Nutrition Focused Physical Assessment in Dietetic Curriculum Practice









- Slides: 68
Nutrition Focused Physical Assessment in Dietetic Curriculum & Practice Miami University Nutrition Program
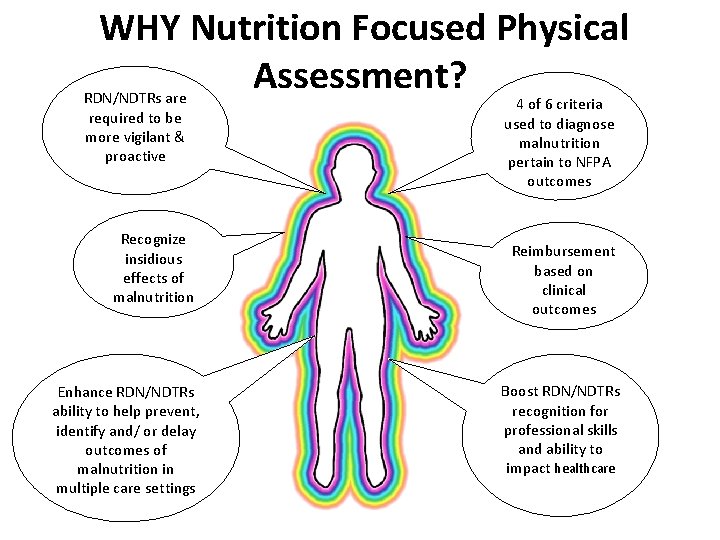
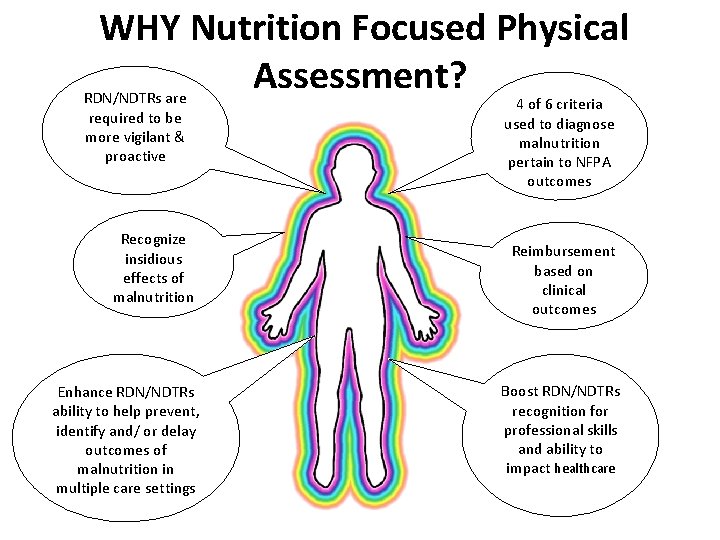
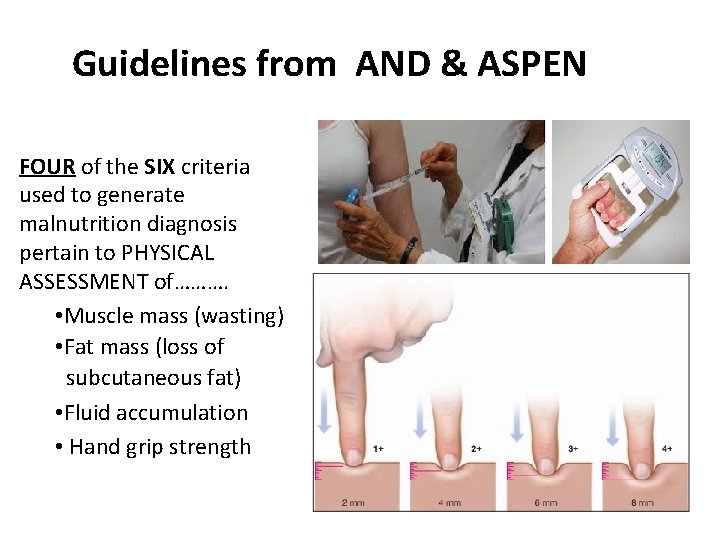
WHY Nutrition Focused Physical Assessment? . RDN/NDTRs are required to be more vigilant & proactive Recognize insidious effects of malnutrition Enhance RDN/NDTRs ability to help prevent, identify and/ or delay outcomes of malnutrition in multiple care settings 4 of 6 criteria used to diagnose malnutrition pertain to NFPA outcomes Reimbursement based on clinical outcomes Boost RDN/NDTRs recognition for professional skills and ability to impact healthcare
Behavioral Objectives 1. Identify the components of a NFPA. 2. List four areas NFPA techniques assess 3. Identify where NFPA fits into the dietetic scope of practice and day-to-day provision of care activities. 4. Define the four techniques used to conduct a NFPA. 5. Review benefits and suggestions for implementation of NFPA into the Dietetics Curriculum 6. Utilize a simulated case scenario and determine malnutrition diagnosis from a demonstrated head-totoe NFPA.
Background • New federal and state guidelines on the dx of malnutrition and reimbursement for related care requires dietitians and technicians to more vigilant and proactive in providing successful interventions. • Goal is to prevent or delay, reverse and limit malnutrition in care settings.
Nutrition Focused Physical Assessment… • Is timely and relevant • Brings significant attention to the subject of malnutrition • RDN/DTR’s can utilize NFPA to… • evaluate nutritional risk • determine more effective nutrition interventions
Components of NFPA Examination (Objective #1) • General Survey Ø visual physical appearance • • • Vital Signs Skin Hair Nails Head & neck: Ø head, eyes, nose, neck • Oral Cavity Ø lips, tongue, mouth • Teeth • Upper/lower body Ø shoulder, clavicle, arms, scapula, ribs, hands, legs • • Respiratory system Cardiovascular system Abdomen Neurologic system
What Do NFPA Techniques Assess? (Objective #2) • overt signs of nutritional deficiency • skin integrity • organ function • loss of muscle & subcutaneous fat stores
Healthcare • Scrutinized based on clinical outcomes • Care plans need to exhibit cost saving measures • AND has requested Council on Future Practice (CFP) to provide guidance & recommendations on the topic of NFPA…… “Moving Forward- A Vision for the Continuum of Dietetic Education, Credentialing and Practice”.
• Published standards that allow currently accredited dietetics programs to assimilate NFPA skill development into coursework.
Challenges • RDN/DTR’s in practice may have not yet been trained in putting new assessment guidelines into practice. • Healthcare facilities have not adopted new guidelines on malnutrition; therefore have not made significant progress toward training their dietetics staff on NFPA techniques.
Malnutrition Diagnosis Guidelines • Developed by AND & American Society for Parenteral & Enteral Nutrition (ASPEN). • Goal…. use guidelines consistently & accurately, to demonstrate the presence of malnutrition. • Facilitate the physicians’ ability to recognize and appropriately diagnose malnourished patients. • Refer to Handout
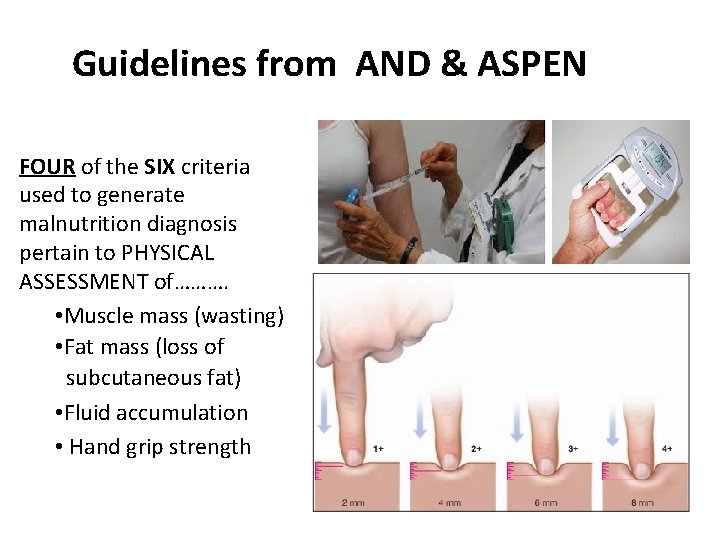
Guidelines from AND & ASPEN FOUR of the SIX criteria used to generate malnutrition diagnosis pertain to PHYSICAL ASSESSMENT of………. • Muscle mass (wasting) • Fat mass (loss of subcutaneous fat) • Fluid accumulation • Hand grip strength
Future Dietetics Education Plan with Expected Outcomes Diagnosis of malnutrition and reimbursement requires RDN/DTR’s to become more in identifying malnutrition!!!
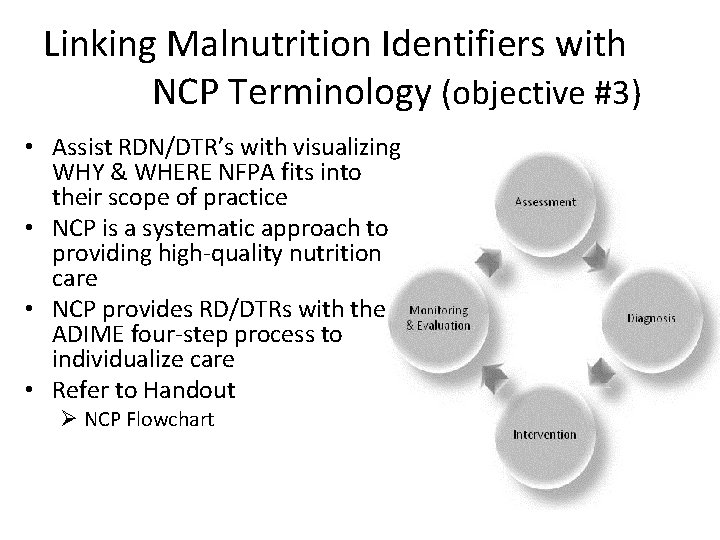
Linking Malnutrition Identifiers with NCP Terminology (objective #3) • Assist RDN/DTR’s with visualizing WHY & WHERE NFPA fits into their scope of practice • NCP is a systematic approach to providing high-quality nutrition care • NCP provides RD/DTRs with the ADIME four-step process to individualize care • Refer to Handout Ø NCP Flowchart
Vision for Dietetics Education • Nutrition related problems are best identified through the NCP – First element is to gather objective & subjective data to complete a thorough nutrition assessment. – NFPA is part of step one of the comprehensive nutrition assessment (NFPA consists of 3 steps) – NFPA (step 3 hands on component) often not performed due to lack of education/training
Comprehensive Nutrition Assessment • Client History • Food/Nutrition History • Laboratory/Medical test results • Physical measurements • NFPA findings…. -conduct steps 1 -3 (refer to handout)
NFPA Steps 1 • Conduct general survey of patient’s appearance Ø often described as “appears cachetic” or “very frail & thin” • Compare findings with available patient data from medical records and other sources
NFPA Step 2 • Evaluate resident’s body habitus and compare body mass index and weight changes to findings • Consider whether the individual’s reported appetite and BMI are consistent with the visual assessment of the individual’s body habitus
NFPA Step 3 • Perform hands on physical assessment, focusing on evaluation of body systems, skin, hair, nails, eyes, oral cavity, upper/ lower body noting signs of nutrient deficiencies or excesses
Approaching the Patient 1) Introduce yourself to the patient/resident. 2) Greet patient warmly and explain the purpose of your visit. Ø Consider using the 10/4 rule: stop 10 feet from the bed while making eye contact and smile, then approach to within 4 feet. 3) Make sure to acknowledge other health care professionals and visitors in the room. Ø Remove distractions (wait for health care professionals to complete their duties and ask permission to turn off television) 4) Ask the patient for permission to examine them. 5) Wash/dry hands thoroughly--don gloves. 6) During exam, ask the patient questions to get a better idea of their nutritional status. 7) Use standard precautions to prevent disease transmission.
