Nursing Care Interventions for the Client with Disorders
- Slides: 19
Nursing Care & Interventions for the Client with Disorders of the Thyroid Gland Keith Rischer RN, MA, CEN 1 1
Today’s Objectives… Ø Ø Ø Compare and contrast pathophysiology & manifestations of thyroid/parathyroid gland dysfunction. Identify, nursing priorities, and client education associated with thyroid/parathyroid gland dysfunction. Interpret abnormal laboratory test indicators of thyroid/parathyroid gland dysfunction. Analyze assessment to determine nursing diagnoses and formulate a plan of care for clients with thyroid/parathyroid gland dysfunction. Describe the mechanism of action, side effects and nursing interventions of pharmological management with thyroid/parathyroid gland dysfunction. 2
Thyroid Glands: Patho Ø Thyroid gland • • Ø Thyroxin (T 3) Triiodothyronine (T 4) Functions • • • Controls metabolism of all cells Regulate protein, CHO, fat metabolism Exert chronotropic/inotropic cardiac effects 3
Hyperthyroidism: Causes Ø Ø Ø Graves disease Goiter T 3 Thyrotoxicosis Thyroid cancer Tumors in body 4 4
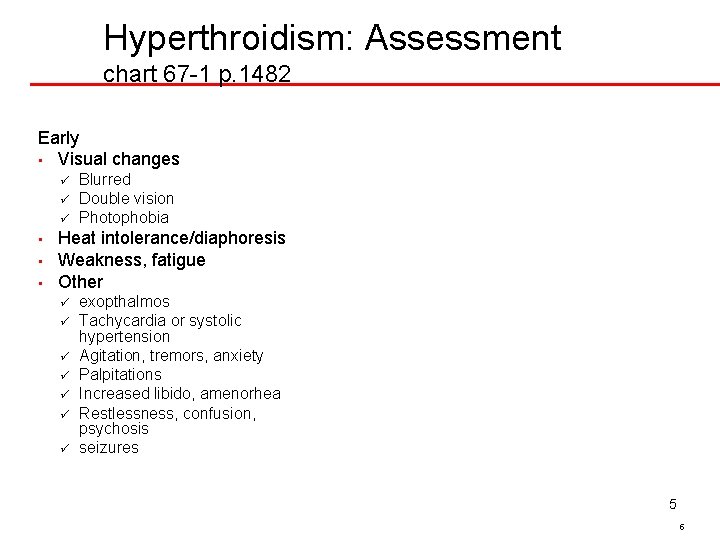
Hyperthroidism: Assessment chart 67 -1 p. 1482 Early • Visual changes ü ü ü • • • Blurred Double vision Photophobia Heat intolerance/diaphoresis Weakness, fatigue Other ü ü ü ü exopthalmos Tachycardia or systolic hypertension Agitation, tremors, anxiety Palpitations Increased libido, amenorhea Restlessness, confusion, psychosis seizures 5 5
