Nuclear Medicine Physics Gamma Camera Scintillation Camera Jerry
- Slides: 47
Nuclear Medicine Physics • Gamma Camera, Scintillation Camera Jerry Allison, Ph. D. Department of Radiology Medical College of Georgia
A note of thanks to Z. J. Cao, Ph. D. Medical College of Georgia And Sameer Tipnis, Ph. D. G. Donald Frey, Ph. D. Medical University of South Carolina for Sharing nuclear medicine presentation content
How to obtain a NM image? Administer radiopharmaceutical (a radionuclide labeled to a pharmaceutical) The radiopharmaceutical is concentrated in the desired locations. Nucleus of the radionuclide decays to emit photons Detect the photons using a “gamma camera” (scintillation camera, Anger camera)
Basic principle - rays directed towards a scintillation crystal - Na. I(Tl) Multiple PMTs detect light flashes Signal ( E) is converted to electrical pulses Pulses fed to energy discrimination and positioning circuits Image of radionuclide distribution formed and displayed 2015 Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
Nuclear medicine is emission imaging. photons are emitted from inside of patient. energy: 70 to 511 ke. V Relatively poor image quality due to limited photon number (severe image noise) and poor spatial resolution Image noise caused by low count density (105 – 106 lower than x-ray imaging) CT is transmission imaging
BUT: Nuclear medicine is molecular imaging Interaction of the radiopharmaceutical with cells or molecules molecular imaging Bound directly to a target molecule (111 Inmonoclonal antibody) Accumulated by molecular or cellular activities (18 F-FDG, 99 m. Tc-sestamibi, 131 I ) Molecular or cellular activities (e. g. perfusion for heart, brain, kidney, lungs and metabolism of cancers) earlier diagnosis
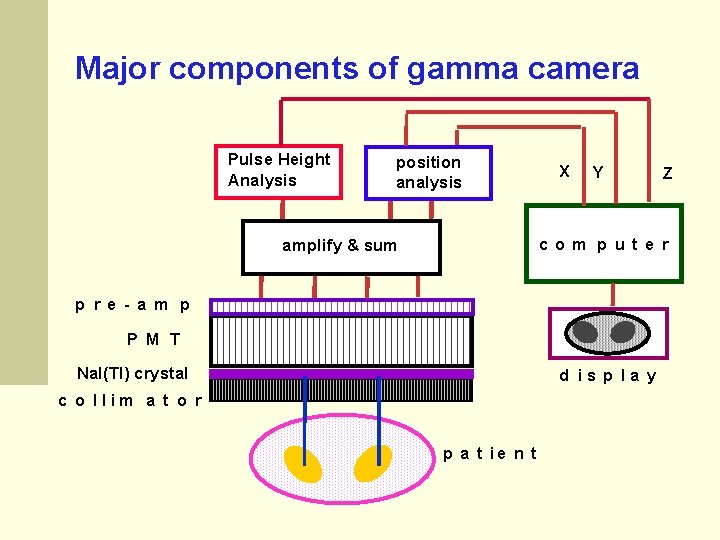
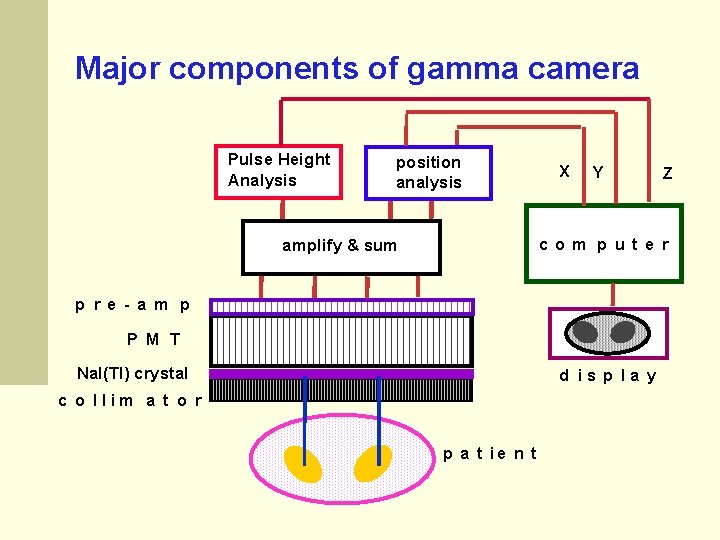
Major components of gamma camera Pulse Height Analysis position analysis X Y Z co m p ut e r amplify & sum p re - a m p P M T Na. I(Tl) crystal d is p la y c o llim a t o r p a t ie n t
Gamma Camera Components 8
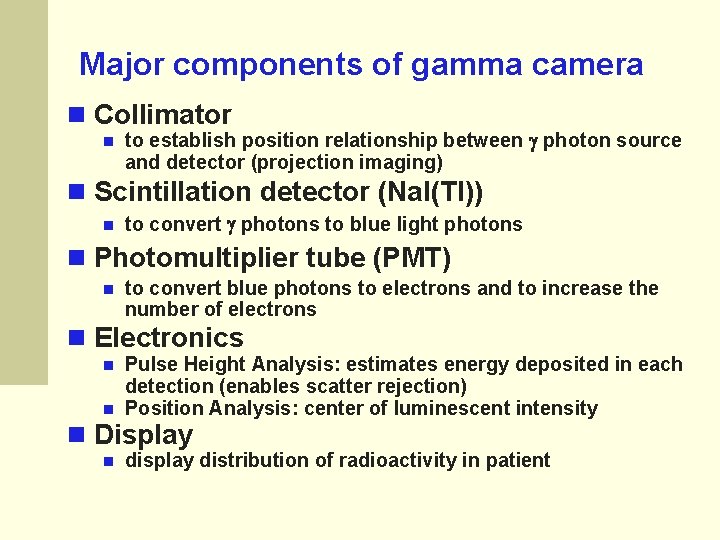
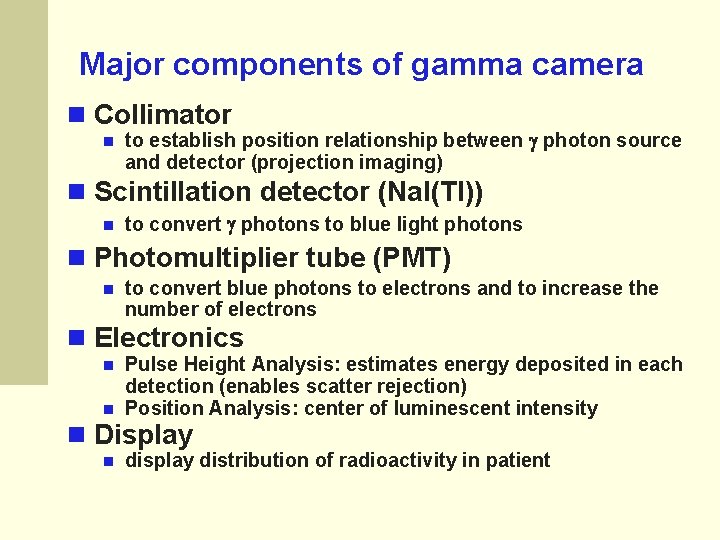
Major components of gamma camera Collimator to establish position relationship between photon source and detector (projection imaging) Scintillation detector (Na. I(Tl)) to convert photons to blue light photons Photomultiplier tube (PMT) to convert blue photons to electrons and to increase the number of electrons Electronics Pulse Height Analysis: estimates energy deposited in each detection (enables scatter rejection) Position Analysis: center of luminescent intensity Display display distribution of radioactivity in patient
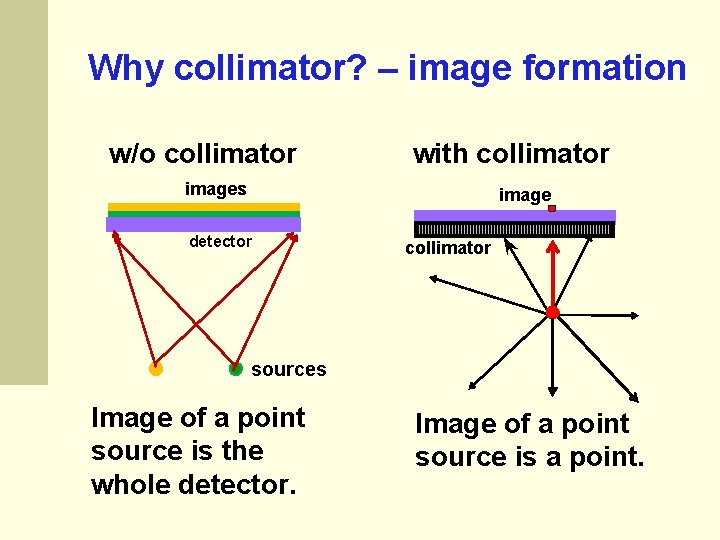
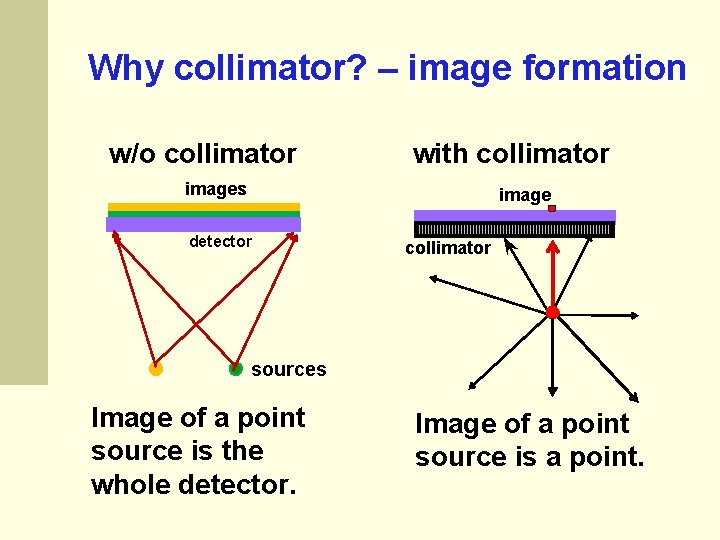
Why collimator? – image formation w/o collimator with collimator images image detector collimator sources Image of a point source is the whole detector. Image of a point source is a point.