Using NFPA Connects the dots to a physician and a malnutrition diagnosis Enhances ability to prevent, identify and/or delay outcomes of malnutrition in multiple care settings.
Goal for Nutrition Assessment • Incorporate more physical assessment training into the dietetics curriculum. • Provide hands-on training for students to gain the self-assurance and skills set necessary to perform NFPA as part of the NCP.
Benefits • Cutting-edge educational experiences. • Increased recognition of the RDN/DTRs in the functioning of the health care team. • Team experiences/ collaboration for students. • Novice level NFPA skills prior to starting entry-level practice.
Suggestions for Implementation Students will …. • Engage in and incorporate NFPA into existing MNT courses • Utilize resources already present – Students will perform NFPA in class – Students willl reflect on NFPA experience • Students will obtain training in classroom
Student Training • Obtain Certificate of Training in Adult Malnutrition through the Abbott Nutrition Health Institute (ANHI) website. – Allows students to obtain a uniform understanding of the NFPA process – Internet based courses from the ANHI

Suggestions continued…. Students will…. • Reach out to preceptors as content/training experts • Collaborate with students to infuse hands-on nutrition focused physical exam education
Implementation NFPA Training Demonstration/simulation lecture in each of the following subjects • Body Composition • Anthropometric Indices • Vital Sign Measurement/Biochemical • NFPA Head-to-Toe

Body Composition • Bod Pod • Bioelectrical Impedance • Skinfold Analysis

Anthropometric Indices • • • Height Body weight Waist circumference Arm span Knee height
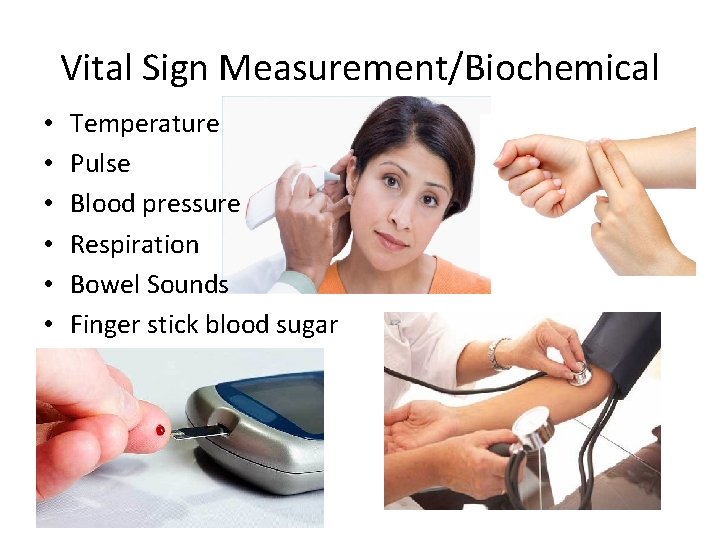
Vital Sign Measurement/Biochemical • • • Temperature Pulse Blood pressure Respiration Bowel Sounds Finger stick blood sugar
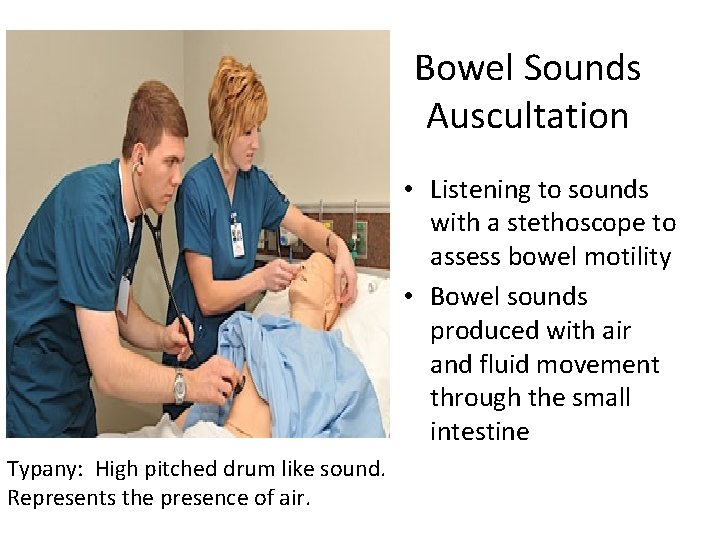
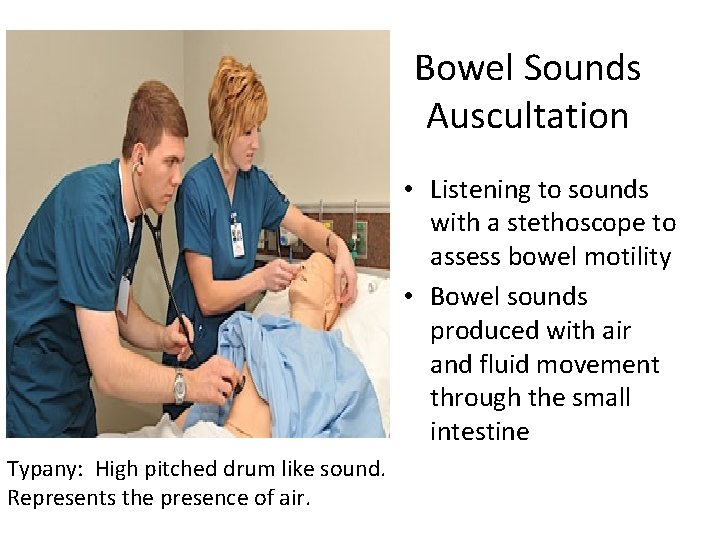
Bowel Sounds Auscultation • Listening to sounds with a stethoscope to assess bowel motility • Bowel sounds produced with air and fluid movement through the small intestine Typany: High pitched drum like sound. Represents the presence of air.
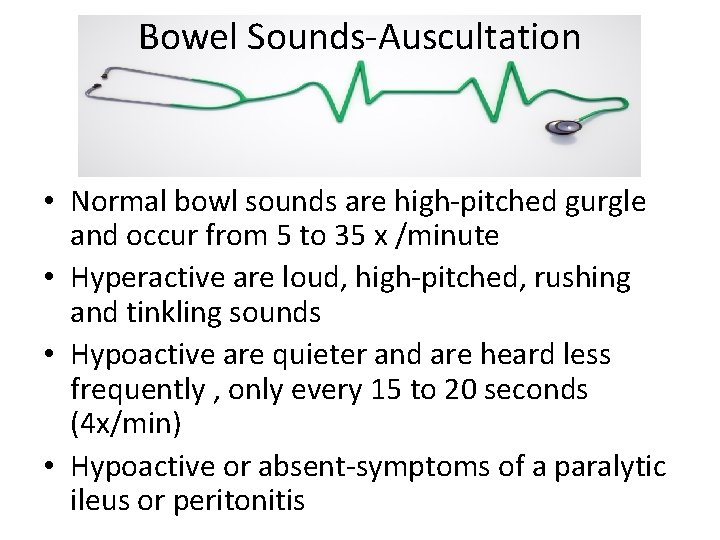
Bowel Sounds-Auscultation • Normal bowl sounds are high-pitched gurgle and occur from 5 to 35 x /minute • Hyperactive are loud, high-pitched, rushing and tinkling sounds • Hypoactive are quieter and are heard less frequently , only every 15 to 20 seconds (4 x/min) • Hypoactive or absent-symptoms of a paralytic ileus or peritonitis

NFPA Getting Started Head-to Toe (Step 3) • Follows review of patient’s medical and social history, laboratory results, and a nutrition history interview • Review of each body system vs focus on a specific system

Components of Head-to-Toe skin hair nails eyes oral cavity (lips, gums, tongue) – upper body (arm, shoulder, clavicle, hands) – lower body (quadriceps, knee, calf) – – –
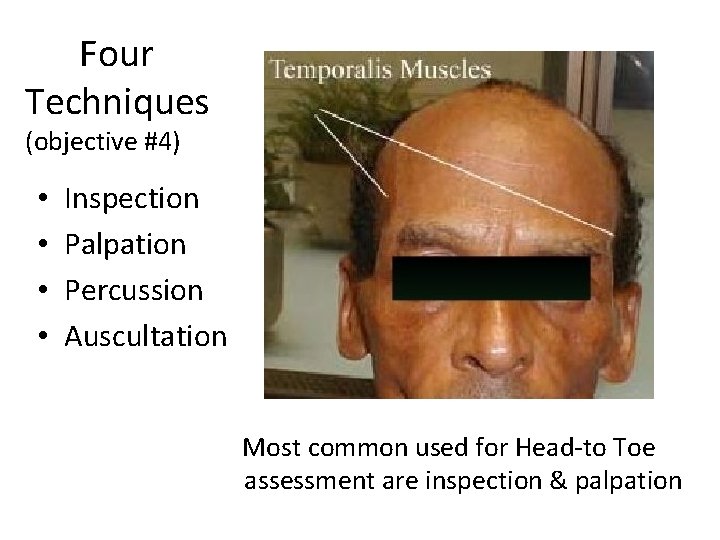
Four Techniques (objective #4) • • Inspection Palpation Percussion Auscultation Most common used for Head-to Toe assessment are inspection & palpation
Inspection Visual observation of color, shape, texture & size.
