Novel protocols for PDT treatment under optical monitoring




- Slides: 29
Novel protocols for PDT treatment under optical monitoring M. Yu. Kirillin 1, A. V. Khilov 1, D. A. Kurakina(Loginova)1, E. A. Sergeeva 1, V. V. Perekatova 1, M. A. Shakhova 1, 2, A. E. Meller 1, 2, D. A. Sapunov 1, 2, A. V. Shakhov 2, 1, N. Yu. Orlinskaya 2, 1, and I. V. Turchin 1 1 Institute of Applied Physics RAS, Nizhny Novgorod, Russia, 2 Privolzhsky Research Medical University, Nizhny Novgorod, Russia Saratov Fall Meeting 2018, Saratov, Russia, 25 -28 September, 2018
Outline • • • Motivation Photodynamic therapy (PDT) Monte Carlo PDT planning Simulation of light dose distribution Dual-wavelength fluorescence PDT monitoring PS photobleaching monitoring with fluorescence imaging Optical coherence tomography (OCT) Response of normal tissue to PDT regimens: animal study OCT monitoring of pharynx antimicrobial photodynamic therapy Conclusions
Motivation • Perspectives of photodynamic therapy in different medical applications • Chlorin-based photosensitizers • Optimized PDT protocols • Personalized medicine: novel diagnostic techniques for PDT-monitoring • Low-dose PDT for treatment of chronic inflammatory diseases and for aesthetic medicine • Development of personalized PDT protocols employing optical monitoring
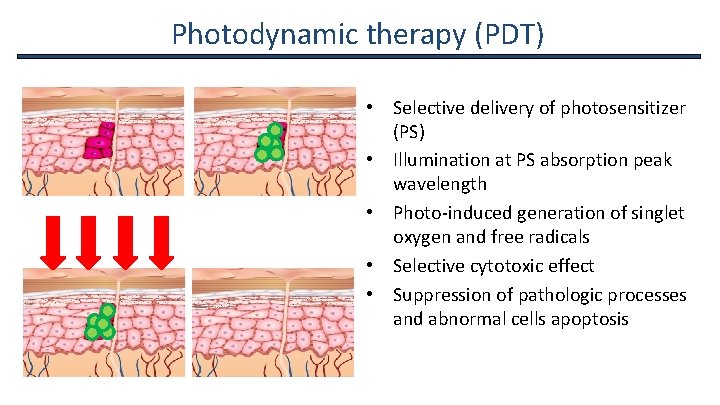
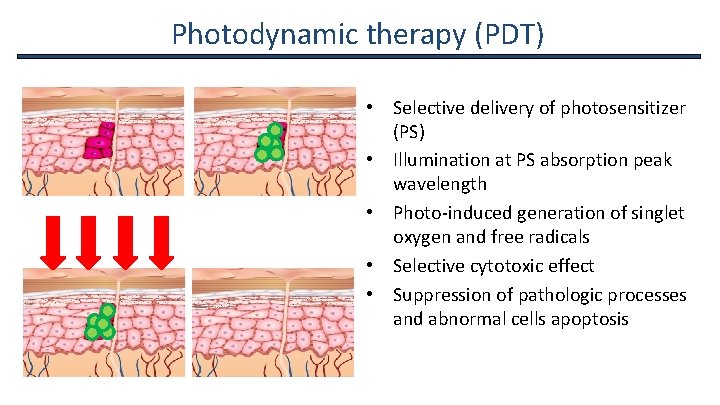
