NUTRITION THERAPY FOR CHYLOTHORAX A Case Study Aleene
- Slides: 40
NUTRITION THERAPY FOR CHYLOTHORAX A Case Study: Aleene Poulsen
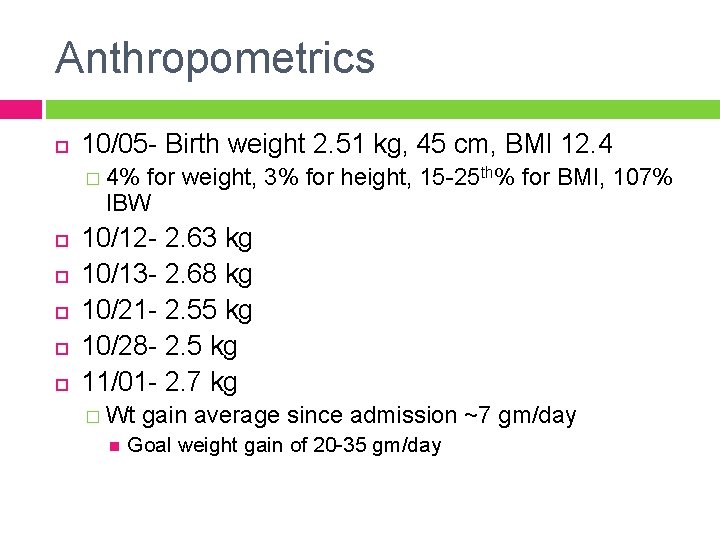
Patient Profile and Social History Newborn Caucasian female ST was a 36 2/7 weeker Birth weight 2. 51 kg, 45 cm, BMI 12. 4 � 4% for weight, 3% for height, 15 -25 th% for BMI, 107% IBW Maternal history of Wilson’s disease and post partum psychosis
Nutrition Therapy for Chylothorax
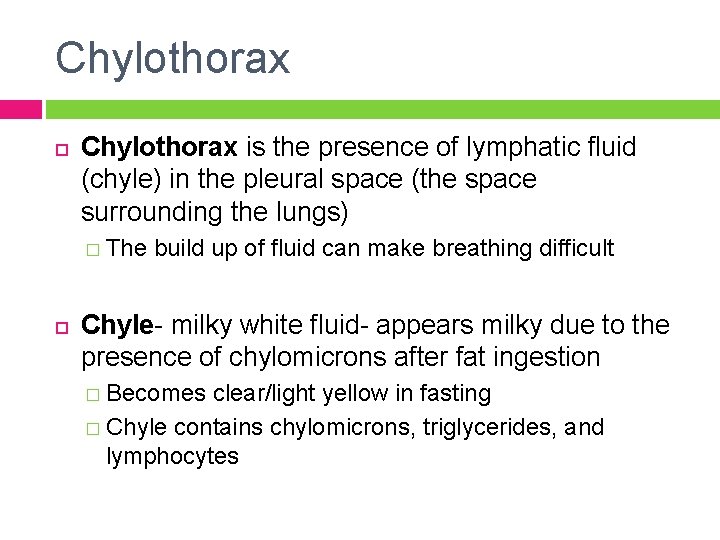
Chylothorax is the presence of lymphatic fluid (chyle) in the pleural space (the space surrounding the lungs) � The build up of fluid can make breathing difficult Chyle- milky white fluid- appears milky due to the presence of chylomicrons after fat ingestion � Becomes clear/light yellow in fasting � Chyle contains chylomicrons, triglycerides, and lymphocytes
Chylothorax Etiology Chylothorax develops as a result of damage to the thoracic duct (by rupture, laceration, tear or compression) � Complication of cardiothoracic surgery � Congenital malformations, trauma, malignancy, Turner’s or Noonan’s Syndrome Diagnosis confirmed by examination of the pleural fluid
Nutrition Concerns During Chylothorax Potentially life threatening disorder � Large losses of nutrients and immune cells put patients at risk for malnutrition, may impair their immune system and may lead to respiratory problems High energy and protein requirements � Increased metabolic demand from the combination of chyle loss and hypermetabolism associated with surgery � Protein supplementation may be necessary
Treatment Strategies Goal- reduce flow of chyle to wait for healing � Dietary modifications- low fat diet � Medications- Somatostatin, Octreotide � Surgical procedures
Nutrition Therapy TPN with intravenous lipid (IL) TPN/IL transitioning to a high MCT formula MCT diet with IL or alone � Concerns- essential fatty acid deficiency Fat free breastmilk fortified with low fat or MCT formula such as Enfaport
Medium Chain Triglyceride Diet Oral diet enriched with MCT preferred (in the absence of raised central venous pressure) � Avoids complications associated with parenteral nutrition (such as thrombosis and sepsis) � Protects gut barrier function with enteral feeding Continue enteral feeds with MCT-diet until chylothorax has resolved (4 -6 weeks), then transition to a normal diet Panthongviriyakul C, Bines JE. Post-operative chylothorax in children: An evidencebased management algorithm. J of Paediatrics and Child Health. 2008; 44: 716 -721
Parenteral Nutrition Parenteral nutrition may be more compatible with other treatments such as somatostatin analogs. Chalret du Rieu M, Mabrut J-Y. Management of postoperative chylothorax. Journal of Visceral Surgery. 2011; doi: 10. 1016/j. jviscsurg. 2011. 09. 006
Enteral Formulas Used for Chylothorax Enfaport LIPIL � Contains all essential fatty acids (EFA), sterile liquid form, 30 kcal/oz can � MCT oil 84%, soy oil (13%), DHA & ARA (3%) � High protein
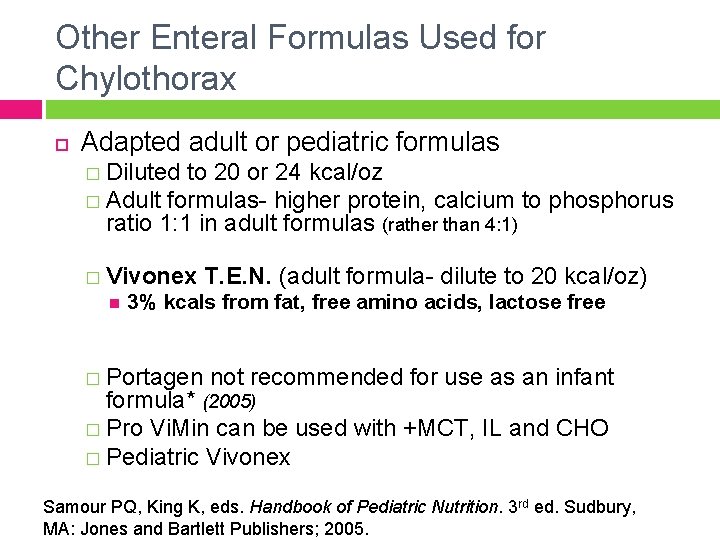
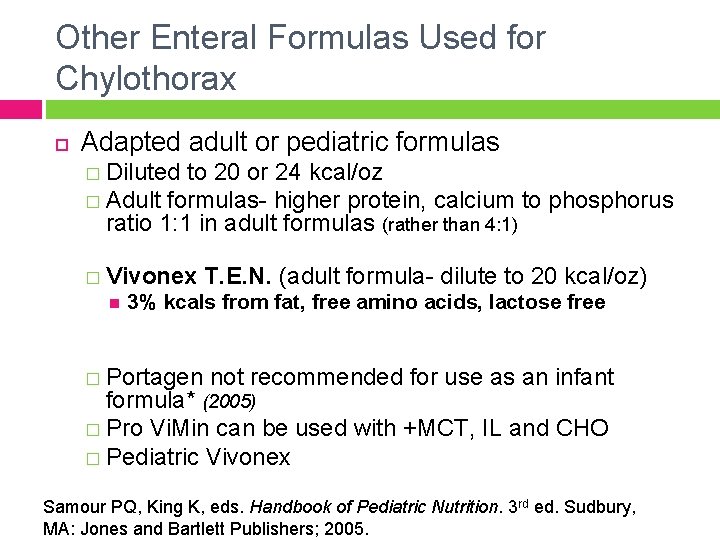
Other Enteral Formulas Used for Chylothorax Adapted adult or pediatric formulas � Diluted to 20 or 24 kcal/oz � Adult formulas- higher protein, calcium to phosphorus ratio 1: 1 in adult formulas (rather than 4: 1) � Vivonex T. E. N. (adult formula- dilute to 20 kcal/oz) 3% kcals from fat, free amino acids, lactose free � Portagen not recommended for use as an infant formula* (2005) � Pro Vi. Min can be used with +MCT, IL and CHO � Pediatric Vivonex Samour PQ, King K, eds. Handbook of Pediatric Nutrition. 3 rd ed. Sudbury, MA: Jones and Bartlett Publishers; 2005.
