Nutrition support and tube feeding a dietitians perspective
Nutrition support and tube feeding: a dietitian’s perspective Amy Guppy Specialist Home Enteral Nutrition (HEN) Dietitian for children Lewisham and Greenwich NHS Trust May 2018
What will we cover? § § § Paediatric HEN team Indications for nutrition support Strategies prior to tube feeding Feeding tubes and feed types Tube weaning Case study
Paediatric HEN team § Support and monitoring of all children living at home with enteral tube feeding in Lewisham, Lambeth and Southwark § Multi Disciplinary Team (MDT) community working § Working closely with Speech and Language Therapists

Indications for nutrition support Inadequate intake +/Increased requirements Increased losses Failure to absorb/utilise Oral motor dysfunction, Unsafe swallow, Food aversion, Poor appetite, Tumours

Increased requirements Failure to absorb/utilise Increased energy needs Prematurity Chronic lung disease Congenital heart disease Weight catch up after illness Major surgery Cystic Fibrosis Short bowel syndrome Inborn Errors of Metabolism Food allergy Increased losses GORD Excessive burns Inflammatory bowel disease
Dietetic strategies prior to tube feeding Infants § High energy infant formula e. g. Infatrini § Concentrate infant formula § Manage reflux Children § High energy, high protein foods § Modified food / fluid consistencies § Food fortification § Oral nutritional supplements
