Nuclear Medicine Introduction What is nuclear medicine The
- Slides: 14
Nuclear Medicine Introduction What is nuclear medicine? • The use of radioactive tracers (radiopharmaceuticals) to obtain diagnostic information [and for targeted radiotherapy]. • Radiation is emitted from inside the human body cf transmitted radiation in x ray imaging. Tracers : • Trace the paths of various biochemical molecules in our body. • Hence can obtain functional information about the bodies workings (i. e. physiology).
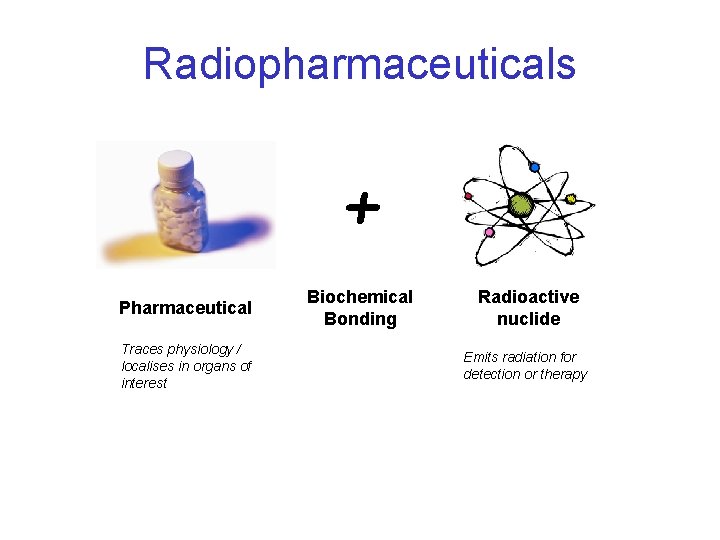
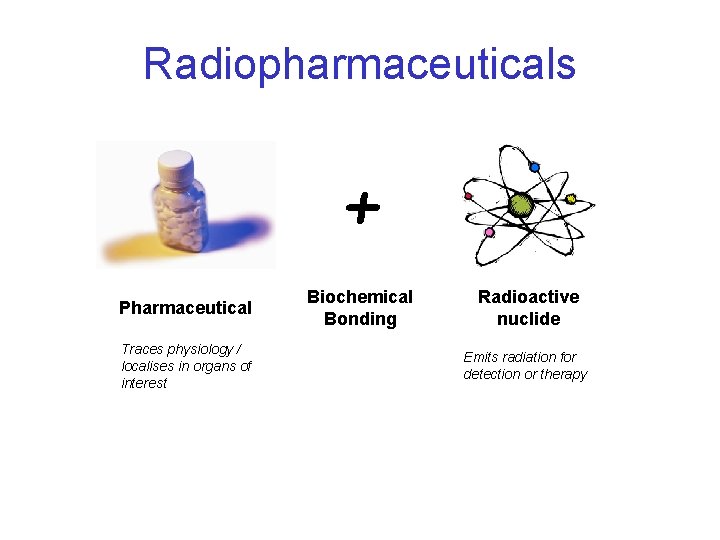
Radiopharmaceuticals + Pharmaceutical Traces physiology / localises in organs of interest Biochemical Bonding Radioactive nuclide Emits radiation for detection or therapy
The Pharmaceutical – The ideal tracer/pharmaceutical should follow only the specific pathways of interest, e. g. there is uptake of the tracer only in the organ of interest and nowhere else in the body. In reality this is never actually achieved. – Typically want no physiological response from the patient – The mechanism of localisation can be as simple as the physical trapping of particles or as sophisticated as an antigen antibody reaction
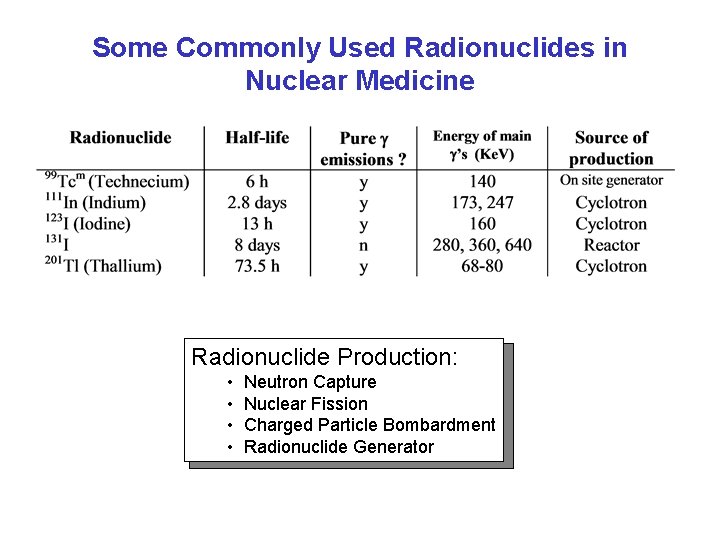
