NRP Neonatal Resuscitation program Bill keenan Father of
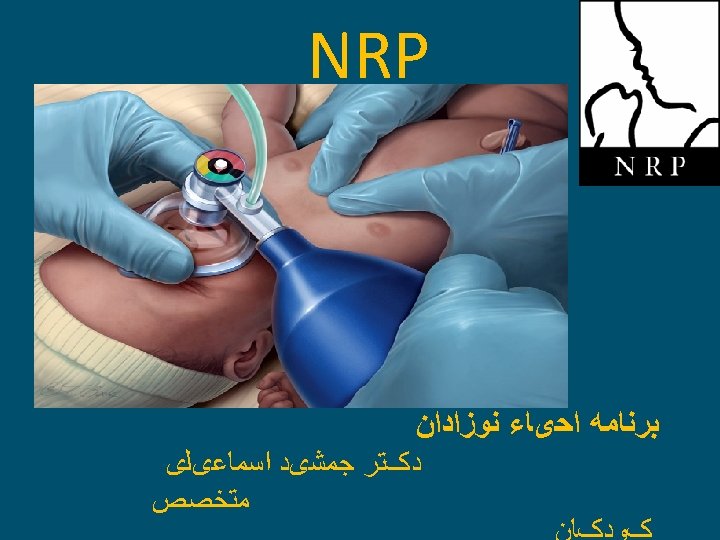
• NRP • Neonatal Resuscitation program ● ﻮﺯﺍﺩﺍﻥ
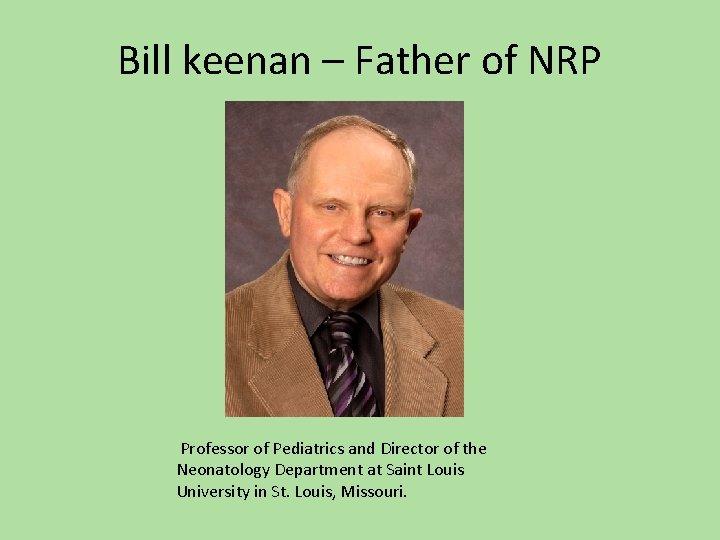
Bill keenan – Father of NRP Professor of Pediatrics and Director of the Neonatology Department at Saint Louis University in St. Louis, Missouri.
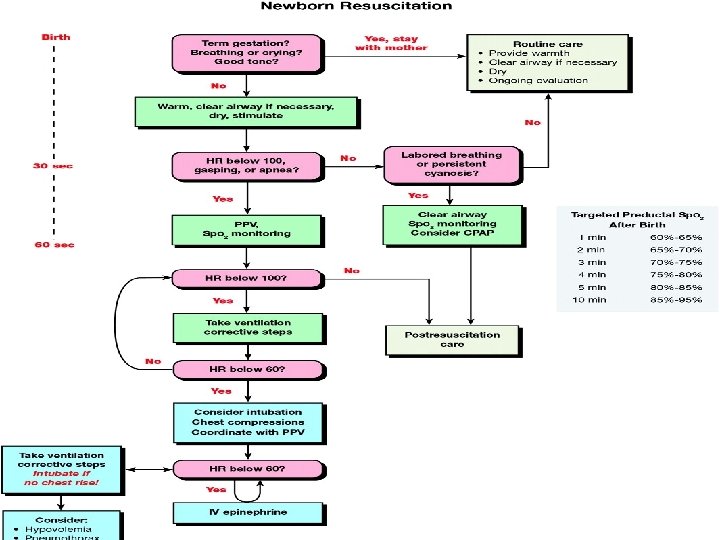
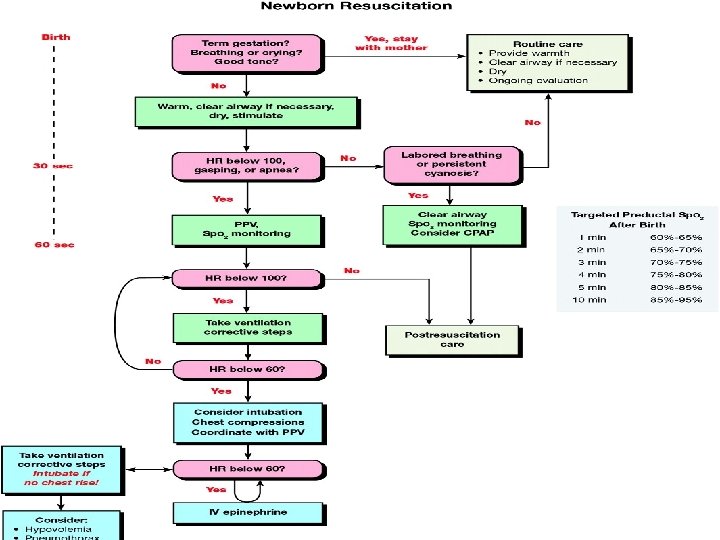
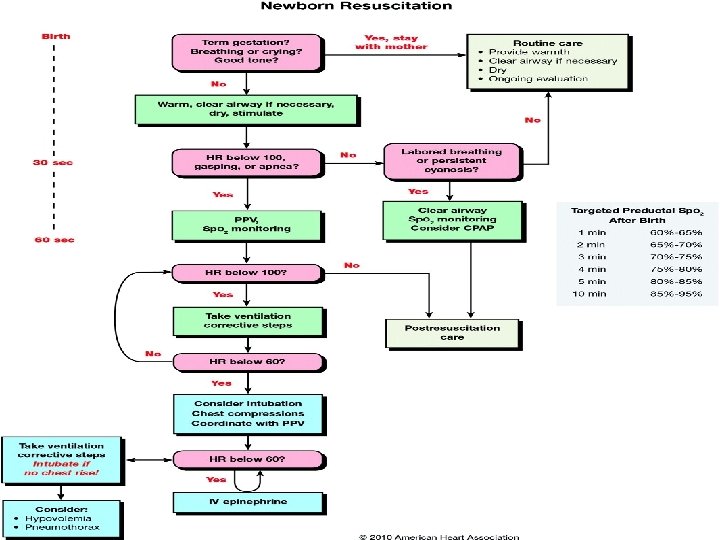
FACTS • 90% Don’t require any intervention • 10% require intervention • 1 % need major resuscitation • Preterms are at high risk
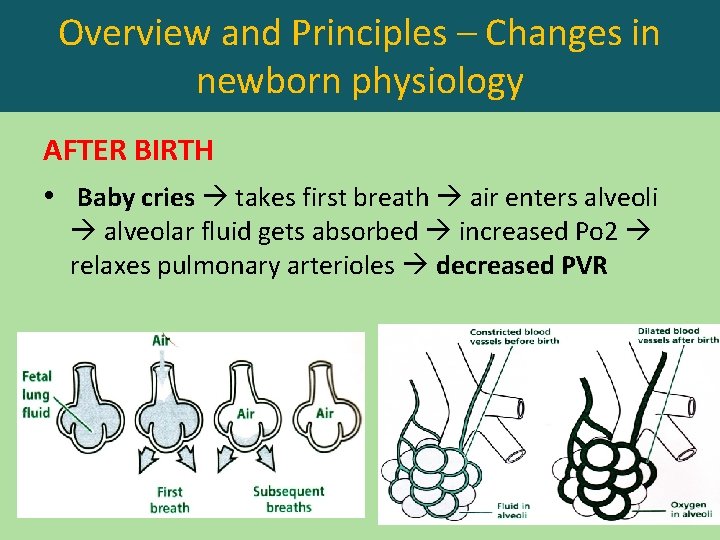
Overview and Principles – Changes in newborn physiology AFTER BIRTH • Baby cries takes first breath air enters alveoli alveolar fluid gets absorbed increased Po 2 relaxes pulmonary arterioles decreased PVR



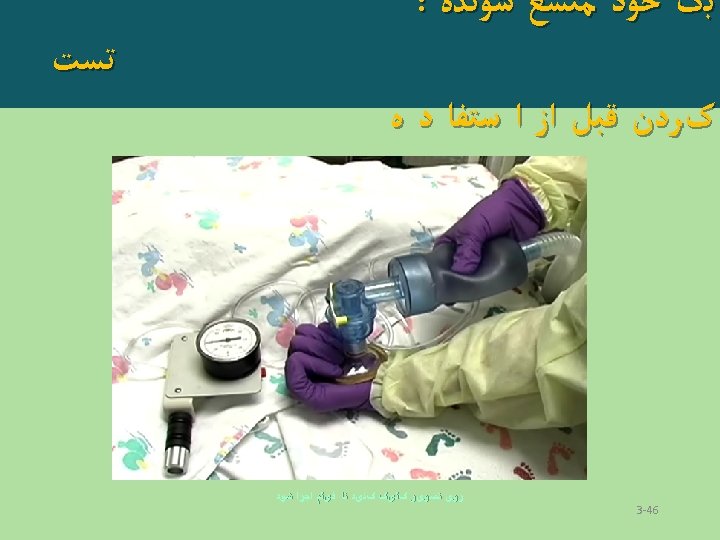
Safety features Pop-up valve
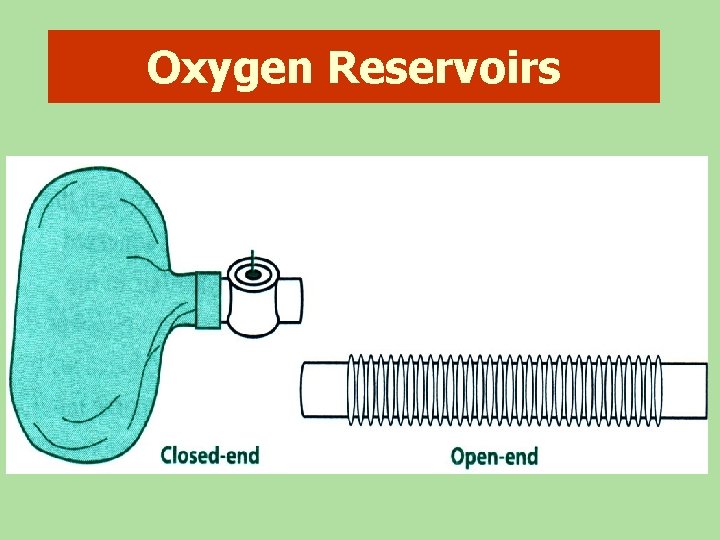
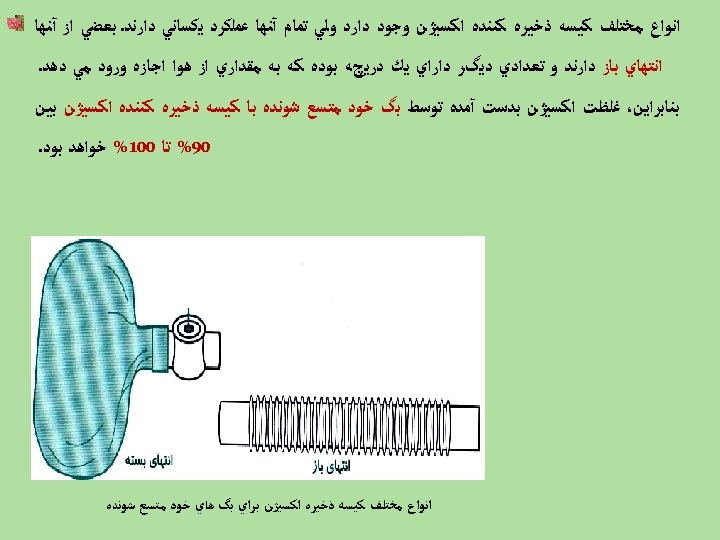
Oxygen Reservoirs


Intubation equipment
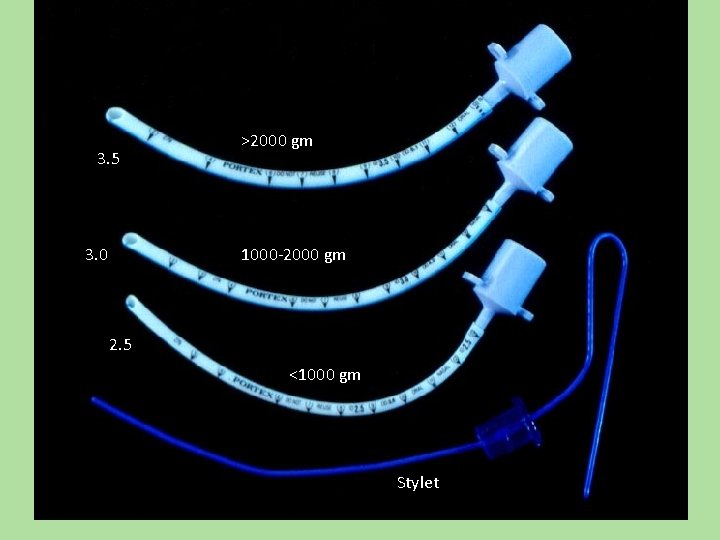
3. 5 3. 0 >2000 gm 1000 -2000 gm 2. 5 <1000 gm Stylet

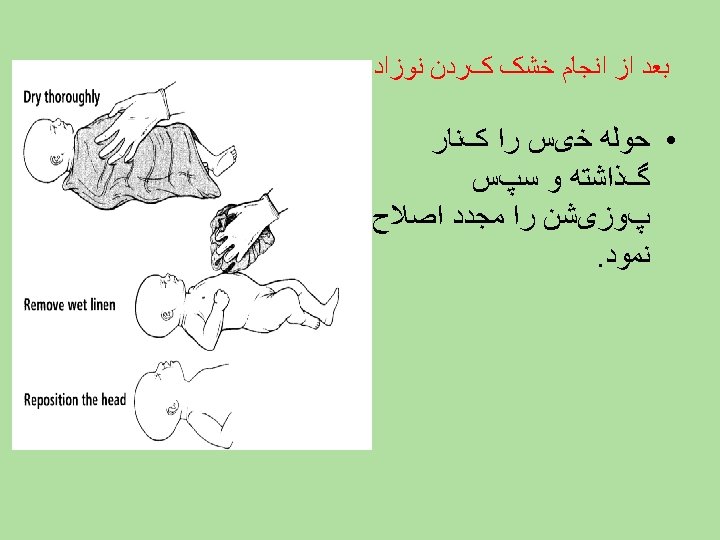
INITIAL STEPS OF RESUSCITATION
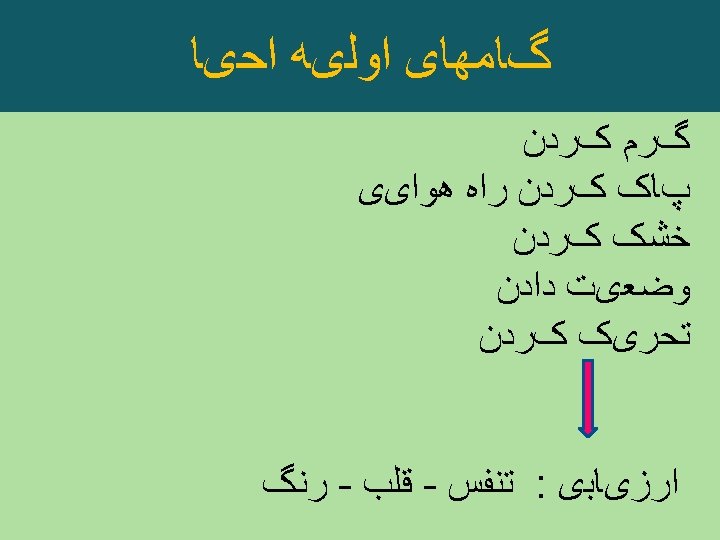
