NURSING CARE OF THE PATIENT RECEIVING AN EPIDURAL
- Slides: 31
NURSING CARE OF THE PATIENT RECEIVING AN EPIDURAL OR INTRATHECAL ANALGESIA Amanda Tracy, BSN, RN-BC
LEARNING OBJECTIVES Upon completion of the course the learner should be able to: identify the anatomy and physiology related to the placement of the epidural or intrathecal analgesia with a focus on the nursing care during this time. Describe the assessments and nursing care of the patient receiving neuraxial analgesia Manage the side effects that may occur when caring for a patient receiving neuraxial analgesia Anticipate and recognize potential complications and emergency situations as well as intervene with appropriate nursing care
TYPES OF EPIDURAL/INTRATHECAL The neuraxial analgesic infusion may be one of four possible programs: 1. Continuous infusion into the epidural space, 2. Continuous infusion into the intrathecal space 3. Patient controlled epidural anesthesia (PCEA) – continuous epidural infusion with the option of having a patient controlled bolus dose 4. Patient controlled intrathecal analgesia (PCIA) – continuous intrathecal analgesia with patient administered bolus dose
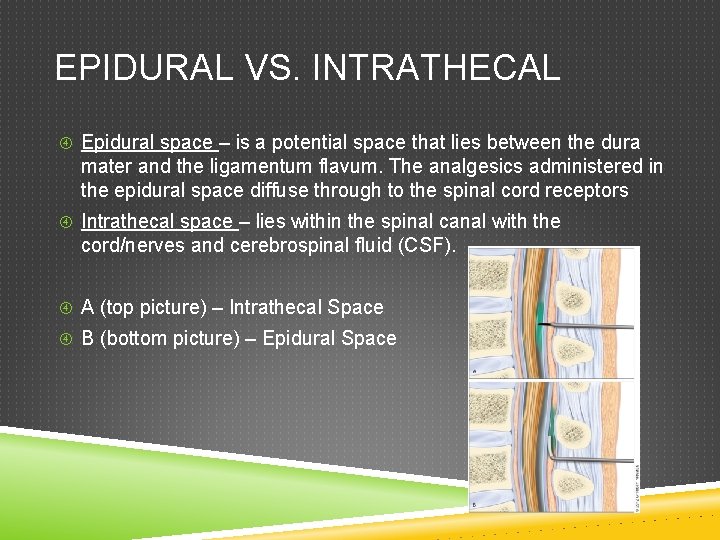
NEURAXIAL ANESTHESIA Neuraxial anesthesia is a general term to describe epidural and intrathecal analgesia Epidural anesthesia will have a slower onset and require a higher dose of medication because it is placed in the outermost layer of the spinal canal Intrathecal anesthesia will have a faster onset and require a smaller dose of medication because it is administered cerebrospinal fluid (CSF) surrounding the spinal cord
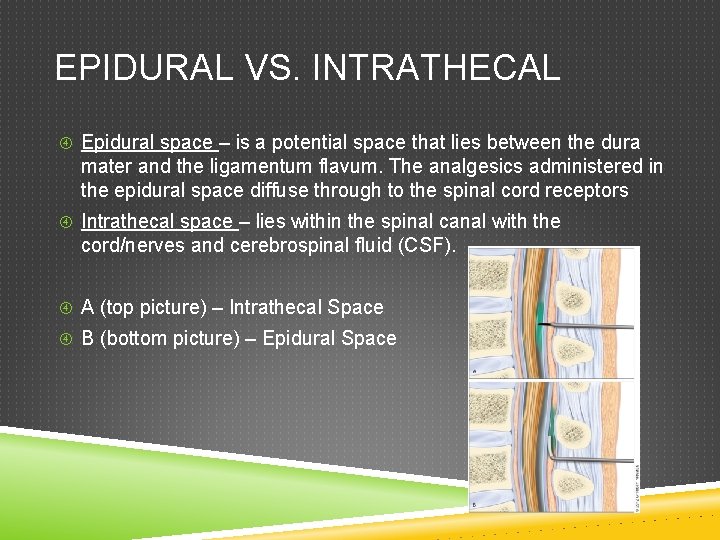
EPIDURAL VS. INTRATHECAL Epidural space – is a potential space that lies between the dura mater and the ligamentum flavum. The analgesics administered in the epidural space diffuse through to the spinal cord receptors Intrathecal space – lies within the spinal canal with the cord/nerves and cerebrospinal fluid (CSF). A (top picture) – Intrathecal Space B (bottom picture) – Epidural Space
KNOWLEDGE CHECK Which of the following are true regarding the mode of action for epidural and intrathecal analgesia? Check all that apply 1. In the epidural space the analgesics administered go directly into the CSF with faster onset 2. In the intrathecal space, the analgesics administered go directly into the CSF with faster onset 3. The epidural space lies within the spinal canal with the spinal cord, nerves, and CSF 4. The intrathecal space lies within the spinal canal with the spinal cord, nerves, and CSF