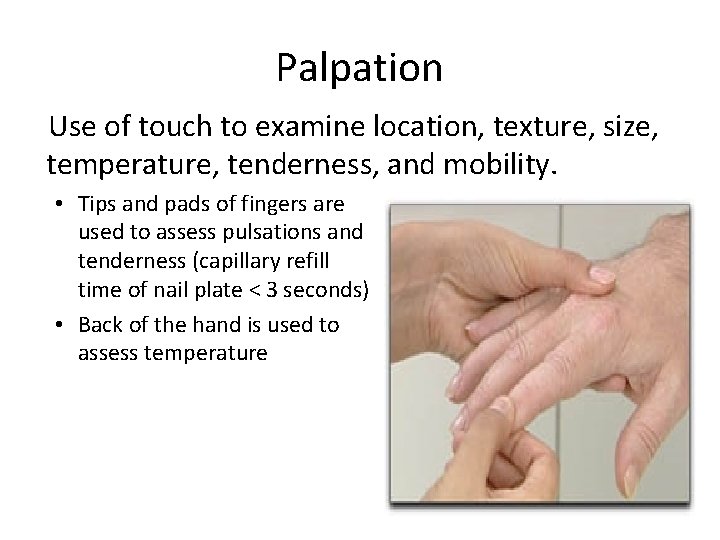
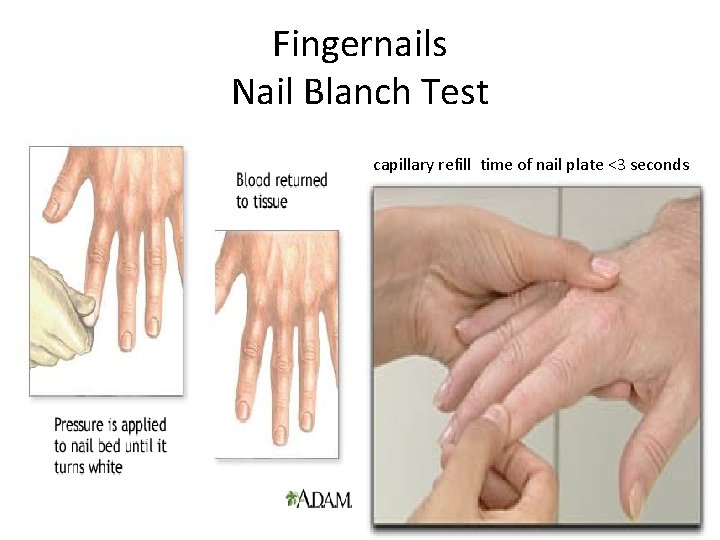
Palpation Use of touch to examine location, texture, size, temperature, tenderness, and mobility. • Tips and pads of fingers are used to assess pulsations and tenderness (capillary refill time of nail plate < 3 seconds) • Back of the hand is used to assess temperature
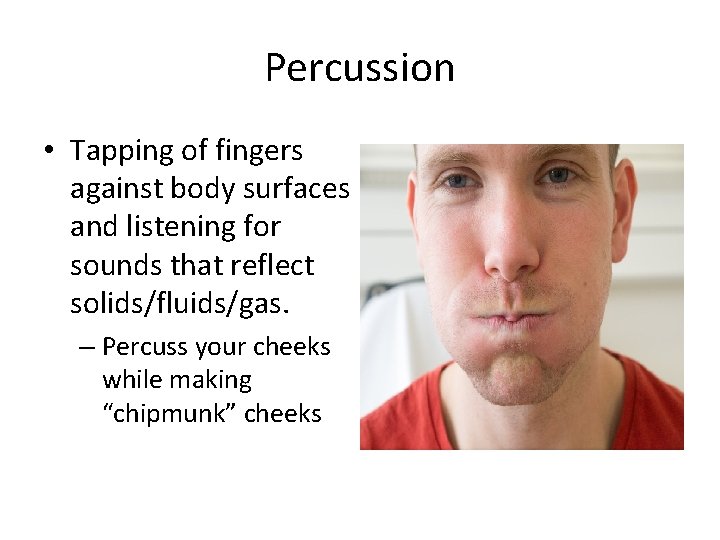
Percussion • Tapping of fingers against body surfaces and listening for sounds that reflect solids/fluids/gas. – Percuss your cheeks while making “chipmunk” cheeks
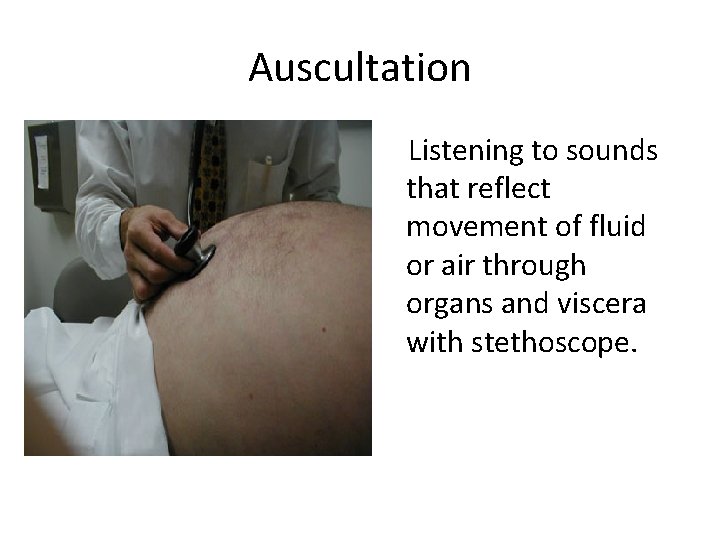
Auscultation Listening to sounds that reflect movement of fluid or air through organs and viscera with stethoscope.
Head-to-Toe Assessment • Simulated Case Study – Demonstrated Assessment • Refer to Malnutrition Assessment Training - Handout NPA Steps 1 -3
