Nursing Workload Acuity and Implementation of an EHR








- Slides: 53
Nursing Workload Acuity and Implementation of an EHR Designing and Implementing an Integrated Patient Classification System Development Elizabeth Petrich – Kennedy BSN, MS RN-BC; Sr. Director, Acute Care Clinical Informatics Optimization & Enhancement Providence St. Joseph Health
I, the undersigned, declare that neither I nor any member of my family have a financial arrangement with any corporate organization offering financial support or grant monies in regards to my Informatics continuing education presentation at the January 27, 2017 Southern California Chapter ANIA Conference. Elizabeth Petrich-Kennedy Instructor/Advisor e-Signature January 26, 2017 Date

Together, we provide an abundance of diverse capabilities and services to our communities. 829 CLINICS 50 HOSPITALS 99 k CAREGIVERS 90 NON- ACUTE SERVICES 23 k PHYSICIAN S HIGH SCHOOL, NURSING SCHOOL AND UNIVERSITY 1. 9 m MEMBERS
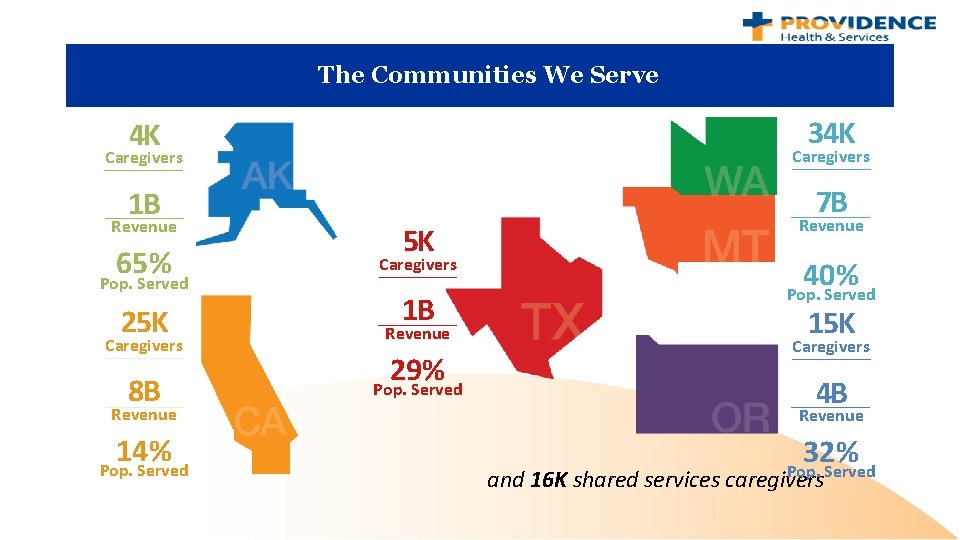
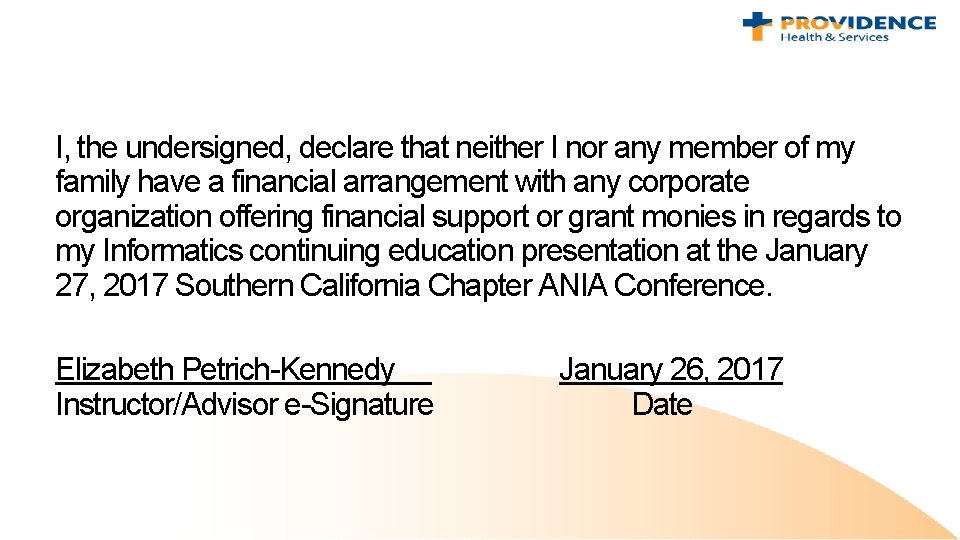
The Communities We Serve 34 K 4 K Caregivers 1 B 7 B Revenue 65% Pop. Served 25 K Caregivers 8 B 5 K Revenue 1 B Pop. Served Caregivers Revenue 29% Pop. Served 40% 15 K Caregivers 4 B Revenue 14% Pop. Served 32% Pop. Served and 16 K shared services caregivers
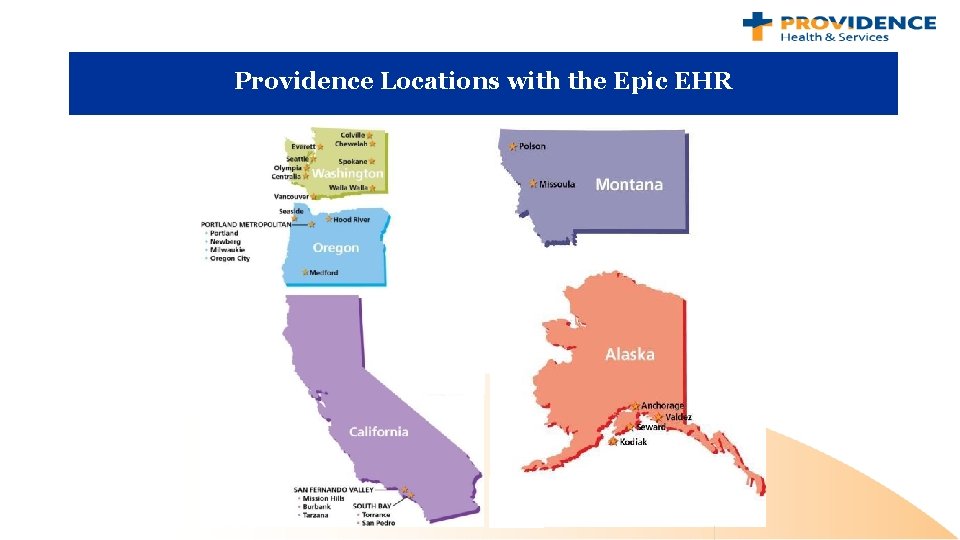
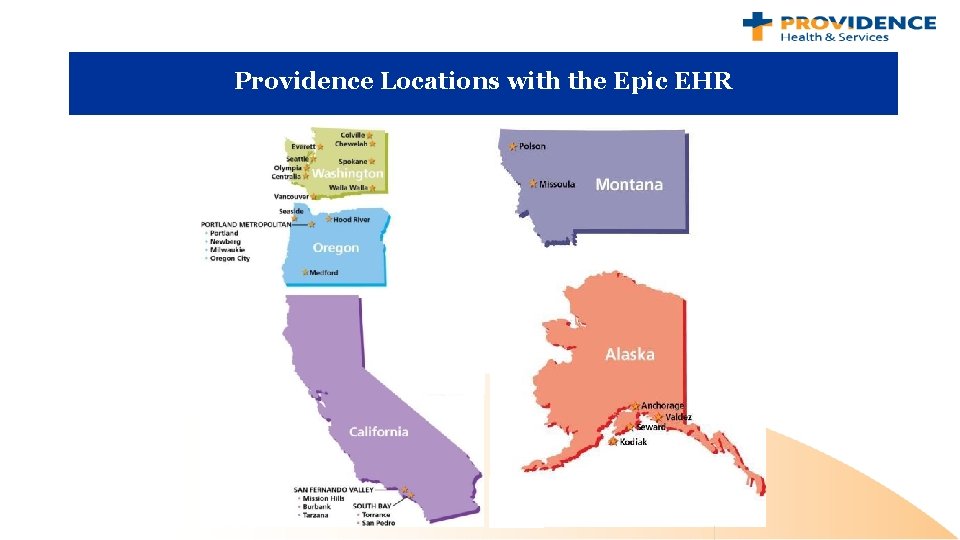
Providence Locations with the Epic EHR
Presentation Objectives: • Identify methods used to design, build and validate integrated nursing workload acuity – patient classification system across a multi-hospital health system. • Describe adoption strategies used to successfully implement an integrated nursing workload acuity – patient classification system. • Recognize the value of the Subject Matter Expert - Informatics partnership in the development and adoption of an integrated nursing workload acuity – patient classification system.
What is a Nursing Workload Acuity (Patient Classification) System?
• Nursing Workload Acuity (Patient Classification) System scoring processes measure the level of care that is expected to be needed during the next shift to support the patients currently on the unit. • CA Title 22 is the regulatory requirement that mandates the use of a Nursing Workload Acuity (Patient Classification) System in inpatient facilities in California. 8
Patient Classification System - California Title 22, 70053. 2 CA Title 22 requires a “method for establishing staffing requirements by unit, patient, and shift that includes: 1. 2. 3. 4. 5. 6. Prediction of nursing care requirements for individual patients; Amount of nursing care needed by category of patient, each shift, in each unit; Mechanism to test and validate if the patient classification system is truly identifying the amount of nursing care needed; Method to discern patterns and trends of nursing care delivery; Method to identify staff resource allocations based on nursing care requirements by shift and by unit; A system for reliability testing 9