ANSWER Which of the following are true regarding the mode of action for epidural and intrathecal analgesia? Check all that apply 1. In the epidural space the analgesics administered go directly into the CSF with faster onset 2. In the intrathecal space, the analgesics administered go directly into the CSF with faster onset 3. The epidural space lies within the spinal canal with the spinal cord, nerves, and CSF 4. The intrathecal space lies within the spinal canal with the spinal cord, nerves, and CSF
MEDICATIONS – NURSING CONSIDERATIONS No oral narcotics, sedatives, or antihistamines can be given for 24 hours following an intrathecal injection or during continuous injection unless prescribed by the anesthesia provider Notify the anesthesia provider if the medications have not worn off in the appropriate amount of time
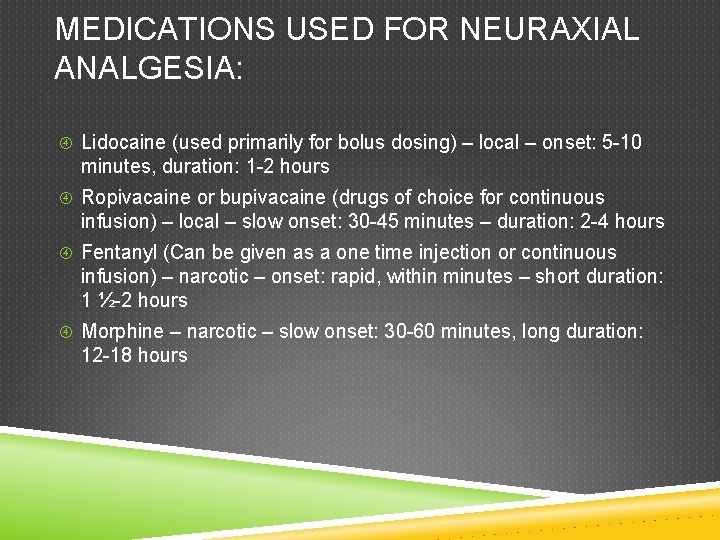
MEDICATIONS USED FOR NEURAXIAL ANALGESIA: Lidocaine (used primarily for bolus dosing) – local – onset: 5 -10 minutes, duration: 1 -2 hours Ropivacaine or bupivacaine (drugs of choice for continuous infusion) – local – slow onset: 30 -45 minutes – duration: 2 -4 hours Fentanyl (Can be given as a one time injection or continuous infusion) – narcotic – onset: rapid, within minutes – short duration: 1 ½-2 hours Morphine – narcotic – slow onset: 30 -60 minutes, long duration: 12 -18 hours
KNOWLEDGE CHECK: WHICH OF THE FOLLOWING STATEMENTS IS FALSE: ? 1. Bupivacaine is a local anesthetic with an onset of 30 minutes and duration of 1 -2 hours 2. Morphine has an onset of 30 -60 minutes and a duration of 1218 hours 3. Fentanyl has an onset of within minutes and a duration of 1 ½-2 hours 4. Lidocaine has a rapid onset, short duration, and used primarily for bolus dosing
ANSWER 1. Bupivacaine is a local anesthetic with an onset of 30 minutes and duration of 1 -2 hours 2. Morphine has an onset of 30 -60 minutes and a duration of 1218 hours 3. Fentanyl has an onset of within minutes and a duration of 1 ½-2 hours 4. Lidocaine has a rapid onset, short duration, and used primarily for bolus dosing
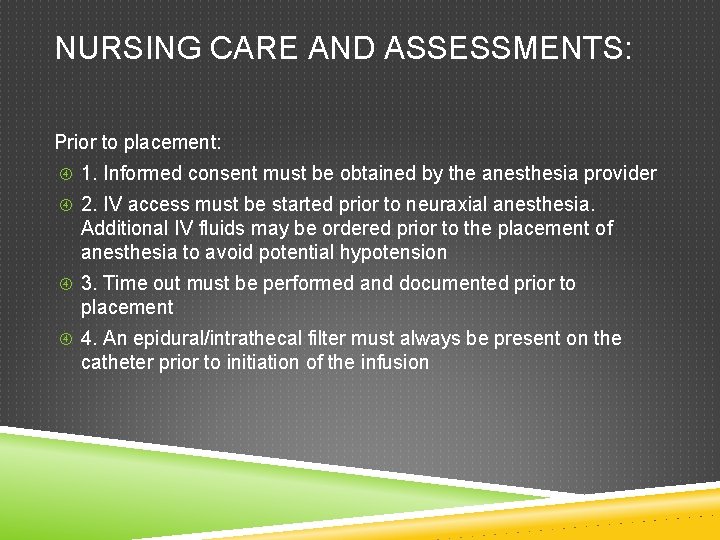
NURSING CARE AND ASSESSMENTS: Prior to placement: 1. Informed consent must be obtained by the anesthesia provider 2. IV access must be started prior to neuraxial anesthesia. Additional IV fluids may be ordered prior to the placement of anesthesia to avoid potential hypotension 3. Time out must be performed and documented prior to placement 4. An epidural/intrathecal filter must always be present on the catheter prior to initiation of the infusion
