Nursing Care and Interventions in Managing Chronic Renal
- Slides: 32
Nursing Care and Interventions in Managing Chronic Renal Failure Keith Rischer RN, MA, CEN 1
Todays Objectives… Ø Ø Ø Review the pathophysiology and causes of chronic renal failure (CRF). Contrast lab findings and physiologic changes associated with acute vs. chronic renal failure. Identify relevant nursing diagnosis statements and prioritize nursing care for clients with CRF including dietary modifications. Compare and contrast the following treatment modalities: peritoneal dialysis, hemodialysis, and continuous renal replacement therapies. Identify nursing care priorities with hemodialysis and peritoneal dialysis. Prioritize teaching needs of clients with CRF. 2
3
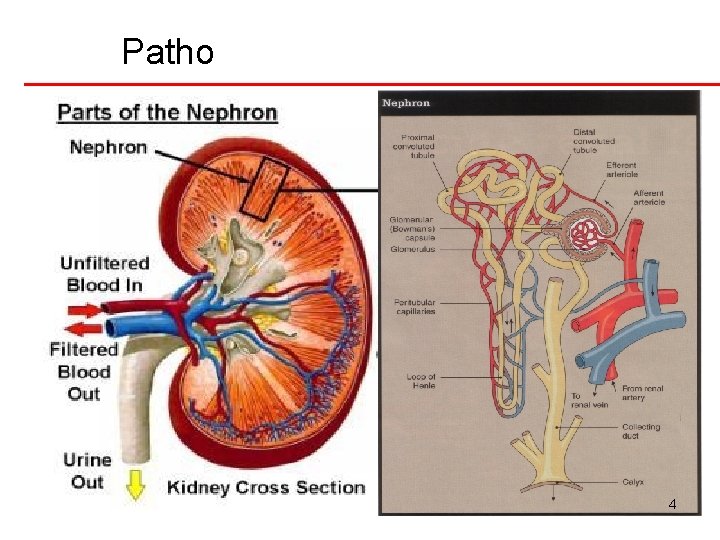
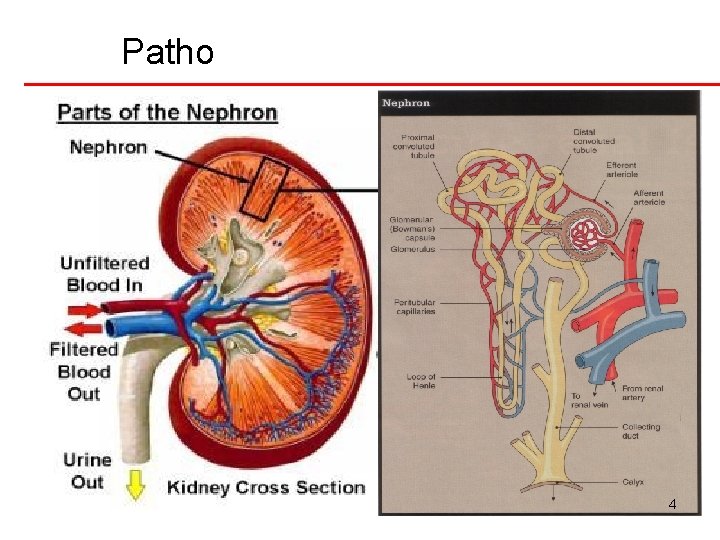
Patho 4
Patho: Chronic Renal Failure Ø Progressive, irreversible kidney injury Kidney function does not recover q Azotemia q Increase nitrogenous wastes such as BUN ü Creatinine ü q Uremia ü ü q azotemia with symptoms (chart 75 -5 p. 1739) Anorexia, N&V, fatigue, SOB Uremic syndrome (urine in the blood) Altered fluid, lyte and acid-base balance ü clinical and lab manifestations of renal failure ü More severe weakness, lethargy, confusion…coma. . death ü 5
