Nursing Management Osteoarthritis and Rheumatoid Arthritis What is
- Slides: 18
Nursing Management: Osteoarthritis and Rheumatoid Arthritis
What is it? 2 § Arthritis Over 100 different types § Prevalence 52. 5 million adults, 1 in 5 (CDC) Disability § Osteoarthritis and Rheumatoid Arthritis §
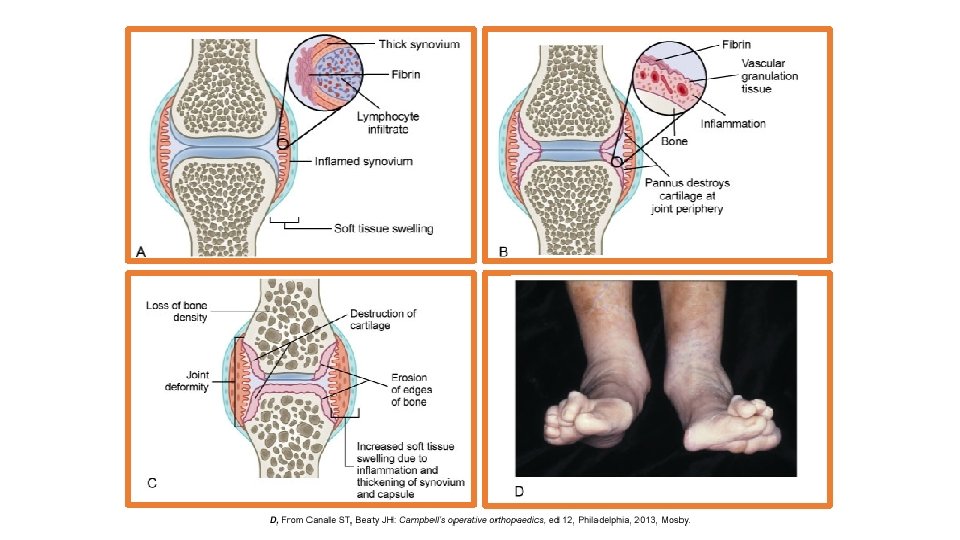