Radionuclides in Nuclear Medicine The ideal radionuclide for in vivo diagnosis : • Optimum half life – of same order as the length of the test (this minimises the radiation dose to the patient) • Pure gamma emitter – No alpha or beta particles, these do not leave the body so merely increase the radiation dose. • Optimum energy for emissions – High enough to exit the body but low enough to be easily detected. Useful range for gamma cameras is 50 500 ke. V (optimum ~ 150 ke. V). • Suitable for incorporating into a pharmaceutical without altering its biochemical behaviour • Readily and cheaply available on the hospital site.
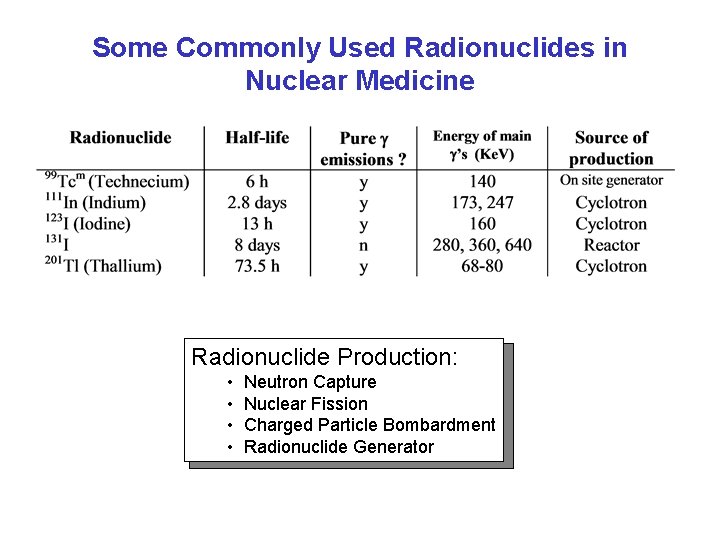
Some Commonly Used Radionuclides in Nuclear Medicine Radionuclide Production: • Neutron Capture • Nuclear Fission • Charged Particle Bombardment • Radionuclide Generator
Producing the Radiopharmaceutical kits • Most common radiopharmaceuticals are available as kits. These contain all the necessary freeze dried ingredients in an air tight vial, usually the pharmaceutical, a stannous compound and stabilizer. On addition of 99 Tcm 04 , the stannous reduces the 99 Tcm 0 , makes it charged and "sticky", and Tc forms a bond 4 with the pharmaceutical, labelling it. • For the longer half life isotopes, the full radiopharmaceutical can be obtained directly from the manufacturer, e. g. Se. HCAT labelled with 75 Se.