Patho: Stages of Chronic Renal Failure Ø Diminished renal reserve q GFR ½ normal q Compensation w/healthy nephrons Ø Renal insufficiency q Nephrons destroyed…remaining adapt q BUN, creatinine, uric acid elevate q Priorities: fluid volume, diet, control of HTN, Ø End-stage renal disease q Severe fluid, acid-base imbalances q Dialysis needed or will die 6
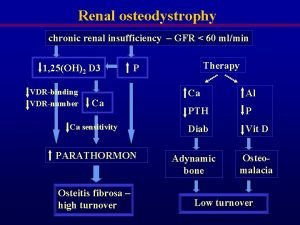
Patho: Physiologic Changes • • • Kidney • Decreased GFR • Poor H 2 O excretion Metabolic – BUN and creatinine increased Electrolytes – Sodium- later stages sodium retention – Potassium increased – EKG changes – Kayexelate • • Acid-base balance: metabolic acidosis Calcium decreased and phosphorus increased 7
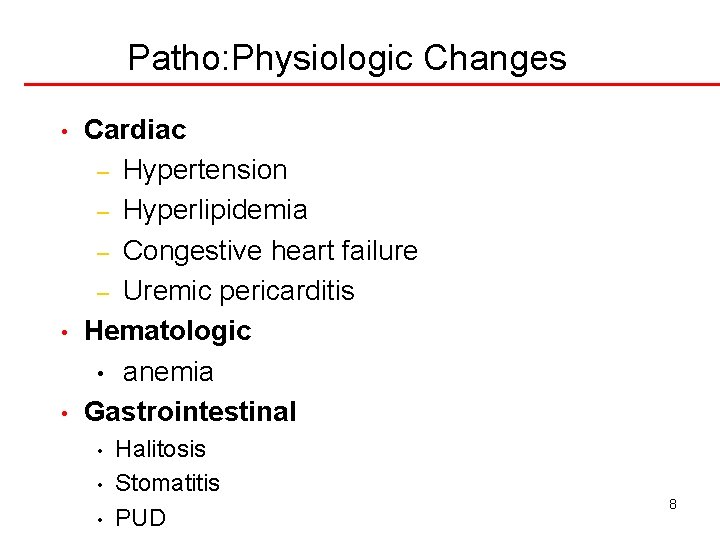
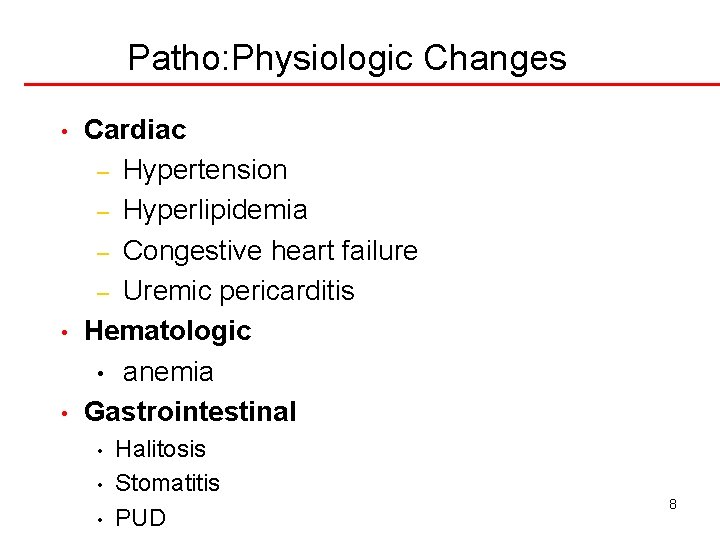
Patho: Physiologic Changes • • • Cardiac – Hypertension – Hyperlipidemia – Congestive heart failure – Uremic pericarditis Hematologic • anemia Gastrointestinal • • • Halitosis Stomatitis PUD 8
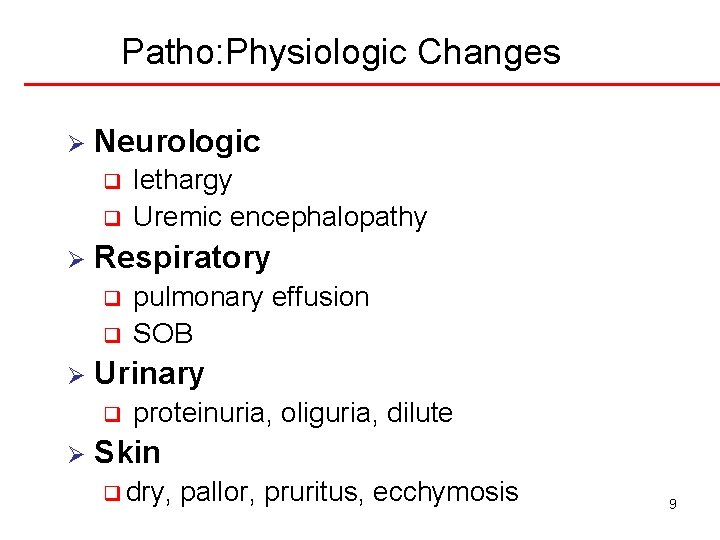
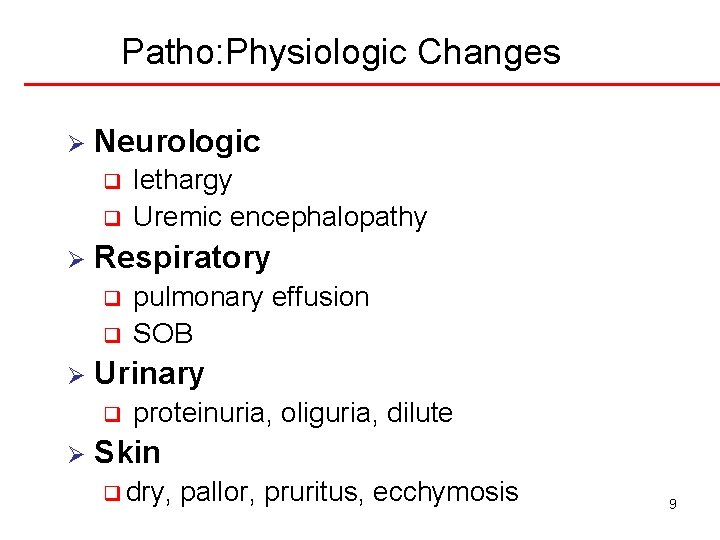
Patho: Physiologic Changes Ø Neurologic q q Ø Respiratory q q Ø pulmonary effusion SOB Urinary q Ø lethargy Uremic encephalopathy proteinuria, oliguria, dilute Skin q dry, pallor, pruritus, ecchymosis 9
