Nuclear Medicine Case Study Presentation Holdorf Introduction to
- Slides: 34
+ Nuclear Medicine Case Study Presentation Holdorf
+ Introduction to Nuclear Medicine n Nuclear Medicine is a branch of medical imaging that uses small amounts of radioactive material to diagnose or treat a variety of disease, including many types of cancers, heart disease and certain other abnormalities within the body.
+ Introduction Cont. n To image the scans radioactive materials called radiopharmaceuticals or radiotracers will be used. n Depending on the type of nuclear medicine exam, you go through the radiotracer which is injected into a vein, swallowed or inhaled as gas. n Ultimately radiotracers build up in the organ or area of your body being examined, where it gives off energy in the form of gamma rays. n This energy is detected by a device called a gamma camera, a positron emission tomography scanner or probe.
+ Introduction Cont. n These devices work together with a computer to measure the amount of radiotracer absorbed by your body and to produce special pictures offering details on both the structure and function of organs and tissues. n Nuclear medicine also offers therapeutic procedures such as radioactive iodine (I-131) therapy that uses radioactive material to treat cancer and other medical conditions affecting the thyroid gland. n When it is time for the imaging to begin, the gamma camera will take a series of images. The camera may rotate around you or move very close to your body. This is necessary to obtain the best quality images n Nuclear medicine can detect the radiation coming from inside a patient’s body, whereas other medical imaging patient is expose to radiation from outside the body
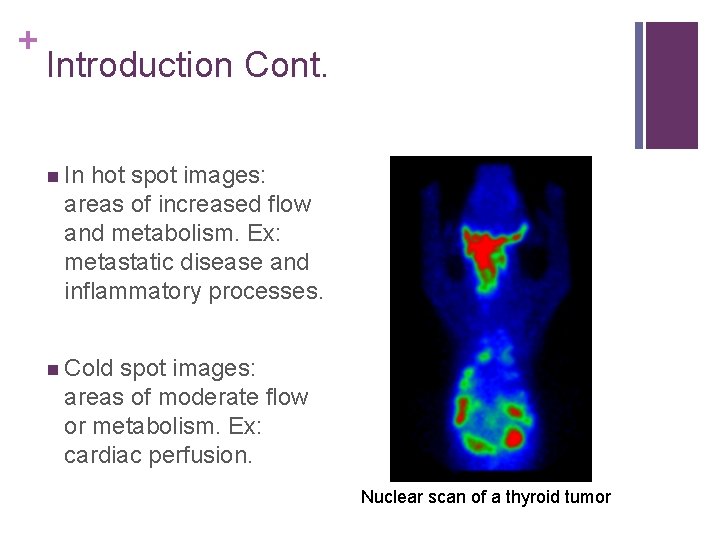
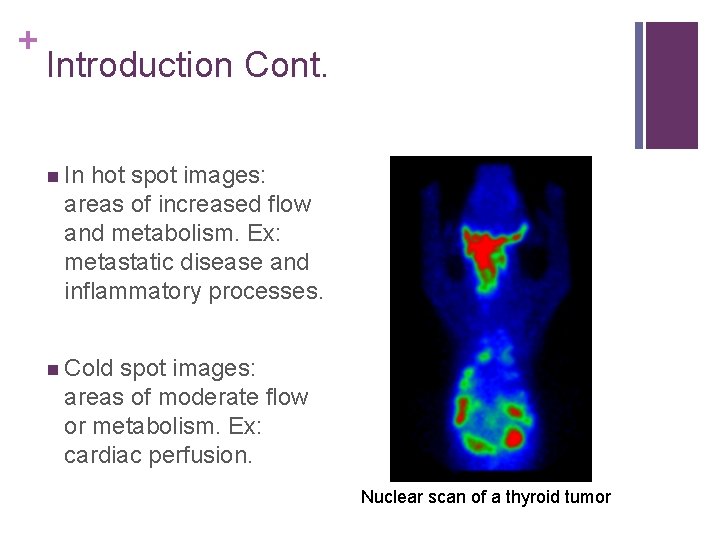
+ Introduction Cont. n In hot spot images: areas of increased flow and metabolism. Ex: metastatic disease and inflammatory processes. n Cold spot images: areas of moderate flow or metabolism. Ex: cardiac perfusion. Nuclear scan of a thyroid tumor
+ History of Nuclear Medicine n Nuclear medicine is a combination of many disciplines from chemistry to engineering, medicine and beyond. n Its exact date of discovery is unknown. It is approximated around 1935 - 1942 although discoveries date back to the late 1800’s. n In December of 1946 an article was published describing success in the treatment of thyroid cancer using radio iodine (I 131) which gained public recognition for nuclear medicine. n Extensive clinical use became prevalent in the early 1950’s.
