Nursing Care of Children with altered Genitourinary Function







- Slides: 36
Nursing Care of Children with altered Genitourinary Function (2) Dr. Manal Kloub
Outline • Nephrotic Syndrome • Renal Failure 1. Acute 2. Chronic

Nephrotic Syndrome ( Nephrosis ) v It is a clinical state that includes massive v 1. 2. Proteinuria, Hypoalbuminemia , hyperlipidemia and edema The disorder can occur as A primary disease known as idiopathic Nephrosis. Childhood Nephrosis, Minimal change nephritic Syndrome (MCNS). A secondary disorder that occur as a clinical manifestation after or in association with Glomerular damage
Nephrotic Syndrome 3. Congenital form inherited as an autosomal recessive disorder. • Nephrotic Syndrome occur in children between 2 -7 years of age ; it is rare in children younger than 6 months of age • Patients with (MCNS) are twice as likely to be male.
Pathophysiology • It is not understood • There may be a metabolic , biochemical, physiochemical or immune- mediated disturbances that cause the basement membrane of the glomeruli to become increasingly permeable to protein
Pathophysiology • Renal Glomerular damage -----Proteinuria ( massive) ---- hypoprotienemia • Hypoprotienemia– increased hepatic synthesis of protein and lipids --hyperlipidemia • hypoprotienemia – deceased oncotic pressure 1 - edema 2 - hypovolemia
Pathophysiology 1. Decreased renal blood flow --- Renin 2. release ---- vasoconstriction increased secretion of ADH and aldosterone --- Na+ and water reabsorption --- Edema
Assessment Clinical Manifestation • Weight gain • Periorbital edema especially in morning from head dependent position • abdominal cavity edema ( ascities ) • Scrotal edema extremely marked • anorexia , vomiting • Diarrhea caused by intestinal edema and poor absorption by edematous membrane • Pleural effusion • Ankle/leg swelling. • Irritability, easily fatigued , lethargic
Diagnostic Evaluation q. Blood pressure normal or slightly decreased q. Susceptibility to infections q. Urine alterations decreased volume and frothy q. Laboratory studies reveal a. Marked Proteinuria ( +3 or higher ) which almost b. q entirely albumin low serum protein concentration , reduced serum albumin significantly , elevated plasma lipids serum and platelets count may be elevated Renal biopsy if the patient dose not respond to a 4 -8 weeks courses of steroids
