Nursing Care of the Adult System with Musculoskeletal










- Slides: 76
Nursing Care of the Adult System with Musculoskeletal Stressors Zelne Zamora, DNP, RN
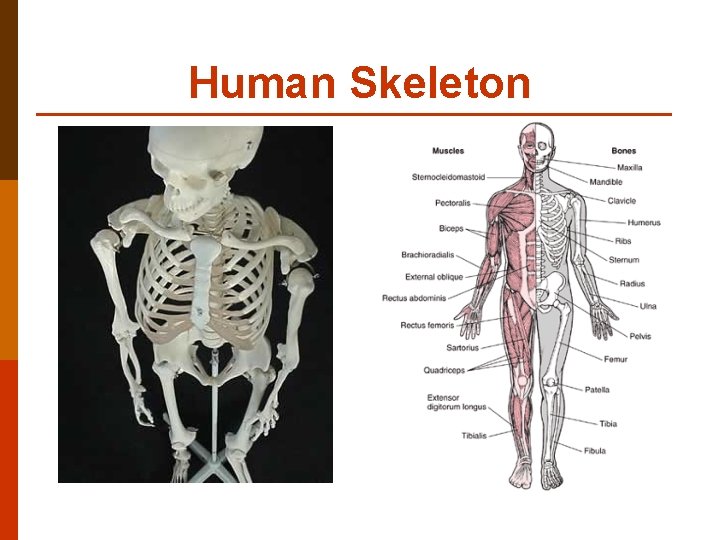
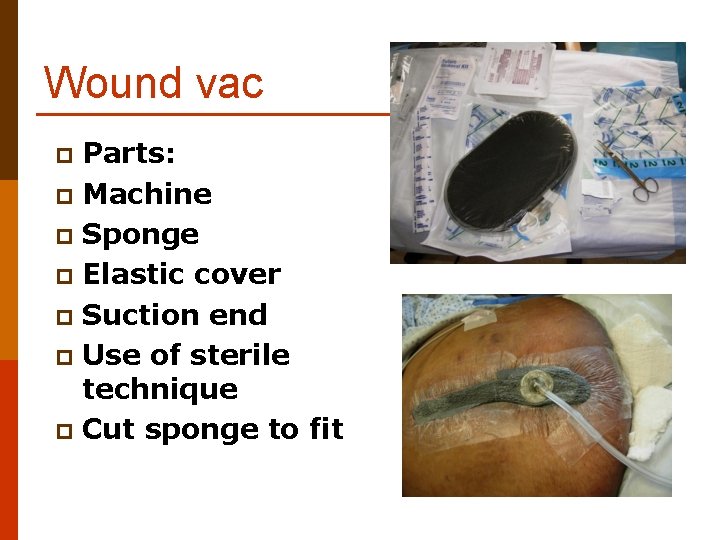
Human Skeleton
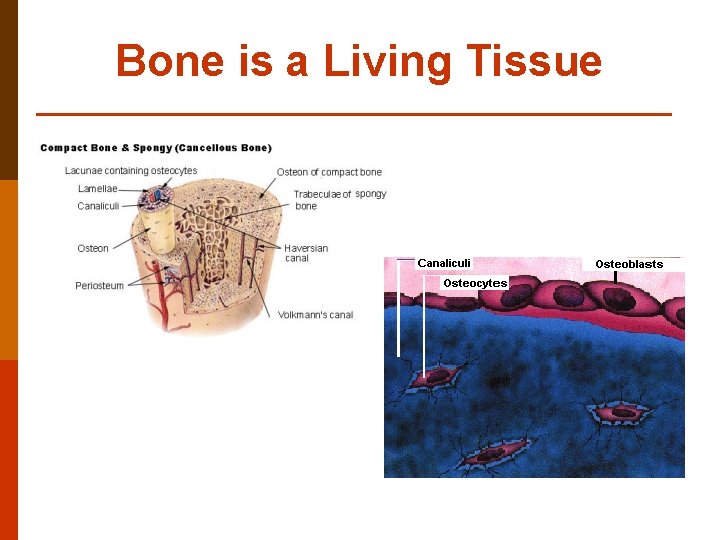
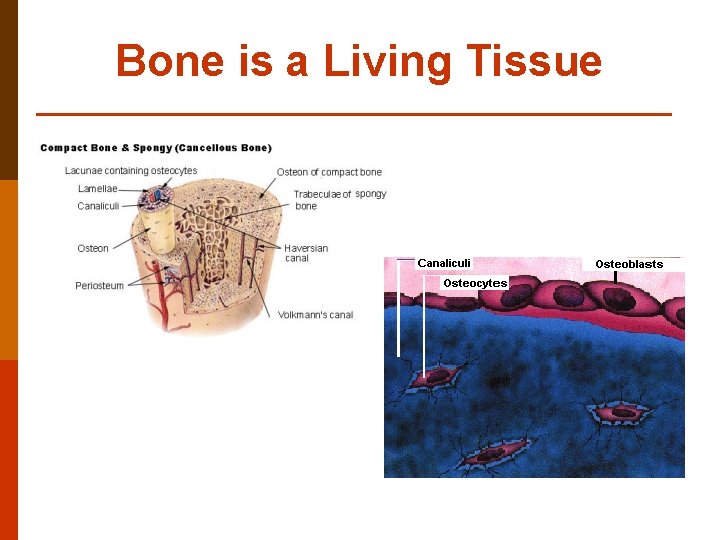
Bone is a Living Tissue
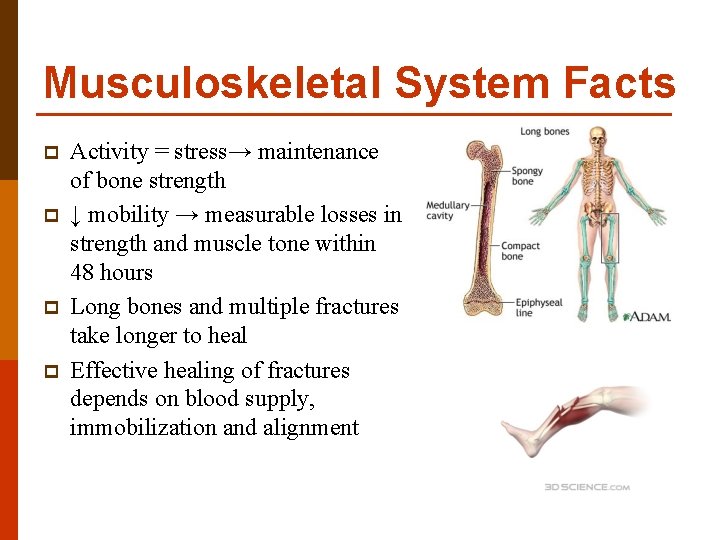
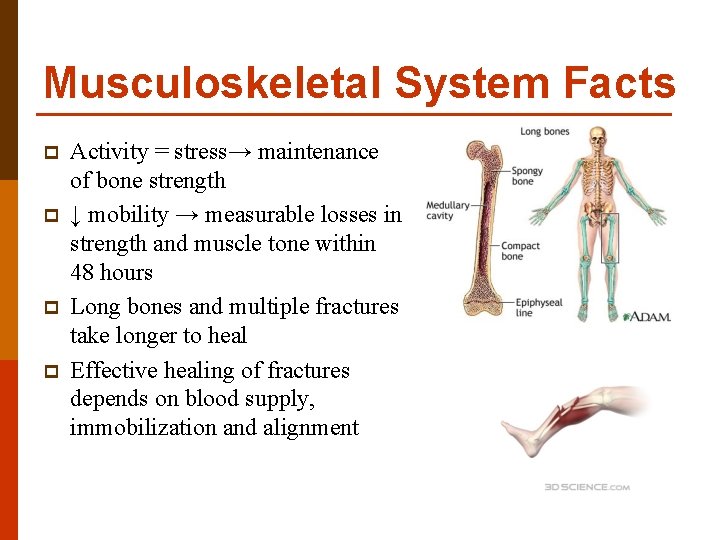
Musculoskeletal System Facts p p Activity = stress→ maintenance of bone strength ↓ mobility → measurable losses in strength and muscle tone within 48 hours Long bones and multiple fractures take longer to heal Effective healing of fractures depends on blood supply, immobilization and alignment
Musculoskeletal System Facts p Major body systems are impacted by immobility n Lungs n Renal n Cardiovascular n Skin
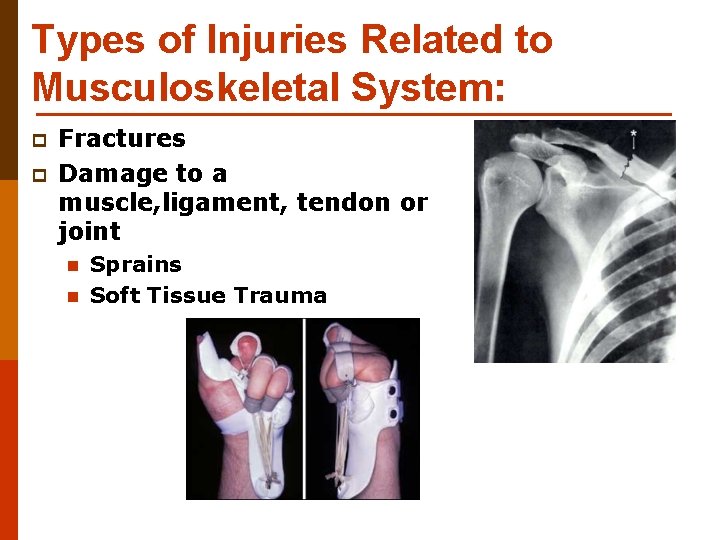
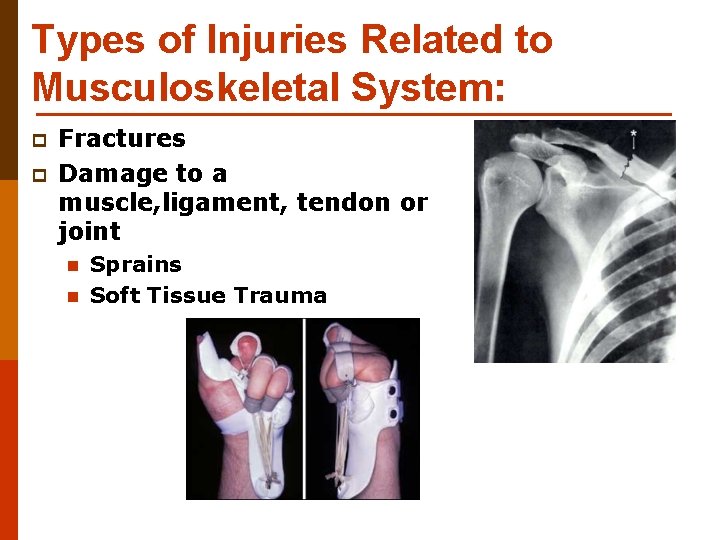
Types of Injuries Related to Musculoskeletal System: p p Fractures Damage to a muscle, ligament, tendon or joint n n Sprains Soft Tissue Trauma
Soft tissue trauma p p p Treatment first aid for soft tissue injuries R – rest I – ice for 48 -72 hours C – compression E – Elevation above level of the heart
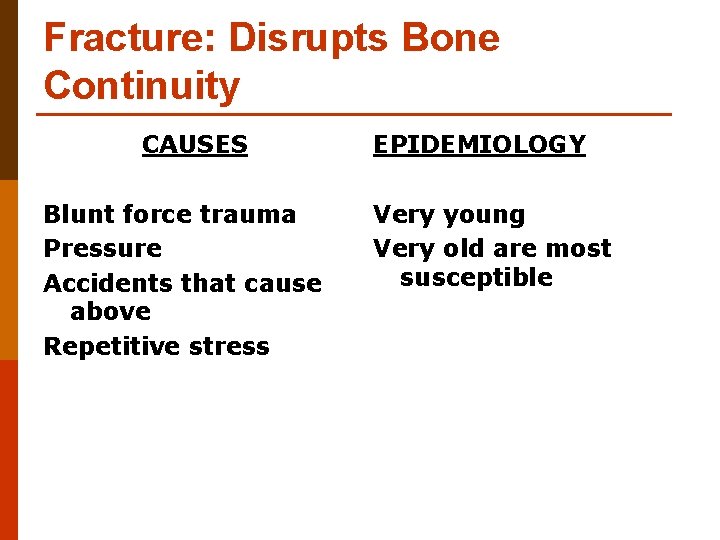
Fracture: Disrupts Bone Continuity CAUSES Blunt force trauma Pressure Accidents that cause above Repetitive stress EPIDEMIOLOGY Very young Very old are most susceptible