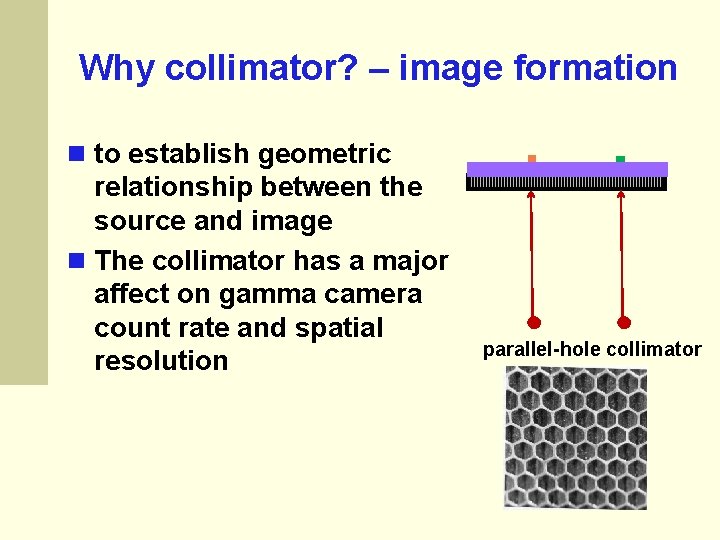
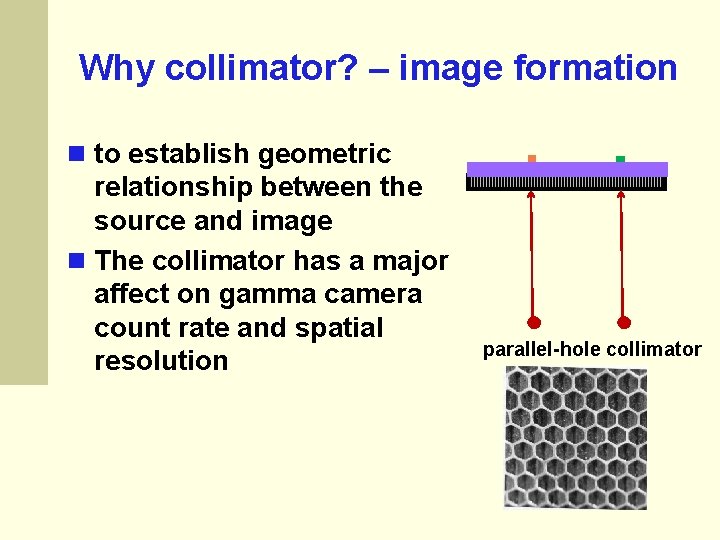
Why collimator? – image formation to establish geometric relationship between the source and image The collimator has a major affect on gamma camera count rate and spatial resolution parallel-hole collimator
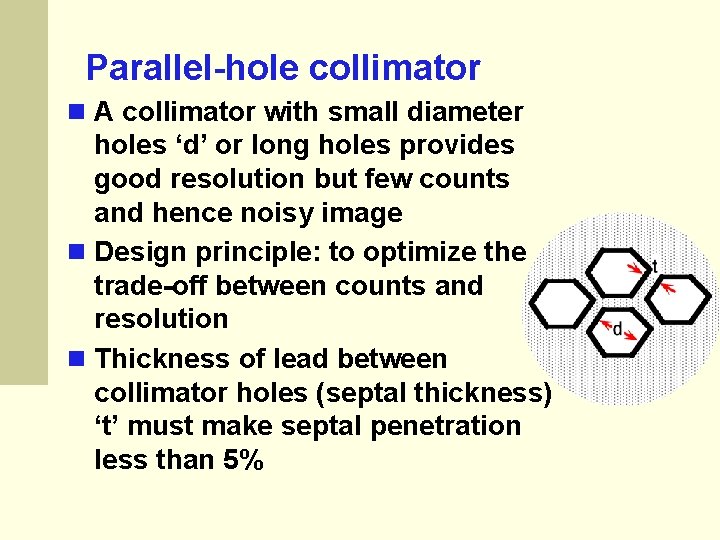
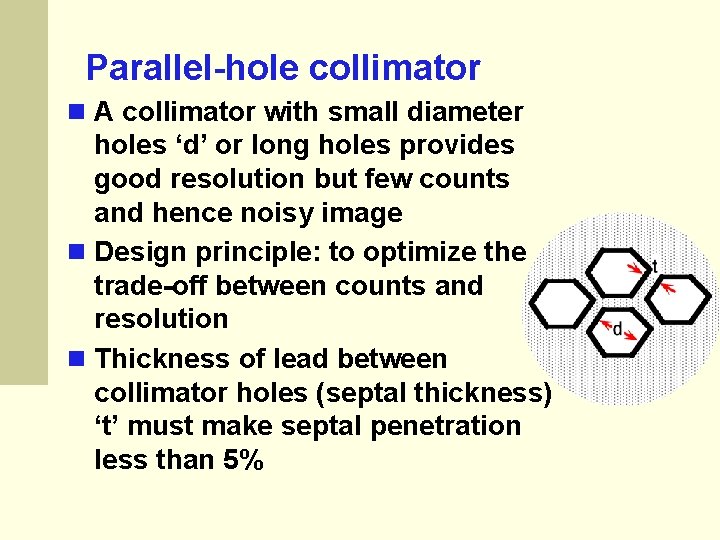
Parallel-hole collimator A collimator with small diameter holes ‘d’ or long holes provides good resolution but few counts and hence noisy image Design principle: to optimize the trade-off between counts and resolution Thickness of lead between collimator holes (septal thickness) ‘t’ must make septal penetration less than 5%
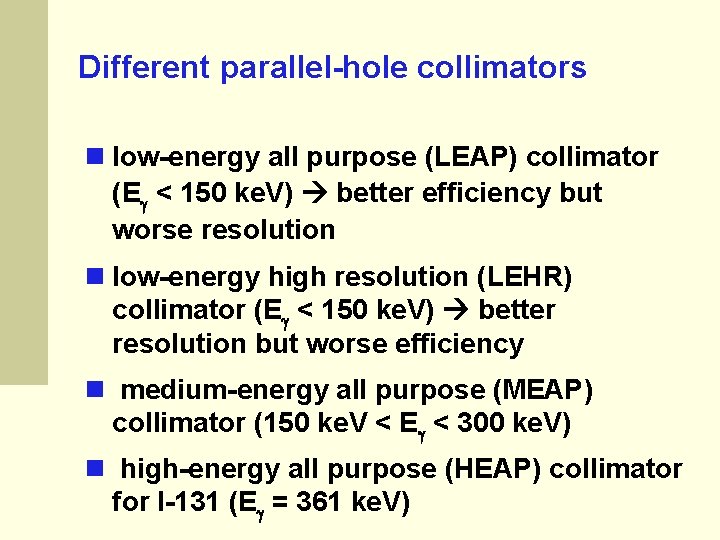
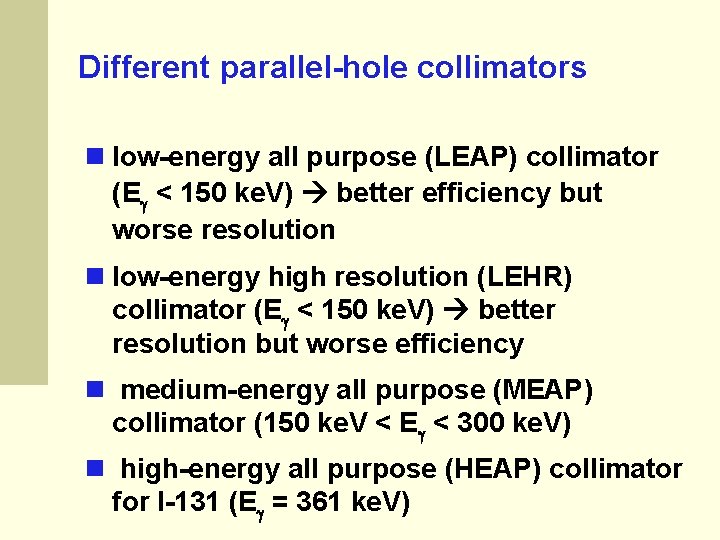
Different parallel-hole collimators low-energy all purpose (LEAP) collimator (E < 150 ke. V) better efficiency but worse resolution low-energy high resolution (LEHR) collimator (E < 150 ke. V) better resolution but worse efficiency medium-energy all purpose (MEAP) collimator (150 ke. V < E < 300 ke. V) high-energy all purpose (HEAP) collimator for I-131 (E = 361 ke. V)
Collimators • Most often used: parallel-hole collimator • For thyroid: pin-hole collimator • For brain and heart: converging collimator 2015 Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
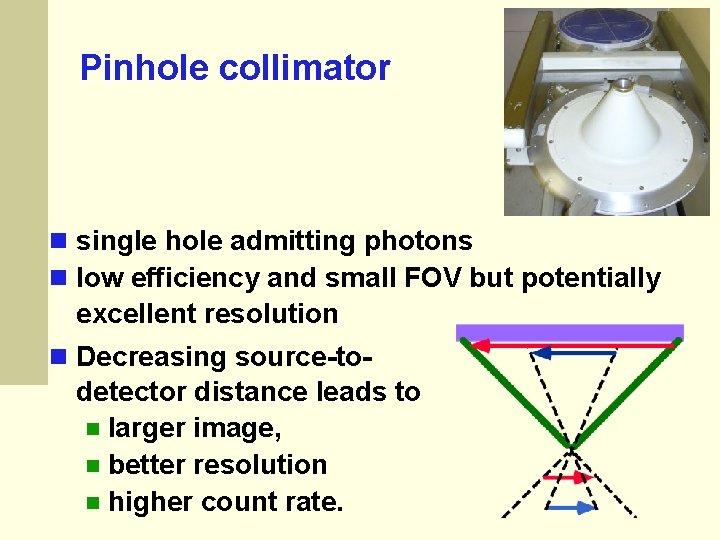
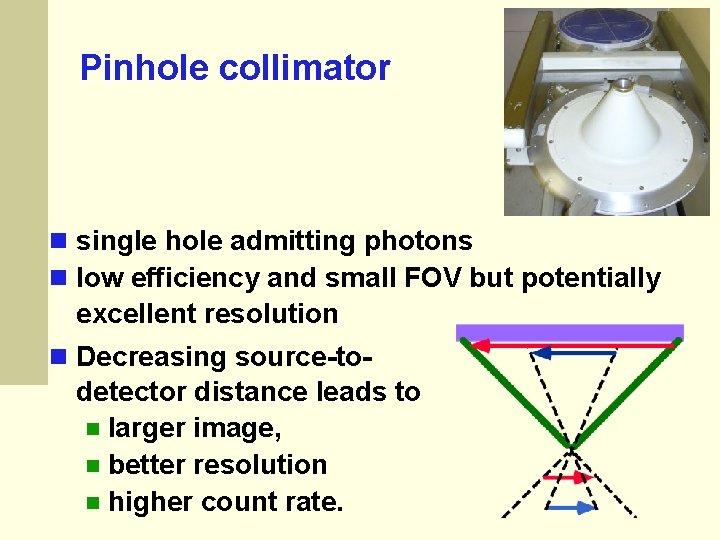
Pinhole collimator single hole admitting photons low efficiency and small FOV but potentially excellent resolution Decreasing source-to- detector distance leads to larger image, better resolution higher count rate.