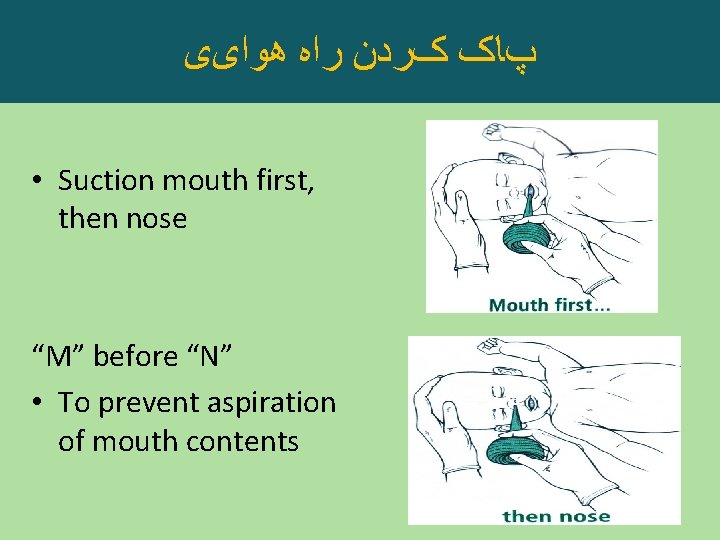
پﺎک کﺮﺩﻥ ﺭﺍﻩ ﻫﻮﺍیی • Suction mouth first, then nose “M” before “N” • To prevent aspiration of mouth contents
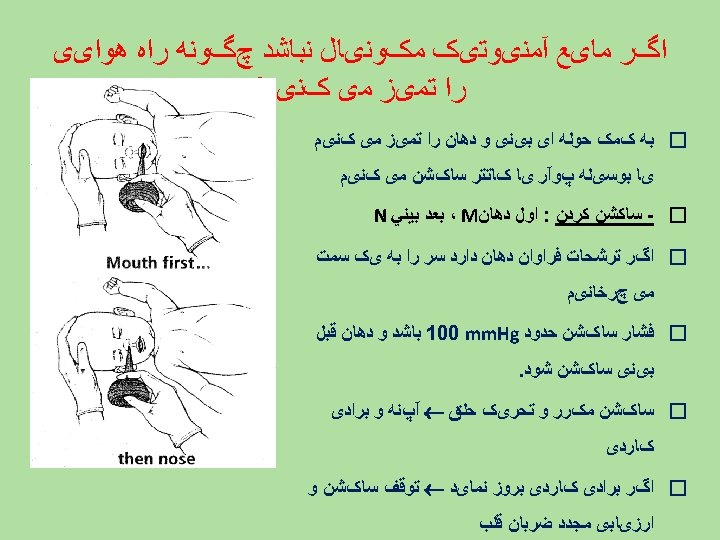
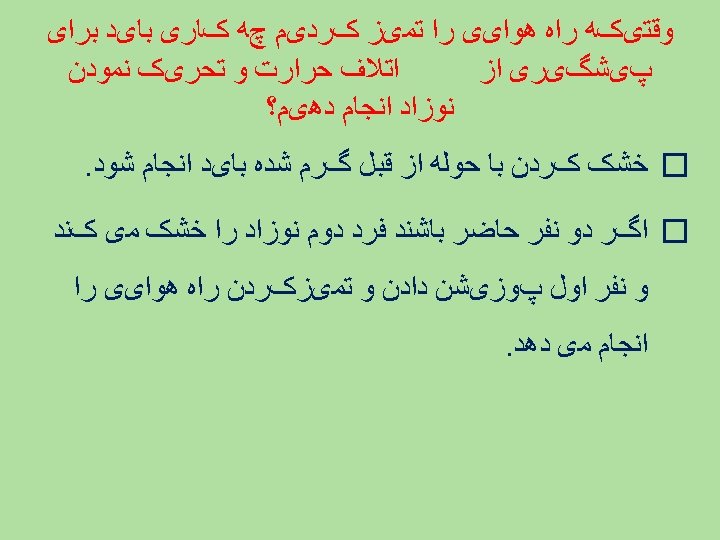
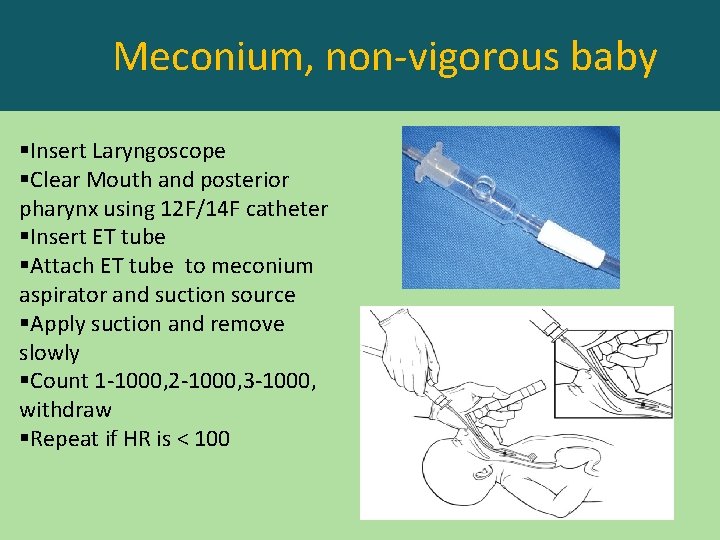
Meconium, non-vigorous baby §Insert Laryngoscope §Clear Mouth and posterior pharynx using 12 F/14 F catheter §Insert ET tube §Attach ET tube to meconium aspirator and suction source §Apply suction and remove slowly §Count 1 -1000, 2 -1000, 3 -1000, withdraw §Repeat if HR is < 100
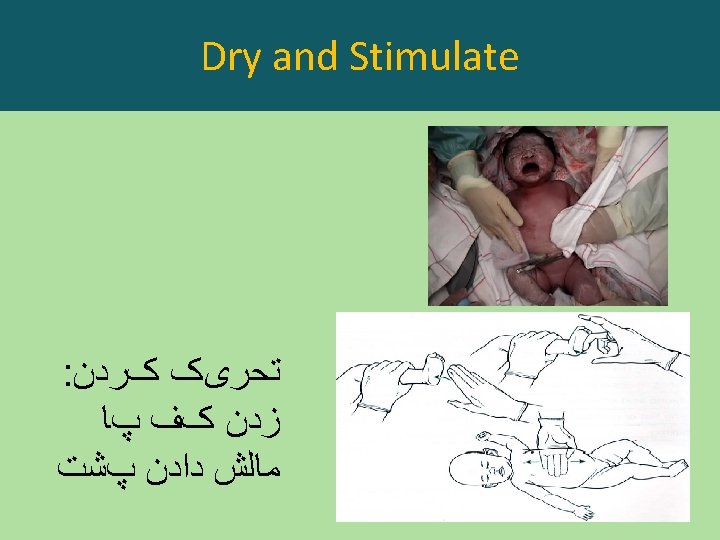
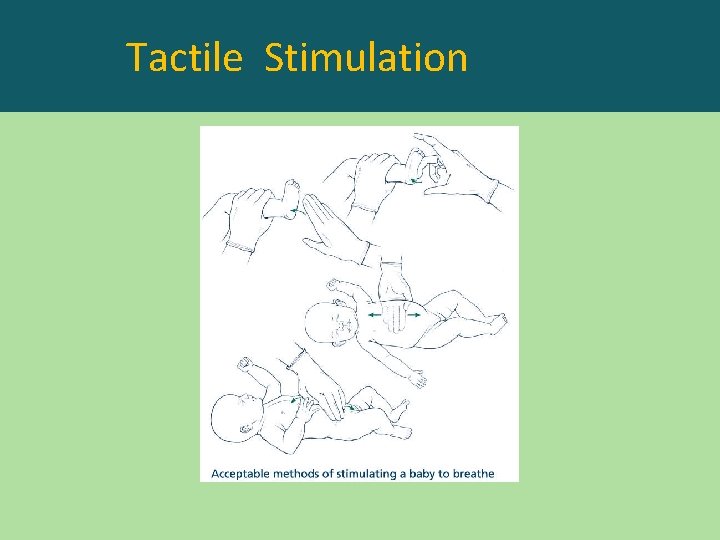
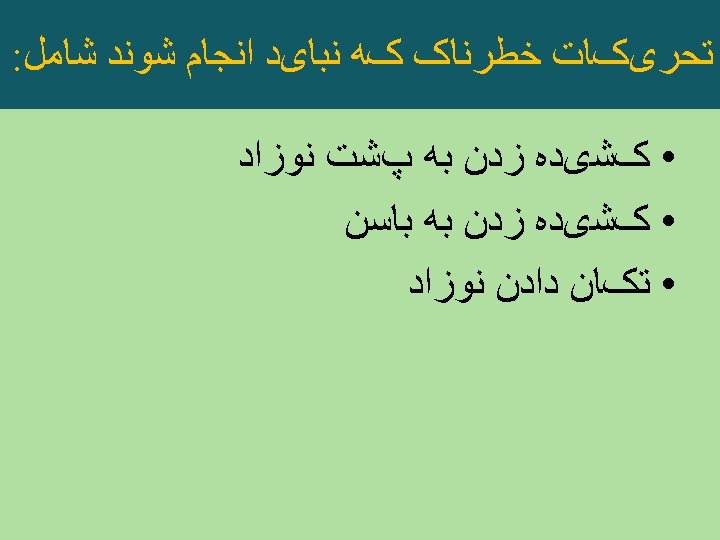
Tactile Stimulation
INITIAL STEPS OF RESUSCITATION

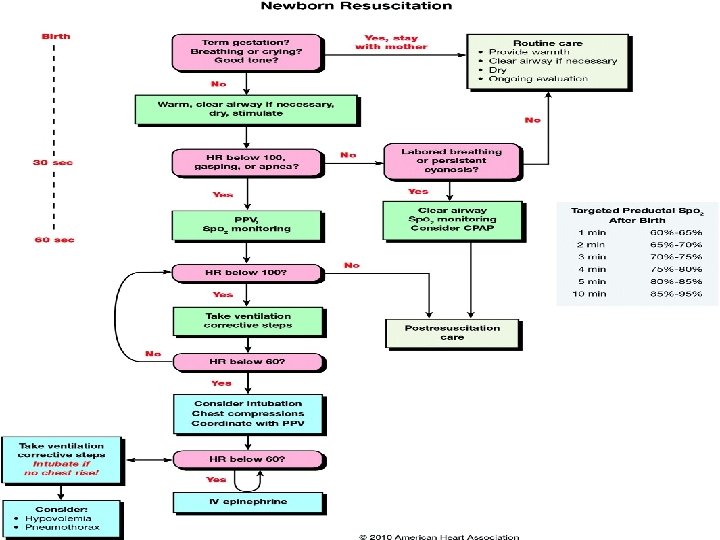
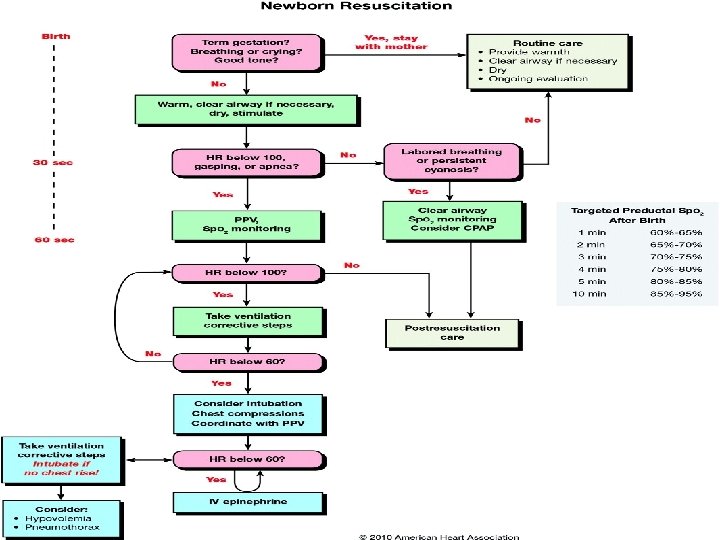
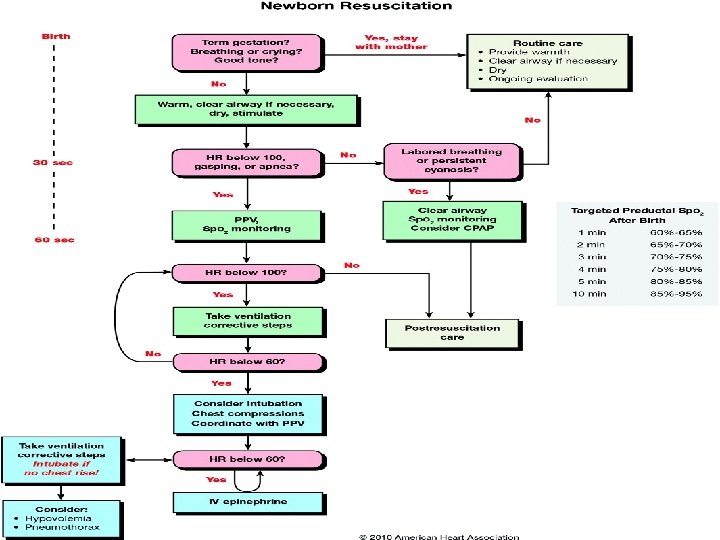
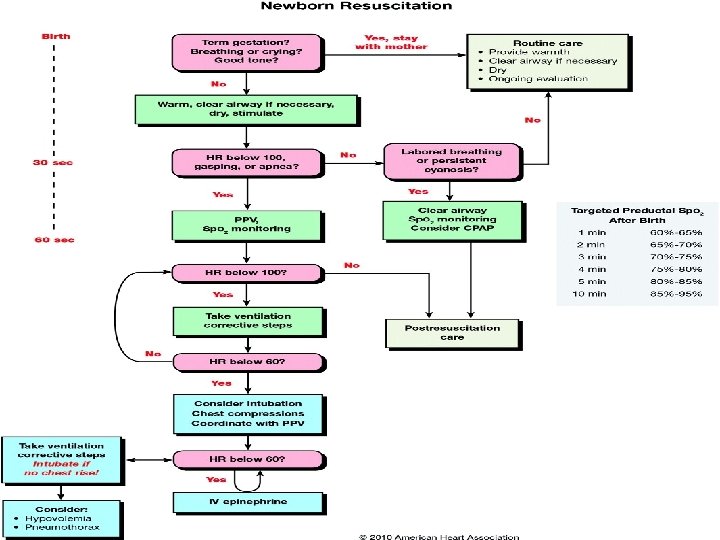
Targeted Preductal Sp. O 2 after Birth • 1 min 60 -65% • 2 min 65 -70% • 3 min 70 -75% • 4 min 75 -80% • 5 min 80 -85% • 10 min 85 -95% •
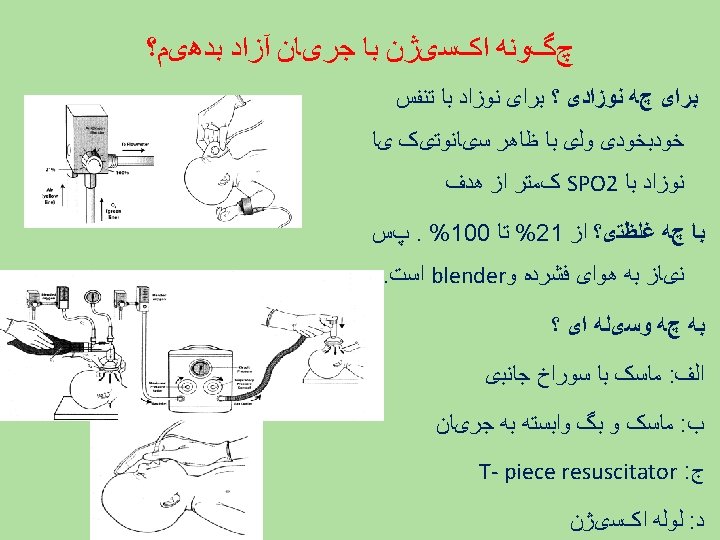
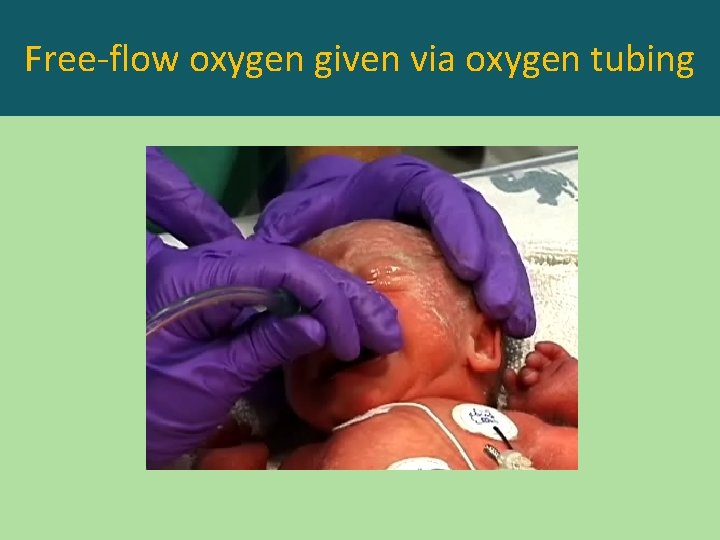
Free-flow oxygen given via oxygen tubing

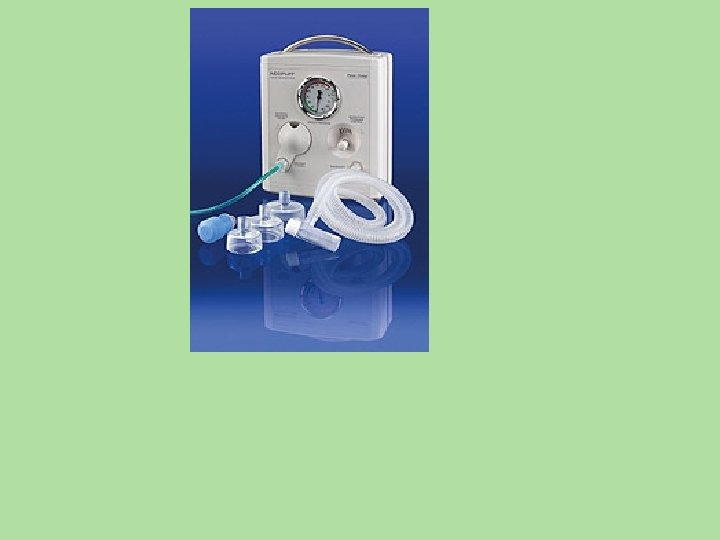
