Nutrition in Care Homes for People with Diabetes

Nutrition in Care Homes for People with Diabetes Kurt Maloney, Specialist Dietitian Bradford Nutrition & Dietetic Department St Luke’s Hospital
Objectives �Identify the CQC regulation for nutrition & hydration �Discuss the dietary management of diabetes �Introduction to dietary advice for overweight & malnourished patients �Outline the importance of screening for malnutrition with examples
Regulation 14: Meeting nutritional & hydration needs (2014) �People must have enough to eat & drink to meet their needs �People must have nutritional needs assessed & food provided to meet their individual needs �Must receive support with nutrition & hydration if needed
�Provide a variety of nutritious & appetising food �Appropriate temperature �Culturally appropriate �Preference & choice �Prompts, encouragement, eating aids �Follow prescribing plan for supplements �Regular assessment of needs �Staff should know when specialist nutritional advice is needed & how to refer
Regulation 14: Meeting nutritional & hydration needs (2014) �When avoidable harm or exposure to significant risk of harm is identified…. �CQC can prosecute for breach of regulation 14 without serving a warning notice �CQC will refuse registration if providers cannot provide evidence of compliance
Dietary Advice for Diabetes
Points to consider… �Priority of the person’s diabetes management �Individualised assessment & treatment �No ‘one size fits all’ approach �Diagnosis, prognosis & quality of life �Social aspects of eating �Pleasure from eating �Respect individuals’ choices
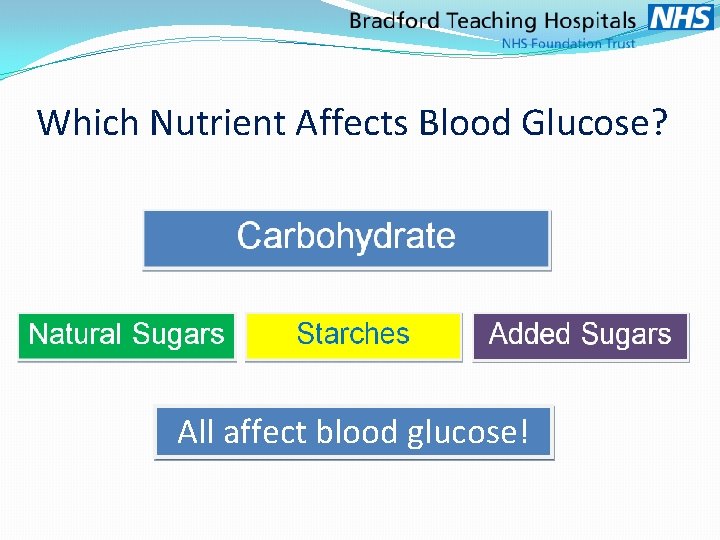
Which Nutrient Affects Blood Glucose? All affect blood glucose!
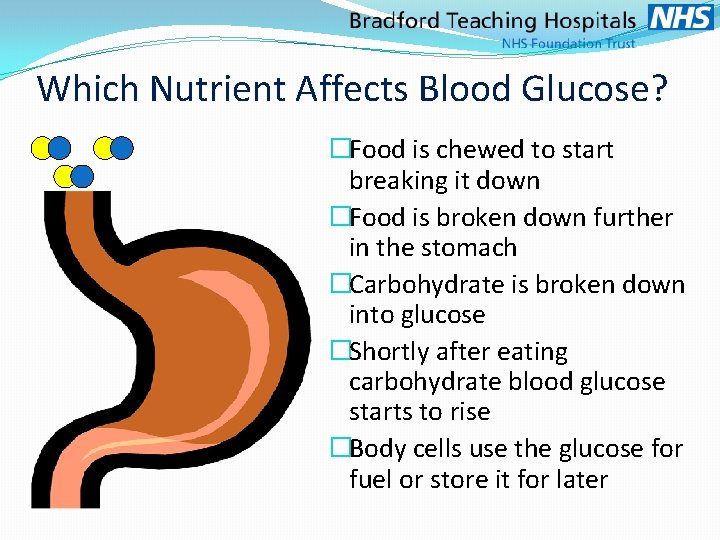
Which Nutrient Affects Blood Glucose? �Food is chewed to start breaking it down �Food is broken down further in the stomach �Carbohydrate is broken down into glucose �Shortly after eating carbohydrate blood glucose starts to rise �Body cells use the glucose for fuel or store it for later