Key Takeaways on Nursing Workload Acuity (NWA) • The Acuity score measures the future workload that can be expected to care for the patients currently on the unit. • At the start of a shift, nurses can use Nursing Workload Acuity scores to determine which of their assigned patients might need more of their time or attention today. • The Nursing Workload Acuity score is not a measure of the work that was already performed today, nor is it a measure of the severity of the patient’s condition.
How Is Nursing Workflow Affected? • KEY TAKEAWAY: The Epic Nursing Workload Acuity tool does not add any new tasks to the nurse’s daily work because real-time documentation of patient care is already our standard at Providence. • Nurses will continue to provide patient care the same way they do now, and they will probably document it in Epic just as they always have. • Aside from real-time documentation, there is nothing else the nurse needs to do to manage the Nursing Workload Acuity process in Epic.
How Are Nursing Workload Acuity Scores Used? • Nursing Workload Acuity scores allow the nurse leader to: – make sure high acuity patients are spread out evenly across the nursing care team – identify unusual patient care needs that might require a different level of staffing than is expected to be available for the next shift • KEY TAKEAWAY: Nursing department leaders have many tools at their disposal to manage staff assignments. A Nursing Workload Acuity score is just one of the tools that informs the staffing process. 12
How can Nursing Workload Acuity Scores Be Used By Individual Nurses? At the start of a shift, nurses can use Nursing Workload Acuity scores to determine which of their assigned patients might need more of their time or attention today. • KEY TAKEAWAY: The Acuity score measures the future workload that can be expected to care for the patients currently on the unit. The Nursing Workload Acuity score is not a measure of the work that was already performed today, nor is it a measure of the severity of the patient’s condition. 13
How Does The New Epic NWA Tool Work? • Almost every digital tool is powered by “if / then” statements. (If a certain condition is present, then a certain activity will take place. ) • These calculations are made in split seconds using complex rules and code. • Nursing Workload Acuity scores are calculated in Epic the same way, based on the presence of orders and nursing documentation.
