Nottinghamshire COPD and Asthma Guidelines Dr Esther Gladman


- Slides: 33

Nottinghamshire COPD and Asthma Guidelines Dr Esther Gladman GP Prescribing Lead, Medicines Management Nottingham City CCG Feb 2012

Where to find & other resources • Google: Nottinghamshire Area Prescribing Committee – Medicines Traffic Light Classification List – Shared Care Protocols – Clinical Guidelines – Formularies – Policies and Prescribing Position Statements • E-healthscope • www. patient. co. uk • www. prodigy. nhs. uk (was CKS)
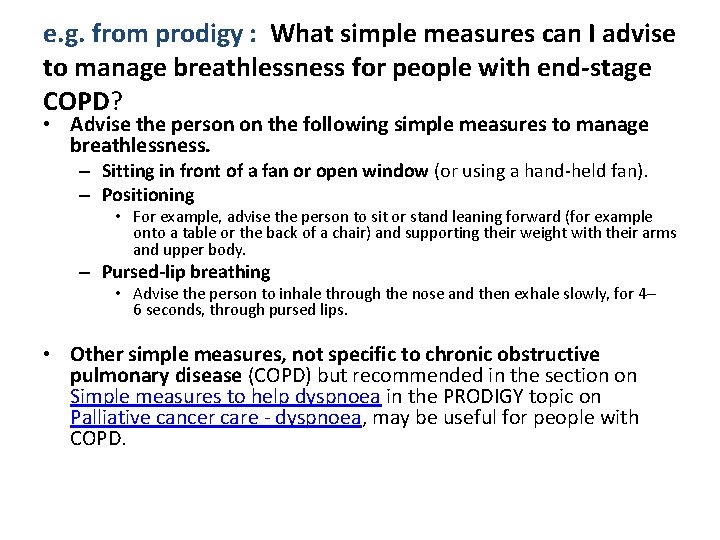
e. g. from prodigy : What simple measures can I advise to manage breathlessness for people with end-stage COPD? • Advise the person on the following simple measures to manage breathlessness. – Sitting in front of a fan or open window (or using a hand-held fan). – Positioning • For example, advise the person to sit or stand leaning forward (for example onto a table or the back of a chair) and supporting their weight with their arms and upper body. – Pursed-lip breathing • Advise the person to inhale through the nose and then exhale slowly, for 4– 6 seconds, through pursed lips. • Other simple measures, not specific to chronic obstructive pulmonary disease (COPD) but recommended in the section on Simple measures to help dyspnoea in the PRODIGY topic on Palliative cancer care - dyspnoea, may be useful for people with COPD.
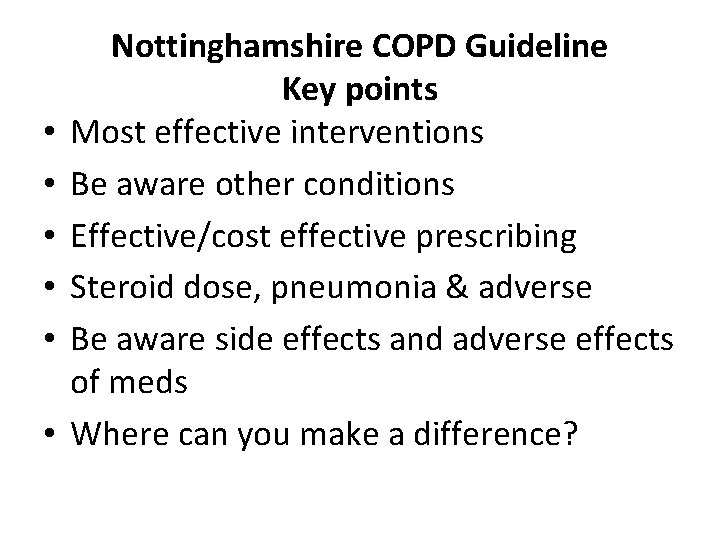
• • • Nottinghamshire COPD Guideline Key points Most effective interventions Be aware other conditions Effective/cost effective prescribing Steroid dose, pneumonia & adverse Be aware side effects and adverse effects of meds Where can you make a difference?
