Nursing Considerations For Prostacyclin Therapy In The Treatment



- Slides: 45

Nursing Considerations For Prostacyclin Therapy In The Treatment Of PAH Johnell Diwan, RN, BSN Pulmonary Hypertension Clinic Coordinator Legacy Medical Group, Pulmonary & Sleep Medicine
Presentation Outline � Background and definition � Clinical classification � Pathophysiology/Natural history � Signs and symptoms/diagnosis � Treatment of PAH � Emergency Considerations
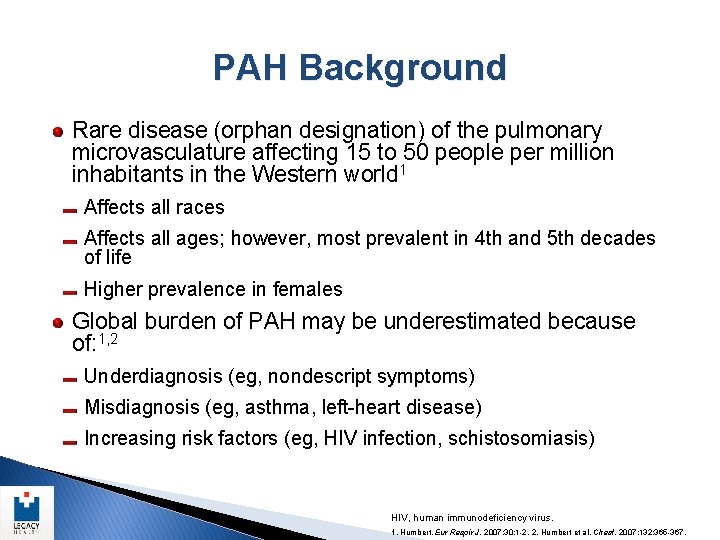
PAH Background Rare disease (orphan designation) of the pulmonary microvasculature affecting 15 to 50 people per million inhabitants in the Western world 1 Affects all races Affects all ages; however, most prevalent in 4 th and 5 th decades of life Higher prevalence in females Global burden of PAH may be underestimated because of: 1, 2 Underdiagnosis (eg, nondescript symptoms) Misdiagnosis (eg, asthma, left-heart disease) Increasing risk factors (eg, HIV infection, schistosomiasis) HIV, human immunodeficiency virus. 1. Humbert. Eur Respir J. 2007; 30: 1 -2. 2. Humbert et al. Chest. 2007; 132: 365 -367.
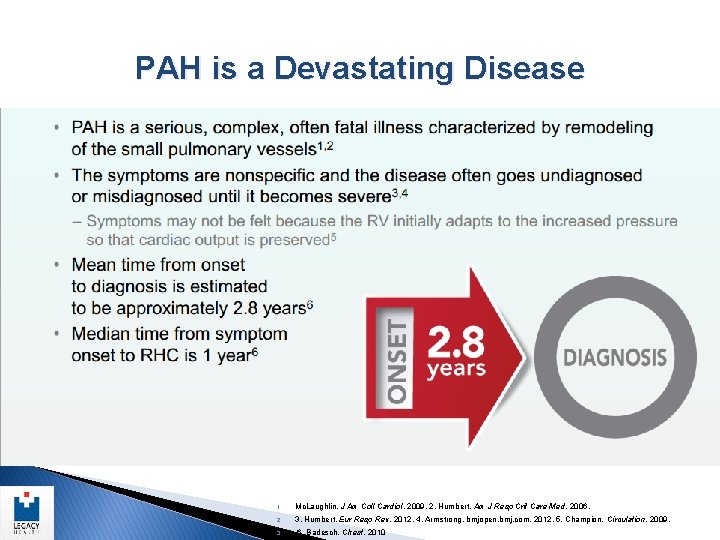
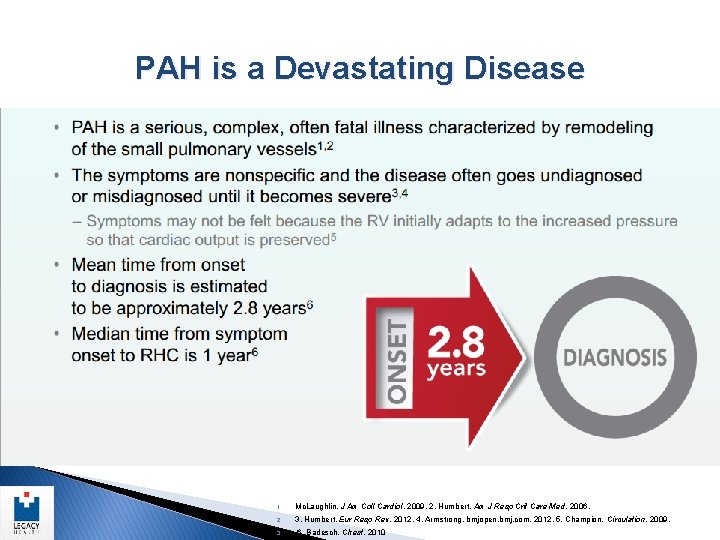
PAH is a Devastating Disease 1. Mc. Laughlin. J Am Coll Cardiol. 2009. 2. Humbert. Am J Resp Crit Care Med. 2006. 2. 3. Humbert. Eur Resp Rev. 2012. 4. Armstrong. bmjopen. bmj. com. 2012. 5. Champion. Circulation. 2009. 3. 6. Badesch. Chest. 2010
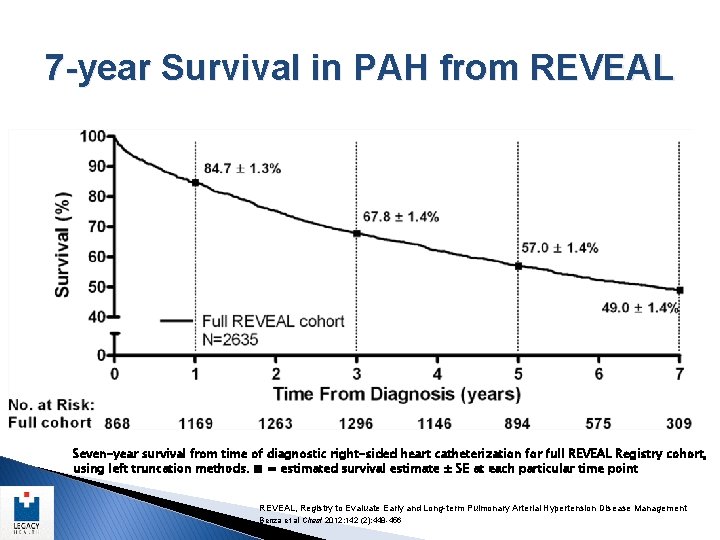
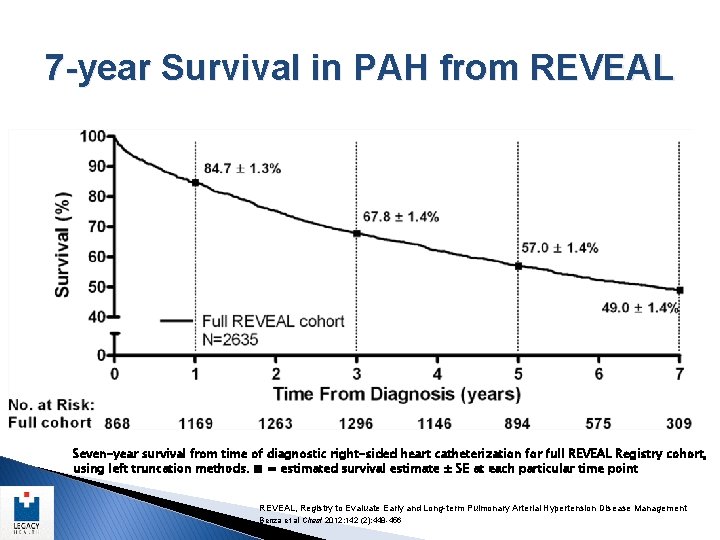
7 -year Survival in PAH from REVEAL Seven-year survival from time of diagnostic right-sided heart catheterization for full REVEAL Registry cohort, using left truncation methods. ■ = estimated survival estimate ± SE at each particular time point REVEAL, Registry to Evaluate Early and Long-term Pulmonary Arterial Hypertension Disease Management Benza et al Chest 2012; 142 (2): 448 -456
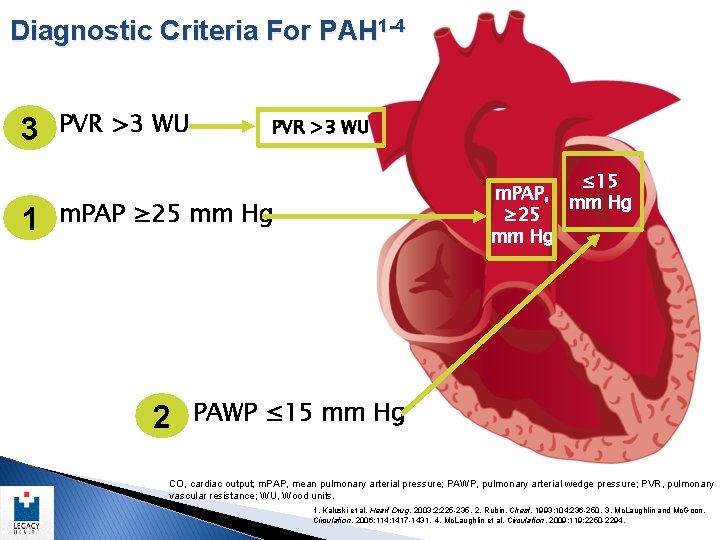
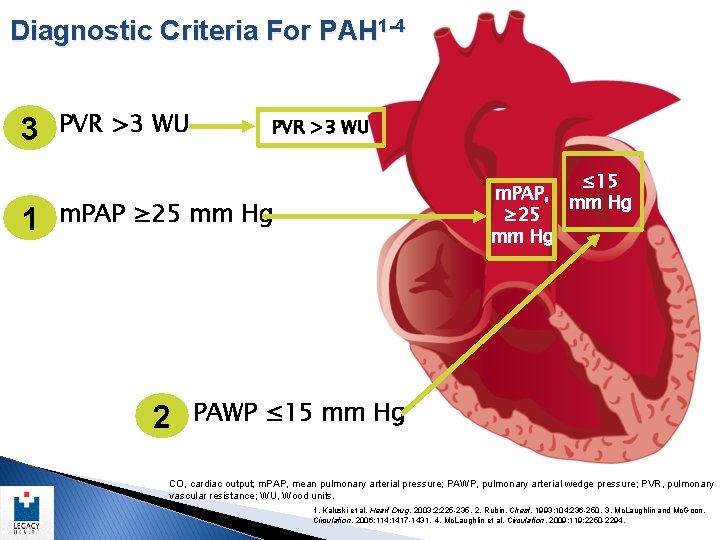
Diagnostic Criteria For PAH 1 -4 3 1 PVR >3 WU ≤ 15 m. PAP, mm Hg ≥ 25 mm Hg m. PAP ≥ 25 mm Hg 2 PAWP ≤ 15 mm Hg CO, cardiac output; m. PAP, mean pulmonary arterial pressure; PAWP, pulmonary arterial wedge pressure; PVR, pulmonary vascular resistance; WU, Wood units. 1. Kaluski et al. Heart Drug. 2003; 2: 225 -235. 2. Rubin. Chest. 1993; 104: 236 -250. 3. Mc. Laughlin and Mc. Goon. Circulation. 2006; 114: 1417 -1431. 4. Mc. Laughlin et al. Circulation. 2009; 119: 2250 -2294.