Supplemental oxygen • Free flow oxygen – – Oxygen mask Flow inflating bag T- piece resuscitator Oxygen tubing held close to baby’s nose • Start with room air and increase to maintain target Sp. O 2 Time Target Spo 2 1 min 60 -65% • CPAP provided with 2 min 65 -70% – Flow inflating bag – T-piece resuscitator 3 min 70 -75% 4 min 75 -80% 5 min 80 -85% 10 min 85 -95%
EVALUATION • RESPIRATION • HEART RATE • COLOR
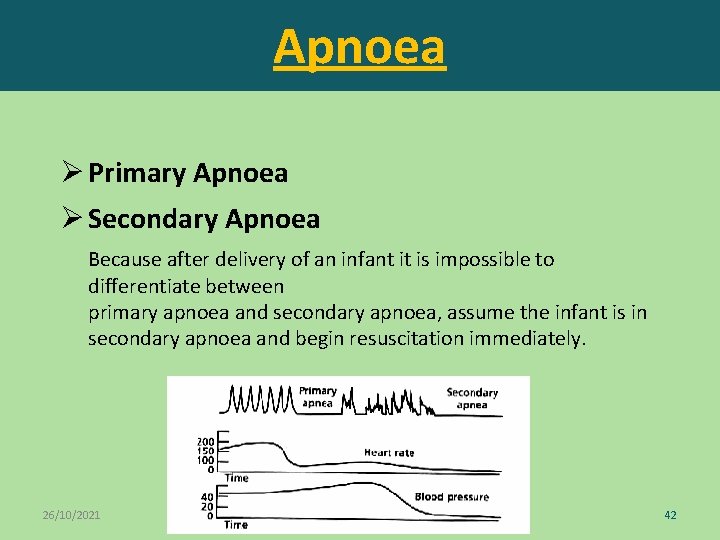
Apnoea Ø Primary Apnoea Ø Secondary Apnoea Because after delivery of an infant it is impossible to differentiate between primary apnoea and secondary apnoea, assume the infant is in secondary apnoea and begin resuscitation immediately. 26/10/2021 42
INITIAL STEPS OF RESUSCITATION
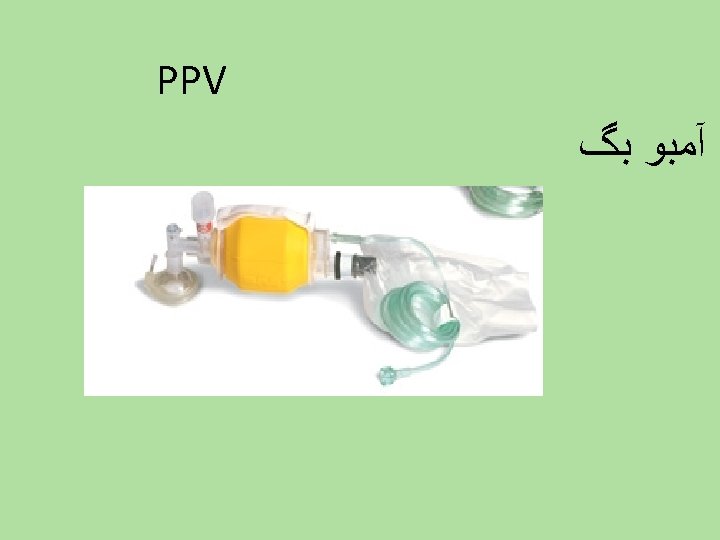
Positive pressure ventilation • Ventilation of the lungs is the single most and most effective step in newborn resuscitation Indications: • Gasping/apnea • HR < 100/min • Sp. O 2 remains below target values despite free flow supplemental oxygen increased to 100%.
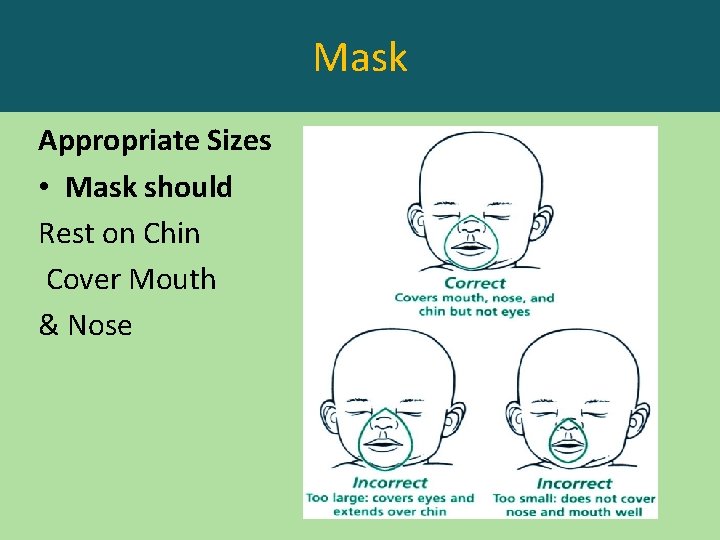
Mask Appropriate Sizes • Mask should Rest on Chin Cover Mouth & Nose
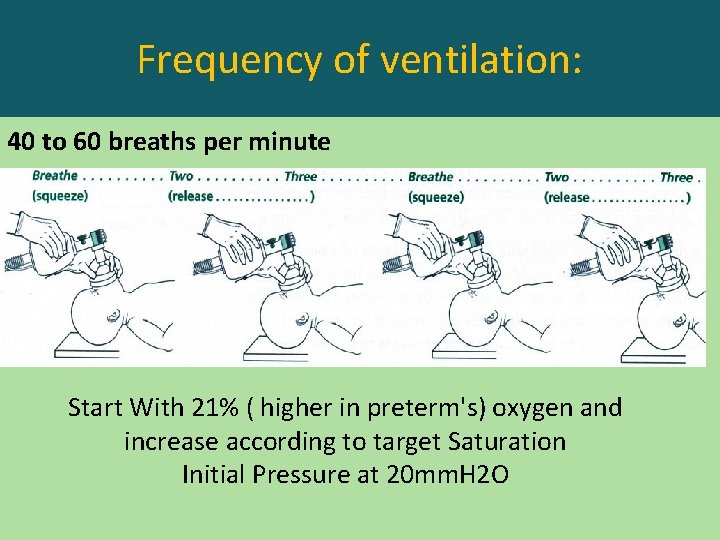
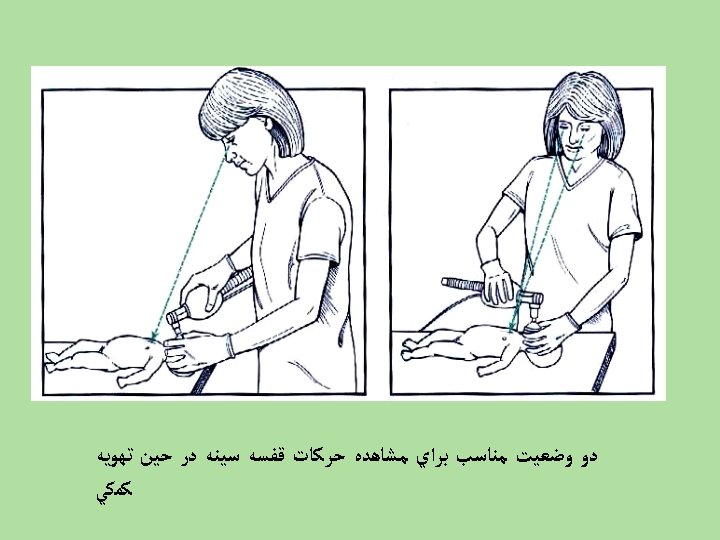