Most Effective Interventions • 1. Stopping smoking is the only treatment that slows the progression of COPD and is the most cost effective treatment in COPD. NNT 5 –to prevent death at age 70 • Motivational questioning, cost cigs & inhalers, Allen Carr, anxiety, dopamine, worsening of symptoms, dementia
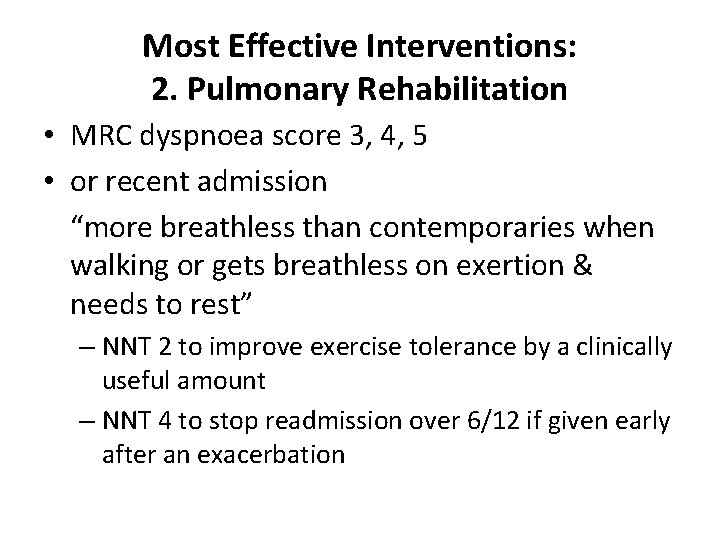
Most Effective Interventions: 2. Pulmonary Rehabilitation • MRC dyspnoea score 3, 4, 5 • or recent admission “more breathless than contemporaries when walking or gets breathless on exertion & needs to rest” – NNT 2 to improve exercise tolerance by a clinically useful amount – NNT 4 to stop readmission over 6/12 if given early after an exacerbation
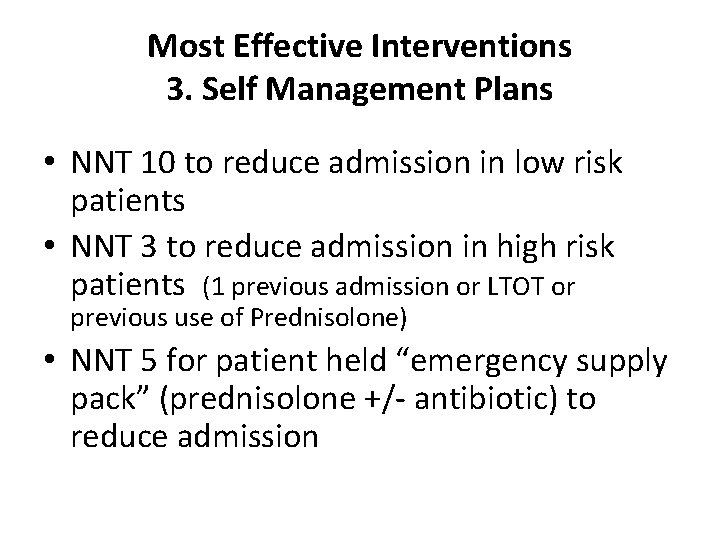
Most Effective Interventions 3. Self Management Plans • NNT 10 to reduce admission in low risk patients • NNT 3 to reduce admission in high risk patients (1 previous admission or LTOT or previous use of Prednisolone) • NNT 5 for patient held “emergency supply pack” (prednisolone +/- antibiotic) to reduce admission
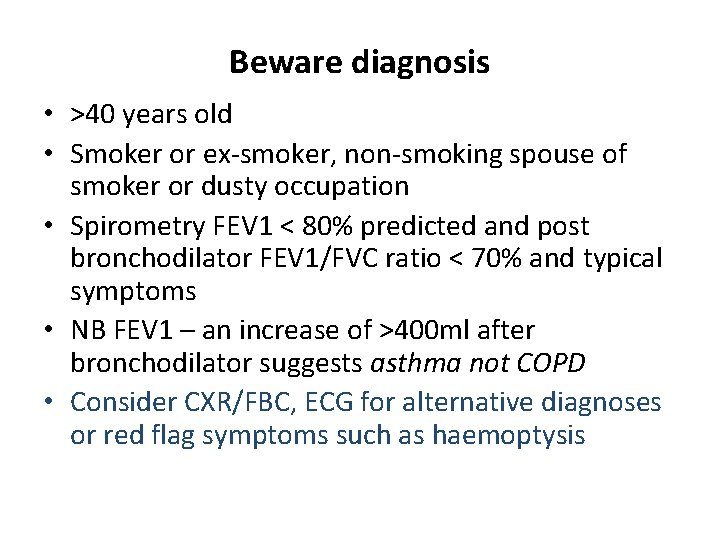