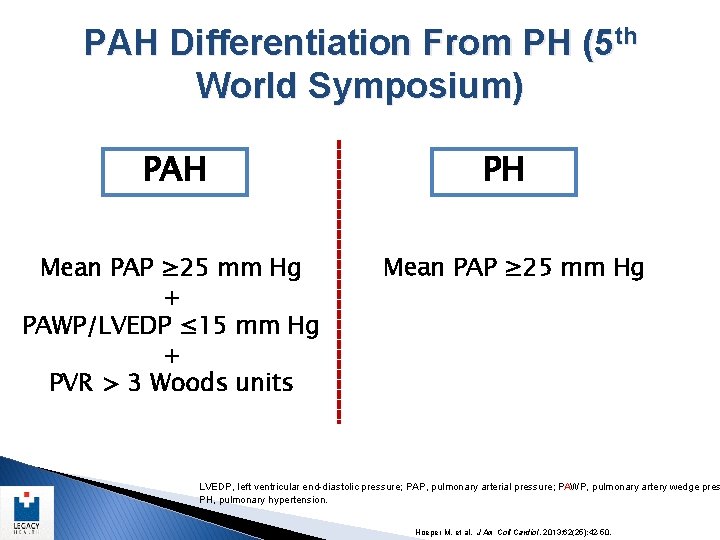
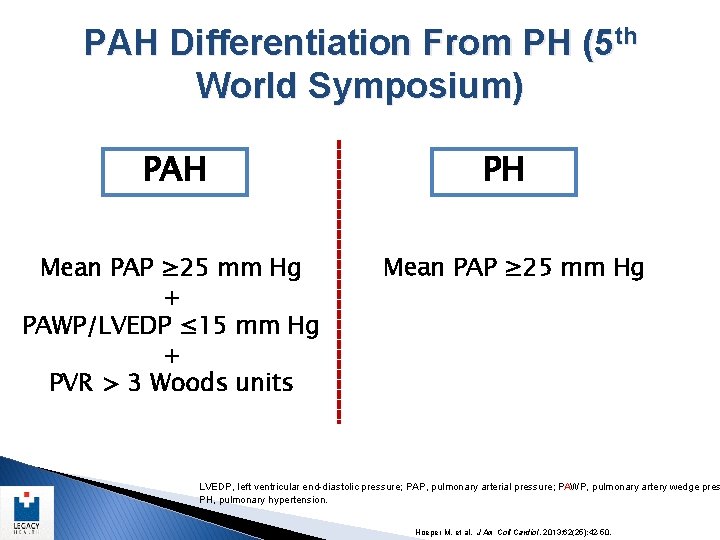
PAH Differentiation From PH (5 th World Symposium) PAH Mean PAP ≥ 25 mm Hg + PAWP/LVEDP ≤ 15 mm Hg + PVR > 3 Woods units PH Mean PAP ≥ 25 mm Hg LVEDP, left ventricular end-diastolic pressure; PAP, pulmonary arterial pressure; PAWP, pulmonary artery wedge pres PH, pulmonary hypertension. Hoeper M, et al. J Am Coll Cardiol. 2013; 62(25): 42 -50.
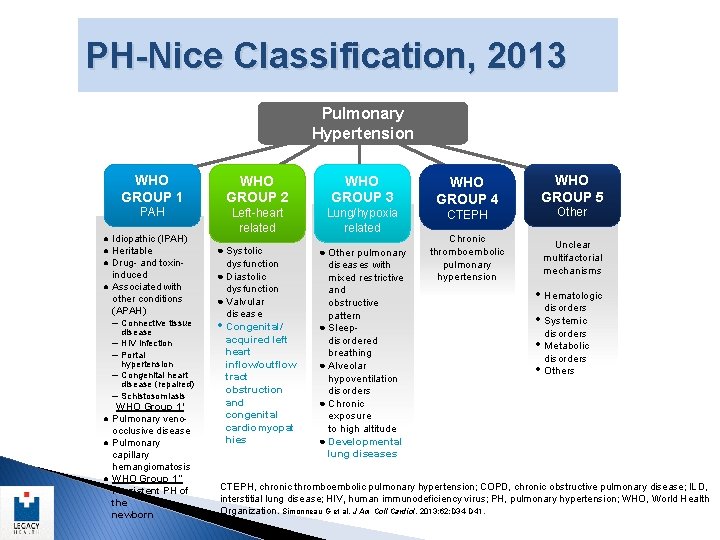
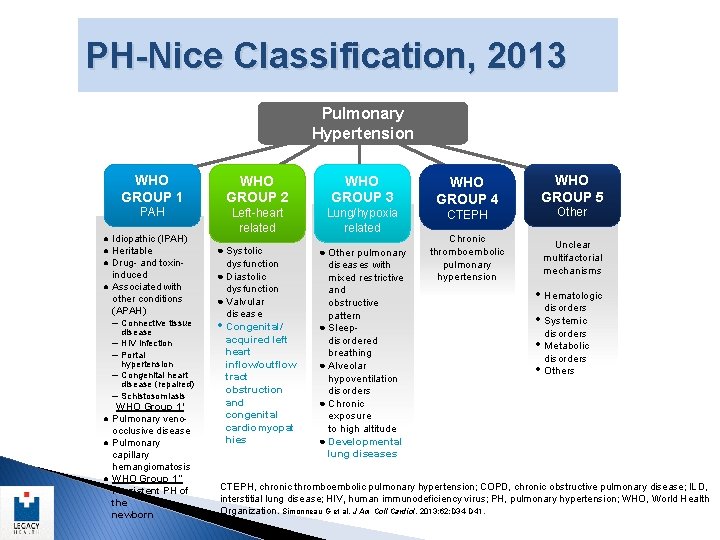
PH-Nice Classification, 2013 Pulmonary Hypertension WHO GROUP 1 WHO GROUP 2 PAH Left-heart related ● Idiopathic (IPAH) ● Heritable ● Drug- and toxininduced ● Associated with other conditions (APAH) – Connective tissue – – disease HIV infection Portal hypertension Congenital heart disease (repaired) Schistosomiasis WHO Group 1′ ● Pulmonary venoocclusive disease ● Pulmonary capillary hemangiomatosis ● WHO Group 1″ Persistent PH of the newborn ● Systolic dysfunction ● Diastolic dysfunction ● Valvular disease • Congenital/ acquired left heart inflow/outflow tract obstruction and congenital cardiomyopat hies WHO GROUP 3 Lung/hypoxia ● COPD related ● ILD ● Other pulmonary diseases with mixed restrictive and obstructive pattern ● Sleepdisordered breathing ● Alveolar hypoventilation disorders ● Chronic exposure to high altitude ● Developmental lung diseases WHO GROUP 5 WHO GROUP 4 CTEPH Other Chronic thromboembolic pulmonary hypertension Unclear multifactorial mechanisms • Hematologic • • • disorders Systemic disorders Metabolic disorders Others CTEPH, chronic thromboembolic pulmonary hypertension; COPD, chronic obstructive pulmonary disease; ILD, interstitial lung disease; HIV, human immunodeficiency virus; PH, pulmonary hypertension; WHO, World Health Organization. Simonneau G et al. J Am Coll Cardiol. 2013; 62: D 34 -D 41.
Pathophysiology/Natural History
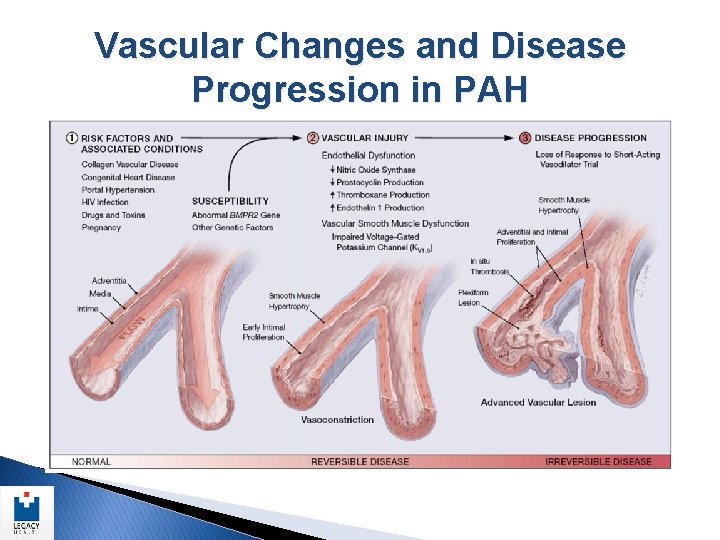
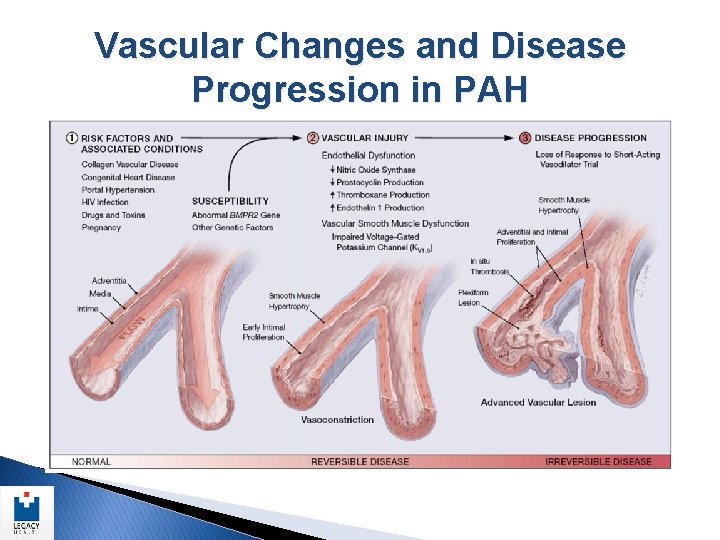
Vascular Changes and Disease Progression in PAH
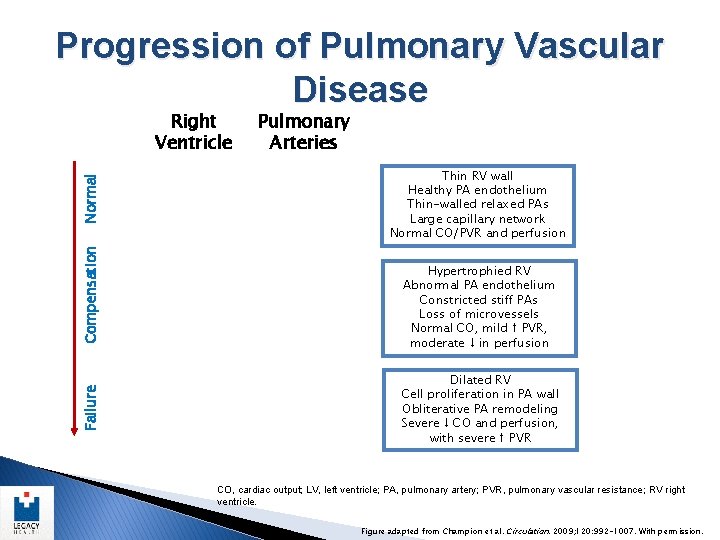
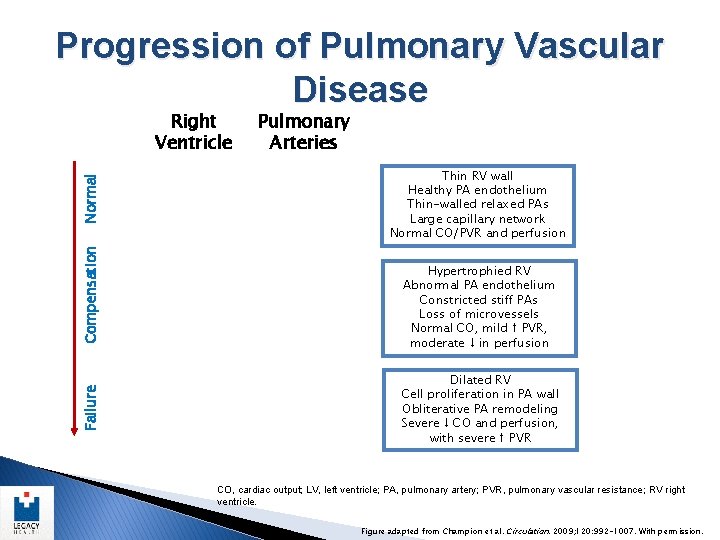
Progression of Pulmonary Vascular Disease Failure Compensation Normal Right Ventricle Pulmonary Arteries Thin RV wall Healthy PA endothelium Thin-walled relaxed PAs Large capillary network Normal CO/PVR and perfusion Hypertrophied RV Abnormal PA endothelium Constricted stiff PAs Loss of microvessels Normal CO, mild ↑ PVR, moderate ↓ in perfusion Dilated RV Cell proliferation in PA wall Obliterative PA remodeling Severe ↓ CO and perfusion, with severe ↑ PVR CO, cardiac output; LV, left ventricle; PA, pulmonary artery; PVR, pulmonary vascular resistance; RV right ventricle. Figure adapted from Champion et al. Circulation. 2009; 120: 992 -1007. With permission.