How Are Nursing Workload Acuity Scores Generated In Epic? • More than 180 rules make up the total Nursing Workload Acuity score for each patient. • These rules look at nursing documentation related to Activities of Daily Living, Patient Admission, Patient Assessments, Patient Discharges, Wounds, Ostomy’s Lines, Drains, Airways, Medications, Orders, Patient Intensity of Needs, and Risks
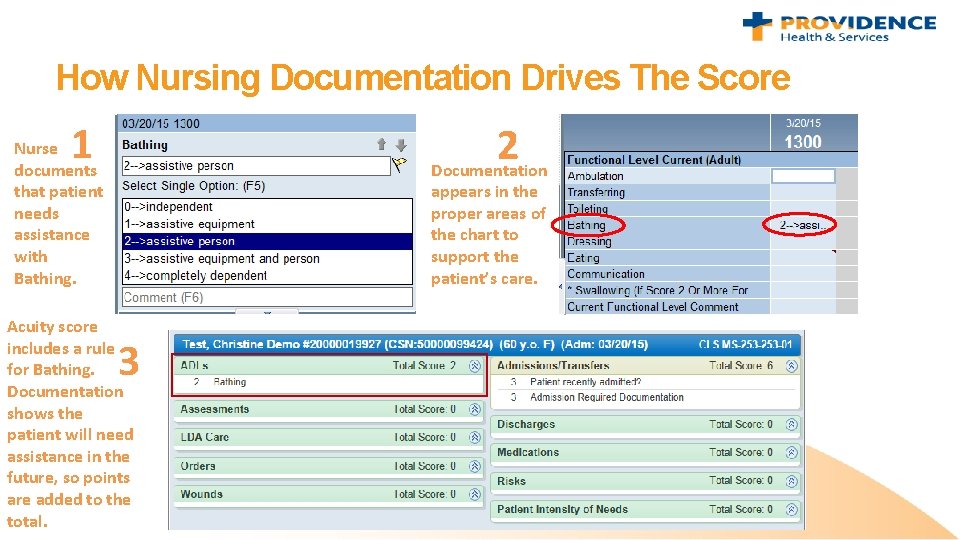
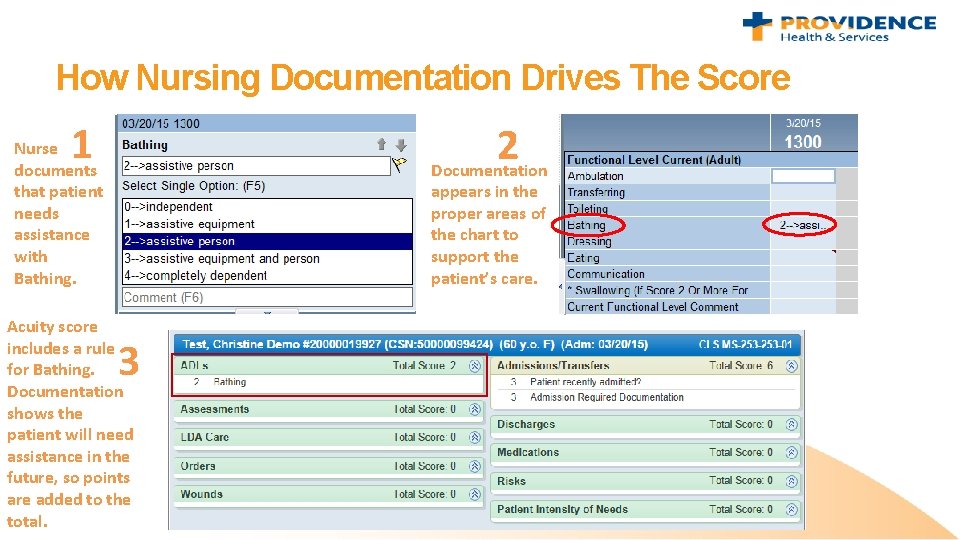
How Nursing Documentation Drives The Score 1 2 Documentation Nurse documents that patient needs assistance with Bathing. appears in the proper areas of the chart to support the patient’s care. Acuity score includes a rule for Bathing. Documentation shows the patient will need assistance in the future, so points are added to the total. 3
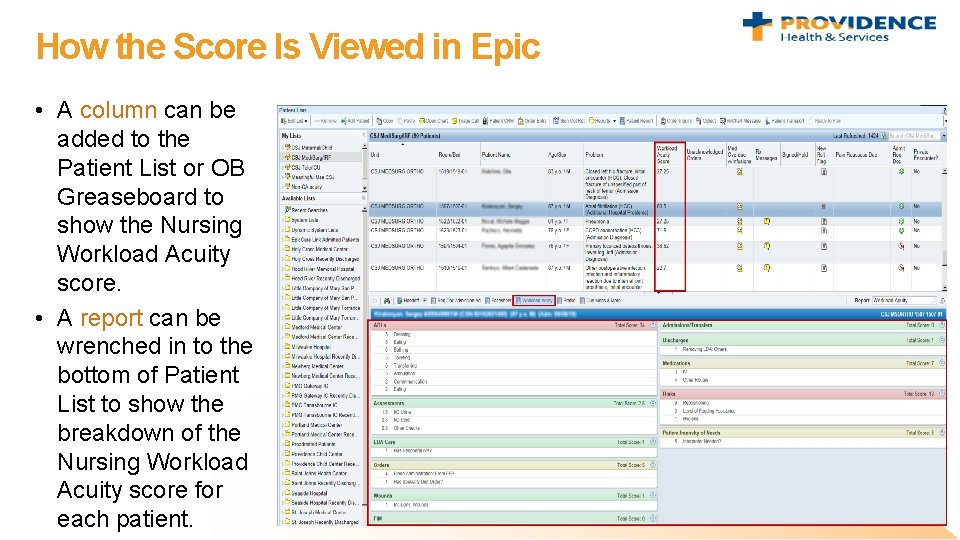
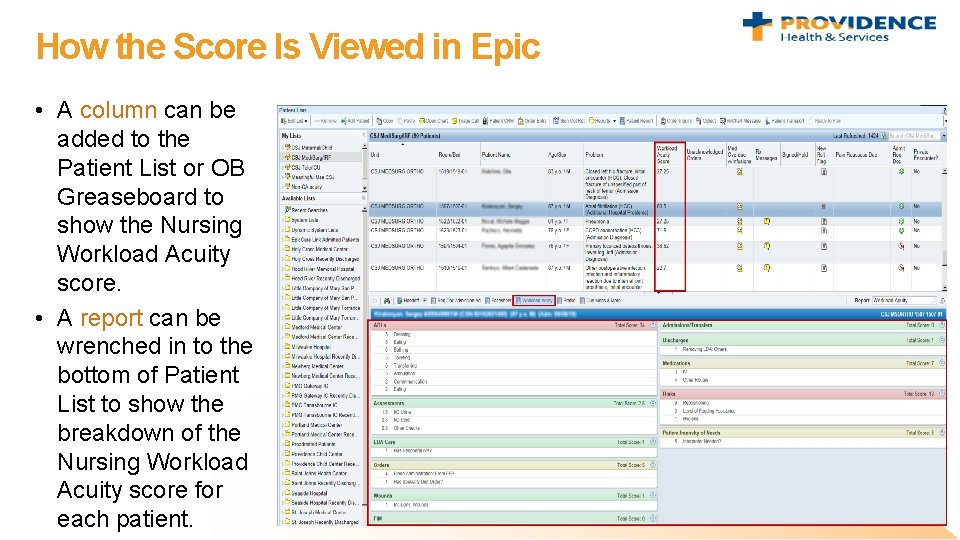
How the Score Is Viewed in Epic • A column can be added to the Patient List or OB Greaseboard to show the Nursing Workload Acuity score. • A report can be wrenched in to the bottom of Patient List to show the breakdown of the Nursing Workload Acuity score for each patient.