Beware diagnosis • >40 years old • Smoker or ex-smoker, non-smoking spouse of smoker or dusty occupation • Spirometry FEV 1 < 80% predicted and post bronchodilator FEV 1/FVC ratio < 70% and typical symptoms • NB FEV 1 – an increase of >400 ml after bronchodilator suggests asthma not COPD • Consider CXR/FBC, ECG for alternative diagnoses or red flag symptoms such as haemoptysis
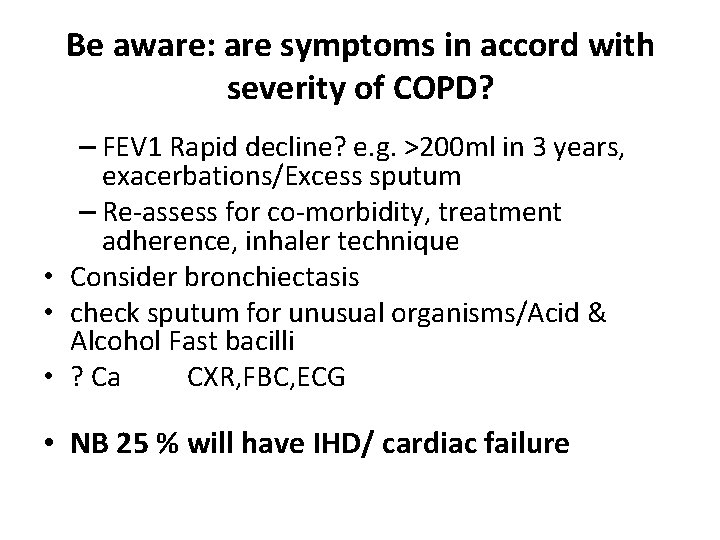
Be aware: are symptoms in accord with severity of COPD? – FEV 1 Rapid decline? e. g. >200 ml in 3 years, exacerbations/Excess sputum – Re-assess for co-morbidity, treatment adherence, inhaler technique • Consider bronchiectasis • check sputum for unusual organisms/Acid & Alcohol Fast bacilli • ? Ca CXR, FBC, ECG • NB 25 % will have IHD/ cardiac failure
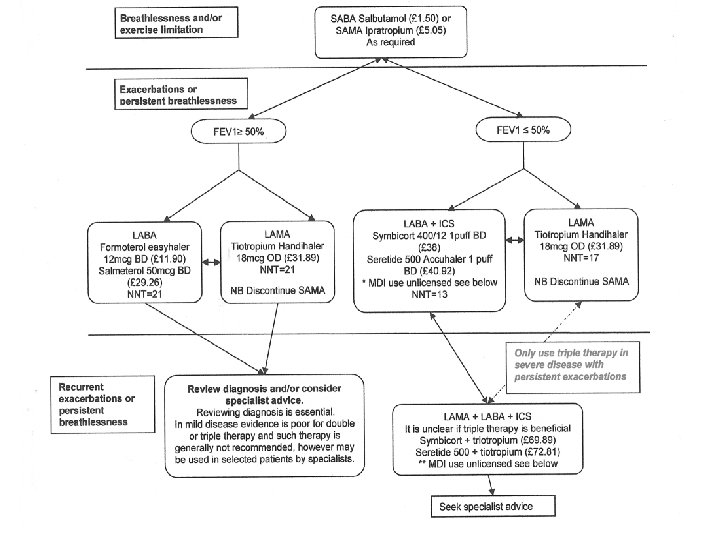
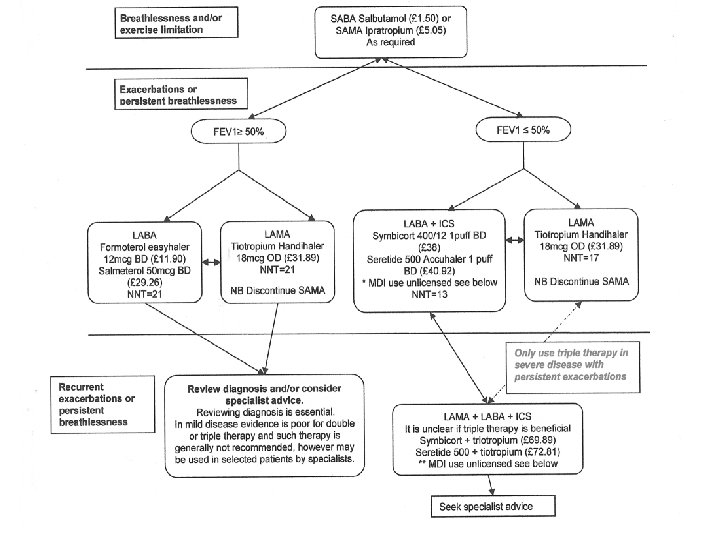
Effective/cost effective prescribing • Stop smoking • Optimise inhaler technique (e. g. spacers with MDIs) • Consider stopping new treatment if patient feels no improvement (4 weeks) – longer may be needed for a reduction in exacerbations • Consider stepping down/swopping
Effective/cost effective prescribing • LABA vs LAMA – there is no significant difference re: reduction in exacerbation or hospitalisation rates.
Effective/cost effective prescribing • There is no combination MDI licensed for COPD • However if patient preference: – Fostair 100/6 (2 puffs BD £ 29. 32) – or Seretide 125 + spacer (2 puffs BD, £ 35) can be considered, which gives similar ICS dose to Accuhaler 500. • NB Seretide 250 MDI is not recommended
Adverse effects of steroid • High dose ICS (ie fluticasone 1000 mcg = Seretide 250) increases the risk of pneumonia, NNH = 47 ie. Beware those with frequent exacerbations • Other steroid effects - Diab/thrush/cataracts • Osteoporosis prophylaxis for patients having 4 courses of oral steroid within 12 months
Be aware side effects and adverse effects of meds • Use tiotropium Spiriva Handihaler® (18 mcg/day) not Spiriva Respimat® (mist device) All patients must be advised not to exceed the maximum daily dose • All anticholinergics have some cardiovascular effect • Fometerol and beta agonists also have effect
NBs • Mucolytic only if troublesome phlegm: carbocisteine 750 mg TDS (£ 24. 60) can be trialled for 4 weeks. – – Stop if no effect. Drop to maintenance dose: 750 mg BD if effective. Consider using in winter months only. Mucolytics do not prevent exacerbations • Consider theophylline 3 rd line: Uniphyllin 200 mg BD (£ 2. 94) care with elderly & concomitant medications see BNF. Theophylline levels? NNT=33
NBs • 25% will have co-morbidity e. g. IHD/cardiac failure. Beta blockers can be used in COPD • Dose of emergency supply pack?
