NURS 101 SKIN INTEGRITY AND WOUND CARE INTEGUMENTARY
- Slides: 34
NURS 101 SKIN INTEGRITY AND WOUND CARE
INTEGUMENTARY SYSTEM � Skin � Epidermis � Dermis � Subcutaneous � Hair � Nails layer
SKIN � Largest organ of body � 15% of adult body weight � Protects against disease carrying organisms � Sensory organ for pain, temp, touch � Synthesizes vitamin D � Regulates temperature � Maintains fluid balance
HEALTH HISTORY � Medications � Soap, shampoo, detergent � Itching or burning sensations � Changes in skin after certain foods � History of hives, asthma, allergies, excema � Occupation � New pets, plants
PHYSICAL ASSESSMENT � Inspection � Well lit room, use penlight if needed � Color, lesions, vascularity, condition of nails � Condition of hair (head and body, lashes) � Texture, � Moist color, distribution or dry appearance
SKIN COLOR ALTERATIONS � Pallor � Jaundice � Cyanosis � Erythema � Brown-tan
PHYSICAL ASSESSMENT � Palpation � Wear gloves to palpate rash or lesions � Mobility, turgor � Texture of skin and nails � Temperature, moist or dry
DIAGNOSTIC STUDIES � Skin biopsy � Description: � Nursing � Woods’ implications light exam � Description: � Nursing implications
OLDER ADULTS’ SKIN � � � � Reduced elasticity…. easily torn Concomitant med conditions and polypharmacy interfere with wound healing Attachment between dermis and epidermis becomes flattened, allowing mechanical tears(tape) Diminished inflammatory response, poor wound healing Dimished subcutaneous padding over bony prominences Poor nutrition is a risk factor for breakdown and pressure ulcers See chart 60 -1 in Hinkle and Cheever