The Project…
Phases of the Project – Informatics 101 • • • Phase 0 – Foundational Work Phase 1 – Development Phase 2 – Technical Build and Testing Phase 3 – Deployment Phase 4 - Validation Testing - Iterative Phase 5 – Ongoing Maintenance and Validation
Phase 0 – Foundational Work
Standardization of Nursing Documentation • Nursing Education and Informatics partnership to define and build in the electronic health record (EHR) evidence based required elements of documentation for each Nursing specialty. – Focus on defining: • • Initial and ongoing assessment Care planning Patient education Common interventions – Regional policies developed to support identified required documentation elements

Phase 1 – Tool Development
Established & Followed Guiding Principles of Collaboration As one ministry committed to excellence, we work together to garner expert to expert knowledge across Providence, and rapidly deploy that knowledge with high reliability for every person in every community we serve. • Provide a framework for decision making while leaving room for creativity and flexibility to accomplish dynamic work. • All standards will be based on the highest level of evidence available, and the expertise of practicing clinicians. • These standards will be consistently applied and implemented to pursue opportunities to improve quality and outcomes, facilitate patient and family centered care, increase efficiency, minimize variation and decrease costs. • The use of technology will be standardized to achieve these objectives. • Deviations from these standards will be approved only in response to or as necessary for: • Unique clinical services (i. e. , Tattoo Removal) • Unique characteristics of a patient population (i. e. , Acute Psychiatric, Chemical Dependency) • Unique regulatory requirements (i. e. , Psychotropic Medications, SNF’s)
Collaborative Design Sessions • Over 125 expert nurses representing five states were in attendance with Providence California nurses comprising 50% of the team. • Two in-person two day long design sessions were held in Burbank, California. • Initial meeting helped the large group to learn about the Acuity process, as it was not familiar to everyone in the room. • Then broke into specialty based teams (Medical/Surgical, Ortho, Telemetry, ICU/CCU, Oncology, Pediatrics, PICU, NICU, Obstetrical, Acute Rehab) to begin to develop our acuity rules. • A series of online specialty based design meetings were held for each Nursing specialty

Phase 2 – Technical Build and Testing
Soft Launch: July-September 2015 • The finished build was moved into a soft launch phase for validation to make sure it was working as planned. • Over 45 days a clinical validation of the build across Providence’s six California acute care ministries was completed. • Tool was available in the EHR but only accessible to project participants • Validation of build was led by the projects subject matter experts (SMEs) in each specialty in partnership with Clinical Informatics. • Tasked with comparing the results from the new tool using two modalities: scoring being submitted to the staffing office using paper acuity tools and expert nursing judgment
Soft Launch: Feedback • Clinical Informatics collected more than 2000 pieces of feedback during the soft launch. Initially grouped feedback: • 50% items that users agreed were working as designed • 24% non-issues (general comments vs a problem) • 20% build issues • 6% training issues • After closer review, the majority of items initially considered to be build issues actually turned out to be training issues – the rule existed and was working, but the documentation was not done correctly… an opportunity to reinforce documentation standards!

Phase 3 – Implementation
Pre- Implementation : Training • Training – 2 hours of required education for every Providence California acute care Nurse and Informaticist – Online learning modules • Documentation policy education • Acuity tool education – In-department training by nursing subject matter experts • Pre - Live Informatics Support – Nursing department shift huddle support – Informatics and SME rounding – Drop in Informatics office hours – Developed implementation guidebooks and “tips and trick” handouts