Etiology 3 Osteoarthritis § Idiopathic Unknown § Secondary Cartilage damage or joint instability Rheumatoid Arthritis Unknown § Autoimmune (? ) §
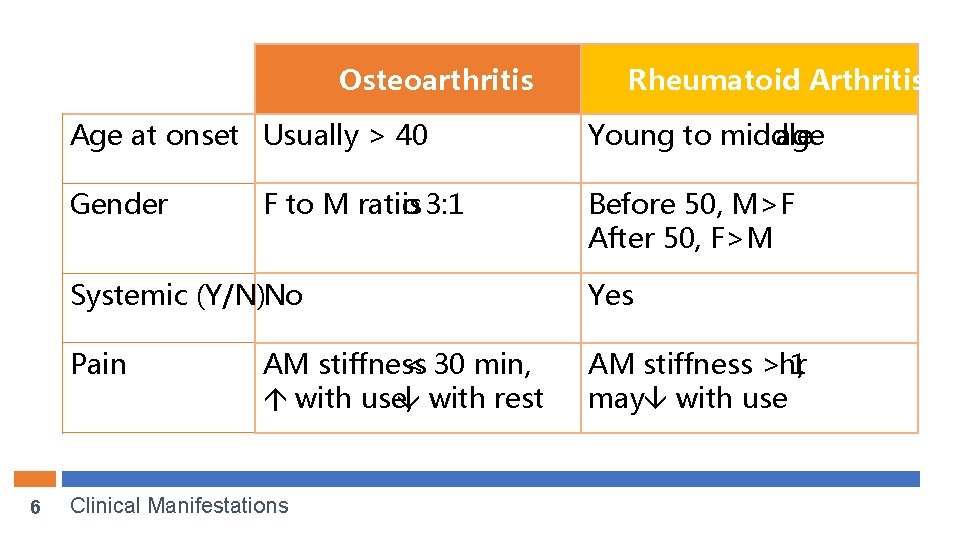
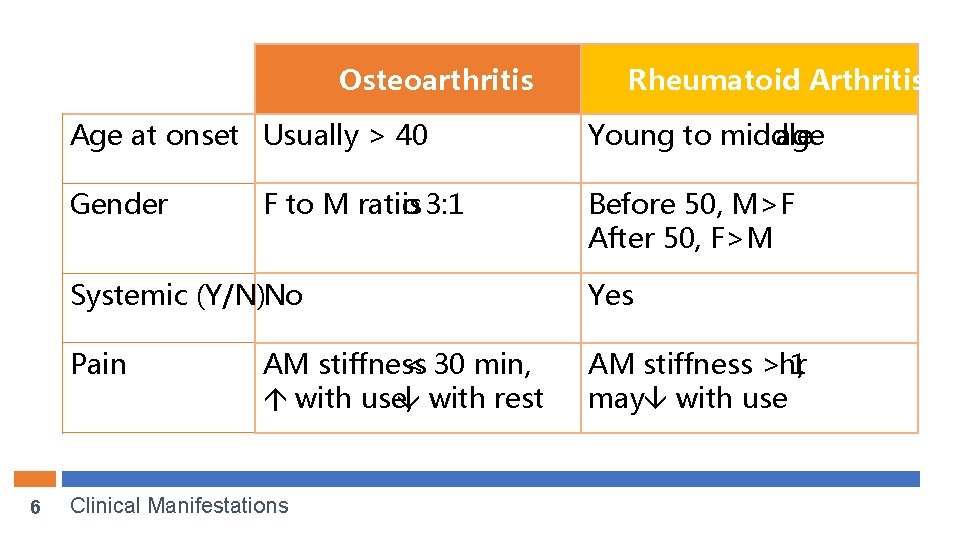
Osteoarthritis 6 Rheumatoid Arthritis Age at onset Usually > 40 Young to middle age Gender Before 50, M>F After 50, F>M F to M ratio is 3: 1 Systemic (Y/N)No Yes Pain AM stiffness >hr 1, may with use AM