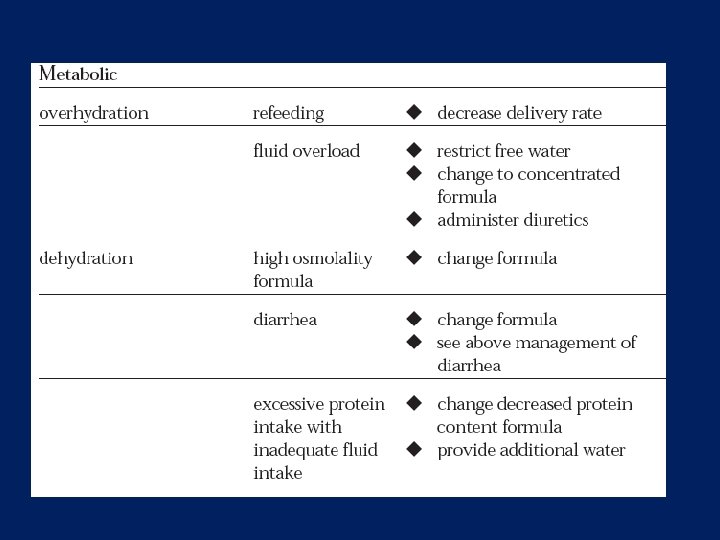
Complications l l Dehydration Possible cause: l. Inadequate fluid support; l. Unaccounted fluid loss (e. g. diarrhea, fistulae, persistent high fever). l Management: l. Start second infusion of appropriate fluid, such as D 5 W, 1/2 NS, NS. l. Estimate fluid requirement and adjust PN accordingly.
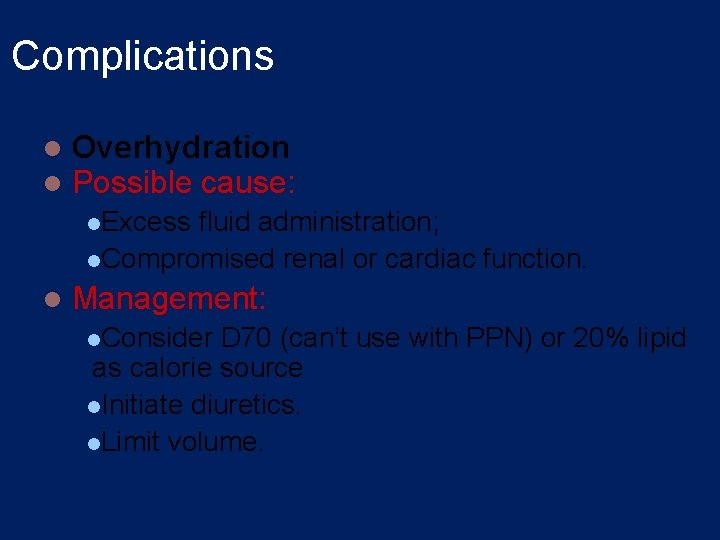
Complications l l Overhydration Possible cause: l. Excess fluid administration; l. Compromised renal or cardiac function. l Management: l. Consider D 70 (can’t use with PPN) or 20% lipid as calorie source l. Initiate diuretics. l. Limit volume.
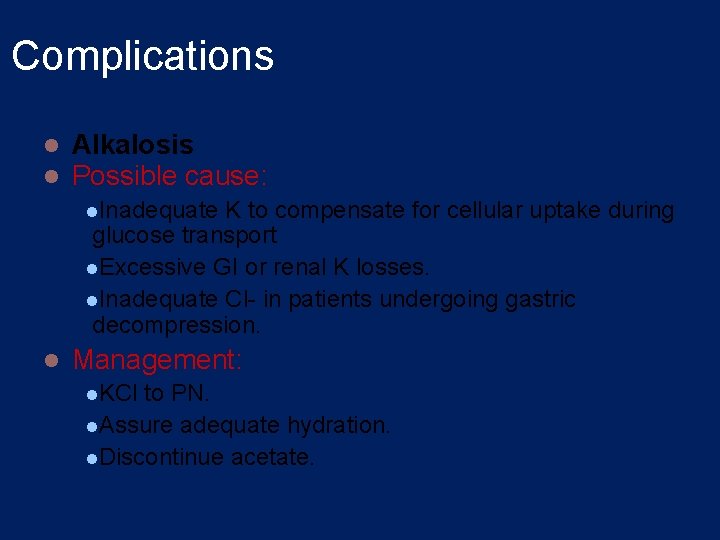
Complications l l Alkalosis Possible cause: l. Inadequate K to compensate for cellular uptake during glucose transport l. Excessive GI or renal K losses. l. Inadequate Cl- in patients undergoing gastric decompression. l Management: l. KCl to PN. l. Assure adequate hydration. l. Discontinue acetate.