Signs and Symptoms/Diagnosis
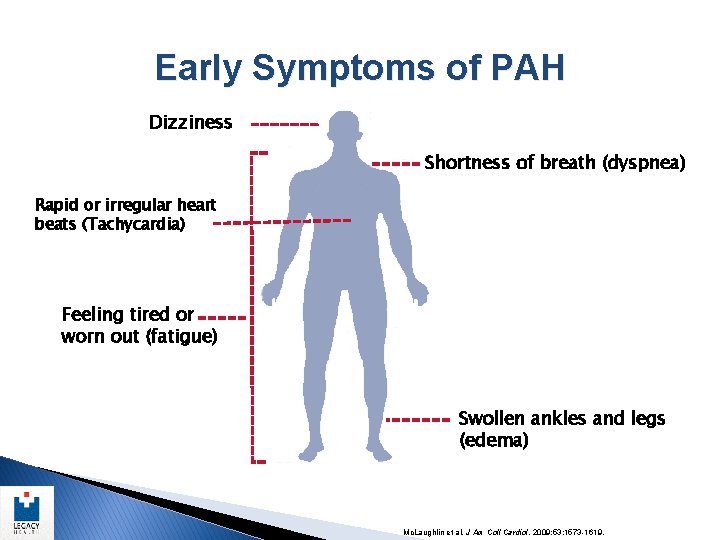
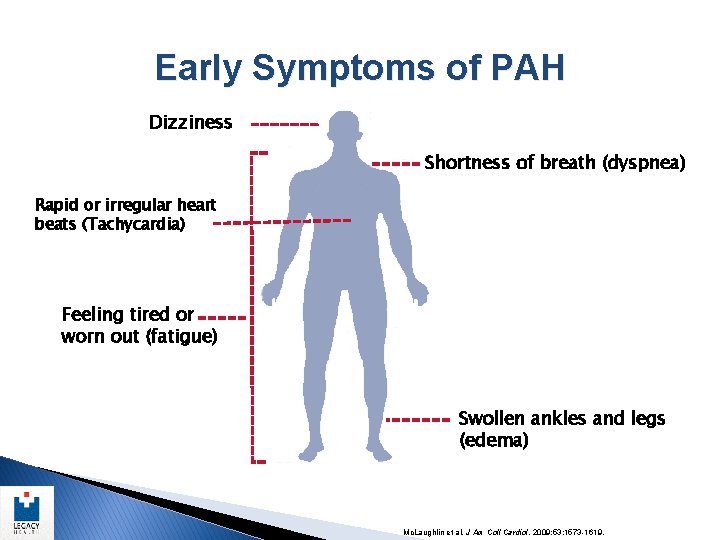
Early Symptoms of PAH Dizziness Shortness of breath (dyspnea) Rapid or irregular heart beats (Tachycardia) Feeling tired or worn out (fatigue) Swollen ankles and legs (edema) Mc. Laughlin et al. J Am Coll Cardiol. 2009; 53: 1573 -1619.
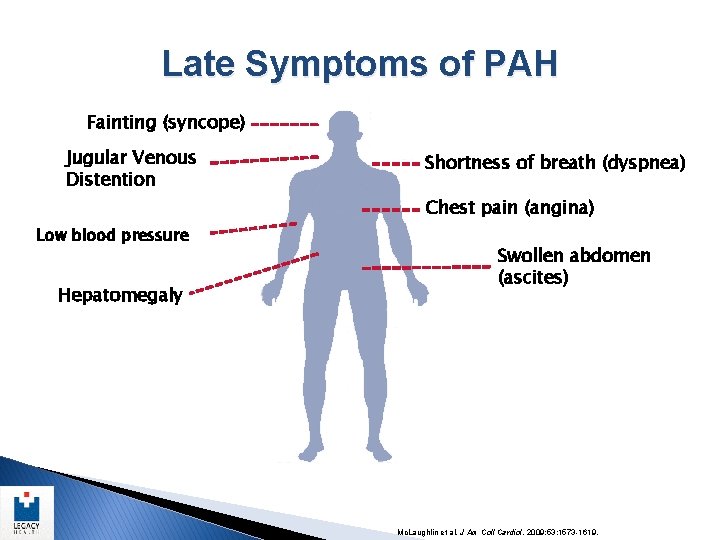
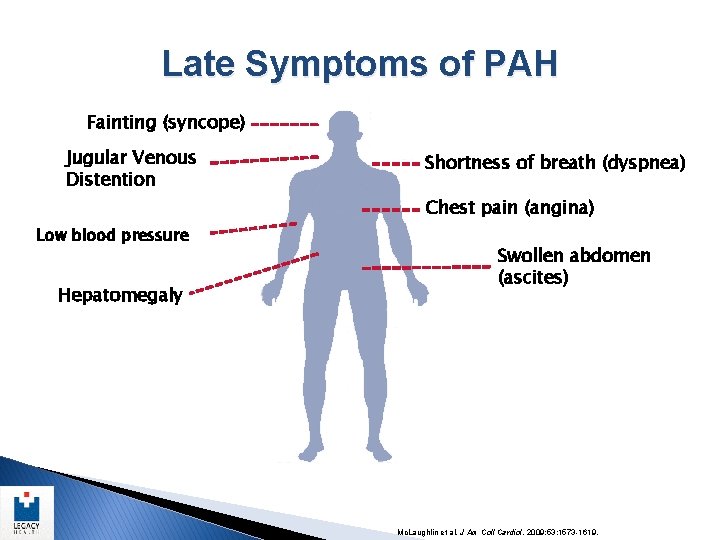
Late Symptoms of PAH Fainting (syncope) Jugular Venous Distention Shortness of breath (dyspnea) Chest pain (angina) Low blood pressure Hepatomegaly Swollen abdomen (ascites) Mc. Laughlin et al. J Am Coll Cardiol. 2009; 53: 1573 -1619.
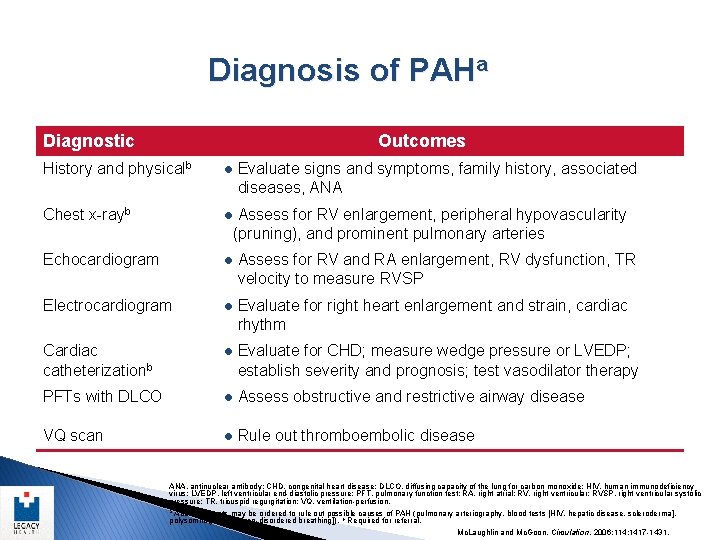
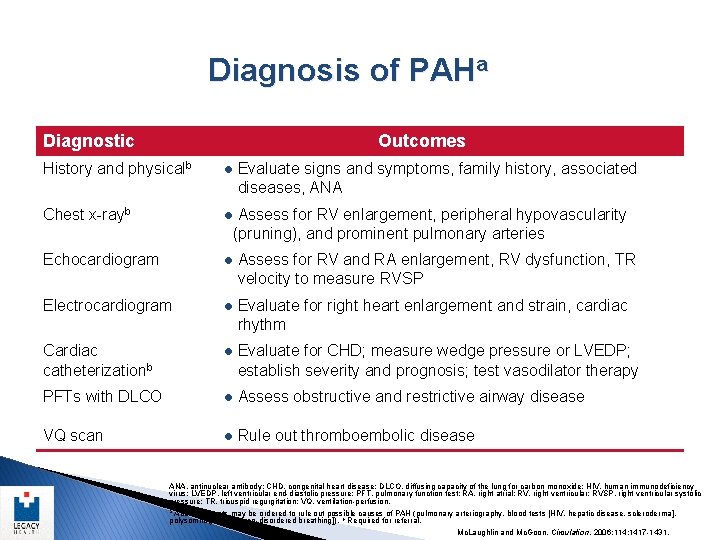
Diagnosis of PAHa Diagnostic Outcomes History and physicalb l Evaluate signs and symptoms, family history, associated diseases, ANA Chest x-rayb l Assess for RV enlargement, peripheral hypovascularity (pruning), and prominent pulmonary arteries Echocardiogram l Assess for RV and RA enlargement, RV dysfunction, TR velocity to measure RVSP Electrocardiogram l Evaluate for right heart enlargement and strain, cardiac rhythm Cardiac catheterizationb l Evaluate for CHD; measure wedge pressure or LVEDP; PFTs with DLCO l Assess obstructive and restrictive airway disease VQ scan l Rule out thromboembolic disease establish severity and prognosis; test vasodilator therapy ANA, antinuclear antibody; CHD, congenital heart disease; DLCO, diffusing capacity of the lung for carbon monoxide; HIV, human immunodeficiency virus; LVEDP, left ventricular end-diastolic pressure; PFT, pulmonary function test; RA, right atrial; RV, right ventricular; RVSP, right ventricular systolic pressure; TR, tricuspid regurgitation; VQ, ventilation-perfusion. a Additional tests may be ordered to rule out possible causes of PAH (pulmonary arteriography, blood tests [HIV, hepatic disease, scleroderma], polysomnography [sleep-disordered breathing]). b Required for referral. Mc. Laughlin and Mc. Goon. Circulation. 2006; 114: 1417 -1431.
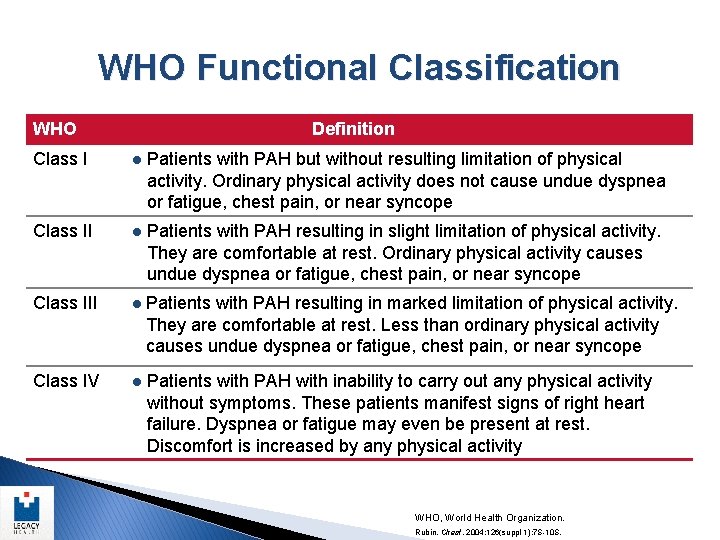
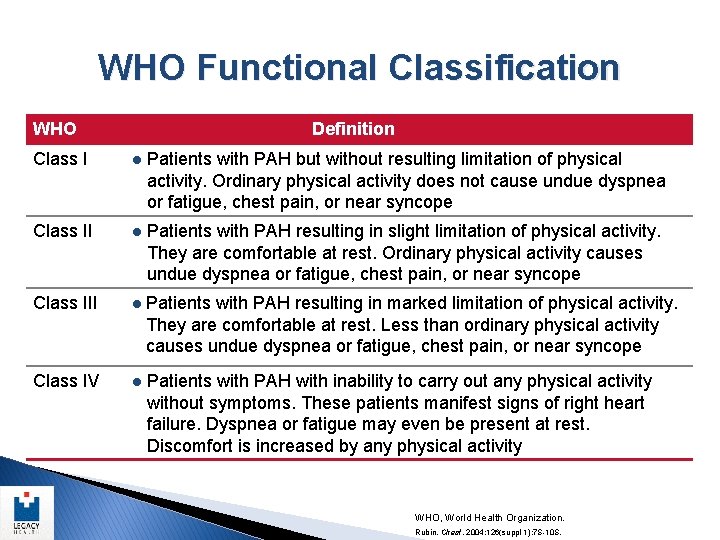
WHO Functional Classification WHO Class I Definition l Patients with PAH but without resulting limitation of physical activity. Ordinary physical activity does not cause undue dyspnea or fatigue, chest pain, or near syncope Class II l Patients with PAH resulting in slight limitation of physical activity. They are comfortable at rest. Ordinary physical activity causes undue dyspnea or fatigue, chest pain, or near syncope Class III l Patients with PAH resulting in marked limitation of physical activity. They are comfortable at rest. Less than ordinary physical activity causes undue dyspnea or fatigue, chest pain, or near syncope Class IV l Patients with PAH with inability to carry out any physical activity without symptoms. These patients manifest signs of right heart failure. Dyspnea or fatigue may even be present at rest. Discomfort is increased by any physical activity WHO, World Health Organization. Rubin. Chest. 2004; 126(suppl 1): 7 S-10 S.