Why is Diet Important? Major influence on diabetes management & health �Blood glucose control �Long & short term complications �Body fat and insulin resistance �Risk of other diet related diseases �Vitamins, Minerals, Protein & Fats are essential for good health
Diet Myths – True or False �People with diabetes shouldn't have: �Bananas, grapes, melon & mango �Sweet foods and puddings �Lots of sugary drinks �People with diabetes should: �Use diabetic products �Always snack between meals �Follow a ‘special’ or ‘diabetic’ diet

Healthy Eating
Healthy Eating in Care Homes �Regular & Balanced Meals �Portion control �Healthy menu planning & cooking �Appetising meals & variety �Healthier snack & pudding options �Limit processed or ‘junk’ foods �Avoid sugary drinks & added sugars �Occasional ‘treat’ foods are fine
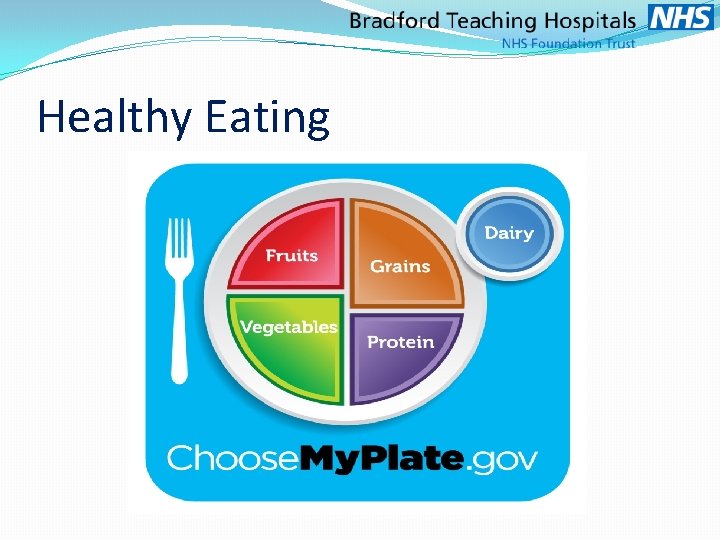
Healthy Eating
How much is important �Regular meals spreads carbs out �Avoid added sugars & sugary food/drinks �Fruit & fruit juices �Don’t double up on starches �Smaller portions of puddings The type is also important �Porridge, basmati rice, new potatoes, seeded bread, whole grain starches & cereals
Weight Management Simple Tips for weight management in care settings �Regular Meals �Portion Control – even healthy food can affect weight! �Healthy, tasty menu choices and healthy snack options �Healthier puddings & desserts or small portions �Avoid added sugars (drinks & foods) �Non restrictive approach with occasional ‘treat’ foods Simple swaps and small changes �Swap Chocolate pudding for chocolate Muller light �Swap Shortcake biscuits for rich tea �Change drinks to diet, sugar free, no added sugar �Swap sugar for sweeteners
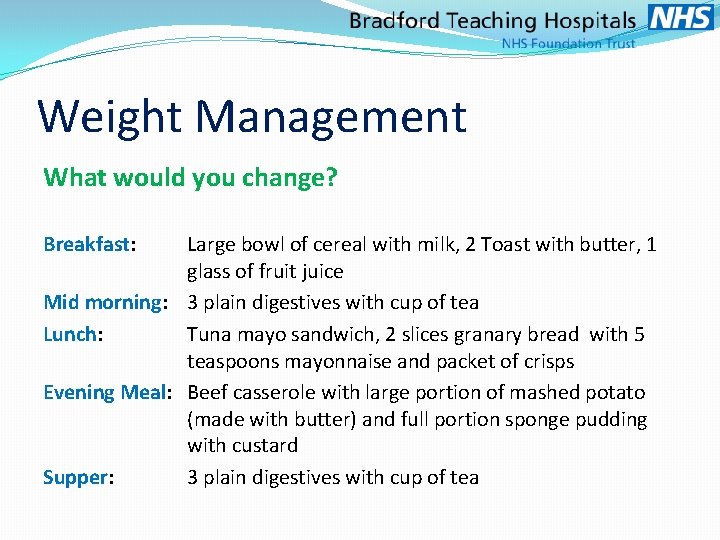
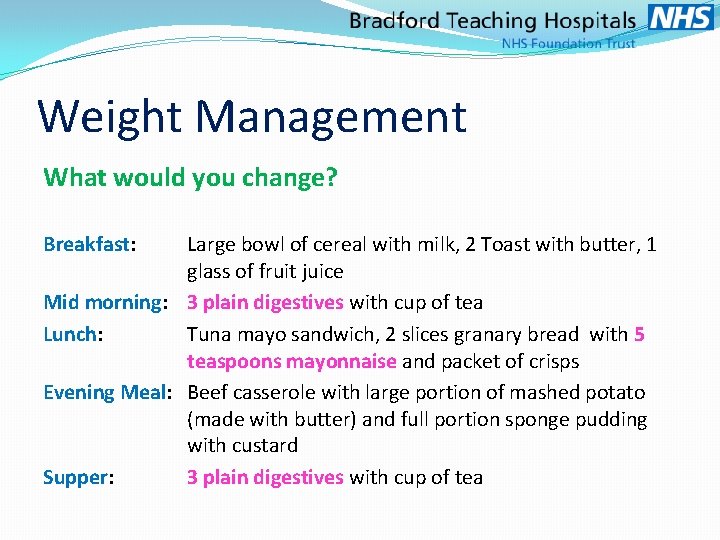