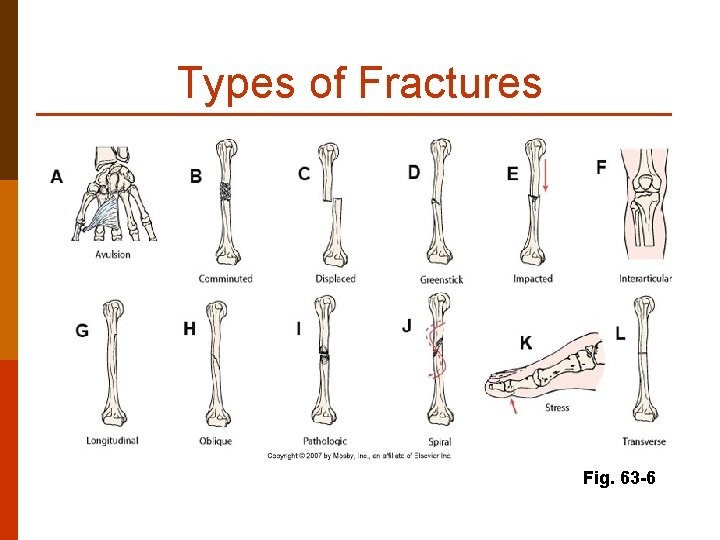
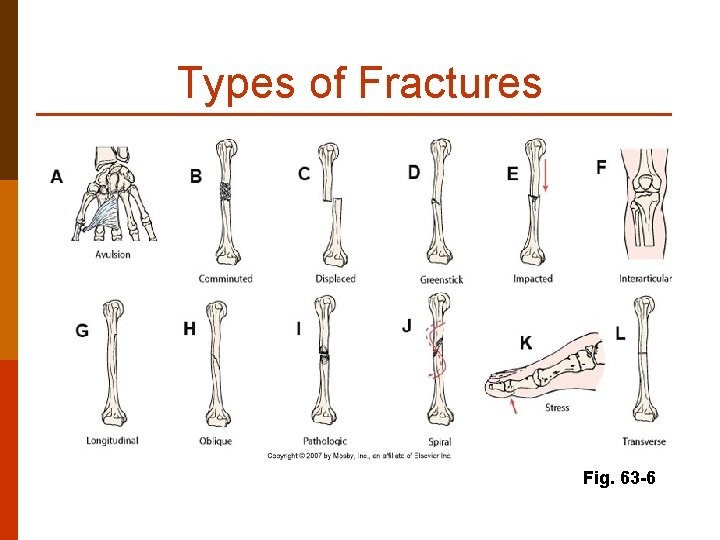
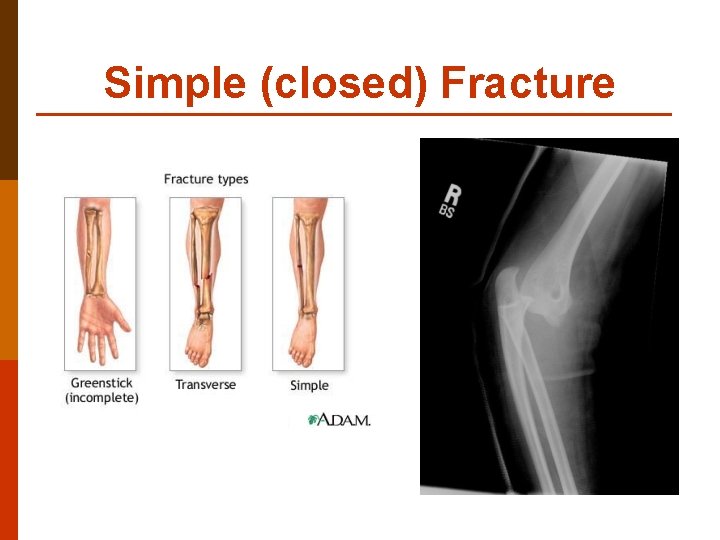
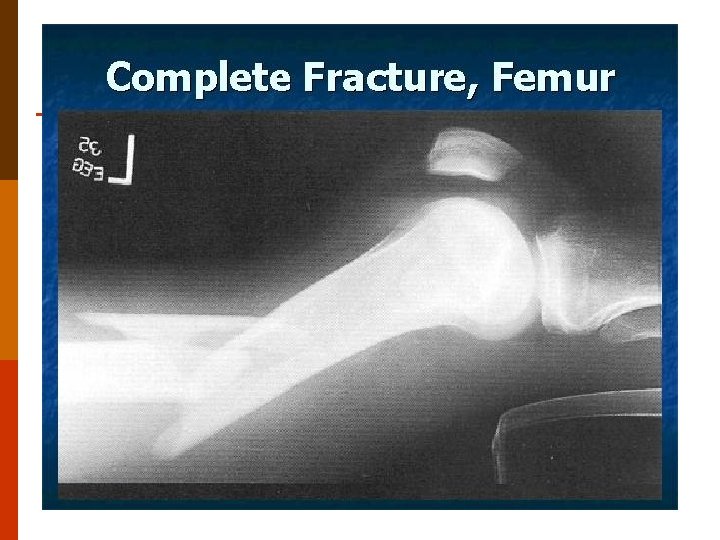
Types of Fractures Fig. 63 -6
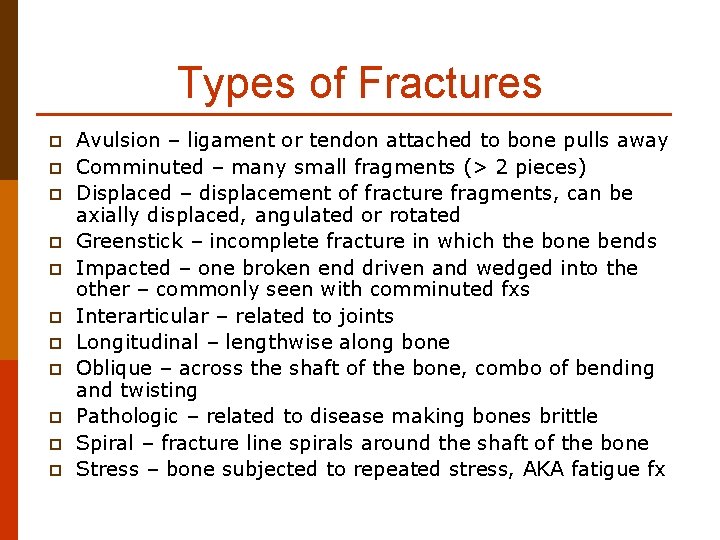
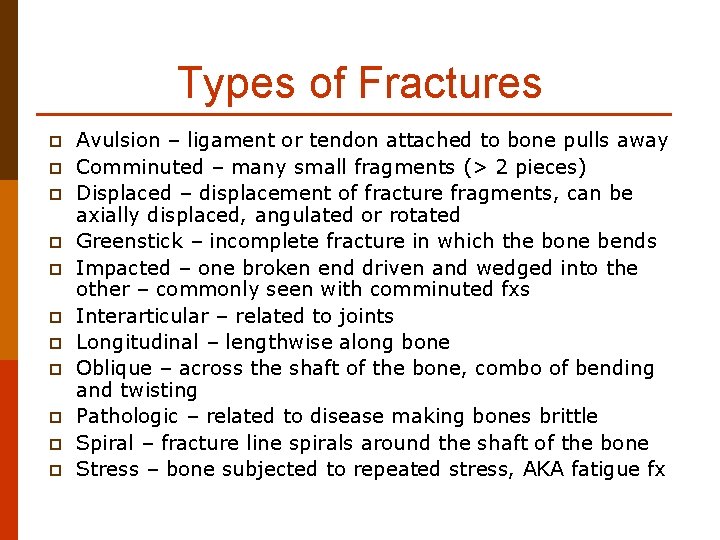
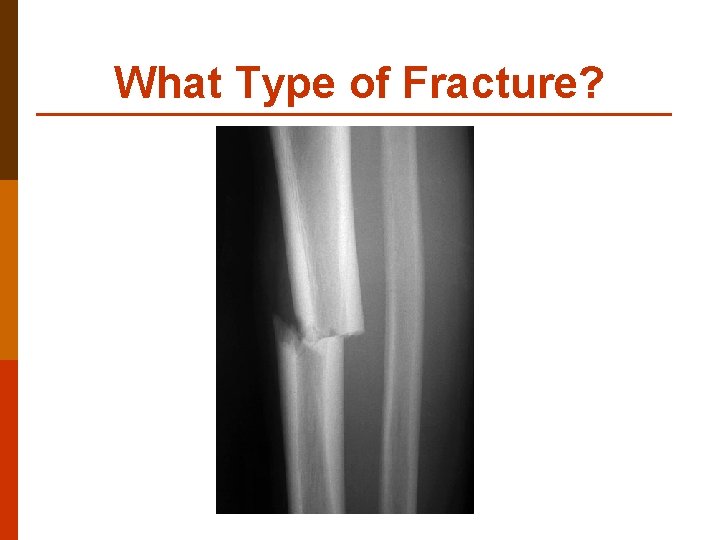
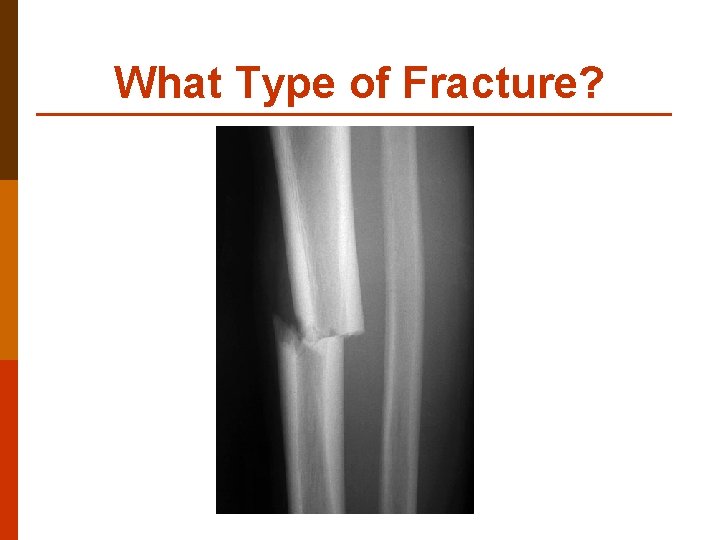
Types of Fractures p p p Avulsion – ligament or tendon attached to bone pulls away Comminuted – many small fragments (> 2 pieces) Displaced – displacement of fracture fragments, can be axially displaced, angulated or rotated Greenstick – incomplete fracture in which the bone bends Impacted – one broken end driven and wedged into the other – commonly seen with comminuted fxs Interarticular – related to joints Longitudinal – lengthwise along bone Oblique – across the shaft of the bone, combo of bending and twisting Pathologic – related to disease making bones brittle Spiral – fracture line spirals around the shaft of the bone Stress – bone subjected to repeated stress, AKA fatigue fx
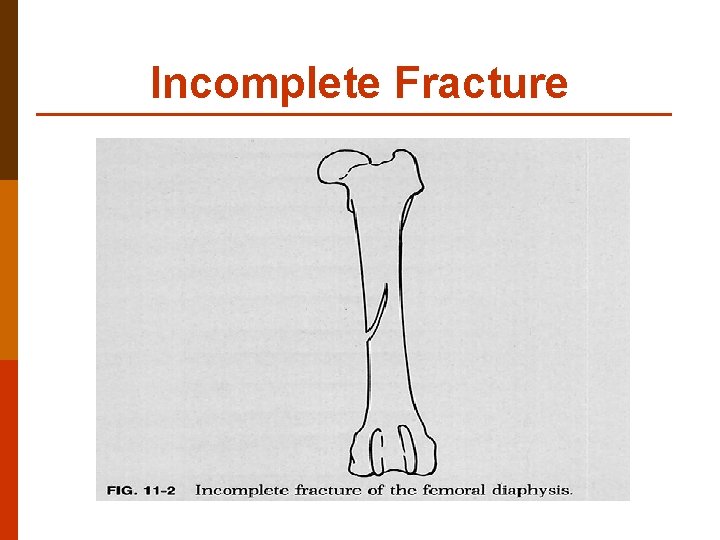
Incomplete Fracture
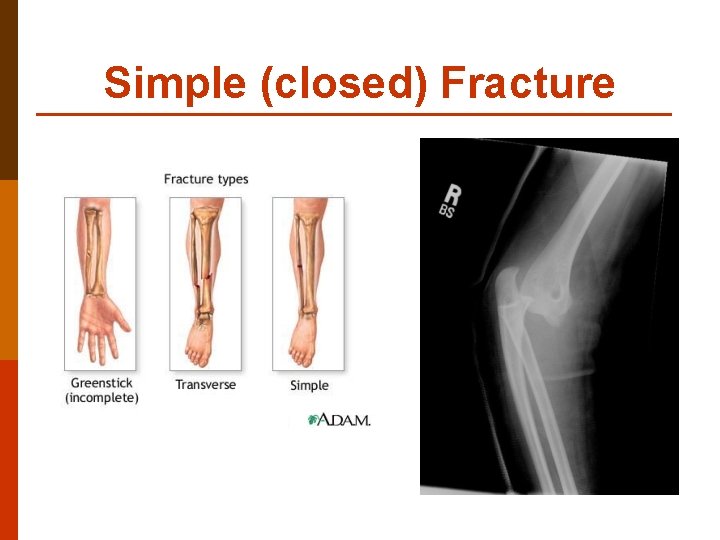
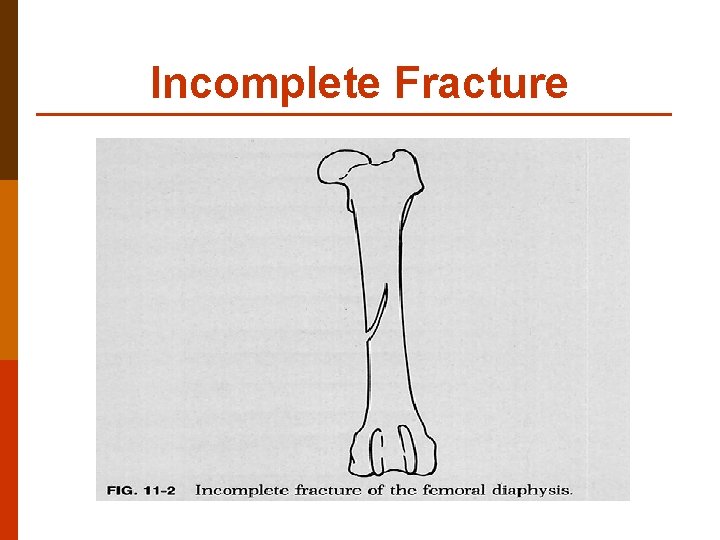
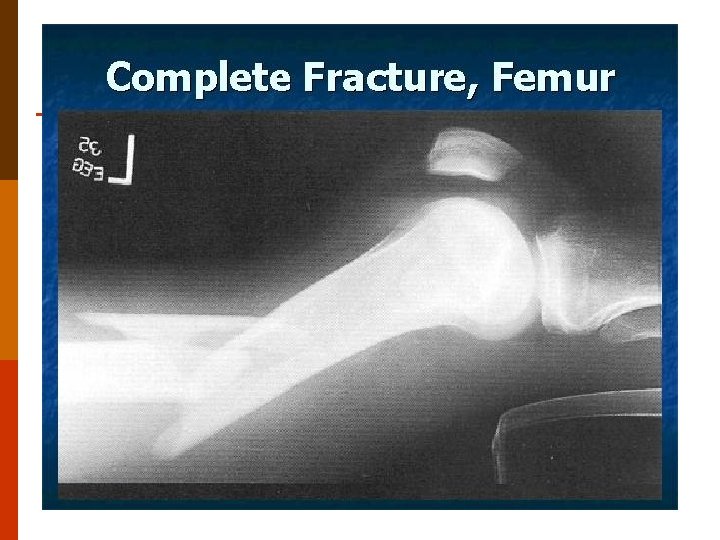
Simple (closed) Fracture
WARNING! p Next slides with graphic photos
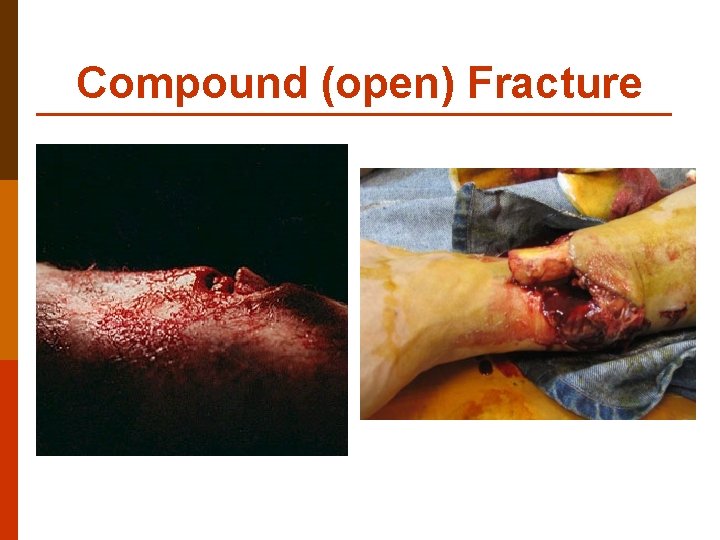
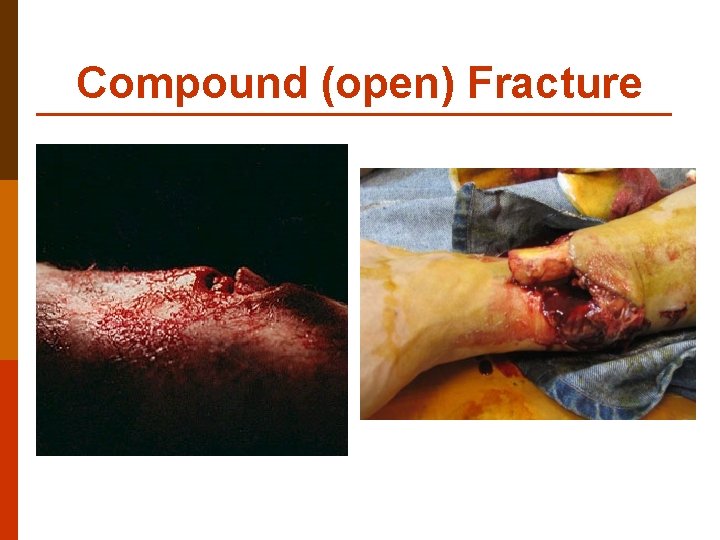
Compound (open) Fracture

What Type of Fracture?