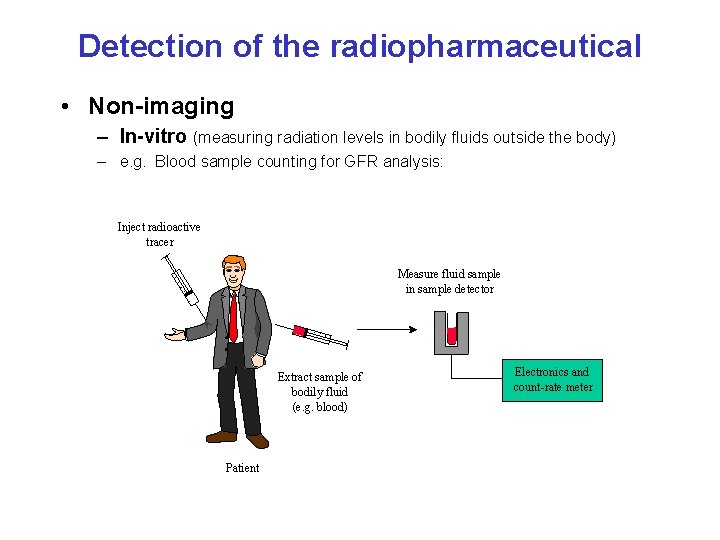
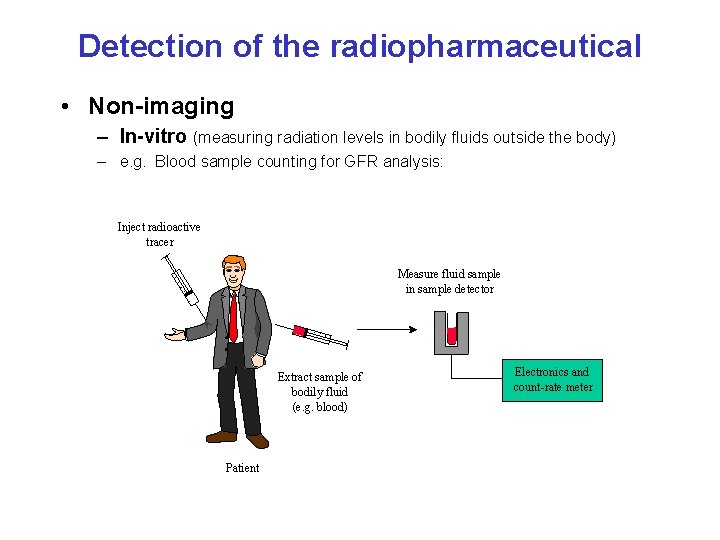
Detection of the radiopharmaceutical • Non-imaging – In-vitro (measuring radiation levels in bodily fluids outside the body) – e. g. Blood sample counting for GFR analysis: Inject radioactive tracer Measure fluid sample in sample detector Extract sample of bodily fluid (e. g. blood) Patient Electronics and count-rate meter
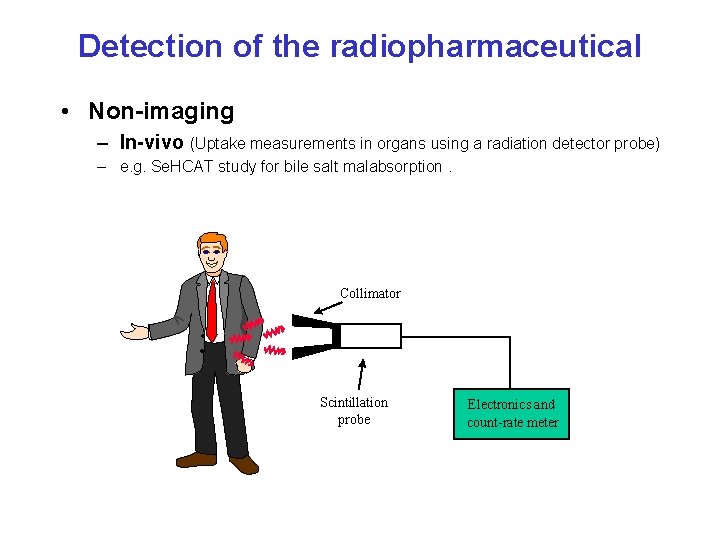
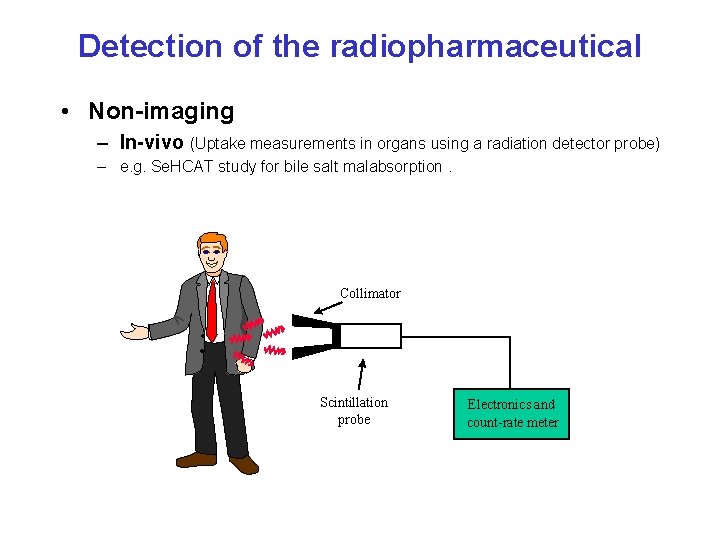
Detection of the radiopharmaceutical • Non-imaging – In-vivo (Uptake measurements in organs using a radiation detector probe) – e. g. Se. HCAT study for bile salt malabsorption. Collimator Scintillation probe Electronics and count-rate meter
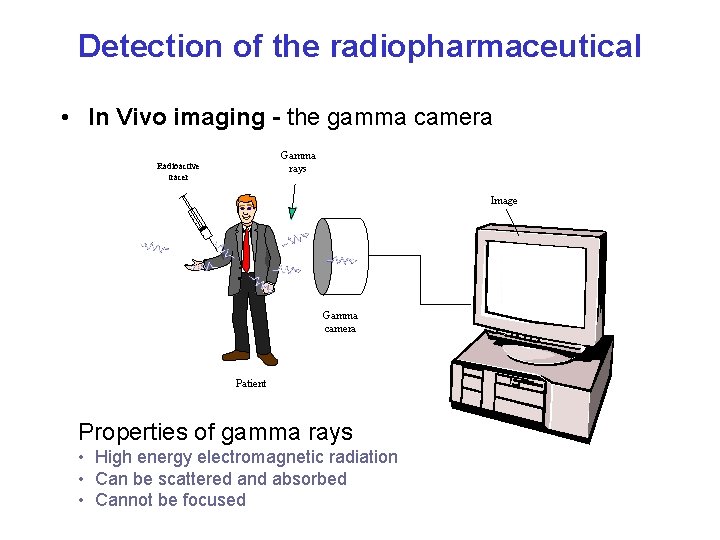