+ History Cont. n The field of nuclear medicine grew rapidly during this time and the Society of Nuclear Medicine was formed in Spokane, Washington in 1954. n In 1971 the AMA officially recognized nuclear medicine as a specialty. n More recent developments in nuclear medicine include the PET (positron emission tomography scanner) and the SPECT (single photon emission computed tomography).
+ Evolution of Nuclear Medicine n In 1971 there were fewer radiopharmaceuticals available. n Many common procedures offered at that time are no longer part of a normal routine in a nuclear medicine clinic. n During this time period, the most common studies were brain scans, liver scans, bone scans, renal scans, lung scans, and thyroid scans. n Nuclear Medicine has evolved over time by using new procedures and agents and limiting the amount of older examinations.
+ Evolution Cont. n There are many useful agents that have come and gone over the past decade for ventilation imaging cerebral perfusion, lung perfusion, etc. n n Since the 1970 s, there have been many new major procedures and materials integrated into nuclear medicine. n n Many of these agents have been withdrawn from the market. Some of these include, myocardial perfusion imaging, fated bloodpool studies, labeled white blood cells, parathyroid imaging, etc. Another drastic transformation since the 1970 s is a change of instrumentation
+ Evolution Cont. n The first nuclear scanning device was the scintillation scanner, or dot scanner, developed in 1949 by Dr. Benedict Cassen at the University of California. n The scintillation counter detected radiation and counts were recorded by a tapper bar making black ink dots on a piece of paper. The amount of dots recorded in a given area was proportional to the amount of activity detected. It was most successful for scanning the thyroid gland because it lies just beneath the skin’s surface so scanning was minimal. For organs deeper in the body improvements in instrumentation had to be made.
+ Evolution Cont. n Today, doctors are able to choose from 3 basic devices for nuclear imaging: gamma ray camera, the SPECT scanner, and the PET scanner. n The gamma ray camera combines radionuclide and computer technology. When a radionuclide has been delivered inside a patient’s body, the gamma ray emissions from it can be detected by the gamma ray camera. n When the amount of radionuclide absorbed into an organ has been discovered, a doctor is able to determine if that organ is overactive, underactive, or normal. This will significantly affect treatment.
+ Evolution Cont. n The SPECT (Single Photon Emission Computer Tomography) scanner is a ring of gamma cameras that rotate around the patient. It takes many closely spaced pictures of the interior of a patient’s body in a series of slices. When combined, a computer is able to put together a 3 -D image. n n This is most useful with heart attacks and showing how much muscle damage has occurred. The PET (Positron Emission Tomography) scanner is the most technically advanced nuclear imaging device. n These are more efficient because the device allows them to view chemical and biological processes of the body in motion pictures.
+ Evolution Cont. n As far as training is concerned, originally training programs were not regulated and the amount of education received in programs varied. n Then the American Board of Nuclear Medicine (ABNM) was established and people were able to sit for examination and become certified as a physician who had interest and experience with nuclear medicine. n “The initial board eligibility criteria were as follows: an internship and 10 years of experience in nuclear medicine; an internship, 1 year of an approved residency in internal medicine, pathology, or radiology, and 5 years of experience in nuclear medicine; certification by an American specialty board plus 1 year of training in nuclear medicine or 3 years of experience in nuclear medicine; or an internship plus 1 year of residency and 2 years of training in nuclear medicine. In the first 5 years, 2, 800 physicians became board certified by the ABNM”
+ Evolution Cont. n The biggest change in nuclear medicine in the future will be the incorporation of molecular imaging. n n Even though nuclear medicine already consists of molecular imaging, there will be new training and practices that will include “metabolism, receptor-targeted agents, reporter genes, apoptosis, hypoxia, and probably other areas not yet envisioned. ” There still needs to be a lot of research and clinical studies performed in order for this to happen. n The integration of molecular imaging opens up a specialty in nuclear medicine that will be a major medical practice in the foreseeable future.