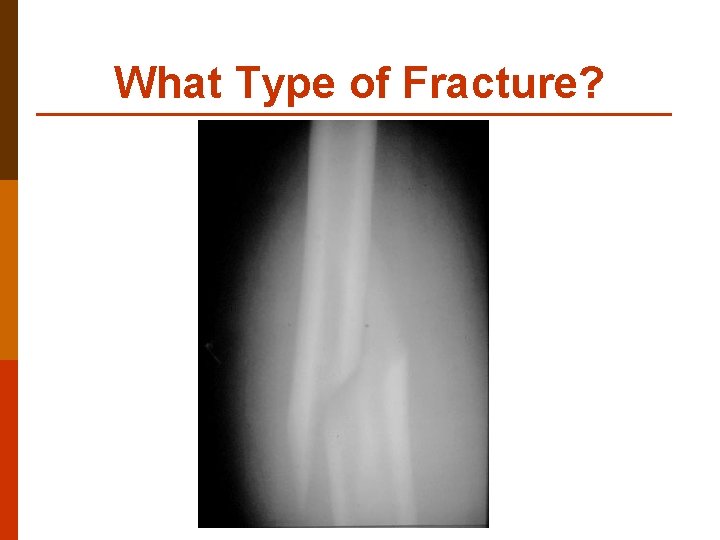
What Type of Fracture?
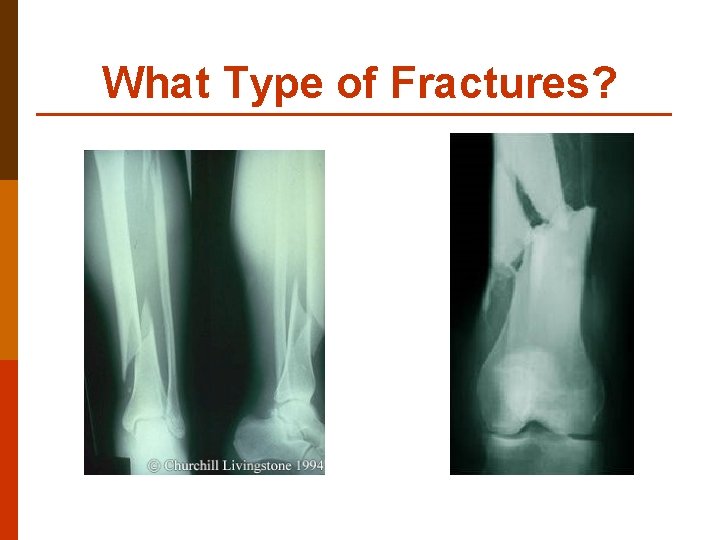
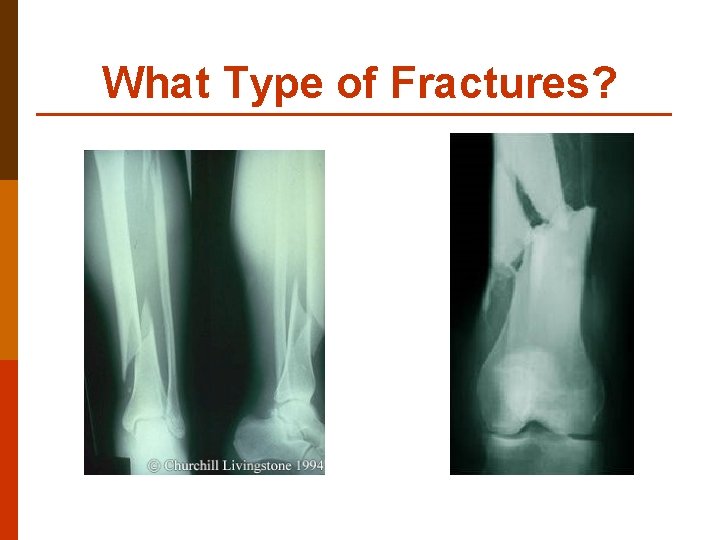
What Type of Fractures?
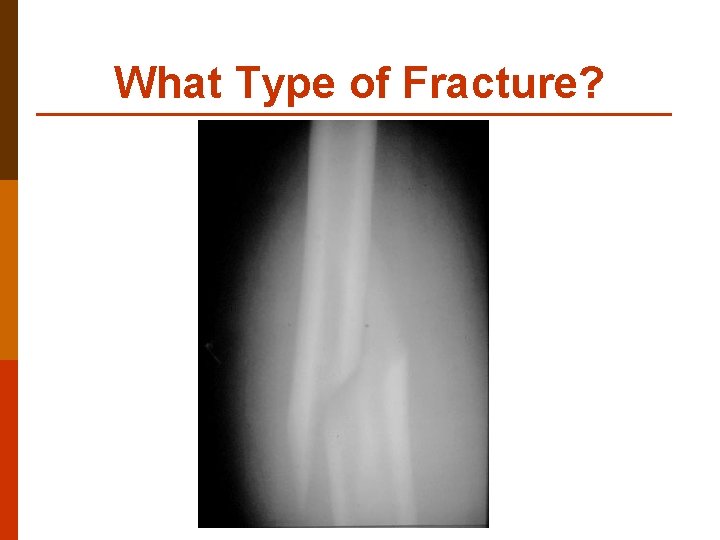
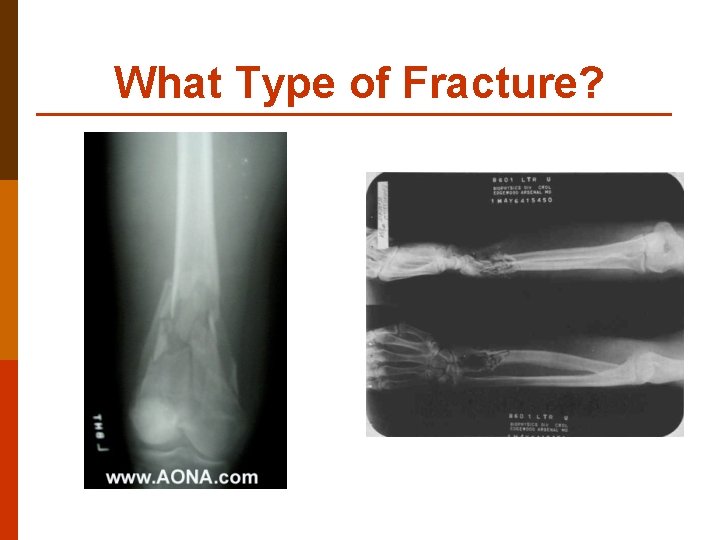
What Type of Fracture?
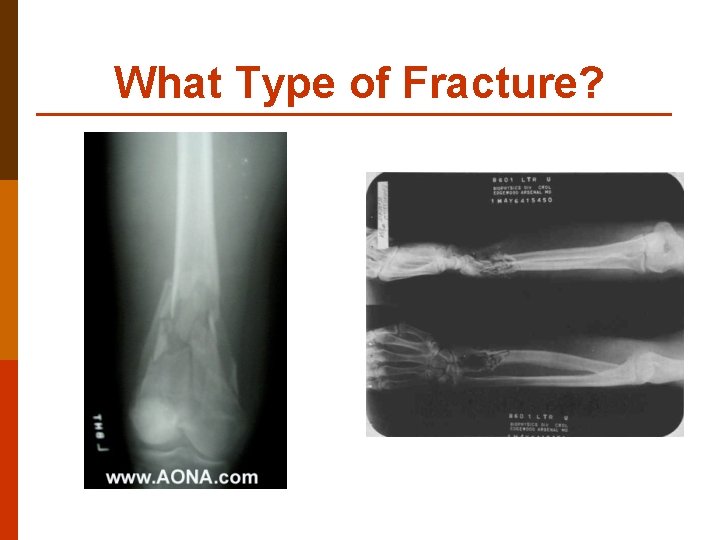
What Type of Fracture?
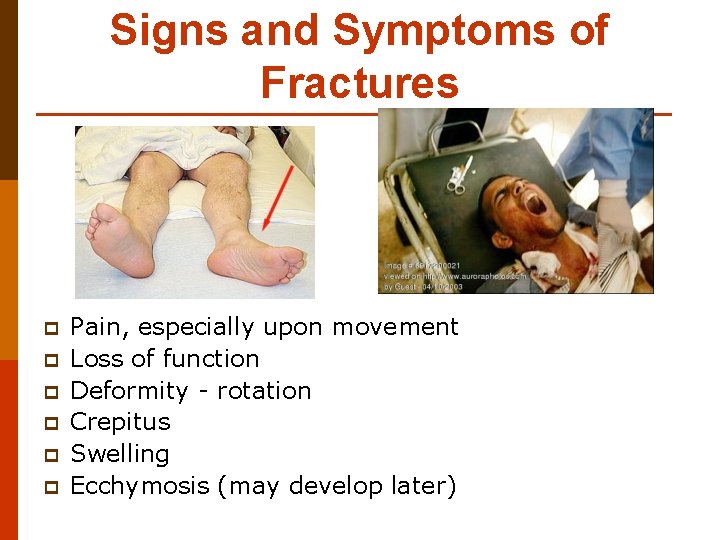
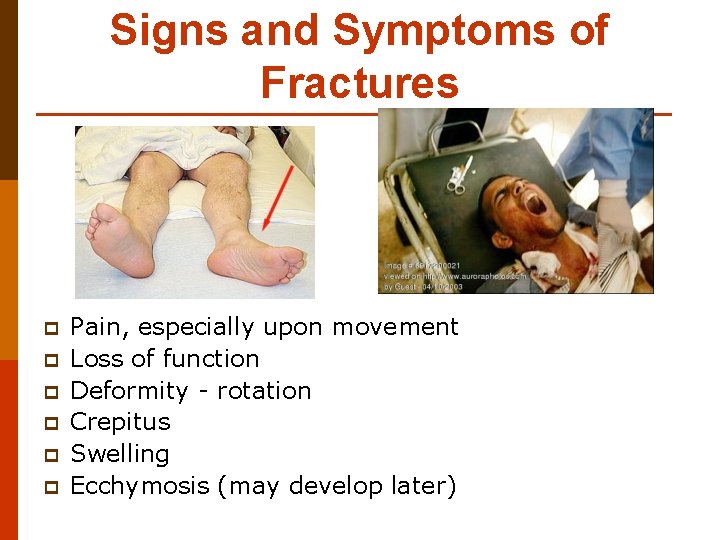
Signs and Symptoms of Fractures p p p Pain, especially upon movement Loss of function Deformity - rotation Crepitus Swelling Ecchymosis (may develop later)
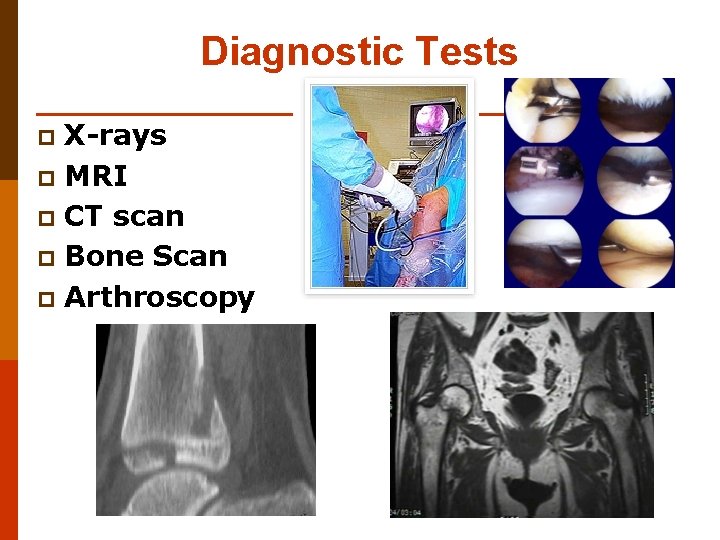
Diagnostic Tests X-rays p MRI p CT scan p Bone Scan p Arthroscopy p
LABS p p p Serum Calcium (9 -11 mg/dl) Phosphorus (2. 5 -4. 5 mg/dl) Alkaline phosphatase (4. 3 -13 U/dl) Calcitonin Vitamin D Myoglobin (negative in both urine and serum)
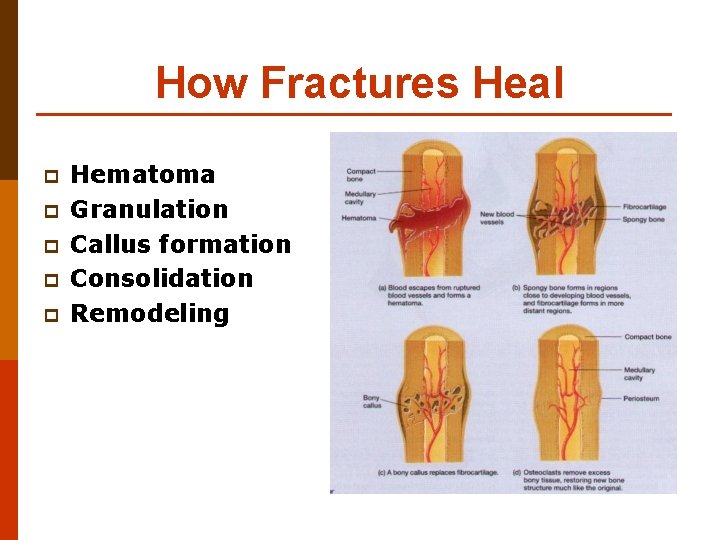
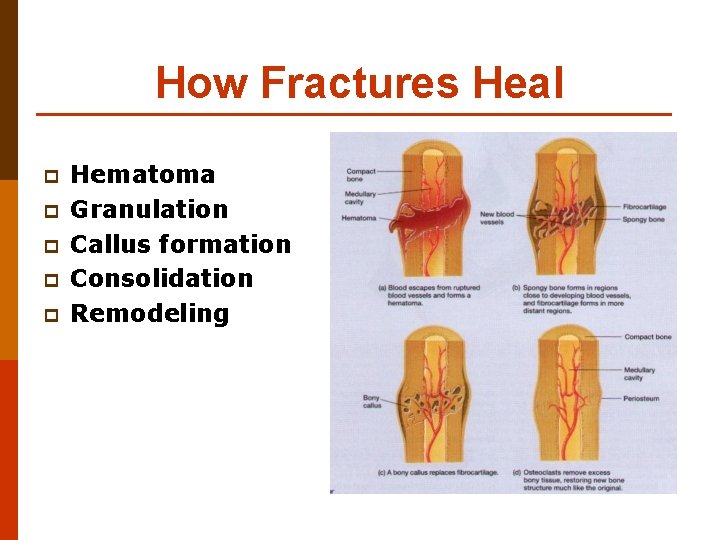
How Fractures Heal p p p Hematoma Granulation Callus formation Consolidation Remodeling
WARNING! p Next slides with graphic photos
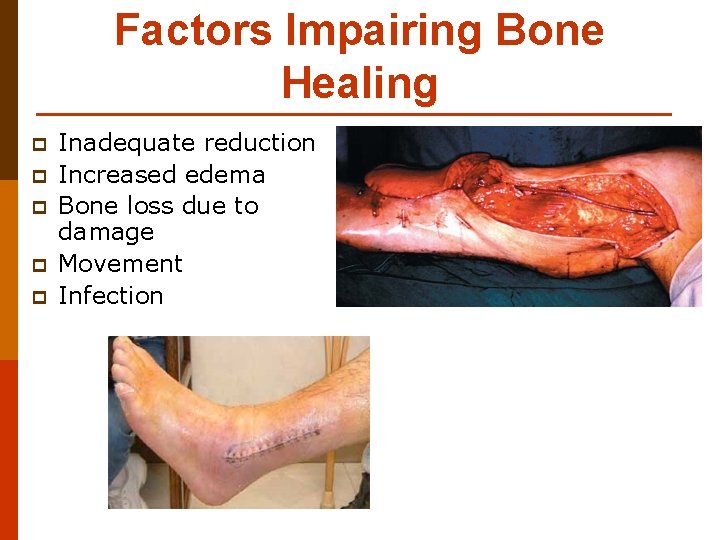
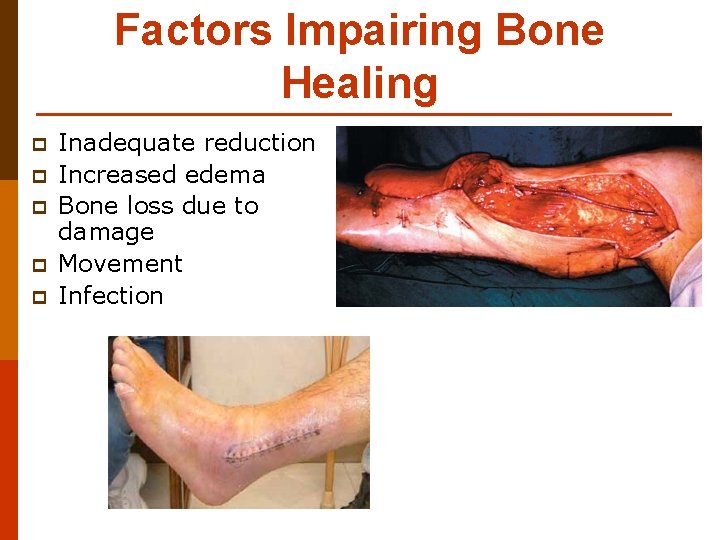
Factors Impairing Bone Healing p p p Inadequate reduction Increased edema Bone loss due to damage Movement Infection
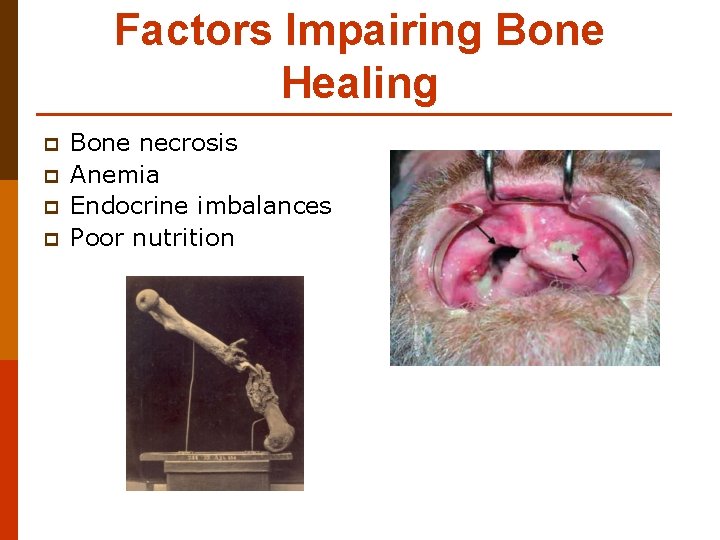
Factors Impairing Bone Healing p p Bone necrosis Anemia Endocrine imbalances Poor nutrition
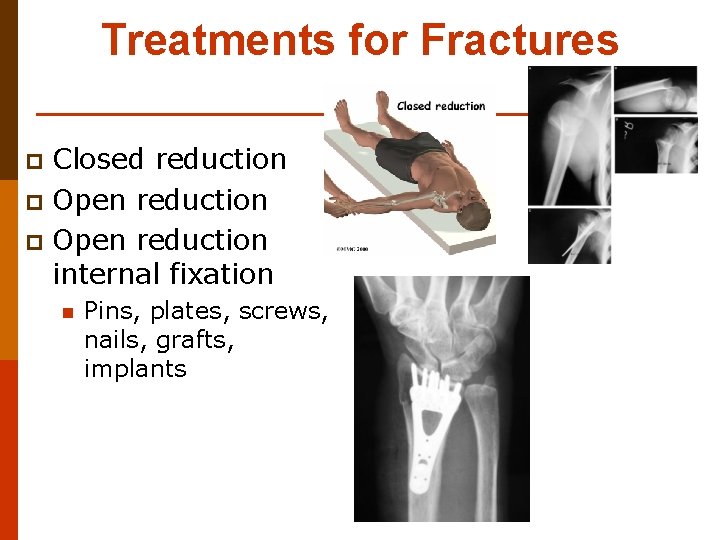
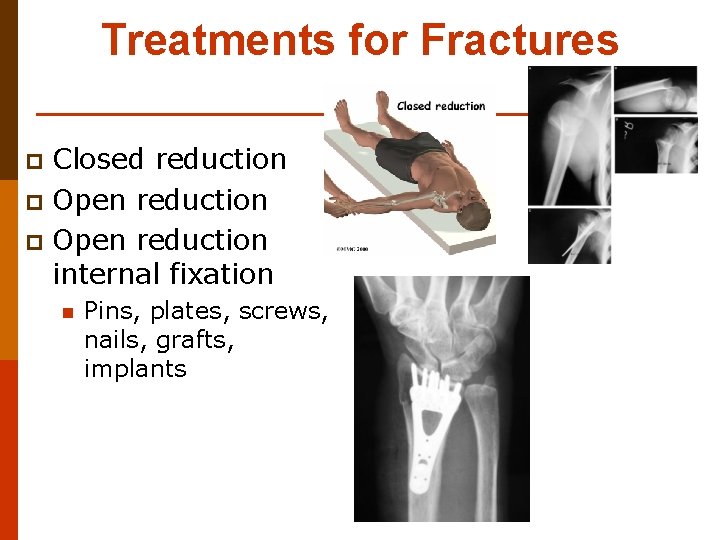
Treatments for Fractures Closed reduction p Open reduction internal fixation p n Pins, plates, screws, nails, grafts, implants