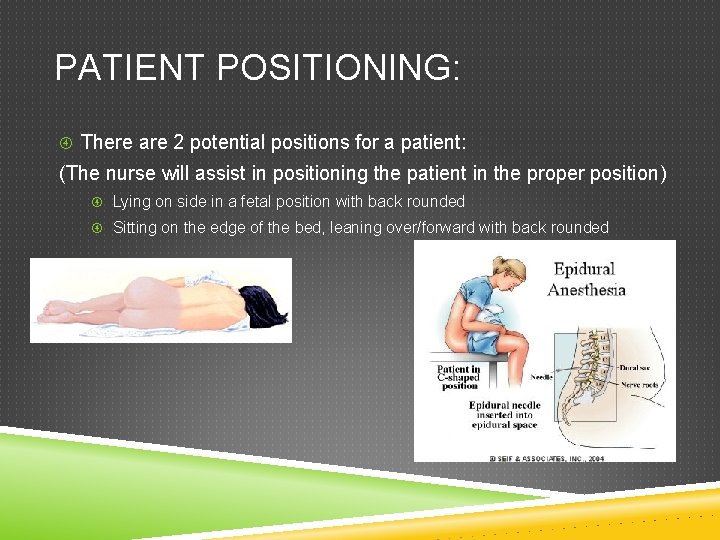
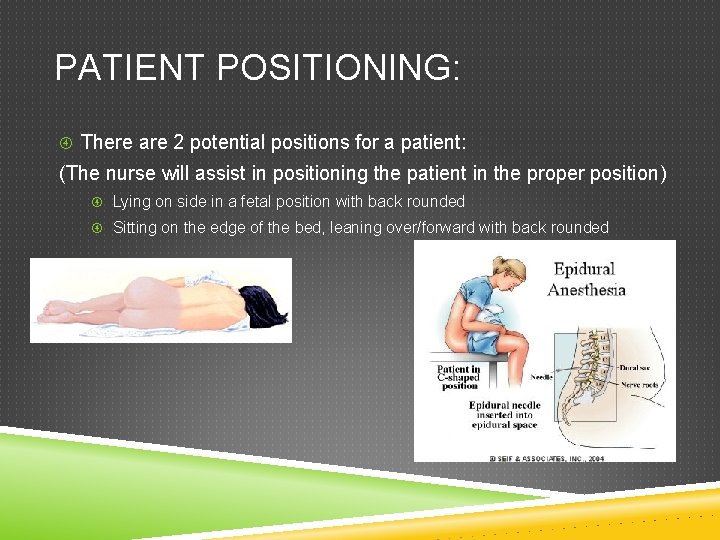
PATIENT POSITIONING: There are 2 potential positions for a patient: (The nurse will assist in positioning the patient in the proper position) Lying on side in a fetal position with back rounded Sitting on the edge of the bed, leaning over/forward with back rounded
DURING PLACEMENT: The patient may jump when the epidural catheter passes between the nerves and is threaded into place. This is a normal response – provide reassurance. Monitor and document vital signs: blood pressure/pulse/RR/oxygen saturation/pain score/ sedation level OB patients continuous electronic fetal monitoring is obtained
POST PLACEMENT PROCEDURES: Monitor and document pain assessment Check vital signs and oxygen saturation as ordered Make sure the epidural catheter is clearly labeled as such Inspect insertion site and catheter Check dressing at insertion site to ensure it is dry and intact
ADDITIONAL CONSIDERATIONS Perform motor and sensory assessments as ordered by provider – hourly Bromage Score When turning the patient use caution to avoid dislodging of the epidural catheter or disconnecting the tubing at any of the connections If catheter becomes disconnected or dislodged, cover exposed tips with a sterile dressing, turn off infusion, and notify provider immediately
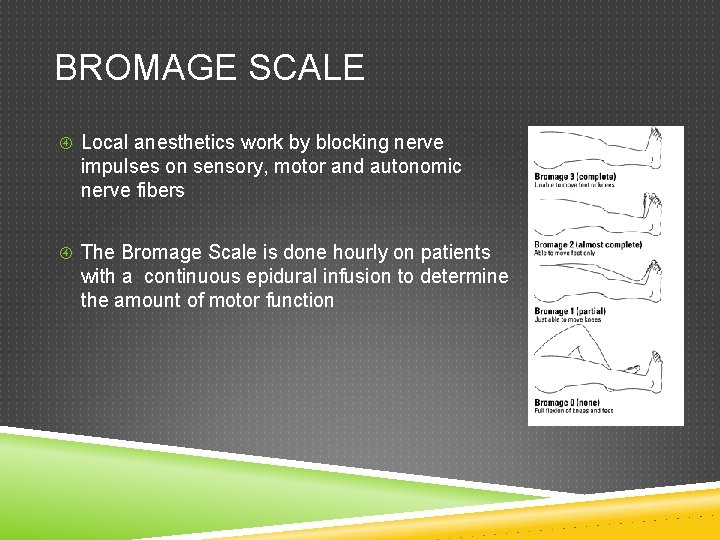
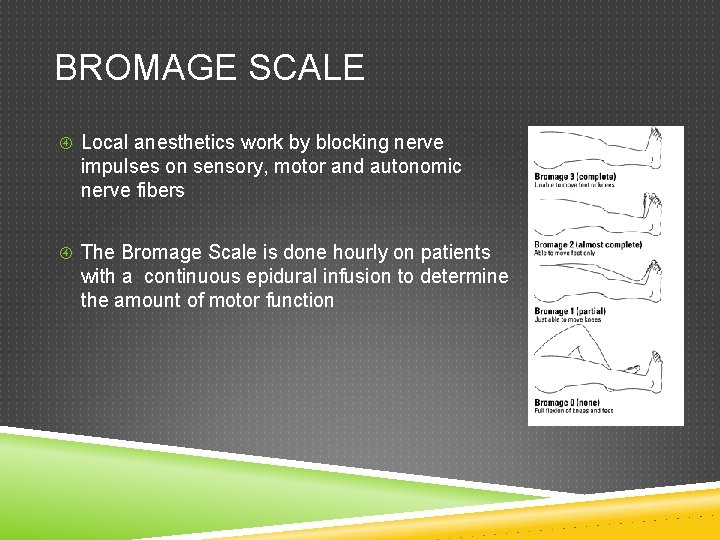
BROMAGE SCALE Local anesthetics work by blocking nerve impulses on sensory, motor and autonomic nerve fibers The Bromage Scale is done hourly on patients with a continuous epidural infusion to determine the amount of motor function
REMOVAL OF THE EPIDURAL CATHETER Only RNs on the FBC can remove an epidural catheter, and only following orientation to the procedure Notify the anesthesia provider immediately if there is any resistance or difficulty in removing the catheter and/or the blue tip is not intact on removal Removal for other patients is done by the anesthesia provider
NDBON PRACTICE STATEMENT North Dakota Board of Nursing Practice Statement – Role of the RN in Management of Analgesia by Catheter Techniques for Obstetrical Patients https: //www. ndbon. org/Regulations. Practice/Practice. Statements/R NMgmt-Analgeciaby. Catheter_OB. asp