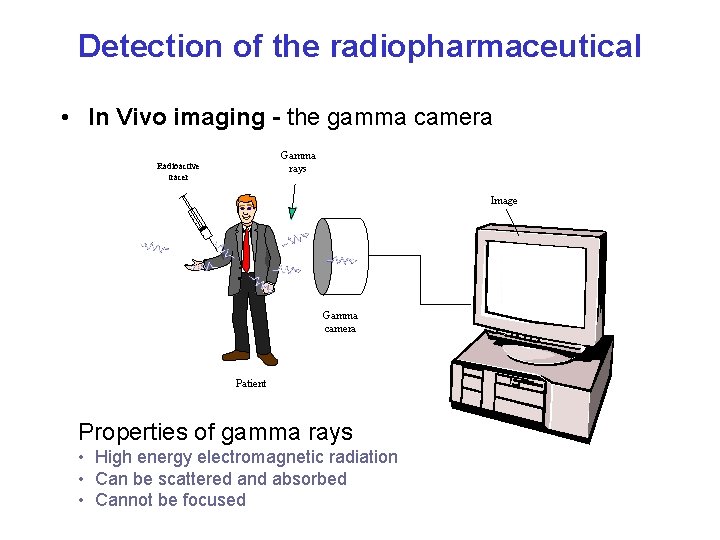
Detection of the radiopharmaceutical • In Vivo imaging - the gamma camera Gamma rays Radioactive tracer Image Gamma camera Patient Properties of gamma rays • High energy electromagnetic radiation • Can be scattered and absorbed • Cannot be focused
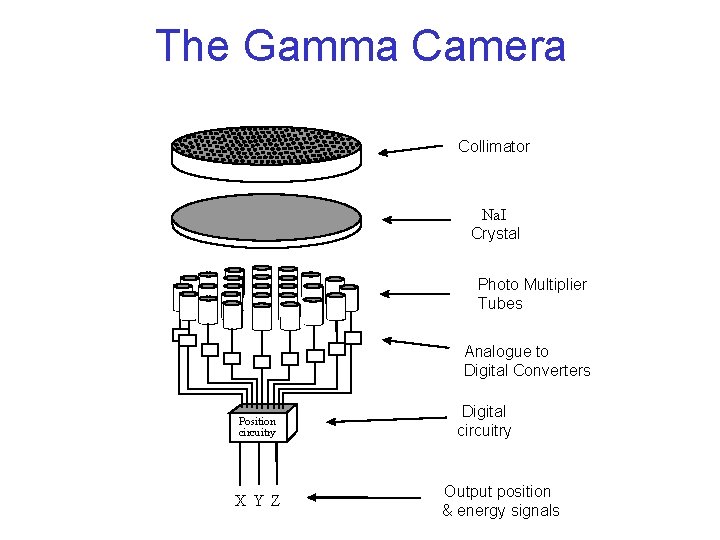
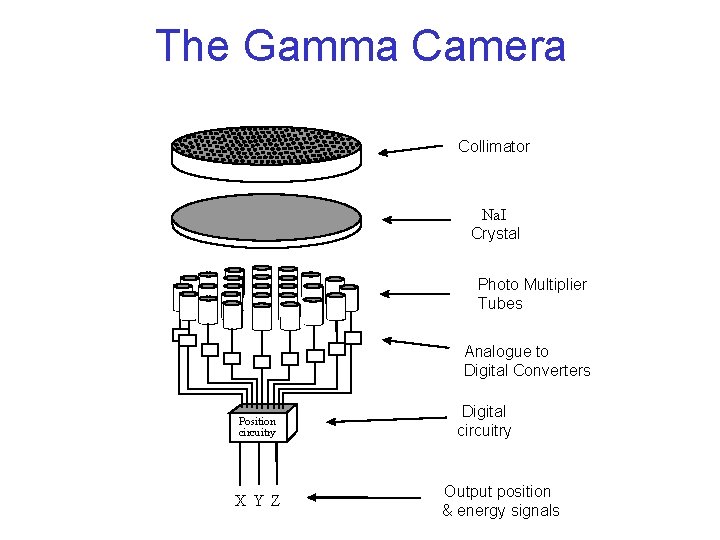
The Gamma Camera Collimator Na. I Crystal Photo Multiplier Tubes Analogue to Digital Converters Position circuitry X Y Z Digital circuitry Output position & energy signals
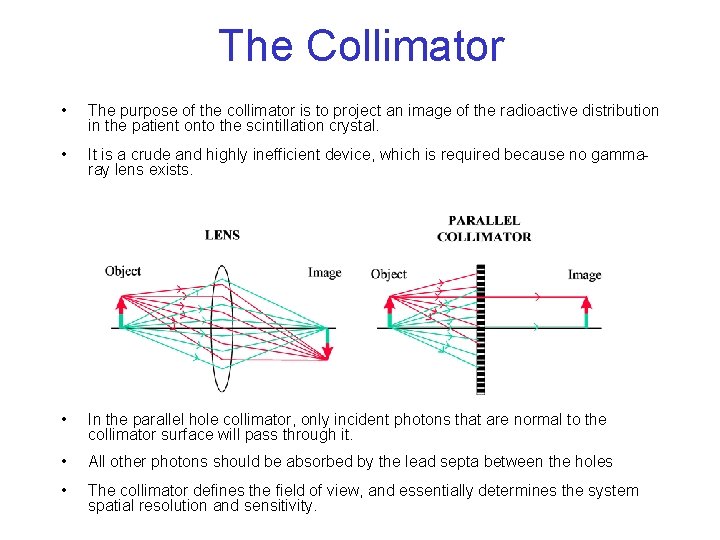
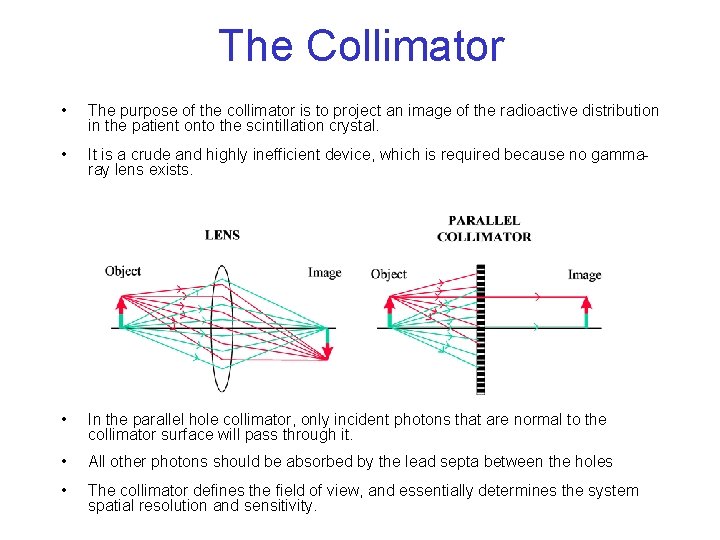
The Collimator • The purpose of the collimator is to project an image of the radioactive distribution in the patient onto the