+ Radiation Exposure n Nuclear Medicine Technicians work with radionuclides which are also known as radioisotopes, markers, or tracers. n Some of their radioactive materials occur naturally in nature, such as radium. n n However, most of them are made artificially in atomic reactors. They work by giving off a type of radiation known as gamma rays. They are similar to X rays but have no mass. n An important difference is that gamma rays give off natural and artificial radioactive materials whereas X rays are generated by a machine.
+ Benefits vs. Risks Benefits n The information provided by nuclear medicine examinations is unique and often unattainable using other imaging procedures. n For many diseases, nuclear medicine scans give the most useful information needed to make a diagnosis or to determine appropriate treatment. n Nuclear medicine is less expensive and may construct more precise information than other types of surgery. n n n Detection of abnormalities early in the progression of a disease, which means prompt treatment and more successful outcomes Provides information before the condition is apparent with other diagnostic tests Offers procedures that are helpful to a broad span of medical specialties, from pediatrics to cardiology to psychiatry
+ Benefits vs. Risks Cont. Risks n The greatest potential risk from a procedure using radiation is the development of cancer. However, there is no evidence that a diagnostic medical procedure, like a nuclear medicine exam, has ever caused cancer. n Doses of radiotracer administered are small so diagnostic nuclear medicine procedures result in low radiation exposure, acceptable for diagnostic exams. So, the radiation risk is very low compared with the potential benefits. n Nuclear medicine diagnostic procedures have been used for more than five decades, and there are no known long-term adverse effects from such low-dose exposure.