Photodynamic therapy (PDT) • Selective delivery of photosensitizer (PS) • Illumination at PS absorption peak wavelength • Photo-induced generation of singlet oxygen and free radicals • Selective cytotoxic effect • Suppression of pathologic processes and abnormal cells apoptosis
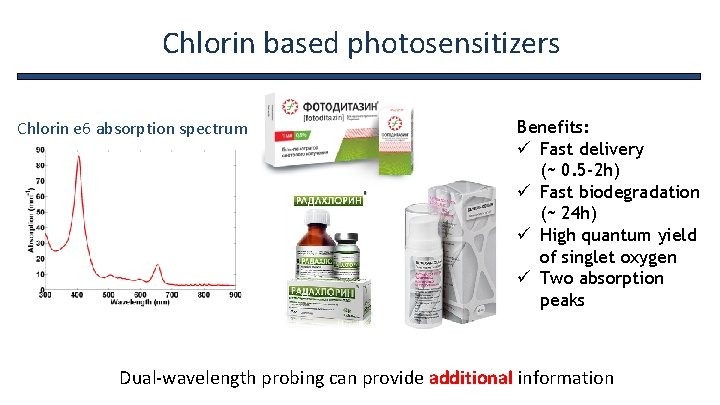
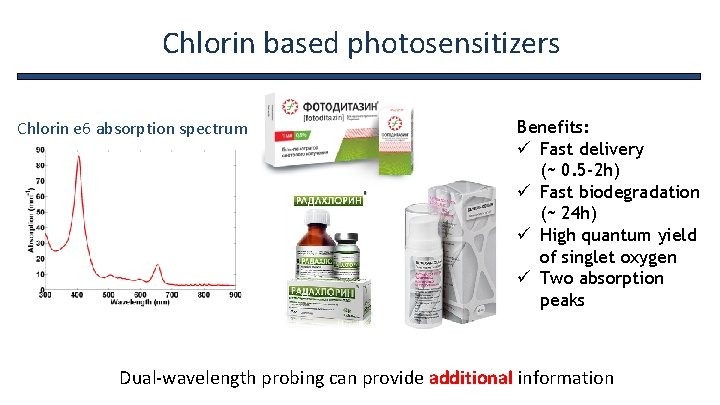
Chlorin based photosensitizers Chlorin e 6 absorption spectrum Benefits: ü Fast delivery (~ 0. 5 -2 h) ü Fast biodegradation (~ 24 h) ü High quantum yield of singlet oxygen ü Two absorption peaks Dual-wavelength probing can provide additional information
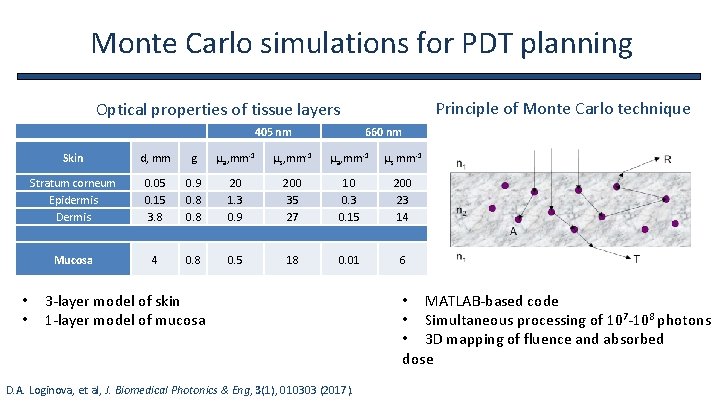
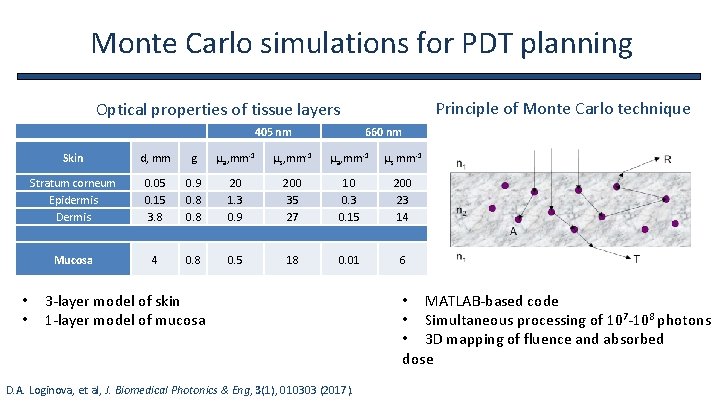
Monte Carlo simulations for PDT planning Principle of Monte Carlo technique Optical properties of tissue layers • • 405 nm 660 nm Skin d, mm g µa, mm-1 µs, mm-1 µa, mm-1 µs mm-1 Stratum corneum Epidermis Dermis 0. 05 0. 15 3. 8 0. 9 0. 8 20 1. 3 0. 9 200 35 27 10 0. 3 0. 15 200 23 14 Mucosa 4 0. 8 0. 5 18 0. 01 6 3 -layer model of skin 1 -layer model of mucosa D. A. Loginova, et al, J. Biomedical Photonics & Eng, 3(1), 010303 (2017). • MATLAB-based code • Simultaneous processing of 107 -108 photons • 3 D mapping of fluence and absorbed dose
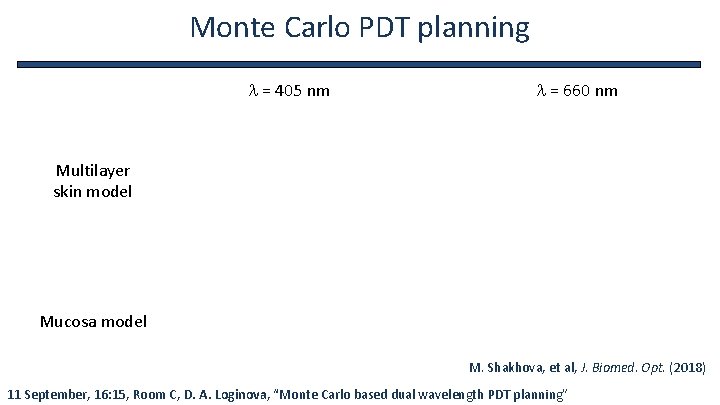
Monte Carlo PDT planning l = 405 nm l = 660 nm Multilayer skin model Mucosa model M. Shakhova, et al, J. Biomed. Opt. (2018) 11 September, 16: 15, Room C, D. A. Loginova, “Monte Carlo based dual wavelength PDT planning”
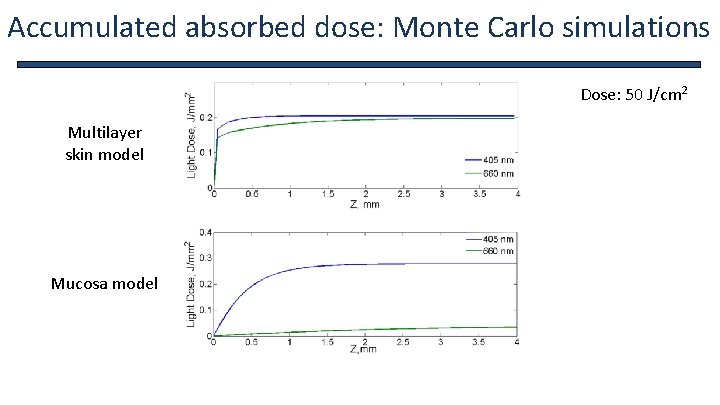
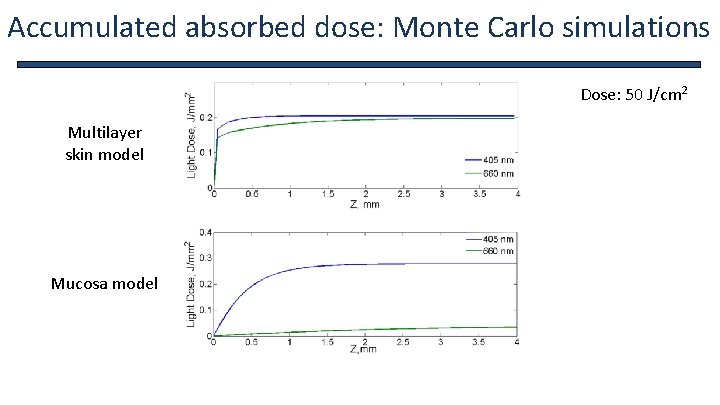