stiffness < 30 min, á with use, with rest Clinical Manifestations
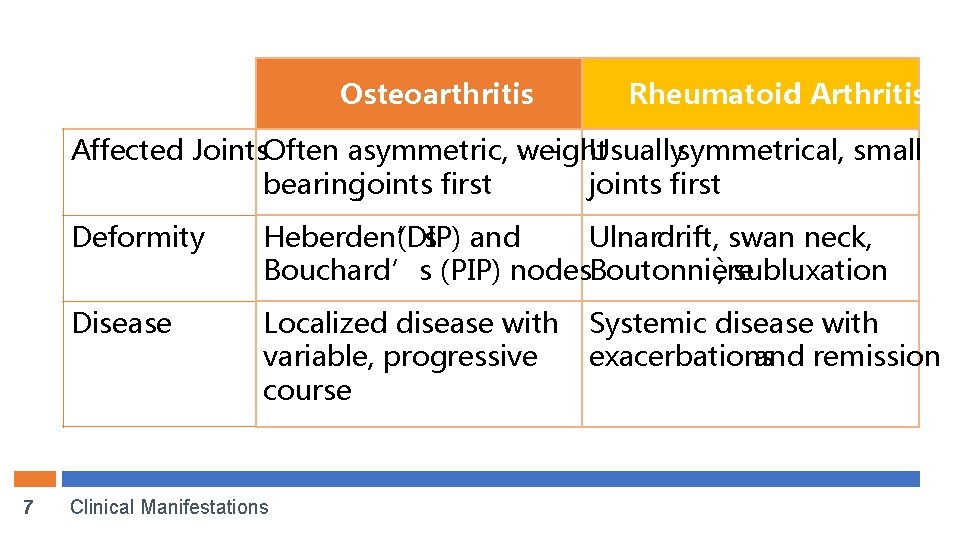
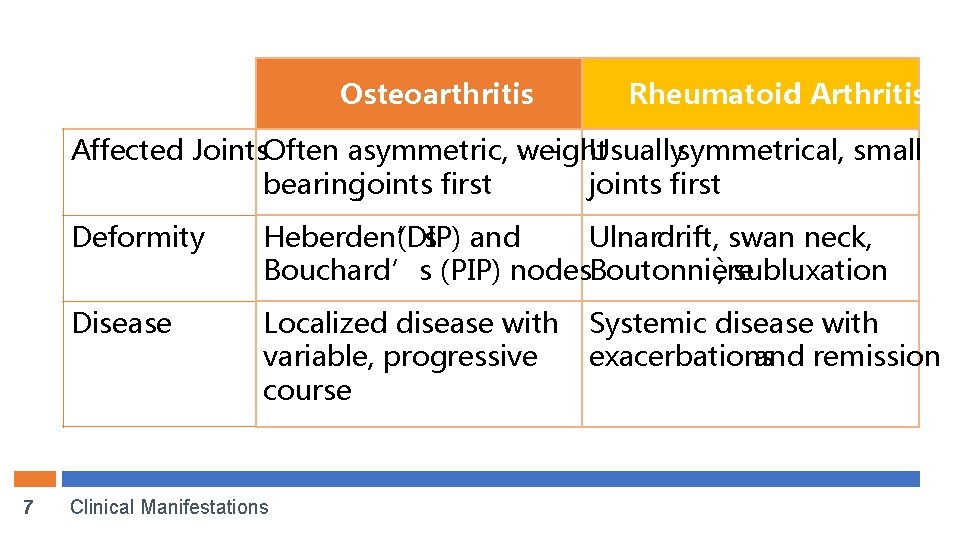
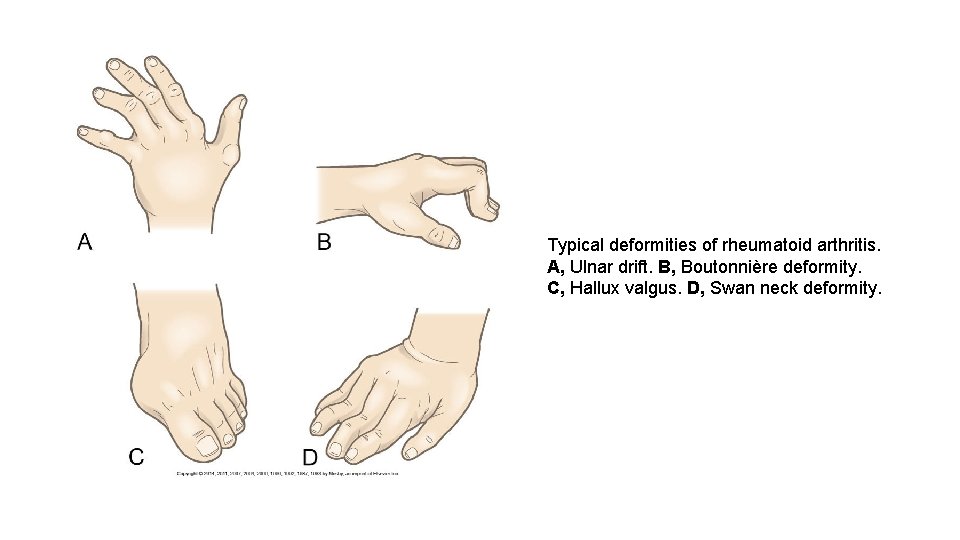
Osteoarthritis Rheumatoid Arthritis Affected Joints. Often asymmetric, weight - Usuallysymmetrical, small bearingjoints first 7 Deformity Heberden’s (DIP) and Ulnardrift, swan neck, Bouchard’s (PIP) nodes. Boutonnière , subluxation Disease Localized disease with variable, progressive course Clinical Manifestations Systemic disease with exacerbations and remission
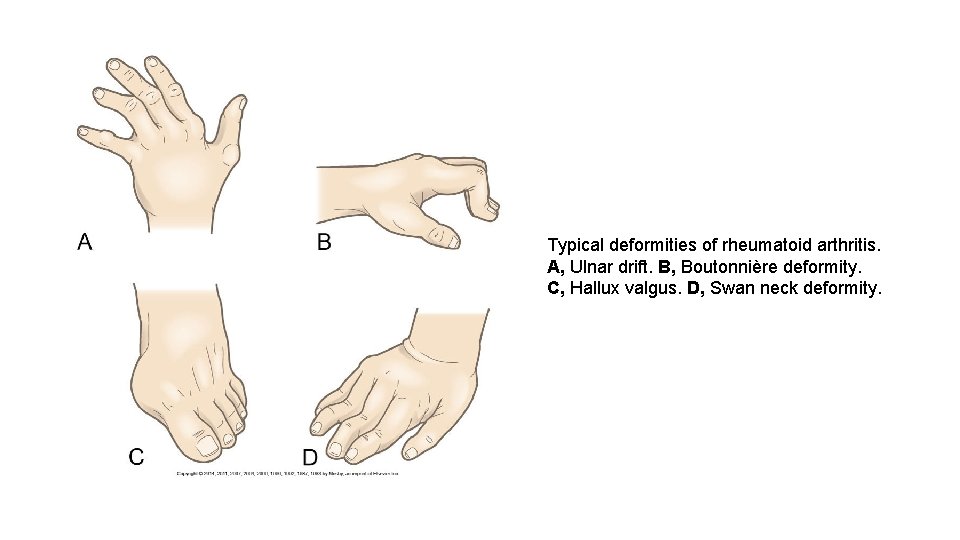
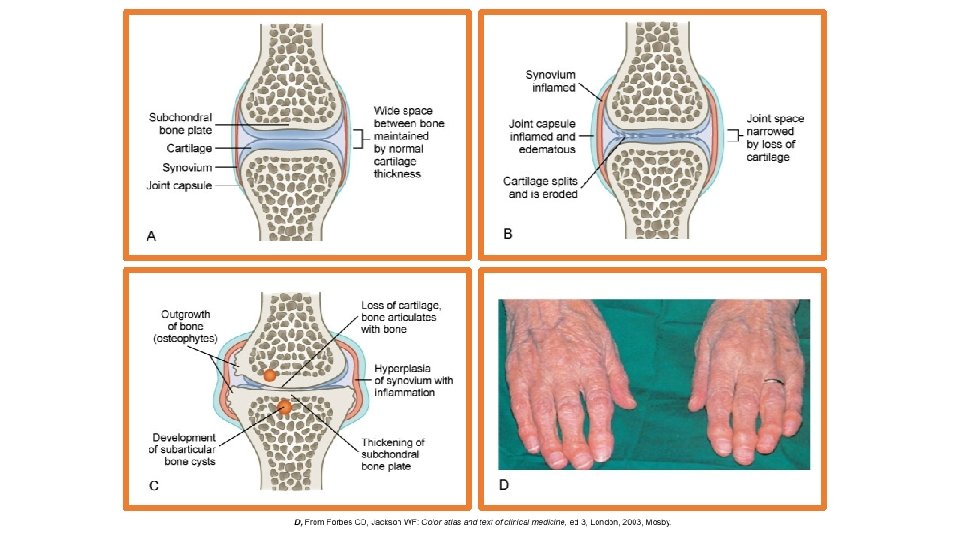
Typical deformities of rheumatoid arthritis. A, Ulnar drift. B, Boutonnière deformity. C, Hallux valgus. D, Swan neck deformity.