Implementation : Go Live and Support • “Big bang” go live across six acute care hospitals – All Nursing specialties with exception of Psychiatric nursing • Nursing SME staffing on each shift for week of go live • At elbow Clinical Informatics support – Informatics department Nursing Workload Acuity project leads at each hospital – Day and night shift Informatics rounding and support for 2 weeks post go live – Leadership of top 10 at 10 – go live issue identification and triage
Phase 4 - Validation Study - Iterative
Nine Month Post – Implementation Validation Study • Validation study performed over 7 days/14 shifts – Data collected from 30% of each inpatient nursing unit’s patient population for each shift – Patients were selected by random drawing at the beginning of the shift by unit Charge Nurse. – Patients scoring was validated after 0200 and 1400 • SMEs managed data collection and discussion of the scores with each nurse while completing the tool and provided education reinforcement during these conversations. • The data was used to: • Validate the patient’s acuity (NWA) score • Validate the patient’s low, moderate, high nursing workload acuity score • Identify any patient “acuity” outliers / trends on unit
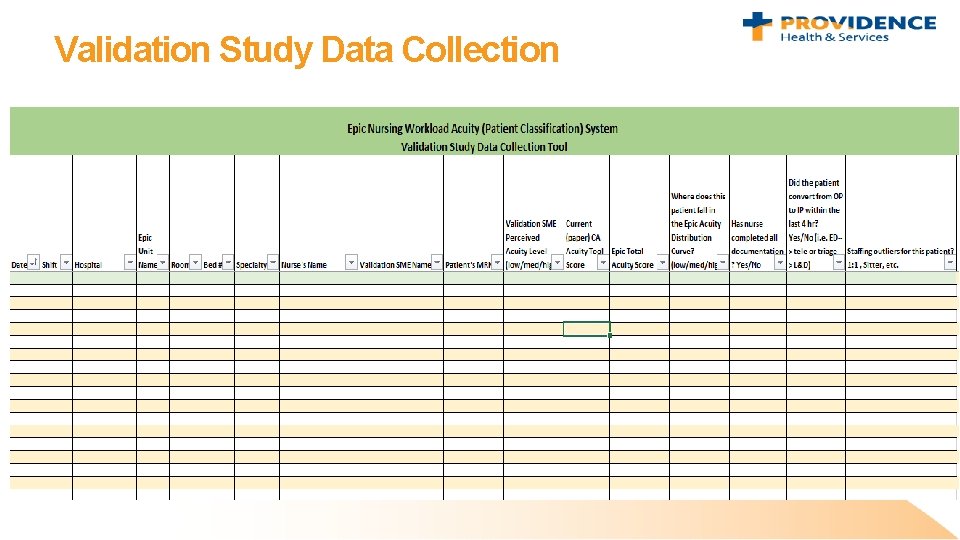
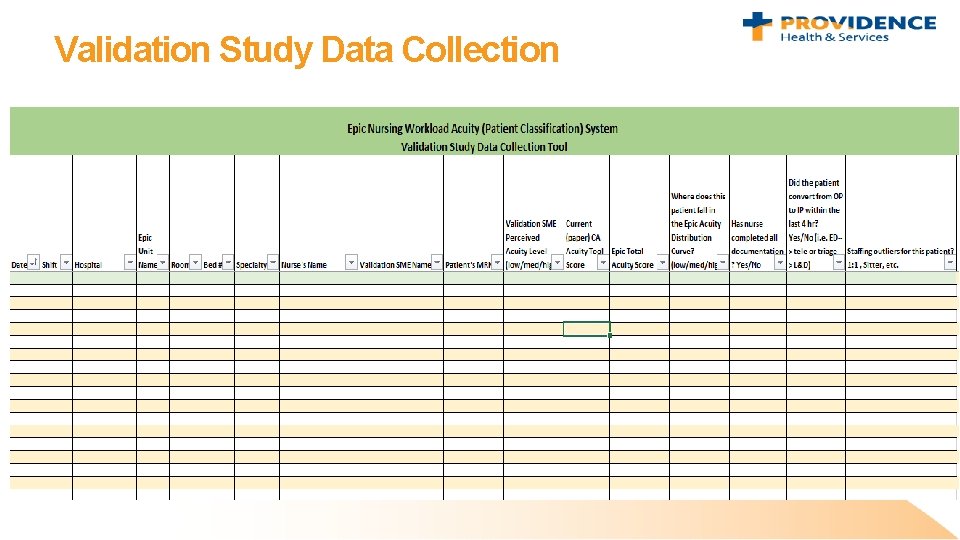
Validation Study Data Collection
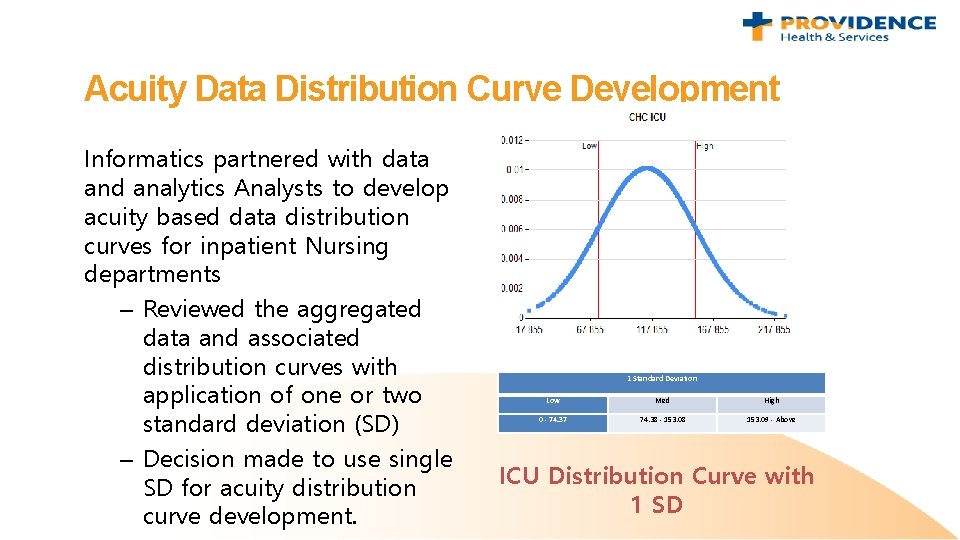
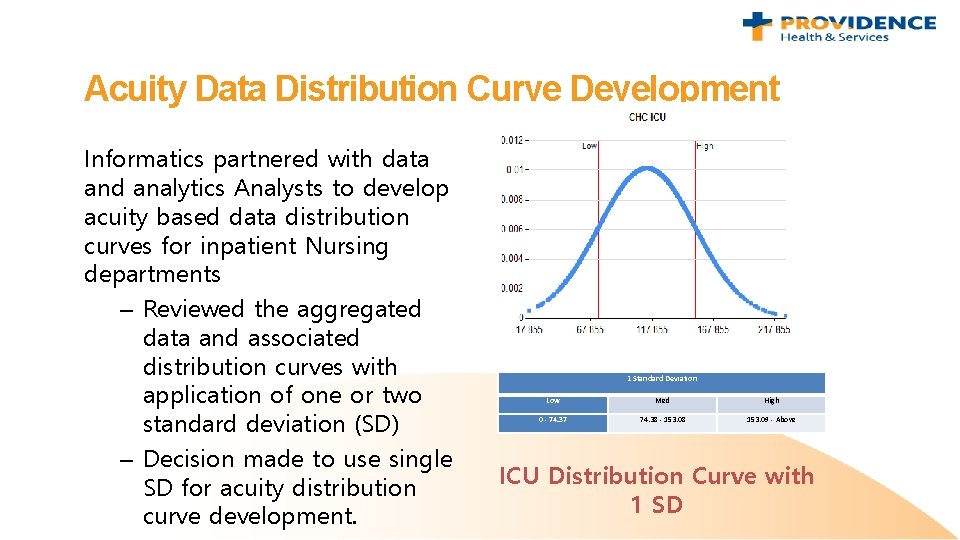
Acuity Data Distribution Curve Development Informatics partnered with data and analytics Analysts to develop acuity based data distribution curves for inpatient Nursing departments – Reviewed the aggregated data and associated distribution curves with application of one or two standard deviation (SD) – Decision made to use single SD for acuity distribution curve development. 1 Standard Deviation Low Med High 0 - 74. 37 74. 38 - 153. 08 153. 09 - Above ICU Distribution Curve with 1 SD

Phase 5 – Ongoing Maintenance and Validation The Care and Feeding…
Need for on-going review, validation and build alignment • EHR Optimization is a continual process – Requires well maintained documentation of all Nursing related documentation changes – Annual review of the prior years changes with update to Acuity tool scoring – Established “slotting” for Acuity soring in optimization cycle with dedicated resources – Annual validation of the Acuity scores and data distribution curves

The Subject Matter Experts (SME) – A Critical Role in Success
The Socializers and Validation Study Leaders. Clinical practice implementation leaders in each ministry • Facilitated communication between ministry, project team, department managers and NWA unit champions • Participated in the development of the implementation plan. • Championed and supported the implementation • Resolved issues and conflict as they arose • Helped clinicians settle into use of new technology and/or clinical practice • Fostered integration of new technology/practice into work culture • Worked to ensure colleague support for new technology/practice • Modeled professional behavior, self development, and positive attitude
The Champions – Department Super Users & Subject Matter Experts • Assisted with organizational change management: – Provided the project with guidance from active clinicians with subject matter expertise. – Led department level communication and guided acceptance by end users. – Demonstrated a greater sense of accountability for the success of the new technology and/or clinical practice implementation • Provided implementation support: – Participate in the validation study for each department assisting with process, training, technical and workflow support, bring direct operational knowledge to these activities. • Post go live support – The SMEs and Champions will provide ongoing day-to-day knowledge triage and department level expert support for end users
What Process Did The Project Team Use?