Frequency of ventilation: 40 to 60 breaths per minute Start With 21% ( higher in preterm's) oxygen and increase according to target Saturation Initial Pressure at 20 mm. H 2 O
**Ventilation of the lungs is the most important and effective action of NRP
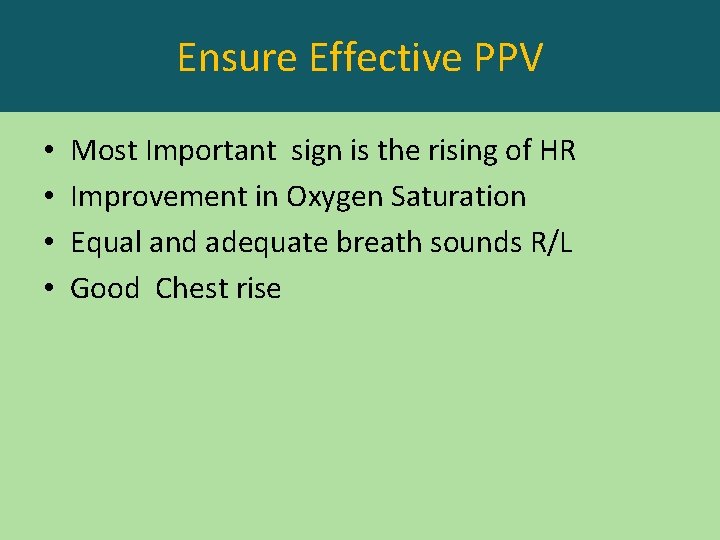
Ensure Effective PPV • • Most Important sign is the rising of HR Improvement in Oxygen Saturation Equal and adequate breath sounds R/L Good Chest rise



Evaluation • Heart rate • Oxygenation by oximeter If heart rate <100 bpm
INITIAL STEPS OF RESUSCITATION
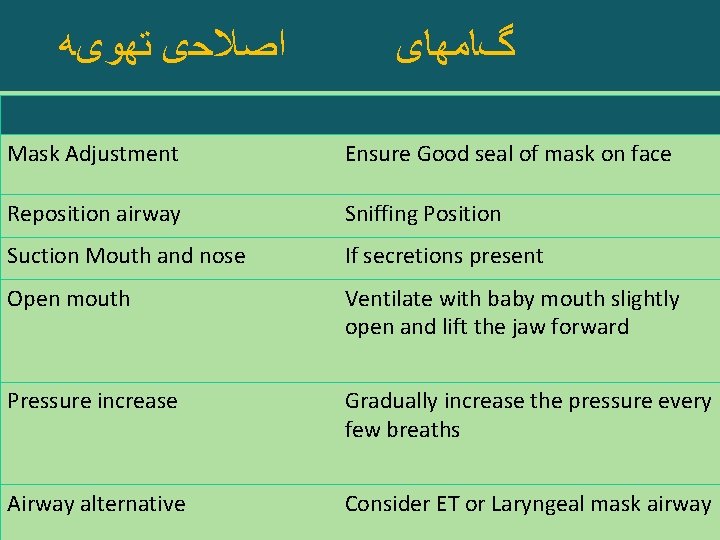
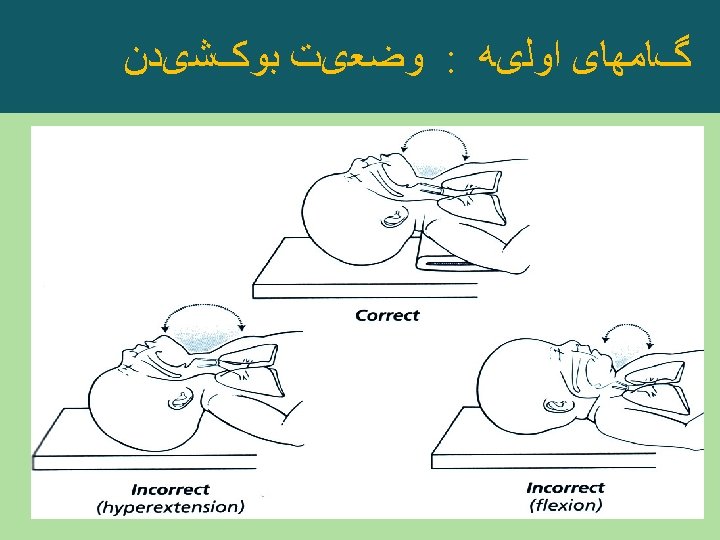
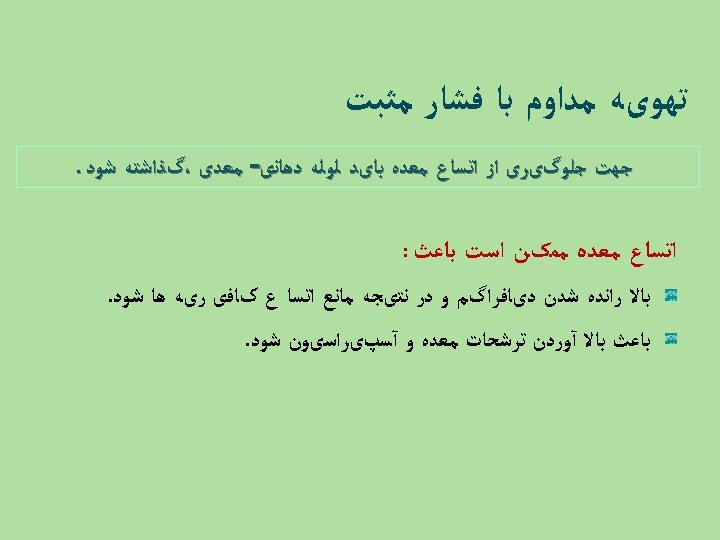
ﺍﺻﻼﺣی ﺗﻬﻮیﻪ گﺎﻣﻬﺎی Mask Adjustment Ensure Good seal of mask on face Reposition airway Sniffing Position Suction Mouth and nose If secretions present Open mouth Ventilate with baby mouth slightly open and lift the jaw forward Pressure increase Gradually increase the pressure every few breaths Airway alternative Consider ET or Laryngeal mask airway

Evaluation If heart rate <60 bpm despite adequate ventilation for 30 seconds,
INITIAL STEPS OF RESUSCITATION

Chest compressions Indications : • HR <60/min despite at least 30 sec of effective PPV ØStrongly consider Endotracheal intubation at this point as it ensures adequate ventilation and facilitates the coordination of ventilation and chest compressions