Fat-Free Breast Milk and Enteral Formula Infants with chylothorax may benefit from using human milk because of it immunologic qualities � After removal of fat HM becomes deficient in calories, essential fatty acids and fat-soluble vitamins � Supplement with formulas with MCT’s, vitamins or glucose polymers “The use of fat-free mother’s milk resulted in no reaccumulation of the chylous pleural effusion” Chan GM, Lechtenberg E. The use of fat-free human milk in infants with chylous pleural effusion. Journal of Perinatology. 2007; 27: 434 -436.
Patient Care Plan
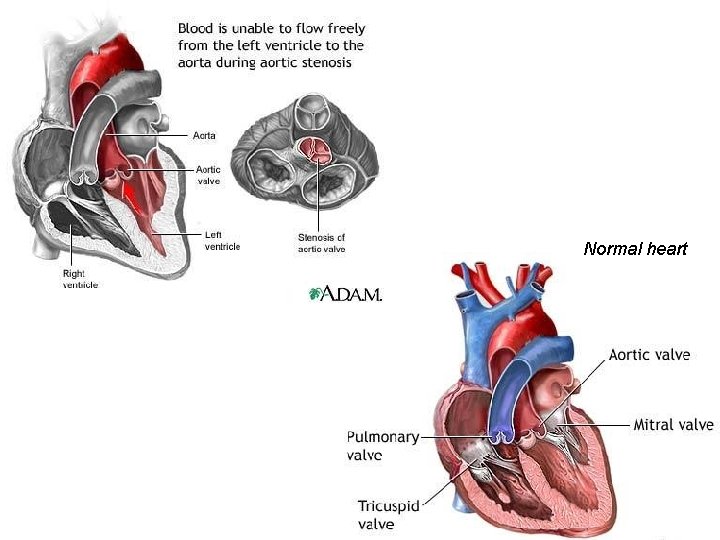
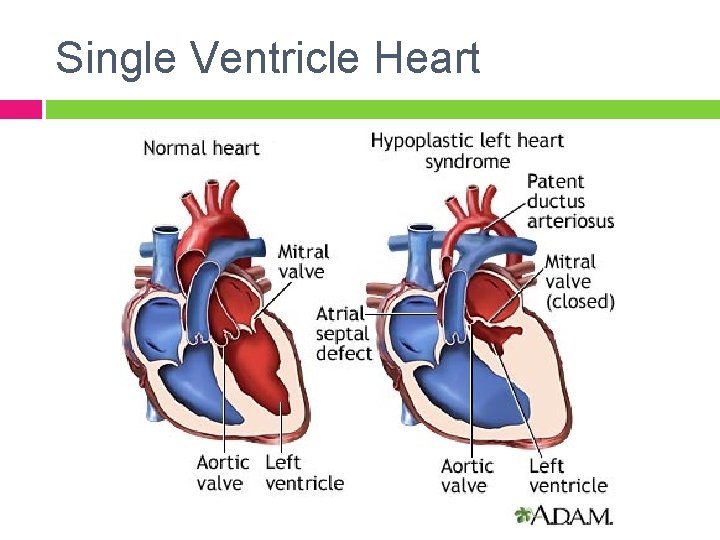
Medical History and Admit Information Congenital heart defect Prenatal diagnosis of critical aortic stenosis � “Single ventricle physiology” 10/05/11 - ST born at University of Utah Medical Center and transferred to the CICU at PCMC
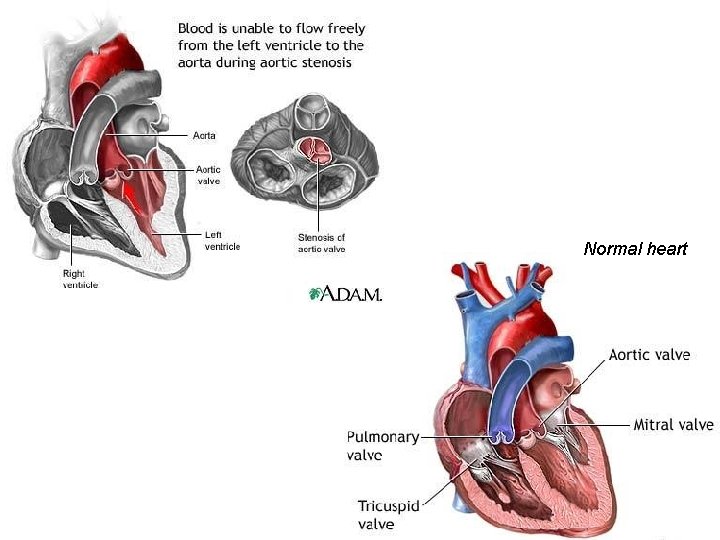
Normal heart
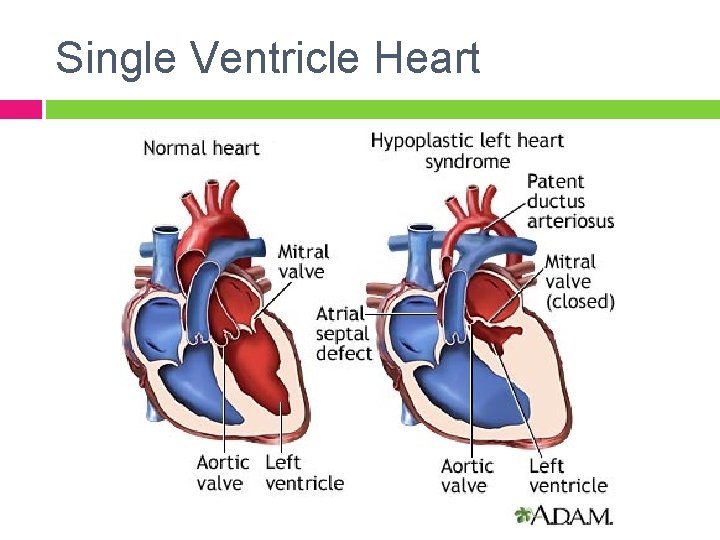
Single Ventricle Heart
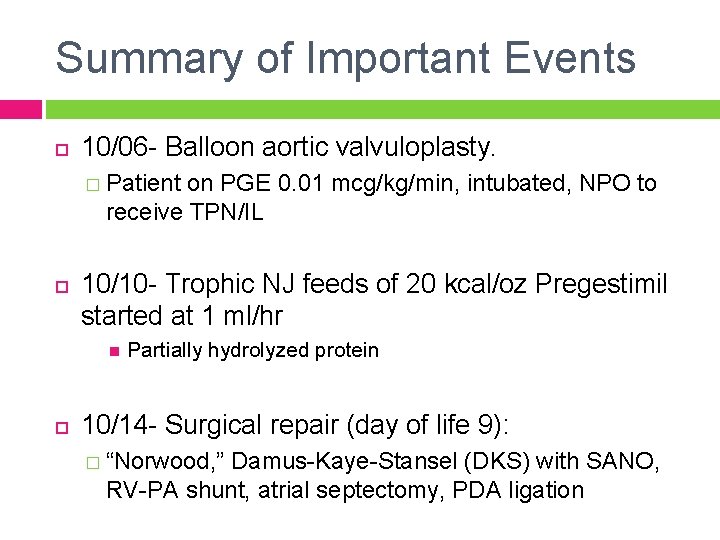
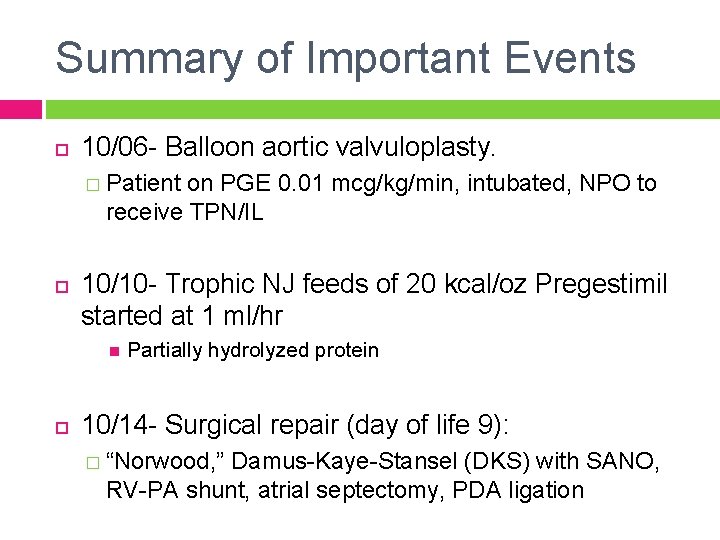