PRESSURE ULCERS � Impaired skin integrity related to unrelieved, prolonged pressure. � AKA pressure sores, decubitus ulcer, bedsore � Localized injury to skin and underlying tissue, usually over a bony prominence � Pressure interferes with blood flow, cellular metabolism, results in tissue ischemia and ultimately tissue death
RISKS FOR PRESSURE ULCERS � Pressure � Decreased mobility � Decreased sensory perception � Altered level of consciousness � Fecal or urinary incontinence � Poor nutrition
STAGING A PRESSURE ULCER � Assessment descriptions � To evaluate wound healing, plan interventions, evaluate progress � Staging describes the depth of tissue destroyed � Necrotic tissue must be removed for proper staging and assessment � Staging I-IV… can stage up but not down
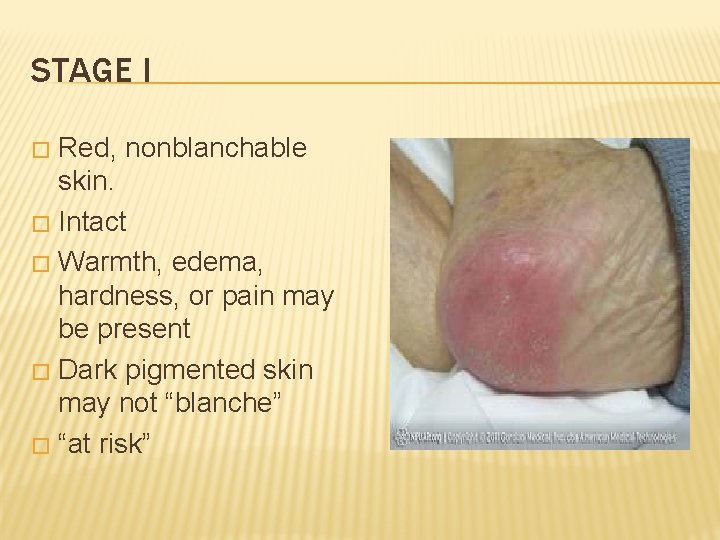
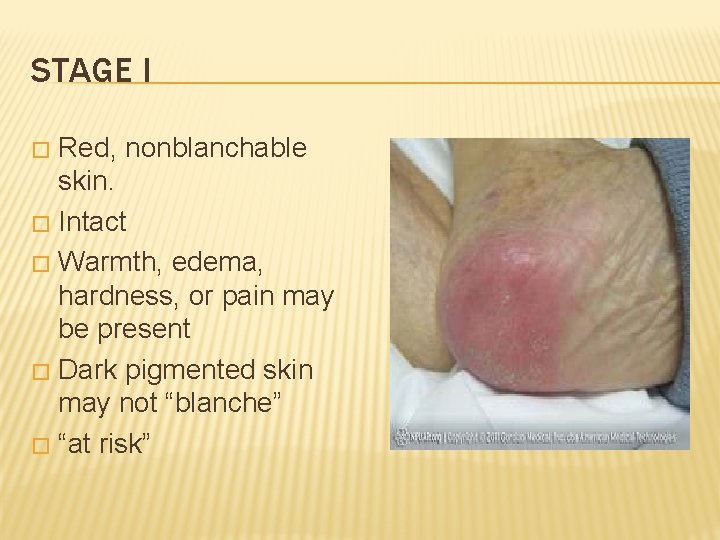
STAGE I Red, nonblanchable skin. � Intact � Warmth, edema, hardness, or pain may be present � Dark pigmented skin may not “blanche” � “at risk” �
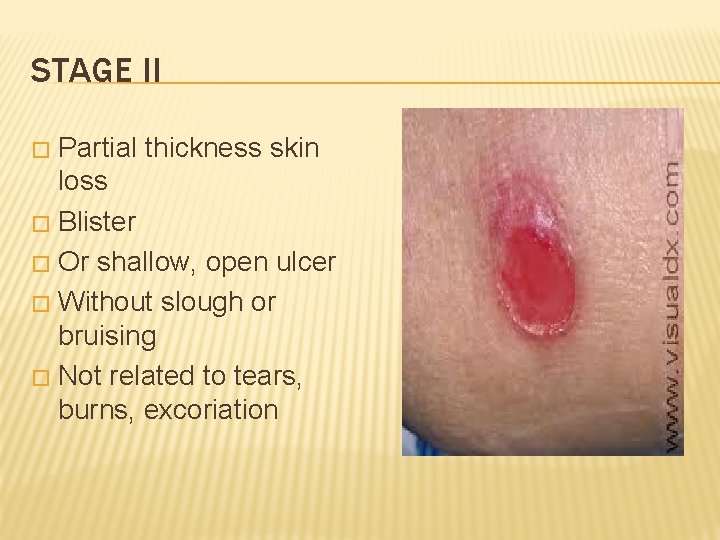
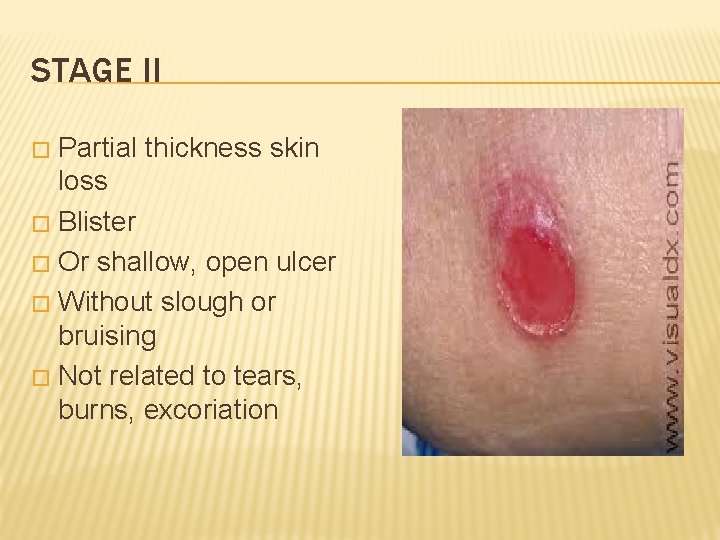
STAGE II Partial thickness skin loss � Blister � Or shallow, open ulcer � Without slough or bruising � Not related to tears, burns, excoriation �
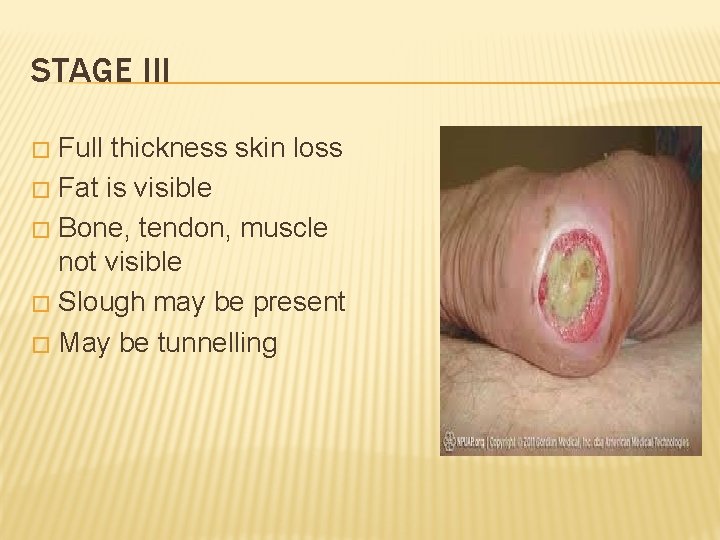
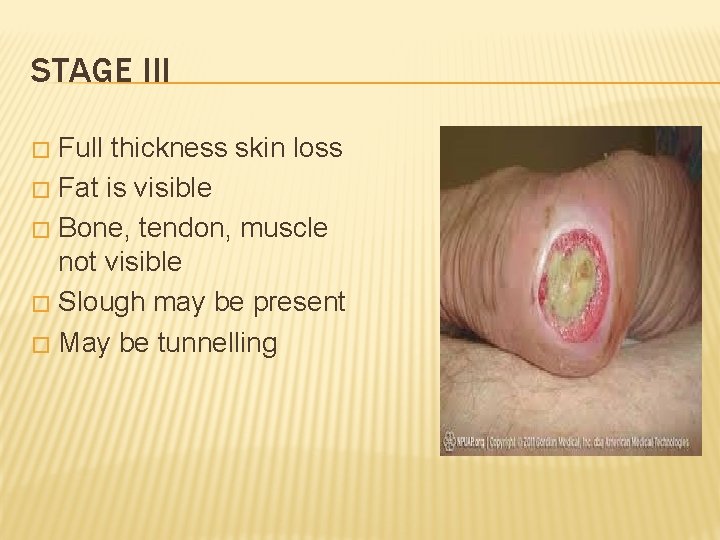
STAGE III Full thickness skin loss � Fat is visible � Bone, tendon, muscle not visible � Slough may be present � May be tunnelling �
