Nursing Process and Nursing Care plan Learning objectives
Nursing Process and Nursing Care plan Learning objectives: v know the meaning of nursing process and critical thinking v Understand the five stages of the nursing process and how these apply to clinical practice and the provision of patient care. v Understand the implementation of nursing care plan
NURSING PROCESS DEFINITION Nursing process - A systematic, rational method of planning and providing individualized nursing care. Critical thinking – a discipline specific, reflective reasoning process that guides a nurse in generating, implementing, and evaluating approaches for dealing with client care and professional concerns. Creativity – is thinking that results in the development of new ideas and products. It is a major component of critical thinking.

Creativity in problem solving and decision making is the ability to develop and implement new and better solutions. Phases of Nursing Process: 1. Assessing 2. Diagnosing 3. Planning 4. Implementing 5. Evaluating

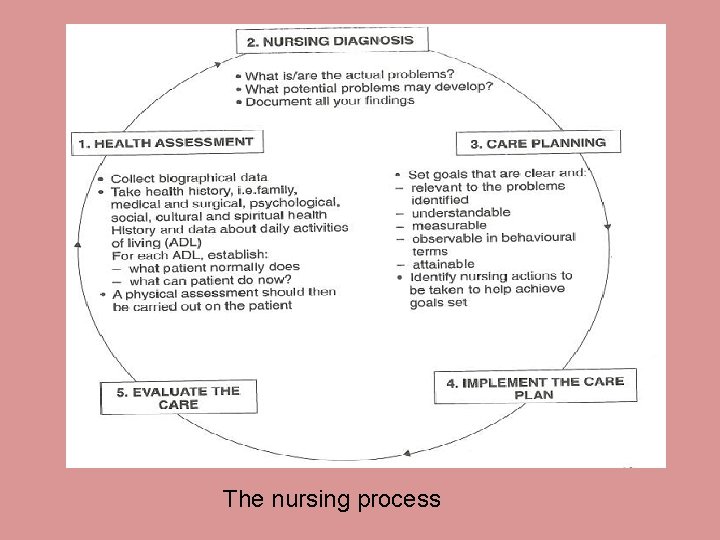
The nursing process
§ Assessment - the first phase of the nursing process involves systematically collecting, organising and analysing information about the patient, and results in the formation of nursing diagnosis. It aims to answer the question: ‘What is the actual or potential problem? ’. The assessment phase has two parts: • Information collection – the information gathered in this phase must include the nurse’s assessment of the patient and the patient’s perceptions of him/herself.
This information is gathered from the patient (primary source) but can also be gathered from other (secondary) sources such as carers, friends and others involved in care of the patient. These perceptions about a condition or disease are subjective data. - Subjective data also referred to as symptoms or covert data, are apparent only to that person affected and can be described or verified only by that person. Example, itching, pain, and feelings of worry. It also include the client’s sensations, feelings, values, beliefs, attitudes, and perception of personal health status and life situation
Objective data – also referred to as signs or overt data, are detectable by an observer or can be measured or tested against an accepted standard. They can be seen, heard or felt, or smelled, and they are obtained by observation or physical examination. During the physical examination the nurse obtains objective data to validate subjective data and to complete the assessment phase of the nursing process. Constant data is information that doesn’t change overtime such as race or blood type.