2011 NRP Cardiac Compression. Guidelines • • • �Compress to depth of 1/3 AP diameter of chest �Compress the lower 1/3 of the sternum �Use 2 -thumb technique rather than 2 -finger technique � 3: 1 compressions to ventilation ratio for asphyxial arrest �Coordinate compressions and ventilations to avoid simultaneous delivery �Avoid frequent interruptions in compressions


Chest compressions Positions : • Chest compressions are of little value unless the lungs are effectively ventilated • 2 persons are required – 1 – chest compressions provider should have access to the chest with his hands positioned correctly – 2 – Ventilation provider should be at head end to maintain effective mask-face seal or to stabilize ET tube

Chest compressions Technique: • Thumb technique: 2 thumbs depress the sternum, hands encircle the torso and the fingers support the spine. Preferred technique • 2 – Finger technique: Tips of middle & index/ring finger of one hand compresses sternum, other hand supports the back.
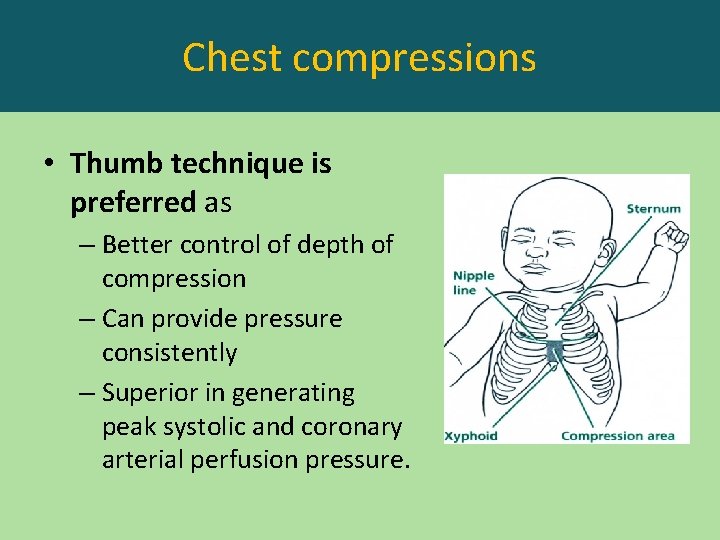
Chest compressions • Thumb technique is preferred as – Better control of depth of compression – Can provide pressure consistently – Superior in generating peak systolic and coronary arterial perfusion pressure.