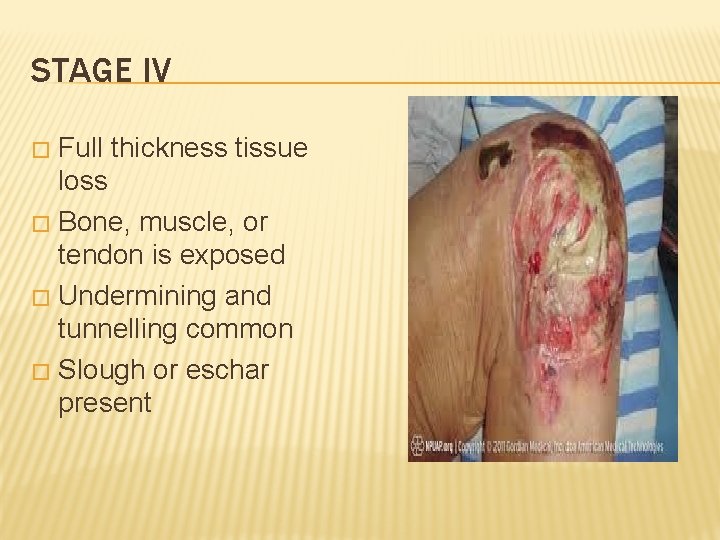
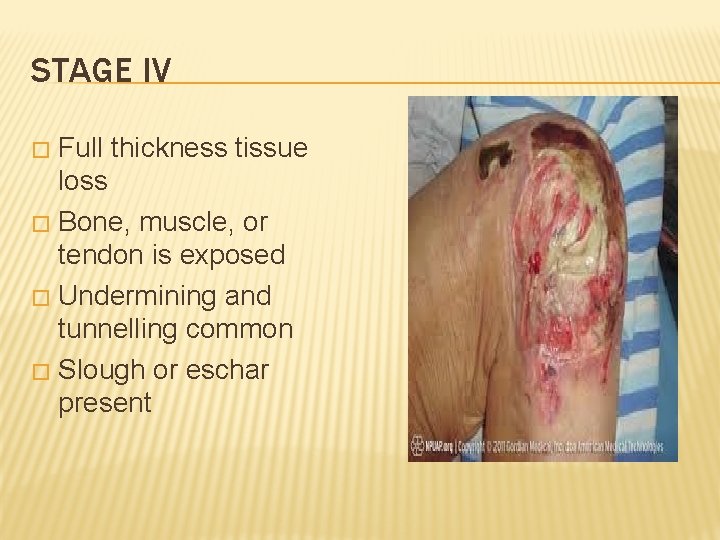
STAGE IV Full thickness tissue loss � Bone, muscle, or tendon is exposed � Undermining and tunnelling common � Slough or eschar present �
PREVENTING PRESSURE ULCERS Avoid prolonged pressure Maximize nutrition Keep skin clean and dry Use skin protectant/defriction ointment Daily assessments Document changes Educate patients
TREATING PRESSURE ULCERS � Easier to prevent than to treat!!!! � Avoid rubbing area � Keep clean and dry � Barrier ointment � Irrigate open ulcers with SALINE � Dressing per facility or wound nurse recommendation (may be moist or dry)
BRADEN SCALE � Sensory TABLE 48 -3 perception 1 -4 � Moisture 1 -4 � Activity 1 -4 � Mobility 1 -4 � Nutrition 1 -4 (usual intake pattern) � Friction and shear 1 -3 � The lower the number, the greater the risk
ACUTE � � Trauma, surgical incision Proceeds through orderly and timely reparitive process Edges are clean and intact Easily cleaned and repaired CHRONIC � � Fails to proceed through an orderly and timely process Does produce anatomical and functional integrity Chronic inflammation, vascular compromise, repetitive insults to tissue Continued exposure to insult impedes healing WOUND CLASSIFICATIONS
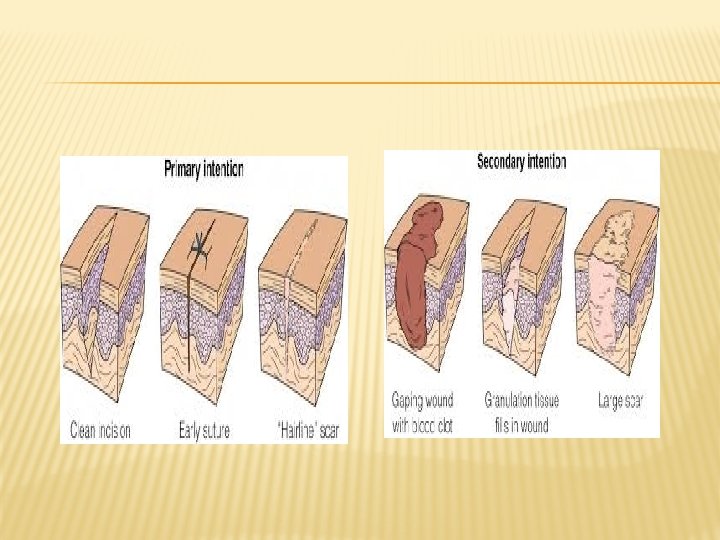
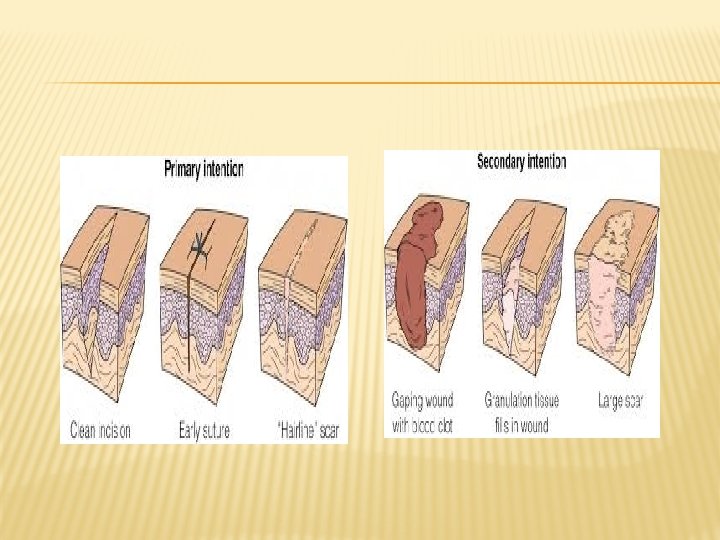
HEALING PROCESSES � Primary intention; edges are closed, risk of infection low. minimal scar formation � Secondary intention: involves loss of tissue. Wound is left open until filled with scar tissue. Longer to heal, more risk of infection � Tertiary intention: delayed closure of wound for several days. Resolve infection before closing