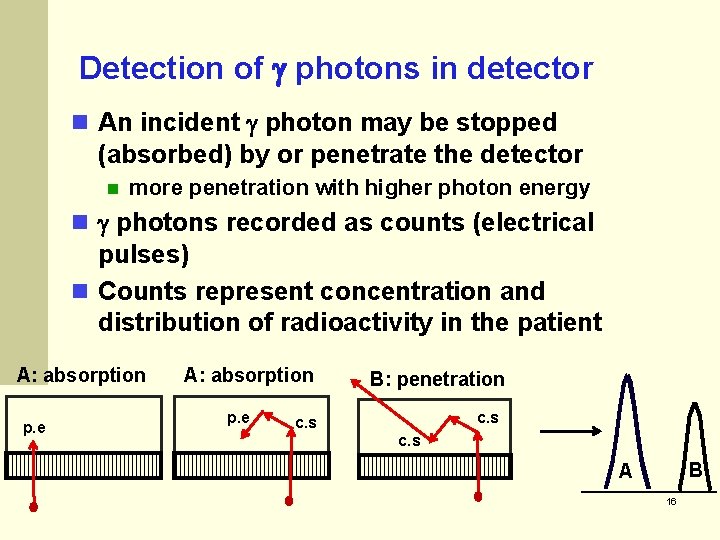
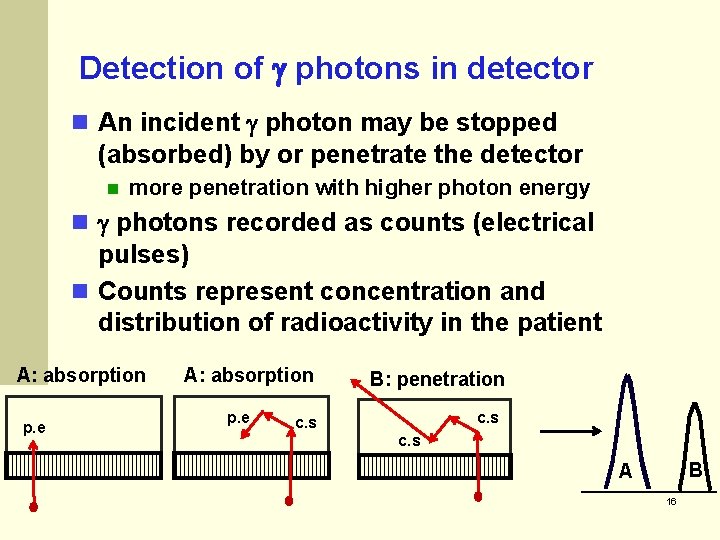
Detection of photons in detector An incident photon may be stopped (absorbed) by or penetrate the detector more penetration with higher photon energy photons recorded as counts (electrical pulses) Counts represent concentration and distribution of radioactivity in the patient A: absorption p. e B: penetration c. s B A 16
Detection of photons in detector The pulse height is determined by the energy deposited by a photon in the detector. A penetrating photon deposits less energy so the electrical pulse is smaller. A photon scattered in the patient loses energy so the pulse is smaller when it is detected. Scatter in detector make it impossible to know the entry point of the photon. 17
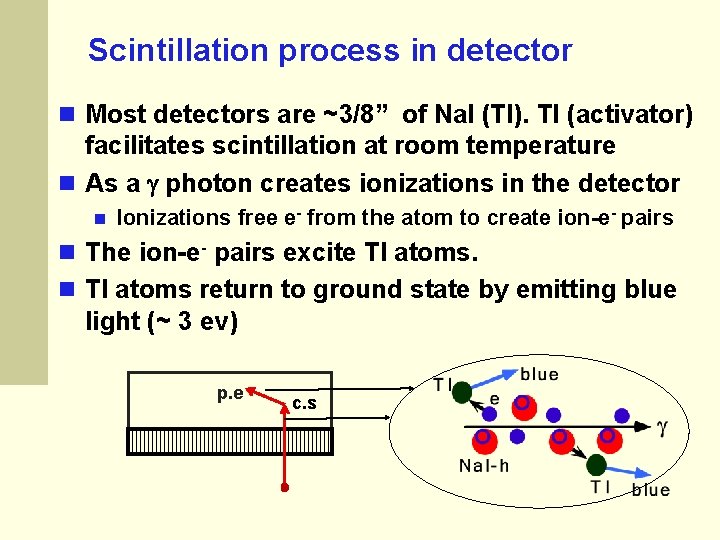
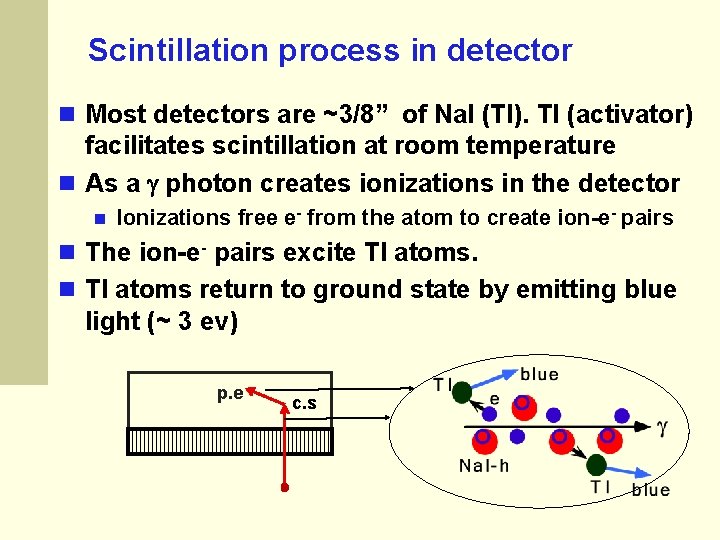
Scintillation process in detector Most detectors are ~3/8” of Na. I (Tl). Tl (activator) facilitates scintillation at room temperature As a photon creates ionizations in the detector Ionizations free e- from the atom to create ion-e- pairs The ion-e- pairs excite Tl atoms return to ground state by emitting blue light (~ 3 ev) p. e c. s
Scintillation process in detector The detector converts photons to a number of blue photons. The number of blue photons is proportional to the energy deposited by photon e. g. 140 ke. V 5000 and 70 ke. V 2500 blue photons The number of blue photons determines the number of electrons liberated in the photocathodes of PMTs and in turn, the electrical pulse height. Electrical pulse height is proportional to photon energy deposited in the crystal