Weight Management What would you change? Breakfast: Large bowl of cereal with milk, 2 Toast with butter, 1 glass of fruit juice Mid morning: 3 plain digestives with cup of tea Lunch: Tuna mayo sandwich, 2 slices granary bread with 5 teaspoons mayonnaise and packet of crisps Evening Meal: Beef casserole with large portion of mashed potato (made with butter) and full portion sponge pudding with custard Supper: 3 plain digestives with cup of tea
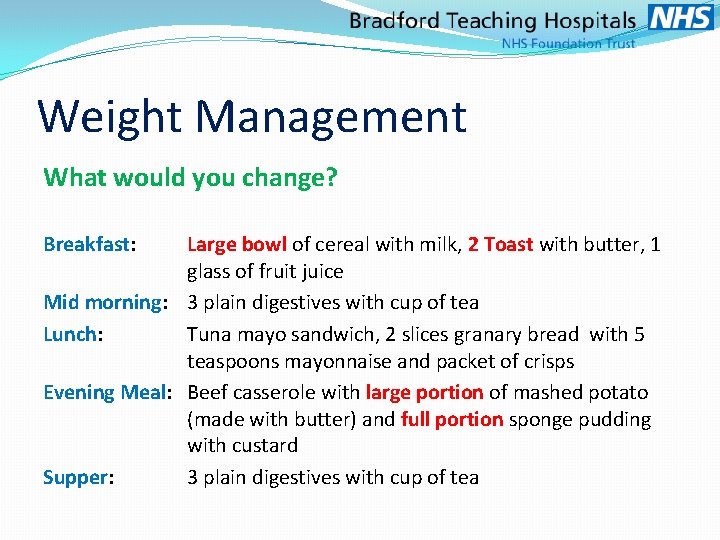
Weight Management What would you change? Breakfast: Large bowl of cereal with milk, 2 Toast with butter, 1 glass of fruit juice Mid morning: 3 plain digestives with cup of tea Lunch: Tuna mayo sandwich, 2 slices granary bread with 5 teaspoons mayonnaise and packet of crisps Evening Meal: Beef casserole with large portion of mashed potato (made with butter) and full portion sponge pudding with custard Supper: 3 plain digestives with cup of tea
Weight Management What would you change? Breakfast: Large bowl of cereal with milk, 2 Toast with butter, 1 glass of fruit juice Mid morning: 3 plain digestives with cup of tea Lunch: Tuna mayo sandwich, 2 slices granary bread with 5 teaspoons mayonnaise and packet of crisps Evening Meal: Beef casserole with large portion of mashed potato (made with butter) and full portion sponge pudding with custard Supper: 3 plain digestives with cup of tea
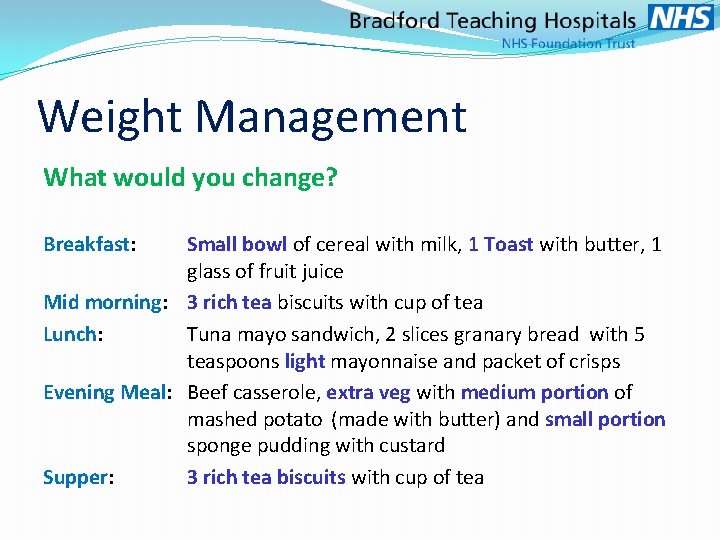
Weight Management What would you change? Breakfast: Small bowl of cereal with milk, 1 Toast with butter, 1 glass of fruit juice Mid morning: 3 rich tea biscuits with cup of tea Lunch: Tuna mayo sandwich, 2 slices granary bread with 5 teaspoons light mayonnaise and packet of crisps Evening Meal: Beef casserole, extra veg with medium portion of mashed potato (made with butter) and small portion sponge pudding with custard Supper: 3 rich tea biscuits with cup of tea
Weight Management Reducing the portions with some simple swaps saves approximately 900 - 1000 calories per day!