PROCESS OF WOUND REPAIR (PARTIAL THICKNESS) � Tissue trauma causes inflammatory response � Epithelial cells begin to regenerate � Epithelial proliferation and migration start at the wound edges, migrate across wound bed � Migration requires a moist surface
PROCESS OF WOUND REPAIR (FULL THICKNESS) Hemostasis- blood vessels constrict, platelets gather. Fibrin matrix formed for cellular repair � Inflammatory phase- damaged cells secrete histamine, causing vasodilation of surrounding capillaries and exudation of serum and WBCs into damaged tissue. Redness, warmth, edema � Proliferative phase- construction of new blood vessels, fill wound with granulation tissue, resurface with epithelial cells. New collagen � Remodeling- maturation of cells. Collagen continues to reorganize. Scar tissue may be lighter or darker than surrounding skin. �
IMPAIRMENT OF HEALING � Age � Anemia � Hypoproteinemia � Zinc deficiency
COMPLICATIONS OF WOUND HEALING � Hemorrhage � Infection � Dehiscience � Evisceration
NUTRITION AND WOUND HEALING � Calories � Protein � Vit C � Vit A � Vit E � Zinc � Fluid
WOUND TERMINOLOGY � Abrasion � Avulsion � Incision � Laceration � Puncture � Ulcer
ASSESSING WOUNDS � Do not remove dressing without order unless you suspect complications � Analgesia if needed 30 mins prior � Edges: approximated? Clean? � Presence of exudate? Color, odor? � Wound base description? � Erythema? Edema? � Surrounding skin? ?