Actions Flu & pneumococcal vaccination Inhaler use/Medication /step Stop smoking advice /refer New Leaf Patient info/empowerment MRC dyspnoea score 3, 4 or 5/functional disability refer for pulmonary rehabilitation • Self management plan and anticipatory prescription pack • Weight/diet/exercise. Little & often leaflets • • •
• Oxygen Sat ≤ 92% - refer to chest clinic /oxygen assessment service • Palliative Care Planning If end-stage COPD/cor pulmonale
Nottinghamshire Adult Asthma Treatment Summary • Micro break & shake
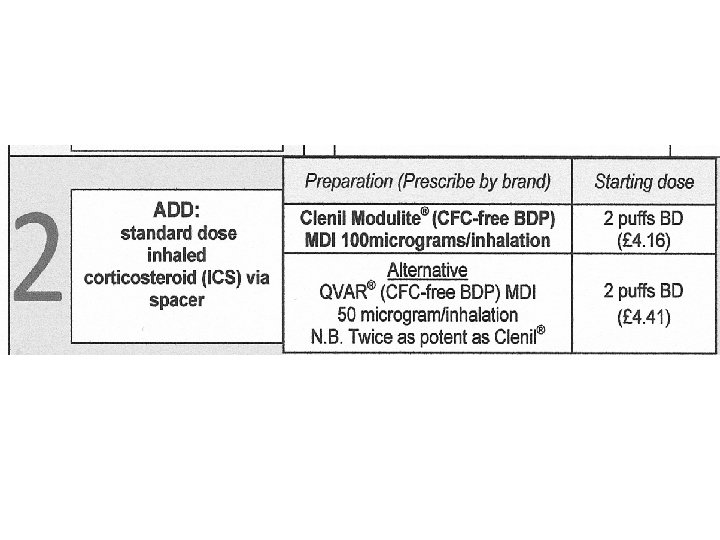
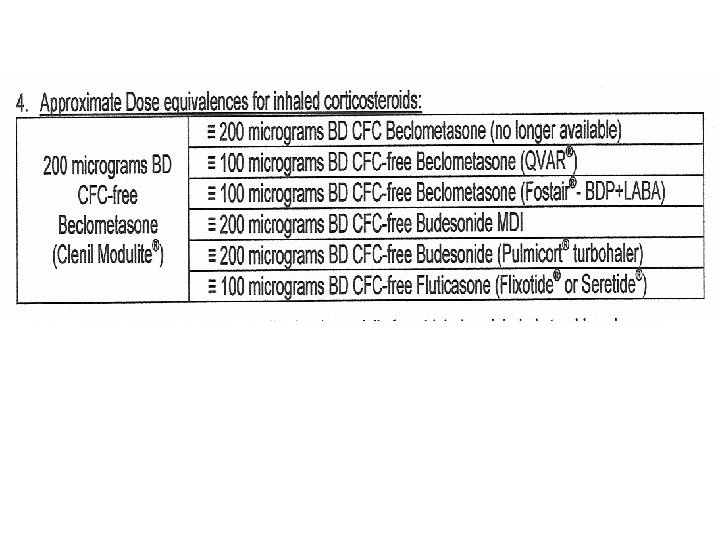
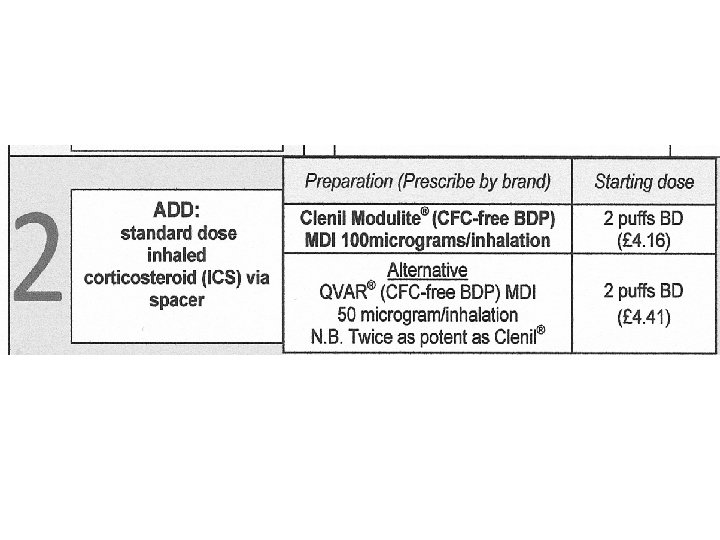
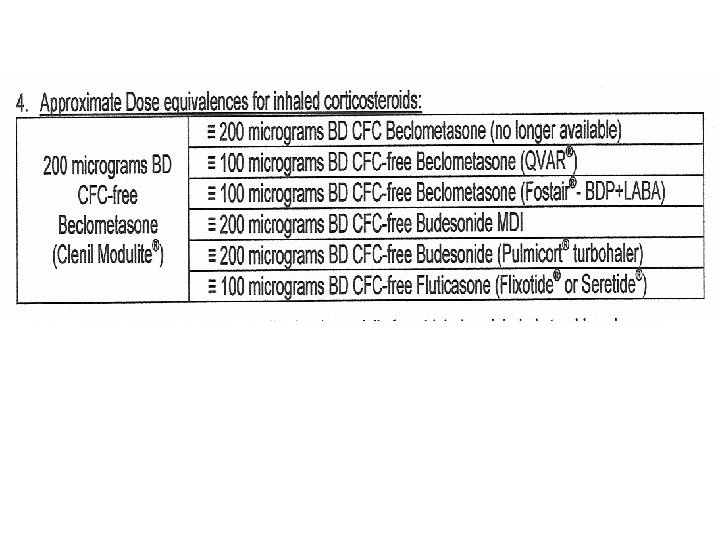