Management • Dietary restriction includes a low salt diet and fluid • • restriction Diuretic therapy Sometimes infusions of 25% albumin are used Acute infection are treated with appropriate antibiotics Corticosteroids are the first line of therapy for MCNS Relapse are treated with a repeated course of high dose steroid therapy MCNS episodes often happen in conjunction with viral or bacterial infection Relapses in children may continue over many years
Complications • Infection peritonitis, cellulites and pneumonia • Circulatory insufficiency secondary to hypovolemia • Thromboembolism
Prognosis • The prognosis for ultimate recovery in most cases is good • It is self limited disease • In children who respond to steroid therapy the tendency to relapse decreases with time
Nursing care • • • Daily monitoring of intake and out put Weight the child daily Examine urine daily for albumin Measure abdominal girth daily Assessment of edema (pitting, color& texture of skin Monitor V/S to detect any signs of shock or infections( respiratory )
Nursing care • Formulate a nutritionally adequate and • • attractive diet Adjust activities according to children tolerance level Edema and fluids restricted during the edema phase and allowed when edema subsides. • Family support and home care ( urine examination , medication taken , prevent infection)
Renal Failure (RF) • RF Is the inability of the kidney to excrete waste material, concentrate urine and conserve electrolytes. • The disorder can be 1. Acute 2. Chronic Terms used in RF • Azotemia : a accumulation of nitrogenous waste products within the blood • Uremia: retention of notoriousness products produce toxic symptoms often involve other body systems • and its a life threatening

Acute Versus Chronic • Acute – – sudden onset rapid reduction in urine output Usually reversible Tubular cell death and regeneration – – – Progressive Not reversible Nephron loss • Chronic • 75% of function can be lost before its noticeable