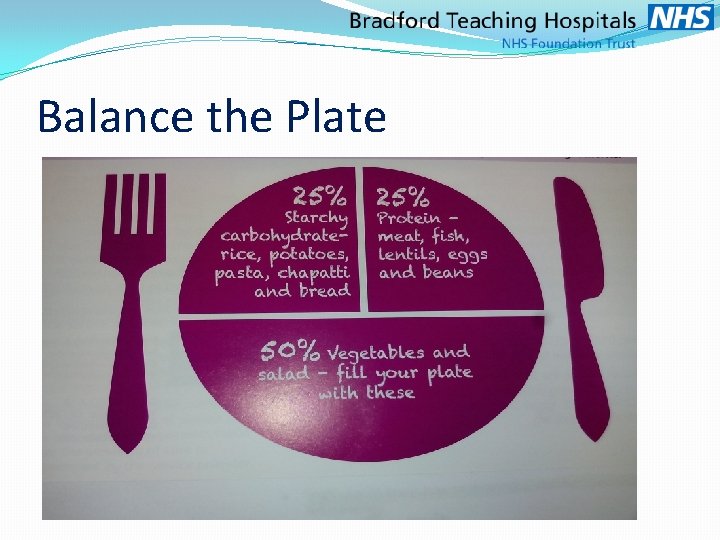
Balance the Plate
Malnutrition ‘The nutritional intake does not meet the person’s needs’
Malnutrition �The priority is getting the patient to eat �At this stage healthy eating is not a priority �Aim to provide nutritious foods which are high in calories & protein �Control Blood glucose with medications during this period
Consequences of malnutrition • Poor wound healing and higher risk of infections • Frequent hospital admissions • Muscle wasting, Lack of energy/Depression • Dehydration • Vitamin and mineral deficiencies
Recognising Malnutrition • Mobility: weakness, impaired movement • Mood: apathy, lethargy, poor concentration • Current intake: reduced appetite, changes in meal pattern and food choice • Physical appearance: loose clothing, rings or dentures, sunken eyes, dry mouth, emaciation, pale complexion, hair loss • Screening tools: e. g. MUST
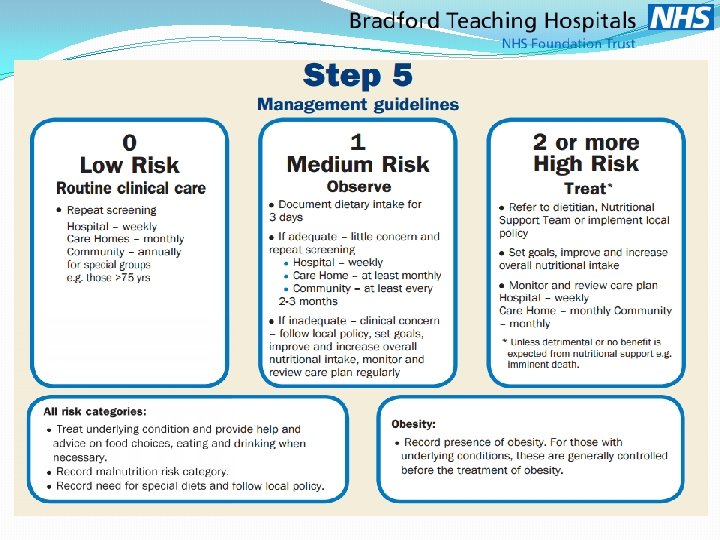
Nutritional Screening