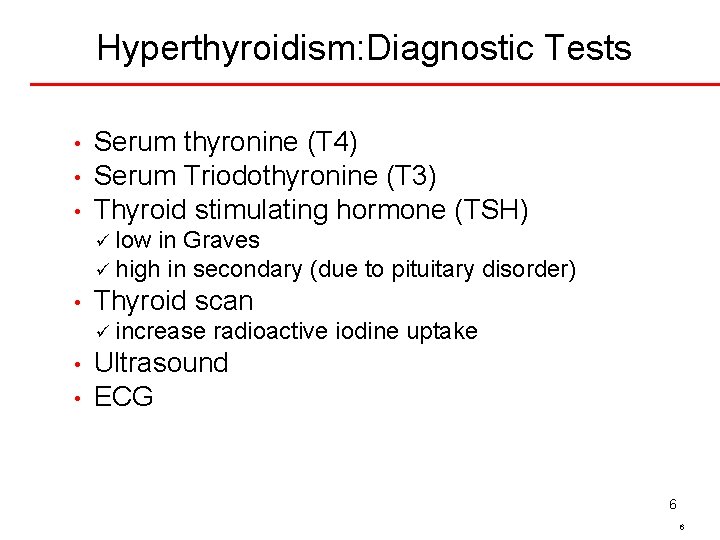
Hyperthyroidism: Diagnostic Tests • • • Serum thyronine (T 4) Serum Triodothyronine (T 3) Thyroid stimulating hormone (TSH) ü low in Graves ü high in secondary (due to pituitary disorder) • Thyroid scan ü increase • • radioactive iodine uptake Ultrasound ECG 6 6
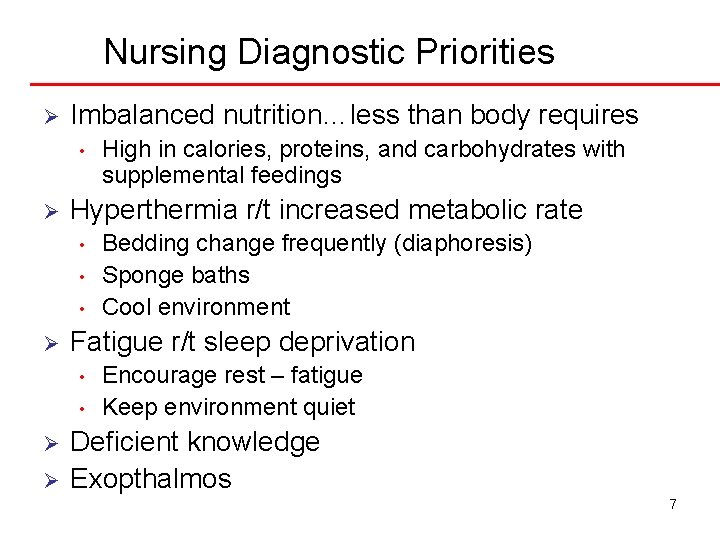
Nursing Diagnostic Priorities Ø Imbalanced nutrition…less than body requires • Ø Hyperthermia r/t increased metabolic rate • • • Ø Bedding change frequently (diaphoresis) Sponge baths Cool environment Fatigue r/t sleep deprivation • Ø High in calories, proteins, and carbohydrates with supplemental feedings Encourage rest – fatigue Keep environment quiet Deficient knowledge Exopthalmos 7
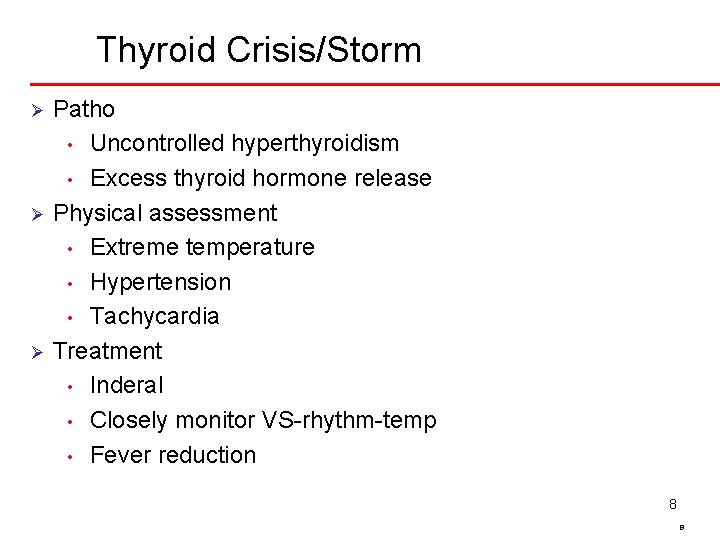
Thyroid Crisis/Storm Patho • Uncontrolled hyperthyroidism • Excess thyroid hormone release Ø Physical assessment • Extreme temperature • Hypertension • Tachycardia Ø Treatment • Inderal • Closely monitor VS-rhythm-temp • Fever reduction Ø 8 8
Hyperthyroidism: Medical Management Ø Antithyroid medications • Propylthiouracal (PTU) ü • block synthesis of thyroid hormone Iodine (SSKI) ü reduce vascularity of thyroid gland Beta blockers Ø Radioactive iodine therapy • To ablate thyroid to make the pt become hypothyroid; ü Taken orally ü Relief of symptoms may take 6 -8 weeks • 9 9