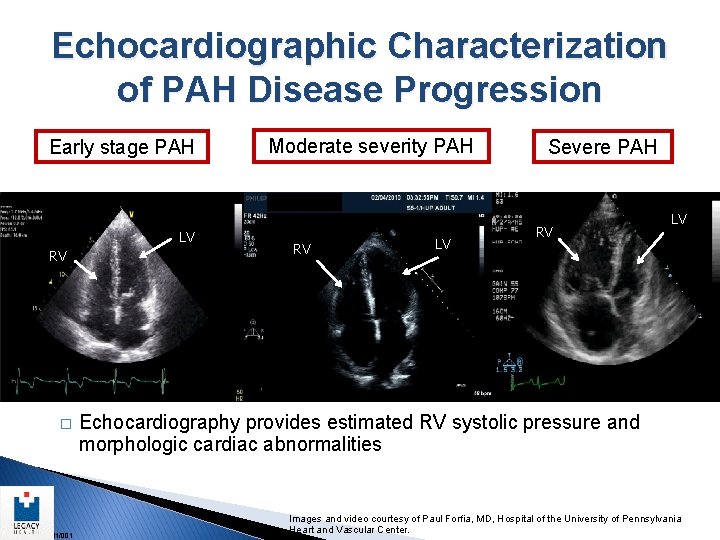
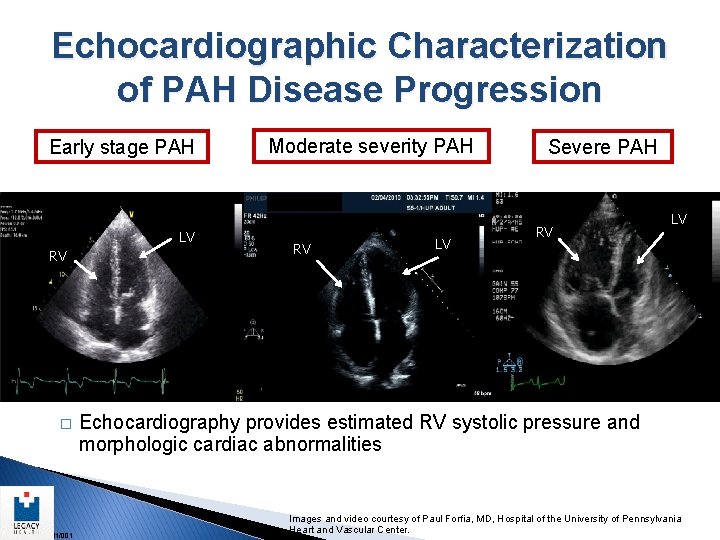
Echocardiographic Characterization of PAH Disease Progression Early stage PAH RV � US/DS/MAR 11/001 LV Moderate severity PAH RV LV Severe PAH RV LV Echocardiography provides estimated RV systolic pressure and morphologic cardiac abnormalities Images and video courtesy of Paul Forfia, MD, Hospital of the University of Pennsylvania Heart and Vascular Center.
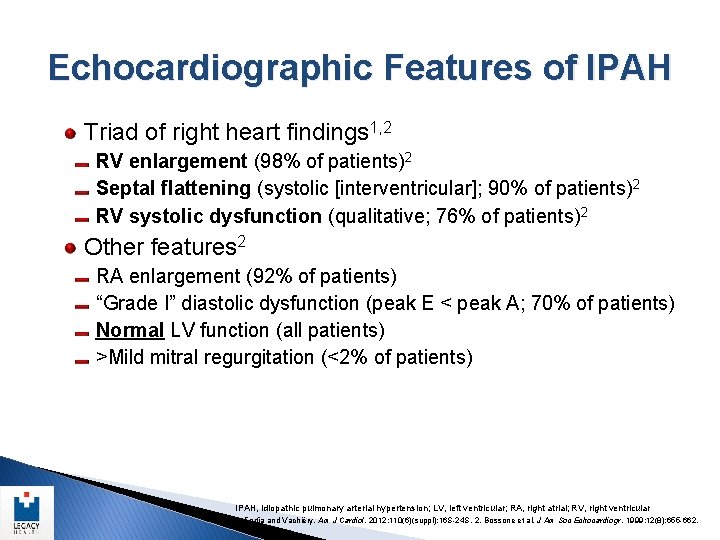
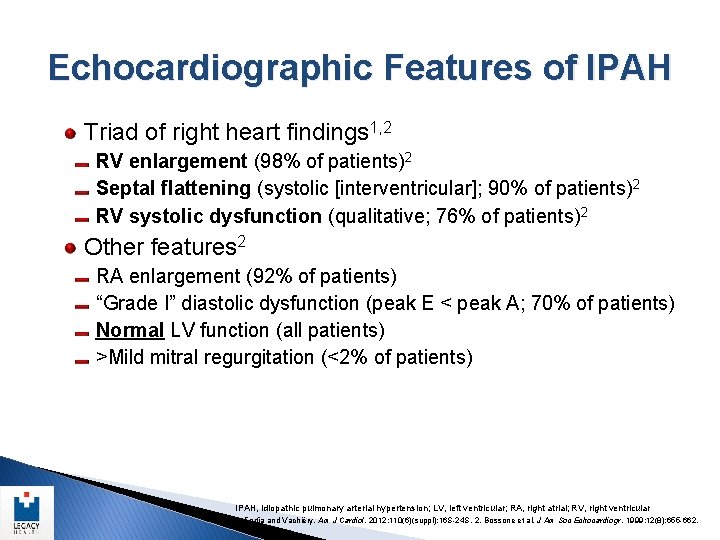
Echocardiographic Features of IPAH Triad of right heart findings 1, 2 RV enlargement (98% of patients)2 Septal flattening (systolic [interventricular]; 90% of patients)2 RV systolic dysfunction (qualitative; 76% of patients)2 Other features 2 RA enlargement (92% of patients) “Grade I” diastolic dysfunction (peak E < peak A; 70% of patients) Normal LV function (all patients) >Mild mitral regurgitation (<2% of patients) IPAH, idiopathic pulmonary arterial hypertension; LV, left ventricular; RA, right atrial; RV, right ventricular. 1. Forfia and Vachiéry. Am J Cardiol. 2012; 110(6)(suppl): 16 S-24 S. 2. Bossone et al. J Am Soc Echocardiogr. 1999; 12(8): 655 -662.
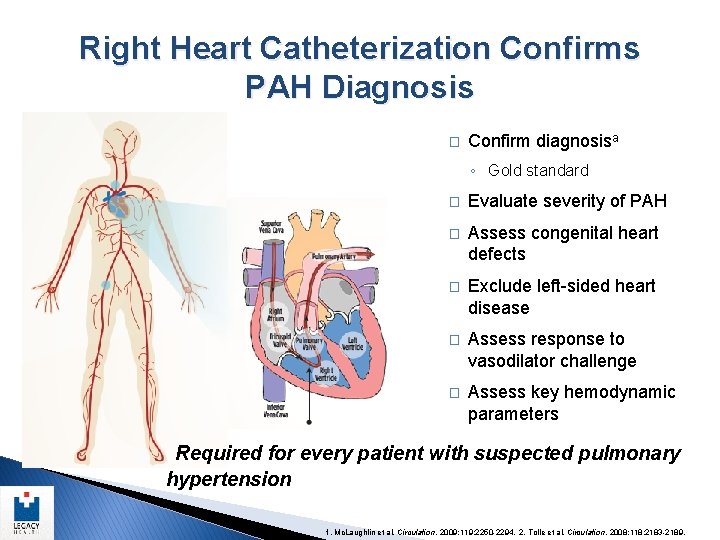
Right Heart Catheterization Confirms PAH Diagnosis � Confirm diagnosisa ◦ Gold standard � Evaluate severity of PAH � Assess congenital heart defects � Exclude left-sided heart disease � Assess response to vasodilator challenge � Assess key hemodynamic parameters Required for every patient with suspected pulmonary hypertension 1. Mc. Laughlin et al. Circulation. 2009; 119: 2250 -2294. 2. Tolle et al. Circulation. 2008; 118: 2183 -2189.
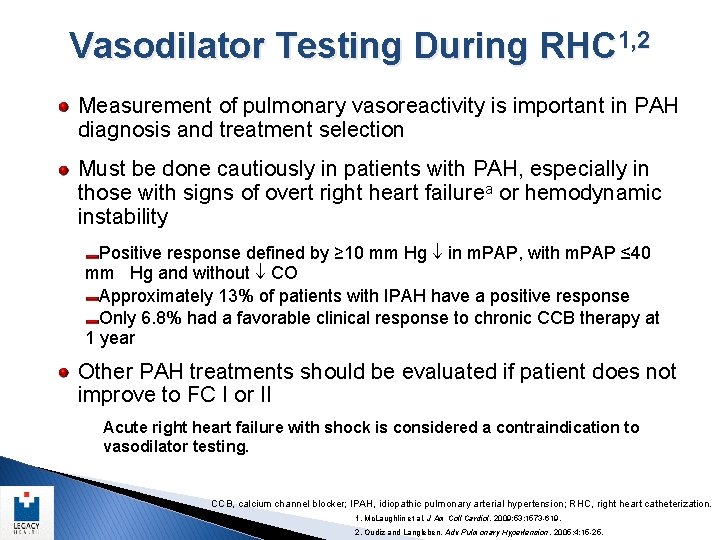
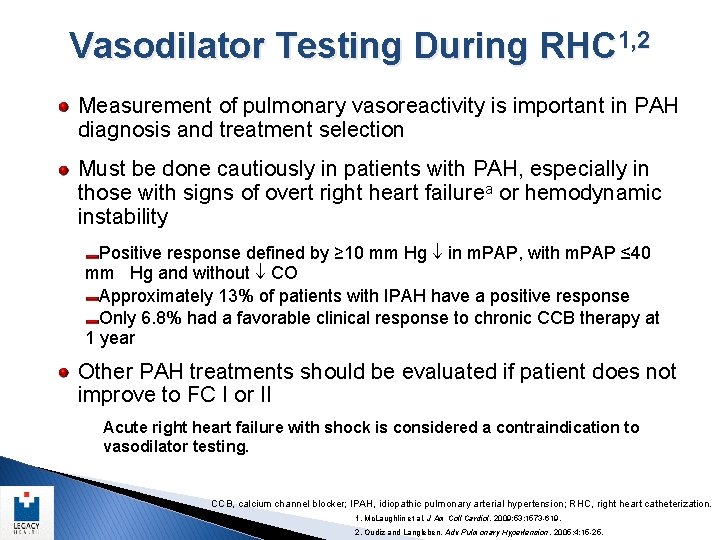
Vasodilator Testing During RHC 1, 2 Measurement of pulmonary vasoreactivity is important in PAH diagnosis and treatment selection Must be done cautiously in patients with PAH, especially in those with signs of overt right heart failurea or hemodynamic instability Positive response defined by ≥ 10 mm Hg in m. PAP, with m. PAP ≤ 40 mm Hg and without CO Approximately 13% of patients with IPAH have a positive response Only 6. 8% had a favorable clinical response to chronic CCB therapy at 1 year Other PAH treatments should be evaluated if patient does not improve to FC I or II Acute right heart failure with shock is considered a contraindication to vasodilator testing. CCB, calcium channel blocker; IPAH, idiopathic pulmonary arterial hypertension; RHC, right heart catheterization. 1. Mc. Laughlin et al. J Am Coll Cardiol. 2009; 53: 1573 -619. 2. Oudiz and Langleben. Adv Pulmonary Hypertension. 2005; 4: 15 -25.