Acute Renal Failure • Most often occurs because of sudden body insult such as • • • 1. 2. 3. sever dehydration Resulted in Oliguria Azotemia Acidosis Diverse electrolytes disturbance Causes Prerenal Intrinsic renal Post renal
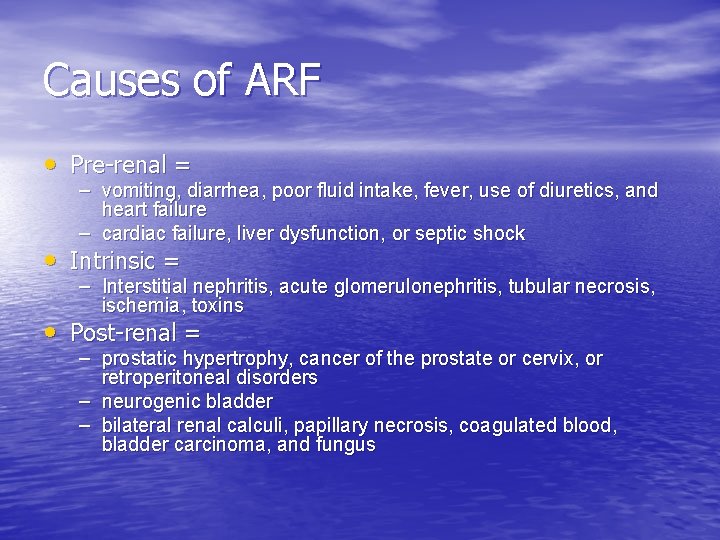
Causes of ARF • Pre-renal = – vomiting, diarrhea, poor fluid intake, fever, use of diuretics, and heart failure – cardiac failure, liver dysfunction, or septic shock • Intrinsic = – Interstitial nephritis, acute glomerulonephritis, tubular necrosis, ischemia, toxins • Post-renal = – prostatic hypertrophy, cancer of the prostate or cervix, or retroperitoneal disorders – neurogenic bladder – bilateral renal calculi, papillary necrosis, coagulated blood, bladder carcinoma, and fungus

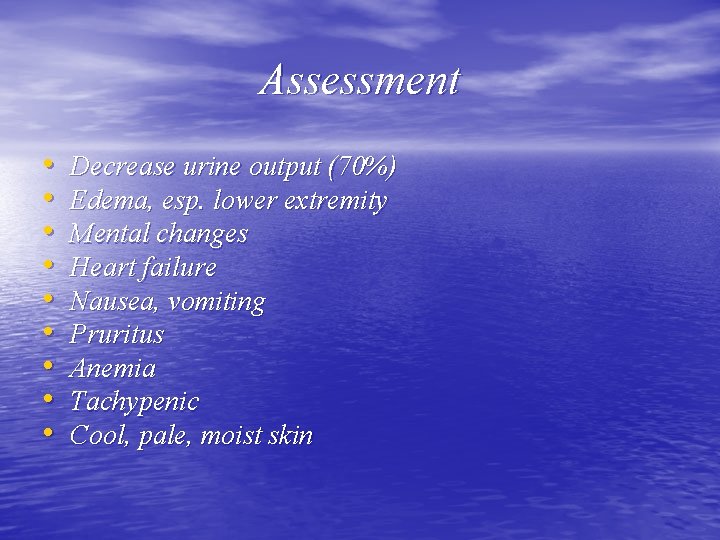
Assessment • • • Decrease urine output (70%) Edema, esp. lower extremity Mental changes Heart failure Nausea, vomiting Pruritus Anemia Tachypenic Cool, pale, moist skin
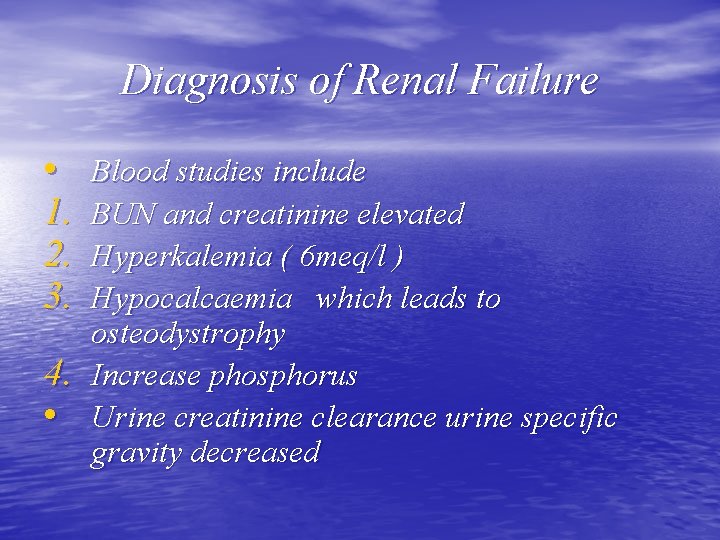
Diagnosis of Renal Failure • 1. 2. 3. 4. • Blood studies include BUN and creatinine elevated Hyperkalemia ( 6 meq/l ) Hypocalcaemia which leads to osteodystrophy Increase phosphorus Urine creatinine clearance urine specific gravity decreased
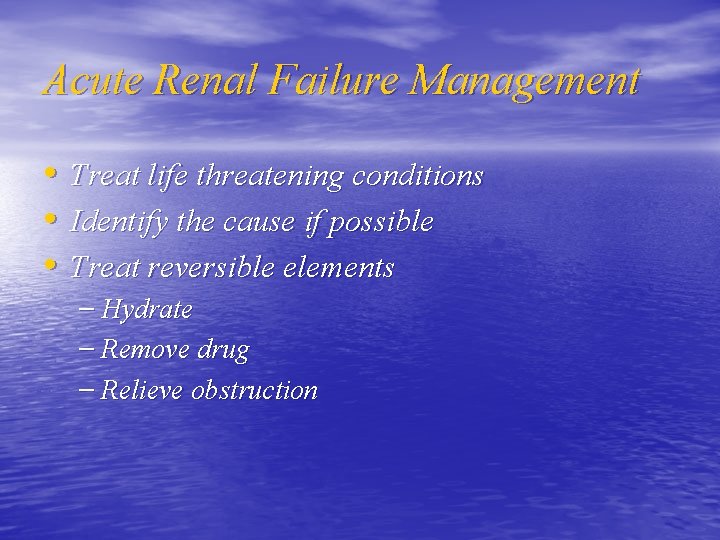
Acute Renal Failure Management • Treat life threatening conditions • Identify the cause if possible • Treat reversible elements – Hydrate – Remove drug – Relieve obstruction


Hyperkalemia Symptoms • • • Weakness Lethargy Muscle cramps Paresthesias Lowered blood pressure Dysrhythmias


Hyperkalemia Treatment • • • Calcium gluconate (carbonate) Sodium Bicarbonate Insulin/glucose Kayexalate Lasix Hemodialysis
Diet • • • low in protein, potassium , sodium Increase Carbohydrates Restrict fluids Daily weight Accurate recording for intake & out put
Chronic Renal Failure • It begins when the diseased kidneys can no • longer maintain the normal chemical structure of body fluids under normal conditions Glomerular filtration rate decreased below 10 to 15 % of normal.