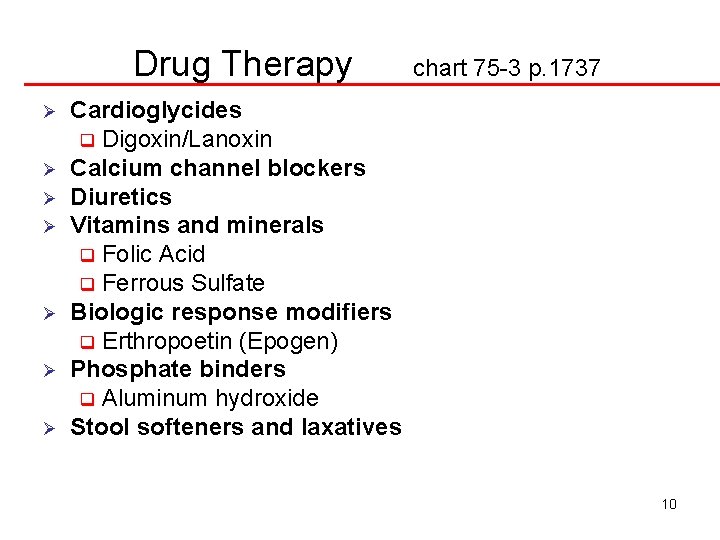
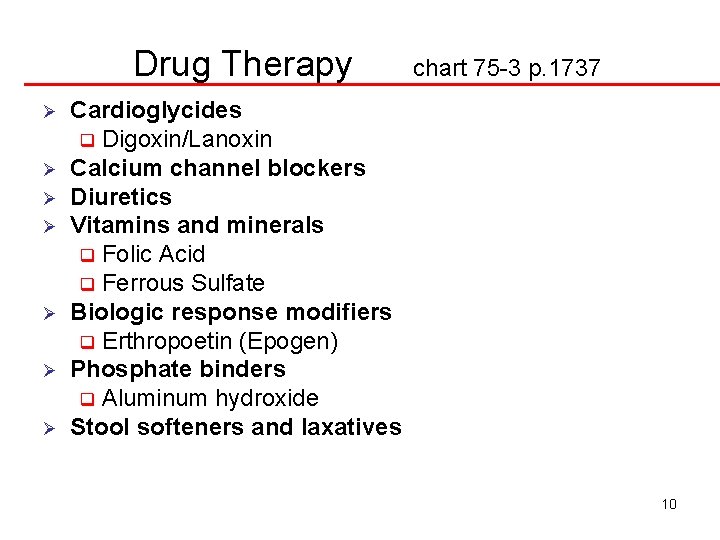
Drug Therapy Ø Ø Ø Ø chart 75 -3 p. 1737 Cardioglycides q Digoxin/Lanoxin Calcium channel blockers Diuretics Vitamins and minerals q Folic Acid q Ferrous Sulfate Biologic response modifiers q Erthropoetin (Epogen) Phosphate binders q Aluminum hydroxide Stool softeners and laxatives 10
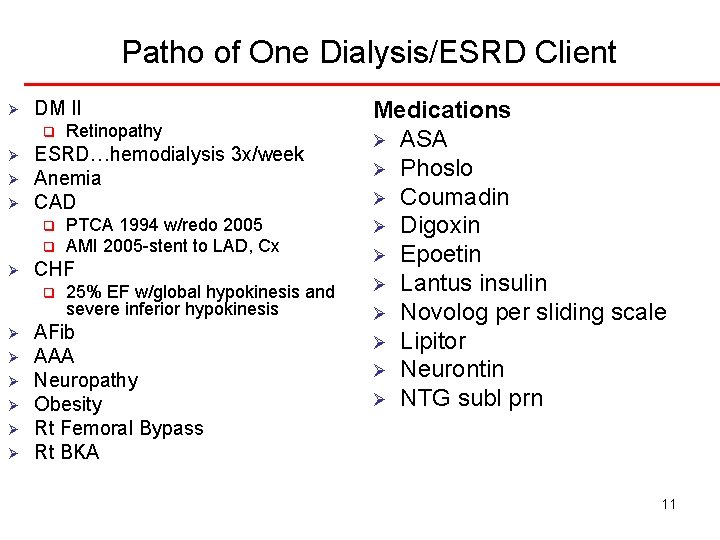
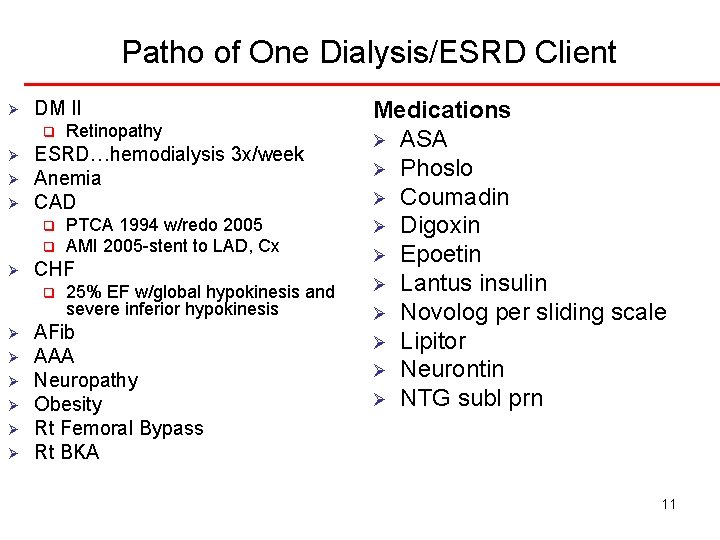
Patho of One Dialysis/ESRD Client Ø DM II q Ø Ø Ø ESRD…hemodialysis 3 x/week Anemia CAD q q Ø Ø Ø PTCA 1994 w/redo 2005 AMI 2005 -stent to LAD, Cx CHF q Ø Retinopathy 25% EF w/global hypokinesis and severe inferior hypokinesis AFib AAA Neuropathy Obesity Rt Femoral Bypass Rt BKA Medications Ø ASA Ø Phoslo Ø Coumadin Ø Digoxin Ø Epoetin Ø Lantus insulin Ø Novolog per sliding scale Ø Lipitor Ø Neurontin Ø NTG subl prn 11
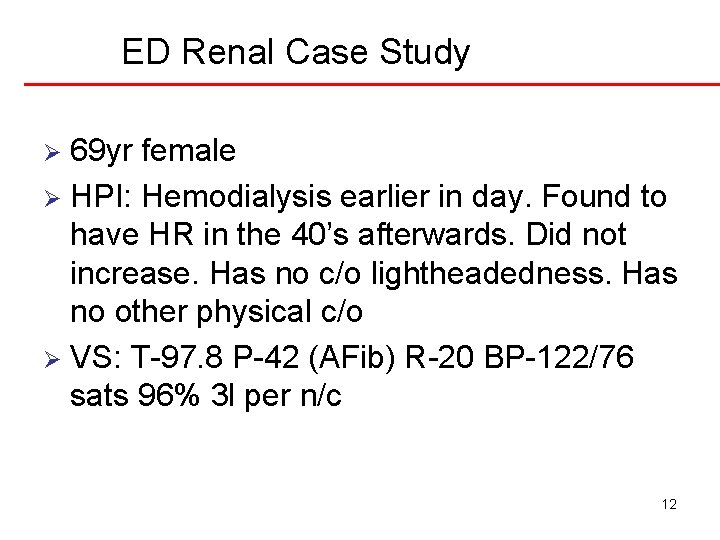
ED Renal Case Study 69 yr female Ø HPI: Hemodialysis earlier in day. Found to have HR in the 40’s afterwards. Did not increase. Has no c/o lightheadedness. Has no other physical c/o Ø VS: T-97. 8 P-42 (AFib) R-20 BP-122/76 sats 96% 3 l per n/c Ø 12
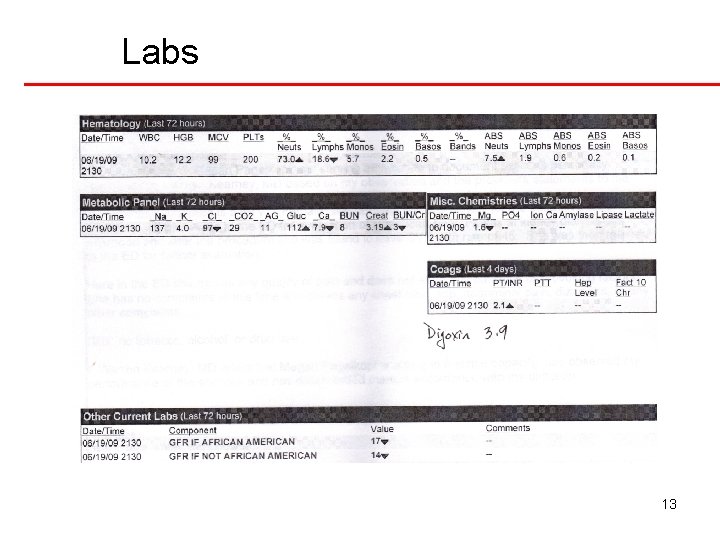
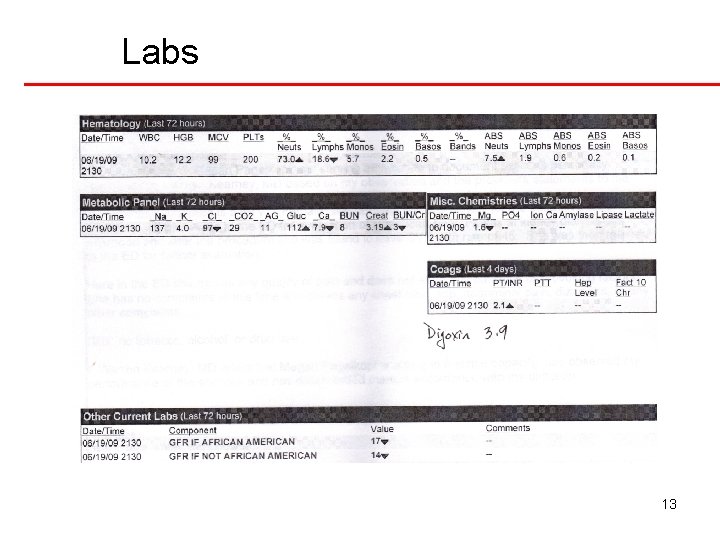
Labs 13