+ Benefits vs. Risks Cont. n Allergic reactions to radio pharmaceuticals may occur but are extremely rare and are usually mild. n Injection of the radiotracer may cause slight pain and redness, which should rapidly resolve. n Women should always inform their physician or radiology technologist if there is any possibility that they are pregnant or if they are breastfeeding their baby due to safety issues
+ How Nuclear Medicine relates to Ultrasound n Nuclear medicine addresses the body’s physiological processes rather than the anatomical structures like in Ultrasound. n Ultrasound is more cost effective and can rapidly evaluate and diagnose abnormalities throughout clinical medicine. n Both Nuclear Medicine and Ultrasound are non-invasive techniques. n Both use imaging as a way of seeing inside the human body, but Nuclear Medicine requires radioactive materials and Ultrasound does not.
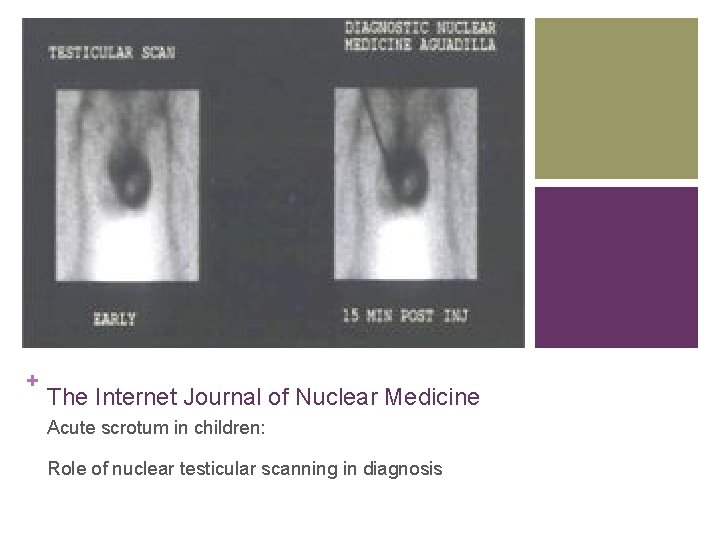
+ The Internet Journal of Nuclear Medicine Acute scrotum in children: Role of nuclear testicular scanning in diagnosis
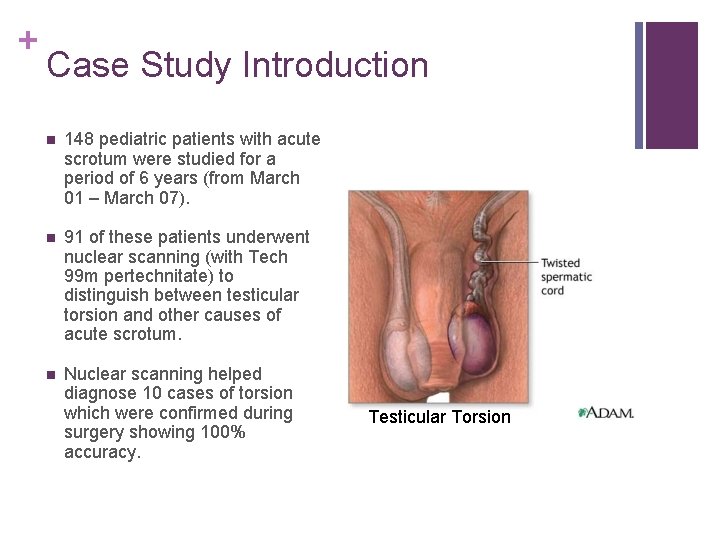
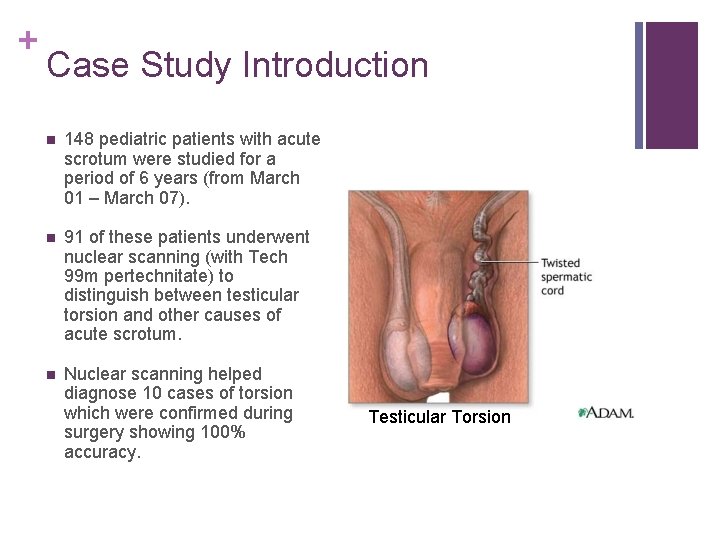
+ Case Study Introduction n 148 pediatric patients with acute scrotum were studied for a period of 6 years (from March 01 – March 07). n 91 of these patients underwent nuclear scanning (with Tech 99 m pertechnitate) to distinguish between testicular torsion and other causes of acute scrotum. n Nuclear scanning helped diagnose 10 cases of torsion which were confirmed during surgery showing 100% accuracy. Testicular Torsion
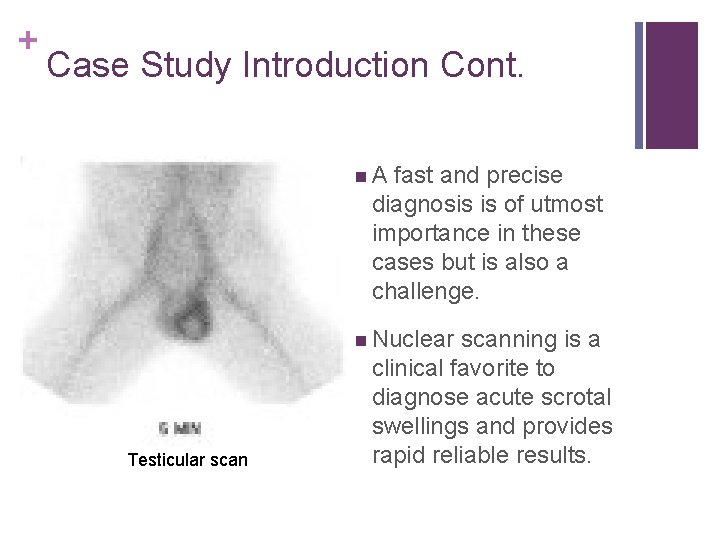
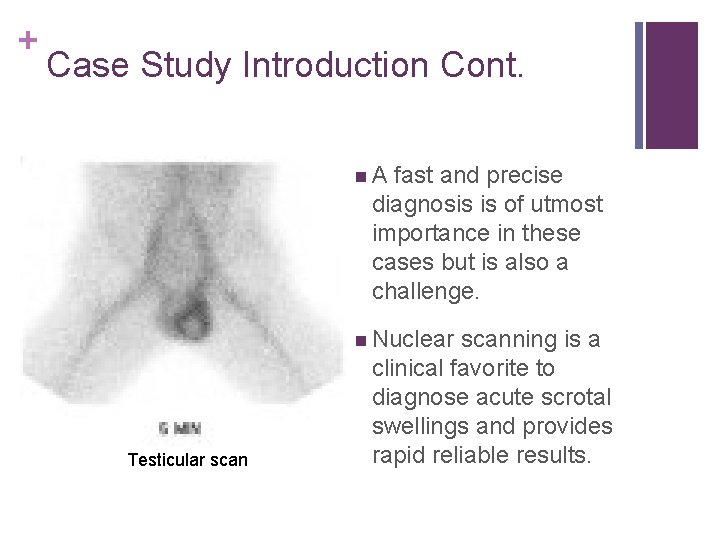
+ Case Study Introduction Cont. n A fast and precise diagnosis is of utmost importance in these cases but is also a challenge. n Nuclear scanning is a Testicular scan clinical favorite to diagnose acute scrotal swellings and provides rapid reliable results.