Desirable Scintillator Properties High , Z high absorption efficiency Improves detector sensitivity High light output (conversion efficiency) Improves energy discrimination, spatial resolution Light output proportional to energy deposited Improves linearity Transparent to light emissions 2015 Improves sensitivity Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
How good (bad) is Na. I (Tl) detector? Good stopping power for low-energy photons by photoelectric process at 69 ke. V, penetration 0% for a thickness (t) of 3/8” at 140 ke. V, penetration = 7. 7% for t of 3//8” at 247 ke. V, penetration = 48. 5% for t of 3/8” Slow scintillation decay (230 ns) which limits count rate (avoid pulse pile-up) 21
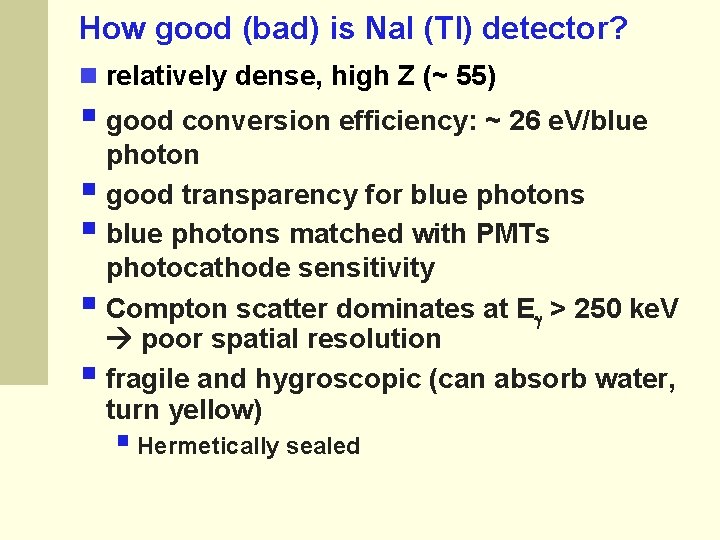
How good (bad) is Na. I (Tl) detector? relatively dense, high Z (~ 55) § good conversion efficiency: ~ 26 e. V/blue photon § good transparency for blue photons § blue photons matched with PMTs photocathode sensitivity § Compton scatter dominates at E > 250 ke. V poor spatial resolution § fragile and hygroscopic (can absorb water, turn yellow) § Hermetically sealed
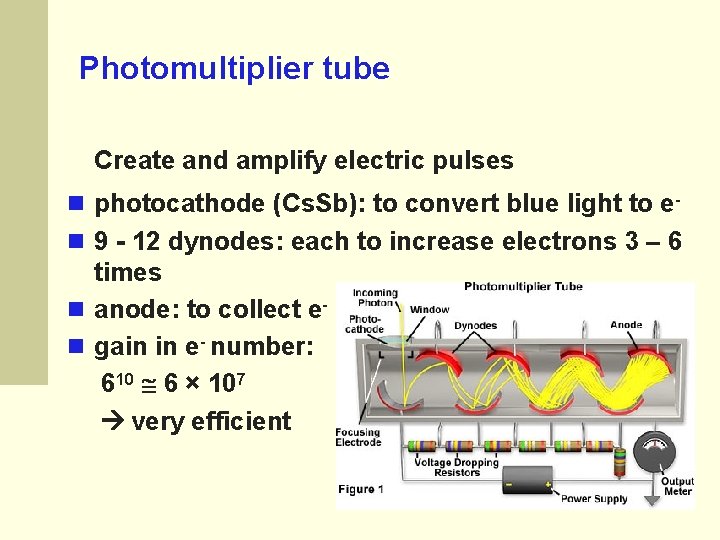
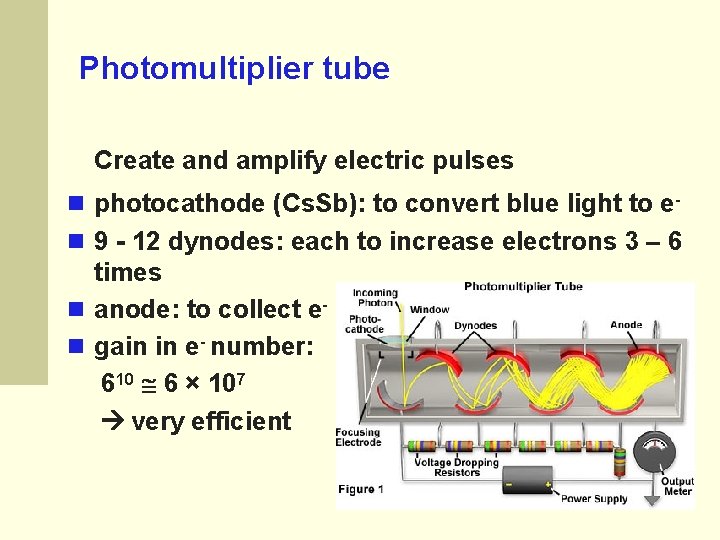