Excess Fluid Volume Ø Interventions: q Monitor I&O q Promote fluid balance ü Daily weights ü 1 kg=1 liter fluid q Assess for manifestations of volume excess: ü Crackles in the bases of the lungs ü Edema ü Distended neck veins q Diuretics ü Contraindicated w/ESRD 14
Decreased Cardiac Output Ø Interventions: q Control hypertension ü calcium channel blockers ü ACE inhibitors ü alpha- and beta-adrenergic blockers ü vasodilators. q Education: monitor blood pressure ü client’s weight ü Diet ü Drug regimen ü 15
Potential for Pulmonary Edema Ø Interventions: q Assess for early signs of pulmonary edema ü Restlessness/anxiety ü Tachycardia ü Tachypnea ü oxygen saturation levels ü Crackles in bases q Hypertension 16
Imbalanced Nutrition Ø Interventions: q Dietary evaluation for: ü Protein ü Fluid ü Potassium ü Sodium ü Phosphorus q Vitamin supplementation ü Iron ü Water soluable vitamins ü Calcium ü Vitamin D 17
Risk for Infection Ø Interventions: q Meticulous skin care q Preventive skin care q Inspection of vascular access site for dialysis q Monitoring of vital signs for manifestations of infection 18
Risk for Injury Ø Interventions: q Drug therapy q Education prevent fall ü Injury ü pathologic fractures ü bleeding ü toxic effects of prescribed drugs ü – Digoxin – Narcotics – Heparin or Coumadin 19