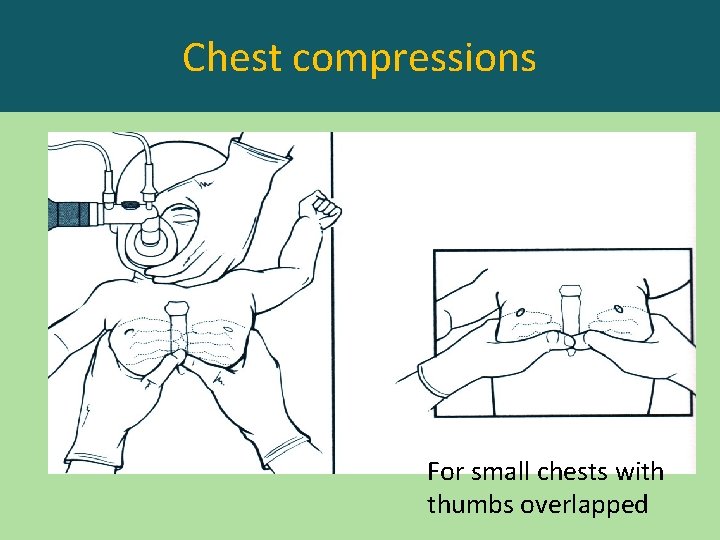
Chest compressions For small chests with thumbs overlapped

Chest compressions
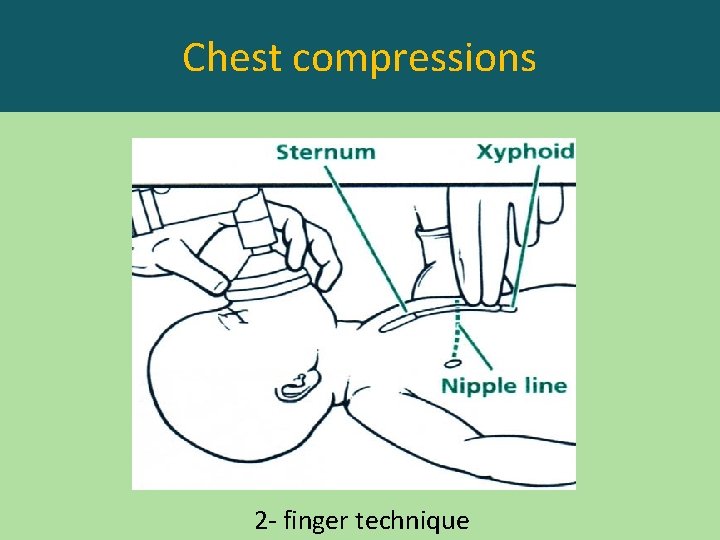
Chest compressions 2 - finger technique
Chest compressions

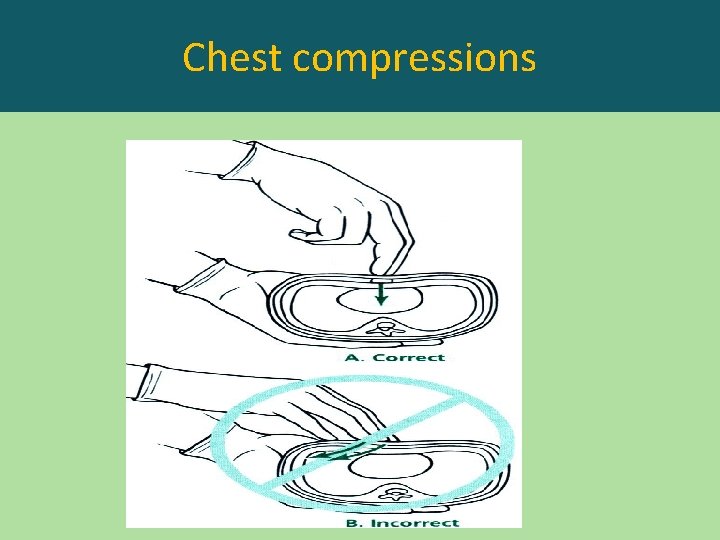
Chest compressions • Depth : 1/3 rd of the anteroposterior diameter of chest. • Duration of downward stroke should be shorter than the duration of release • Do not lift the fingers off the chest
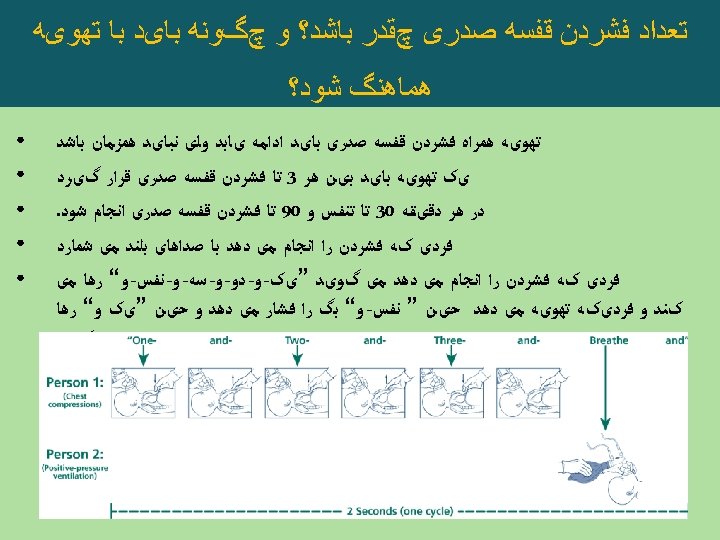
Chest compressions Complications: • Laceration of liver • Breakage of ribs
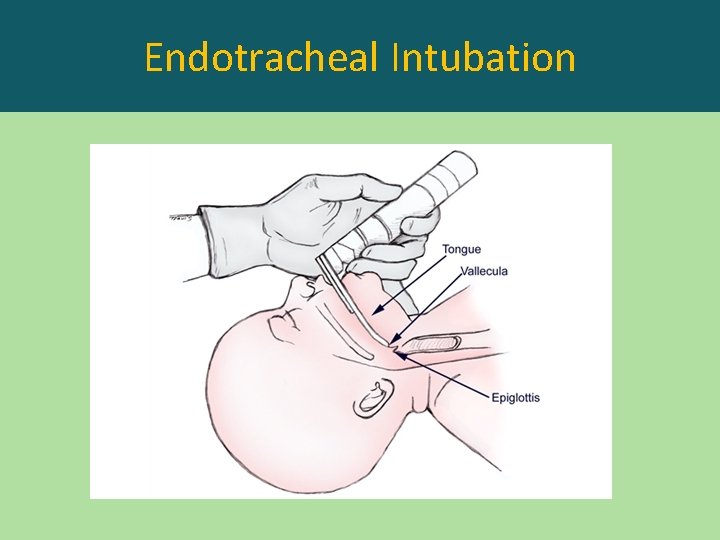
Endotracheal Intubation
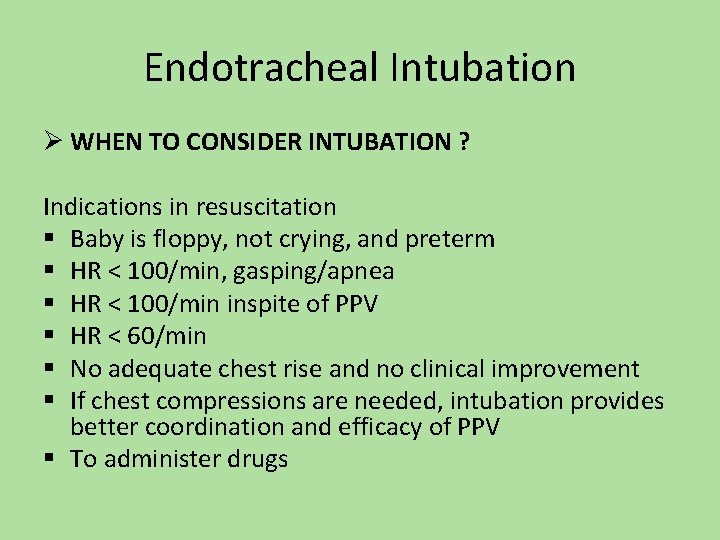
Endotracheal Intubation Ø WHEN TO CONSIDER INTUBATION ? Indications in resuscitation § Baby is floppy, not crying, and preterm § HR < 100/min, gasping/apnea § HR < 100/min inspite of PPV § HR < 60/min § No adequate chest rise and no clinical improvement § If chest compressions are needed, intubation provides better coordination and efficacy of PPV § To administer drugs