Chronic Renal Failure Causes • The most common causes before 5 years are congenital renal and urinary tract malformation such as renal hypoplasia, obstructive uropathy & Vesicoureteral reflux • Glomerular and hereditary diseases in children ages 5 -15 years • Chronic pyelonephritis , chronic glomerulonephritis • Systematic diseases such as (Lupus erythematosus, anaphylactic purpura) • Polycystic kidney disease • Renal vascular disorder such as hemolytic Uremic syndrome (HUS) vascular thrombosis
CRF Symptoms • • Malaise Weakness Fatigue Neuropathy CHF Anorexia Nausea Vomiting • • • Seizure Constipation Peptic ulceration Anemia Pruritus Abnormal hemostasis
Treatment 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. low protein, phos, & potassium diet Daily fluid intake restriction Low sodium intake such as ( chips) Calcium supplement anti- hypertension blood transfusion Human erythropoietin Growth hormone may be given in some children Dialysis kidney transplant
Dialysis • • • Patients with CRF eventually require dialysis Diffuse harmful waste out of body Control BP Keep safe level of chemicals in body 2 types – Hemodialysis – Peritoneal dialysis
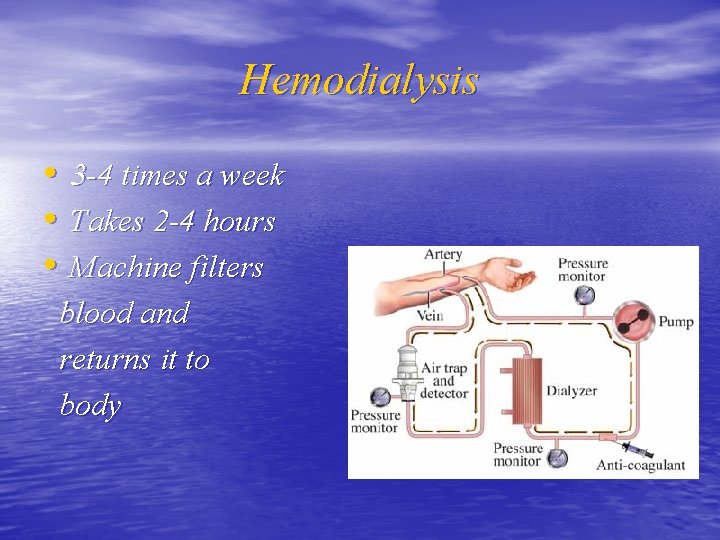
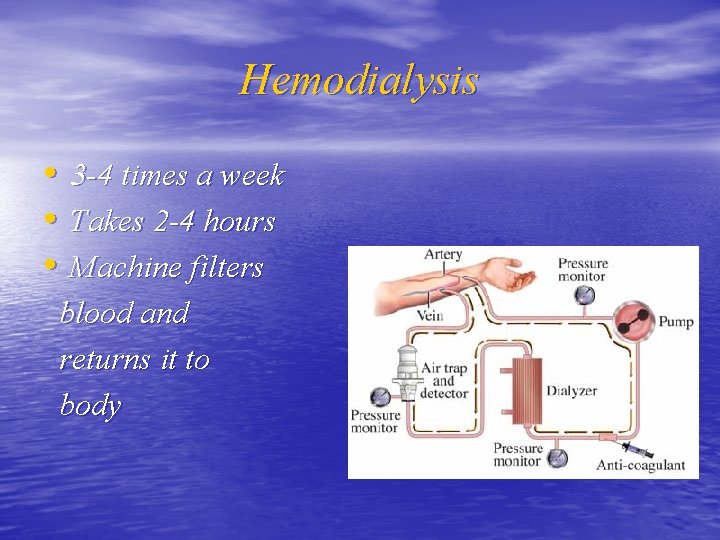
Hemodialysis • 3 -4 times a week • Takes 2 -4 hours • Machine filters blood and returns it to body
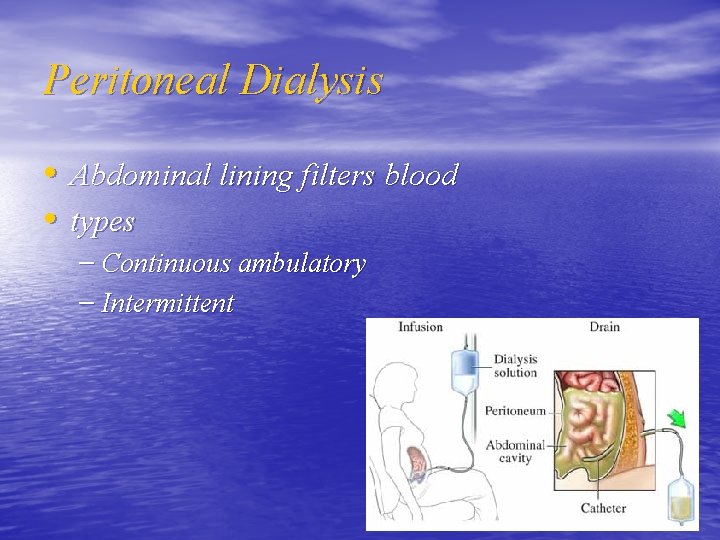
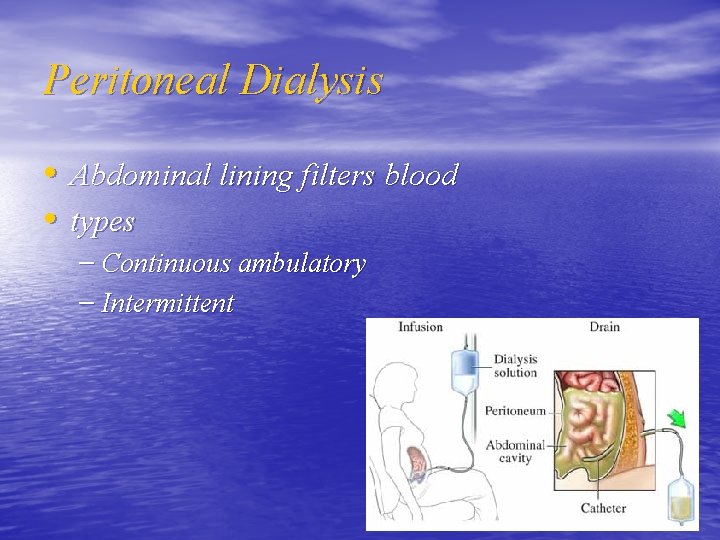
Peritoneal Dialysis • Abdominal lining filters blood • types – Continuous ambulatory – Intermittent
Thank you
 Nursing diagnosis for undescended testis
Nursing diagnosis for undescended testis Chapter 29 the child with a genitourinary condition
Chapter 29 the child with a genitourinary condition Chapter 29 the child with a genitourinary condition
Chapter 29 the child with a genitourinary condition Genitourinary & stds
Genitourinary & stds Male genitourinary anatomy
Male genitourinary anatomy Ocd nursing care plan
Ocd nursing care plan Nursing management of patient with cataract