Accumulated absorbed dose: Monte Carlo simulations Dose: 50 J/cm 2 Multilayer skin model Mucosa model
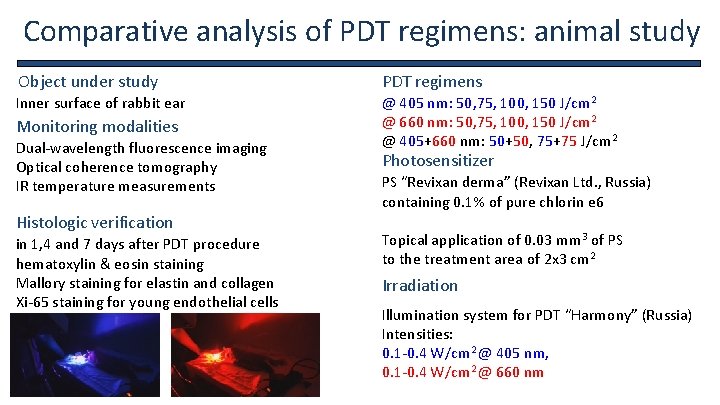
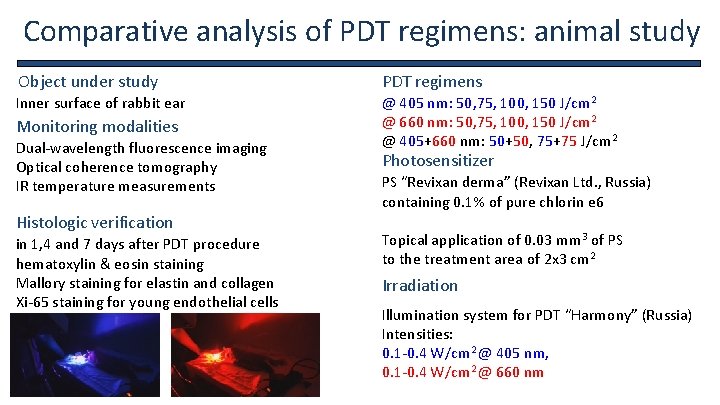
Comparative analysis of PDT regimens: animal study Object under study PDT regimens Inner surface of rabbit ear @ 405 nm: 50, 75, 100, 150 J/cm 2 @ 660 nm: 50, 75, 100, 150 J/cm 2 @ 405+660 nm: 50+50, 75+75 J/cm 2 Monitoring modalities Dual-wavelength fluorescence imaging Optical coherence tomography IR temperature measurements Histologic verification in 1, 4 and 7 days after PDT procedure hematoxylin & eosin staining Mallory staining for elastin and collagen Xi-65 staining for young endothelial cells Photosensitizer PS “Revixan derma” (Revixan Ltd. , Russia) containing 0. 1% of pure chlorin e 6 Topical application of 0. 03 mm 3 of PS to the treatment area of 2 x 3 cm 2 Irradiation Illumination system for PDT “Harmony” (Russia) Intensities: 0. 1 -0. 4 W/cm 2 @ 405 nm, 0. 1 -0. 4 W/cm 2 @ 660 nm
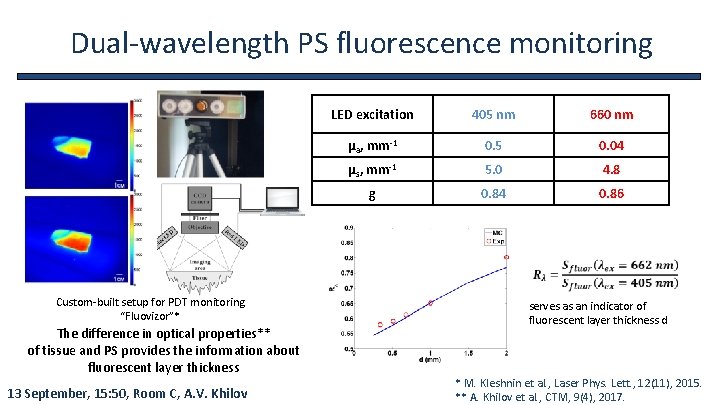
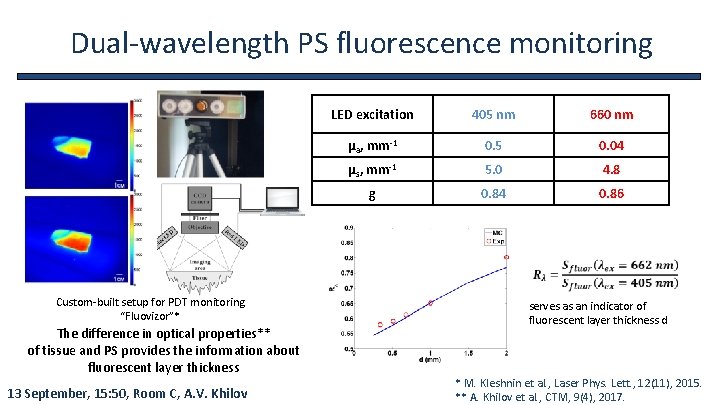
Dual-wavelength PS fluorescence monitoring LED excitation 405 nm 660 nm μa, mm-1 0. 5 0. 04 μs, mm-1 5. 0 4. 8 g 0. 84 0. 86 Custom-built setup for PDT monitoring “Fluovizor”* The difference in optical properties** of tissue and PS provides the information about fluorescent layer thickness 13 September, 15: 50, Room C, A. V. Khilov serves as an indicator of fluorescent layer thickness d * M. Kleshnin et al. , Laser Phys. Lett. , 12(11), 2015. ** A. Khilov et al. , CTM, 9(4), 2017.
