NSTEMI Pathway Education for Nurses Objectives Demonstrate an

NSTEMI Pathway Education for Nurses
Objectives • Demonstrate an understanding of the NSTEMI clinical pathway. • Understand the importance of early and consistent education throughout hospital stay. • Demonstrate the knowledge of the educational material and where to access the material. • Understand the discharge criteria including follow-up appointment and supply of medications for home.
What is the NSTEMI Pathway • An evidence based, streamlined approach to NSTEMI patient management starting when a patient enters the system through the ED and continues to post discharge. • The focus is on early treatment and diagnosis including: troponins, medications, interventions if necessary, and focused education. • Each patient that meets the criteria for an NSTEMI will be placed on the clinical pathway through the acute admission. • The Cardio Chest Pain/ MI Admission Power Plan MD 5712 has been optimized to support the pathway roll out. – Pathway NSTEMI will be checked on the order set. It will also appear in the problem list in power chart. • The orders and educational materials for these patients are standardized.
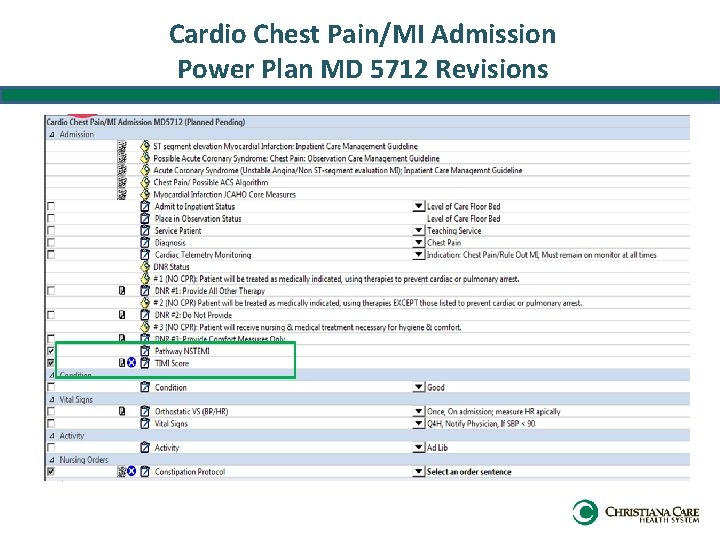
Cardio Chest Pain/MI Admission Power Plan MD 5712 Revisions
What is my role as the nurse in this pathway? • Early and consistent education! • Patient advisors made it clear: – Too much information is provided in a short period of time – Patients need time to understand accept the diagnosis of a heart attack – Major lifestyle changes are hard to comprehend in the acute hospital stay – Patients want to know the essentials to keep them safe upon discharge • Focus is on providing the essentials of diagnosis, procedures, medications, and follow up with secondary prevention. • Cardiac rehab will reinforce lifestyle changes such as: – – Weight loss Dietary Changes Smoking Cessation Lifestyle Modifications

NSTEMI Clinical Pathway

What is my role as the nurse in this pathway? • You will know if your patient is on the NSTEMI pathway by: – Checking off the order to place the patient on the pathway – Checking the Problems/Diagnosis List – Checking the Non-categorized orders for NSTEMI pathway • Provide the education listed under Psychosocial Support/Education on the NSTEMI Clinical Pathway Form for each day. • Document the education you provide as well as the patient comprehension of the teaching on the back of the Supplemental Plan of Care-Ineffective Tissue Perfusion Cardiopulmonary Percutaneous Intervention. • Eventually this flowsheet will be available in I-View. • Partner with Pharmacy and Case Management to obtain new AMI medications prior to discharge where applicable.