KNOWLEDGE CHECK Mrs. Anderson is a 66 year old who is post-op day #2 after a major abdominal exploration. She has an epidural for pain management. While doing bedside report you notice a wet spot on the bed underneath her back. You find the epidural tubing is disconnected from the catheter. What would be the best course of action? Reconnect the catheter and tubing and notify the provider Clean the exposed tips with alcohol wipes and reconnect the ends Apply a sterile cover the exposed tips and notify the anesthesia provider Remove the epidural catheter
ANSWER Mrs. Anderson is a 66 year old who is post-op day #2 after a major abdominal exploration. She has an epidural for pain management. While doing bedside report you notice a wet spot on the bed underneath her back. You find the epidural tubing is disconnected from the catheter. What would be the best course of action? Reconnect the catheter and tubing and notify the provider Clean the exposed tips with alcohol wipes and reconnect the ends Apply a sterile cover the exposed tips and notify the anesthesia provider Remove the epidural catheter
MANAGEMENT OF SIDE EFFECTS: Monitoring for side effects that may occur allows for prompt treatment (per physician’s orders) Urinary retention – consider a bladder scan, use a straight catheter, or place an indwelling catheter as ordered Decreased lower extremity motor function – activity ordered is typically bed rest Prior to any ambulation, an assessment of motor function should be performed. Two staff members should assist in ambulating patient for the first time up and prn after that. Instruct the patient to call for help before getting out of bed Nausea/vomiting – standing order set or per anesthesia provider orders for N/V. Pruritus (itching) – use standing order set for itching
COMPLICATIONS Hypotension Hypothermia Respiratory depression High or total spinal blockade Post. Dural Puncture Headache (PDPH)
HYPOTENSION May occur because of vasodilation of blood vessels, resulting in pooling of blood in lower extremities. Adequate IV fluid prior to placement helps in reducing incidence of hypotension. Notify provider for consideration of IV fluids or vasopressors, if indicated. The use of Trendelenburg is contraindicated as it may lead to a higher level of block than desired.
HYPOTHERMIA Occurs due to the peripheral dilation related to the affects of the anesthesia. Provide warm blankets
RESPIRATORY DEPRESSION Monitor for trending down of respiratory effort Morbidly obese patients or patients with sleep apnea at increased risk Notify anesthesia provider Naloxone (IV) is ordered for respiratory rate of 6 breaths/min or less. If used, notify provider. Be prepared to call for assistance and give breaths per Ambu bag if patient worsens