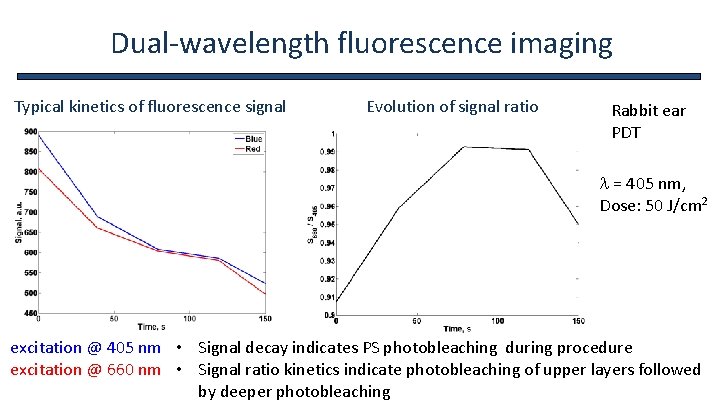
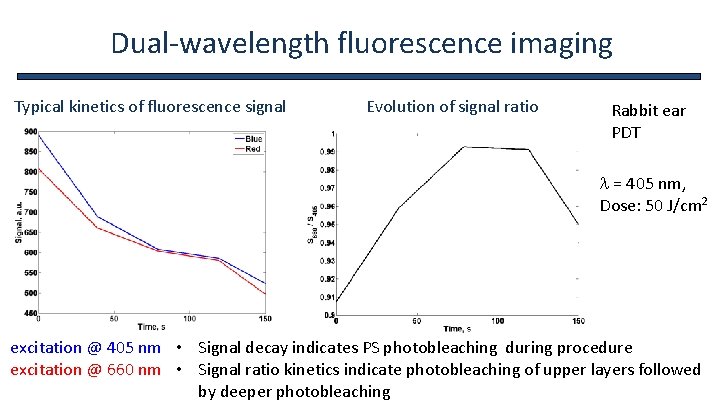
Dual-wavelength fluorescence imaging Typical kinetics of fluorescence signal Evolution of signal ratio Rabbit ear PDT l = 405 nm, Dose: 50 J/cm 2 excitation @ 405 nm • Signal decay indicates PS photobleaching during procedure excitation @ 660 nm • Signal ratio kinetics indicate photobleaching of upper layers followed by deeper photobleaching
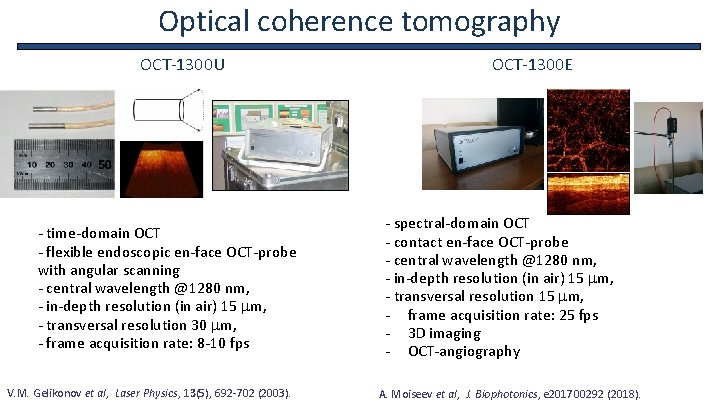
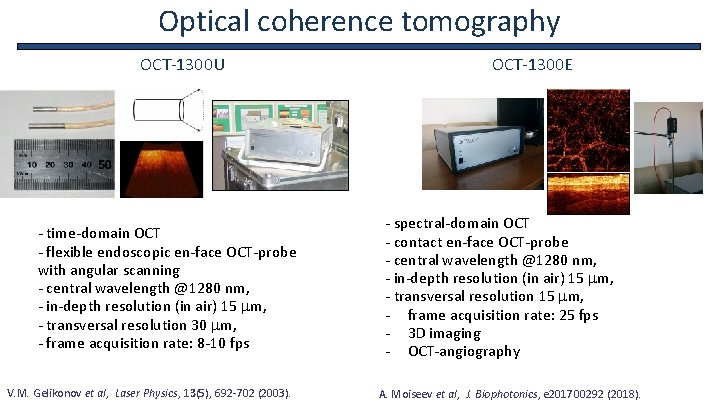
Optical coherence tomography OCT-1300 U - time-domain OCT - flexible endoscopic en-face OCT-probe with angular scanning - central wavelength @1280 nm, - in-depth resolution (in air) 15 mm, - transversal resolution 30 mm, - frame acquisition rate: 8 -10 fps V. M. Gelikonov et al, Laser Physics, 13(5), 692 -702 (2003). OCT-1300 E - spectral-domain OCT - contact en-face OCT-probe 1 mm - central wavelength @1280 nm, - in-depth resolution (in air) 15 mm, - transversal resolution 15 mm, - frame acquisition rate: 25 fps - 3 D imaging - OCT-angiography A. Moiseev et al, J. Biophotonics, e 201700292 (2018).
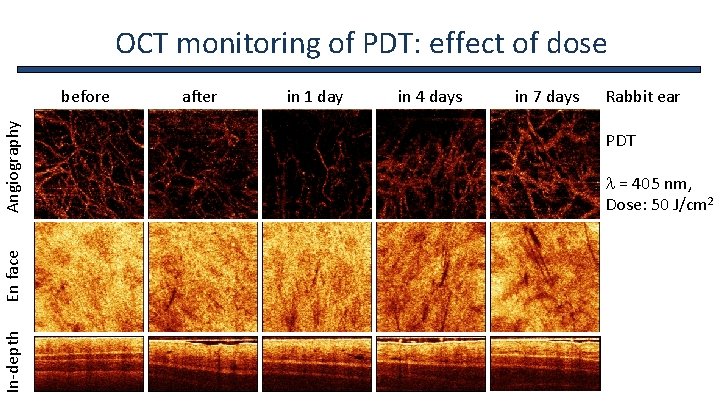
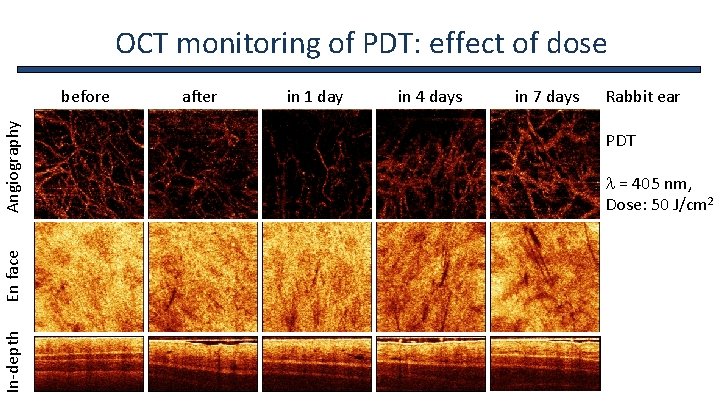
OCT monitoring of PDT: effect of dose before after in 1 day in 4 days in 7 days Rabbit ear In-depth En face Angiography PDT l = 405 nm, Dose: 50 J/cm 2
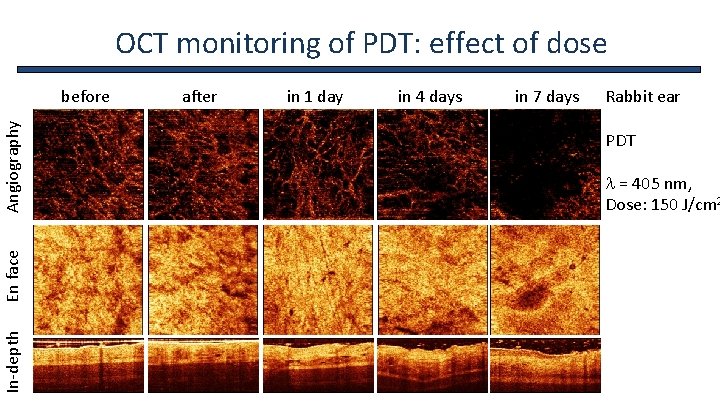
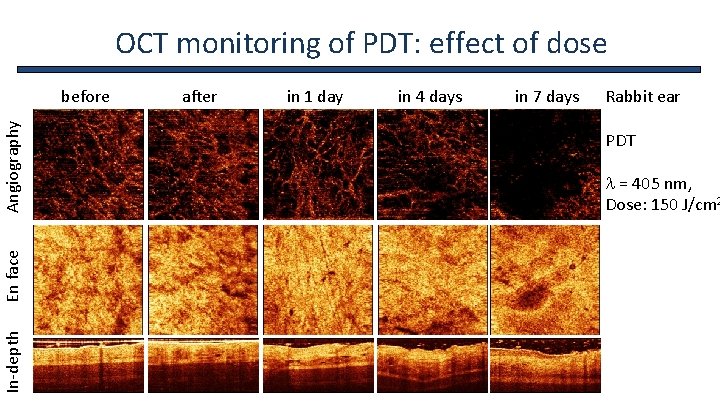