Appendix
Rules for Activities of Daily Living (ADL) • • Ambulation Bathing Communication Dressing Eating Swallowing Toileting Transferring
Rules for Admissions • • Patient recently admitted Admission documentation is complete Orders placed Transfer order out of unit
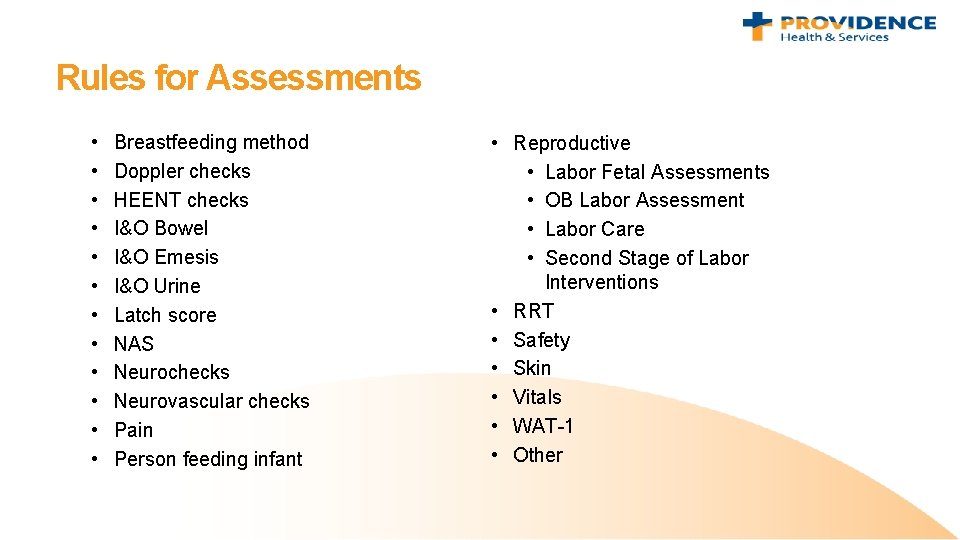
Rules for Assessments • • • Breastfeeding method Doppler checks HEENT checks I&O Bowel I&O Emesis I&O Urine Latch score NAS Neurochecks Neurovascular checks Pain Person feeding infant • Reproductive • Labor Fetal Assessments • OB Labor Assessment • Labor Care • Second Stage of Labor Interventions • RRT • Safety • Skin • Vitals • WAT-1 • Other
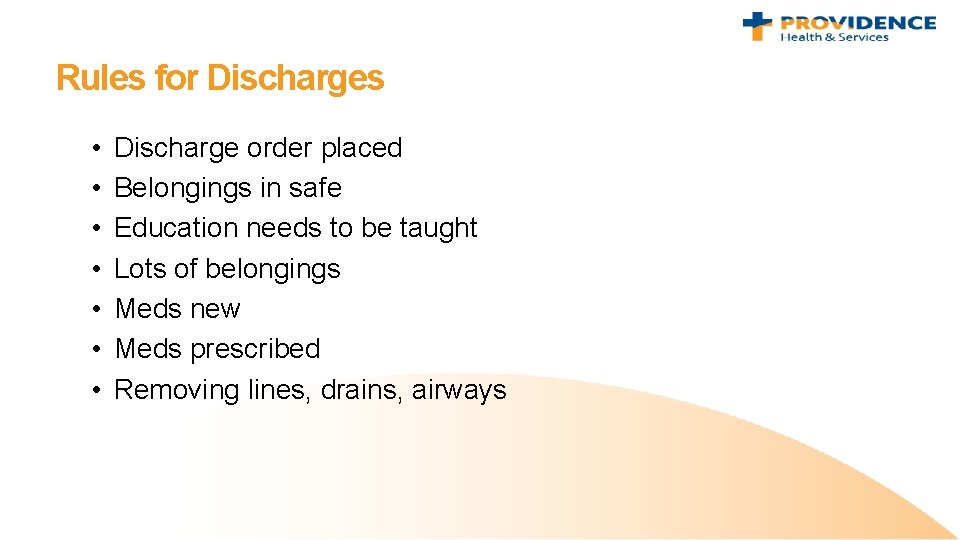
Rules for Discharges • • Discharge order placed Belongings in safe Education needs to be taught Lots of belongings Meds new Meds prescribed Removing lines, drains, airways
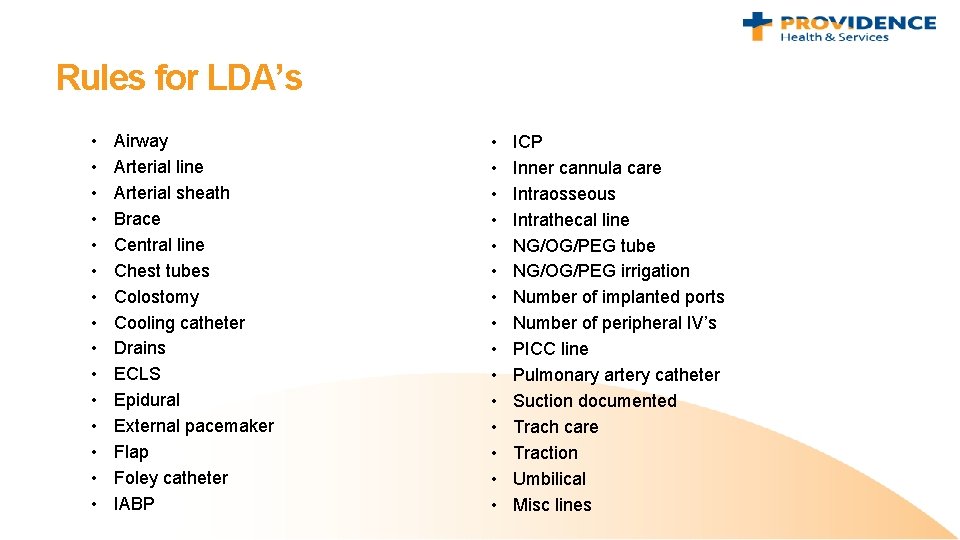