Photomultiplier tube Create and amplify electric pulses photocathode (Cs. Sb): to convert blue light to e 9 - 12 dynodes: each to increase electrons 3 – 6 times anode: to collect e gain in e- number: 610 6 × 107 very efficient
Photomultiplier tube (PMT) § 40 to 100 PM tubes (d = 5 cm) in a modern gamma camera § photocathod directly coupled to detector or connected using plastic light guides § anode connected to electronics in the tube base § ultrasensitive to magnetic field
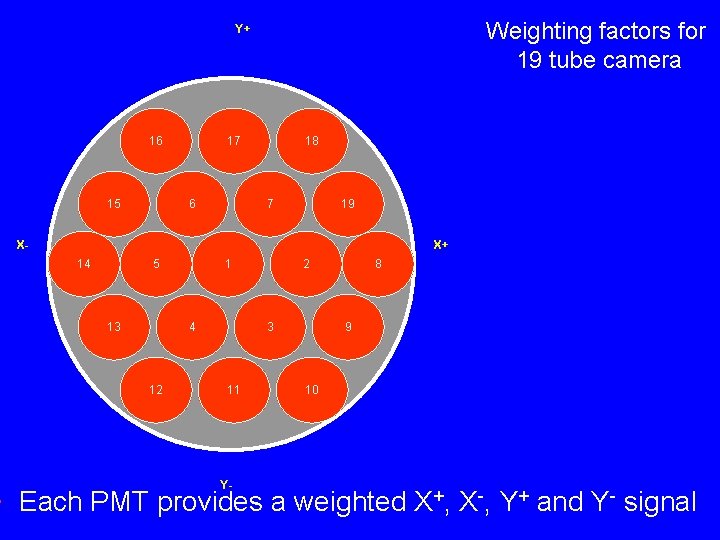
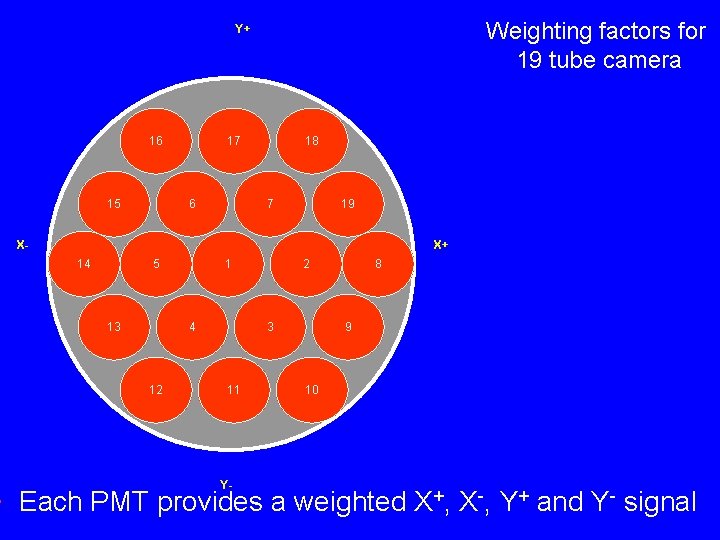
Weighting factors for 19 tube camera Y+ 16 15 17 6 18 7 19 X- X+ 14 5 13 1 4 12 2 3 11 Y- 8 9 10 • Each PMT provides a weighted X+, X-, Y+ and Y- signal
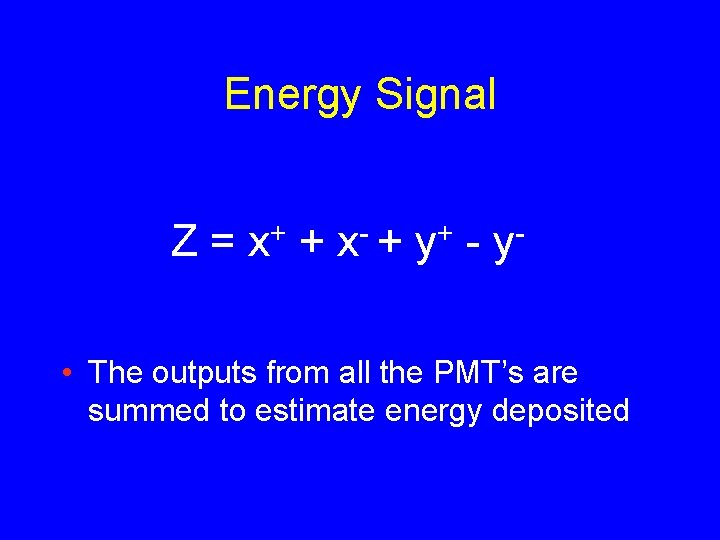
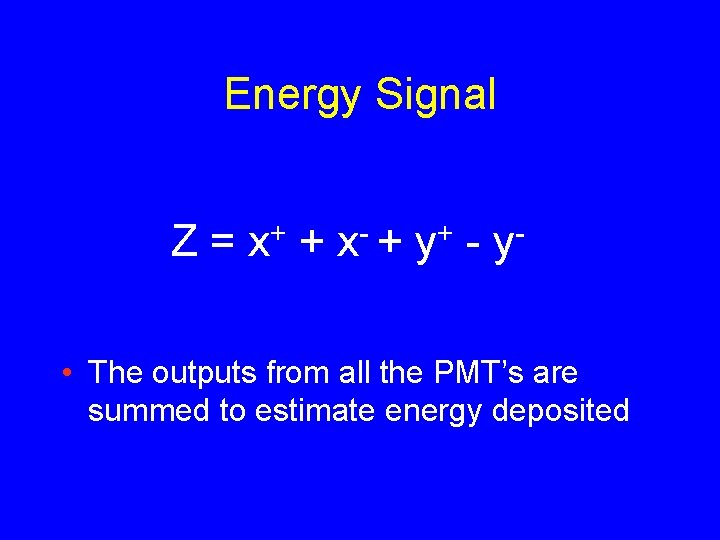
Energy Signal Z= + x + + y - y • The outputs from all the PMT’s are summed to estimate energy deposited
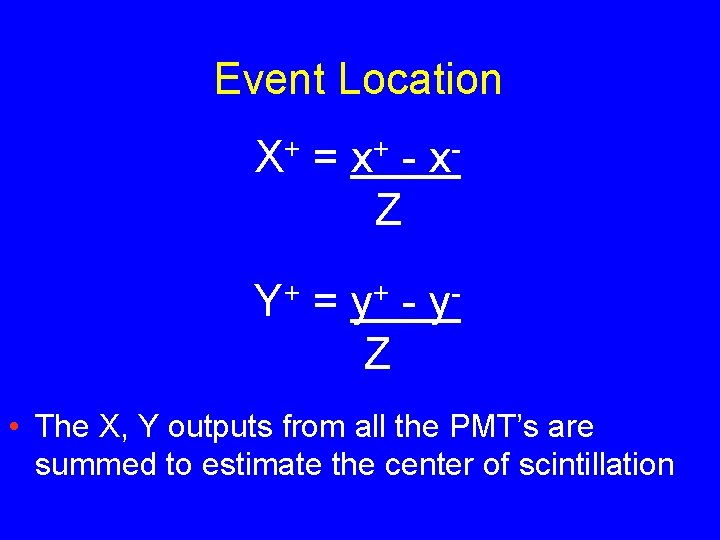
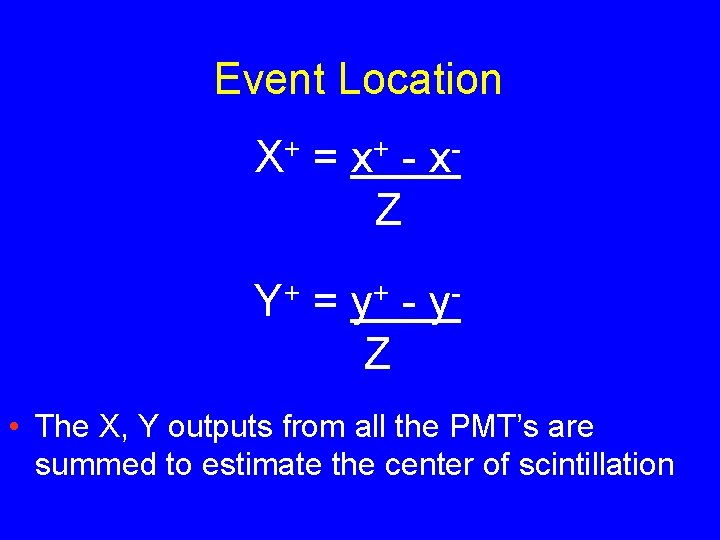
Event Location + X = + x - y Z + Y = + y Z • The X, Y outputs from all the PMT’s are summed to estimate the center of scintillation
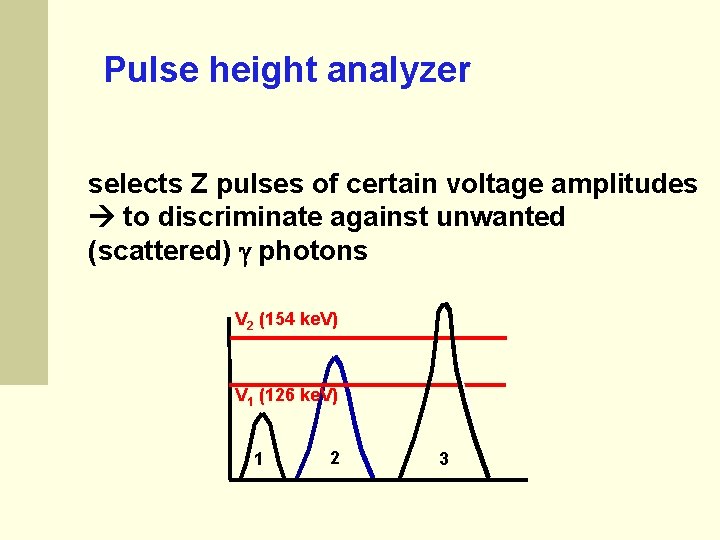
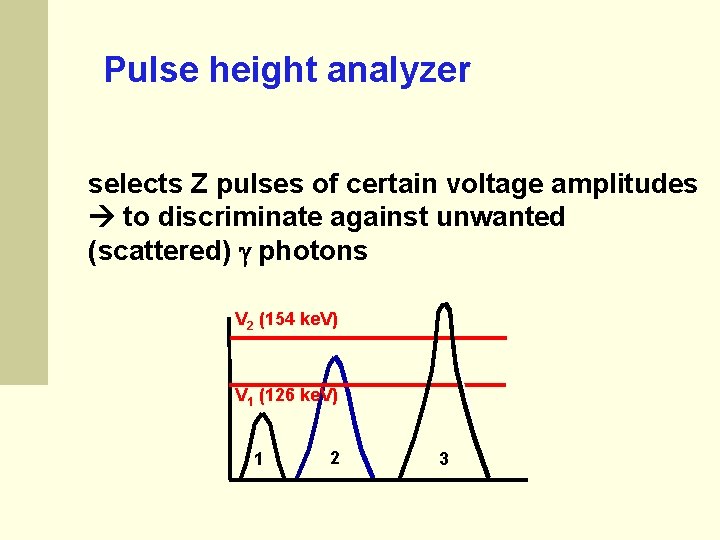
Pulse height analyzer selects Z pulses of certain voltage amplitudes to discriminate against unwanted (scattered) photons V 2 (154 ke. V) V 1 (126 ke. V) 1 2 3
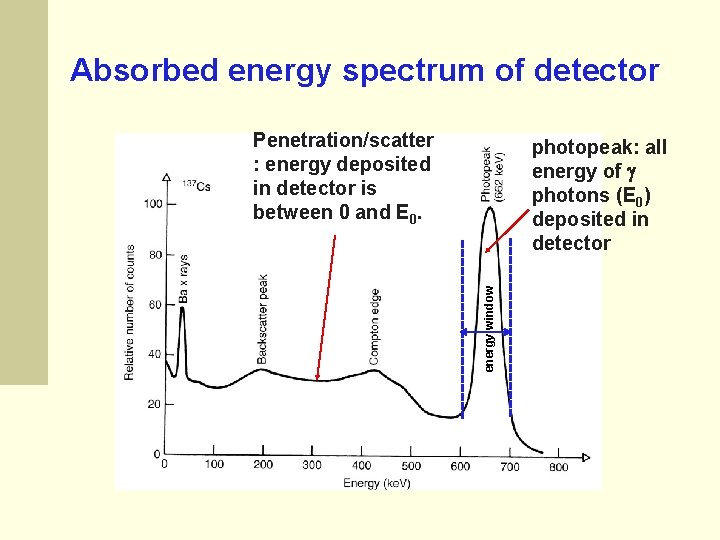
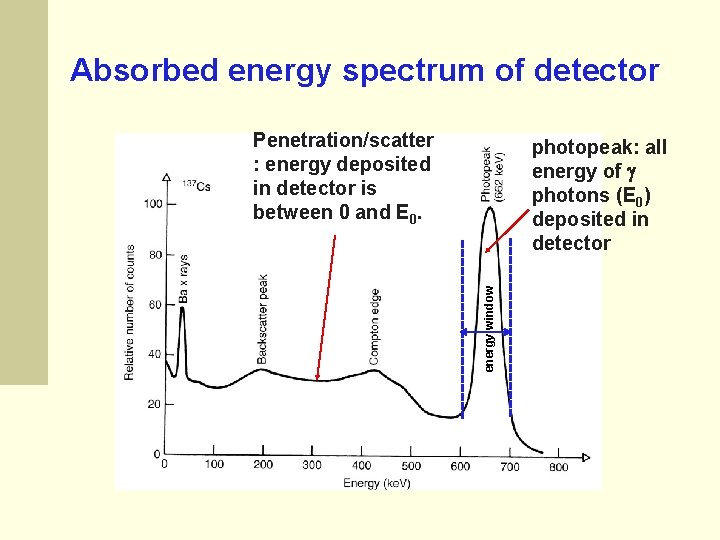