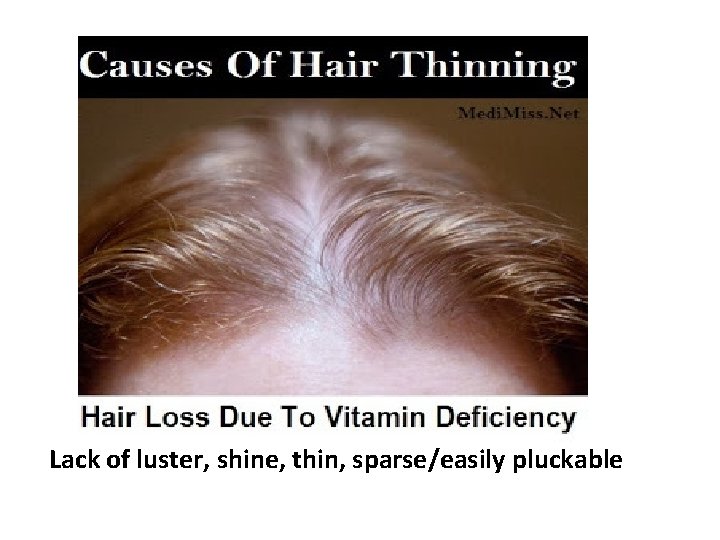
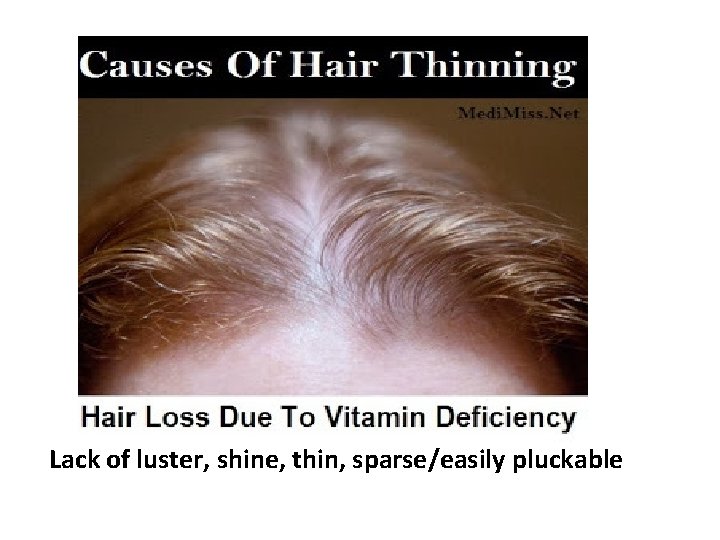
Hair Lack of luster, shine, thin, sparse/easily pluckable
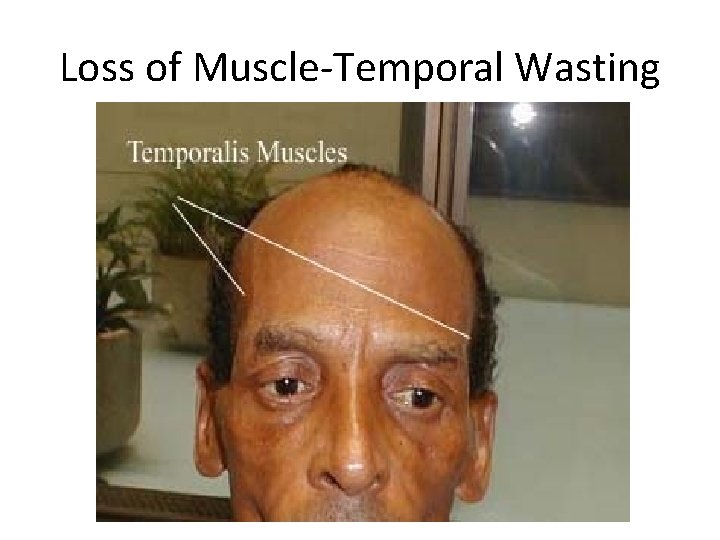
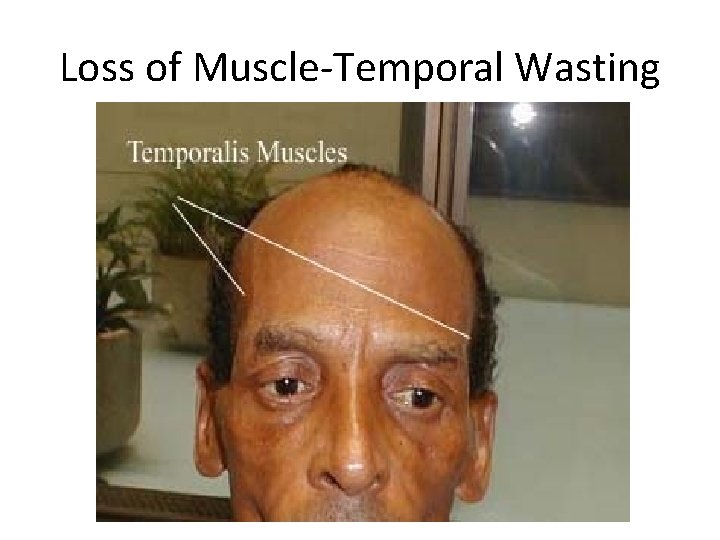
Loss of Muscle-Temporal Wasting
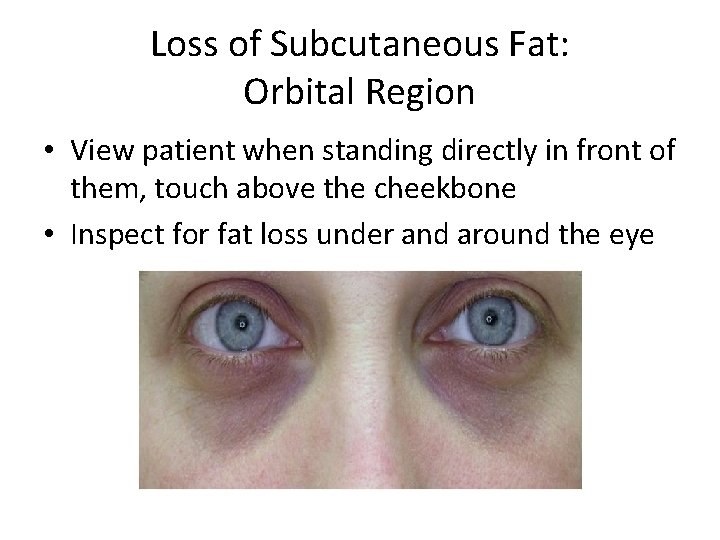
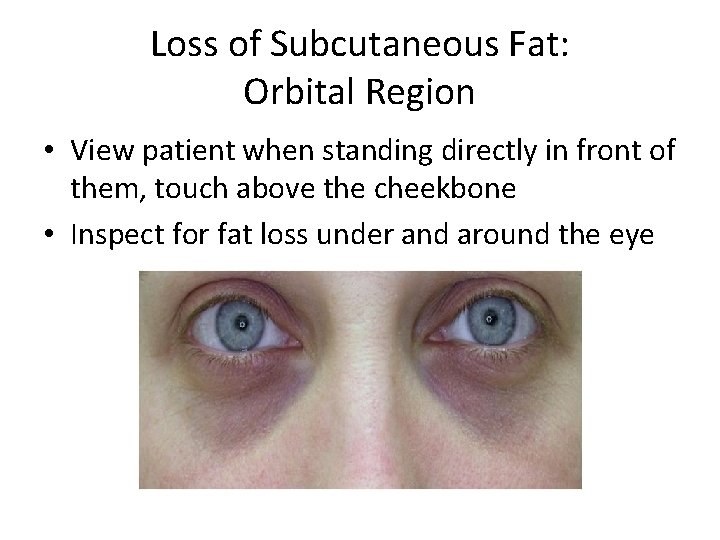
Loss of Subcutaneous Fat: Orbital Region • View patient when standing directly in front of them, touch above the cheekbone • Inspect for fat loss under and around the eye
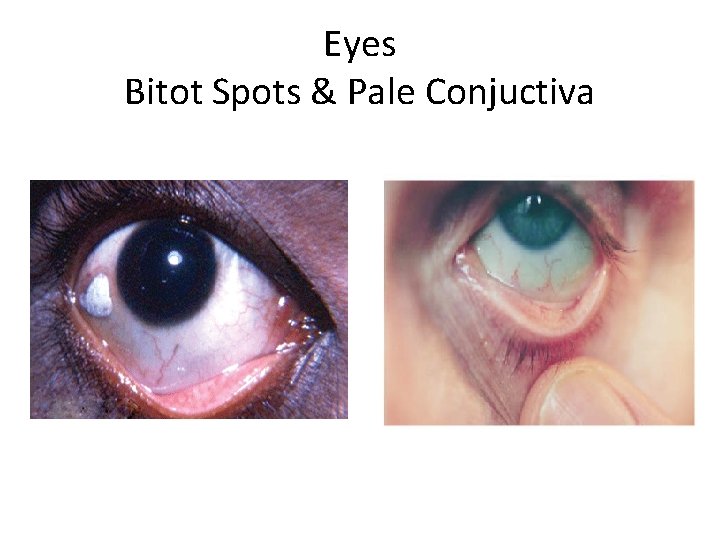
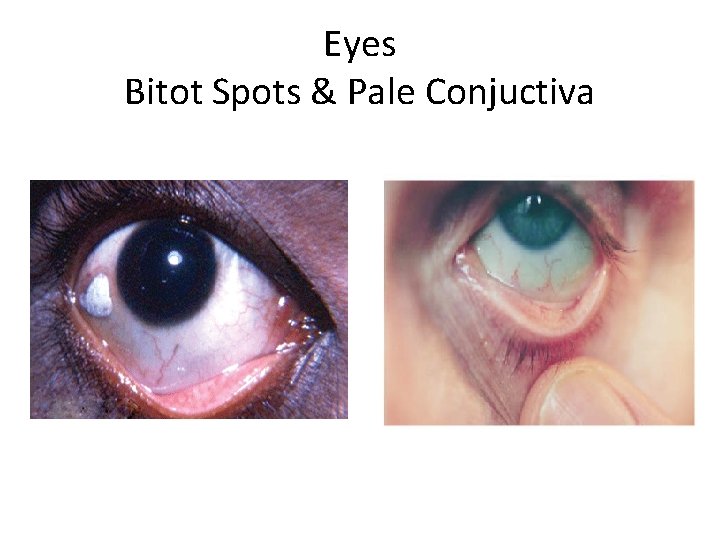
Eyes Bitot Spots & Pale Conjuctiva
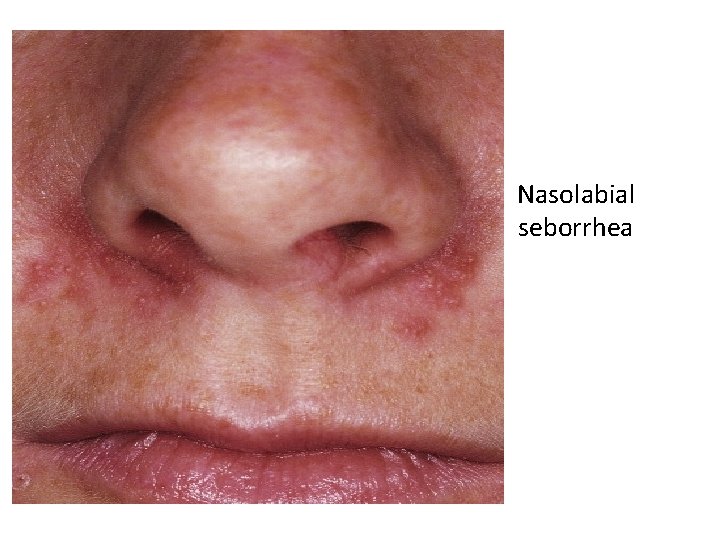
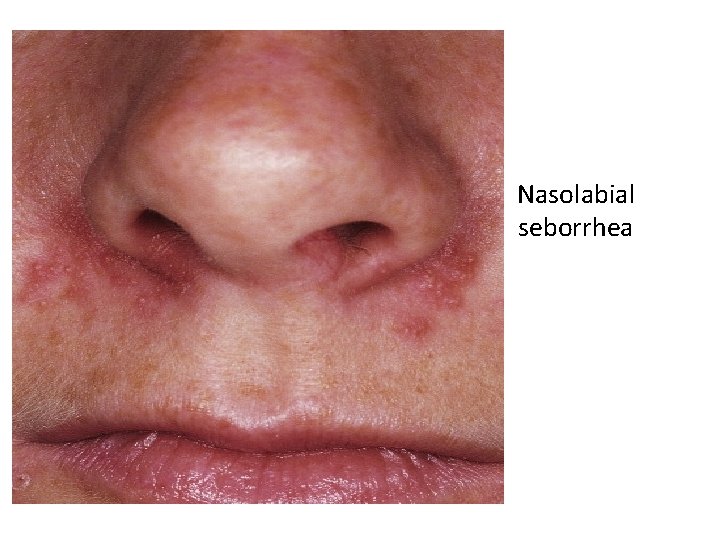
Nasolabial seborrhea
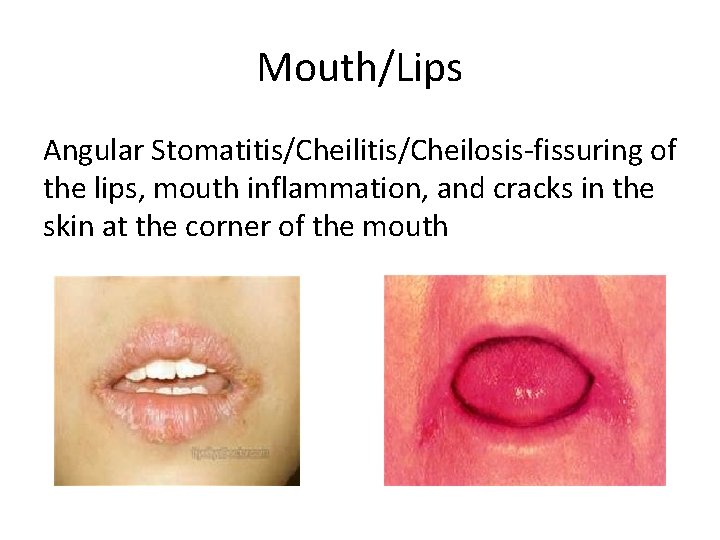
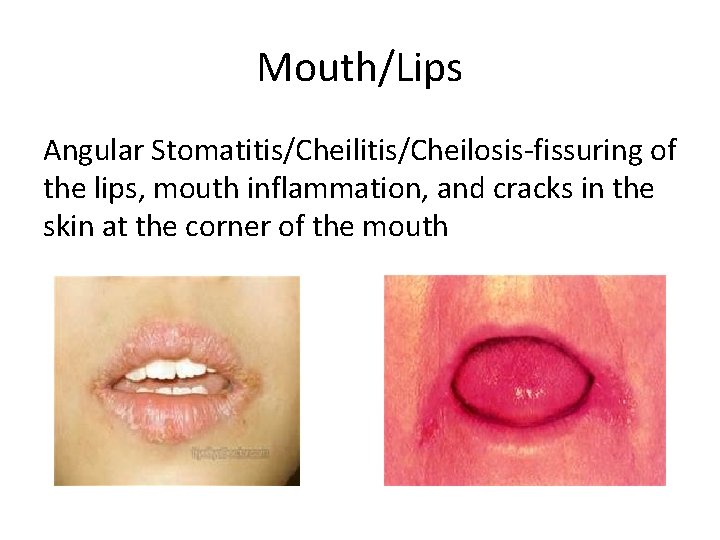