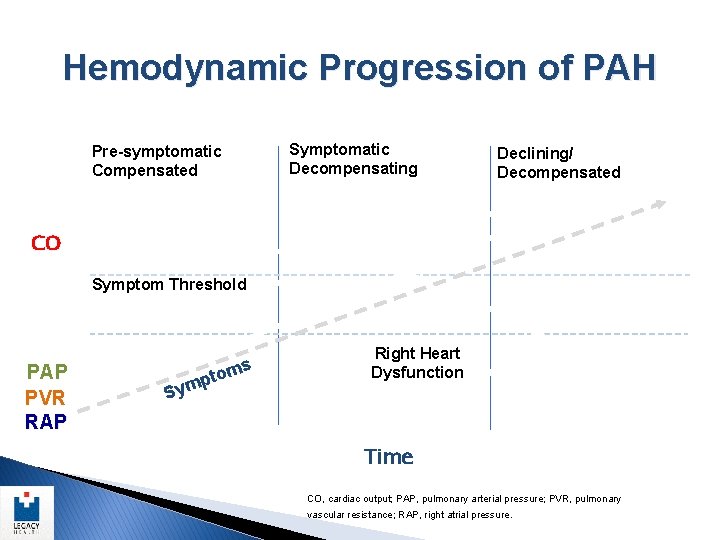
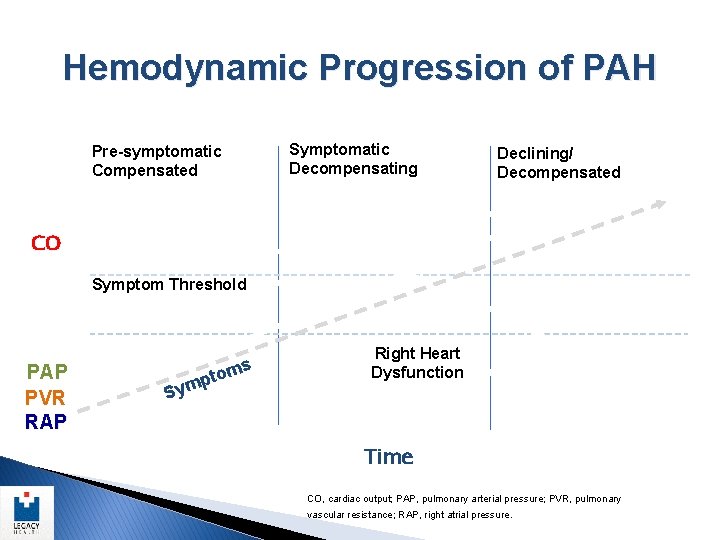
Hemodynamic Progression of PAH Symptomatic/ Decompensating Pre-symptomatic/ Compensated Declining/ Decompensated CO Symptom Threshold PAP PVR RAP ms to ymp Right Heart Dysfunction S Time CO, cardiac output; PAP, pulmonary arterial pressure; PVR, pulmonary vascular resistance; RAP, right atrial pressure.
Treatment of PAH
Management Priniciples � Protect the Right Side of the Heart, Improve Right Ventricular Function ♥ Digoxin ♥ Oxygen ♥ Control Volume status with diuretics and fluid restriction ♥ DRY IS GOOD!!! ♥ Anti-coagulants
Considerations in Treatment Choice ◦ Responsiveness to acute vasodilators ◦ Functional class ◦ Rate of progression ◦ Prior or concomitant drug therapy (therapeutic pathway) ◦ Pulmonary hemodynamics, RV function ◦ Comorbidities (liver, heart disease, immunity) ◦ Psychosocial/financial ◦ Patient/clinician preference
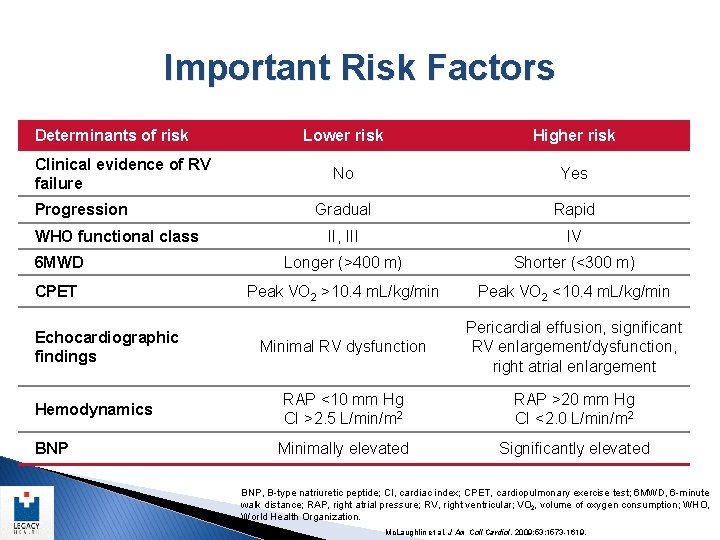
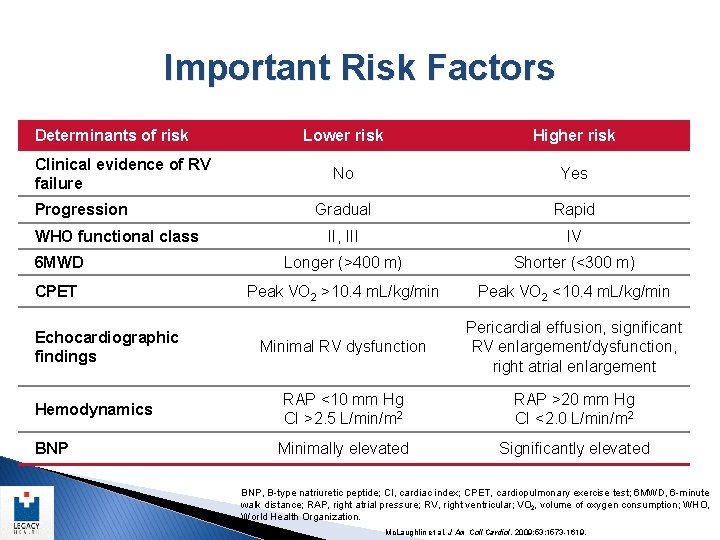
Important Risk Factors Determinants of risk Lower risk Higher risk No Yes Gradual Rapid II, III IV 6 MWD Longer (>400 m) Shorter (<300 m) CPET Peak VO 2 >10. 4 m. L/kg/min Peak VO 2 <10. 4 m. L/kg/min Minimal RV dysfunction Pericardial effusion, significant RV enlargement/dysfunction, right atrial enlargement RAP <10 mm Hg CI >2. 5 L/min/m 2 RAP >20 mm Hg CI <2. 0 L/min/m 2 Minimally elevated Significantly elevated Clinical evidence of RV failure Progression WHO functional class Echocardiographic findings Hemodynamics BNP, B-type natriuretic peptide; CI, cardiac index; CPET, cardiopulmonary exercise test; 6 MWD, 6 -minute walk distance; RAP, right atrial pressure; RV, right ventricular; VO 2, volume of oxygen consumption; WHO, World Health Organization. Mc. Laughlin et al. J Am Coll Cardiol. 2009; 53: 1573 -1619.
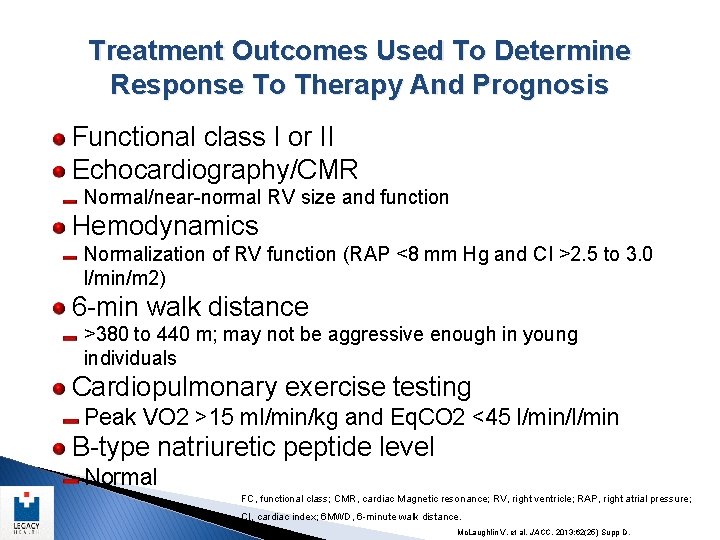
Treatment Outcomes Used To Determine Response To Therapy And Prognosis Functional class I or II Echocardiography/CMR Normal/near-normal RV size and function Hemodynamics Normalization of RV function (RAP <8 mm Hg and CI >2. 5 to 3. 0 l/min/m 2) 6 -min walk distance >380 to 440 m; may not be aggressive enough in young individuals Cardiopulmonary exercise testing Peak VO 2 >15 ml/min/kg and Eq. CO 2 <45 l/min/l/min B-type natriuretic peptide level Normal FC, functional class; CMR, cardiac Magnetic resonance; RV, right ventricle; RAP, right atrial pressure; CI, cardiac index; 6 MWD, 6 -minute walk distance. Mc. Laughlin V, et al. JACC. 2013; 62(25) Supp D.
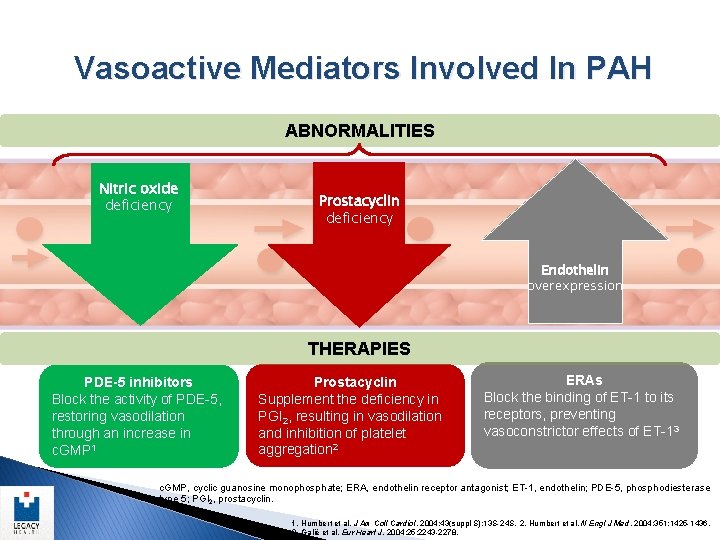
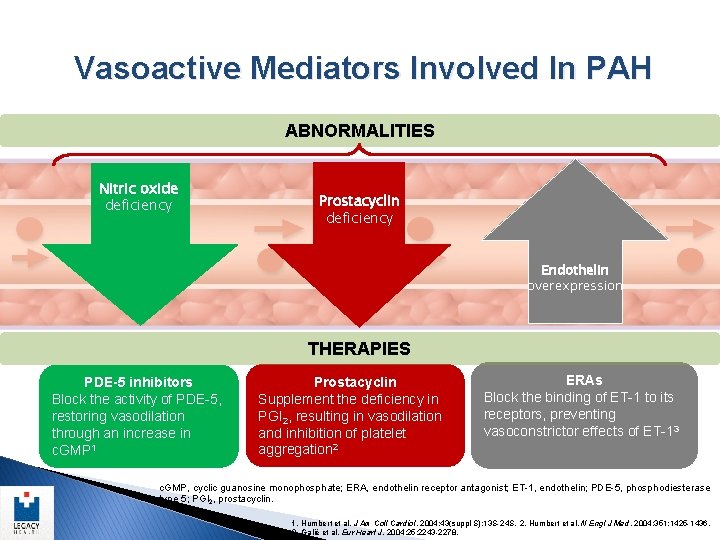
Vasoactive Mediators Involved In PAH ABNORMALITIES Nitric oxide deficiency Prostacyclin deficiency Endothelin overexpression THERAPIES PDE-5 inhibitors Block the activity of PDE-5, restoring vasodilation through an increase in c. GMP 1 Prostacyclin Supplement the deficiency in PGI 2, resulting in vasodilation and inhibition of platelet aggregation 2 ERAs Block the binding of ET-1 to its receptors, preventing vasoconstrictor effects of ET-13 c. GMP, cyclic guanosine monophosphate; ERA, endothelin receptor antagonist; ET-1, endothelin; PDE-5, phosphodiesterase type 5; PGI 2, prostacyclin. 1. Humbert et al. J Am Coll Cardiol. 2004; 43(suppl S): 13 S-24 S. 2. Humbert et al. N Engl J Med. 2004; 351: 1425 -1436. 3. Galiè et al. Eur Heart J. 2004; 25: 2243 -2278.