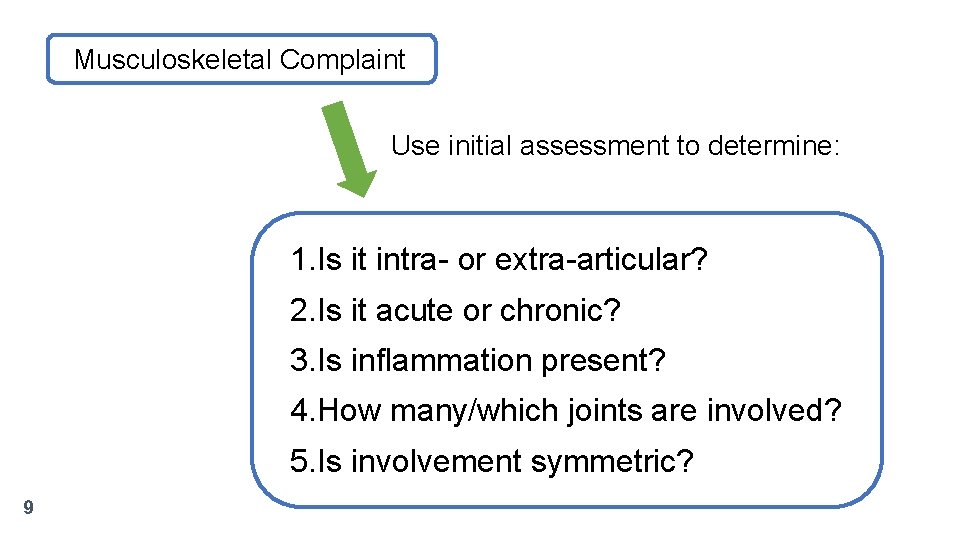
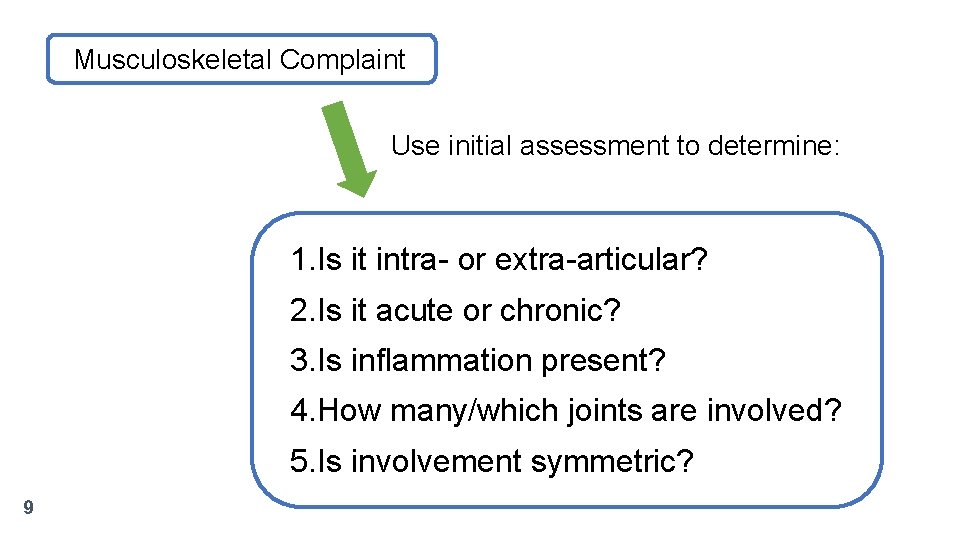
Musculoskeletal Complaint Use initial assessment to determine: 1. Is it intra- or extra-articular? 2. Is it acute or chronic? 3. Is inflammation present? 4. How many/which joints are involved? 5. Is involvement symmetric? 9
Assessment: Subjective 10 History of present illness: Symptoms Past Medical History: Medical & Surgical Hx, trauma, medication hx, menopause Social History: Diet, exercise, repetitive physical activity (sports and/or occupation) Family History: Genetic factors (RA)
Assessment: Objective 11 General: VS, appearance, demeanor, affect MSK: Symmetry, surrounding tissues, ROM, muscle strength, swelling, warmth, tenderness, redness Integument: Keratoconjunctivitis, subcutaneous rheumatoid nodules, skin ulcers Sjögren’s syndrome: lacrimal and salivary secretion GI: Splenomegaly (Felty syndrome)
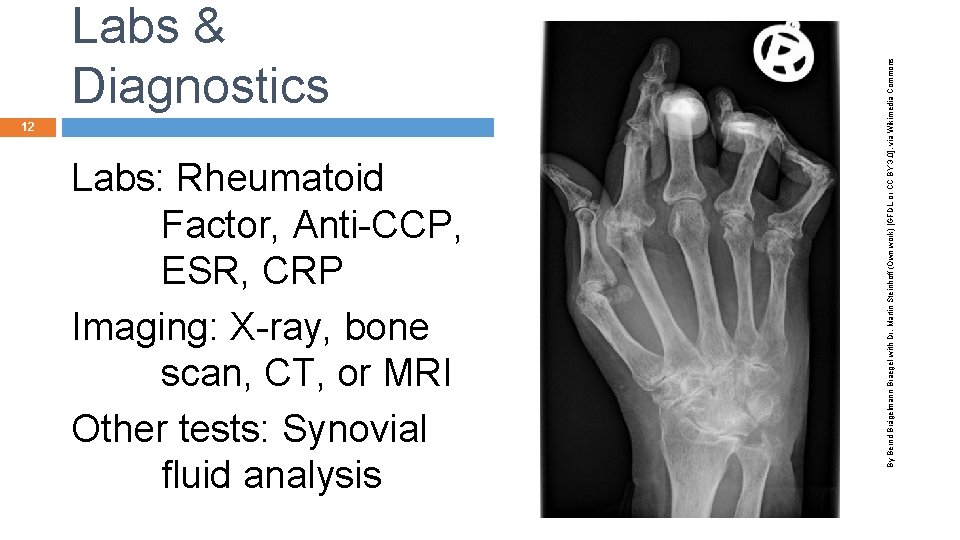
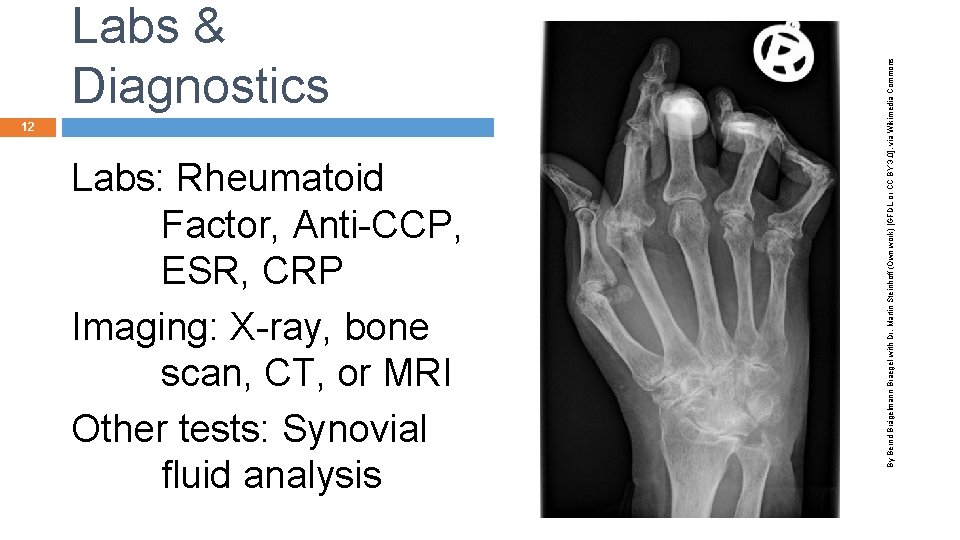
12 Labs: Rheumatoid Factor, Anti-CCP, ESR, CRP Imaging: X-ray, bone scan, CT, or MRI Other tests: Synovial fluid analysis By Bernd Brägelmann Braegel with Dr. Martin Steinhoff (Own work) [GFDL or CC BY 3. 0], via Wikimedia Commons Labs & Diagnostics
Physiological: ABCD 13 Acute or chronic pain § Impaired physical mobility § Self-care deficit §
Psychological 14 Chronic low selfesteem § Disturbed body image §
Interventions 15 Monitor: Pain, ROM, participation in ADLs Administer: Medications: NSAIDS, DMARDS Pain-relieving measures: therapeutic heat/cold, rest, relaxation techniques, biofeedback, TENS, splints, psychologic support