Hyperthyroidism: Surgical Management ØPreop care ØPost op care • ABC’s ü Humidified O 2 • Support of neck with movement & coughing • Semi-Fowlers position • Incisional care ØPostoperative complications • Hemorrhage • Respiratory ü ü Stridor Tracheotomy equipment readily available • Laryngeal ü distress nerve damage Hoarseness/weak voice 10 10
Hypothyroidism Ø Patho • • Decreased metabolism Myxedema coma ü Cellular edema – Generalized NP edema…eyes, hands, feet, tongue Ø Causes • • Thyroid surgery/radioactive iodine treatment Iodide deficiency 11 11
Hypothyroidism: Assessment Ø Change • chart 67 -5 p. 1488 in sleep habits more lethargic Ø Decreased libido Ø Generalized weakness Ø Muscles aches Ø Cold intolerance Ø Constipation 12 12
Myxedema Coma Ø Ø Ø Those at highest risk • Surgery • Chemo • Withdrawal thyroid meds Assessment • Respiratory failure • Hypotension • Labs Emergency care • ABC’s • Replace fluids • Administering meds. Steroids, IV glucose, Levothyroxine sodium (thyroid) • Monitor Temp. & BP frequently 13 13
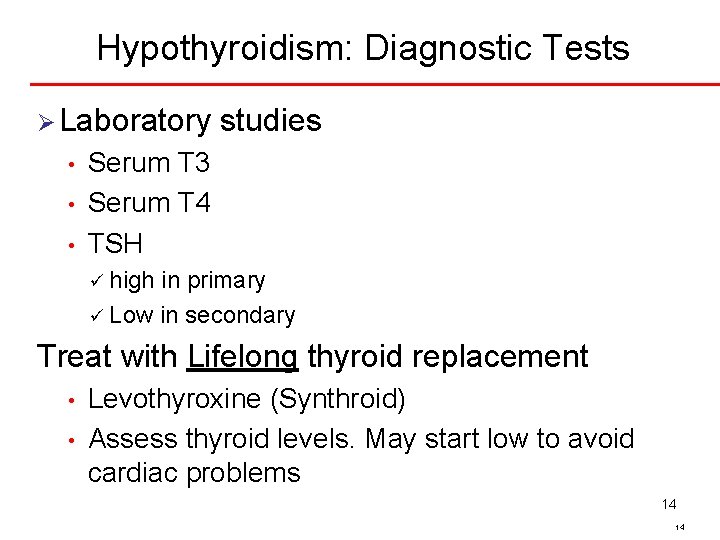
Hypothyroidism: Diagnostic Tests Ø Laboratory • • • studies Serum T 3 Serum T 4 TSH ü high in primary ü Low in secondary Treat with Lifelong thyroid replacement • • Levothyroxine (Synthroid) Assess thyroid levels. May start low to avoid cardiac problems 14 14
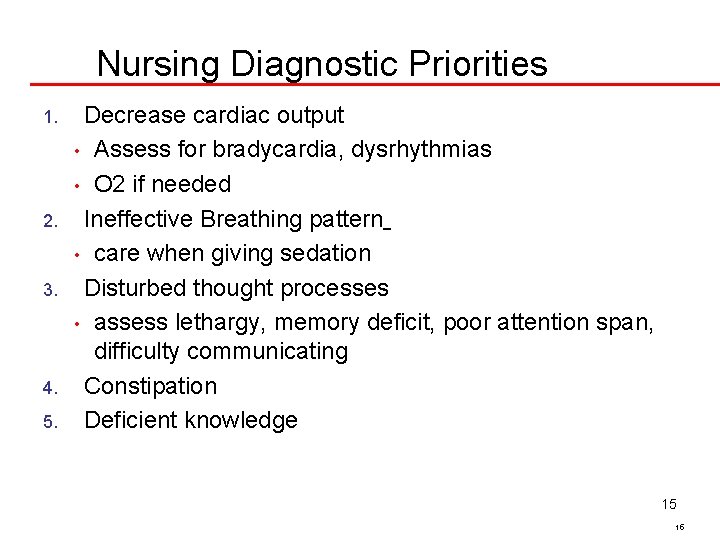