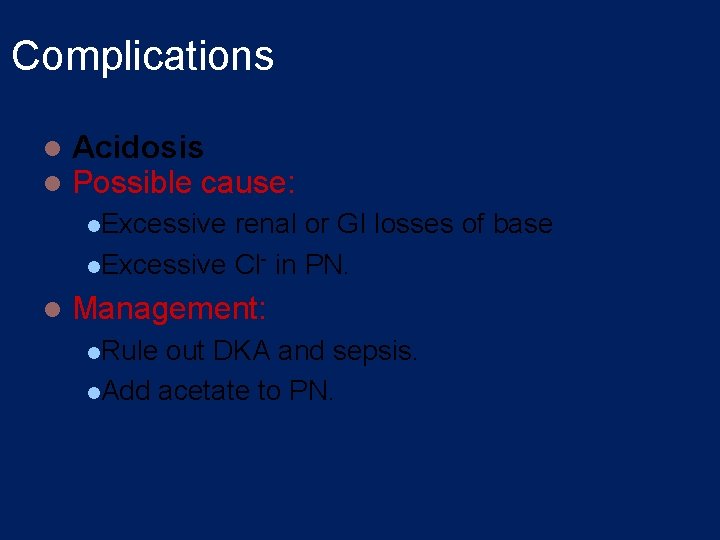
Complications l l Acidosis Possible cause: l. Excessive renal or GI losses of base l. Excessive Cl- in PN. l Management: l. Rule out DKA and sepsis. l. Add acetate to PN.
Complications l l Hypercarbia Possible cause: l. Excessive l calorie or carbohydrate load. Management: l. Decrease total calories or l. CHO load.
Complications l l Hypocalcemia Possible cause: l. Excessive PO 4 salts l. Low serum albumin. l. Inadequate Ca in PN. l Management: l. Slowly increase calcium in PN prescription.
Complications l l Hypercalcemia Possible cause: l. Excessive Ca in PN l. Administration of vitamin A in patients with renal failure. l. Can lead to pancreatitis. l Management: l. Decrease calcium in PN. l. Ensure adequate hydration. l. Limit vitamin supplements in patients with renal failure to vitamin C and B vitamins.
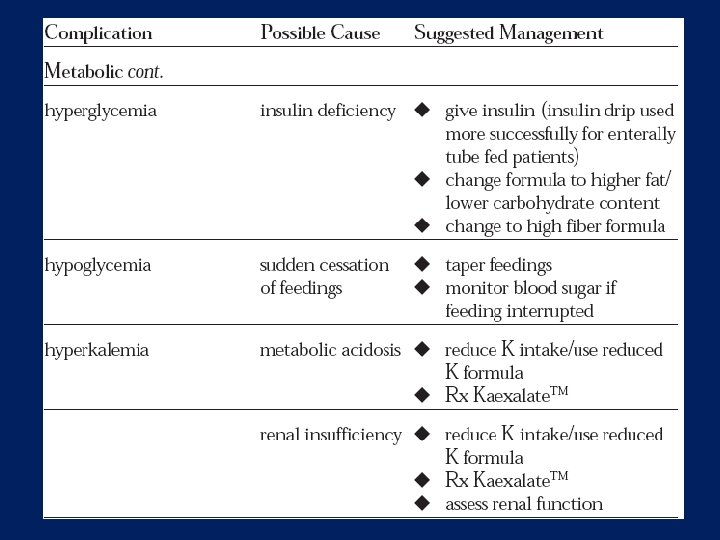
Complications l Hyperglycemia l Possible cause: l. Stress response. Occurs approximately 25% of cases. Management: l. Rule out infection. l. Decrease carbohydrate in PN. l. Provide adequate insulin.
Complications l Hypoglycemia l Possible cause: l. Sudden withdrawal of concentrated glucose. l. More common in children. l Management: l. Taper PN. Start D 10.
Complications l Cholestasis l Possible cause: l. Lack of GI stimulation. l. Sludge present in 50% of patients on PN for 4 -6 weeks; lresolves with resumption of enteral feeding. l Management: l. Promote enteral feeding.
- Slides: 55