OCT monitoring of PDT: effect of dose before after in 1 day in 4 days in 7 days Rabbit ear In-depth En face Angiography PDT l = 405 nm, Dose: 150 J/cm 2
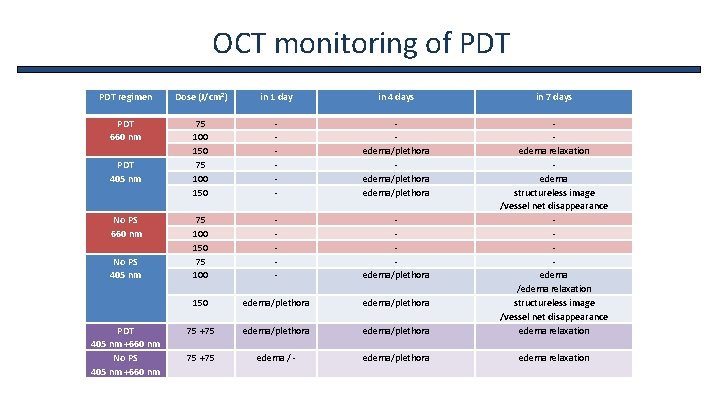
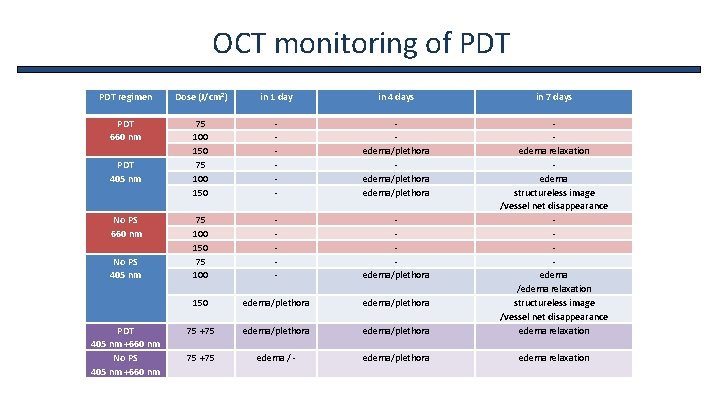
OCT monitoring of PDT regimen Dose (J/cm 2) in 1 day in 4 days in 7 days PDT 660 nm 75 100 150 - edema/plethora 75 100 150 75 100 - edema/plethora 150 edema/plethora 75 +75 edema/plethora edema relaxation edema structureless image /vessel net disappearance edema /edema relaxation structureless image /vessel net disappearance edema relaxation 75 +75 edema / - edema/plethora edema relaxation PDT 405 nm No PS 660 nm No PS 405 nm PDT 405 nm +660 nm No PS 405 nm +660 nm
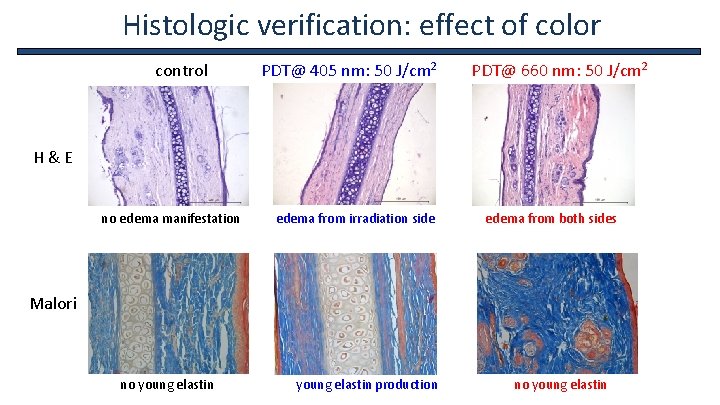
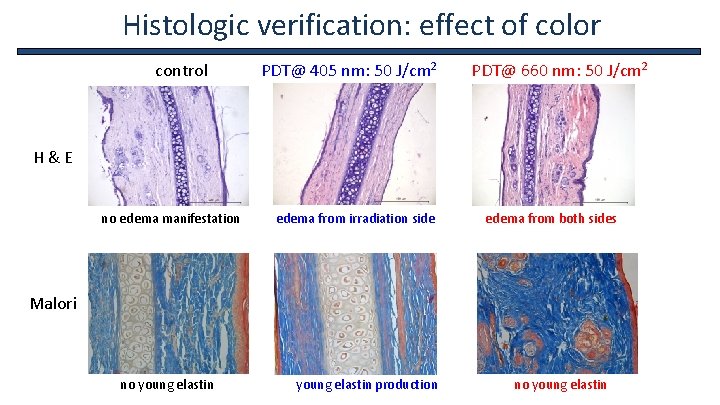
Histologic verification: effect of color control PDT@ 405 nm: 50 J/cm 2 PDT@ 660 nm: 50 J/cm 2 H & E no edema manifestation edema from irradiation side edema from both sides Malori no young elastin young elastin production no young elastin
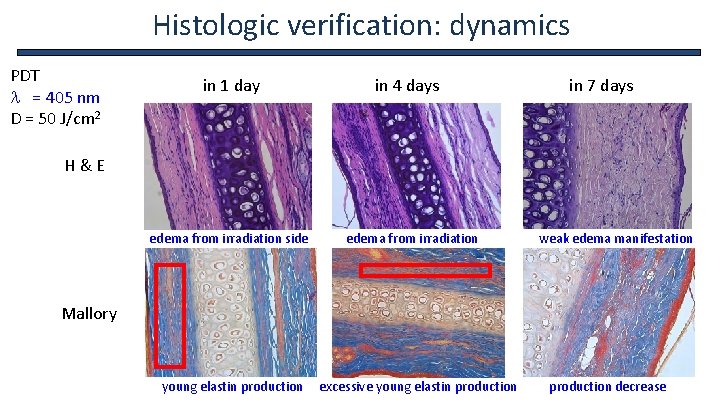
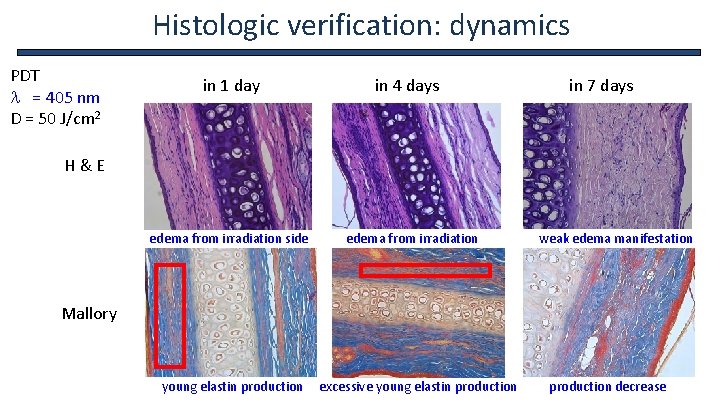
Histologic verification: dynamics PDT l = 405 nm D = 50 J/cm 2 in 1 day in 4 days in 7 days H & E edema from irradiation side edema from irradiation weak edema manifestation Mallory young elastin production excessive young elastin production decrease
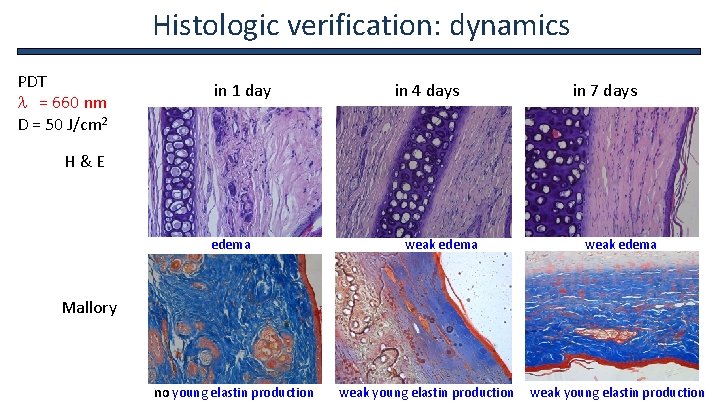