Nursing Diagnostic Priorities 1. 2. 3. 4. 5. Decrease cardiac output • Assess for bradycardia, dysrhythmias • O 2 if needed Ineffective Breathing pattern • care when giving sedation Disturbed thought processes • assess lethargy, memory deficit, poor attention span, difficulty communicating Constipation Deficient knowledge 15 15
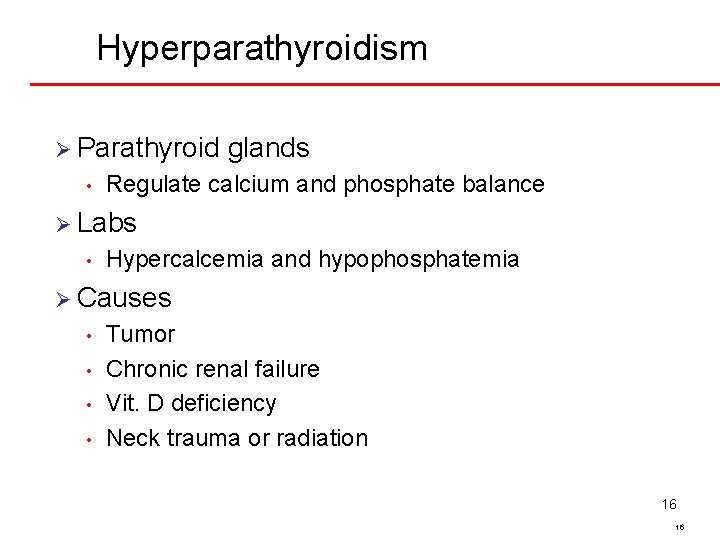
Hyperparathyroidism Ø Parathyroid • glands Regulate calcium and phosphate balance Ø Labs • Hypercalcemia and hypophosphatemia Ø Causes • • Tumor Chronic renal failure Vit. D deficiency Neck trauma or radiation 16 16
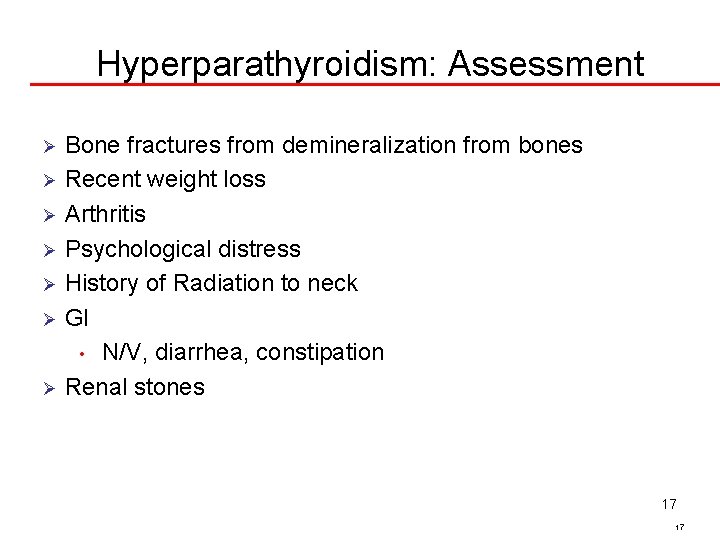
Hyperparathyroidism: Assessment Bone fractures from demineralization from bones Ø Recent weight loss Ø Arthritis Ø Psychological distress Ø History of Radiation to neck Ø GI • N/V, diarrhea, constipation Ø Renal stones Ø 17 17
Hyperparathyroidism: Medical Management Diet • restrict Calcium…esp milk products Ø Medications • Lasix ü Increased excretion of calcium • Phosphates ü Inhibits bone resorption and interferes with calcium absorption • Calcitonin ü Use to decrease skeletal calcium release Ø Hyperparathyroidectomy • Same Ø 18 18
Hyperparathyroidism: Nursing Interventions Ø Hydration • • • (strict I & O) IV saline in large amounts and lasix to excrete calcium Assess for Congestive heart failure R/T fluid overload Cardiac monitoring Ø Serum Calcium levels need to be done frequently Ø Educate client to report N/V, palpations, numbness Ø Care to reduce fractures – lift gently Ø • Ø Ambulation helps prevent demineralization Observe for renal calculi 19 19