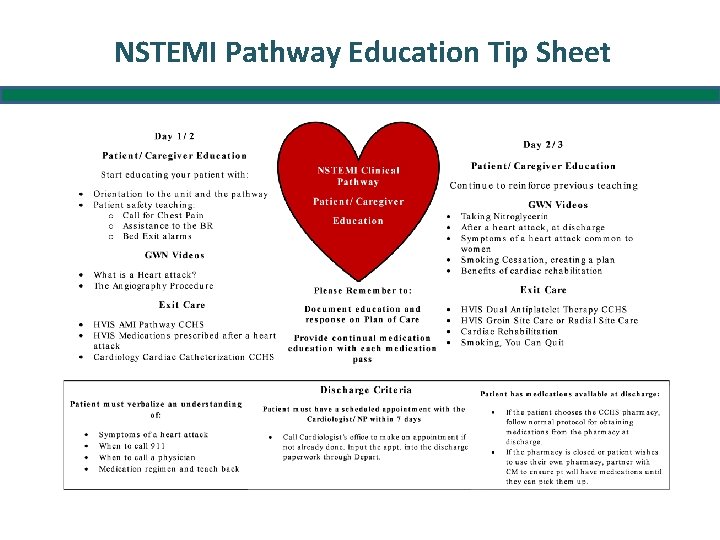
NSTEMI Pathway Education Tip Sheet
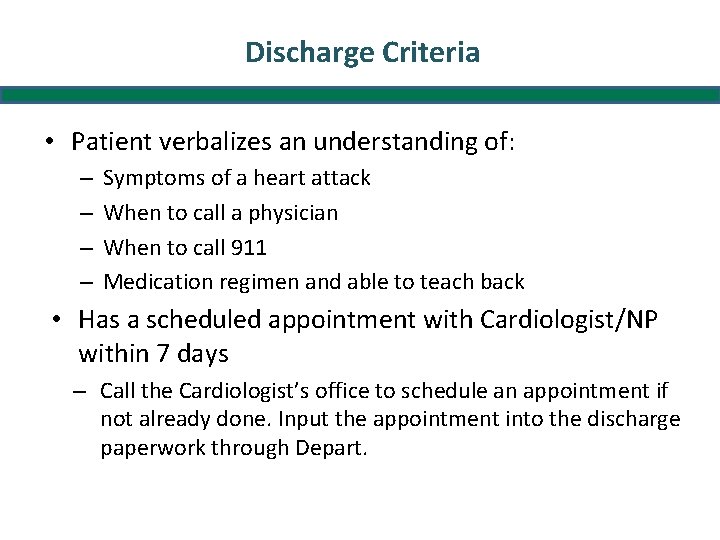
Discharge Criteria • Patient verbalizes an understanding of: – – Symptoms of a heart attack When to call a physician When to call 911 Medication regimen and able to teach back • Has a scheduled appointment with Cardiologist/NP within 7 days – Call the Cardiologist’s office to schedule an appointment if not already done. Input the appointment into the discharge paperwork through Depart.
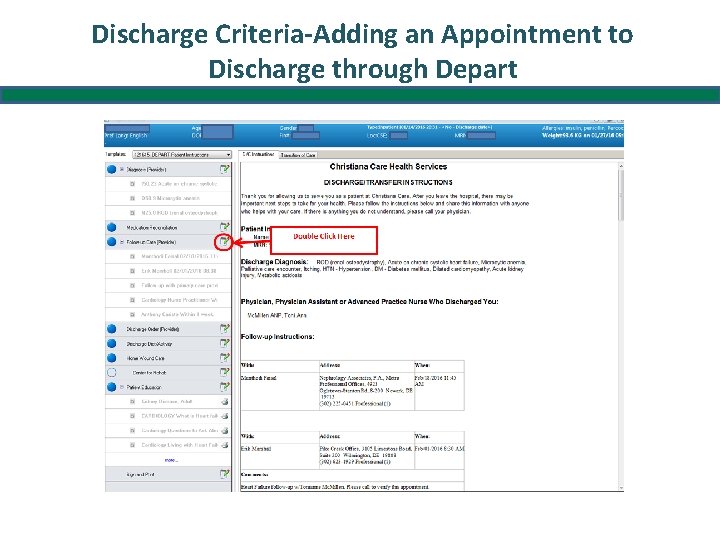
Discharge Criteria-Adding an Appointment to Discharge through Depart
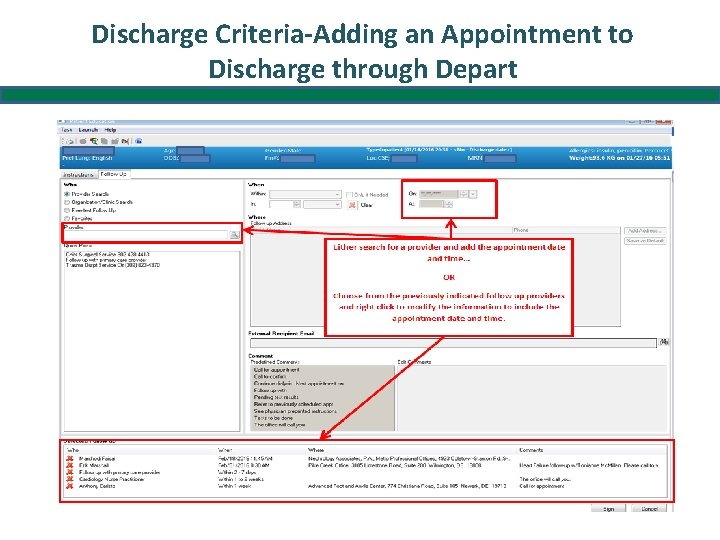
Discharge Criteria-Adding an Appointment to Discharge through Depart
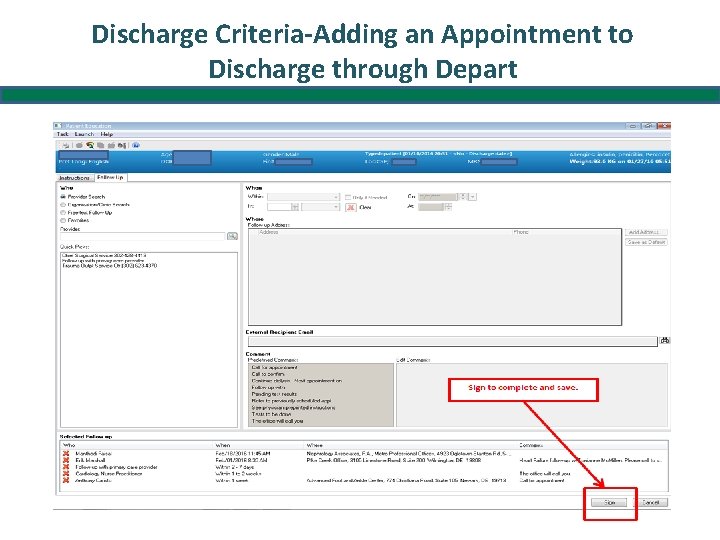
Discharge Criteria-Adding an Appointment to Discharge through Depart
Discharging with Medications • If the patient chooses to use CCHS’s pharmacy: – RN sends Pharmacy Discharge Program Form (“Purple Sheet”) to Pharmacy – RN Confirms meds are ready for pick up at pharmacy • Patient can