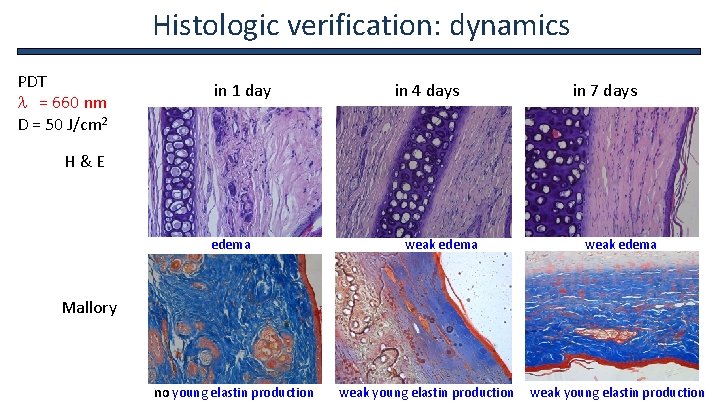
Histologic verification: dynamics PDT l = 660 nm D = 50 J/cm 2 in 1 day in 4 days in 7 days H & E edema weak edema Mallory no young elastin production weak young elastin production
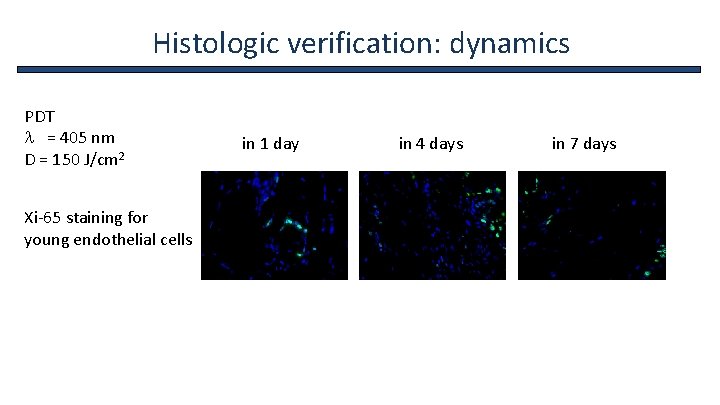
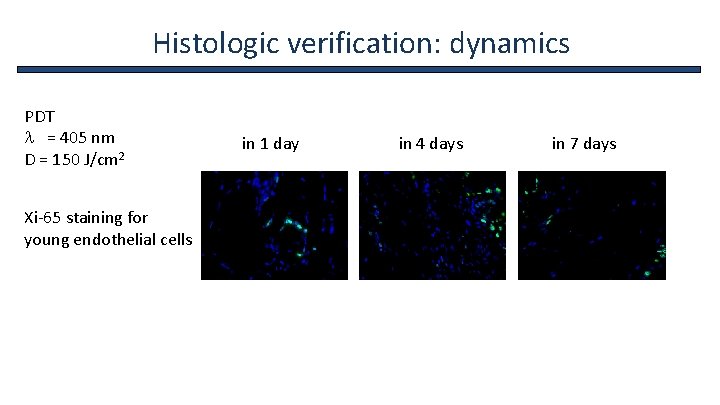
Histologic verification: dynamics PDT l = 405 nm D = 150 J/cm 2 in 1 day in 4 days in 7 days Xi-65 staining for young endothelial cells
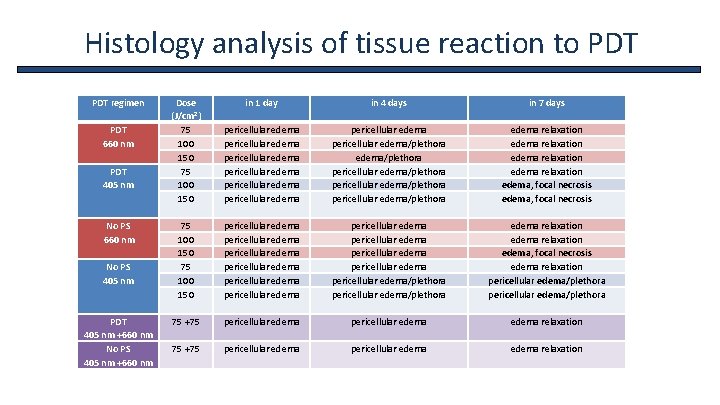
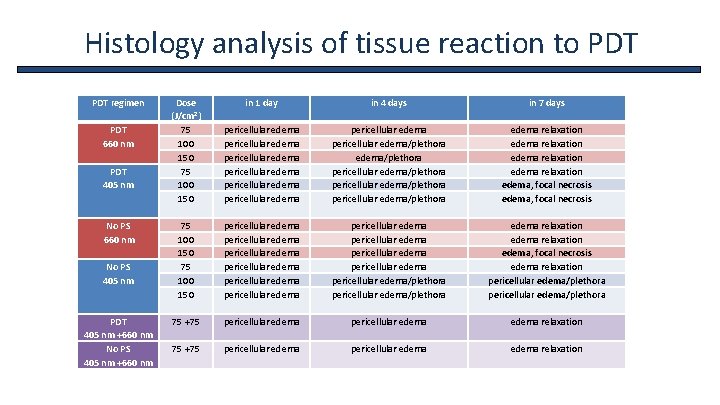
Histology analysis of tissue reaction to PDT regimen PDT 660 nm PDT 405 nm No PS 660 nm No PS 405 nm PDT 405 nm +660 nm No PS 405 nm +660 nm Dose (J/cm 2) 75 100 150 in 1 day in 4 days in 7 days pericellular edema pericellular edema/plethora edema/plethora pericellular edema/plethora edema relaxation edema, focal necrosis 75 100 150 pericellular edema pericellular edema pericellular edema/plethora edema relaxation edema, focal necrosis edema relaxation pericellular edema/plethora 75 +75 pericellular edema edema relaxation
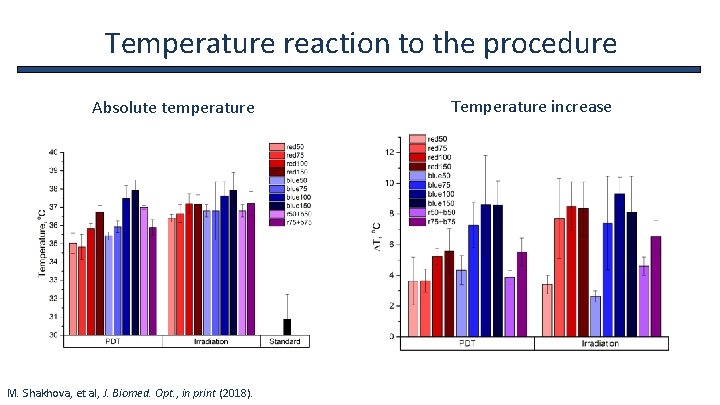
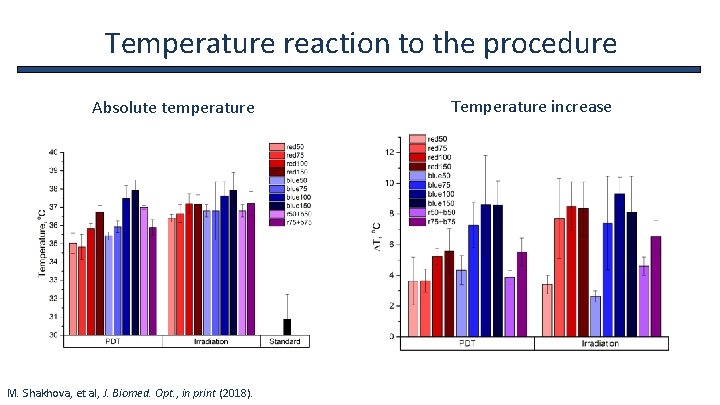
Temperature reaction to the procedure Absolute temperature M. Shakhova, et al, J. Biomed. Opt. , in print (2018). Temperature increase