Treatments for Fractures p Open reduction external fixation n p p Casts, splints, braces, traction Compound fractures may involve cleaning, debriding and infection prevention Traction
Casts – Extremities p p p Re-alignment Maintaining alignment Uniform pressure on encased soft tissue
Casts p Plaster n n n p Softer Heat given off during application Hardens over time – easily “dented” Skin irritation/breakdown Usually applied first, then changed to fiberglass Assess CMS – circulation, motion, sensation

Casts p Non-plaster or fiberglass n n Lighter weight Stronger – dry thoroughly Durable Water resistant
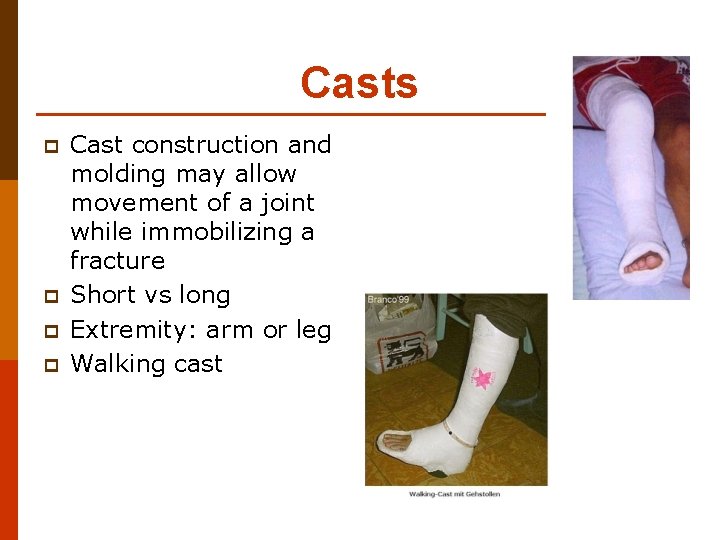
Casts p p Cast construction and molding may allow movement of a joint while immobilizing a fracture Short vs long Extremity: arm or leg Walking cast
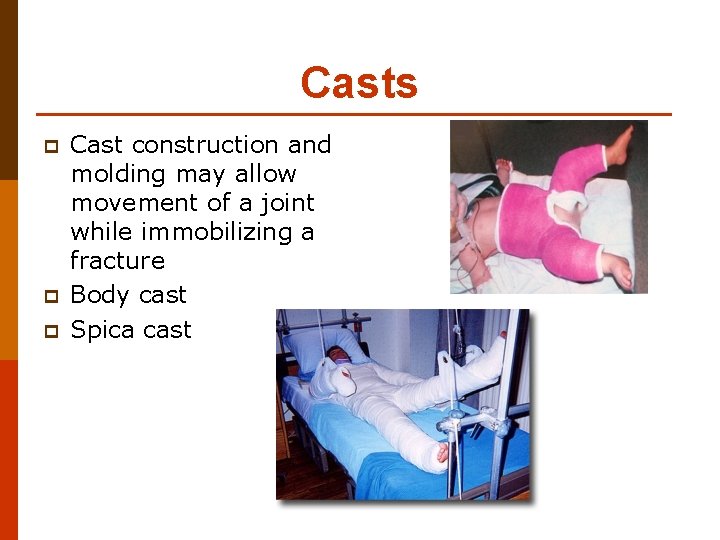
Casts p p p Cast construction and molding may allow movement of a joint while immobilizing a fracture Body cast Spica cast
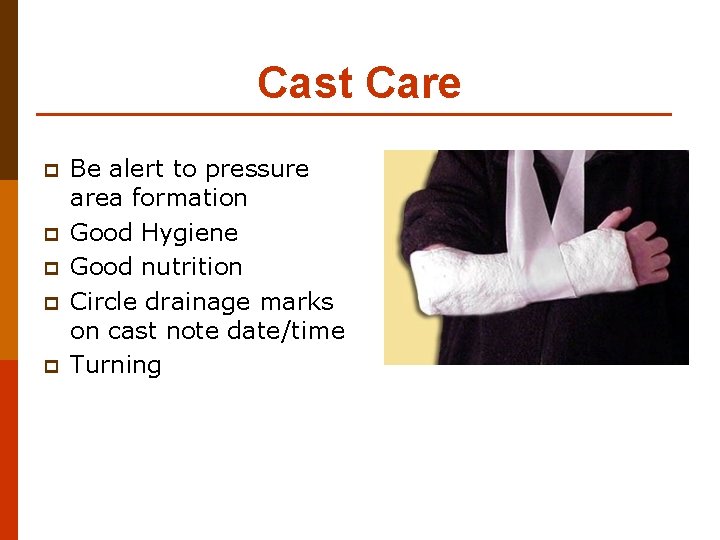
Cast Care p p Elevate, elevate, elevate! Neurovascular checks (CMS) Care of skin Pain management
Cast Care p p p Be alert to pressure area formation Good Hygiene Good nutrition Circle drainage marks on cast note date/time Turning
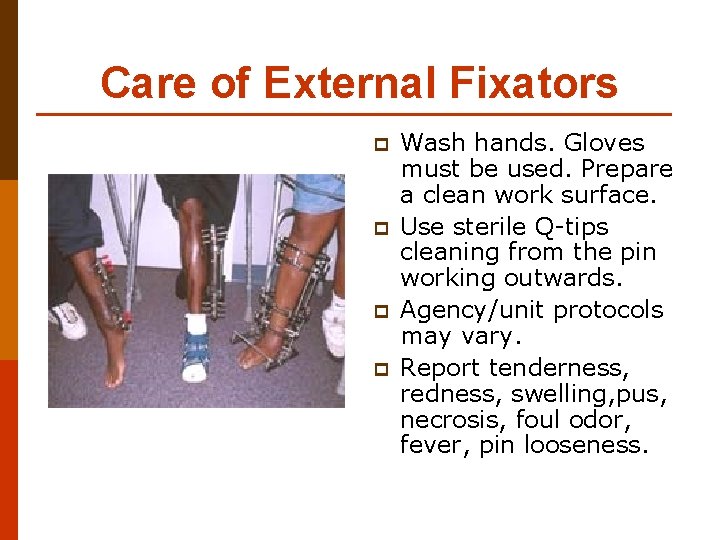
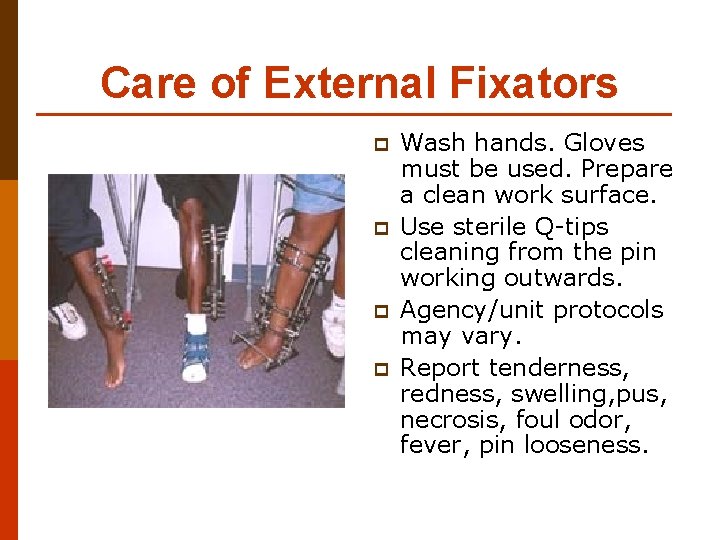
Care of External Fixators p p Wash hands. Gloves must be used. Prepare a clean work surface. Use sterile Q-tips cleaning from the pin working outwards. Agency/unit protocols may vary. Report tenderness, redness, swelling, pus, necrosis, foul odor, fever, pin looseness.