Why Screen for malnutrition? • Early identification of patients at risk • Early intervention • When repeated weekly allows monitoring where nutritional care plans in place • Audit practice

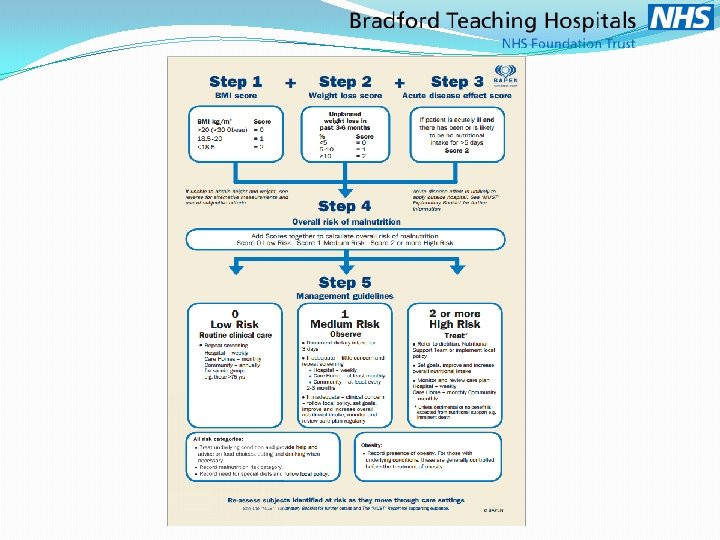
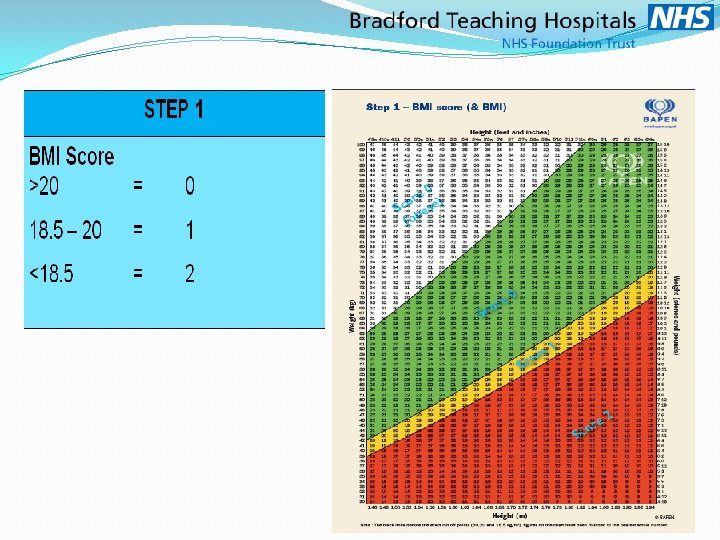
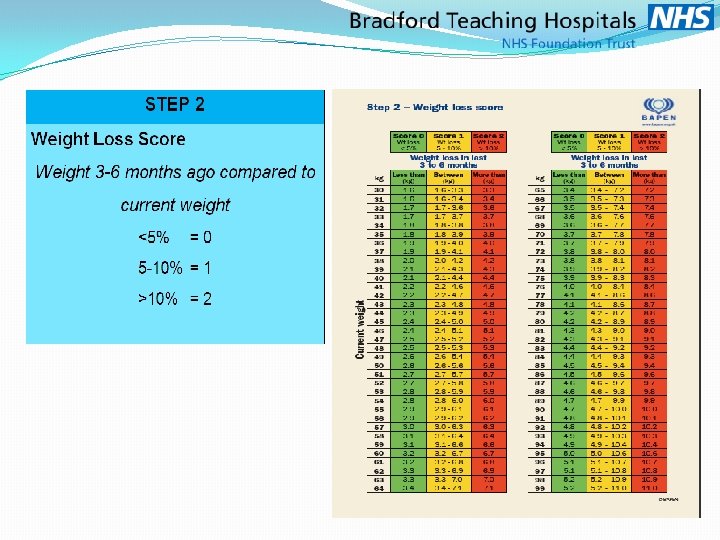
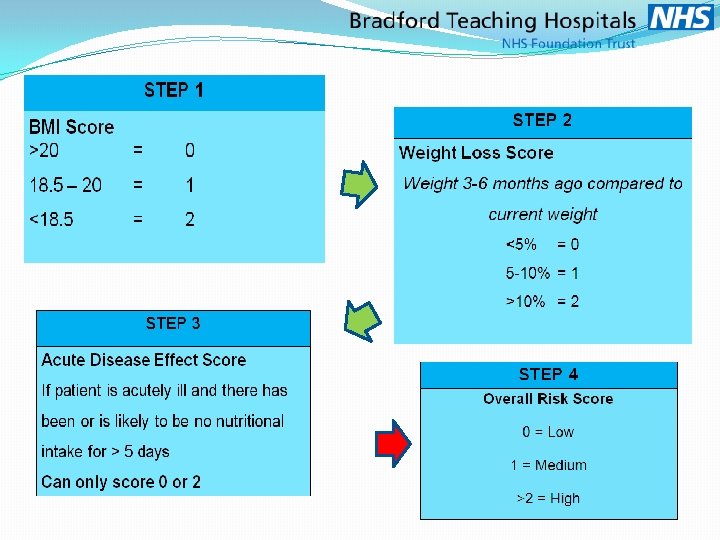
‘MUST’
Benefits of using MUST • Easy to use, rapid and reproducible • Any care worker can be trained to use ‘MUST’ • Can be used with patients who can’t be weighed and measured • Available on line from www. bapen. org, as well as paper format in a variety of sizes
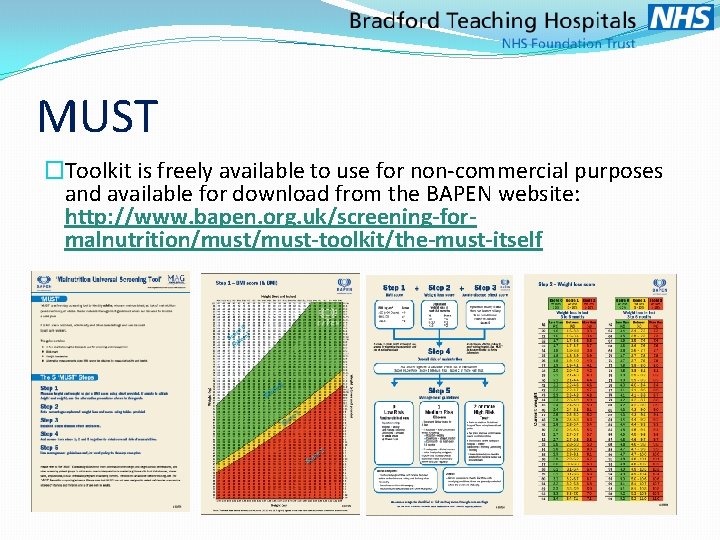
MUST �Toolkit is freely available to use for non-commercial purposes and available for download from the BAPEN website: http: //www. bapen. org. uk/screening-formalnutrition/must-toolkit/the-must-itself
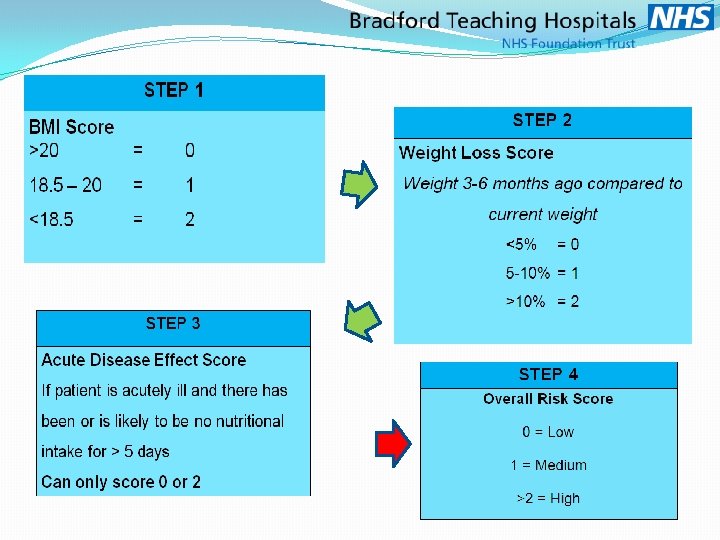
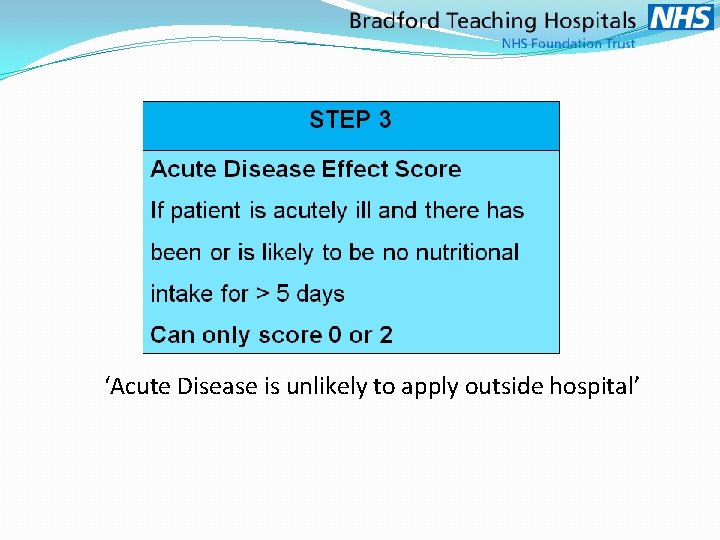