Diagnostics and treatment of chronic pharyngitis • Chronic rhinitis is among the most frequent pathologies of ENT organs • Traditional diagnostic approaches provide low accuracy in differential diagnostics of chronic pharyngitis • Subjective evaluation of pharynx mucosa state by a clinician in pharyngoscopy may cause incorrect interpretation • Fast non-invasive diagnostic techniques are required • Correct choice of drug treatment requires knowledge the causative agent of the disease • OCT inspection in course of standard pharyngoscopy • PDT may produce wide-range antibacterial effect
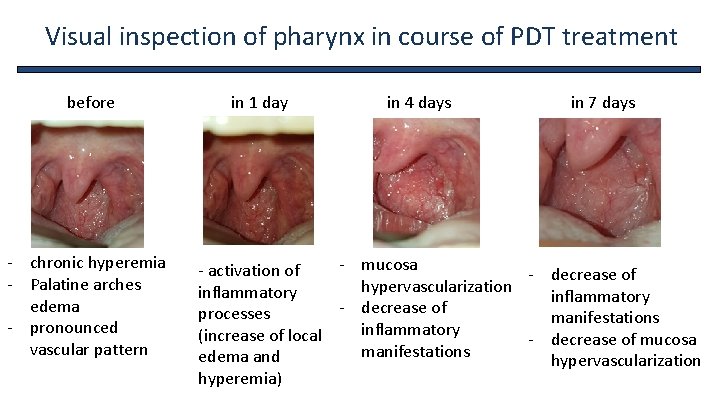
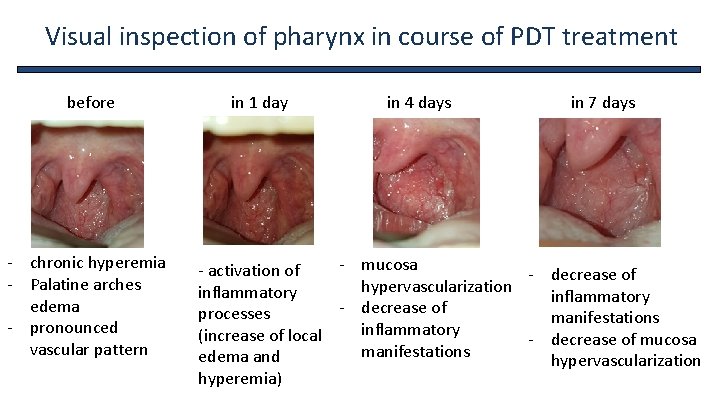
Visual inspection of pharynx in course of PDT treatment before - chronic hyperemia - Palatine arches edema - pronounced vascular pattern in 1 day in 4 days in 7 days - mucosa - activation of - decrease of hypervascularization inflammatory decrease of processes manifestations inflammatory (increase of local - decrease of mucosa manifestations edema and hypervascularization hyperemia)
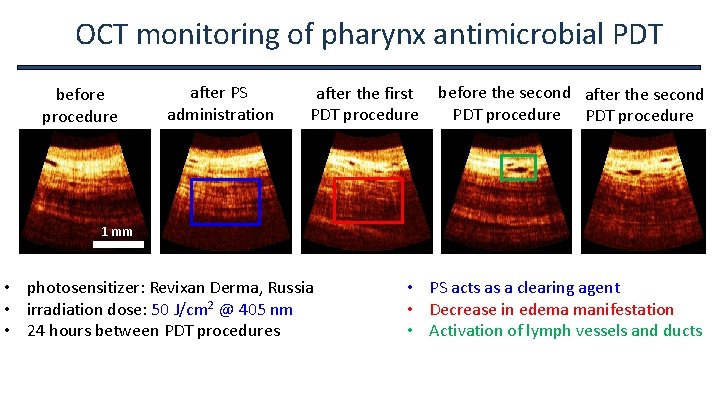
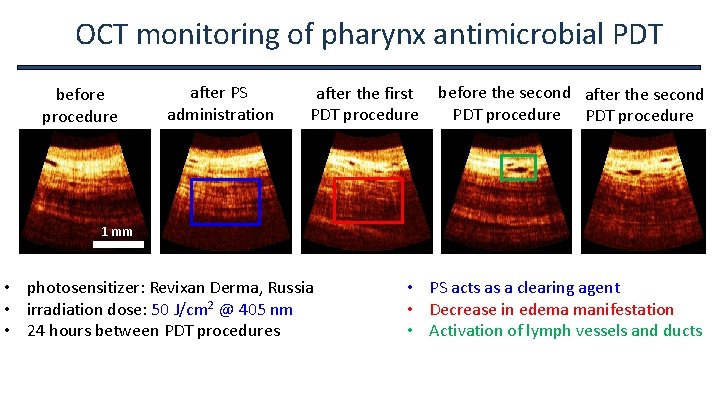
OCT monitoring of pharynx antimicrobial PDT before procedure after PS administration after the first before the second after the second PDT procedure 1 mm • photosensitizer: Revixan Derma, Russia • irradiation dose: 50 J/cm 2 @ 405 nm • 24 hours between PDT procedures • PS acts as a clearing agent • Decrease in edema manifestation • Activation of lymph vessels and ducts