Fatigue Ø Interventions: q Assess for vitamin deficiency ü Administer q vitamin and mineral supplements anemia ü Give iron supplements as needed ü Erythropoietin therapy q Buildup of urea 20
Anxiety Ø Interventions: q Health care team involvement q Client and family education q Continuity of care q Encouragement of client to ask questions and discuss fears about the diagnosis of renal failure 21
Indications for Dialysis Uremia Ø Persistent hyperkalemia Ø Uncompensated metabolic acidosis Ø Fluid volume excess unresponsive to diuretics Ø Uremic pericarditis Ø Uremic encephalopathy Ø 22
Hemodialysis Ø Client selection q Irreversible renal failure q Expectation for rehab q Acceptance of regimen Ø Dialysis settings q Acute-hospital q Out patient centers 23
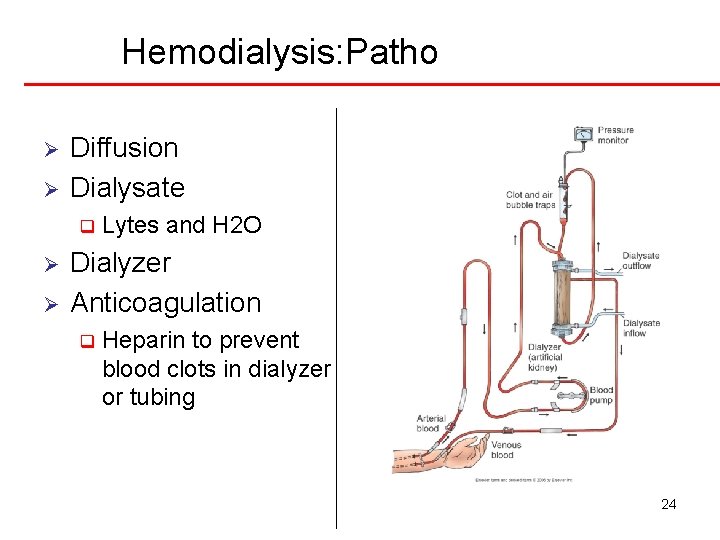
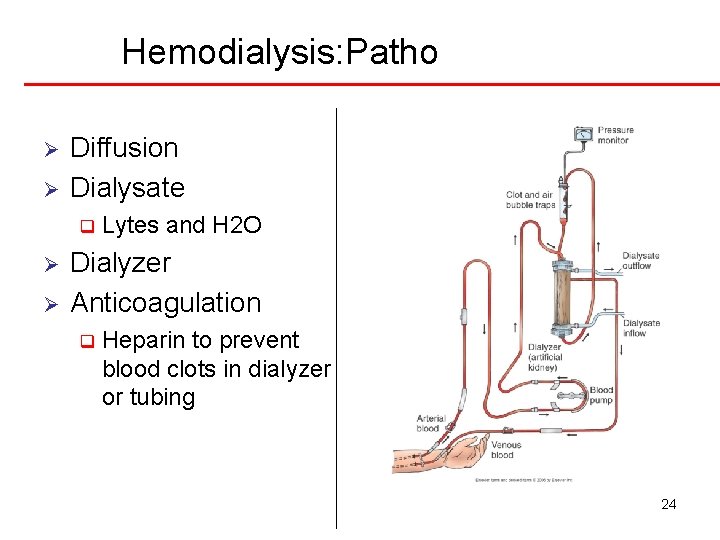
Hemodialysis: Patho Ø Ø Diffusion Dialysate q Ø Ø Lytes and H 2 O Dialyzer Anticoagulation q Heparin to prevent blood clots in dialyzer or tubing 24
Complications of Hemodialysis Dialysis disequilibrium syndrome Ø Infectious diseases Ø Hepatitis B and C infections Ø HIV exposure—poses some risk for clients undergoing dialysis Ø 25
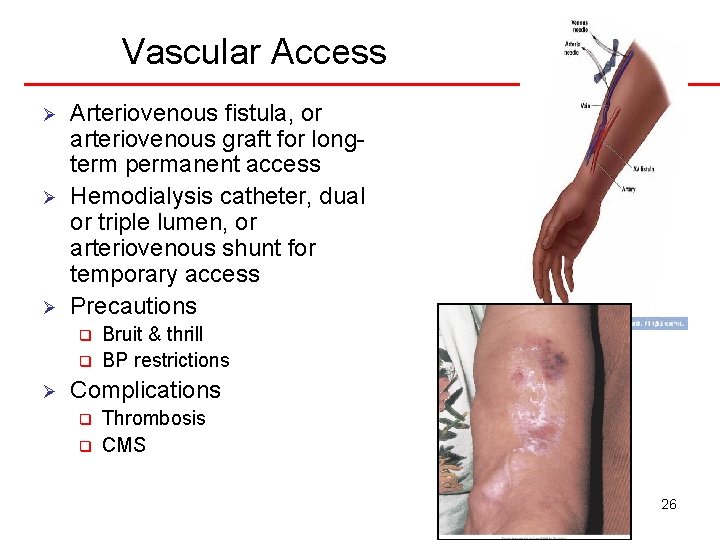
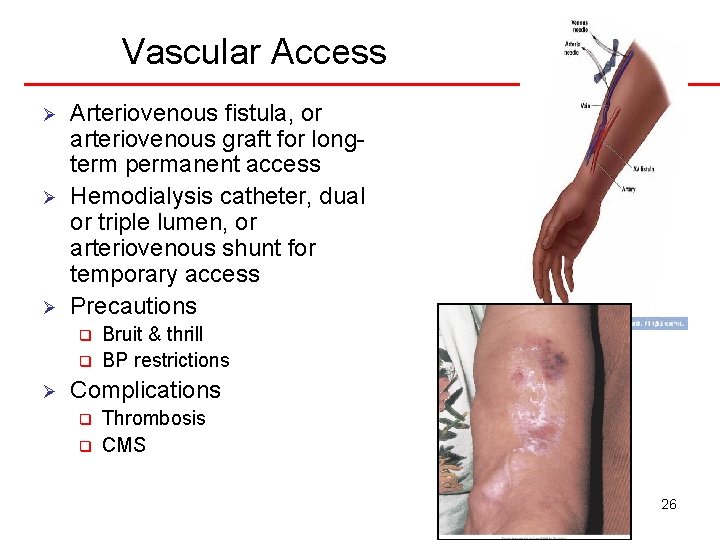