Mouth/Lips Angular Stomatitis/Cheilosis-fissuring of the lips, mouth inflammation, and cracks in the skin at the corner of the mouth
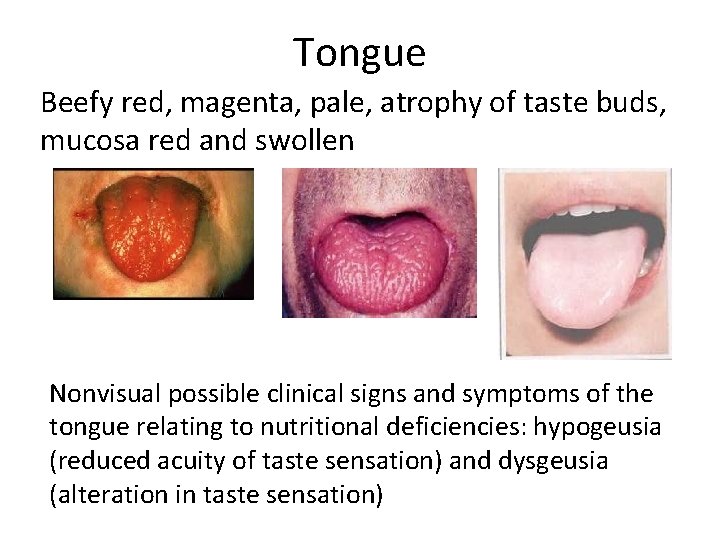
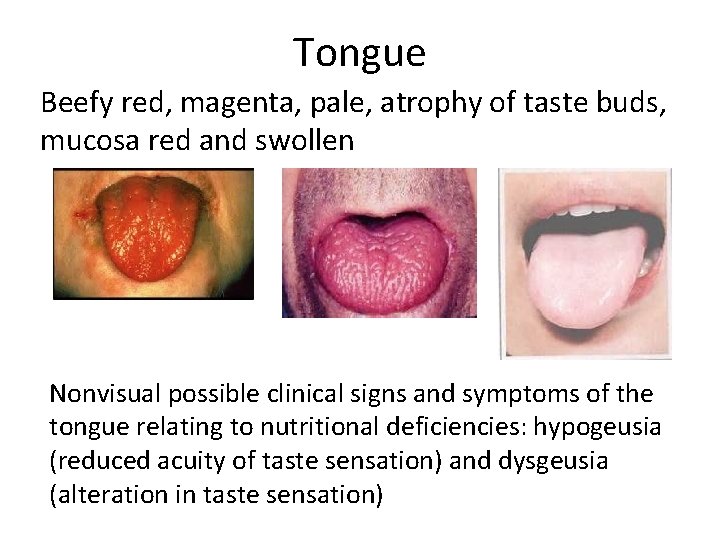
Tongue Beefy red, magenta, pale, atrophy of taste buds, mucosa red and swollen Nonvisual possible clinical signs and symptoms of the tongue relating to nutritional deficiencies: hypogeusia (reduced acuity of taste sensation) and dysgeusia (alteration in taste sensation)
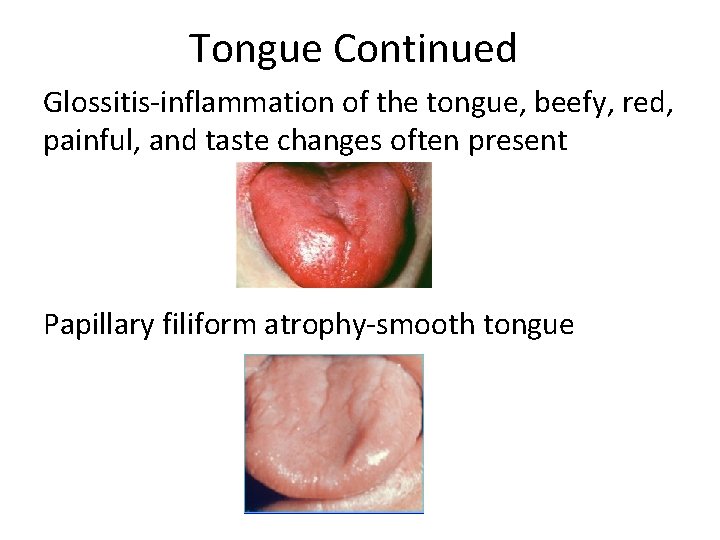
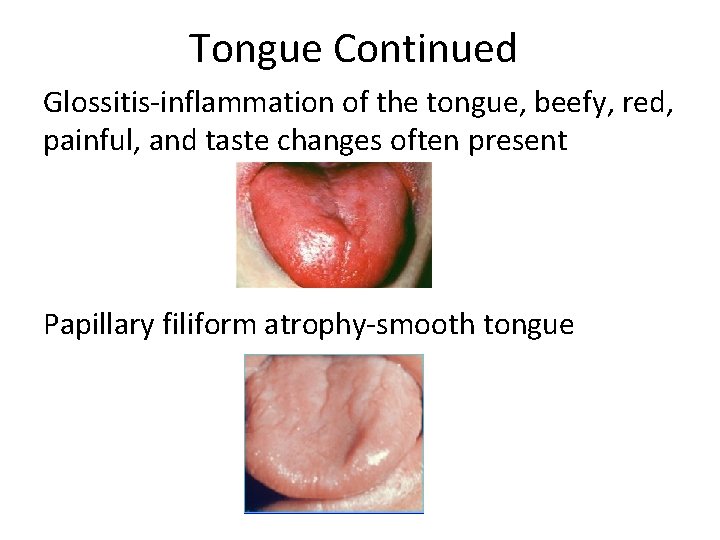
Tongue Continued Glossitis-inflammation of the tongue, beefy, red, painful, and taste changes often present Papillary filiform atrophy-smooth tongue
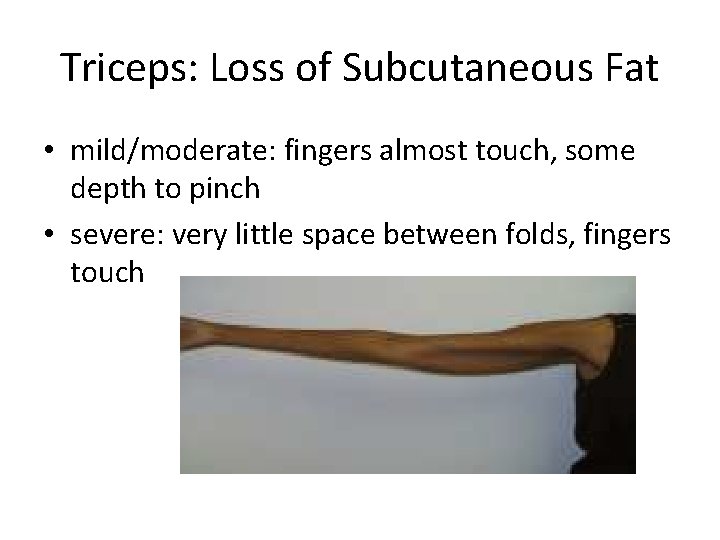
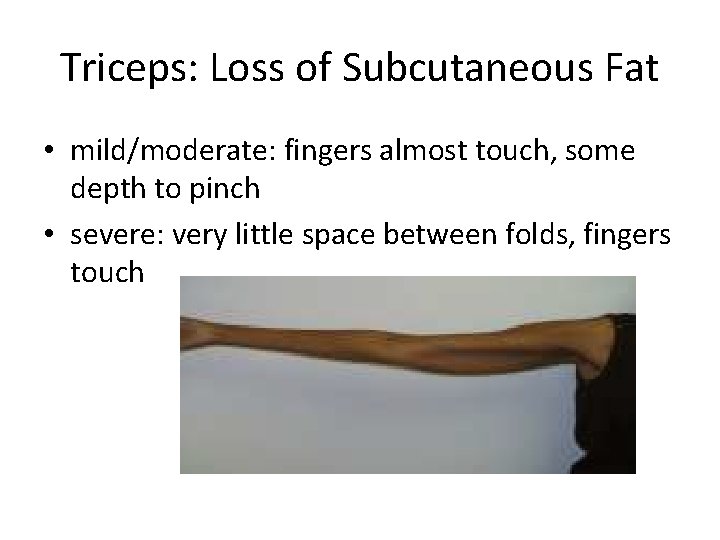
Triceps: Loss of Subcutaneous Fat • mild/moderate: fingers almost touch, some depth to pinch • severe: very little space between folds, fingers touch