+ Case Study Materials & Methods n The study was conducted over a period of six years with patients in an age group of 0 – 13 years. n Patients were given a form of a nuclear isomer Tc 99 m orally about two hours before the procedure. n It is usually used as a radioactive tracer in the body. n Gamma cameras were placed in proper areas of the scrotum for each person to establish images to check for testicular torsion. n There were high rates of accuracy by applying these techniques distinguishing testicular torsion from other abnormalities.
+ Case Study Results n n 148 patients studied over a sixyear study period: only 38 patients were subjected to surgical intervention. n 4 patients had missed torsion n 6 patients had hematocele n 11 patients had idiopathic scrotal edema n 88 patients had non-specific scrotal pain and swelling n 1 patients had epididymoorchitis Mean age of patients was 5. 3 years (range 1 – 15) n 27 patients had torsion of testis n 10 patients had incarcerated inguino (scrotal hernia) n 110 patients were managed conservatively
+ Case Study Results Cont. n Ultrasonography was performed on 3 patients with clinical picture of torsion, all of which was reported as normal; however on scrotal exploration all the three patients were found to have torsion; indicating positive predictive value of zero percent for scrotal ultrasonography. n Doppler scan was performed on 4 patients with clinical picture of torsion of testis and torsion was reported in only one patient. On surgical exploration all the four patients had torsion of testis giving a predictive value of 25%.
+ Case Study Results Cont. Nuclear testicular scan was performed on 91 patients. n Out of these 91 patients, 5 patients had clinical picture of torsion n 5 had clinical picture of epididymoorchitis, testicular scan revealed missed torsion of testicle in 4 patients and epididymoorchitits in 1 patient. n 15 had suspicion of torsion, 6 were found to have torsion on nuclear scan, subsequently confirmed on exploration and 9 had a normal scan. n 69 patients presented with an equivocal clinical picture, 5 were found to have underlying torsion, 64 had a normal testicular scan and were managed conservatively.
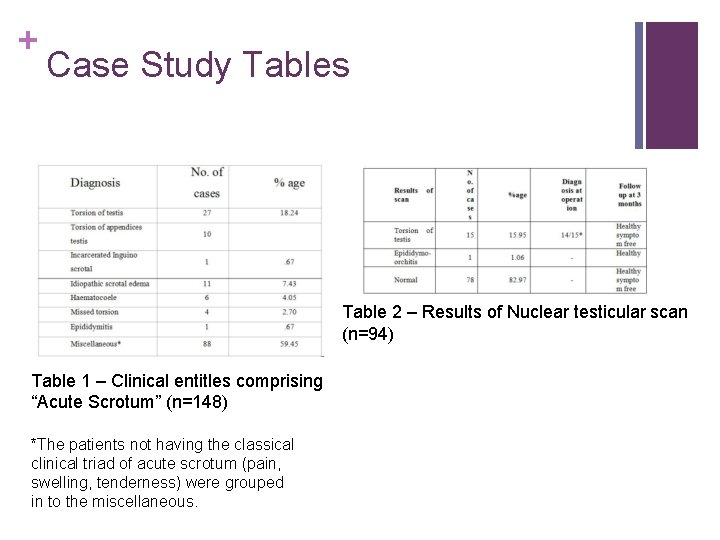
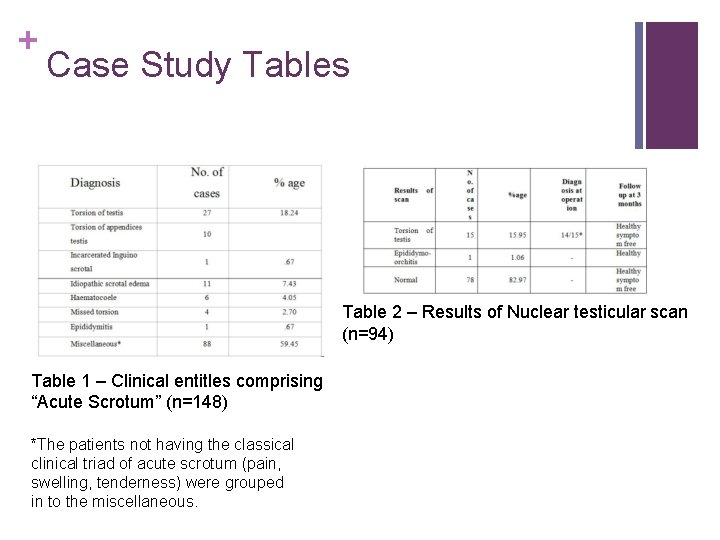
+ Case Study Tables Table 2 – Results of Nuclear testicular scan (n=94) Table 1 – Clinical entitles comprising “Acute Scrotum” (n=148) *The patients not having the classical clinical triad of acute scrotum (pain, swelling, tenderness) were grouped in to the miscellaneous.
+ Case Study Discussion n Doppler scanning was not a valuable tool for evaluation of the patient with acute scrotum because it is significantly more difficult with children and consequently does not give accurate results. n In the sample study the majority of patients were adults and the size of the tests are larger in adult patients. n Furthermore, adult patients are more cooperative whereas young boys are difficult to work with and the sizes of the testes are smaller limiting the study. n Therefore, the scans were giving high false negative rates in boys.