Rules for LDA’s • • • • Airway Arterial line Arterial sheath Brace Central line Chest tubes Colostomy Cooling catheter Drains ECLS Epidural External pacemaker Flap Foley catheter IABP • • • • ICP Inner cannula care Intraosseous Intrathecal line NG/OG/PEG tube NG/OG/PEG irrigation Number of implanted ports Number of peripheral IV’s PICC line Pulmonary artery catheter Suction documented Trach care Traction Umbilical Misc lines
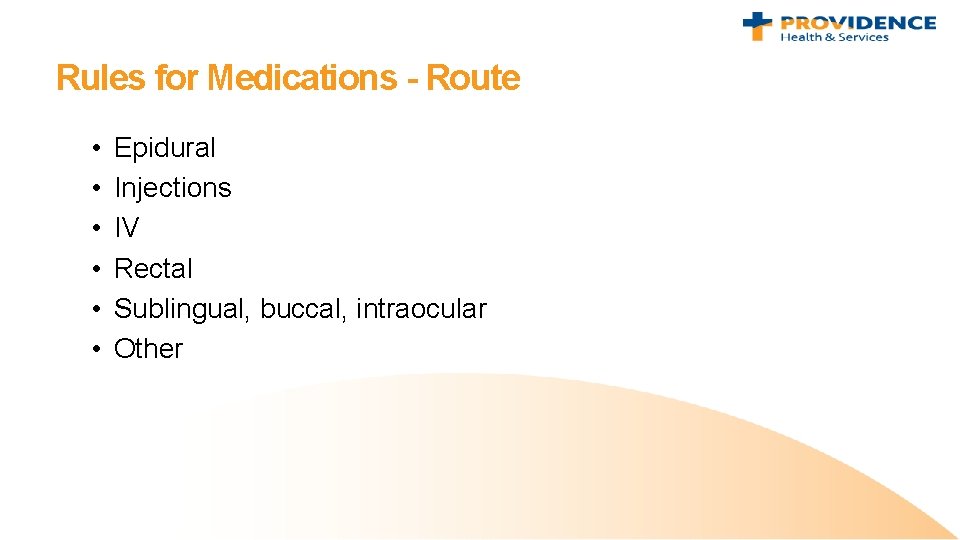
Rules for Medications - Route • • • Epidural Injections IV Rectal Sublingual, buccal, intraocular Other
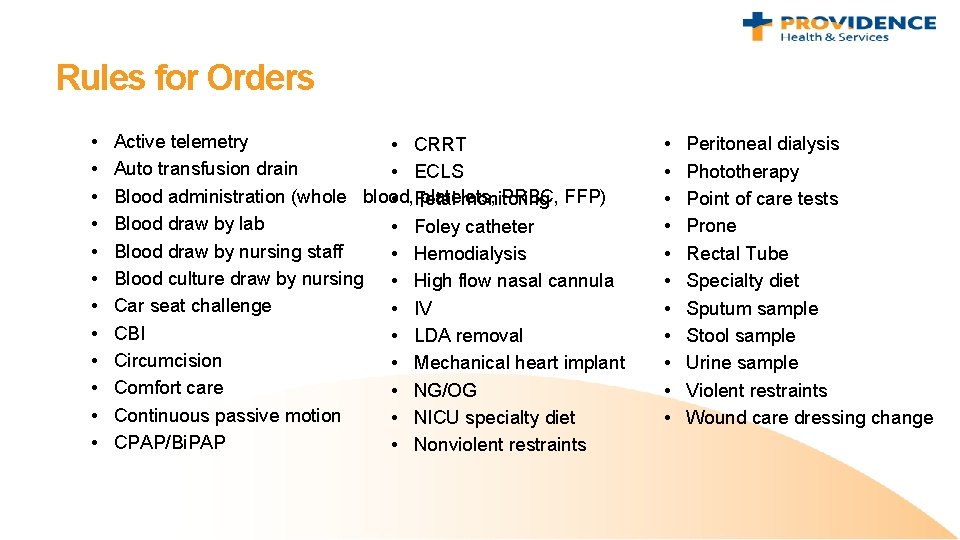
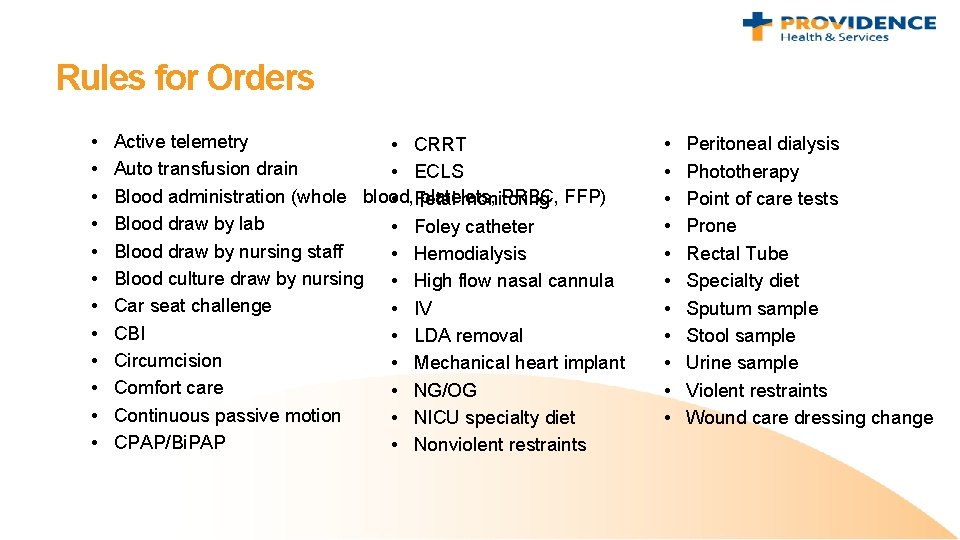
Rules for Orders • • • Active telemetry • CRRT Auto transfusion drain • ECLS Blood administration (whole blood, platelets, PRBC, FFP) • Fetal monitoring Blood draw by lab • Foley catheter Blood draw by nursing staff • Hemodialysis Blood culture draw by nursing • High flow nasal cannula Car seat challenge • IV CBI • LDA removal Circumcision • Mechanical heart implant Comfort care • NG/OG Continuous passive motion • NICU specialty diet CPAP/Bi. PAP • Nonviolent restraints • • • Peritoneal dialysis Phototherapy Point of care tests Prone Rectal Tube Specialty diet Sputum sample Stool sample Urine sample Violent restraints Wound care dressing change