have family member obtain meds from pharmacy OR • Upon discharge, RN can direct escort to take patient to pharmacy for med pick up • If the patient wishes to use their own pharmacy or CCHS pharmacy is closed: – Case Management and RN should partner to ensure scripts are sent to pharmacy and patient can bridge the gap between discharge and prescription pick up. – Inpatient pharmacy is able to bridge medications with a physician’s order.
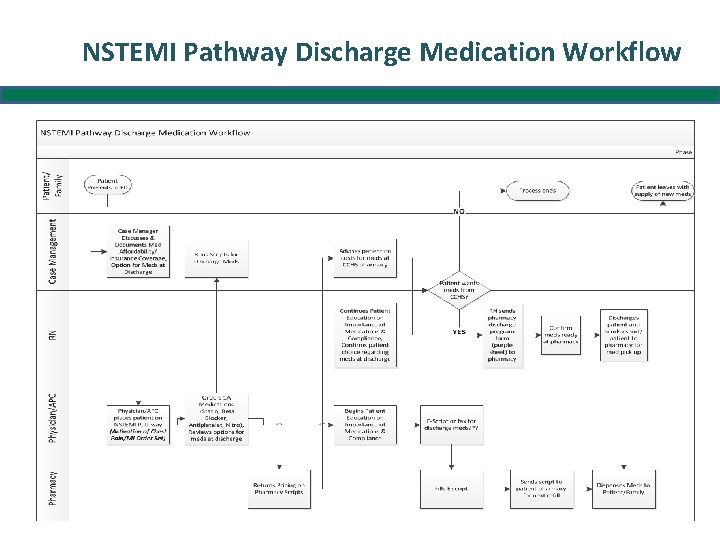
NSTEMI Pathway Discharge Medication Workflow
Thank you! • The pathways will help us to streamline and provide consistent, patient focused care to a critical patient population. – It will promote efficient use of resources that reduces unnecessary variation and costs of care. – It maximizes the value of care and treatment by formally integrating best practices and evidence based guidelines to support team based care delivery. • We will continue to learn and adapt the pathways as needed to support continual process improvements. • Your feedback is welcome!
- Slides: 16