‘Acute Disease is unlikely to apply outside hospital’
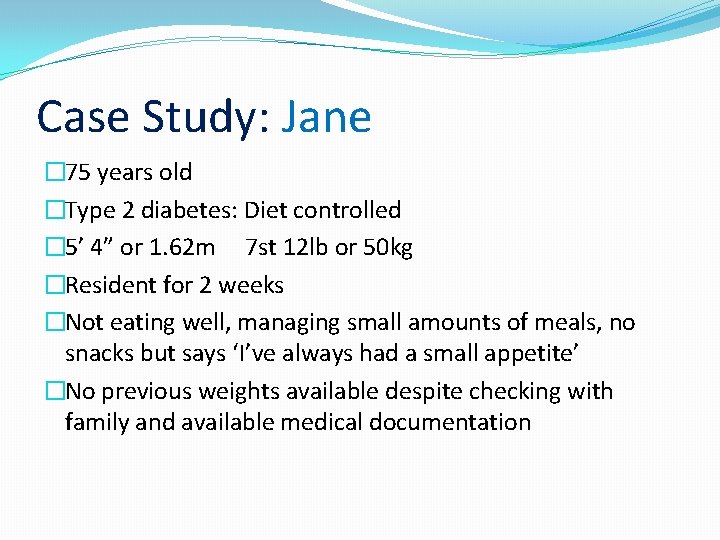
Case Study: Jane � 75 years old �Type 2 diabetes: Diet controlled � 5’ 4” or 1. 62 m 7 st 12 lb or 50 kg �Resident for 2 weeks �Not eating well, managing small amounts of meals, no snacks but says ‘I’ve always had a small appetite’ �No previous weights available despite checking with family and available medical documentation
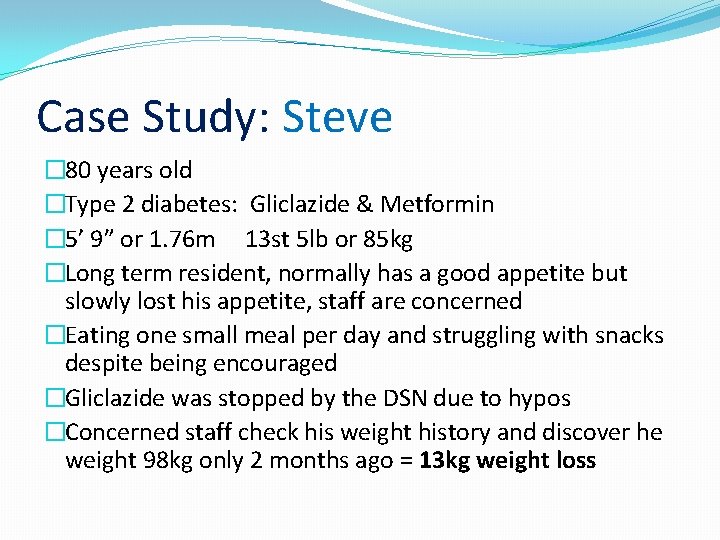
Case Study: Steve � 80 years old �Type 2 diabetes: Gliclazide & Metformin � 5’ 9” or 1. 76 m 13 st 5 lb or 85 kg �Long term resident, normally has a good appetite but slowly lost his appetite, staff are concerned �Eating one small meal per day and struggling with snacks despite being encouraged �Gliclazide was stopped by the DSN due to hypos �Concerned staff check his weight history and discover he weight 98 kg only 2 months ago = 13 kg weight loss
Treating Malnutrition
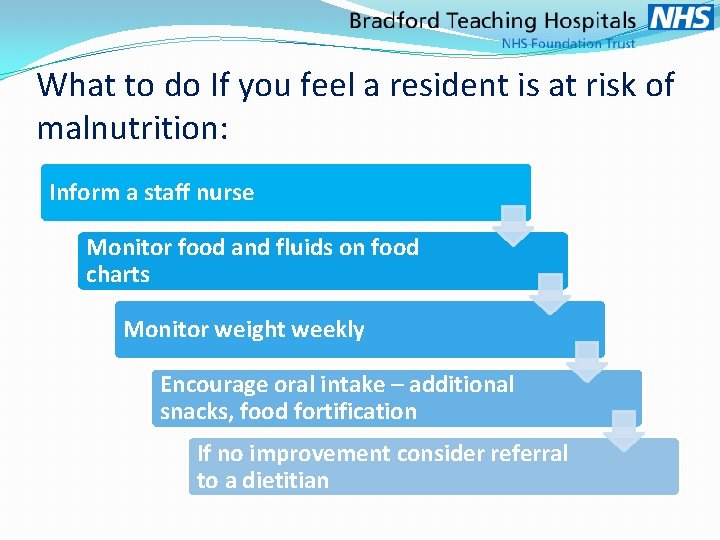