Summary of Important Events 10/06 - Balloon aortic valvuloplasty. � Patient on PGE 0. 01 mcg/kg/min, intubated, NPO to receive TPN/IL 10/10 - Trophic NJ feeds of 20 kcal/oz Pregestimil started at 1 ml/hr Partially hydrolyzed protein 10/14 - Surgical repair (day of life 9): � “Norwood, ” Damus-Kaye-Stansel (DKS) with SANO, RV-PA shunt, atrial septectomy, PDA ligation
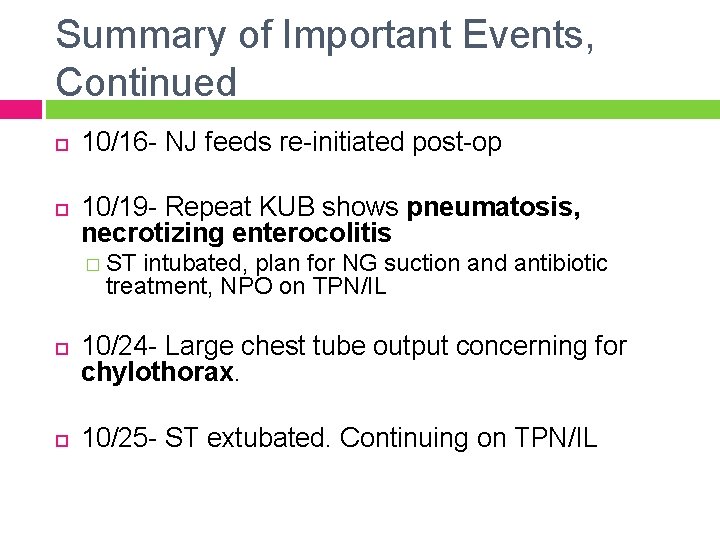
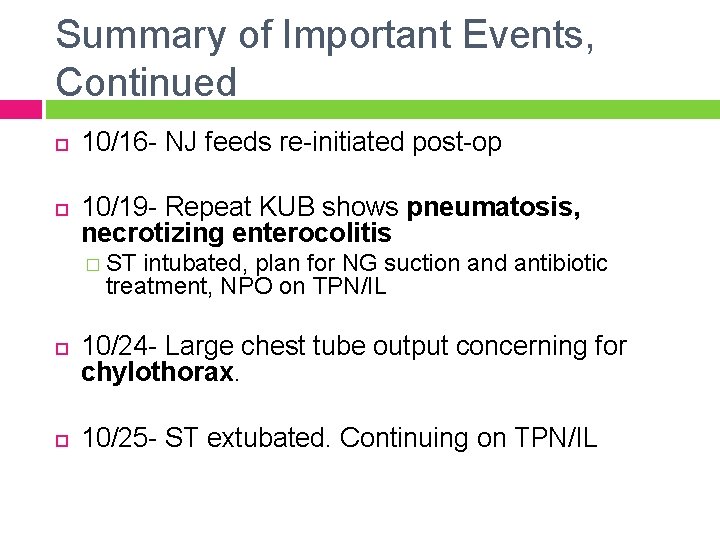
Summary of Important Events, Continued 10/16 - NJ feeds re-initiated post-op 10/19 - Repeat KUB shows pneumatosis, necrotizing enterocolitis � ST intubated, plan for NG suction and antibiotic treatment, NPO on TPN/IL 10/24 - Large chest tube output concerning for chylothorax. 10/25 - ST extubated. Continuing on TPN/IL
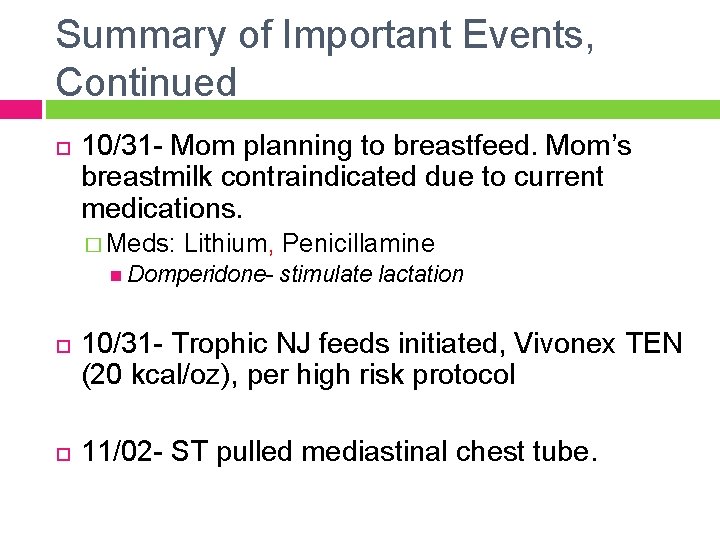
Summary of Important Events, Continued 10/31 - Mom planning to breastfeed. Mom’s breastmilk contraindicated due to current medications. � Meds: Lithium, Penicillamine Domperidone- stimulate lactation 10/31 - Trophic NJ feeds initiated, Vivonex TEN (20 kcal/oz), per high risk protocol 11/02 - ST pulled mediastinal chest tube.