HIGH OR TOTAL SPINAL BLOCKADE High neuraxial blocks can cause dyspnea, hypotension, agitation, and nausea. Total blocks (rare) can cause difficulty speaking, apnea, profound hypotension and possible unconsciousness Emergency steps: call for assistance and notify anesthesia provider immediately Administer supplemental oxygen, if dyspnea is mild or provide ventilator assistance via Ambu if severe respiratory distress or apnea Support circulation with fluids Discontinue continuous anesthesia infusion Avoid Aortacaval compression (FBC)
POSTDURAL PUNCTURE HEADACHE (PDPH) Results from a puncture of the dura during the procedure, allowing CSF to leak. The loss of CSF allows the brain to “settle”, causing a headache. Risk factors include – younger age, females, previous history of PDPH. Onset is typically 24 -48 hours after placement. Symptoms – pain in the frontal or occipital lobe, headache worsens when upright, neck ache, backache, nausea, visual disturbance, auditory disturbance, Treatment – bedrest, hydration with oral and iv fluids, analgesics, caffeine (orally or IV), epidural blood patch
KNOWLEDGE CHECK: Mrs. Thompson reports a pounding frontal headache that she states has been getting worse since surgery and is more intense when sitting up. What is the likely cause and course of action? A. CSF leak due to Dural puncture, notify anesthesia provider B. Caffeine withdrawal due to NPO status, obtain an order for IV caffeine C. Dehydration, obtain order for IV fluid bolus D. Common side effect of epidural, medicate with analgesics as ordered
ANSWER: Mrs. Thompson reports a pounding frontal headache that she states has been getting worse since surgery and is more intense when sitting up. What is the likely cause and course of action? A. CSF leak due to Dural puncture, notify anesthesia provider B. Caffeine withdrawal due to NPO status, obtain an order for IV caffeine C. Dehydration, obtain order for IV fluid bolus D. Common side effect of epidural, medicate with analgesics as ordered
REFERENCES Baylor Scott & White Health. (2014). Risks and Benefits of Epidural Anesthesia. Retrieved from http: //www. sw. org/Health. Library? page=Risks%20 and%20 Be nefits% 20 of%20 Epidural%20 Anesthesia Krames. (2015). What is Epidural Anesthesia? Retrieved from http: //resurgens. kramesonline. com/Health. Sheets/3, S, 84977 The Royal Children’s Hospital Melbourne. (2015). Assessment of Motor Block. Retrieved from http: //www. rch. org. au/anaes/pain_management/Assessment _of_m otor_block/