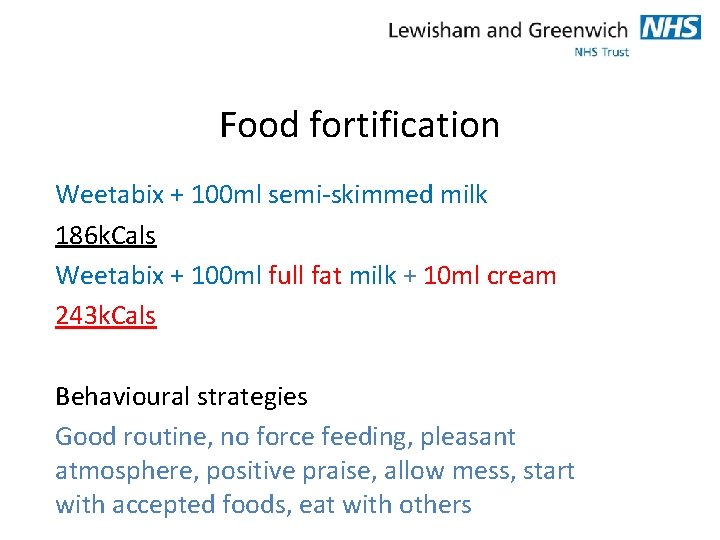
Food fortification Weetabix + 100 ml semi-skimmed milk 186 k. Cals Weetabix + 100 ml full fat milk + 10 ml cream 243 k. Cals Behavioural strategies Good routine, no force feeding, pleasant atmosphere, positive praise, allow mess, start with accepted foods, eat with others
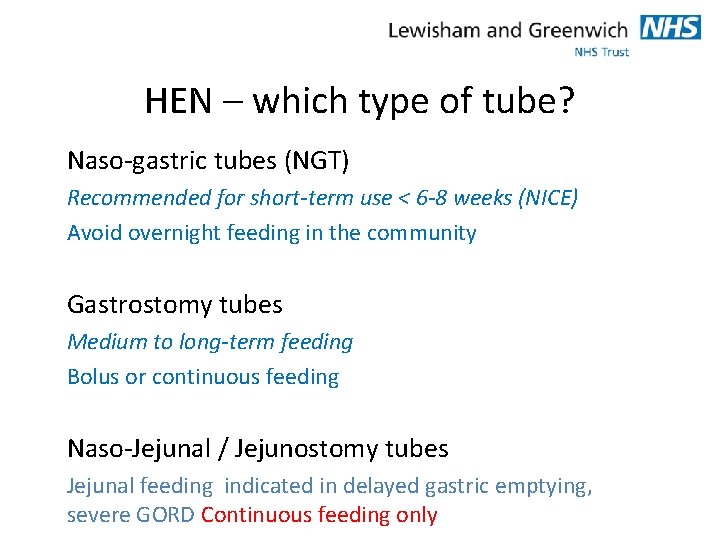
HEN – which type of tube? Naso-gastric tubes (NGT) Recommended for short-term use < 6 -8 weeks (NICE) Avoid overnight feeding in the community Gastrostomy tubes Medium to long-term feeding Bolus or continuous feeding Naso-Jejunal / Jejunostomy tubes Jejunal feeding indicated in delayed gastric emptying, severe GORD Continuous feeding only
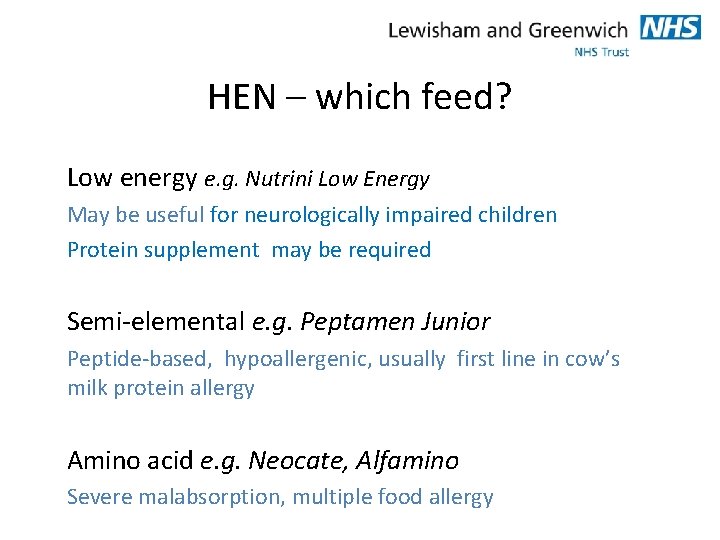
HEN – which feed? Low energy e. g. Nutrini Low Energy May be useful for neurologically impaired children Protein supplement may be required Semi-elemental e. g. Peptamen Junior Peptide-based, hypoallergenic, usually first line in cow’s milk protein allergy Amino acid e. g. Neocate, Alfamino Severe malabsorption, multiple food allergy
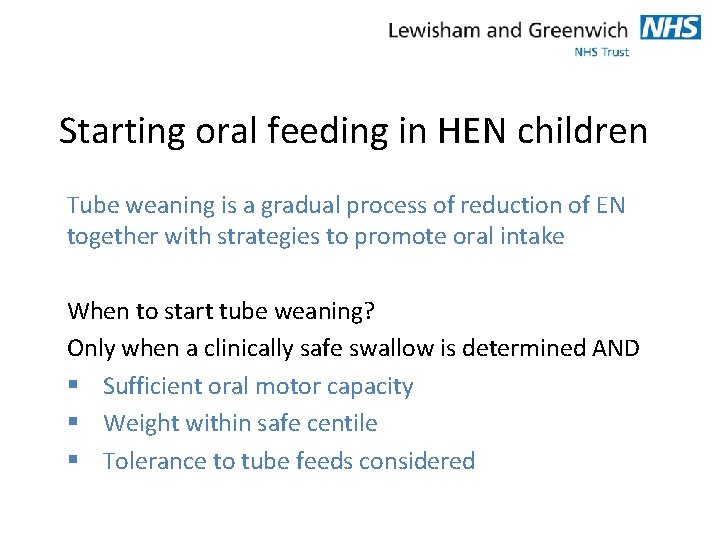
Starting oral feeding in HEN children Tube weaning is a gradual process of reduction of EN together with strategies to promote oral intake When to start tube weaning? Only when a clinically safe swallow is determined AND § Sufficient oral motor capacity § Weight within safe centile § Tolerance to tube feeds considered