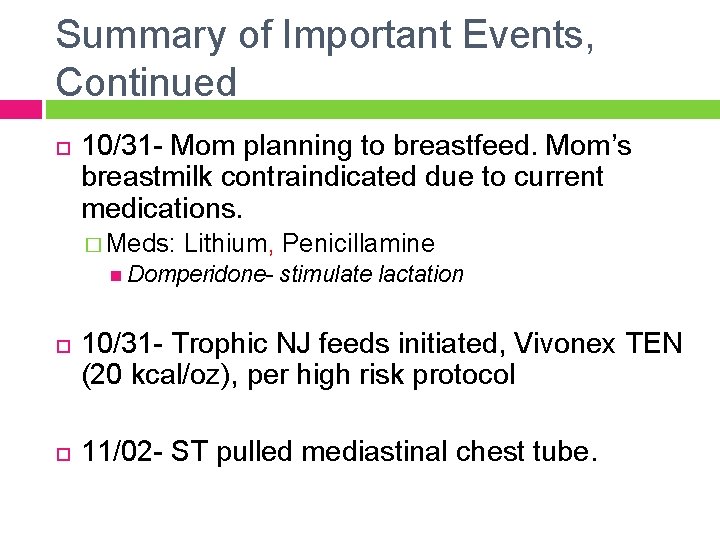
Summary of Important Events, Continued 11/03 - Small bouts of emesis, enteral feeds held at 6 ml/hr, TPN/IL continued 11/04 - Frequent emesis, brown emesis. ST develops NEC (for the second time). � Started on 10 day course of antibiotic treatment. � After antibiotic course planning barium enema to assess for bowel stricture
Necrotizing Enterocolitis 75% of cases in premature infants. Higher incidence in those with cyanotic CHD. 20 -40% mortality rate Pneumatosis intestinalis is a diagnostic of NEC � Treatment- stop feeding immediately, NG suction, TPN/IL and IV fluids, systemic antibiotics � TPN needed while intestine heals Research- When to feed? Breastmilk? Probiotics?
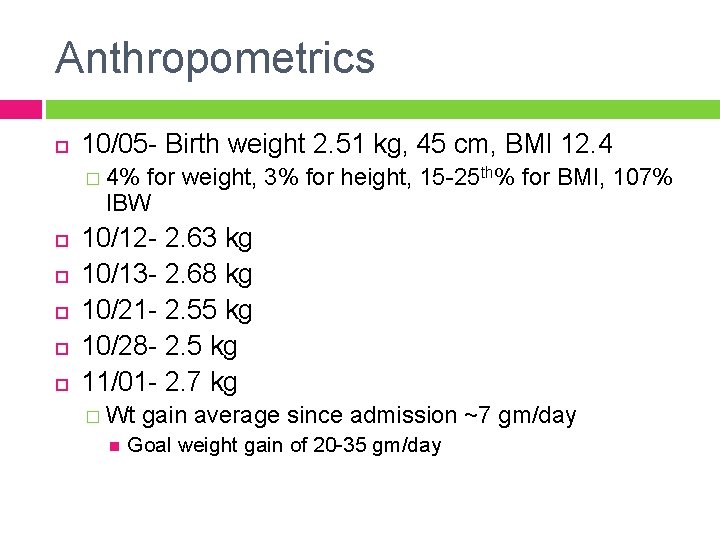
Anthropometrics 10/05 - Birth weight 2. 51 kg, 45 cm, BMI 12. 4 � 4% for weight, 3% for height, 15 -25 th% for BMI, 107% IBW 10/12 - 2. 63 kg 10/13 - 2. 68 kg 10/21 - 2. 55 kg 10/28 - 2. 5 kg 11/01 - 2. 7 kg � Wt gain average since admission ~7 gm/day Goal weight gain of 20 -35 gm/day
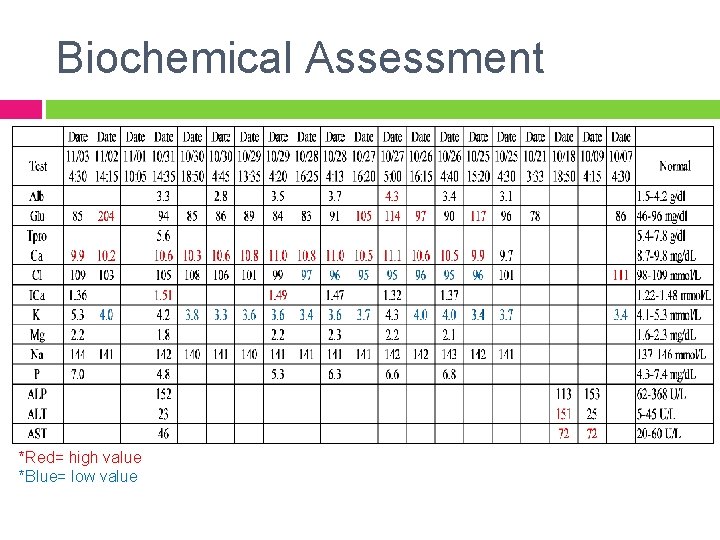
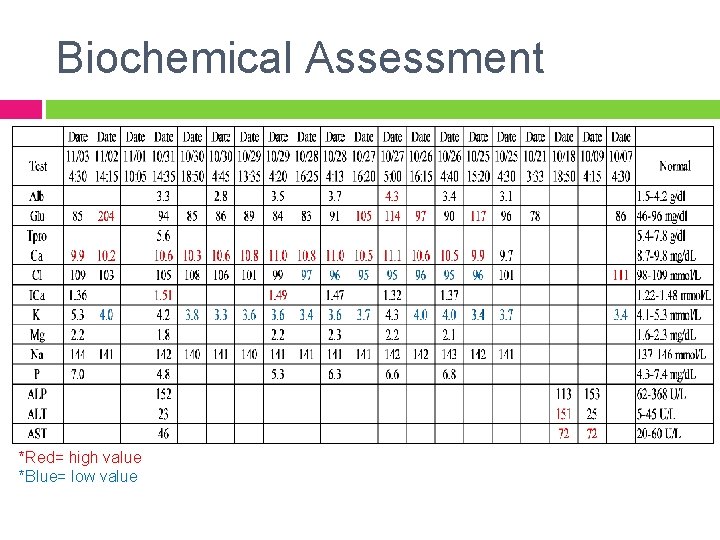
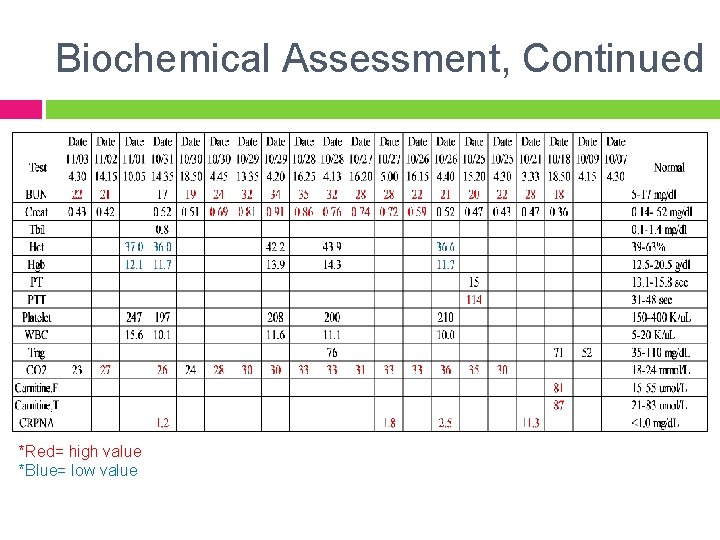
Biochemical Assessment *Red= high value *Blue= low value
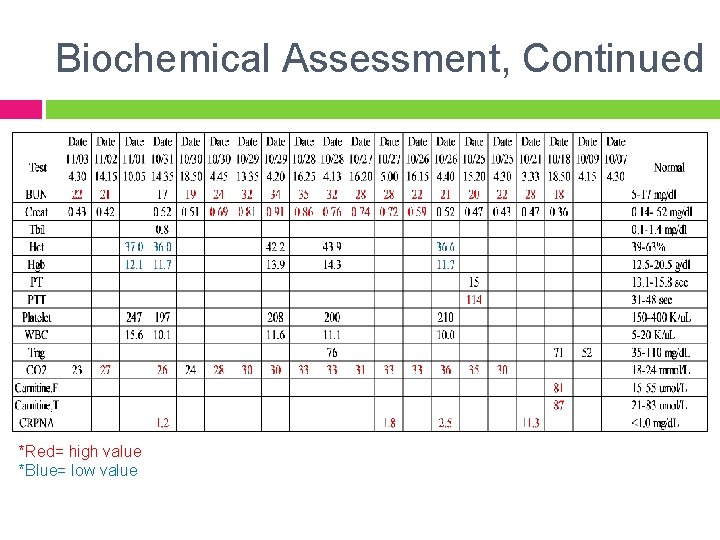
Biochemical Assessment, Continued *Red= high value *Blue= low value
Clinical Observations 11/01 - 27 day old female Extubated Warm, well perfused In mother’s arms Pacifier in mouth
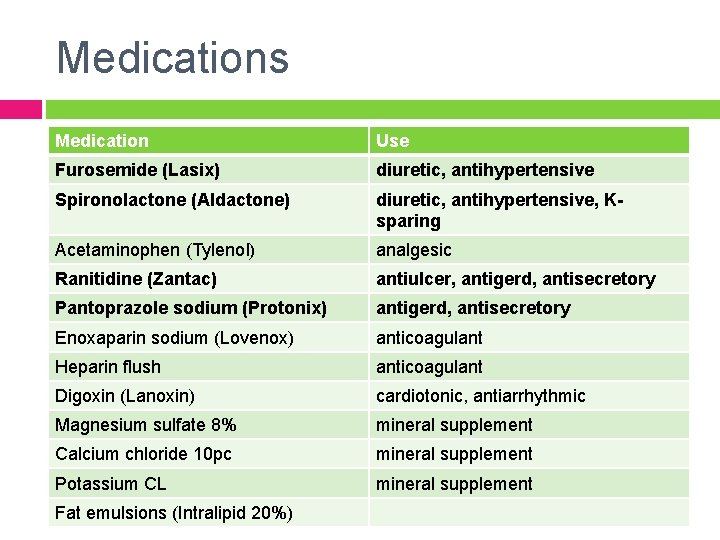
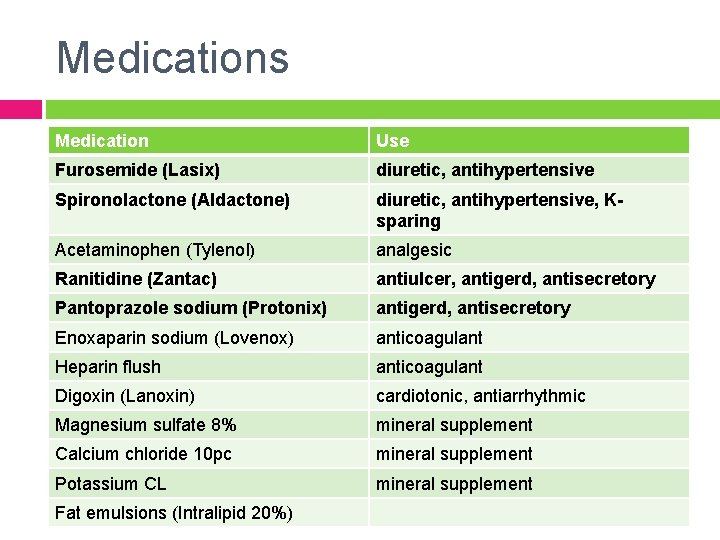