Conclusions • Employment of two wavelengths provide additional optimization of the PDT procedure protocol • Equal light doses provide different effect at different wavelengths • Optical diagnostics techniques allow for non-invasive monitoring and evaluation of the procedure outcome • Monte Carlo OCT simulations allow to predict absorbed dose evaluation provides additional accuracy to adrenaline test results • Dual wavelengths fluorescence monitoring allows to evaluate both penetration and photobleaching of PS

Team Clinicians M. Shakhova A. Meller D. Sapunov A. Shakhov N. Orlinskaya Physicists M. Kirillin E. Sergeeva D. Loginova A. Khilov V. Perekatova I. Turchin

Acknowledgements Russian Science (project 17 -15 -01264) Foundation REVIXAN Ltd. Dr. Natalia Shakhova, MD, D. Sc. , Prof. Institute of Applied Physics RAS, Russia Dr. Sergey Gamayunov, MD, Republican clinical oncologic dispensary, Chuvash Republic, Russia

2019 Nizhny Novgorod - Uglich - Nizhny Novgorod "Konstantin Korotkov" boat 3 -7 August 2019 http: //www. biophotonics. sci-nnov. ru/ Symposium Program Optical Bioimaging (Conference) Biophotonics in Cancer Research (Conference) Clinical Biophotonics (Workshop) Biophotonics in Stem Cells Research (Workshop) Symposium Chairs Amasi Periasami, University of Virginia, USA Ilya Turchin, Institute of Applied Physics RAS, Russia Alfred Vogel, University of Luebeck, Germany Elena Zagaynova, Privolzhskiy Research Medical University, Russia

Thank you for your attention! Questions?