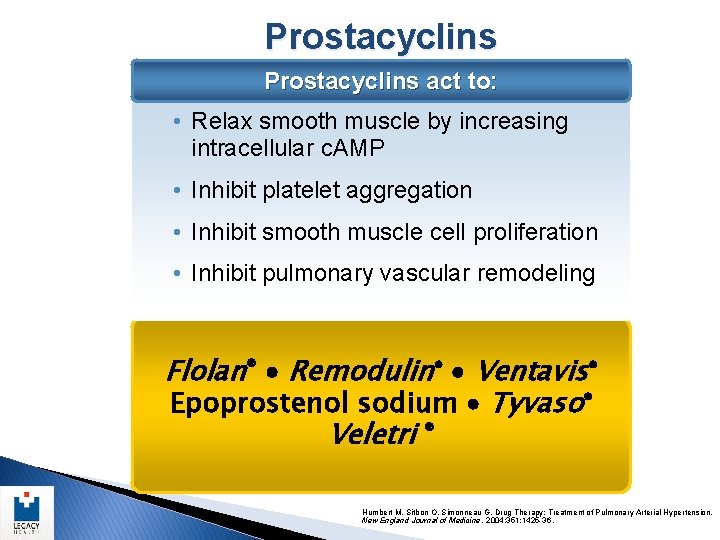
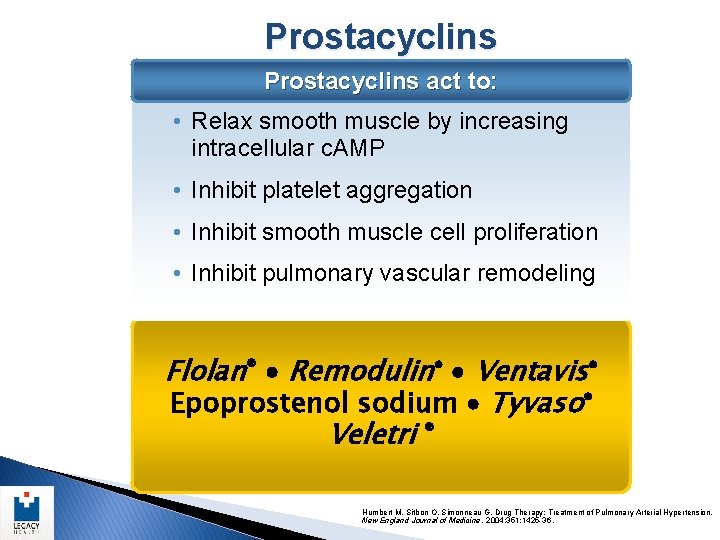
Prostacyclins act to: • Relax smooth muscle by increasing intracellular c. AMP • Inhibit platelet aggregation • Inhibit smooth muscle cell proliferation • Inhibit pulmonary vascular remodeling Flolan® Remodulin® Ventavis® Epoprostenol sodium Tyvaso® Veletri ® Humbert M, Sitbon O, Simonneau G. Drug Therapy: Treatment of Pulmonary Arterial Hypertension. New England Journal of Medicine. 2004; 351: 1425 -36.
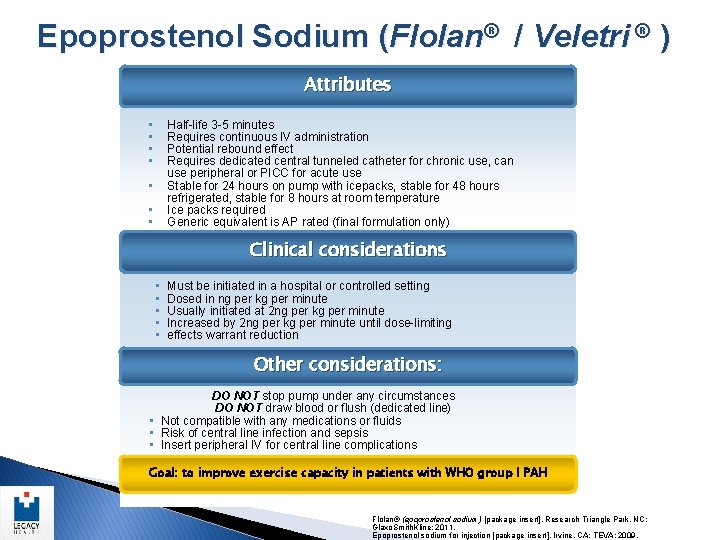
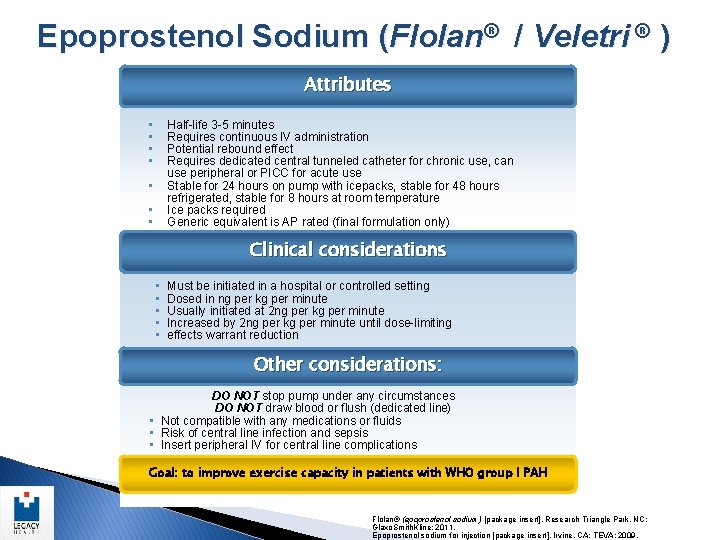
Epoprostenol Sodium (Flolan® / Veletri ® ) Attributes • • Half-life 3 -5 minutes Requires continuous IV administration Potential rebound effect Requires dedicated central tunneled catheter for chronic use, can use peripheral or PICC for acute use Stable for 24 hours on pump with icepacks, stable for 48 hours refrigerated, stable for 8 hours at room temperature Ice packs required Generic equivalent is AP rated (final formulation only) Clinical considerations • Must be initiated in a hospital or controlled setting • Dosed in ng per kg per minute • Usually initiated at 2 ng per kg per minute • Increased by 2 ng per kg per minute until dose-limiting • effects warrant reduction Other considerations: DO NOT stop pump under any circumstances DO NOT draw blood or flush (dedicated line) • Not compatible with any medications or fluids • Risk of central line infection and sepsis • Insert peripheral IV for central line complications Goal: to improve exercise capacity in patients with WHO group I PAH Flolan® (epoprostenol sodium) [package insert]. Research Triangle Park, NC: Glaxo. Smith. Kline; 2011. Epoprostenol sodium for injection [package insert]. Irvine, CA: TEVA; 2009.
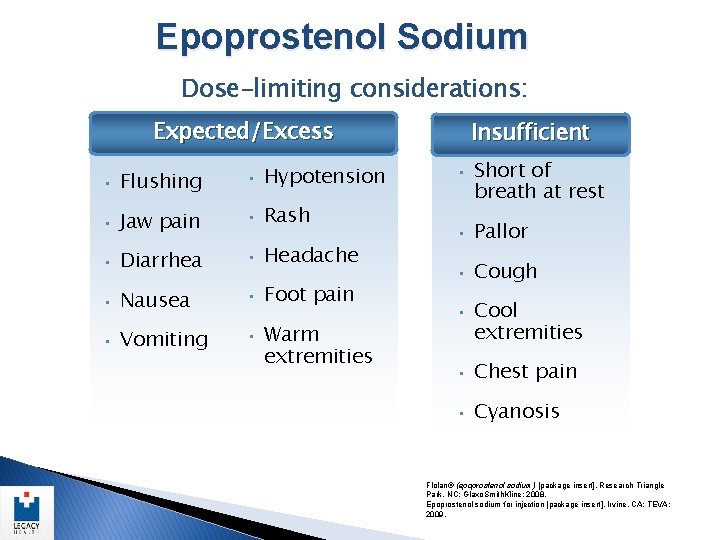
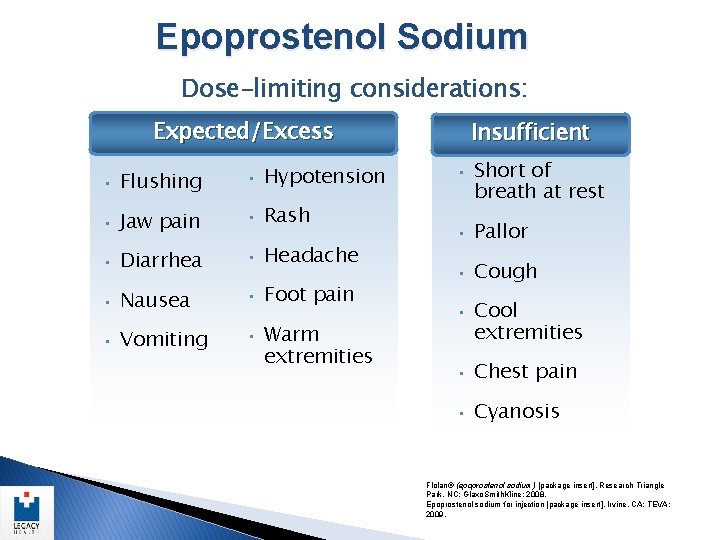
Epoprostenol Sodium Dose-limiting considerations: Expected/Excess • Flushing • Hypotension • Jaw pain • Rash • Diarrhea • Headache • Nausea • Foot pain • Vomiting • Warm extremities Insufficient • Short of breath at rest • Pallor • Cough • Cool extremities • Chest pain • Cyanosis Flolan® (epoprostenol sodium) [package insert]. Research Triangle Park, NC: Glaxo. Smith. Kline; 2008. Epoprostenol sodium for injection [package insert]. Irvine, CA: TEVA; 2009.