MORE ASSESSMENT DATA � Serum albumin level � White blood cell count � Wound culture, gram stain results � Vital signs � Palpation of periwound skin
ASSESSING DRAINAGE � Amount (scant, small, moderate, copious, saturated dressing) � Weigh the dressing if needed for exact measure � Record output from drain � Serous, sanguinous, serosanguinous, purulent
DRAINS � Change dressings with caution to avoid dislodging drains � Yes, Penrose drains are supposed to have that safety pin. � Nurses may “pull” drains with surgeon’s orders � Empty receptacle as needed, at least q shift � Make sure suction and drainage continue, “strip” tubing with order only.
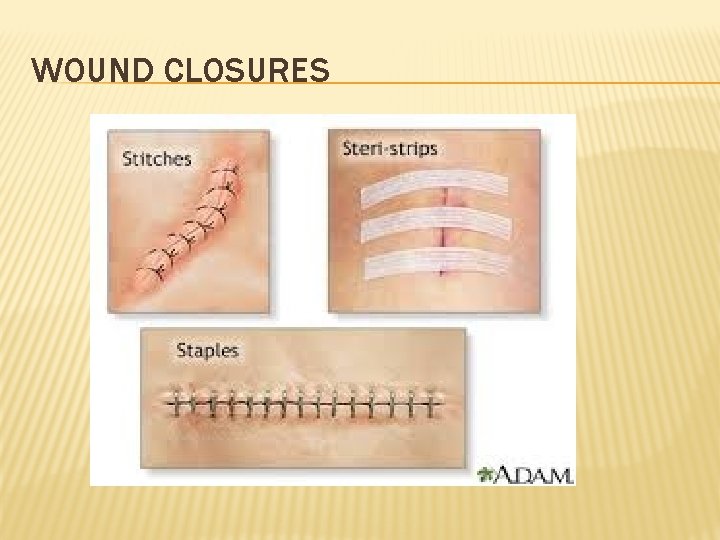
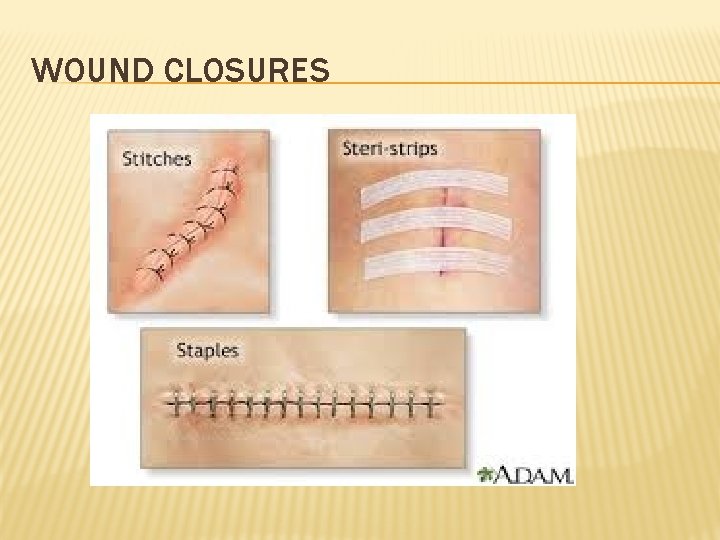
WOUND CLOSURES
COLLABORATE WITH � Physicians and surgeons � Physical therapists � Wound/ostomy nurse � Dieticians