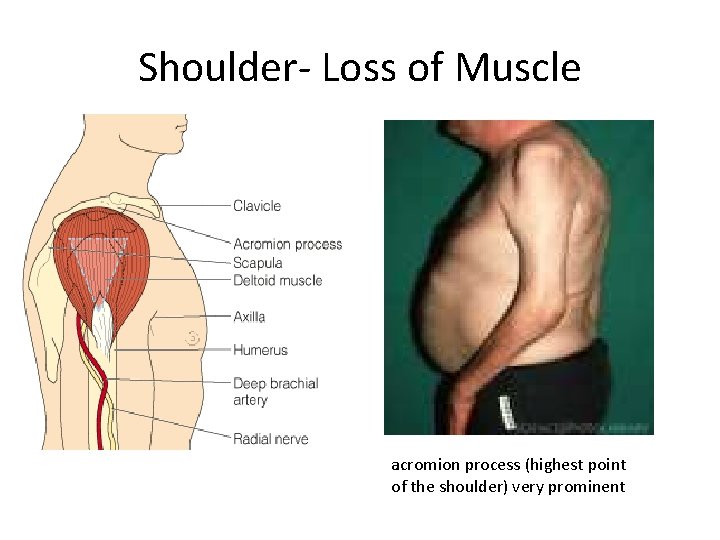
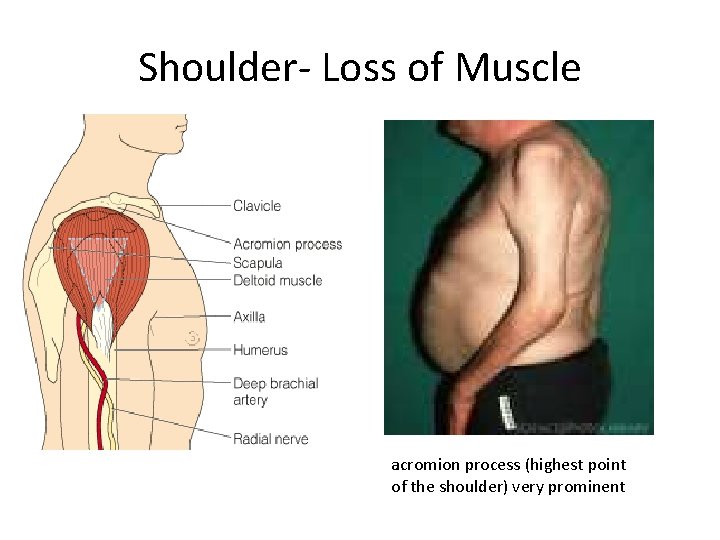
Shoulder- Loss of Muscle acromion process (highest point of the shoulder) very prominent
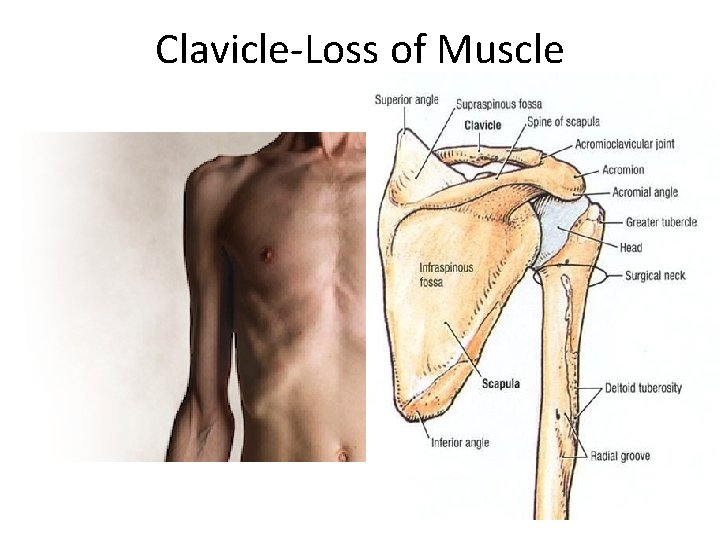
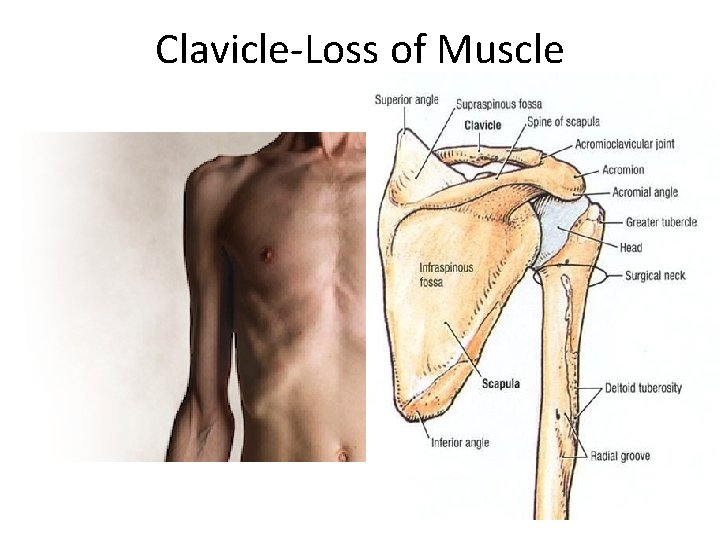
Clavicle-Loss of Muscle
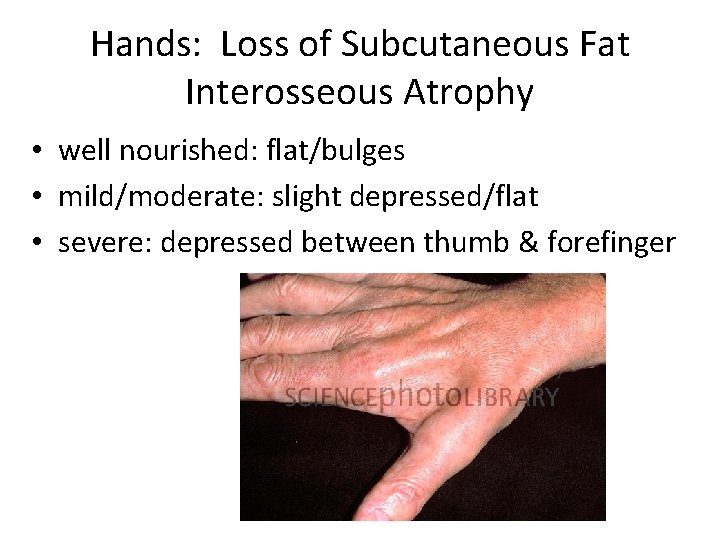
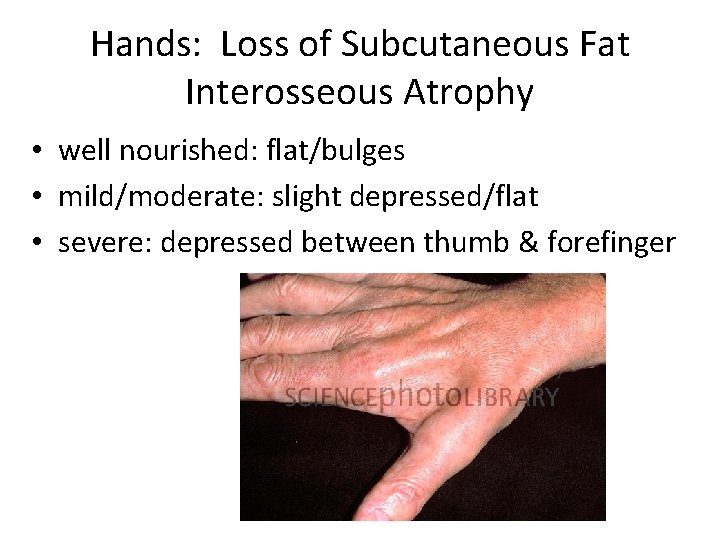
Hands: Loss of Subcutaneous Fat Interosseous Atrophy • well nourished: flat/bulges • mild/moderate: slight depressed/flat • severe: depressed between thumb & forefinger
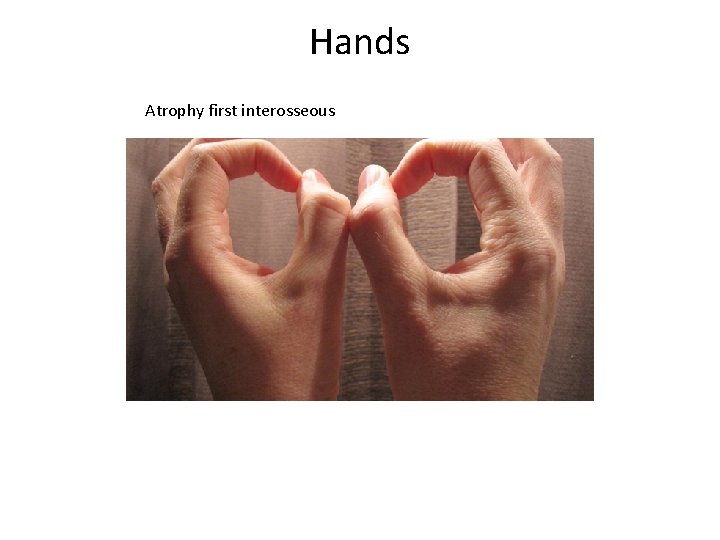
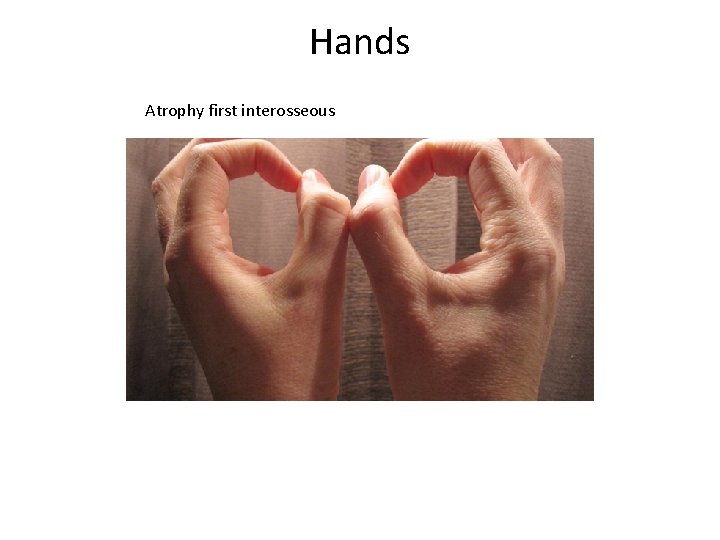
Hands Atrophy first interosseous
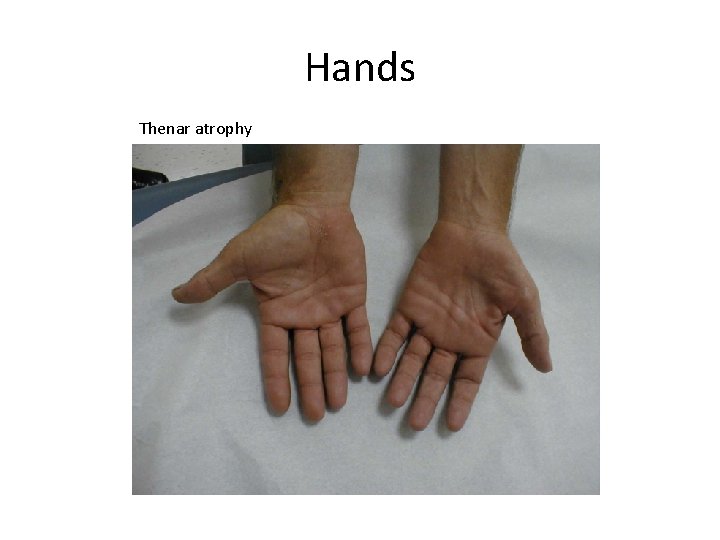
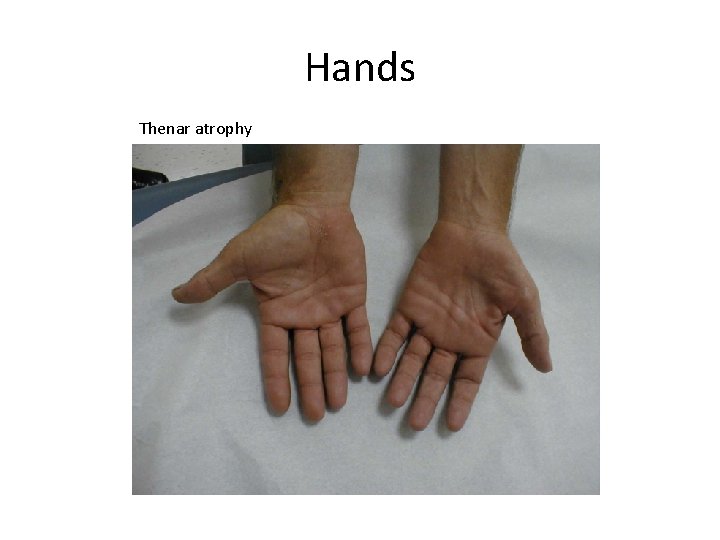
Hands Thenar atrophy
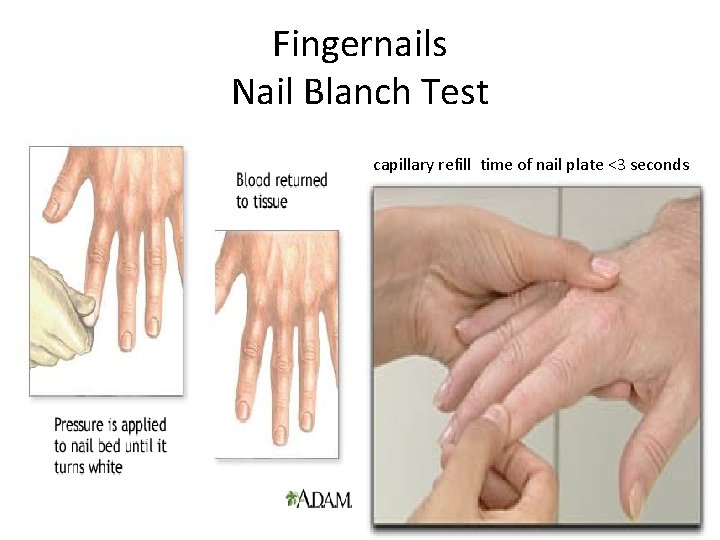
Fingernails Nail Blanch Test capillary refill time of nail plate <3 seconds