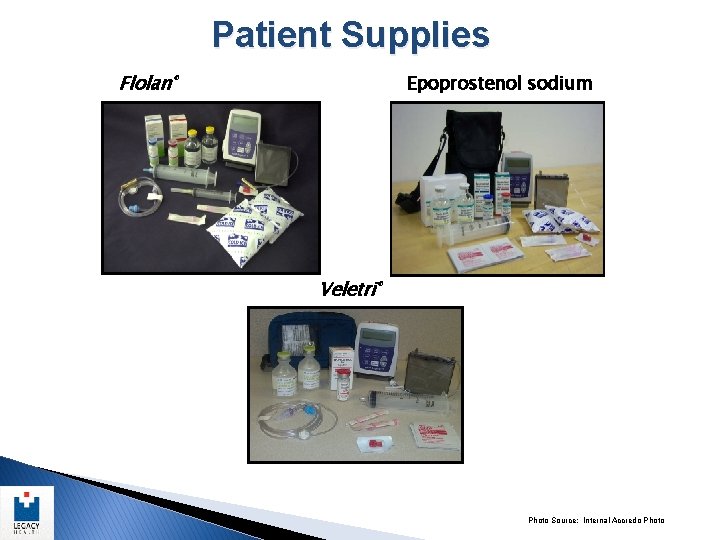
Patient Supplies Flolan® Epoprostenol sodium Veletri® Photo Source: Internal Accredo Photo
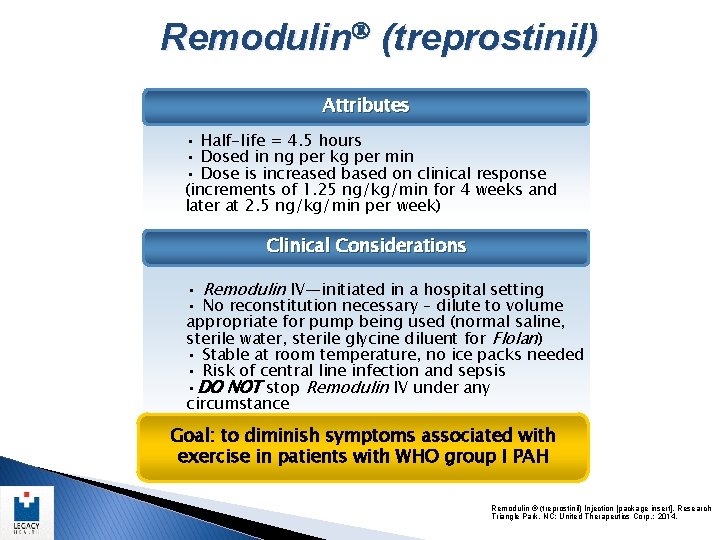
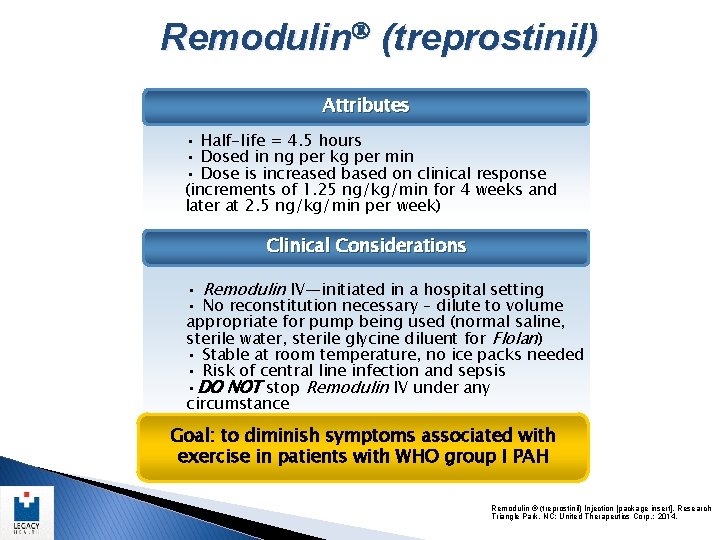
Remodulin (treprostinil) Attributes • Half-life = 4. 5 hours • Dosed in ng per kg per min • Dose is increased based on clinical response (increments of 1. 25 ng/kg/min for 4 weeks and later at 2. 5 ng/kg/min per week) Clinical Considerations • Remodulin IV—initiated in a hospital setting • No reconstitution necessary – dilute to volume appropriate for pump being used (normal saline, sterile water, sterile glycine diluent for Flolan) • Stable at room temperature, no ice packs needed • Risk of central line infection and sepsis • DO NOT stop Remodulin IV under any circumstance Goal: to diminish symptoms associated with exercise in patients with WHO group I PAH Remodulin ® (treprostinil) Injection [package insert]. Research Triangle Park, NC: United Therapeutics Corp. ; 2014.
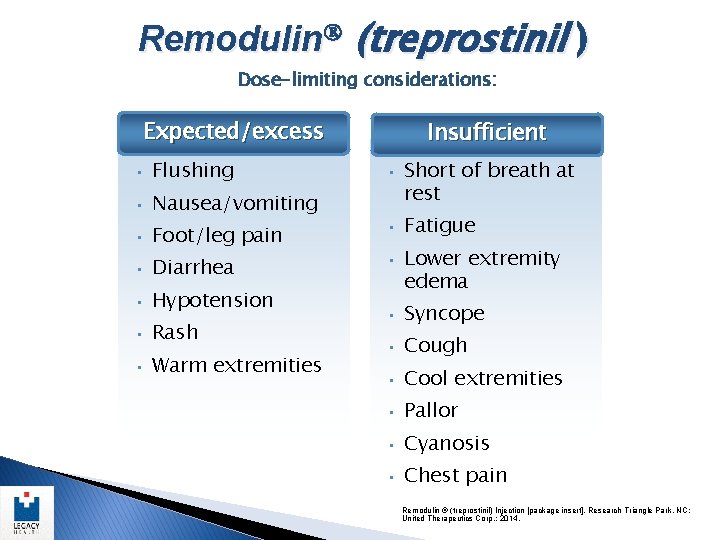
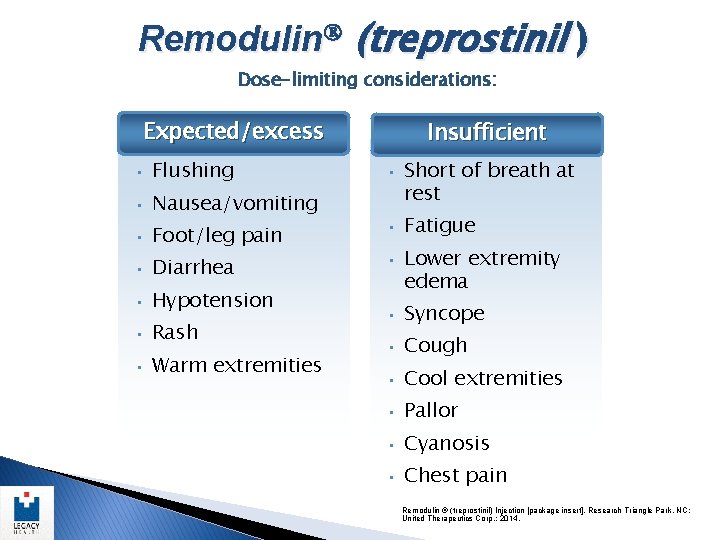
Remodulin (treprostinil ) Dose-limiting considerations: Expected/excess • Flushing • Nausea/vomiting • Foot/leg pain • Diarrhea • Hypotension • Rash • Warm extremities Insufficient • Short of breath at rest • Fatigue • Lower extremity edema • Syncope • Cough • Cool extremities • Pallor • Cyanosis • Chest pain Remodulin ® (treprostinil) Injection [package insert]. Research Triangle Park, NC: United Therapeutics Corp. ; 2014.
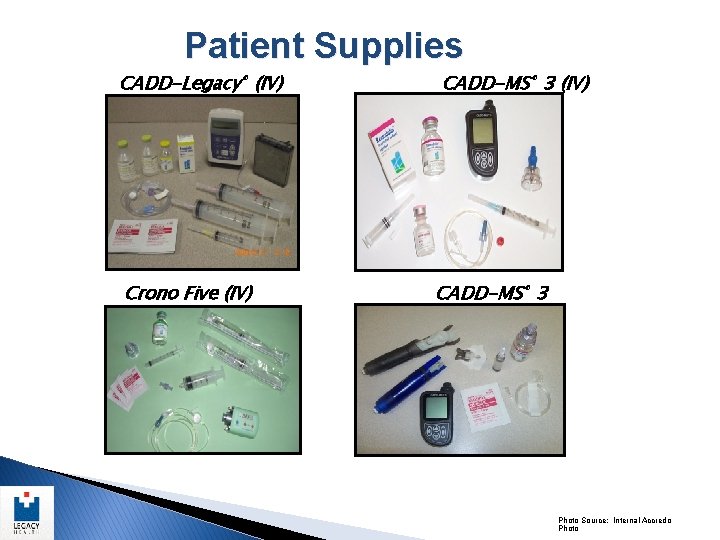
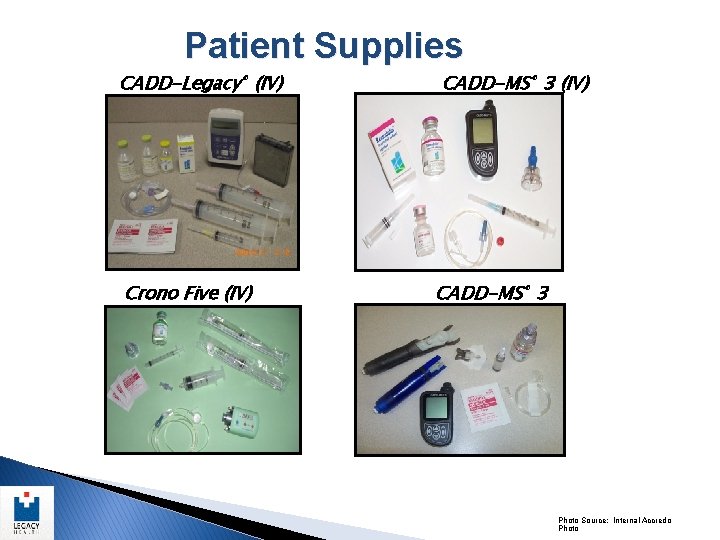
Patient Supplies CADD-Legacy® (IV) Crono Five (IV) (subcutaneous) CADD-MS® 3 (IV) CADD-MS® 3 Photo Source: Internal Accredo Photo
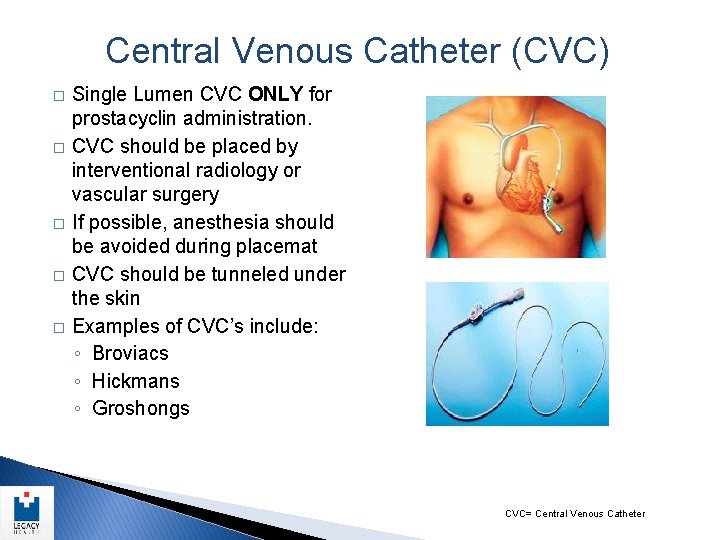
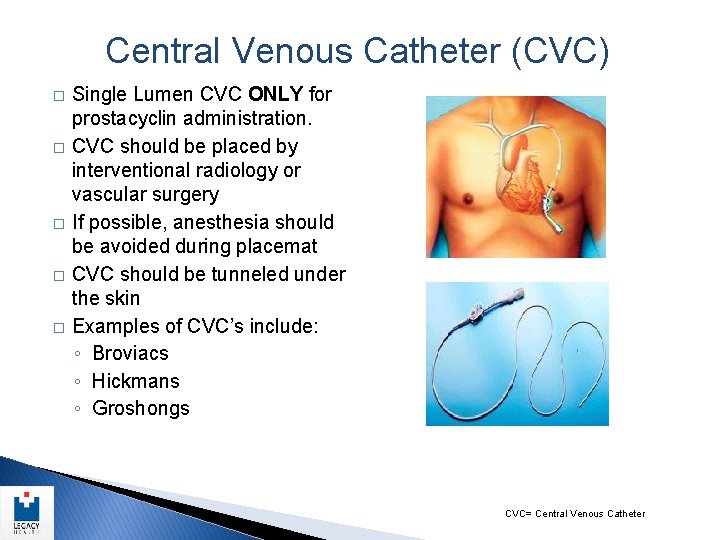
Central Venous Catheter (CVC) � � � Single Lumen CVC ONLY for prostacyclin administration. CVC should be placed by interventional radiology or vascular surgery If possible, anesthesia should be avoided during placemat CVC should be tunneled under the skin Examples of CVC’s include: ◦ Broviacs ◦ Hickmans ◦ Groshongs CVC= Central Venous Catheter
Emergency Considerations
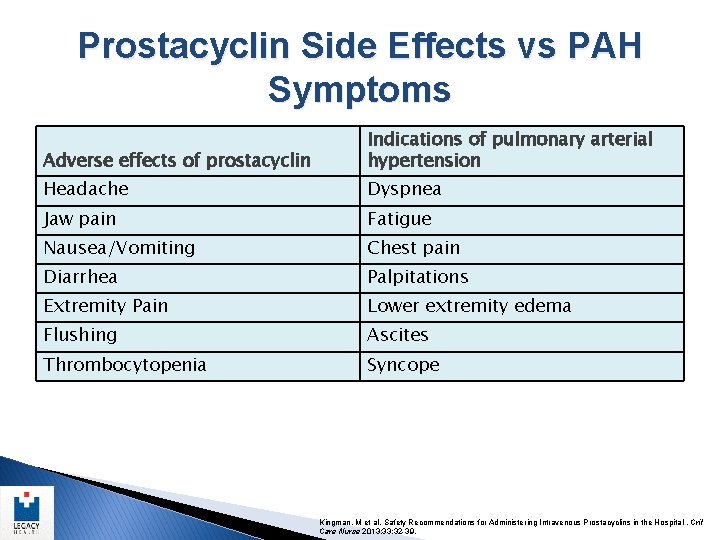
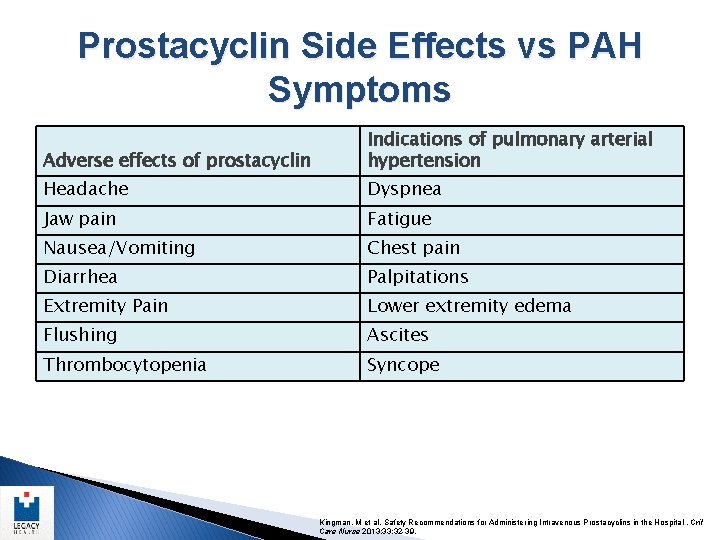
Prostacyclin Side Effects vs PAH Symptoms Adverse effects of prostacyclin Indications of pulmonary arterial hypertension Headache Dyspnea Jaw pain Fatigue Nausea/Vomiting Chest pain Diarrhea Palpitations Extremity Pain Lower extremity edema Flushing Ascites Thrombocytopenia Syncope Kingman, M et al. Safety Recommendations for Administering Intravenous Prostacyclins in the Hospital. Crit Care Nurse 2013; 33: 32 -39.