Vascular Access Ø Ø Ø Arteriovenous fistula, or arteriovenous graft for longterm permanent access Hemodialysis catheter, dual or triple lumen, or arteriovenous shunt for temporary access Precautions q q Ø Bruit & thrill BP restrictions Complications q q Thrombosis CMS 26
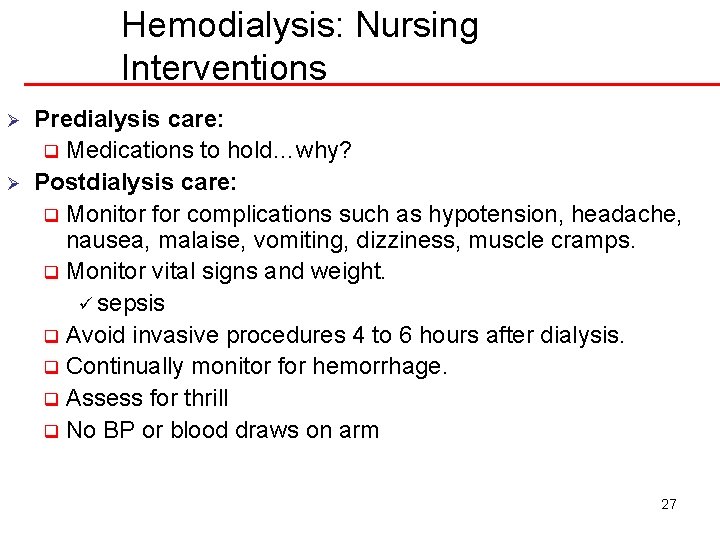
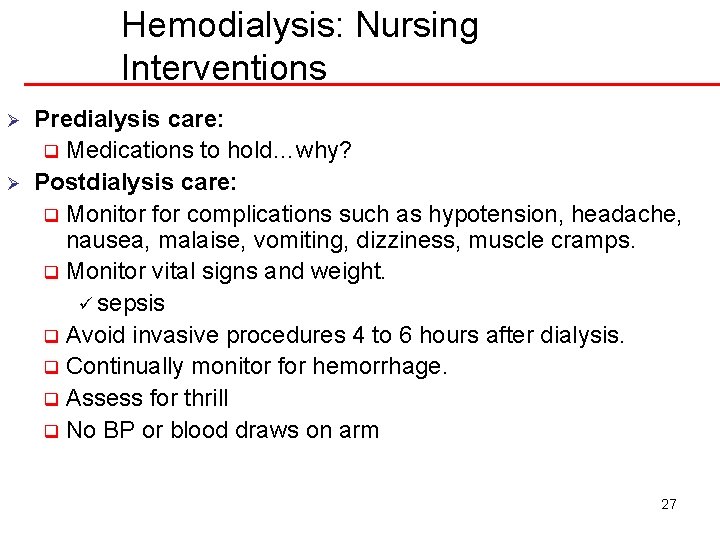
Hemodialysis: Nursing Interventions Ø Ø Predialysis care: q Medications to hold…why? Postdialysis care: q Monitor for complications such as hypotension, headache, nausea, malaise, vomiting, dizziness, muscle cramps. q Monitor vital signs and weight. ü sepsis q Avoid invasive procedures 4 to 6 hours after dialysis. q Continually monitor for hemorrhage. q Assess for thrill q No BP or blood draws on arm 27
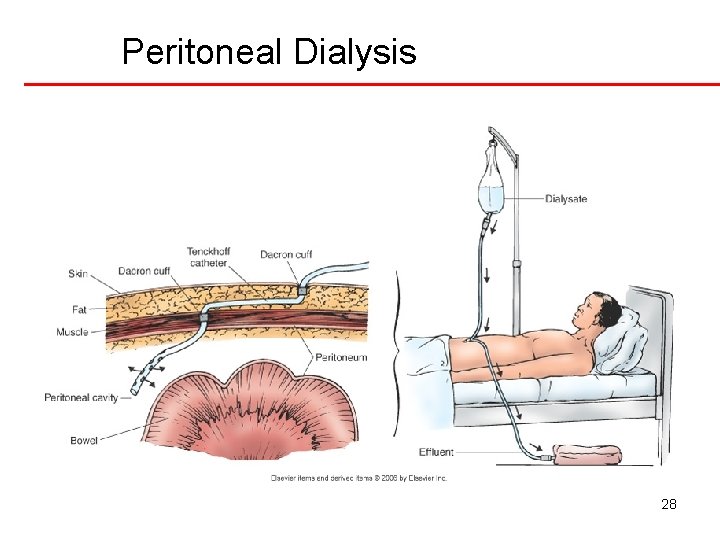
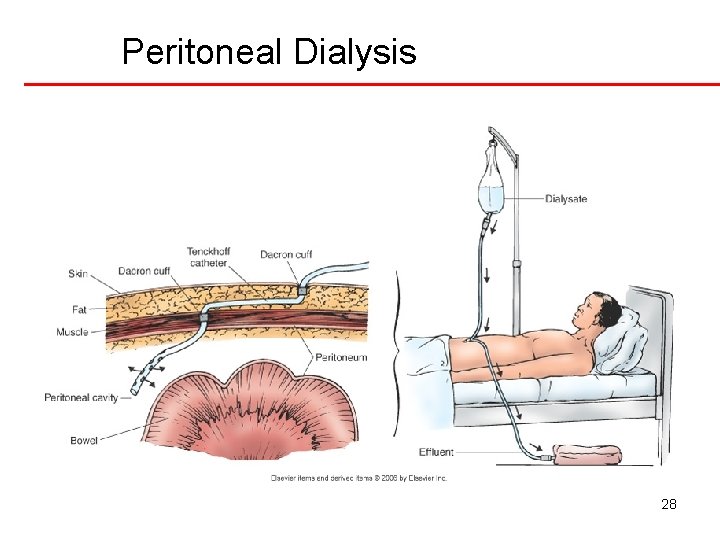
Peritoneal Dialysis 28
Peritoneal Dialysis Ø Phases q q q Ø Inflow Dwell Drain Contraindications q history of abd surgeries q recurrent hernias q excessive obesity q preexisting vertebral disease q severe obstructive pulmonary disease 29
Complications of Peritoneal Dialysis Ø Ø Ø Peritonitis (cloudy outflow) Pain Exit site and tunnel infections Poor dialysate flow Dialysate leakage Monitor color of outflow q cloudy (peritonitis) q brown (bowel) q bloody (first week OK) q urine (bladder) 30