+ Case Study Discussion Cont. n. Three patients had scrotal ultrasounds performed with clinical picture of testicular torsion. n. However, all three patients were unable to have documentation of the torsion. Therefore, the use of ultrasounds is not considered beneficial in distinguishing torsion.
+ Case Study Discussion Cont. n Testicular scanning with technetium 99 m (Tc 99 m) was performed on 91 patients. n 5 patients had unequivocal clinical pictures of torsion of testes, and after scanning all 5 patients had the same diagnosis revealed and scrotal exploration took place n n After exploration one patient had a confirmed scan and the other 4 had findings of a missed torsion. 15 patents had clinical suspicion of testicular torsion n Of these 15 patients, 6 were found to have testicular torsion and 9 had normal scans. n 3 patients had a clinical picture of epididymoorchitis. n 68 patients had equivocal clinical picture.
+ Case Study Discussion Cont. n Patients with normal scans were managed conservatively and saved from surgical exploration. n After 3 weeks, patients were rescanned and follow up scans were reported as normal. n It is believed that nuclear testicular scanning is helpful in evaluating acute scrotum in pediatric patients and helps to determine which patients need surgical intervention. n However, it is also said that nuclear scanning should only be used where the clinical diagnosis is doubtful.
+ Case Study Conclusion n The most common clinical article leading to acute scrotum in children are testicular torsion and torsion of appendices of testis, where as epididymoorchitis is rare in pediatric age group. n Imaging modalities like scrotal USG and Doppler scanning are not helpful in pediatric patients with acute scrotum to confirm or exclude underlying testicular torsion. n Nuclear testicular scintigraphy is the investigation of choice to confirm or exclude testicular torsion in pediatric patients with acute scrotum, especially in patients with oblique clinical picture
+ Works Cited nhttp: //www. medhunters. com/articles/his tory. Of. Nuclear. Medicine. html nhttp: //www. lbl. gov/Science- Articles/Archive/nuclear-medhistory. html n. The Internet Journal of Nuclear Medicine ISSN: 1539 -4638
+ Resources n Graham, Michael M. , and Darlene F. Metter. "Evolution of Nuclear Medicine Training: Past, Present, and Future. " Journal of Nuclear Medicine 48. 2 (2007): 257 -268. Web. 4 Jun 2010. <http: //jnm. snmjournals. org/cgi/content/full/4 8/2/257>. n Murphy, Wendy, and Jack Murphy. Nuclear Medicine. Chelsea House Pub, 1993. Print.