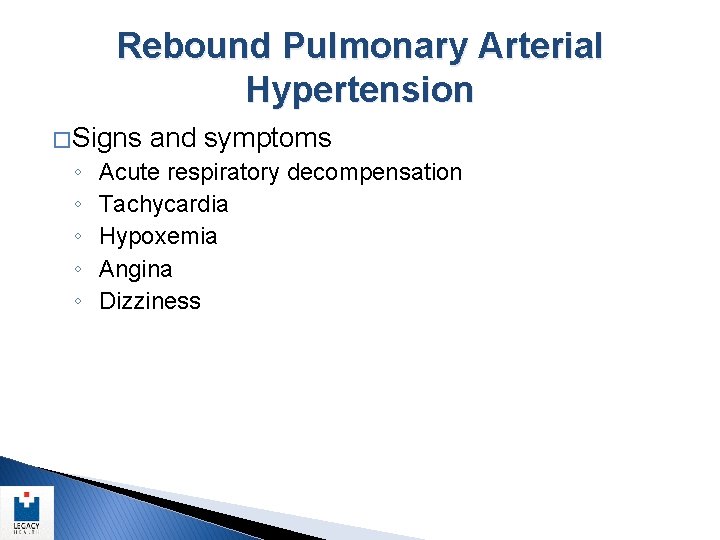
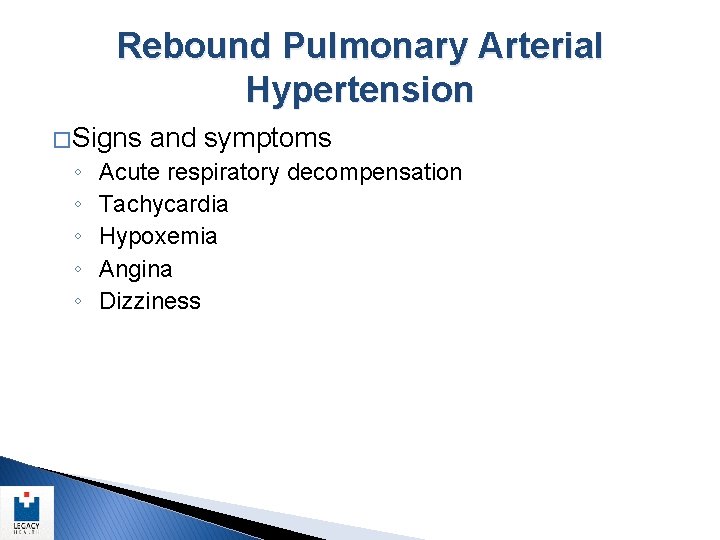
Rebound Pulmonary Arterial Hypertension � Signs and symptoms ◦ ◦ ◦ Acute respiratory decompensation Tachycardia Hypoxemia Angina Dizziness
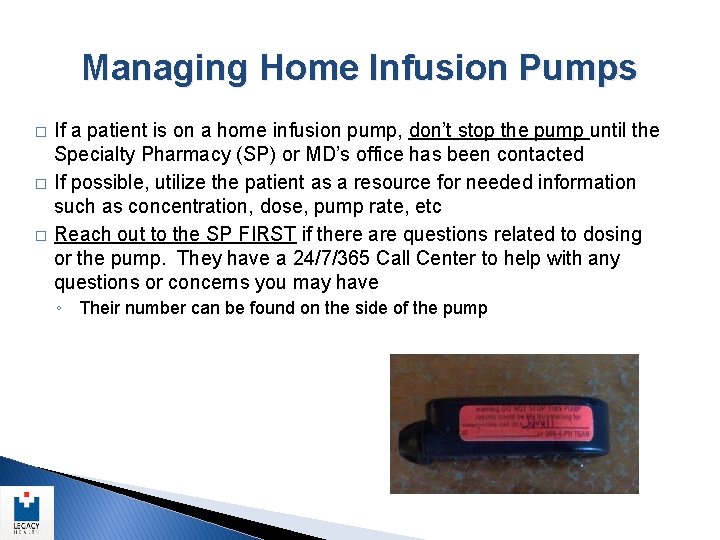
Managing Home Infusion Pumps � � � If a patient is on a home infusion pump, don’t stop the pump until the Specialty Pharmacy (SP) or MD’s office has been contacted If possible, utilize the patient as a resource for needed information such as concentration, dose, pump rate, etc Reach out to the SP FIRST if there are questions related to dosing or the pump. They have a 24/7/365 Call Center to help with any questions or concerns you may have ◦ Their number can be found on the side of the pump

Specialty Pharmacy Service Offerings Specialty pharmacies can make initiating Remodulin therapy easier for you by providing continuous patient support with ongoing services and resources for long-term success • All third-party reimbursement management – New patients – Patients transitioning from other PAH therapies • Patient assessment and evaluation • Teaching – Pre-teaching and ongoing support – In-home, hospital, or clinic • Discharge planning support • 24/7 patient hotline access
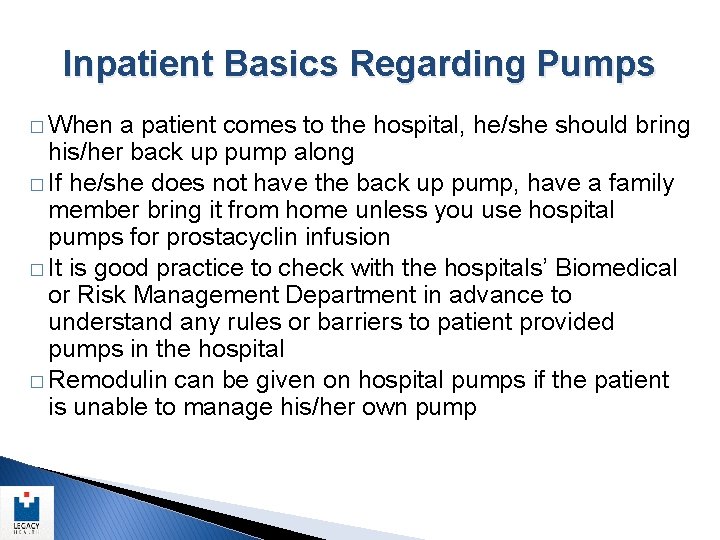
Inpatient Basics Regarding Pumps � When a patient comes to the hospital, he/she should bring his/her back up pump along � If he/she does not have the back up pump, have a family member bring it from home unless you use hospital pumps for prostacyclin infusion � It is good practice to check with the hospitals’ Biomedical or Risk Management Department in advance to understand any rules or barriers to patient provided pumps in the hospital � Remodulin can be given on hospital pumps if the patient is unable to manage his/her own pump
Transitioning to a Hospital Pump � When switching to a hospital pump from a home infusion pump, consider what actions should be taken if the new concentration for Remodulin is different than the patient’s home concentration ◦ Withdraw the drug from the central line before starting the newly mixed drug (different concentration/different pump rate) ◦ Consider re-priming the line with the new concentration of drug (avoid disruption in therapy)
IV Administration – Line Issues � � � If patient has a central line NEVER flush the line – flushing could result in prostacyclin bolus Do NOT interrupt the infusion A single lumen catheter (ie. Hickman) is the preferred route for prostacyclin delivery ◦ If you must give Remodulin in a double or triple lumen catheter, use the most distal port � If the patient’s central line is occluded, it is essential to place peripheral access and utilize the peripheral line until new central access can be established ◦ Due to the risks associated with sudden infusion disruption, the patient should have two peripheral lines placed to ensure that there is back up access if the initial peripheral access is lost
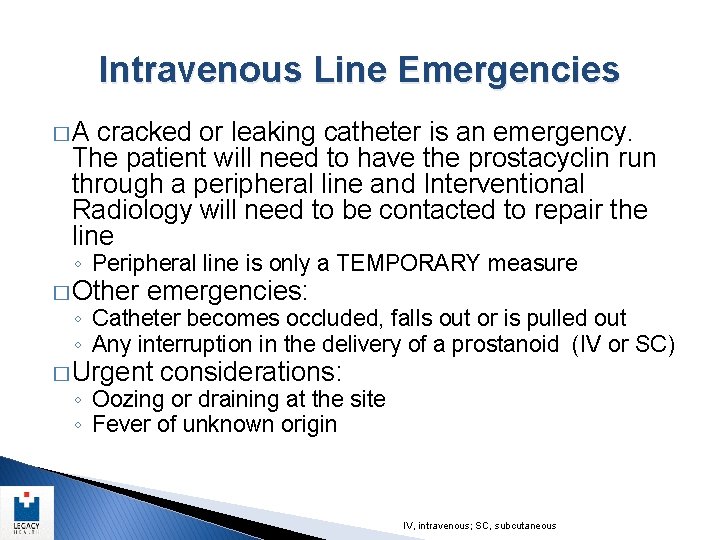
Intravenous Line Emergencies � A cracked or leaking catheter is an emergency. The patient will need to have the prostacyclin run through a peripheral line and Interventional Radiology will need to be contacted to repair the line ◦ Peripheral line is only a TEMPORARY measure � Other emergencies: ◦ Catheter becomes occluded, falls out or is pulled out ◦ Any interruption in the delivery of a prostanoid (IV or SC) � Urgent considerations: ◦ Oozing or draining at the site ◦ Fever of unknown origin IV, intravenous; SC, subcutaneous
Questions