Fingernails (spoon shaped-iron deficiency)
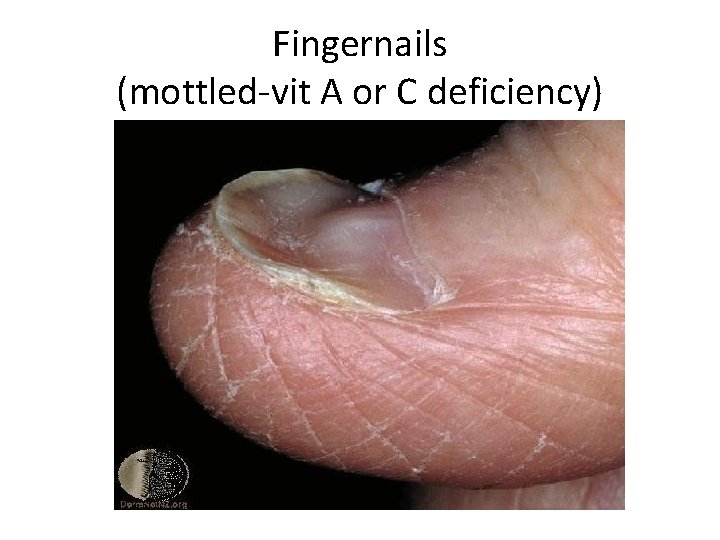
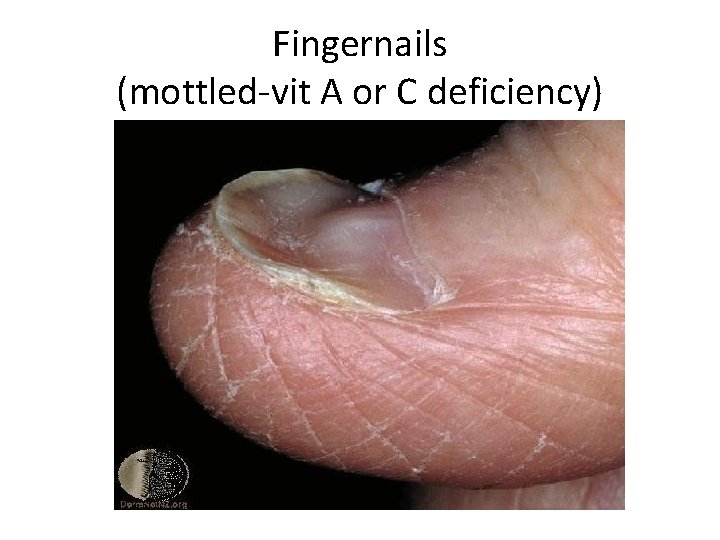
Fingernails (mottled-vit A or C deficiency)
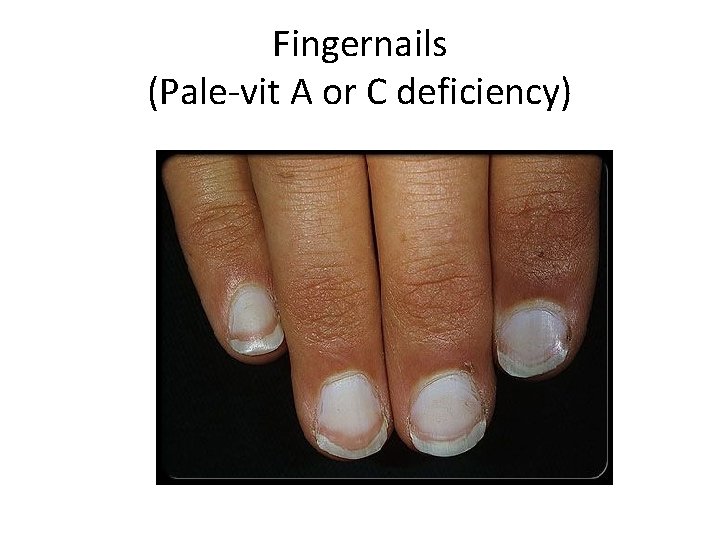
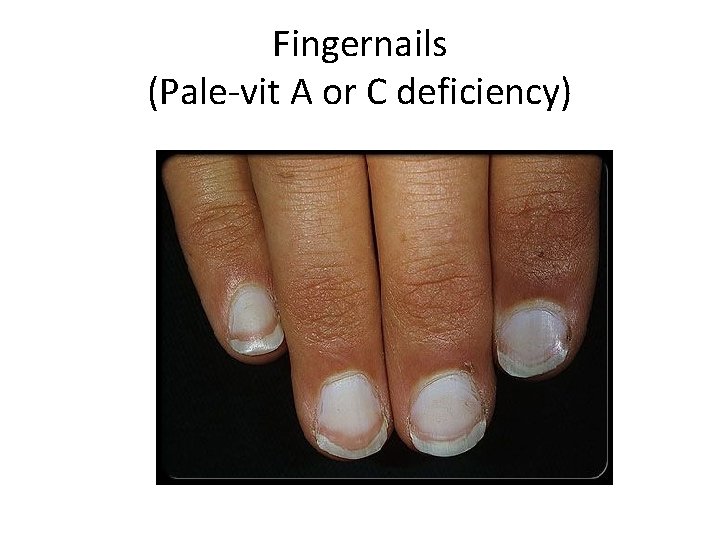
Fingernails (Pale-vit A or C deficiency)

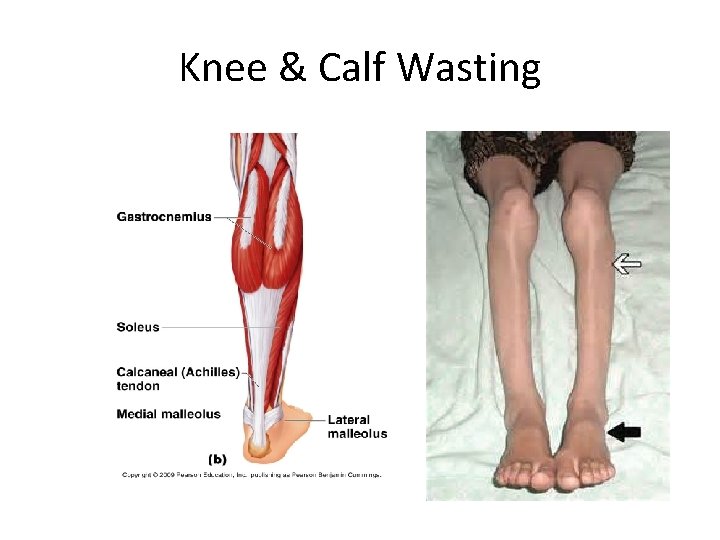
Quadriceps/Calf- Muscle Wasting
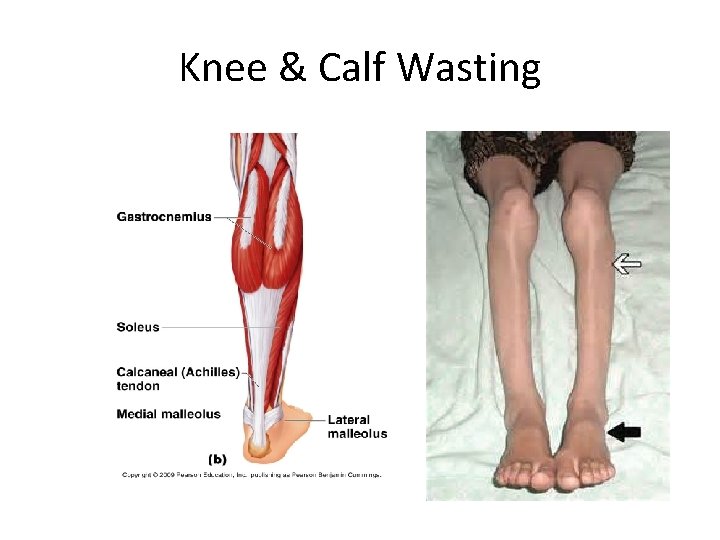
Knee & Calf Wasting
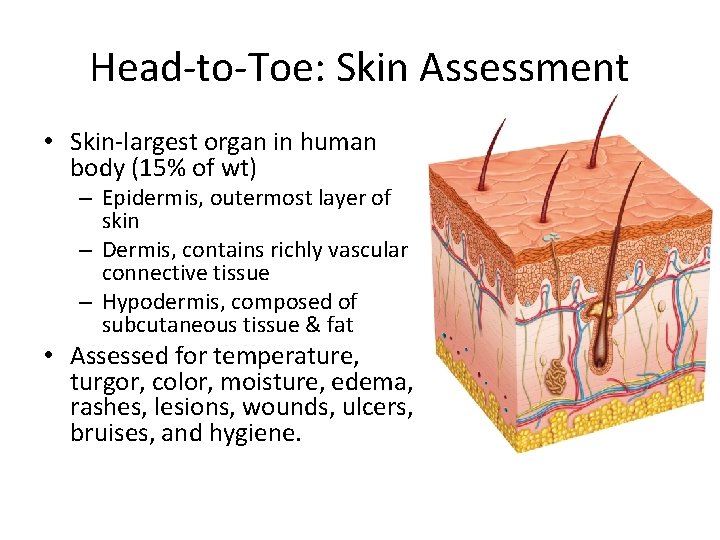
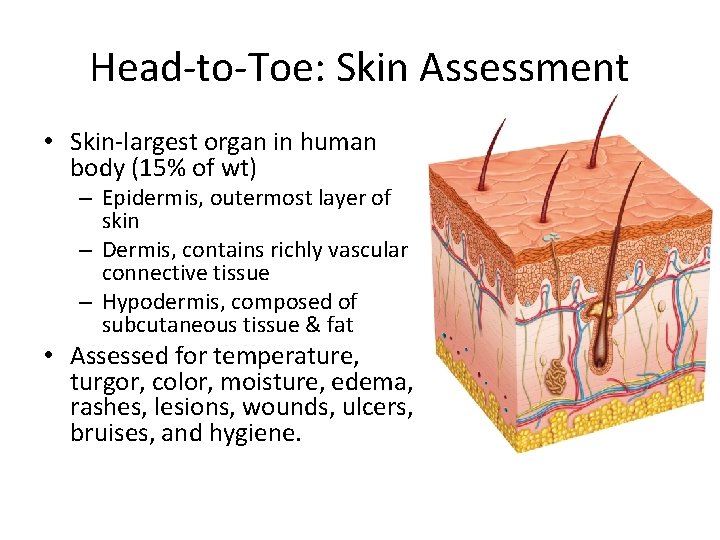
Head-to-Toe: Skin Assessment • Skin-largest organ in human body (15% of wt) – Epidermis, outermost layer of skin – Dermis, contains richly vascular connective tissue – Hypodermis, composed of subcutaneous tissue & fat • Assessed for temperature, turgor, color, moisture, edema, rashes, lesions, wounds, ulcers, bruises, and hygiene.