S/S of neurovascular impairment p p p Pallor Cyanosis Prolonged capillary refill Edema Increased pain

S/S of neurovascular impairment p p p Cool/cold tissue Diminished or absent pulses Changes in sensation
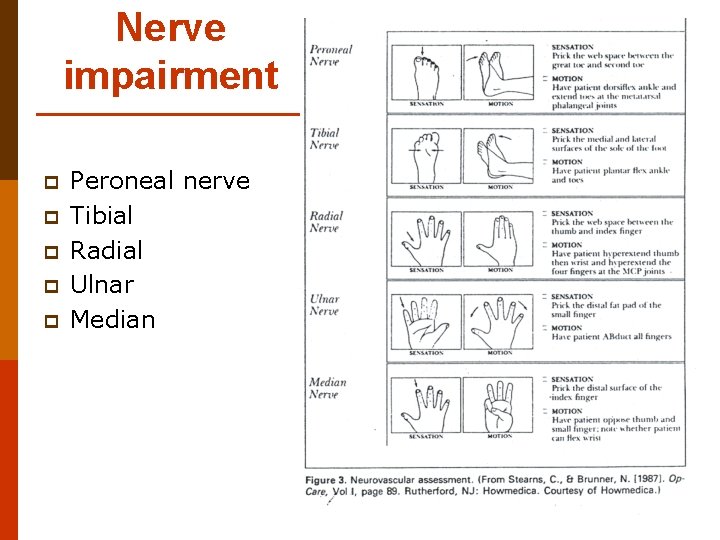
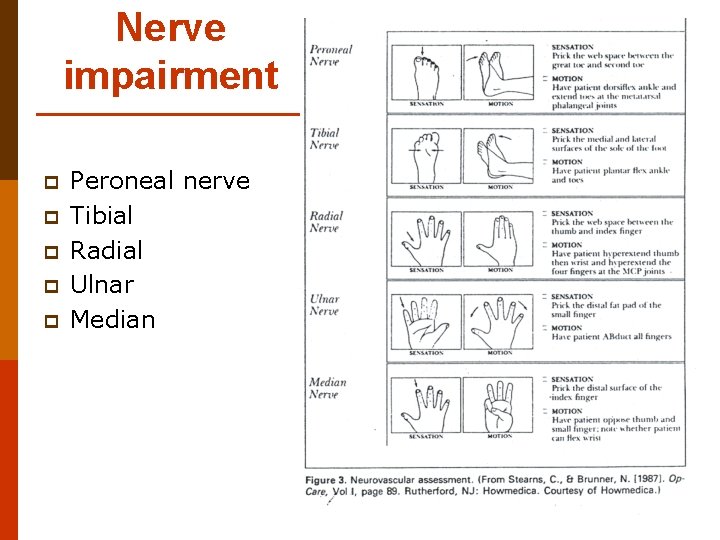
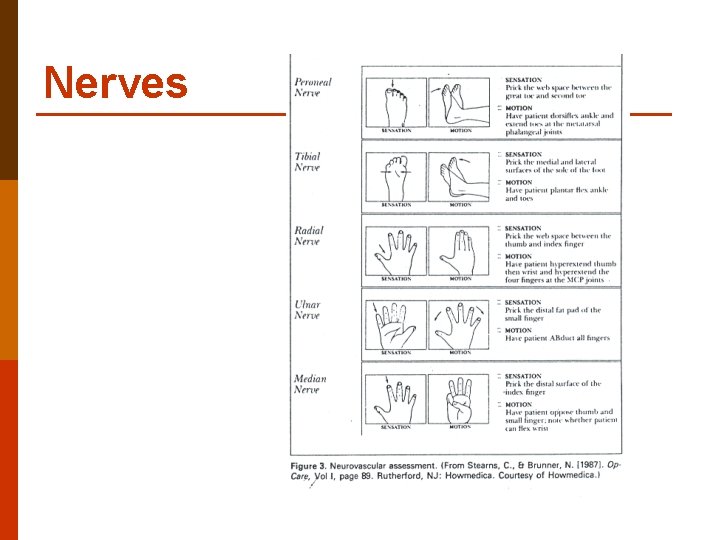
Nerve impairment p p p Peroneal nerve Tibial Radial Ulnar Median
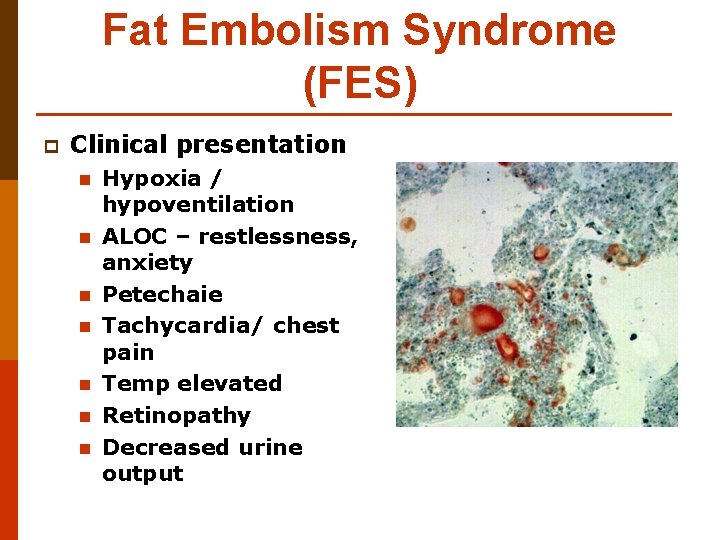
Fat Embolism Syndrome (FES) p Pathophysiology n n Fat particles enter circulation via fracture site Increase clotting and viscosity
Fat Embolism Syndrome (FES) p Clinical presentation n n n Hypoxia / hypoventilation ALOC – restlessness, anxiety Petechaie Tachycardia/ chest pain Temp elevated Retinopathy Decreased urine output
Fat Embolism Syndrome (FES) p Medical Treatment n n n p Early immobilization of fx Adequate oxygenation Adequate hydration Nursing interventions n n Awareness & vigilance – 1224 hrs Accurate I&O
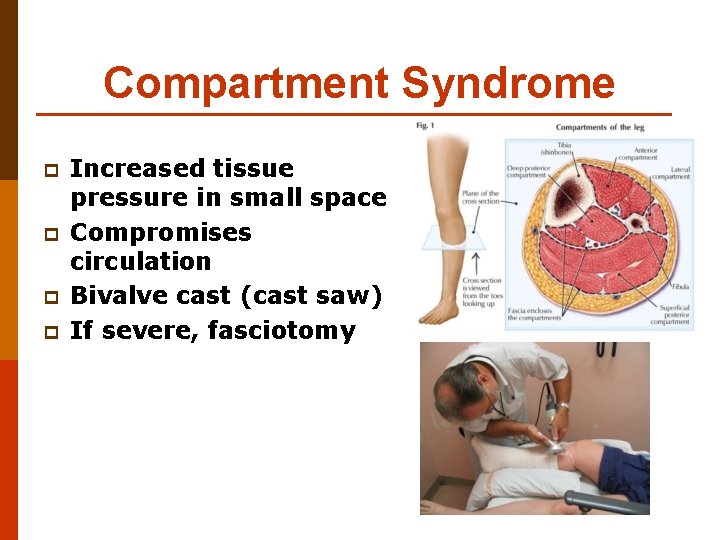
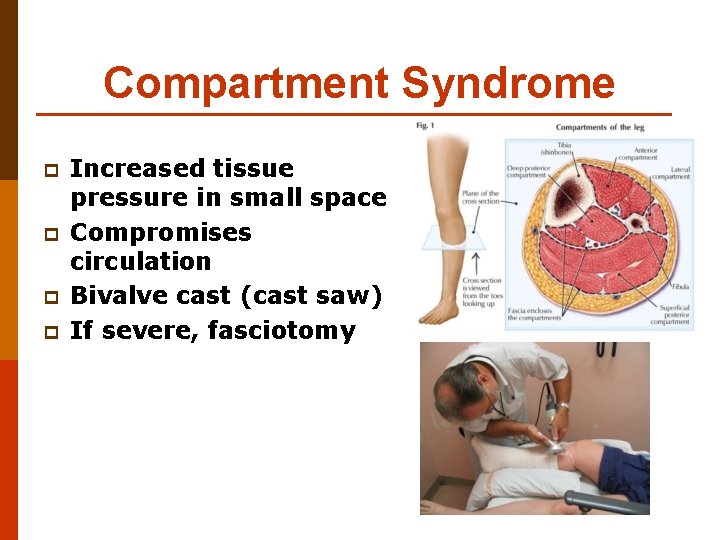
Compartment Syndrome p p Increased tissue pressure in small space Compromises circulation Bivalve cast (cast saw) If severe, fasciotomy

Compartment Syndrome p Commonly caused by: Poor cast care - CMS
Compartment Syndrome p http: //www. youtube. com/watch? v=k 1 Qn. E c. TP-c. Y p Warning: Graphic slide All rights and images to “Rizzoli & Isles” are courtesy of TNT broadcasting.

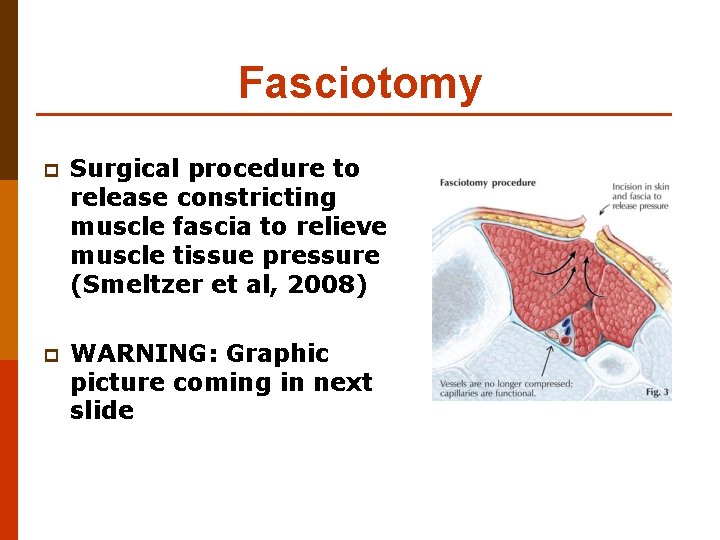
Fasciotomy
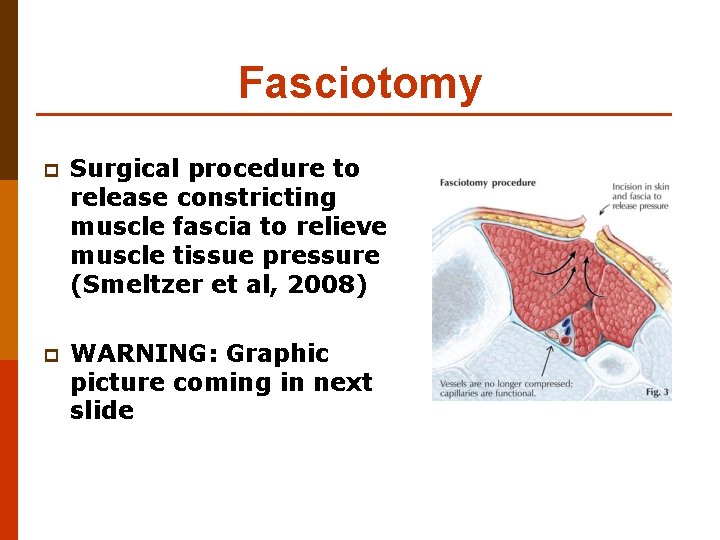
Fasciotomy p Surgical procedure to release constricting muscle fascia to relieve muscle tissue pressure (Smeltzer et al, 2008) p WARNING: Graphic picture coming in next slide
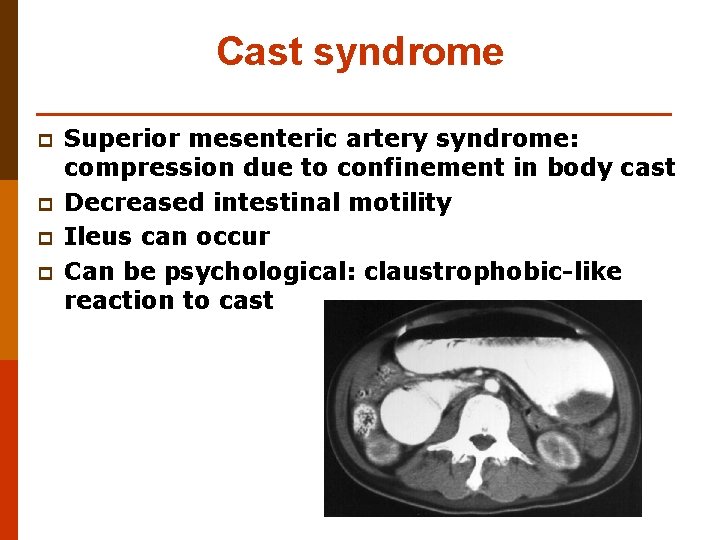
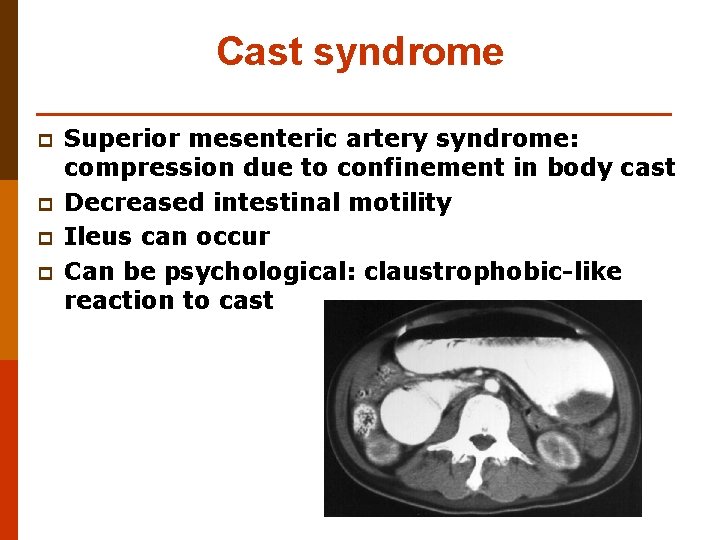