Endotracheal Intubation Ø WHEN TO CONSIDER INTUBATION ? Ø Special conditions § Meconium aspiration if baby is depressed in which it is the first step to be done § Extreme Prematurity § Surfactant administration § Suspected diaphragmatic hernia
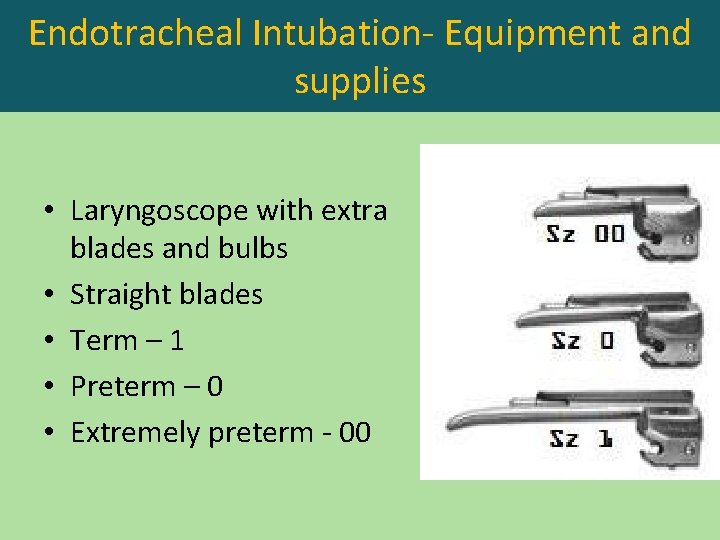
Endotracheal Intubation- Equipment and supplies • Laryngoscope with extra blades and bulbs • Straight blades • Term – 1 • Preterm – 0 • Extremely preterm - 00
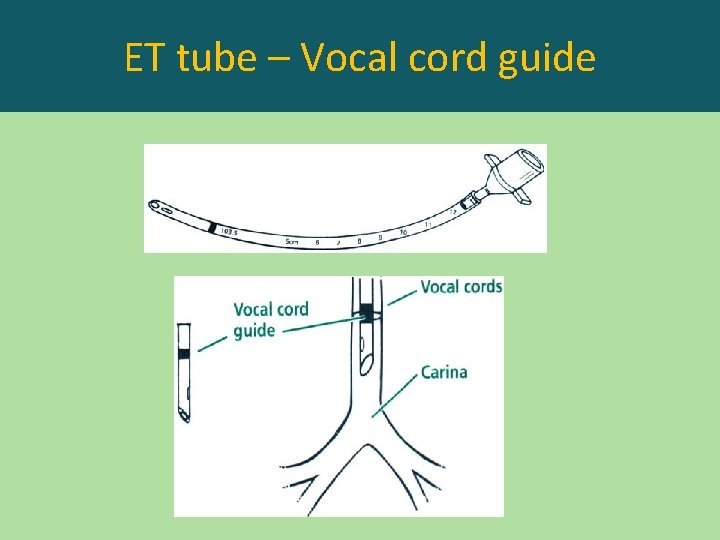
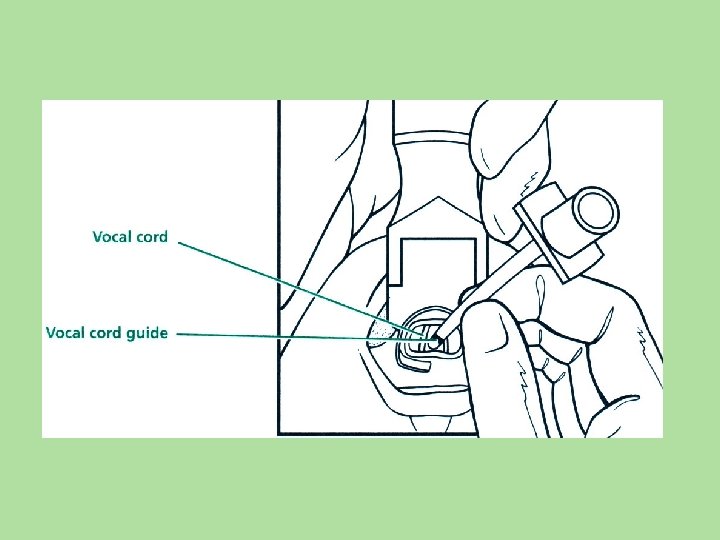
ET tube – Vocal cord guide
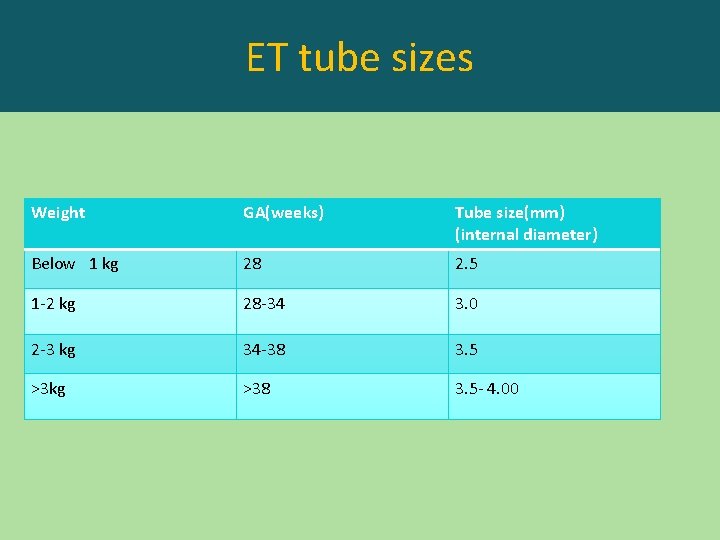
ET tube sizes Weight GA(weeks) Tube size(mm) (internal diameter) Below 1 kg 28 2. 5 1 -2 kg 28 -34 3. 0 2 -3 kg 34 -38 3. 5 >3 kg >38 3. 5 - 4. 00
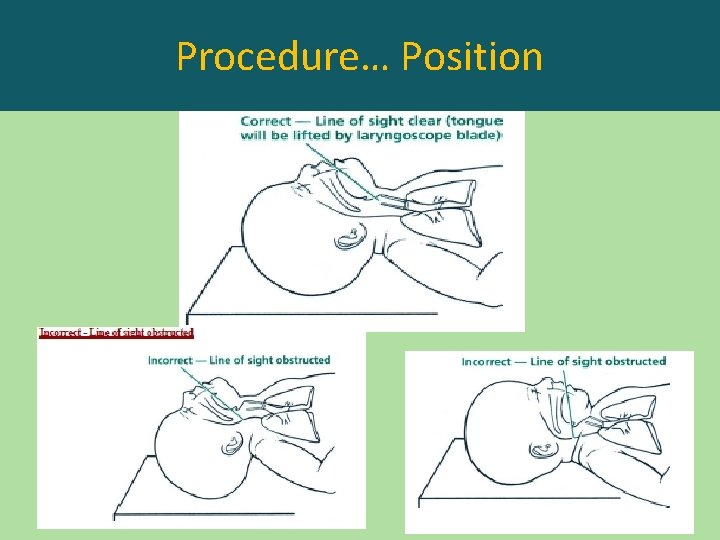
Procedure… Position
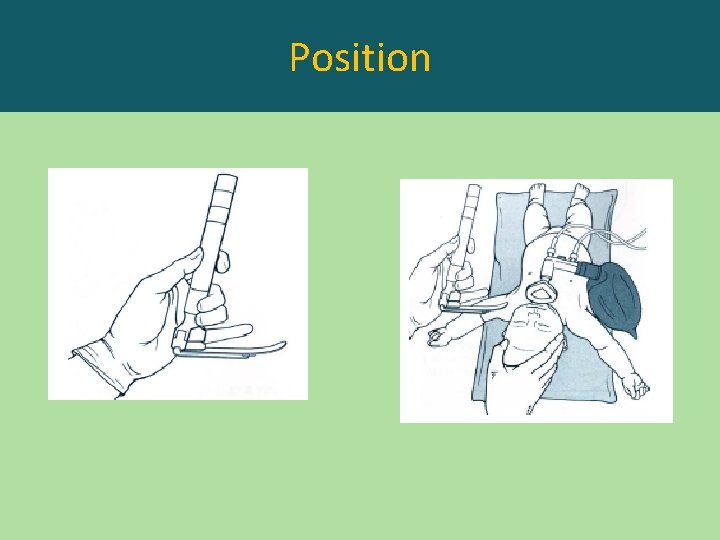
Position
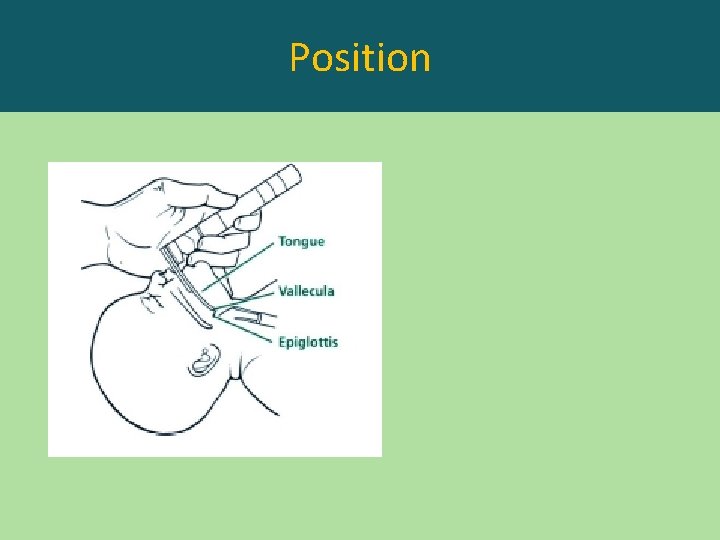
Position
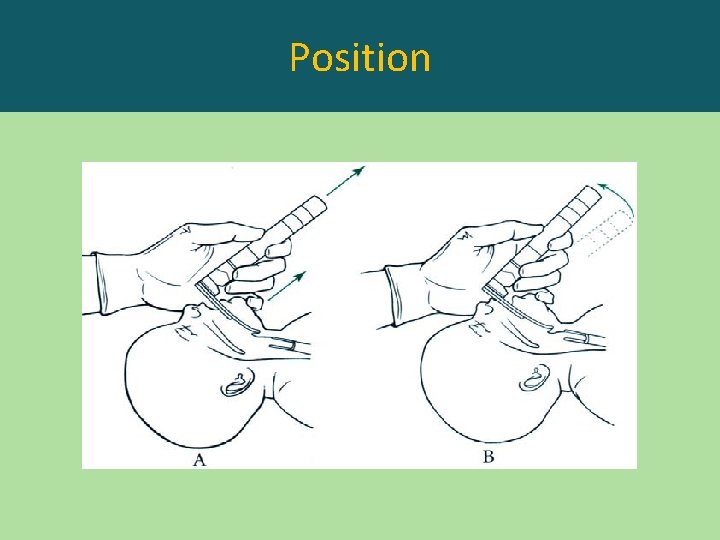
Position
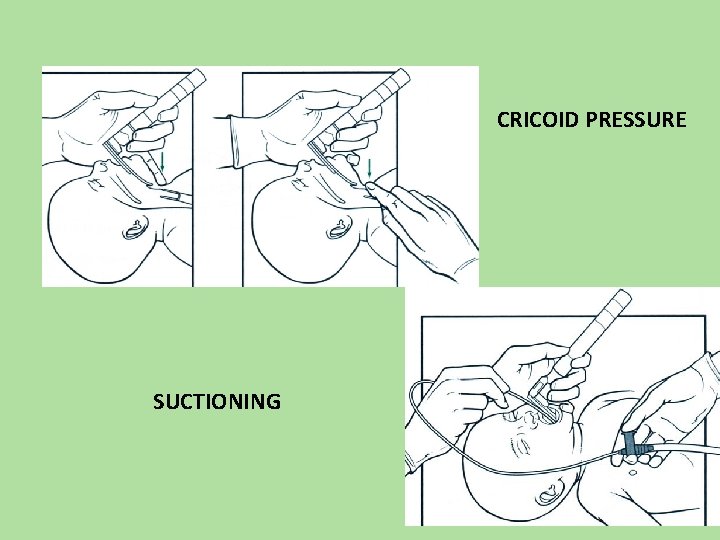
CRICOID PRESSURE SUCTIONING
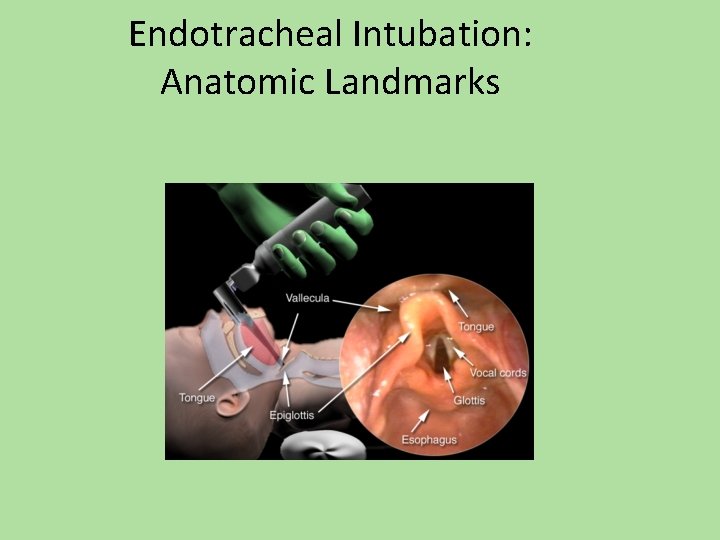
Endotracheal Intubation: Anatomic Landmarks
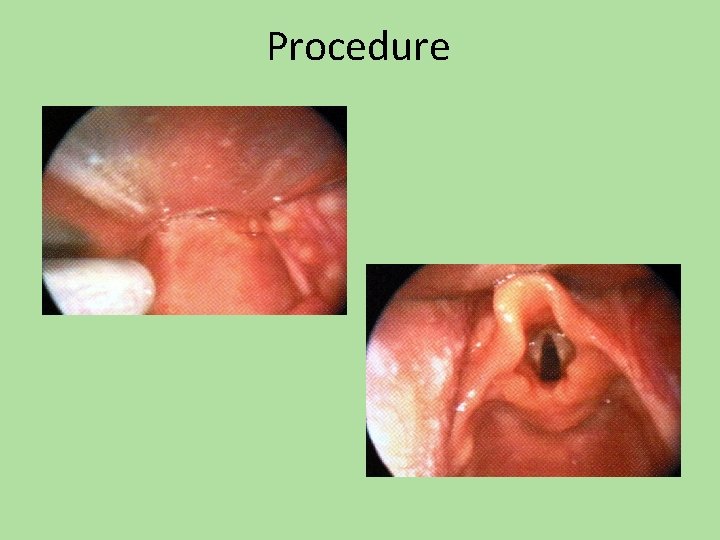
Procedure
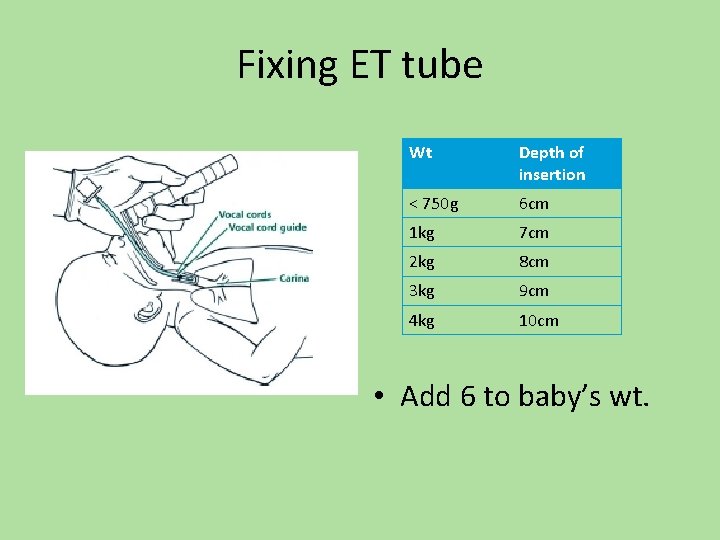
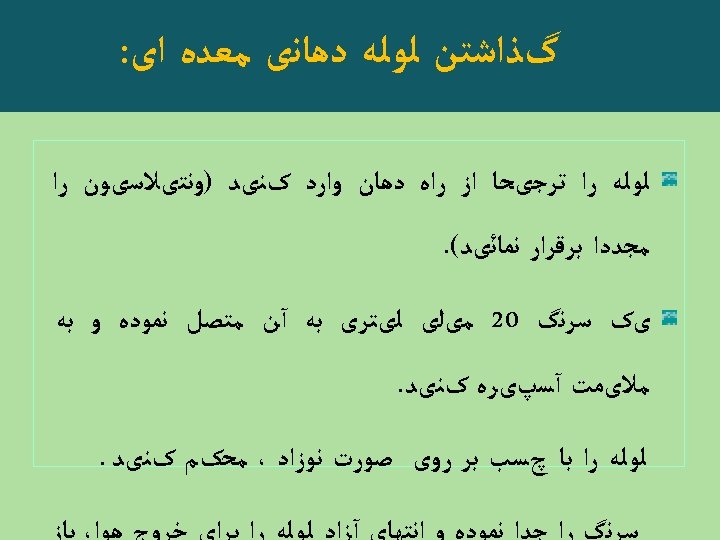
Fixing ET tube Wt Depth of insertion < 750 g 6 cm 1 kg 7 cm 2 kg 8 cm 3 kg 9 cm 4 kg 10 cm • Add 6 to baby’s wt.