What to do If you feel a resident is at risk of malnutrition: Inform a staff nurse Monitor food and fluids on food charts Monitor weight weekly Encourage oral intake – additional snacks, food fortification If no improvement consider referral to a dietitian
Food Fortification Adds calories & protein without increasing volume Little & often, high calorie
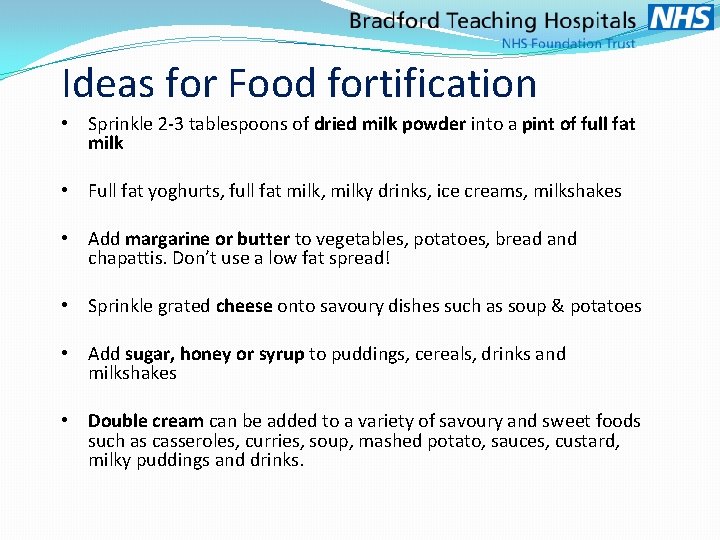
Ideas for Food fortification • Sprinkle 2 -3 tablespoons of dried milk powder into a pint of full fat milk • Full fat yoghurts, full fat milk, milky drinks, ice creams, milkshakes • Add margarine or butter to vegetables, potatoes, bread and chapattis. Don’t use a low fat spread! • Sprinkle grated cheese onto savoury dishes such as soup & potatoes • Add sugar, honey or syrup to puddings, cereals, drinks and milkshakes • Double cream can be added to a variety of savoury and sweet foods such as casseroles, curries, soup, mashed potato, sauces, custard, milky puddings and drinks.