Nursing Care During Peritoneal Dialysis Ø Ø Pre PD: q Vital signs pre and q 15 -30” during q Weight q laboratory tests Continually monitor the client for: q respiratory distress q pain q discomfort Monitor prescribed dwell time and initiate outflow Observe outflow amount & pattern of fluid 31
Education Priorities Pathophysiology and manifestations Ø Complications Ø When to call the doctor Ø Keep record of all labs Ø Take medications and follow plan of care set out by case manager Ø Monitor weight, fatigue levels closely Ø 32
 Res extra commercium
Res extra commercium Diagnostico etiologico
Diagnostico etiologico Distinguish between renal corpuscle and renal tubule
Distinguish between renal corpuscle and renal tubule Patho
Patho Earthy look in chronic renal failure
Earthy look in chronic renal failure Ongoing planning in nursing
Ongoing planning in nursing Independent nursing interventions
Independent nursing interventions Collaborative interventions nursing
Collaborative interventions nursing Nursing care plans examples
Nursing care plans examples Nursing interventions for dvt
Nursing interventions for dvt Collaborative interventions nursing
Collaborative interventions nursing How to write a care plan
How to write a care plan Goals and expected outcomes
Goals and expected outcomes What is esr
What is esr Thyroid storm pathophysiology
Thyroid storm pathophysiology Bucks traction weight
Bucks traction weight Nursing interventions for ineffective coping
Nursing interventions for ineffective coping Nursing interventions for ocd patients
Nursing interventions for ocd patients Collaborative nursing interventions
Collaborative nursing interventions Dependent intervention nursing
Dependent intervention nursing Gout care plan
Gout care plan Independent nursing interventions
Independent nursing interventions Prolapsed cord nursing interventions
Prolapsed cord nursing interventions Acute pancreatitis pathophysiology nursing
Acute pancreatitis pathophysiology nursing Nursing diagnosis for pancreatitis
Nursing diagnosis for pancreatitis Cataracts nursing interventions
Cataracts nursing interventions Hypophysectomy nursing interventions
Hypophysectomy nursing interventions Nursing care plan for syncope
Nursing care plan for syncope Pediatric hospitalist near freedom
Pediatric hospitalist near freedom Sad persons scale
Sad persons scale Nursing diagnosis for aspiration pneumonia
Nursing diagnosis for aspiration pneumonia Colostomy procedure
Colostomy procedure Diaphrosis
Diaphrosis