Absorbed energy spectrum of detector Penetration/scatter : energy deposited in detector is between 0 and E 0. energy window photopeak: all energy of photons (E 0) deposited in detector
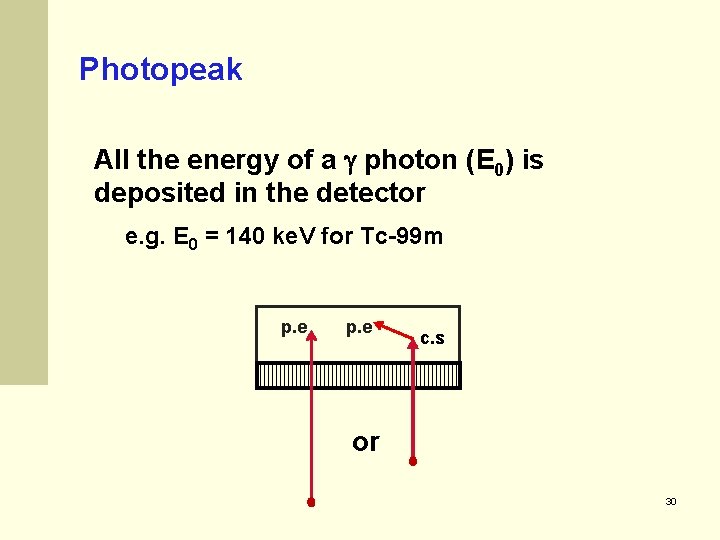
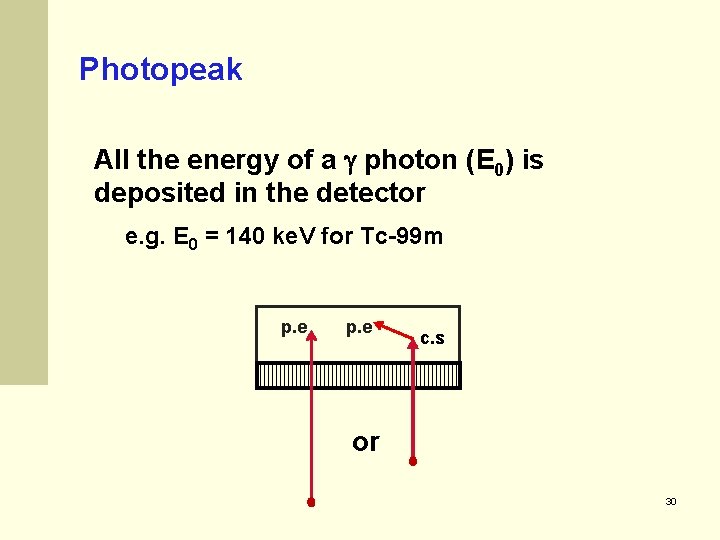
Photopeak All the energy of a photon (E 0) is deposited in the detector e. g. E 0 = 140 ke. V for Tc-99 m p. e c. s or 30
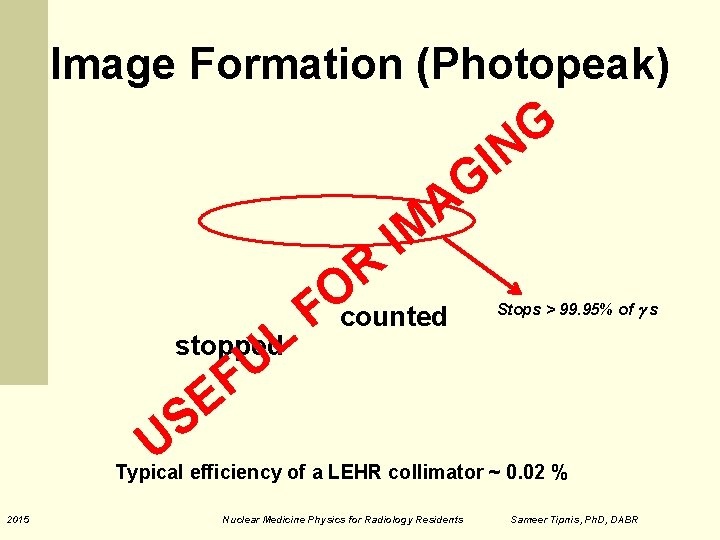
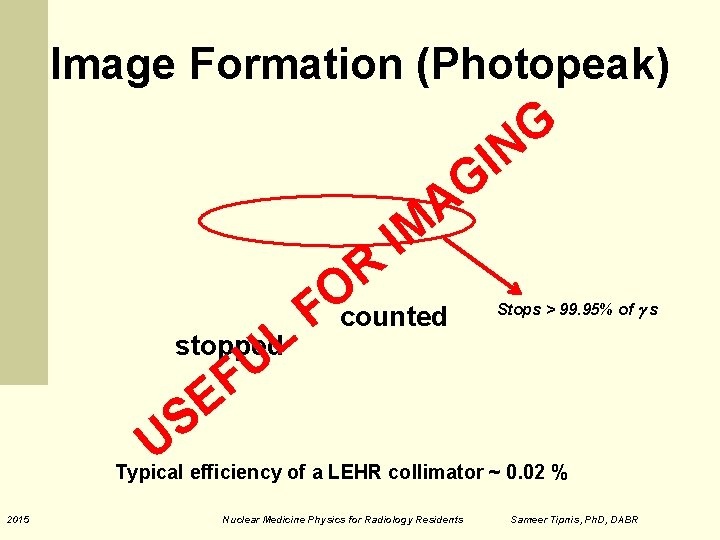
Image Formation (Photopeak) A L U F E stopped F R O IM counted G N I G Stops > 99. 95% of s S U Typical efficiency of a LEHR collimator ~ 0. 02 % 2015 Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
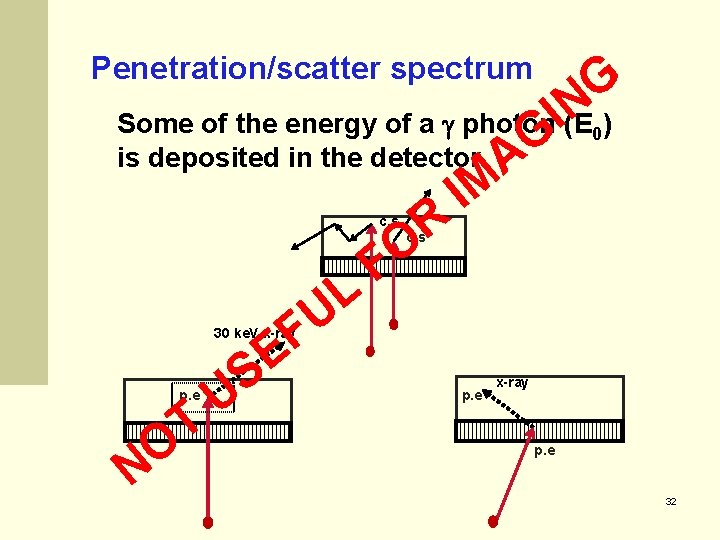
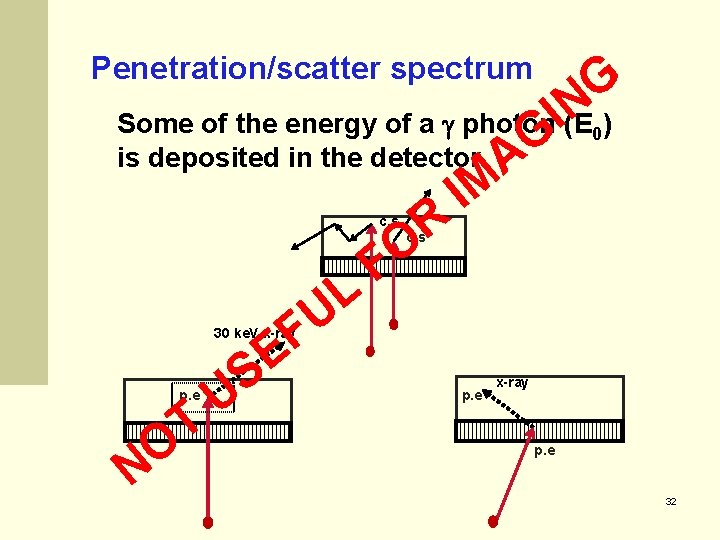
Penetration/scatter spectrum G N) Some of the energy of a photon I(E is deposited in the detector AG IM R O F L U F E S U T O N 0 c. s 30 ke. V x-ray p. e 32
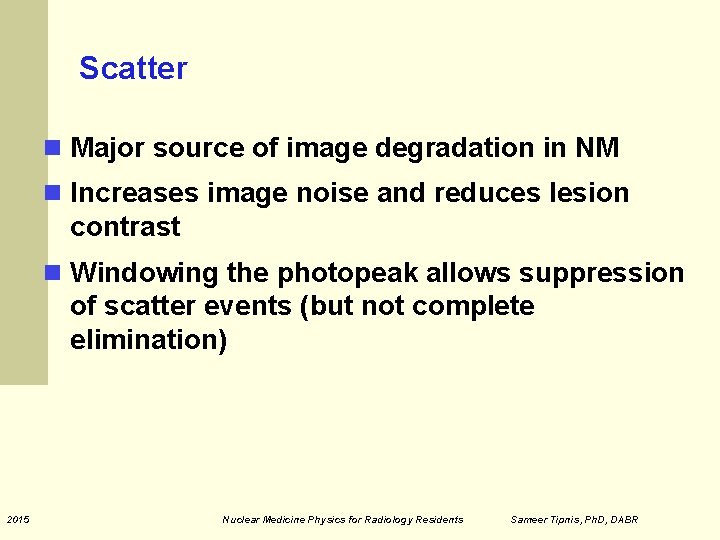
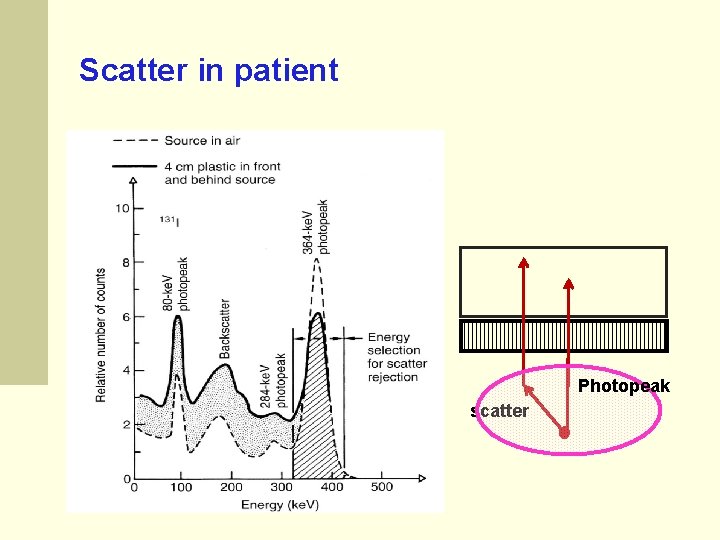
Scatter Major source of image degradation in NM Increases image noise and reduces lesion contrast Windowing the photopeak allows suppression of scatter events (but not complete elimination) 2015 Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
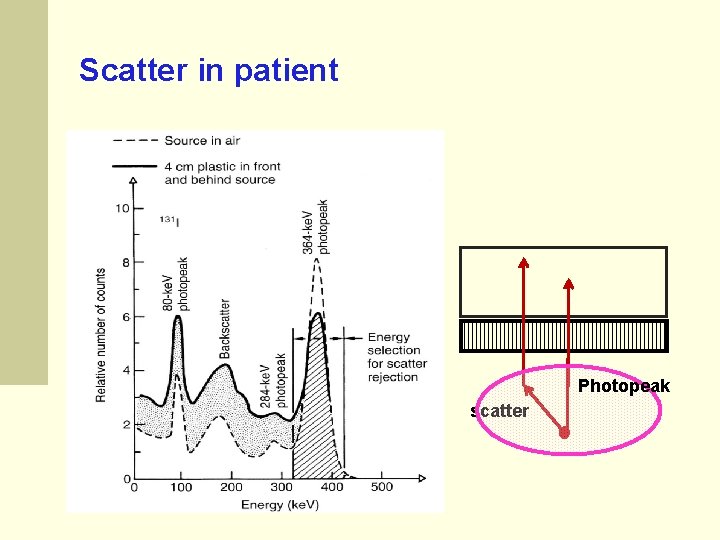
Scatter in patient Photopeak scatter
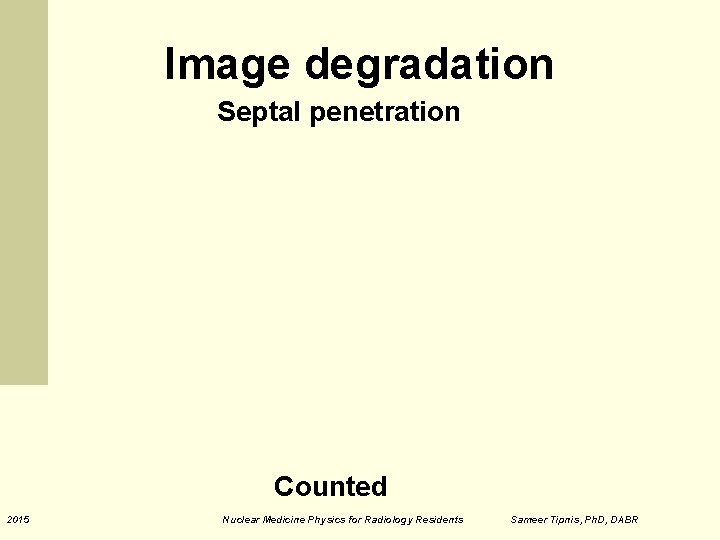
Image degradation Septal penetration Counted 2015 Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