Medications Medication Use Furosemide (Lasix) diuretic, antihypertensive Spironolactone (Aldactone) diuretic, antihypertensive, Ksparing Acetaminophen (Tylenol) analgesic Ranitidine (Zantac) antiulcer, antigerd, antisecretory Pantoprazole sodium (Protonix) antigerd, antisecretory Enoxaparin sodium (Lovenox) anticoagulant Heparin flush anticoagulant Digoxin (Lanoxin) cardiotonic, antiarrhythmic Magnesium sulfate 8% mineral supplement Calcium chloride 10 pc mineral supplement Potassium CL mineral supplement Fat emulsions (Intralipid 20%)
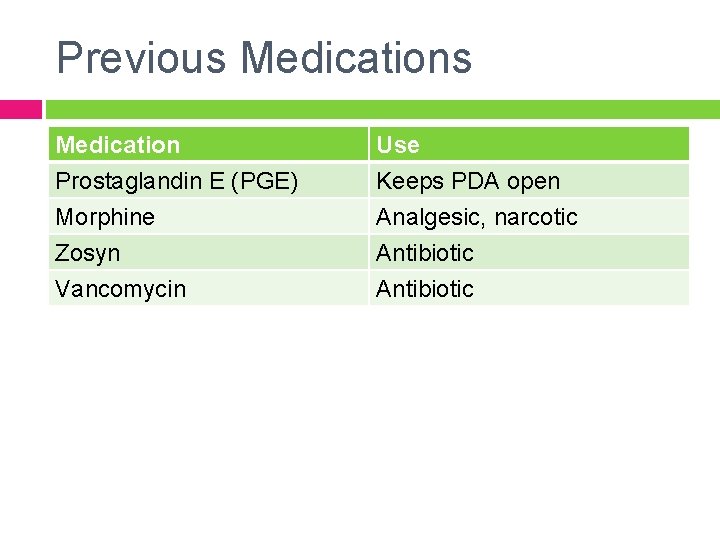
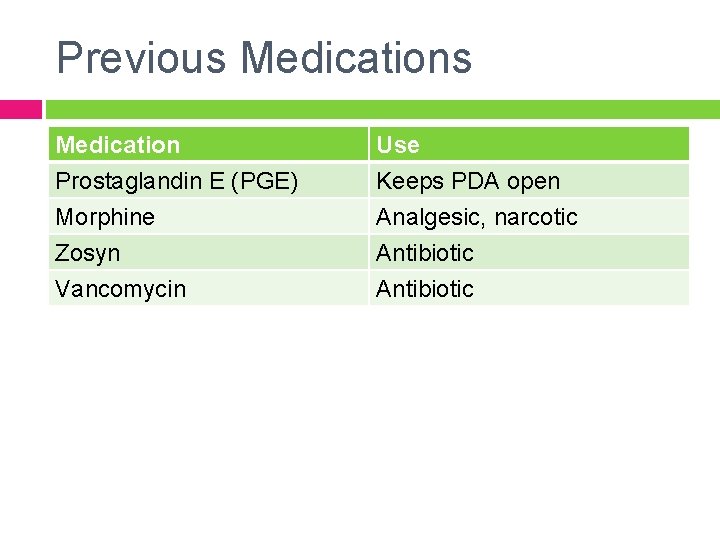
Previous Medication Prostaglandin E (PGE) Morphine Zosyn Use Keeps PDA open Analgesic, narcotic Antibiotic Vancomycin Antibiotic
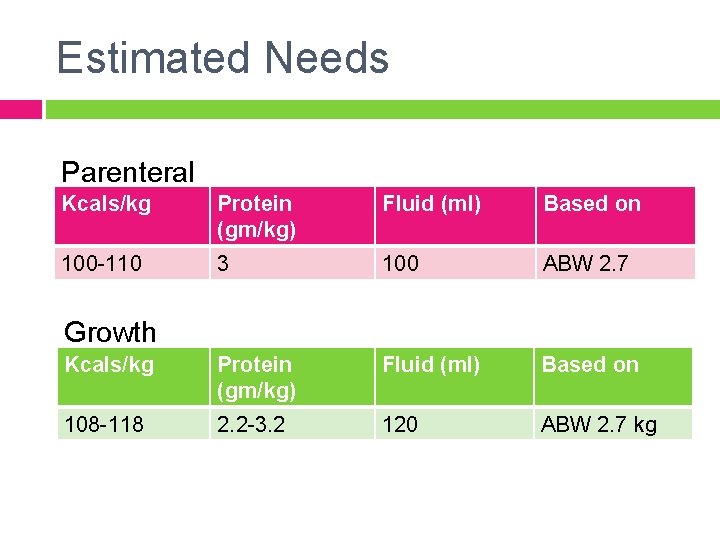
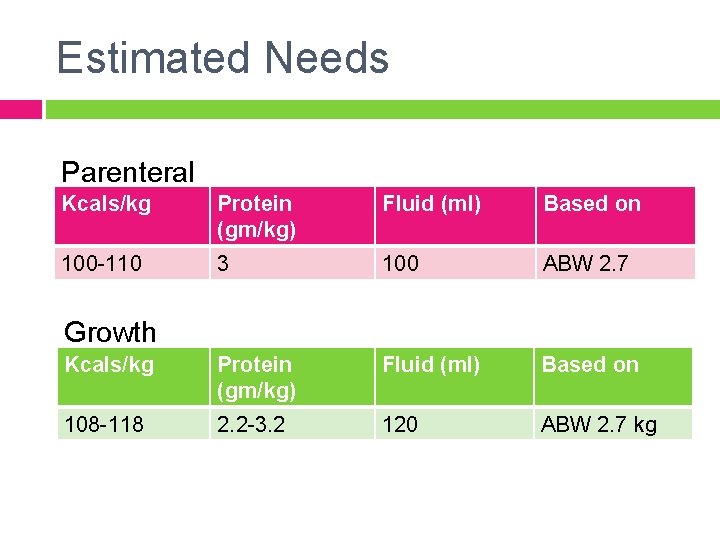
Estimated Needs Parenteral Kcals/kg Protein (gm/kg) Fluid (ml) Based on 100 -110 3 100 ABW 2. 7 Kcals/kg Protein (gm/kg) Fluid (ml) Based on 108 -118 2. 2 -3. 2 120 ABW 2. 7 kg Growth
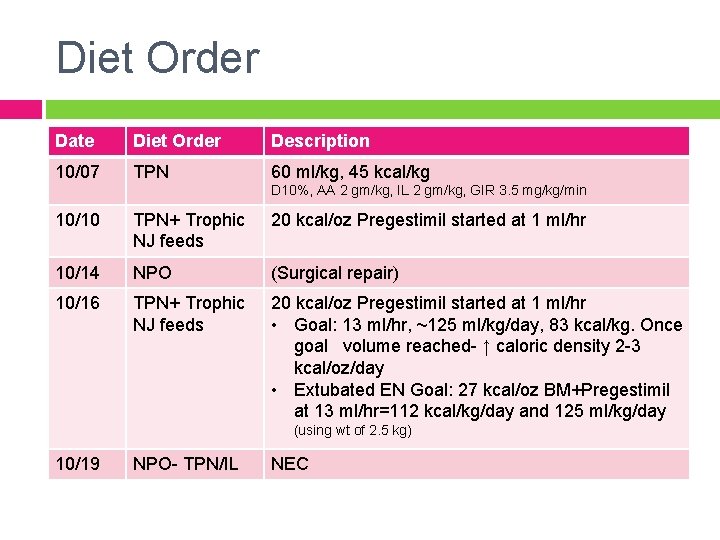
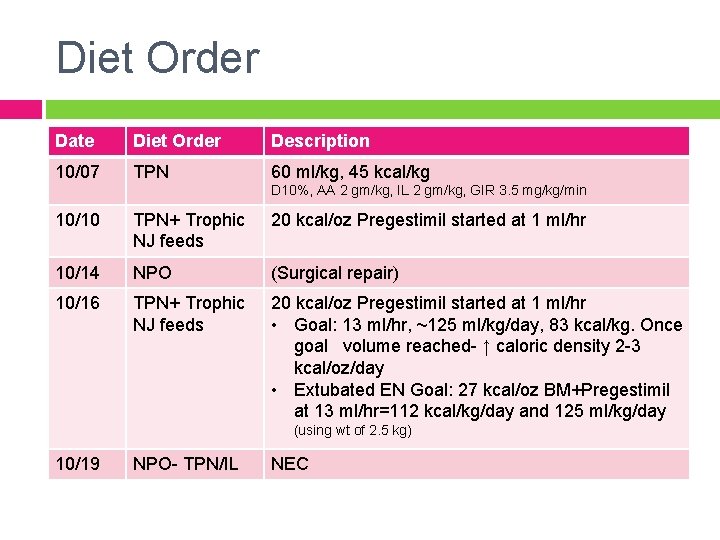
Diet Order Date Diet Order Description 10/07 TPN 60 ml/kg, 45 kcal/kg D 10%, AA 2 gm/kg, IL 2 gm/kg, GIR 3. 5 mg/kg/min 10/10 TPN+ Trophic NJ feeds 20 kcal/oz Pregestimil started at 1 ml/hr 10/14 NPO (Surgical repair) 10/16 TPN+ Trophic NJ feeds 20 kcal/oz Pregestimil started at 1 ml/hr • Goal: 13 ml/hr, ~125 ml/kg/day, 83 kcal/kg. Once goal volume reached- ↑ caloric density 2 -3 kcal/oz/day • Extubated EN Goal: 27 kcal/oz BM+Pregestimil at 13 ml/hr=112 kcal/kg/day and 125 ml/kg/day (using wt of 2. 5 kg) 10/19 NPO- TPN/IL NEC