Cast syndrome p p Superior mesenteric artery syndrome: compression due to confinement in body cast Decreased intestinal motility Ileus can occur Can be psychological: claustrophobic-like reaction to cast
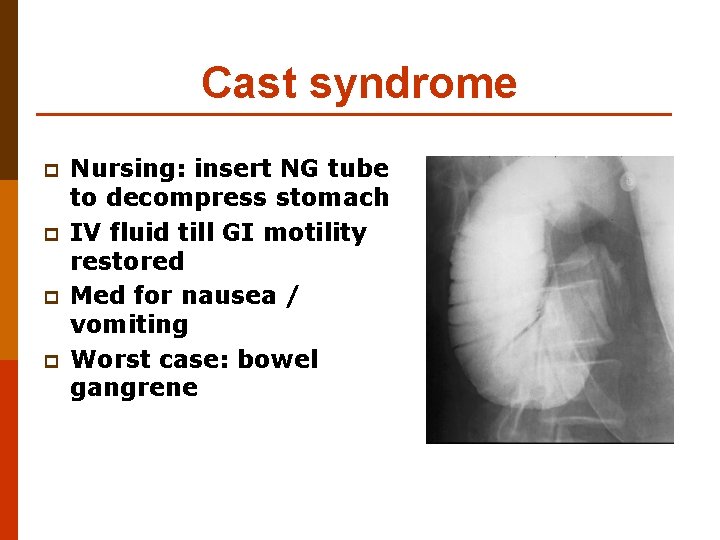
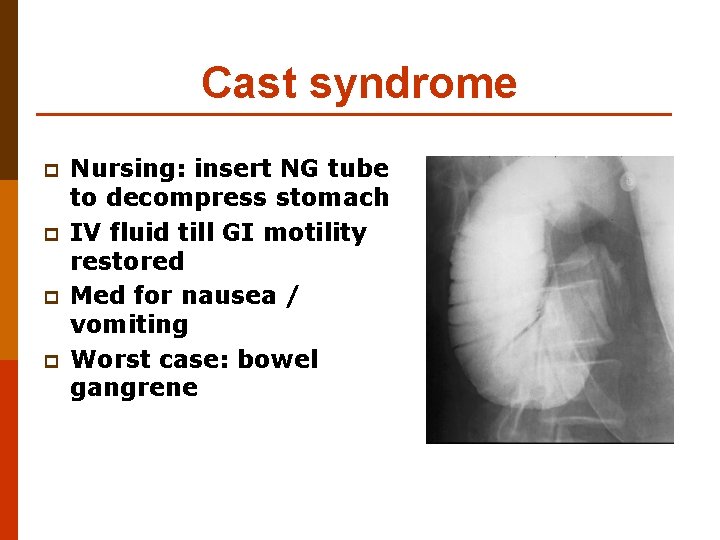
Cast syndrome p p Nursing: insert NG tube to decompress stomach IV fluid till GI motility restored Med for nausea / vomiting Worst case: bowel gangrene
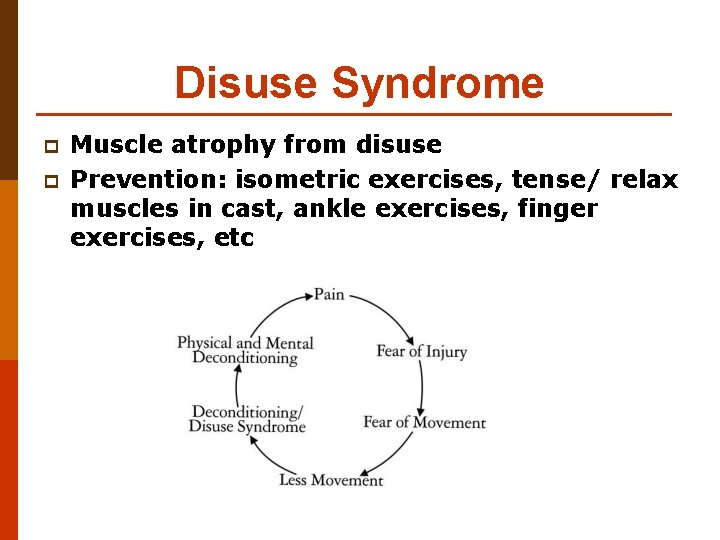
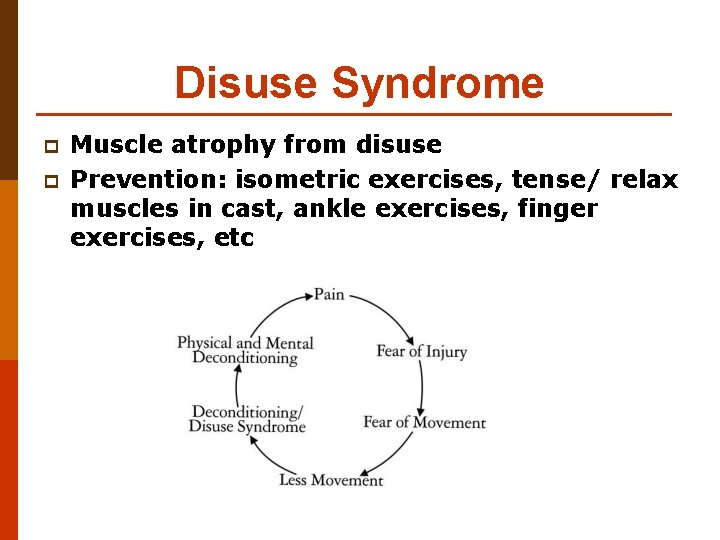
Disuse Syndrome p p Muscle atrophy from disuse Prevention: isometric exercises, tense/ relax muscles in cast, ankle exercises, finger exercises, etc

Traction
Uses To reduce a fracture or dislocation p Immobilize and maintain alignment p Prevent or reduce muscle spasm p Correct or prevent deformity p Provide rest and comfort post-op p
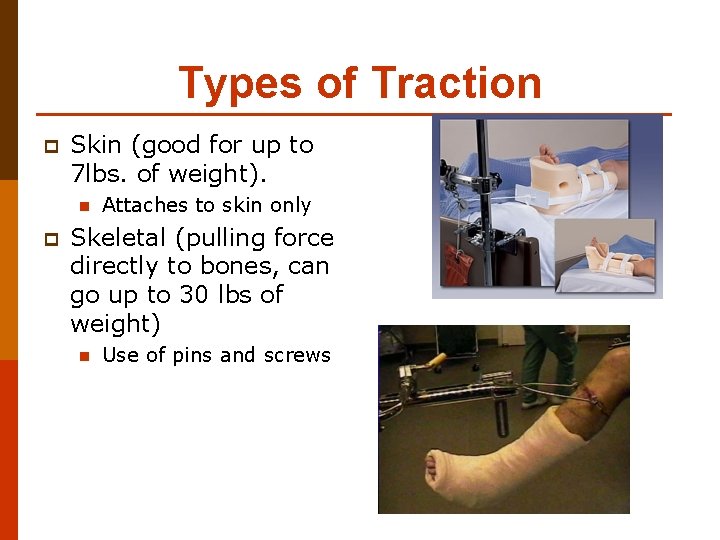
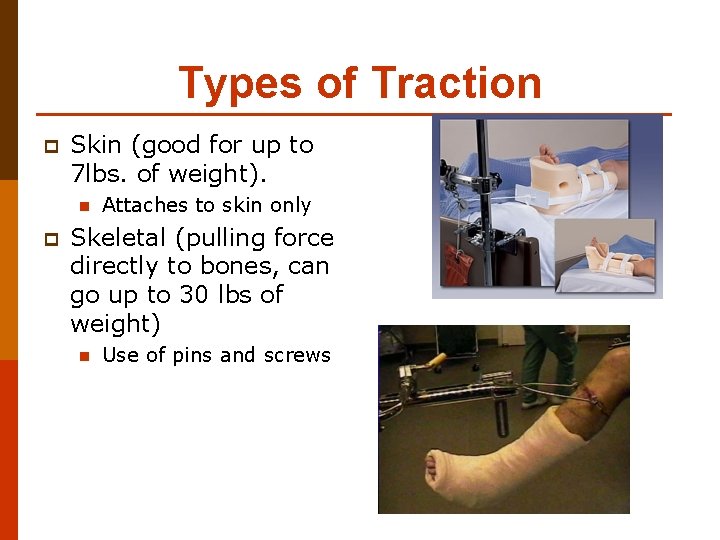
Types of Traction p Skin (good for up to 7 lbs. of weight). n p Attaches to skin only Skeletal (pulling force directly to bones, can go up to 30 lbs of weight) n Use of pins and screws
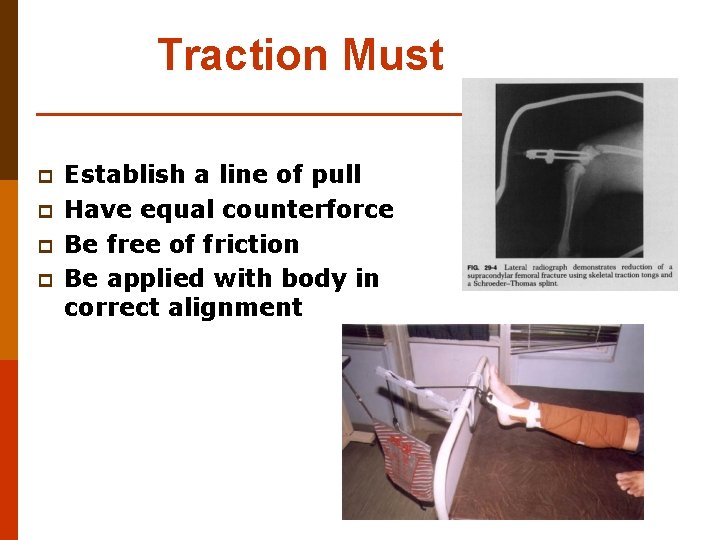
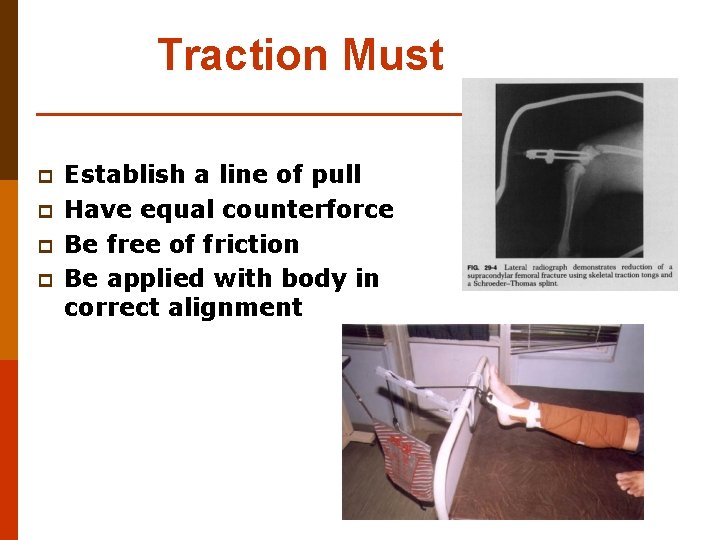
Traction Must p p Establish a line of pull Have equal counterforce Be free of friction Be applied with body in correct alignment
Buck’s Traction Uses an external pulling force p Leg must be fully in boot, heel touching p CMS remains priority in care p DOES NOT use countertraction p Skin breakdown with boot p
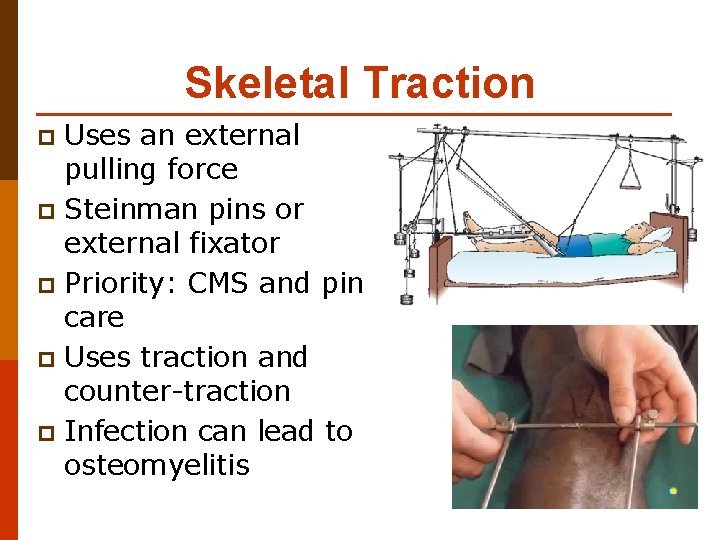
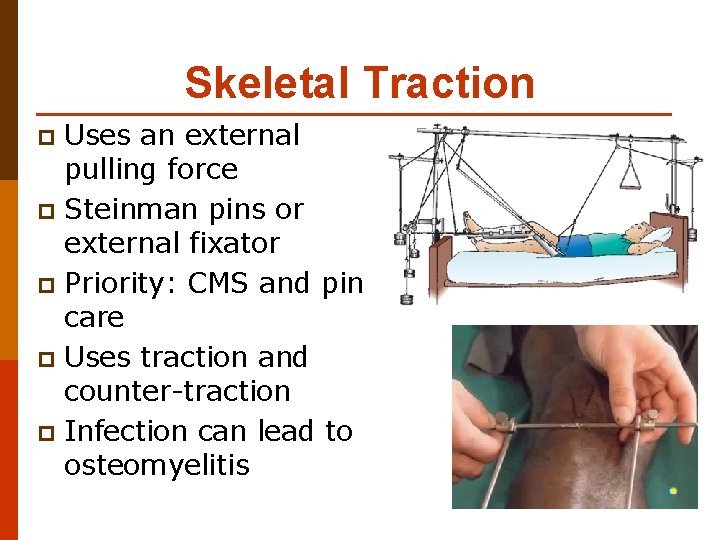
Skeletal Traction Uses an external pulling force p Steinman pins or external fixator p Priority: CMS and pin care p Uses traction and counter-traction p Infection can lead to osteomyelitis p
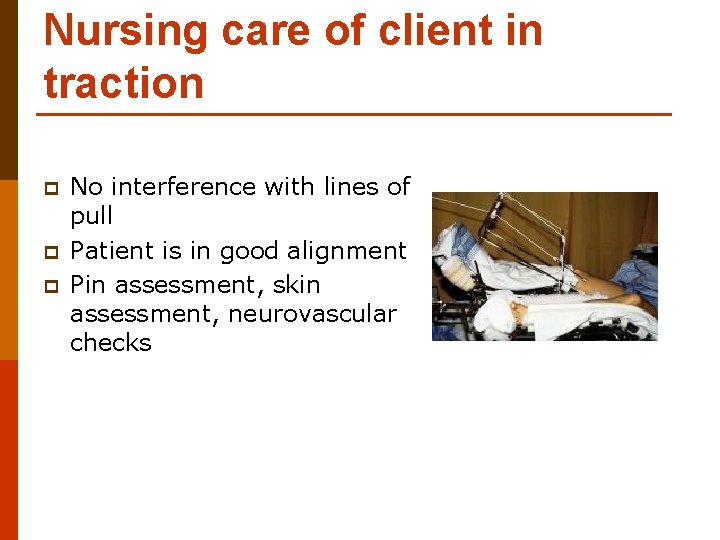