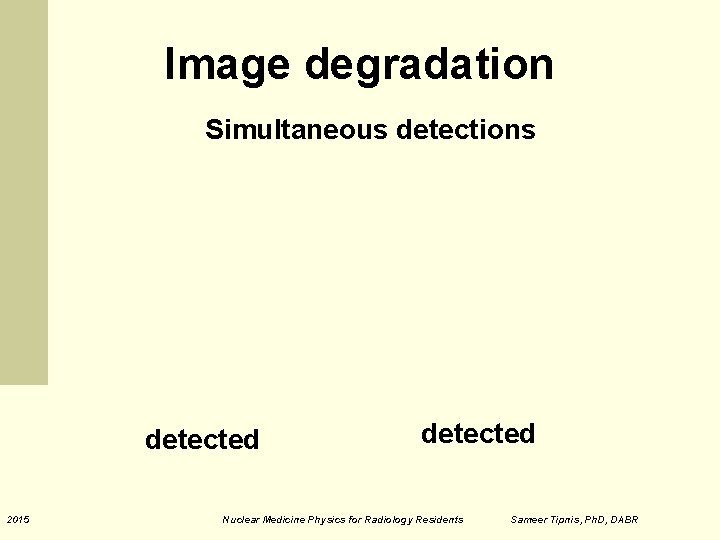
Image degradation Simultaneous detections detected 2015 detected Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
Image degradation Scatter detected 2015 Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
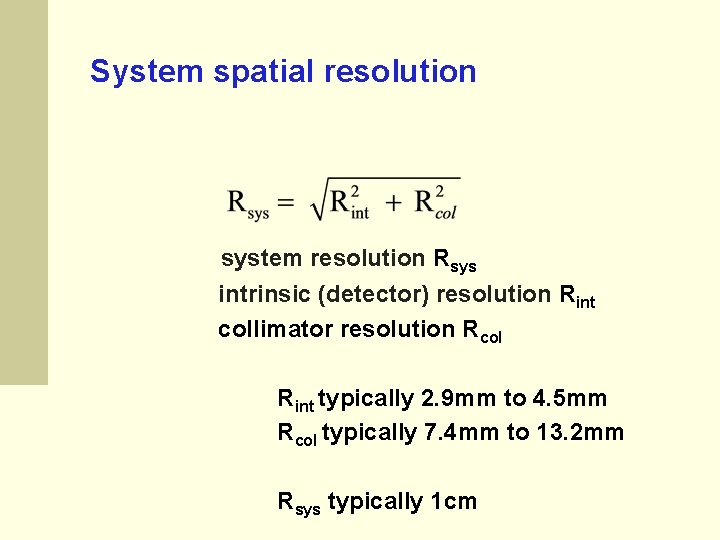
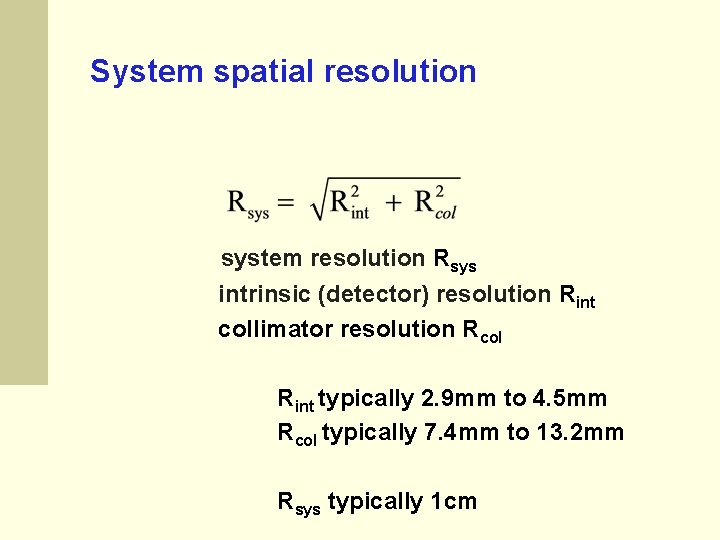
System spatial resolution system resolution Rsys intrinsic (detector) resolution Rint collimator resolution Rcol Rint typically 2. 9 mm to 4. 5 mm Rcol typically 7. 4 mm to 13. 2 mm Rsys typically 1 cm
Collimator Resolution Spatial resolution degrades with increasing pt – collimator distance. 2015 Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
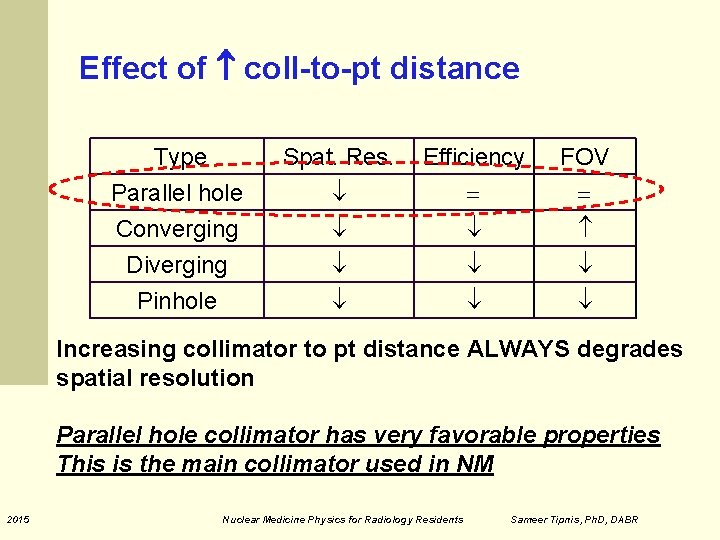
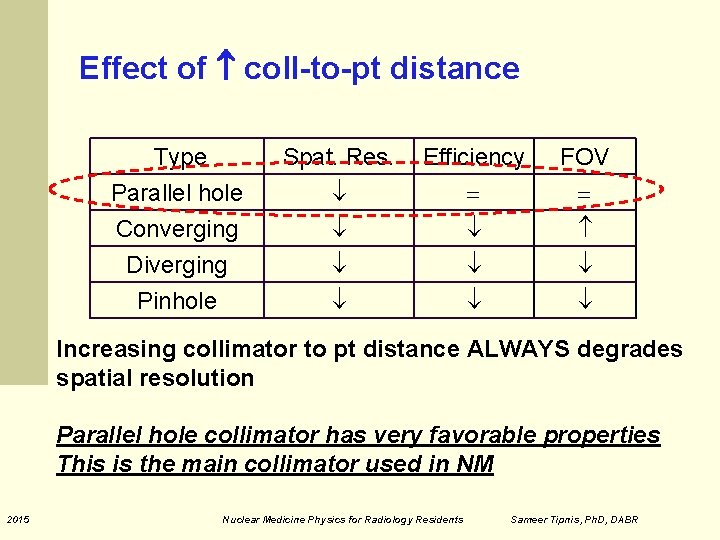
Effect of coll-to-pt distance Type Parallel hole Converging Diverging Spat. Res. Efficiency FOV Pinhole Increasing collimator to pt distance ALWAYS degrades spatial resolution Parallel hole collimator has very favorable properties This is the main collimator used in NM 2015 Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
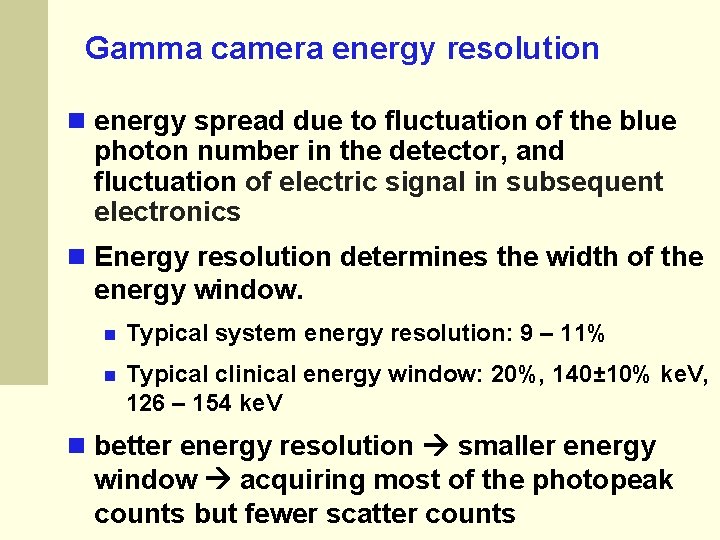
Gamma camera energy resolution energy spread due to fluctuation of the blue photon number in the detector, and fluctuation of electric signal in subsequent electronics Energy resolution determines the width of the energy window. Typical system energy resolution: 9 – 11% Typical clinical energy window: 20%, 140± 10% ke. V, 126 – 154 ke. V better energy resolution smaller energy window acquiring most of the photopeak counts but fewer scatter counts