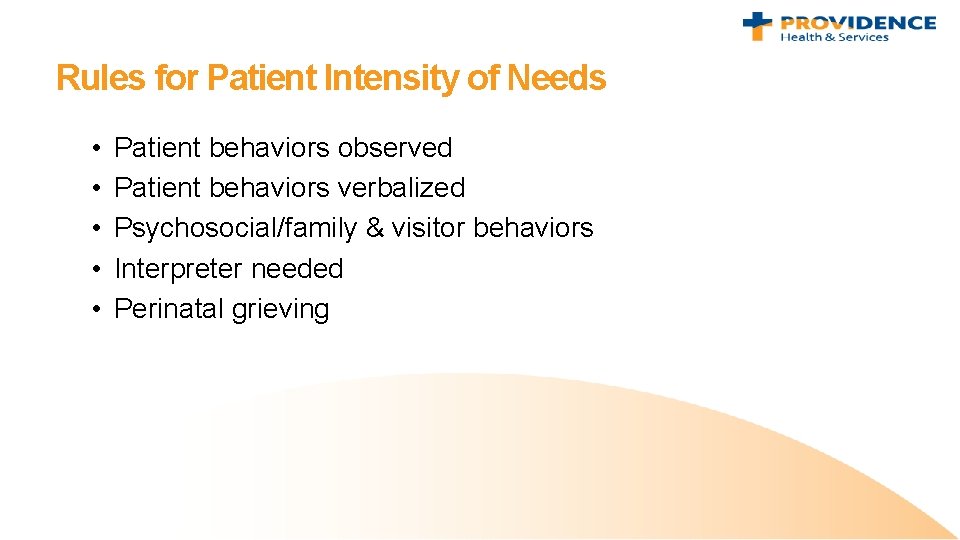
Rules for Patient Intensity of Needs • • • Patient behaviors observed Patient behaviors verbalized Psychosocial/family & visitor behaviors Interpreter needed Perinatal grieving
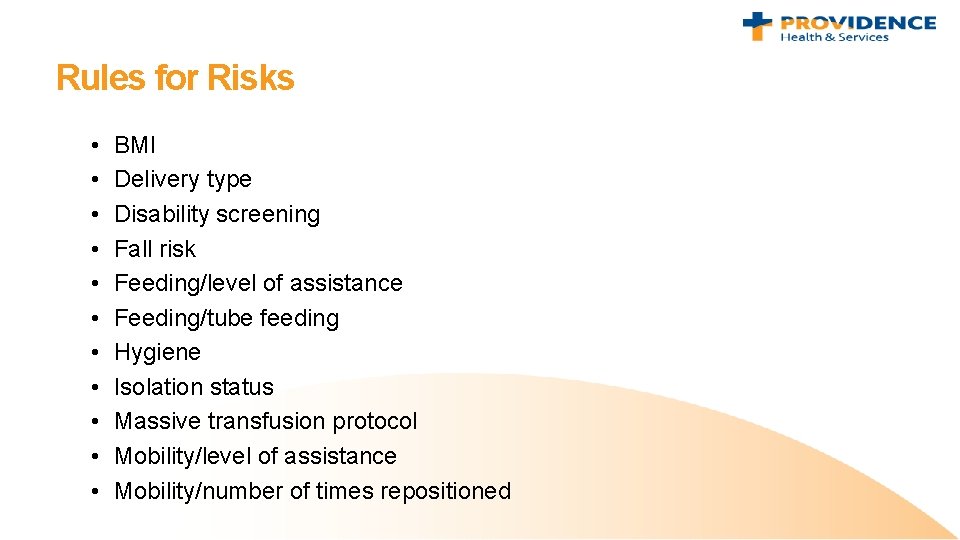
Rules for Risks • • • BMI Delivery type Disability screening Fall risk Feeding/level of assistance Feeding/tube feeding Hygiene Isolation status Massive transfusion protocol Mobility/level of assistance Mobility/number of times repositioned
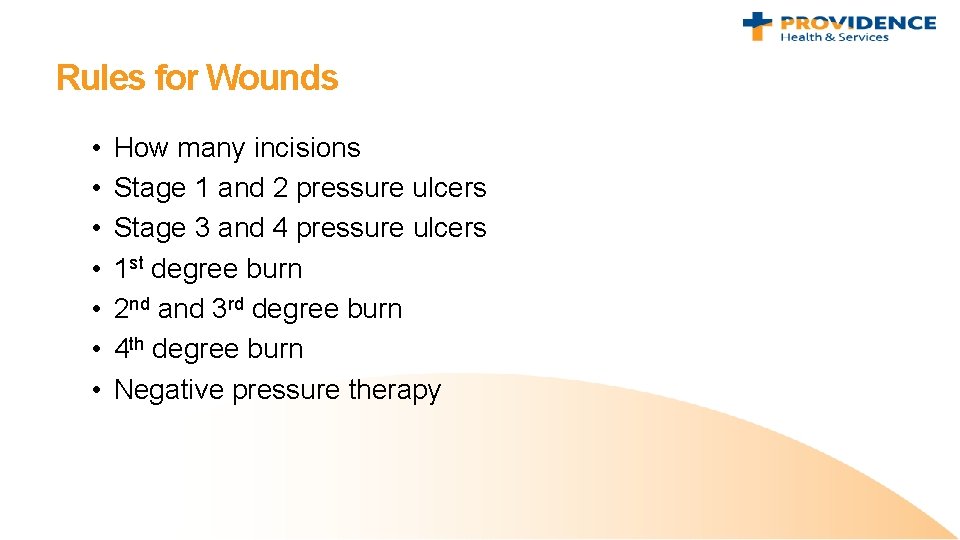
Rules for Wounds • • How many incisions Stage 1 and 2 pressure ulcers Stage 3 and 4 pressure ulcers 1 st degree burn 2 nd and 3 rd degree burn 4 th degree burn Negative pressure therapy
Rules for Acute Rehab • These rules apply to patients in all inpatient care areas except Acute Psych/IP Behavioral Health. • To fill in gaps for Acute Rehab, additional rules were devised to capture patient care tasks documented on the FIM Score Flowsheet.