Nursing management of patient with cataract Primary secondary tertiary health care definition
Primary secondary tertiary health care definition Safeguarding children care certificate
Safeguarding children care certificate Nj children's system of care
Nj children's system of care Care and protection of children act
Care and protection of children act Altered state of consciousness psychology
Altered state of consciousness psychology An altered state of consciousness
An altered state of consciousness Modular enteral formula example
Modular enteral formula example Mechanically altered diet
Mechanically altered diet Altered cognition in older adults is commonly attributed to
Altered cognition in older adults is commonly attributed to Sleep theories ap psychology
Sleep theories ap psychology Altered state of consciousness psychology
Altered state of consciousness psychology Altered state of consciousness psychology
Altered state of consciousness psychology Altered cellular and tissue biology
Altered cellular and tissue biology Corrected cast technique
Corrected cast technique Crash course states of consciousness
Crash course states of consciousness Is hypnosis an altered state of consciousness
Is hypnosis an altered state of consciousness Can fingerprints be altered or disguised
Can fingerprints be altered or disguised Color shades
Color shades How fossils are formed
How fossils are formed Lesson quiz 7-1 altered states of consciousness
Lesson quiz 7-1 altered states of consciousness Altered state of conciousness
Altered state of conciousness Sex altered state of consciousness
Sex altered state of consciousness Composition of alginate impression material
Composition of alginate impression material Dinopoopicus
Dinopoopicus Support for distal extension rpd
Support for distal extension rpd Altered skin integrity
Altered skin integrity Altered states game
Altered states game Jounalizing
Jounalizing Chapter 7 altered states of consciousness
Chapter 7 altered states of consciousness Chapter 7 altered states of consciousness
Chapter 7 altered states of consciousness