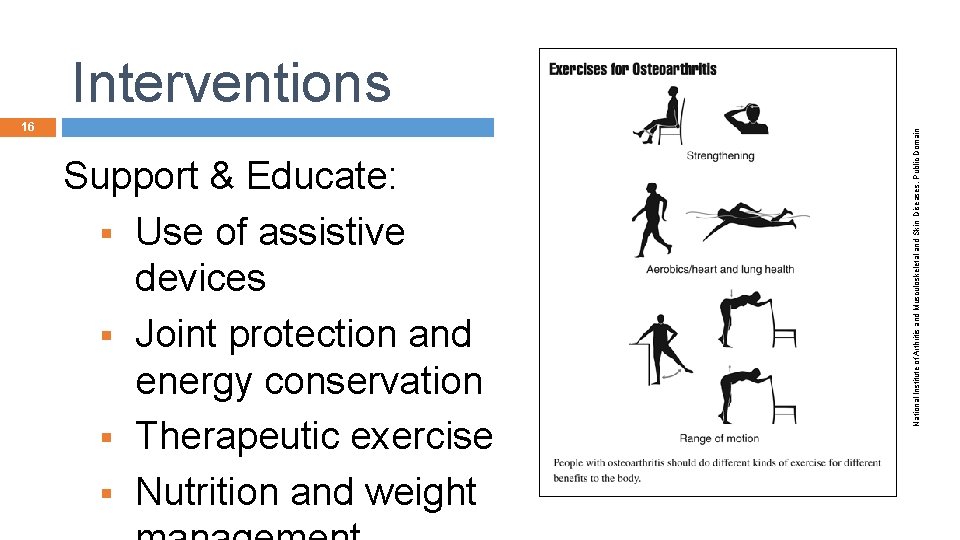
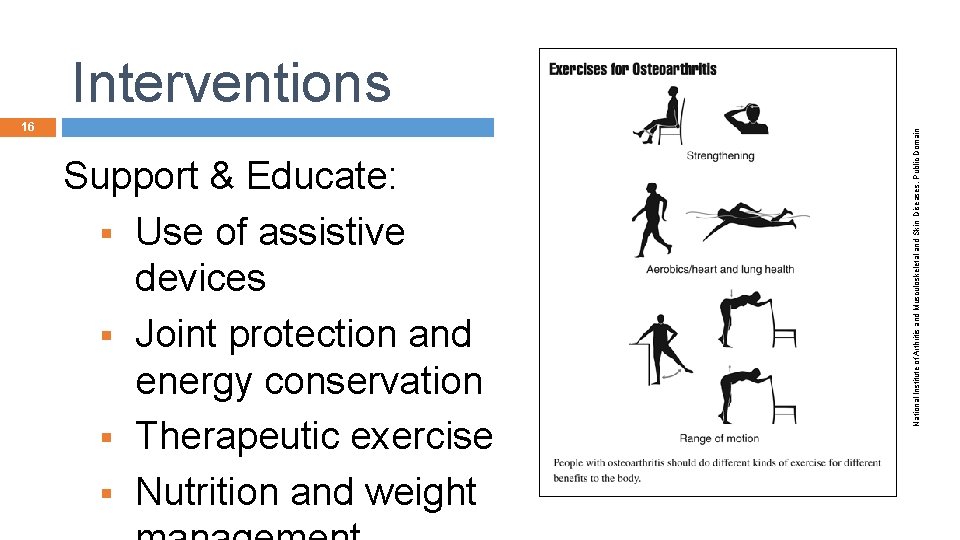
16 Support & Educate: § Use of assistive devices § Joint protection and energy conservation § Therapeutic exercise § Nutrition and weight National Institute of Arthritis and Musculoskeletal and Skin Diseases, Public Domain Interventions
Evaluation: Desired Outcomes 17 Maintenance or improvement in joint function § Effective use of joint protective measures § Management of pain through the use of both pharmacologic and non-pharmacologic strategies §
Evaluation: Desired Outcomes 18 Achievement of maximal amount of independence with ADLs § Maintenance of a positive self-image §