Nursing care of client in traction p p p No interference with lines of pull Patient is in good alignment Pin assessment, skin assessment, neurovascular checks
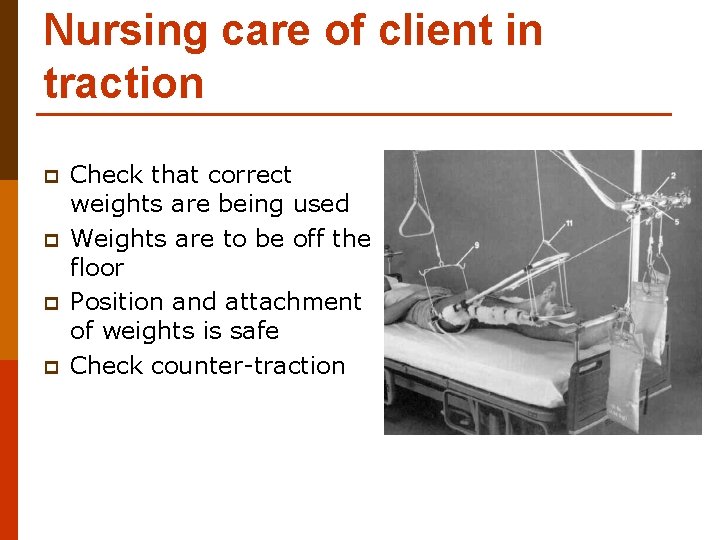
Nursing care of client in traction p p Check that correct weights are being used Weights are to be off the floor Position and attachment of weights is safe Check counter-traction
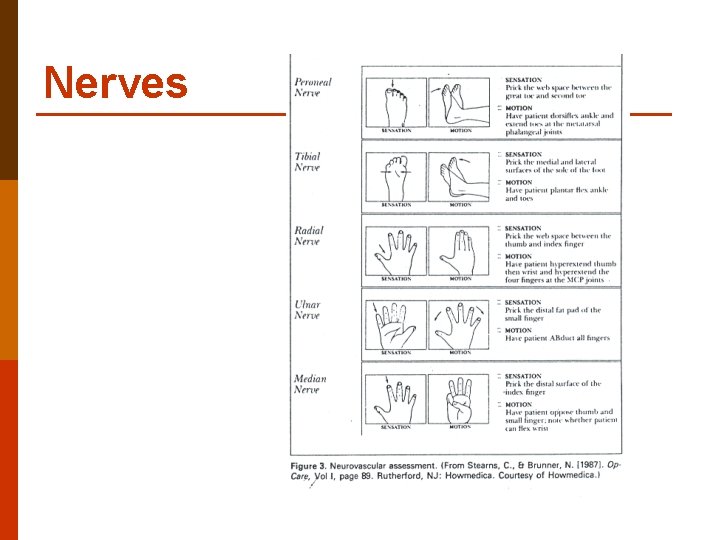
Nerves
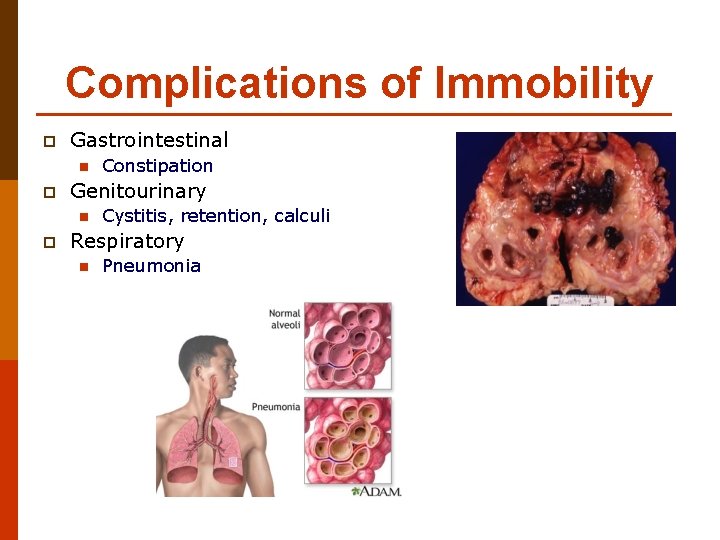
Complications of Immobility p Gastrointestinal n p Genitourinary n p Constipation Cystitis, retention, calculi Respiratory n Pneumonia
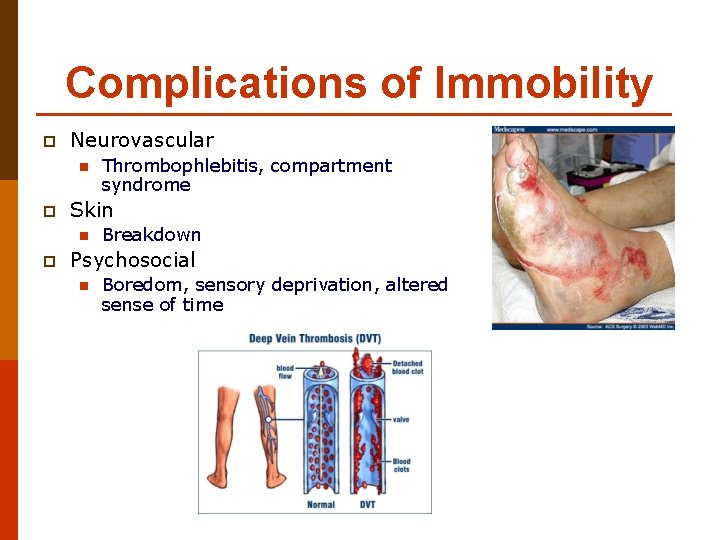
Complications of Immobility p Neurovascular n p Skin n p Thrombophlebitis, compartment syndrome Breakdown Psychosocial n Boredom, sensory deprivation, altered sense of time
Amputations
Reasons for amputation p p p Trauma Tumor Infection Advanced PVD Compartment syndrome complications WARNING: graphic picture coming
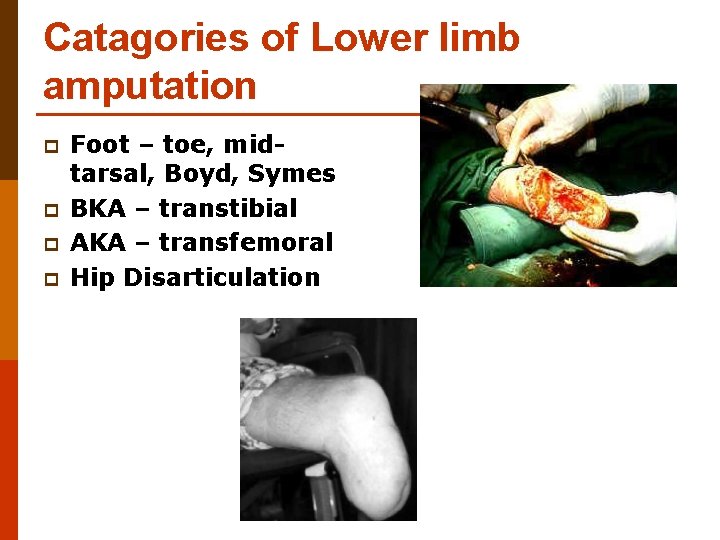
Catagories of Lower limb amputation p p Foot – toe, midtarsal, Boyd, Symes BKA – transtibial AKA – transfemoral Hip Disarticulation
Pre-Op Care p p p Stabilization of diabetes Well nourished and hydrated PT and OT consultations Emotional Support Teaching n n Pain management, phantom limb Prosthetic preparation
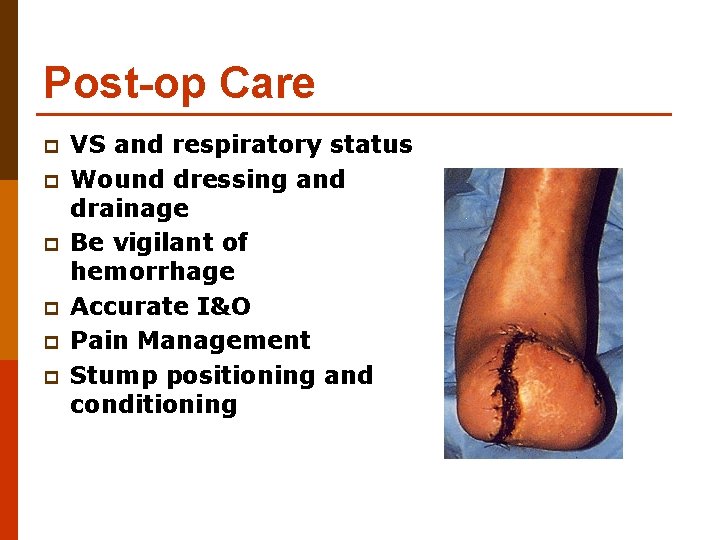
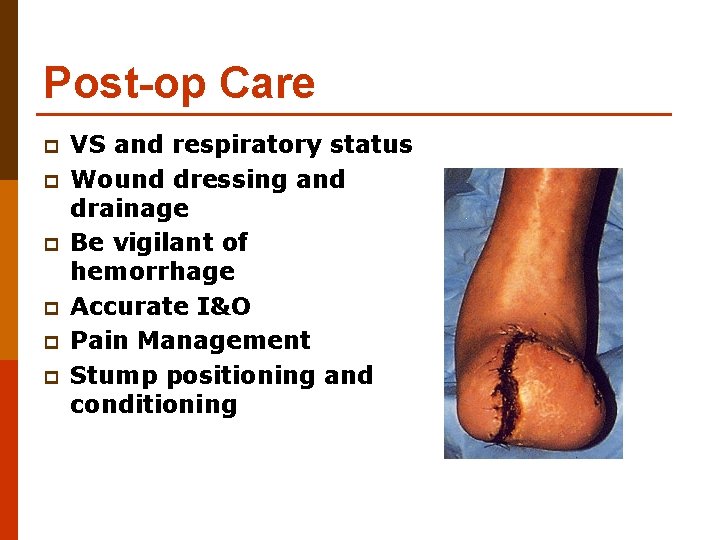
Post-op Care p p p VS and respiratory status Wound dressing and drainage Be vigilant of hemorrhage Accurate I&O Pain Management Stump positioning and conditioning
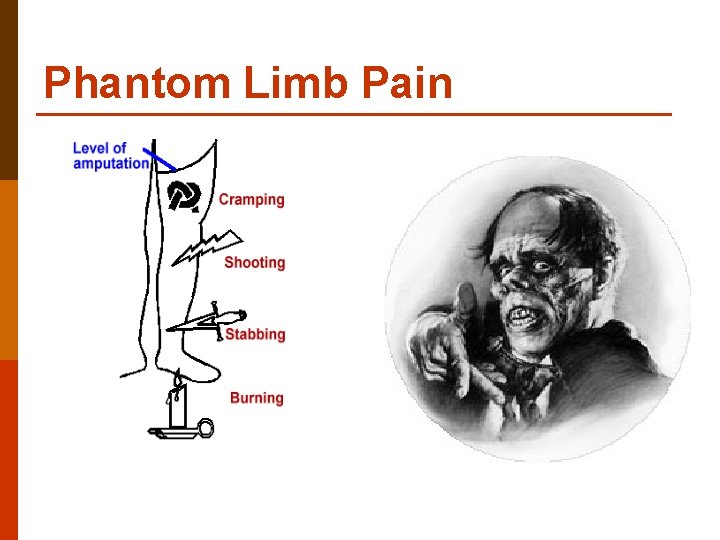
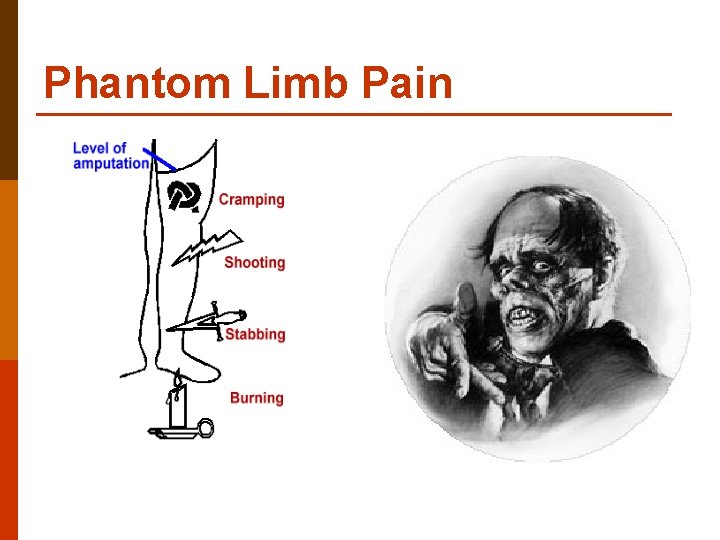
Phantom Limb Pain

Crutch Walking
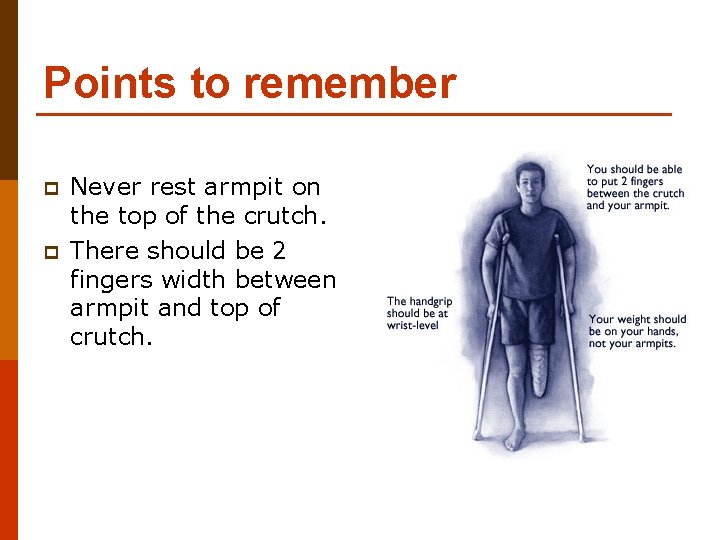
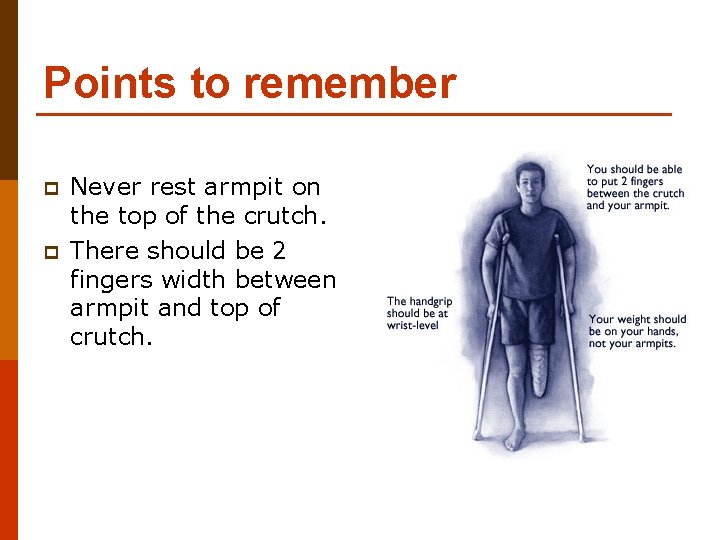
Points to remember p p Never rest armpit on the top of the crutch. There should be 2 fingers width between armpit and top of crutch.