scintillation crystal. • It is a crude and highly inefficient device, which is required because no gamma ray lens exists. • In the parallel hole collimator, only incident photons that are normal to the collimator surface will pass through it. • All other photons should be absorbed by the lead septa between the holes • The collimator defines the field of view, and essentially determines the system spatial resolution and sensitivity.
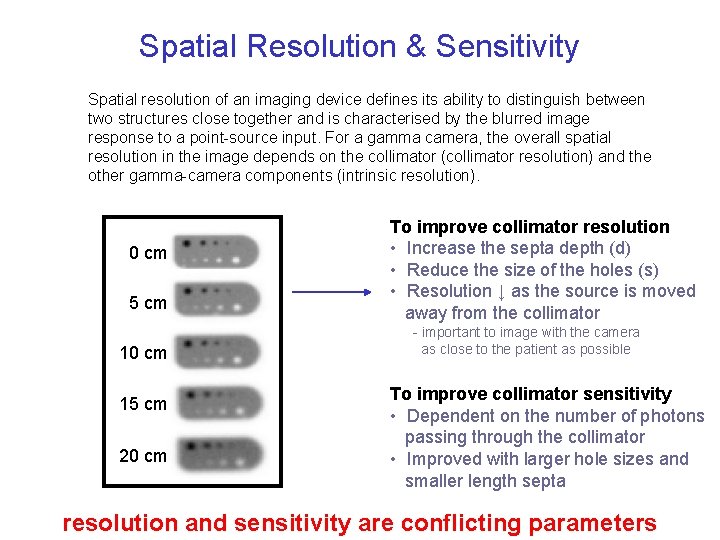
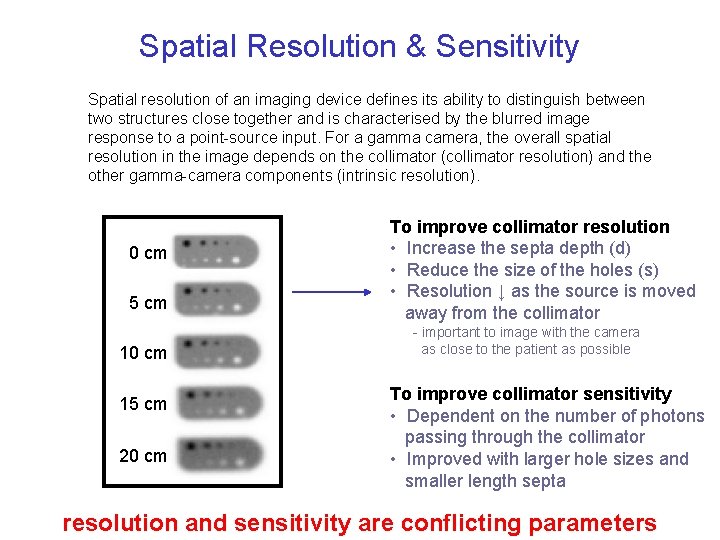
Spatial Resolution & Sensitivity Spatial resolution of an imaging device defines its ability to distinguish between two structures close together and is characterised by the blurred image response to a point source input. For a gamma camera, the