Starting oral feeding in HEN children Possible oral feeding barriers Lack of motivation for oral feeding / understanding of hunger Dietitian strategies Establish appropriate feeding schedule, establish appropriate calories/fluid, use of high energy feeds, offer oral feeding before tube feeds Lack of feeding skills / oral or Oral stimulation, introduce food feeding aversion related activities, messy play, taste experiences, manage reflux

Tube removal… EN can be stopped if weight gain/ growth is appropriate and oral intake meets nutrition and hydration requirements Longer term feeding tubes § Keep in-situ for at least a season (4 -6 months) § Aim to maintain weight during periods of illness (winter) and aim to maintain hydration (summer) without use of the tube

Case study – Background ‘Baby O’ born at 38+3 weeks with a diagnosis of Congenital left hydroephrosis, central hypotonia, ventrical septal defect Under Neurology and Cardiology teams Discharged from Neonatal unit (age 3 weeks) established on full bottle feeds

Baby O – 11 weeks Referral made from SLT to Complex Needs Dietitian Reason for referral: § Slow weight gain (dropped to <0. 4 th centile from 2 nd centile) § Avoidant feeding behaviours § Prolonged feed times, not finishing bottle feeds
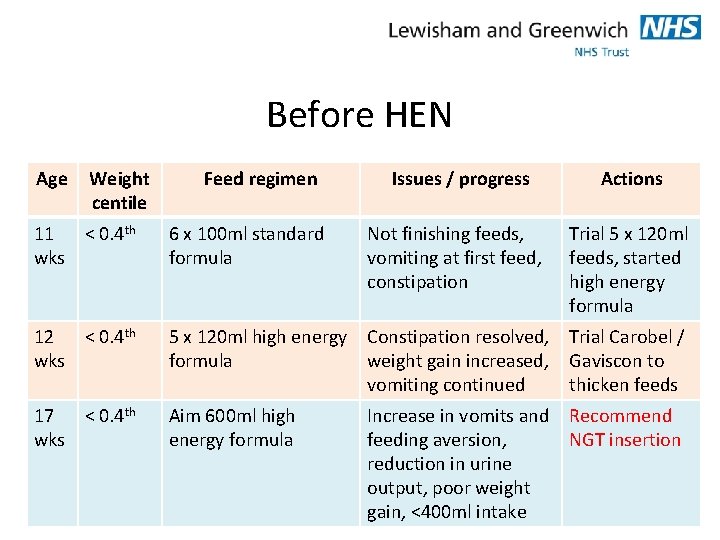
Before HEN Age Weight centile Feed regimen Issues / progress Not finishing feeds, vomiting at first feed, constipation Actions 11 < 0. 4 th wks 6 x 100 ml standard formula 12 < 0. 4 th wks 5 x 120 ml high energy Constipation resolved, formula weight gain increased, vomiting continued Trial Carobel / Gaviscon to thicken feeds 17 < 0. 4 th wks Aim 600 ml high energy formula Recommend NGT insertion Increase in vomits and feeding aversion, reduction in urine output, poor weight gain, <400 ml intake Trial 5 x 120 ml feeds, started high energy formula
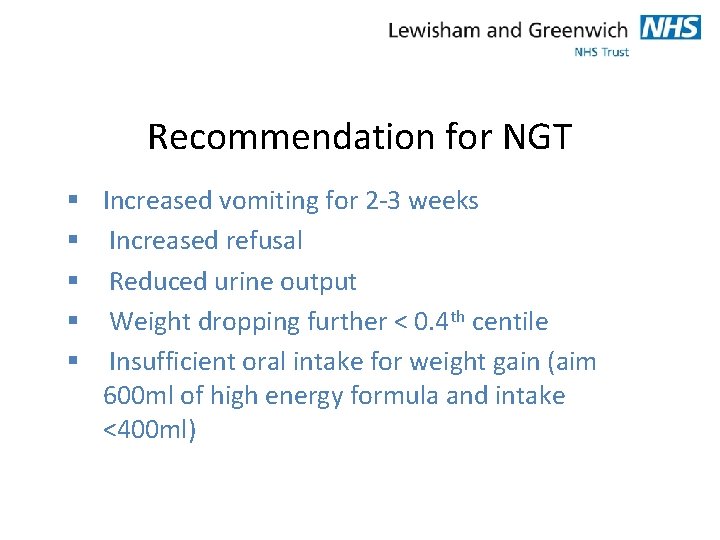
Recommendation for NGT § Increased vomiting for 2 -3 weeks § Increased refusal § Reduced urine output § Weight dropping further < 0. 4 th centile § Insufficient oral intake for weight gain (aim 600 ml of high energy formula and intake <400 ml)