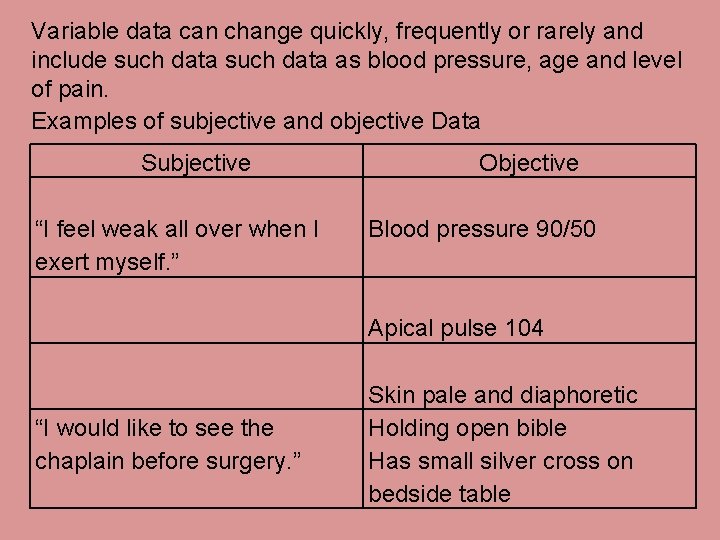
Variable data can change quickly, frequently or rarely and include such data as blood pressure, age and level of pain. Examples of subjective and objective Data Subjective “I feel weak all over when I exert myself. ” Objective Blood pressure 90/50 Apical pulse 104 “I would like to see the chaplain before surgery. ” Skin pale and diaphoretic Holding open bible Has small silver cross on bedside table
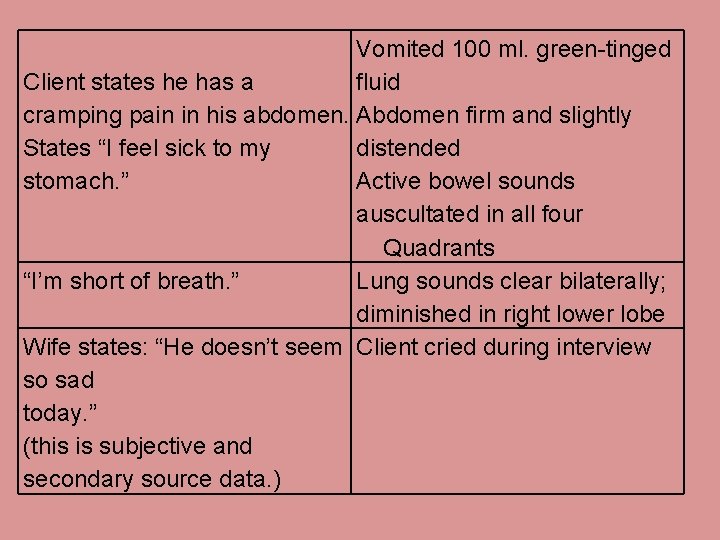
Vomited 100 ml. green-tinged Client states he has a fluid cramping pain in his abdomen. Abdomen firm and slightly States “I feel sick to my distended stomach. ” Active bowel sounds auscultated in all four Quadrants “I’m short of breath. ” Lung sounds clear bilaterally; diminished in right lower lobe Wife states: “He doesn’t seem Client cried during interview so sad today. ” (this is subjective and secondary source data. )
Assessment should include the following: 1. A brief statement about the patient’s general appearance and behaviour. 2. A comprehensive health history: a) Demographic data b) presenting complaint c) history of present illness d) Past medical history e) family medical history f) Psychosocial history
Information analysis involves organising the formation that has Been collected to make it more meaningful and easier to manage. It also reduces the chances of missing important information and allows problems to be prioritised. The analysis also includes identifying the patient’s needs, actual and /or potential problems, strengths and or diagnosis.
Nursing Diagnosis - it is a statement that describes an actual or potential health problem that requires nursing intervention. The introduction that standardised nursing diagnosis, came about in part, as a result of the nursing profession’s desire to define the scope of nursing practice, and to standardise the care given by nurses.
The difference between nursing and medical diagnosis Medical diagnosis – reach on the basis of abnormalities of structure or function. Have a narrower focus because they are based on pathology. Nursing diagnosis - reach a diagnosis on the basis of the patient’s ability to function as a result of (actual or potential) problem(s) caused by the abnormal structure or function. It is taken into account the psychological, social, spiritual, and physiological responses of the client and the family.
A doctor would make a diagnosis of “stroke” while a nurse, would make a diagnosis of “impaired physical mobility” which has occurred as a result of the stroke. Information needed to make a nursing diagnosis; P = problem (actual or potential): the key to accurate nursing diagnosis is identification that focuses attention on a current risk or potential physical or behavioural response to health or illness that may interfere with the patient’s quality of life. It deals with concerns of patient (and others) and the nurse that require nursing intervention and management.
E = Aetiology: this is the suspected cause or reason for the response that has been identified from the assessment. The nurse makes inferences based on knowledge and expertise, such as understanding of pathophysiology, and situational or developmental factors. One problem or need may have several suspected causes. S = signs and symptoms: these are manifestation (or cues) identified in the assessment that substantiate the nursing diagnosis. They are listed as subjective and objective data.
Examples: Ø Pyrexia, related to a wound infection, evidenced by inflammation around the wound, elevated temperature, flushed skin, tachycardia and tachypnoea. Ø Acute pain, related to abdominal distention as evidenced by verbal reports, non-verbal communication (guarding and posture), tachycardia and tachypnoea.
- Slides: 17