overall spatial resolution in the image depends on the collimator (collimator resolution) and the other gamma camera components (intrinsic resolution). 0 cm Collimator Radioactive pt. source Output from collimator 5 cm important to image with the camera as close to the patient as possible 10 cm 15 cm s d Spatial distance 20 cm To improve collimator resolution • Increase the septa depth (d) • Reduce the size of the holes (s) • Resolution ↓ as the source is moved away from the collimator Spread of response to pt. source defines collimator resolution To improve collimator sensitivity • Dependent on the number of photons passing through the collimator • Improved with larger hole sizes and smaller length septa resolution and sensitivity are conflicting parameters
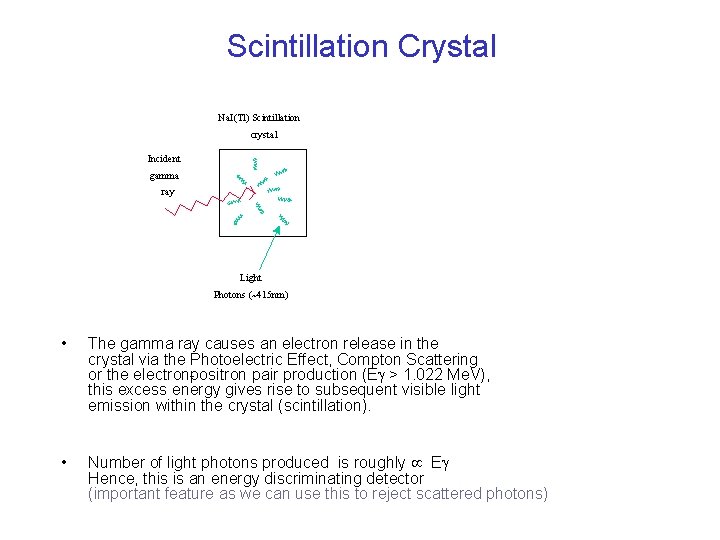
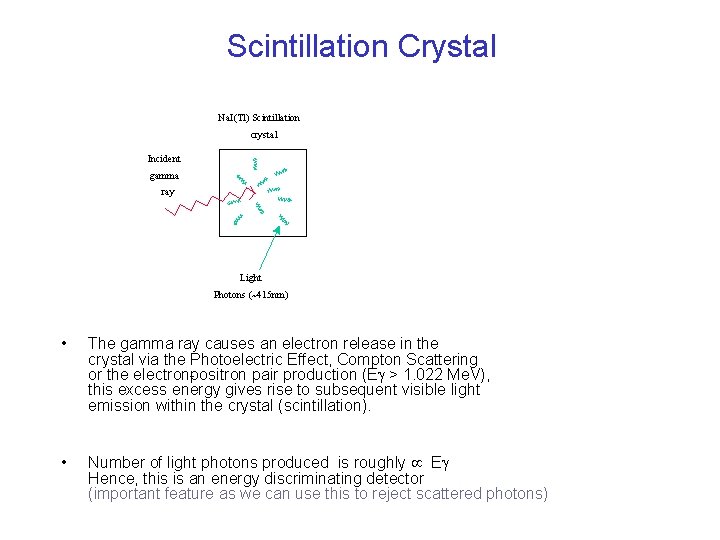
Scintillation Crystal Na. I(Tl) Scintillation crystal Incident gamma ray Light Photons (~415 nm) • The gamma ray causes an electron release in the crystal via the Photoelectric Effect, Compton Scattering or the electron positron pair production (E > 1. 022 Me. V), this excess energy gives rise to subsequent visible light emission within the crystal (scintillation). • Number of light photons produced is roughly E Hence, this is an energy discriminating detector (important feature as we can use this to reject scattered photons)
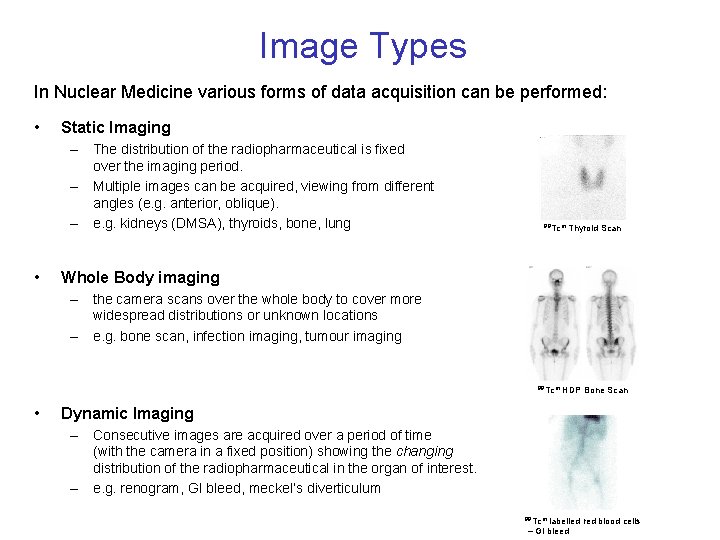
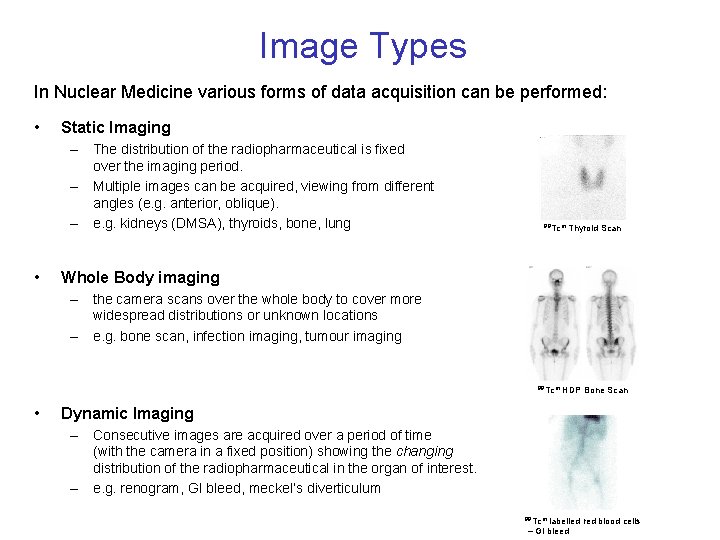
Image Types In Nuclear Medicine various forms of data acquisition can be performed: • Static Imaging – The distribution of the radiopharmaceutical is fixed over the imaging period. – Multiple images can be acquired, viewing from different angles (e. g. anterior, oblique). – e. g. kidneys (DMSA), thyroids, bone, lung • 99 Tcm Thyroid Scan Whole Body imaging – the camera scans over the whole body to cover more widespread distributions or unknown locations – e. g. bone scan, infection imaging, tumour imaging 99 Tcm HDP Bone Scan • Dynamic Imaging – Consecutive images are acquired over a period of time (with the camera in a fixed position) showing the changing distribution of the radiopharmaceutical in the organ of interest. – e. g. renogram, GI bleed, meckel’s diverticulum 99 Tcm labelled red blood cells – GI bleed