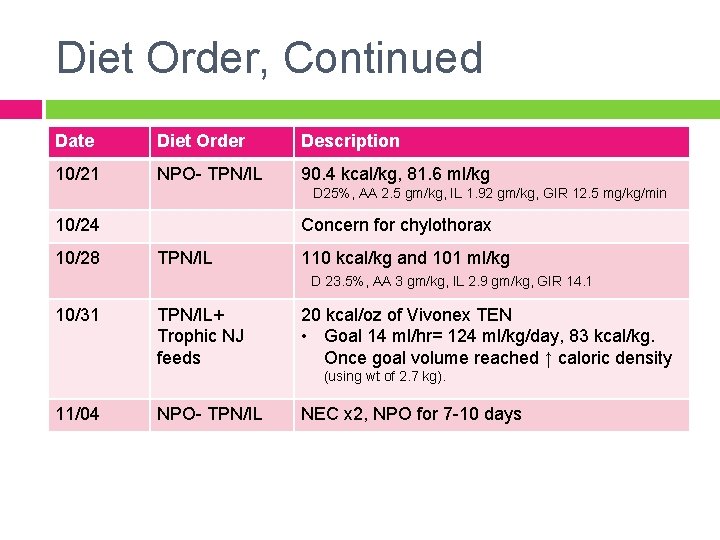
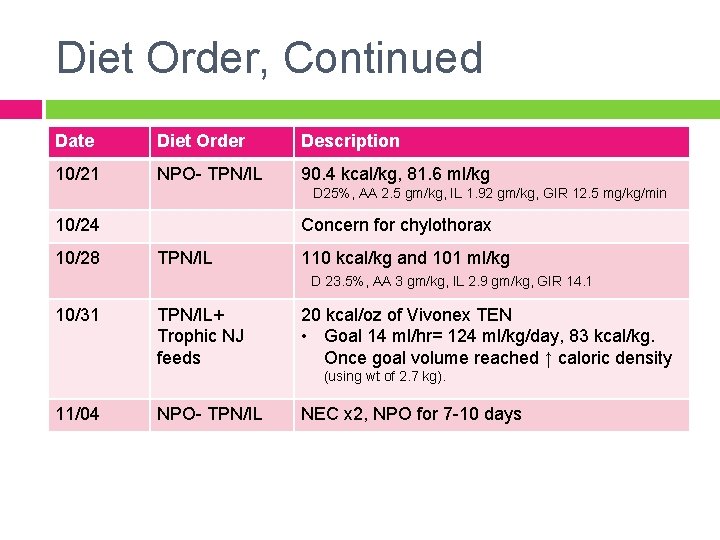
Diet Order, Continued Date Diet Order Description 10/21 NPO- TPN/IL 90. 4 kcal/kg, 81. 6 ml/kg D 25%, AA 2. 5 gm/kg, IL 1. 92 gm/kg, GIR 12. 5 mg/kg/min 10/24 10/28 Concern for chylothorax TPN/IL 110 kcal/kg and 101 ml/kg D 23. 5%, AA 3 gm/kg, IL 2. 9 gm/kg, GIR 14. 1 10/31 TPN/IL+ Trophic NJ feeds 20 kcal/oz of Vivonex TEN • Goal 14 ml/hr= 124 ml/kg/day, 83 kcal/kg. Once goal volume reached ↑ caloric density (using wt of 2. 7 kg). 11/04 NPO- TPN/IL NEC x 2, NPO for 7 -10 days
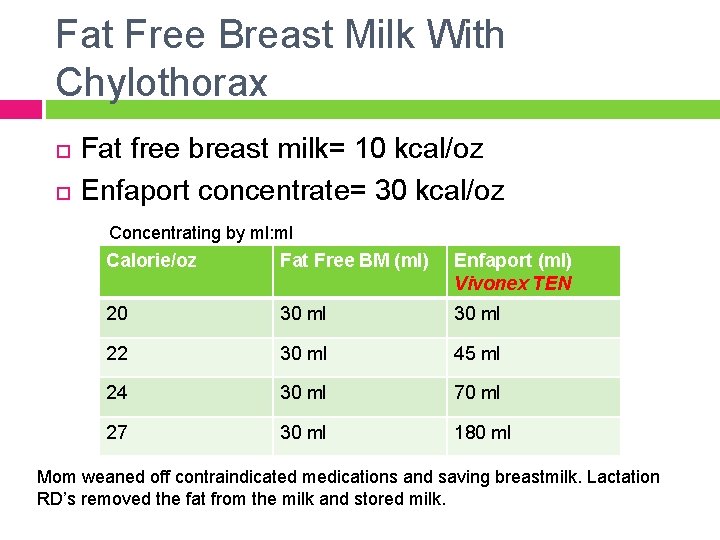
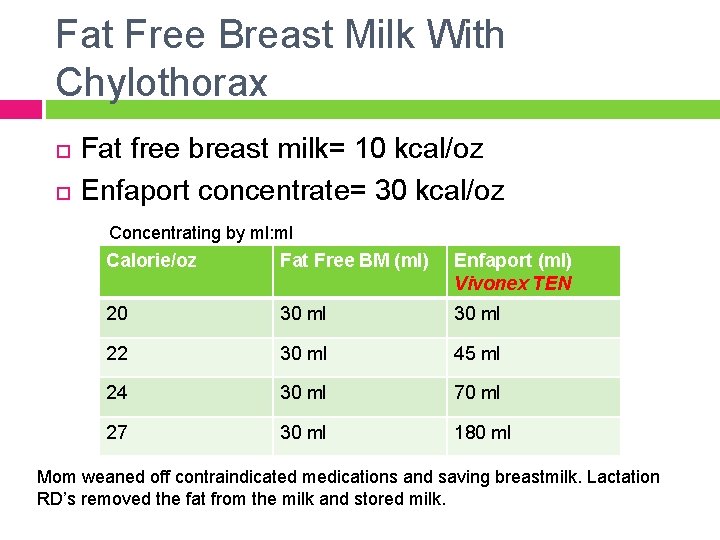
Fat Free Breast Milk With Chylothorax Fat free breast milk= 10 kcal/oz Enfaport concentrate= 30 kcal/oz Concentrating by ml: ml Calorie/oz Fat Free BM (ml) Enfaport (ml) Vivonex TEN 20 30 ml 22 30 ml 45 ml 24 30 ml 70 ml 27 30 ml 180 ml Mom weaned off contraindicated medications and saving breastmilk. Lactation RD’s removed the fat from the milk and stored milk.
Nutrition Care Plan: Assessment 11/01/11 - Current wt 2. 7 kg which is up from wt of 2. 5 kg (10/28) and up from admit wt of 2. 51 kg (10/5). Wt gain since admission has averaged ~7 gm/day which is suboptimal to meet pt's goal of 20 -35 gm/day. Pt started on trophic NG feeds of 20 kcal/oz Vivonex TEN which are ↑ per high risk protocol. Vivonex TEN 20 kcal/oz is an appropriate formula choice at this time as it is elemental and low fat. This is appropriate given pt's history of NEC and chylothorax. Pt reported to be tolerating EN feeds. No stool output doc’d 10/31/11. � � Noted lactation services