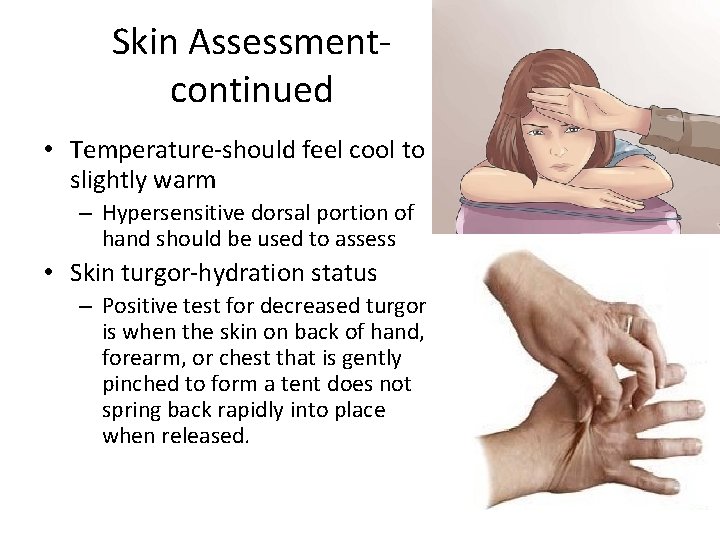
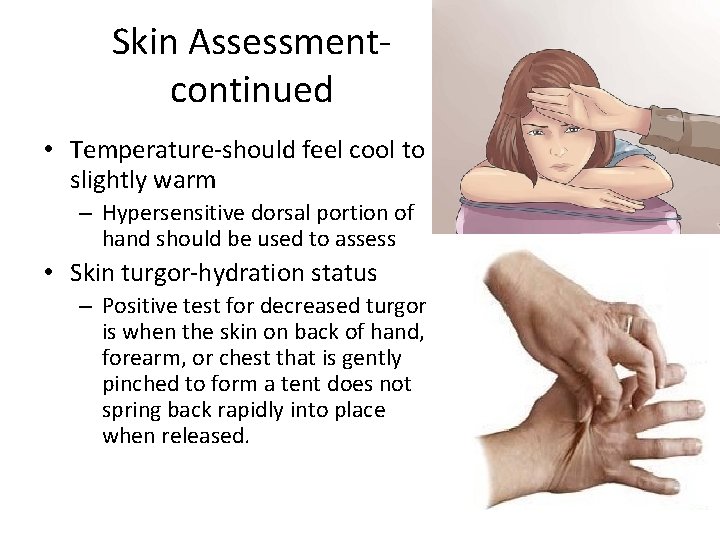
Skin Assessmentcontinued • Temperature-should feel cool to slightly warm – Hypersensitive dorsal portion of hand should be used to assess • Skin turgor-hydration status – Positive test for decreased turgor is when the skin on back of hand, forearm, or chest that is gently pinched to form a tent does not spring back rapidly into place when released.
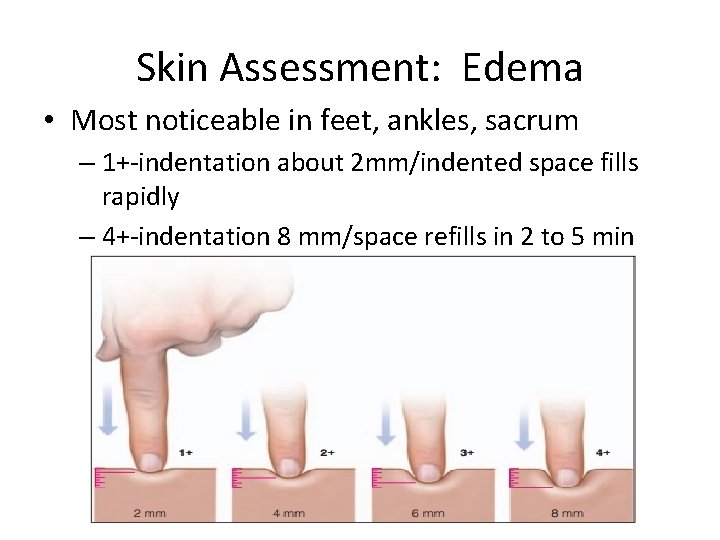
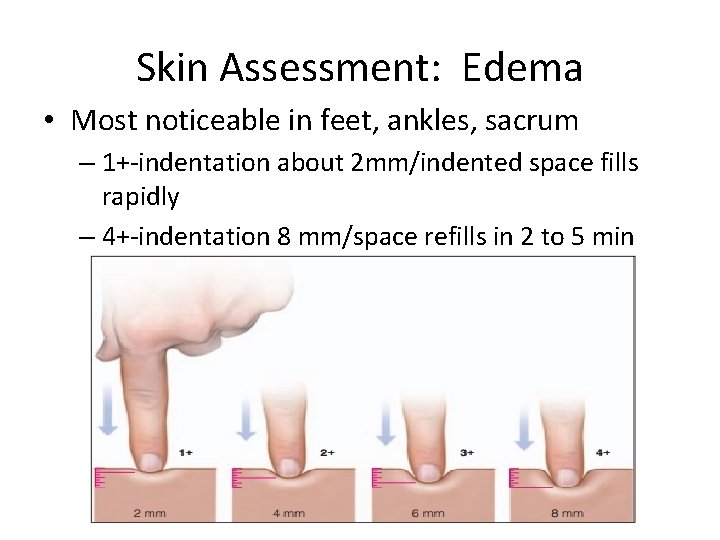
Skin Assessment: Edema • Most noticeable in feet, ankles, sacrum – 1+-indentation about 2 mm/indented space fills rapidly – 4+-indentation 8 mm/space refills in 2 to 5 min
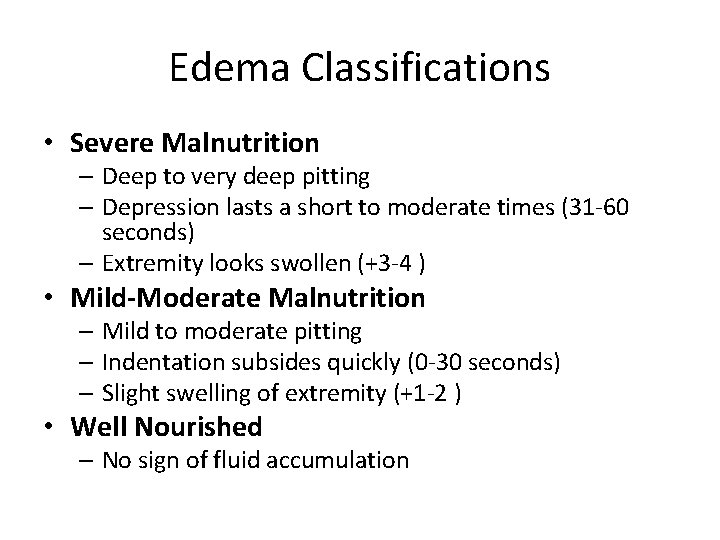
Edema Classifications • Severe Malnutrition – Deep to very deep pitting – Depression lasts a short to moderate times (31 -60 seconds) – Extremity looks swollen (+3 -4 ) • Mild-Moderate Malnutrition – Mild to moderate pitting – Indentation subsides quickly (0 -30 seconds) – Slight swelling of extremity (+1 -2 ) • Well Nourished – No sign of fluid accumulation

Edema
Hand Grip Strength • The strongest correlation with muscle mass and nutrition status • Determined using a Dynamometer – Measures the maximum isometric strength of the hand forearm.
Summary…. Value of NFPA • Requires RDN/NDTR’s to be more vigilant and proactive • Boosts recognition for professional skills • Brings significant attention to the subject of malnutrition • Connects the dots to a physician and a medical malnutrition diagnosis • Enhances ability to prevent, identify, and /or delay outcomes of malnutrition in multiple care settings
 How to assess edema
How to assess edema Palpation percussion auscultation
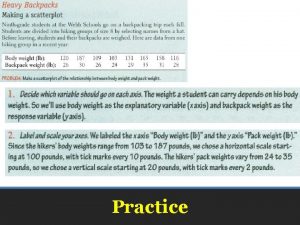
Palpation percussion auscultation Percentage of meal intake chart
Percentage of meal intake chart Ongoing professional practice evaluation template
Ongoing professional practice evaluation template Fast scan
Fast scan Dietetic support worker
Dietetic support worker Csulb dietetic internship
Csulb dietetic internship Viterbo dietetic internship
Viterbo dietetic internship Sodexo dietetic internships
Sodexo dietetic internships Keiser university dietetic internship
Keiser university dietetic internship Wladek minor uva
Wladek minor uva Cal poly pomona dietetic internship
Cal poly pomona dietetic internship Texas dietetic association
Texas dietetic association Montclair state university dietetic internship
Montclair state university dietetic internship Dietetic internships in georgia
Dietetic internships in georgia Dietetic internships in georgia
Dietetic internships in georgia Sodexo distance dietetic internship
Sodexo distance dietetic internship Mechanic task 1
Mechanic task 1 Chapter 10 nutrition for health vocabulary practice
Chapter 10 nutrition for health vocabulary practice Physical activity and nutrition coordinator
Physical activity and nutrition coordinator Community nutrition assessment
Community nutrition assessment Abcd method of nutritional assessment
Abcd method of nutritional assessment Jhu ois cpt
Jhu ois cpt Daniel tanner 1980 definition of curriculum explanation
Daniel tanner 1980 definition of curriculum explanation Primary care practice facilitation curriculum
Primary care practice facilitation curriculum Problem-focused coping examples
Problem-focused coping examples Upside down focused grid
Upside down focused grid Unfocused task example
Unfocused task example Process focus strategy in operations management
Process focus strategy in operations management Product oriented layout example
Product oriented layout example Problem focused coping examples
Problem focused coping examples Adaptive focused acoustics
Adaptive focused acoustics Active listening is focused and purposeful
Active listening is focused and purposeful Outcomes focused regulation
Outcomes focused regulation Stress experience
Stress experience Criminal psychology serial killers
Criminal psychology serial killers Note taking process
Note taking process Focused imaging learning
Focused imaging learning Problem focused trigger
Problem focused trigger Emotionally focused therapy techniques
Emotionally focused therapy techniques Ego-focused emotions relate to:
Ego-focused emotions relate to: Focused strategy
Focused strategy Adaptive focused acoustics
Adaptive focused acoustics Sociopath vs psychopath venn diagram
Sociopath vs psychopath venn diagram Solution focused therapy powerpoint
Solution focused therapy powerpoint Target marketing
Target marketing Short term scheduling in operations management
Short term scheduling in operations management Struktur horizontal
Struktur horizontal Focused note
Focused note Solution focused therapy youtube
Solution focused therapy youtube Metaphysical poets focused on _____.
Metaphysical poets focused on _____. Customer focused innovation
Customer focused innovation Grid cut off
Grid cut off Introduction of nursing research
Introduction of nursing research The externally focused church
The externally focused church Solution focused play therapy
Solution focused play therapy Customer focused skills
Customer focused skills Nation and macalister 2010
Nation and macalister 2010 Get focused get results
Get focused get results Focused management
Focused management Focused note taking process
Focused note taking process Focused note taking process
Focused note taking process Trait focused performance dimensions
Trait focused performance dimensions Positive connotation for non-athletic
Positive connotation for non-athletic Purposeful listening meaning
Purposeful listening meaning A zoom lens produces an inverted real image
A zoom lens produces an inverted real image Focused library
Focused library Realism in literature
Realism in literature Providence college library
Providence college library