During HEN Age Weight centile Issues/progress Actions 19 wks <0. 4 th Frequent vomiting, optimal antireflux meds prescribed, prolonged oral feed times (1. 5 hrs) Trial AA feed Start slow dairy free weaning 30 minute oral feeds + NG top up 24 wks 2 nd Slight reduction in vomits, rapid weight gain, oral feeds taking 1 hour, baby rice 1/day Reduce feed volume, 6 x 135 ml feeds, offer puree 2/day, maximum 40 minutes oral feeds 28 wks 0. 4 th-2 nd Oral feeds <45 minutes, some NG top ups, giving NG feed at night as not waking, baby rice and F+V Stop night feed, 5 x 135 ml feeds, increase concentration 32 wks 0. 4 th-2 nd Mainly oral feeds with occasional NGT top up of ~30 ml and full NG feed 1/week, vomits 1 -2/day Increase feed concentration, 45 minute feeds, optimise anti-reflux meds, tube out 35 wks Manging oral feeds but Mum concerned with feed spillage, well hydrated, oral puree 3/day Assess weight before reinserting tube, food fortification (dairy free) 0. 4 th-2 nd

§ § Trial AA feed Vomiting ½ of all feeds Poor weight – already <0. 4 th centile Gradual 120 ml → 160 ml x 6 feeds Wean dairy free to minimise any chance of reflux Trial NGT out § Weight within safe centile § Reduced use of tube § ↑ oral aversion with tube in

HEN last review – 36 weeks NGT to remain out § Continued weight gain § Well hydrated § Feed times 20 -45 minutes § Continue food fortification of 3 meals/day § Refer back to Complex Needs Dietitian
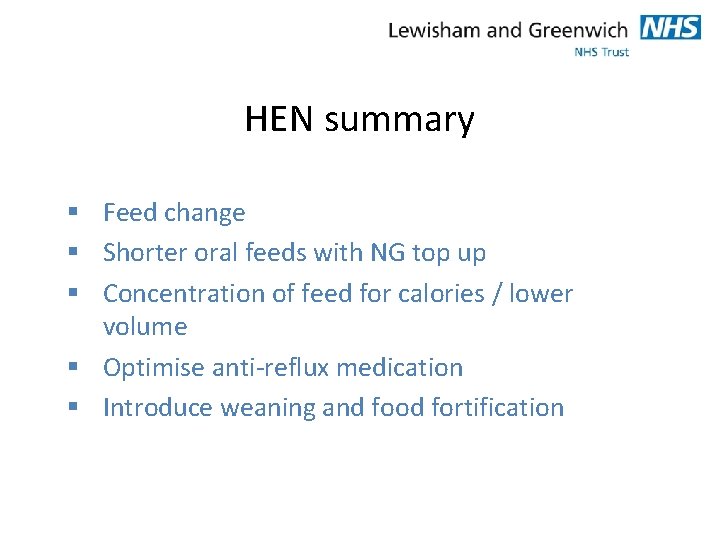
HEN summary § Feed change § Shorter oral feeds with NG top up § Concentration of feed for calories / lower volume § Optimise anti-reflux medication § Introduce weaning and food fortification

Baby O after HEN § Continues joint Dietitian / SLT reviews § Remains on anti reflux medication § Remains on Amino Acid formula Recent allergy testing negative Intervention Reintroducing cow’s milk products, continues food fortification, messy play, aiming to increase food textures and offering finger foods…
Thank you for listening
- Slides: 22