have met with pt's mother and noted that the use of mother's milk or breastfeeding is not recommended while mother is taking current medications. Labs reviewed. Urine Iodine level 1529 mcg/L. Discussed with Pharmacy given pt's urine iodine level, no adjustments needed in patient's TPN at this time.
Nutrition Care Plan: Diagnosis Inadequate oral intake related to NEC and cardiac surgery as evidenced by need for TPN/IL and NG feeds for nutrition support
Nutrition Care Plan: Goal To provide age/condition appropriate nutrition to support weight gain of 20 -35 gm/day
Nutrition Care Plan: Interventions 1. 2. Enteral formula- NG feeds of 20 kcal/oz Vivonex TEN running at 2 ml/hour provides patient 12 kcal/kg/day, 18 ml/kg/day and 0. 4 gm/kg/day protein using weight of 2. 7 kg Parenteral formula- TPN/IL: (to start this evening) D 24%, AA 2. 5 gm/kg, IL 2. 88 gm/kg, GIR 9. 6 mg/kg/min, 72 ml/kg, 85. 8 kcal/kg
Nutrition Care Plan: Recommendations Continue to advance pt's EN feeds per high risk protocol to goal of 14 ml/hour= 124 ml/kg/day using wt of 2. 7 kg. Once goal volume reached, ↑ caloric density of pt's formula per high risk protocol to closer meet pt's estimated energy needs for growth. Once patient's TPN is d/c, if patient continues on the Vivonex TEN formula would recommend addition of a daily MVI. TPN/IL monitoring: Daily BMP, ICa, Mg, Phos. Weekly LFTs and TG.
Recommendations, Continued Adjust nutrition provision as medically able to promote weight gain of 20 -35 gm/day. Wean TPN/IL as enteral feeds advance. Lactation services available to patient's mother prn. Daily weights as medically able.