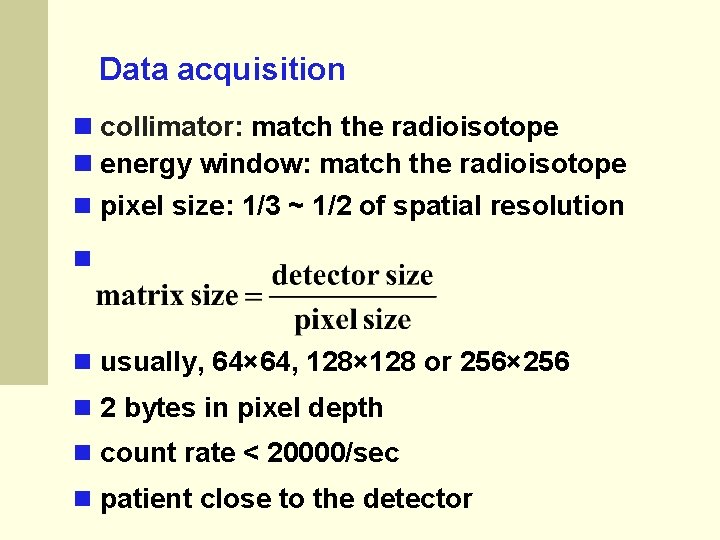
Data acquisition collimator: match the radioisotope energy window: match the radioisotope pixel size: 1/3 ~ 1/2 of spatial resolution usually, 64× 64, 128× 128 or 256× 256 2 bytes in pixel depth count rate < 20000/sec patient close to the detector
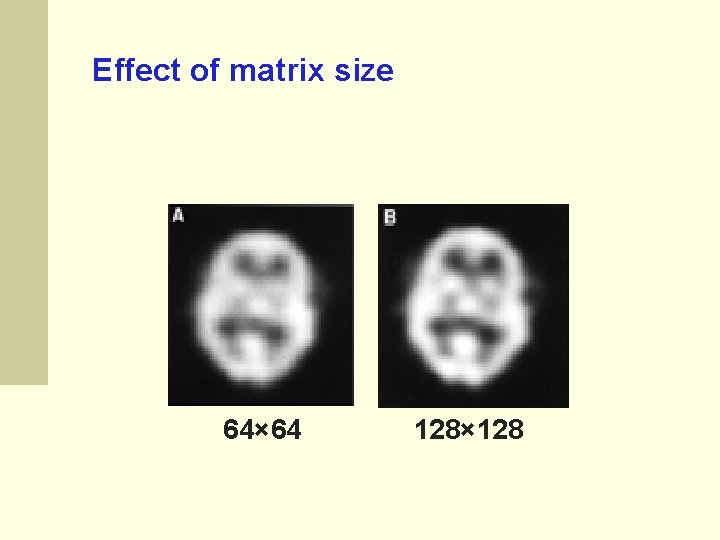
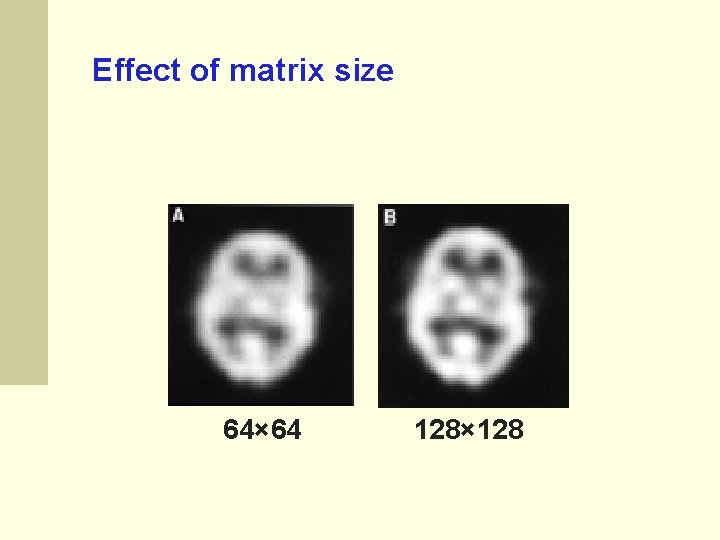
Effect of matrix size 64× 64 128× 128
Planar NM Imaging 2015 Nuclear Medicine Physics for Radiology Residents Sameer Tipnis, Ph. D, DABR
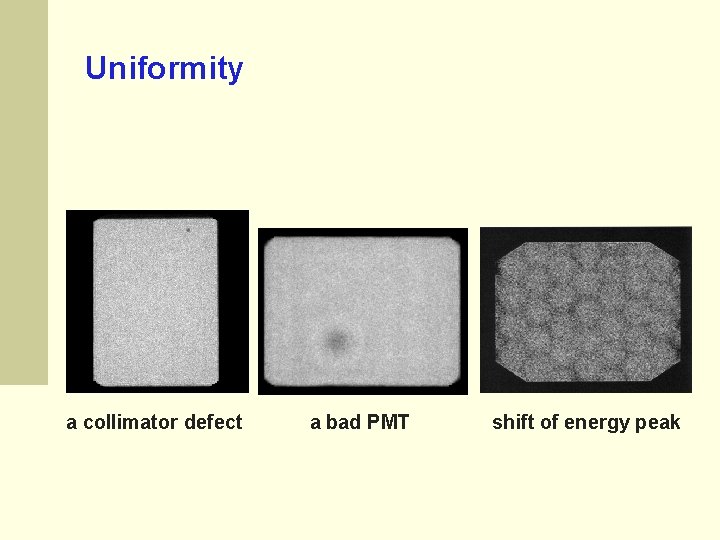
Quality control of gamma camera uniformity: daily, 256× 256, > 4 M counts resolution: weekly, 512× 512, > 4 M counts acquisition of new uniformity maps and possible energy map: quarterly, > 30 M counts
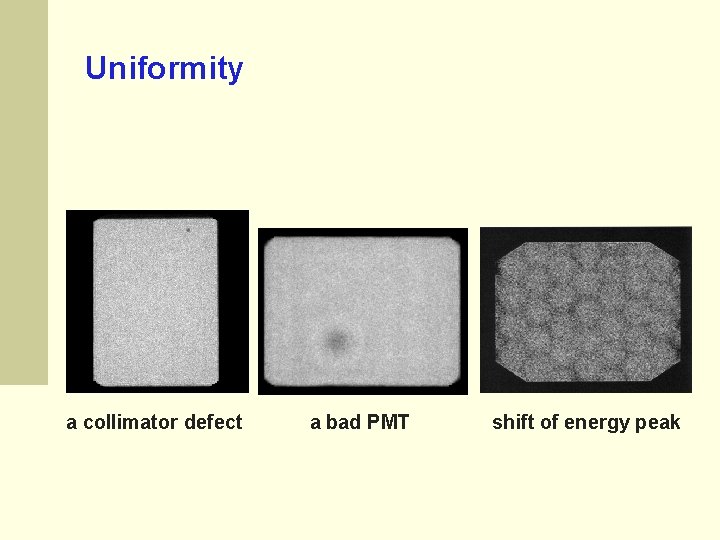
Uniformity a collimator defect a bad PMT shift of energy peak
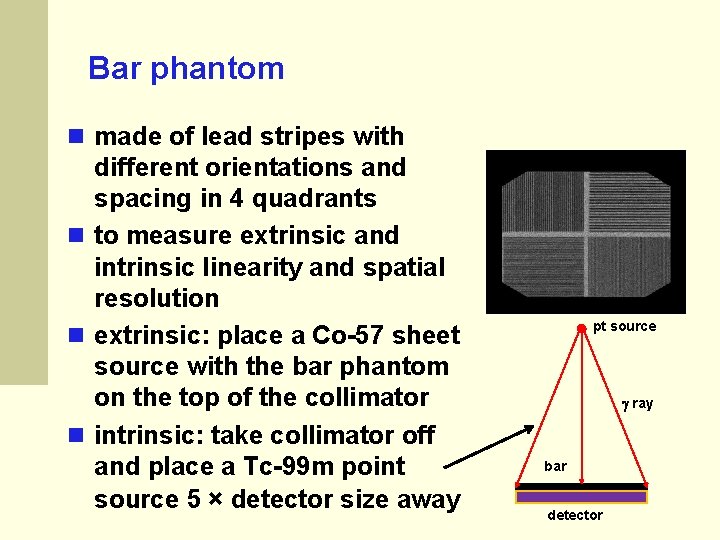
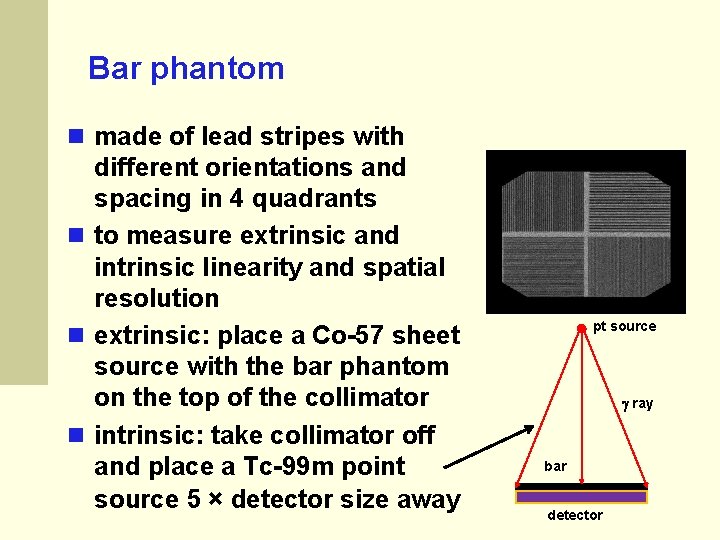
Bar phantom made of lead stripes with different orientations and spacing in 4 quadrants to measure extrinsic and intrinsic linearity and spatial resolution extrinsic: place a Co-57 sheet source with the bar phantom on the top of the collimator intrinsic: take collimator off and place a Tc-99 m point source 5 × detector size away pt source ray bar detector