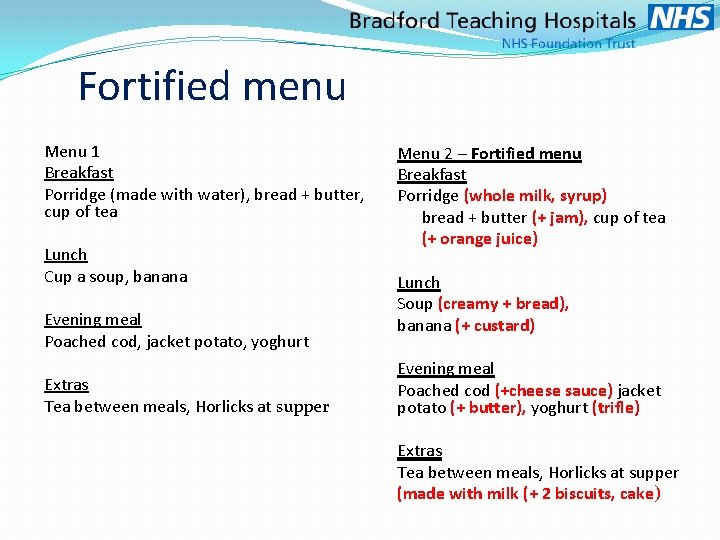
Fortified menu Menu 1 Breakfast Porridge (made with water), bread + butter, cup of tea Lunch Cup a soup, banana Evening meal Poached cod, jacket potato, yoghurt Extras Tea between meals, Horlicks at supper Menu 2 – Fortified menu Breakfast Porridge (whole milk, syrup) bread + butter (+ jam), cup of tea (+ orange juice) Lunch Soup (creamy + bread), banana (+ custard) Evening meal Poached cod (+cheese sauce) jacket potato (+ butter), yoghurt (trifle) Extras Tea between meals, Horlicks at supper (made with milk (+ 2 biscuits, cake)
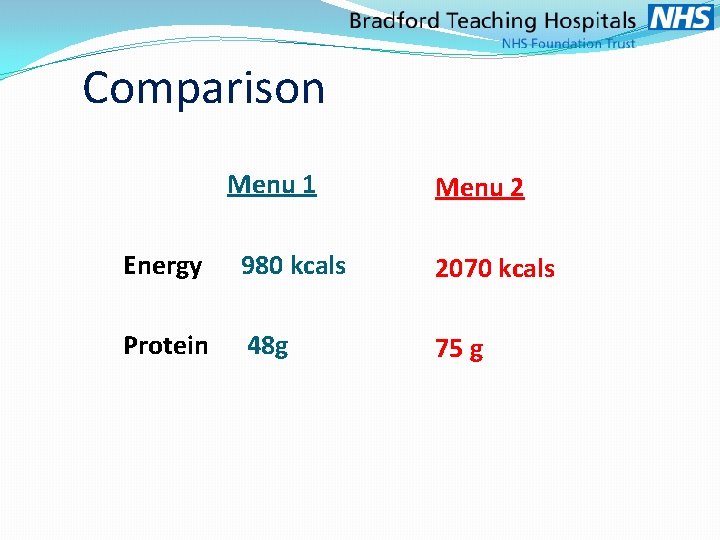
Comparison Menu 1 Menu 2 Energy 980 kcals 2070 kcals Protein 48 g 75 g
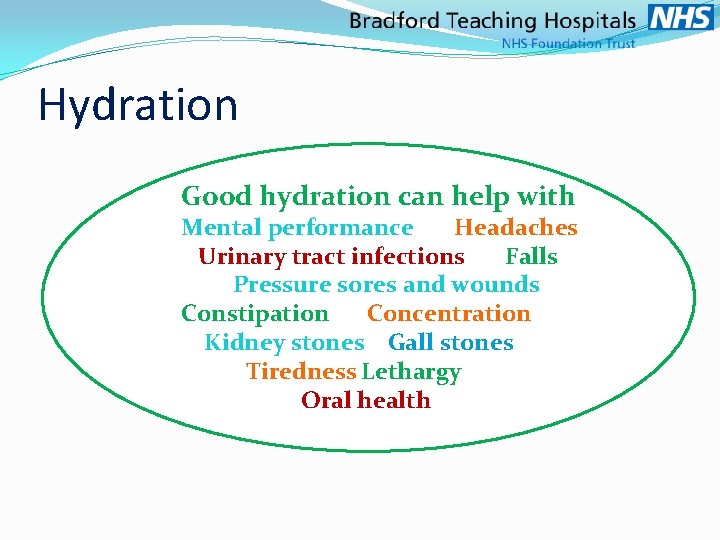
Hydration Good hydration can help with Mental performance Headaches Urinary tract infections Falls Pressure sores and wounds Constipation Concentration Kidney stones Gall stones Tiredness Lethargy Oral health
Oral Nutritional Supplements �Prescribed supplements – Ensure Plus, Pro Cal Shot �High energy, high protein in small volume �Expensive to use & compliance is poor �Quick & Easy to use �Follow prescribing information �Timing �Flavours
Referring to the Dietitian �Community Matron ( Nursing Homes) �District Nurses (Residential Homes) �GP
- Slides: 50