Summary As of November 4, 2011 infant ST was still a patient in the CICU at PCMC. ST had developed NEC for the second time and was made NPO on TPN/IL and was to continue on a low fat diet for chylothorax. � She would receive a 10 day course of antibiotic therapy and then be evaluated for a bowel stricture via barium enema. Gut perfusion/heart function would be evaluated for risk of NEC. Upon re-feeding ST was planned to receive BM/Vivonex TEN at 20 kcal/oz. ST was screened as a high nutrition risk patient and her prognosis was fair.
References Panthongviriyakul C, Bines JE. Post-operative chylothorax in children: An evidence-based management algorithm. J of Paediatrics and Child Health. 2008; 44: 716 -721. Chalret du Rieu M, Mabrut J-Y. Management of postoperative chylothorax. Journal of Visceral Surgery. 2011; doi: 10. 1016/j. jviscsurg. 2011. 09. 006 Chan GM, Lechtenberg E. The use of fat-free human milk in infants with chylous pleural effusion. Journal of Perinatology. 2007; 27: 434 -436. Biewer ES, Zurn C, Arnold R, et al. Chylothorax after surgery on congenital heart disease in newborns and infants- risk factors and efficacy of MCT-diet. Journal of Cardiothoracic Surgery. 2010; 5: 127 -134. Soto-Martinez M, Massie J. Chylothorax: Diagnosis and Management in Children. Paediatric Respiratory Reviews. 2009; 10: 199 -207. Samour PQ, King K, eds. Handbook of Pediatric Nutrition. 3 rd ed. Sudbury, MA: Jones and Bartlett Publishers; 2005. The Merck Manual of Diagnosis and Therapy. 18 th ed. Whitehouse Station, NJ: Merck and Co; 2006.