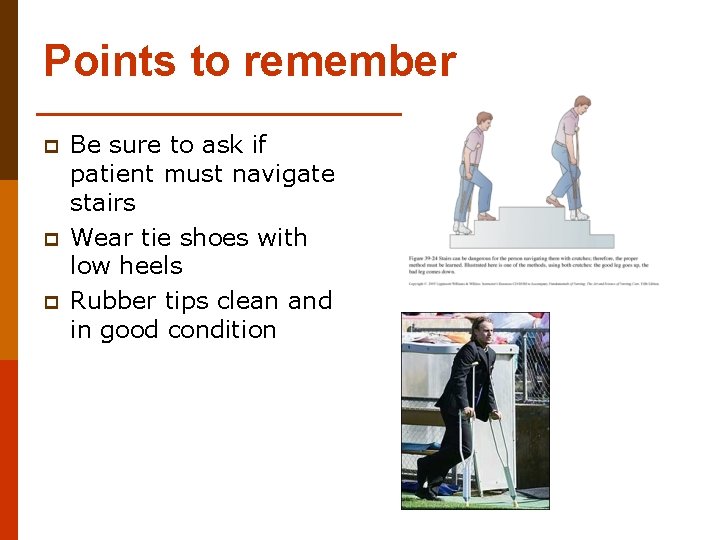
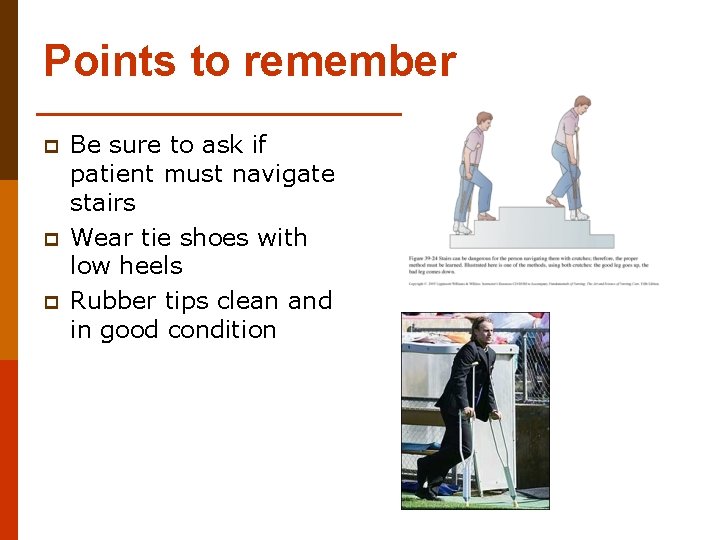
Points to remember p p p Be sure to ask if patient must navigate stairs Wear tie shoes with low heels Rubber tips clean and in good condition

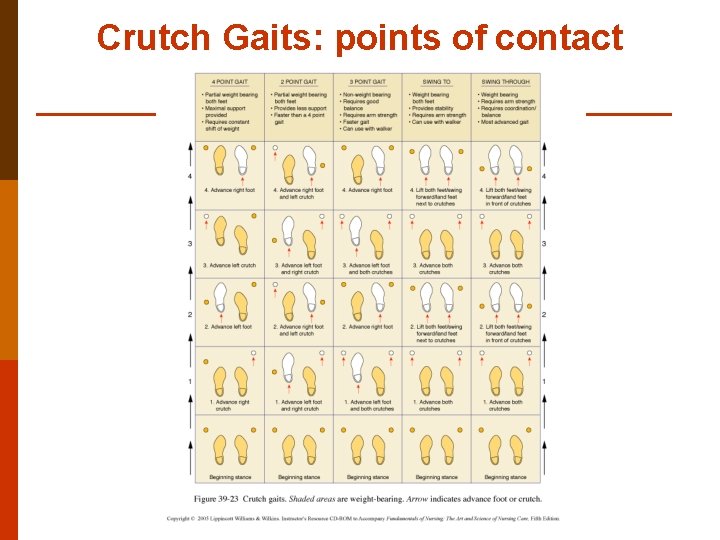
Crutch Gaits: points of contact 2 point p 3 point p 4 point p Swing to p Swing through p
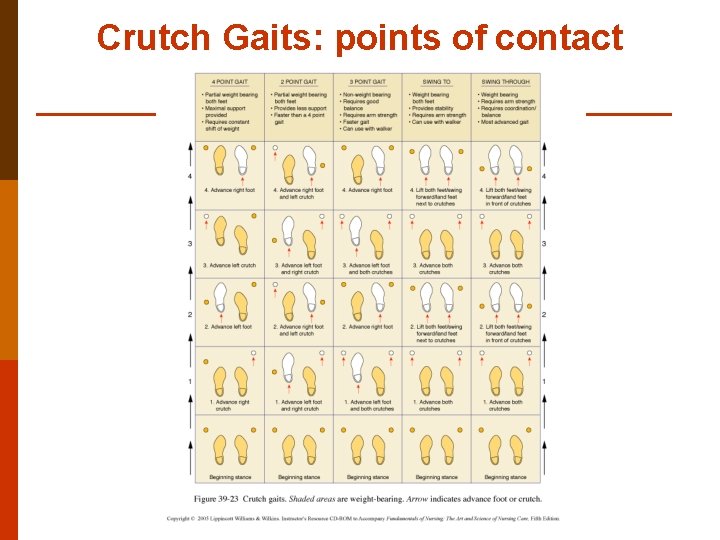
Crutch Gaits: points of contact
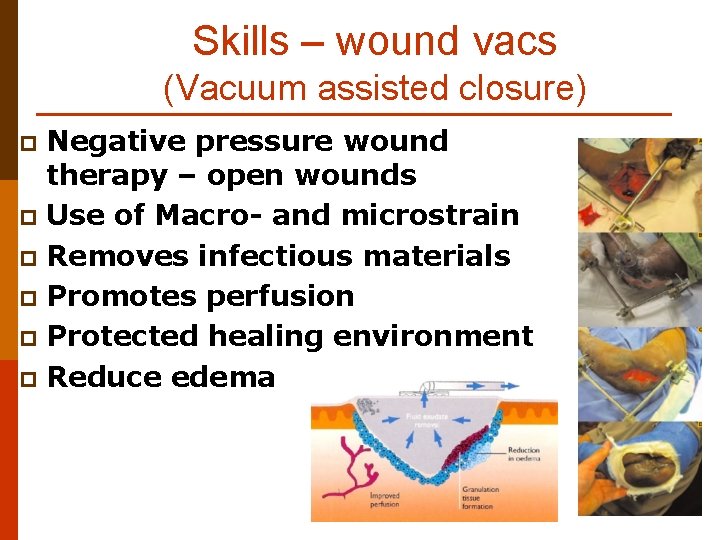
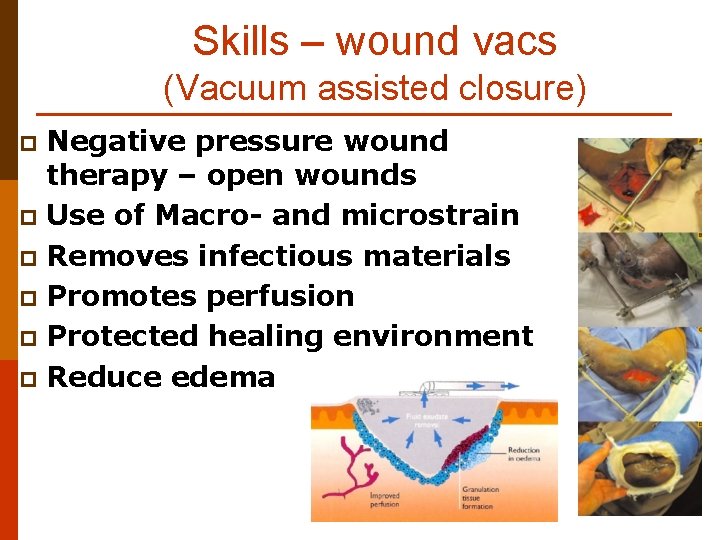
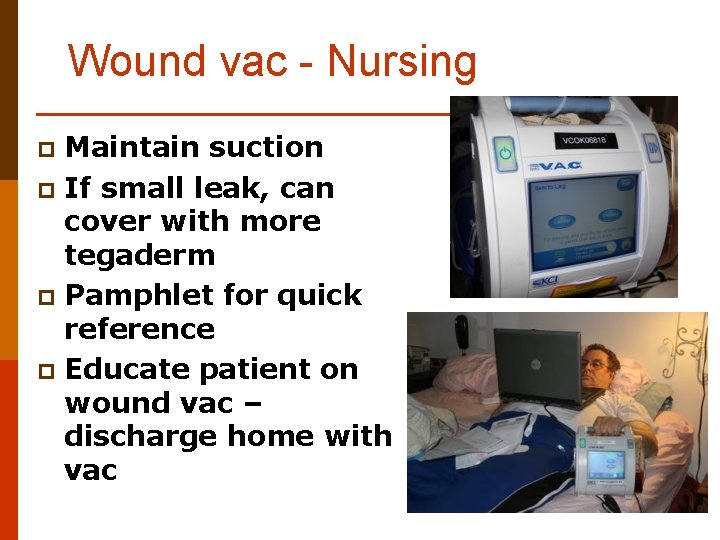
Skills – wound vacs (Vacuum assisted closure) Negative pressure wound therapy – open wounds p Use of Macro- and microstrain p Removes infectious materials p Promotes perfusion p Protected healing environment p Reduce edema p
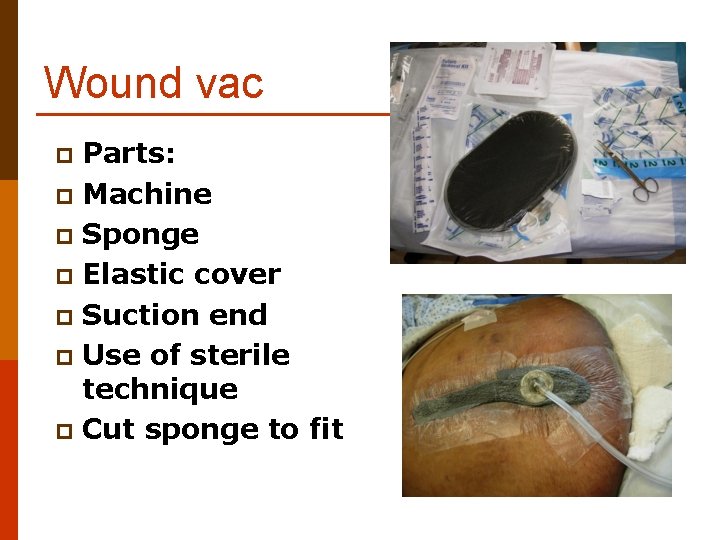
Wound vac Parts: p Machine p Sponge p Elastic cover p Suction end p Use of sterile technique p Cut sponge to fit p
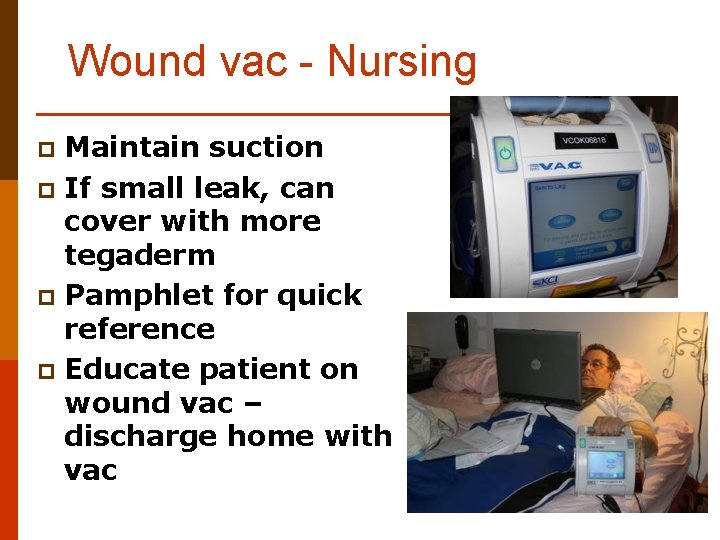
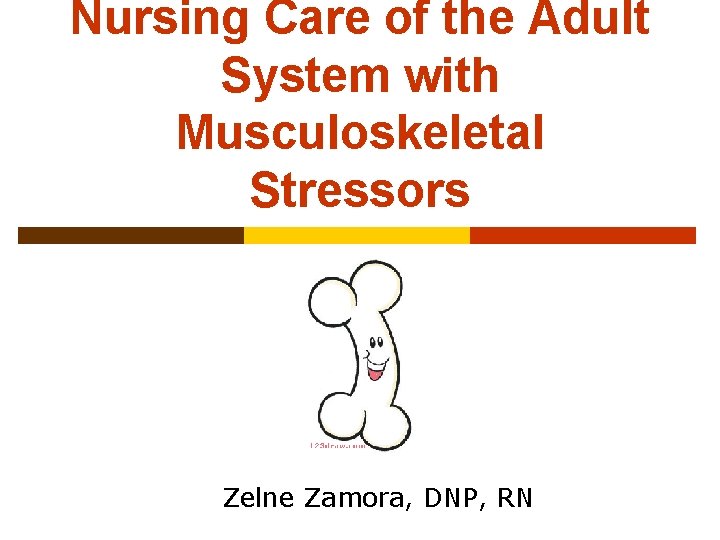
Wound vac - Nursing Maintain suction p If small leak, can cover with more tegaderm p Pamphlet for quick reference p Educate patient on wound vac – discharge home with vac p