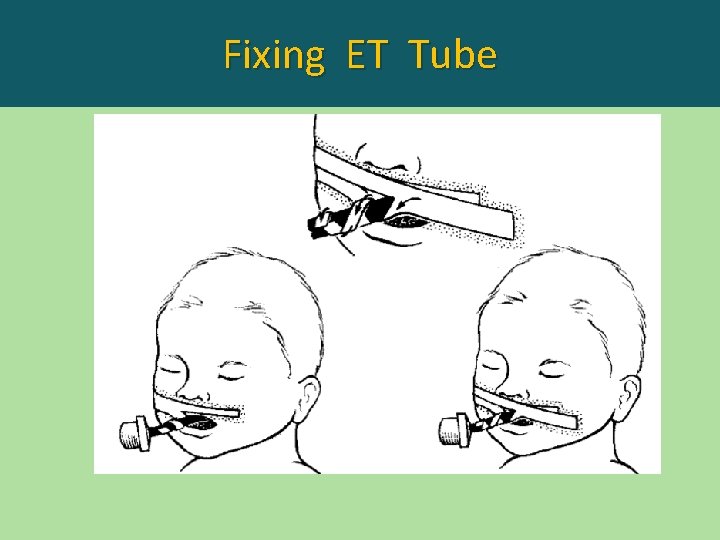
Fixing ET Tube
ﺍﺭﺯیﺎﺑی Drugtherapy is indicated: • If HR remains < 60/min even after 30 sec of • effective ventilation preferably after intubation and atleast another 45 -60 sec of coordinated chest compressions and effective ventilation
ﺩﺍﺭﻭﺩﺭﻣﺎﻧی • Epinephrin • Volume Expander : N/S R/L O negative
INITIAL STEPS OF RESUSCITATION
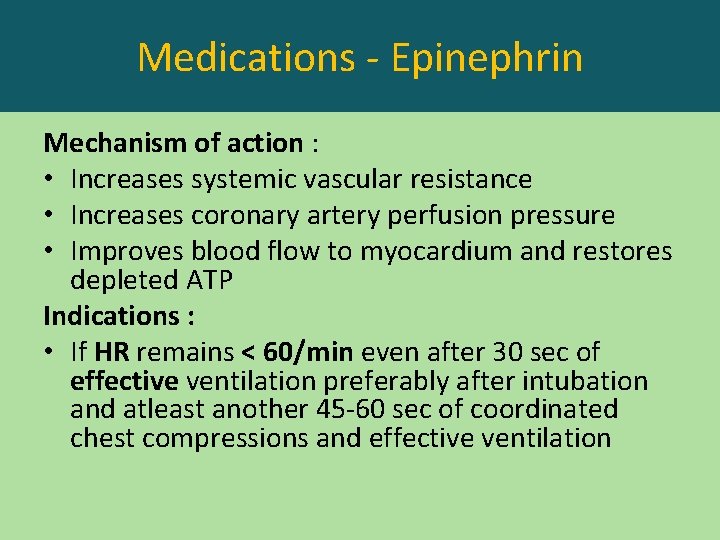
Medications - Epinephrin Mechanism of action : • Increases systemic vascular resistance • Increases coronary artery perfusion pressure • Improves blood flow to myocardium and restores depleted ATP Indications : • If HR remains < 60/min even after 30 sec of effective ventilation preferably after intubation and atleast another 45 -60 sec of coordinated chest compressions and effective ventilation
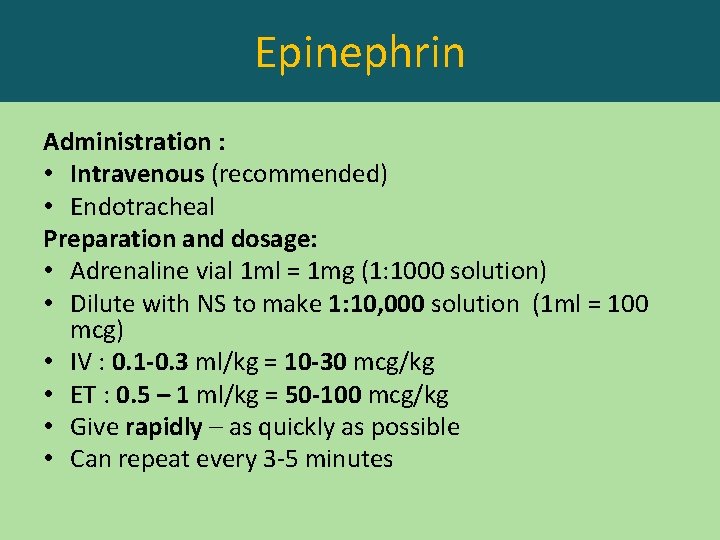
Epinephrin Administration : • Intravenous (recommended) • Endotracheal Preparation and dosage: • Adrenaline vial 1 ml = 1 mg (1: 1000 solution) • Dilute with NS to make 1: 10, 000 solution (1 ml = 100 mcg) • IV : 0. 1 -0. 3 ml/kg = 10 -30 mcg/kg • ET : 0. 5 – 1 ml/kg = 50 -100 mcg/kg • Give rapidly – as quickly as possible • Can repeat every 3 -5 minutes
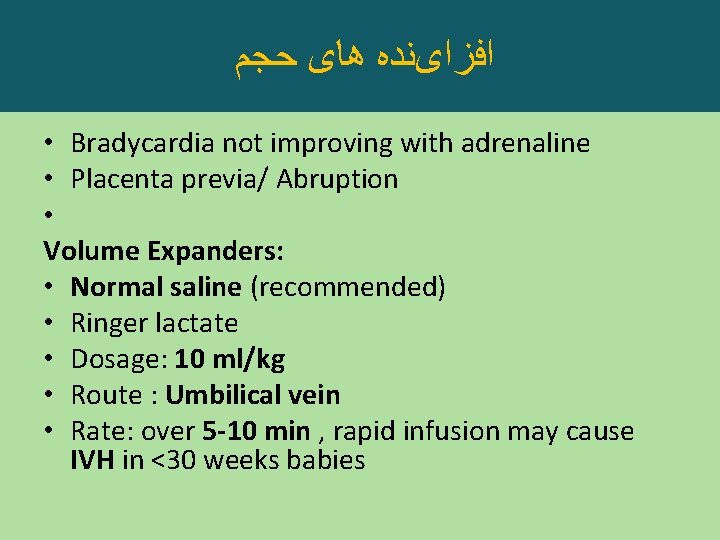
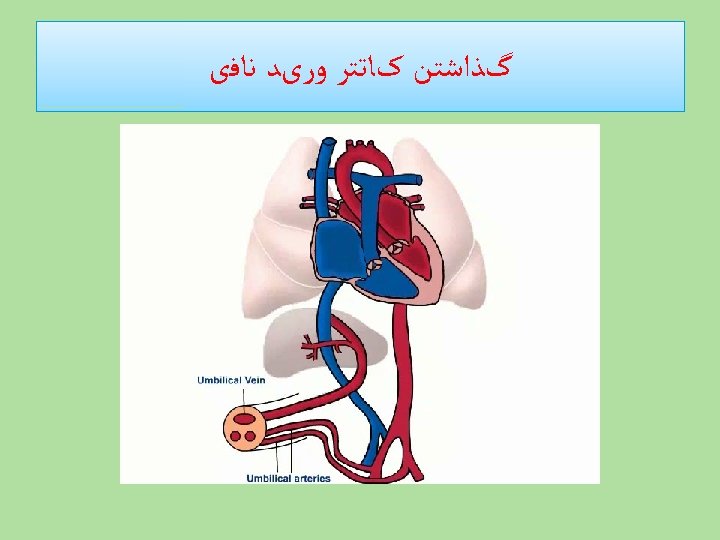
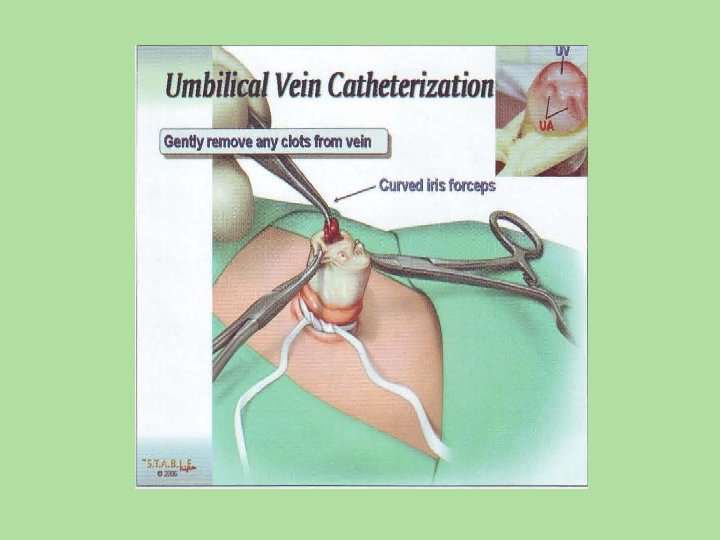
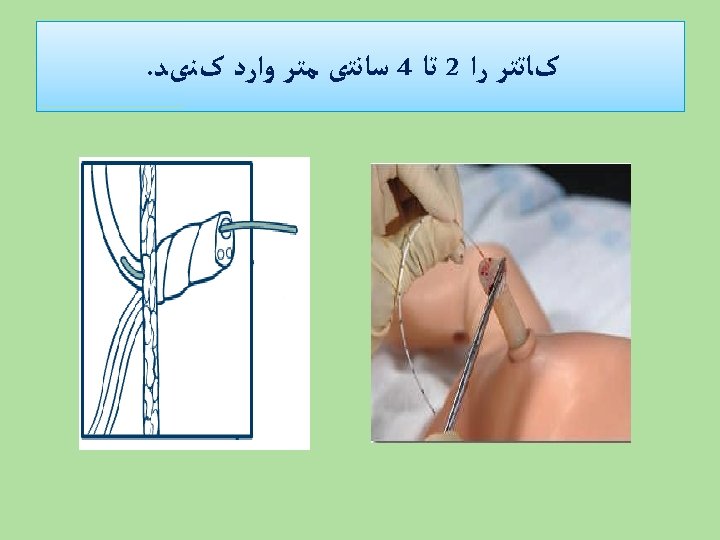
ﺍﻓﺰﺍیﻨﺪﻩ ﻫﺎی ﺣﺠﻢ • Bradycardia not improving with adrenaline • Placenta previa/ Abruption • Volume Expanders: • Normal saline (recommended) • Ringer lactate • Dosage: 10 ml/kg • Route : Umbilical vein • Rate: over 5 -10 min , rapid infusion may cause IVH in <30 weeks babies
INITIAL STEPS OF RESUSCITATION

!! THANK YOU !!
- Slides: 105