Nottinghamshire Asthma Guideline Key points • • Step up and down Use LABA and ICS in a combination inhaler Be aware of inhaler equivalent steroid doses Step 3 a is addition of LABA not increase ICS too Twitchiness of asthma Same steroid risks as for COPD Pros & cons of SMART Theophylline levels/interactions
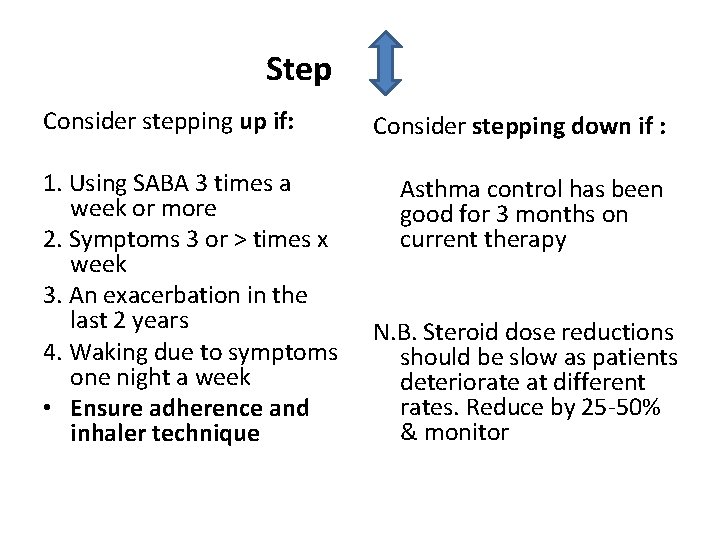
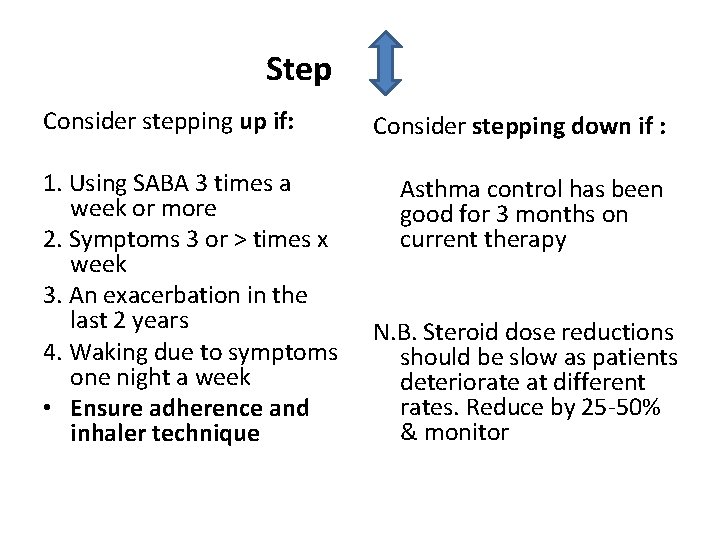
Step Consider stepping up if: 1. Using SABA 3 times a week or more 2. Symptoms 3 or > times x week 3. An exacerbation in the last 2 years 4. Waking due to symptoms one night a week • Ensure adherence and inhaler technique Consider stepping down if : Asthma control has been good for 3 months on current therapy N. B. Steroid dose reductions should be slow as patients deteriorate at different rates. Reduce by 25 -50% & monitor
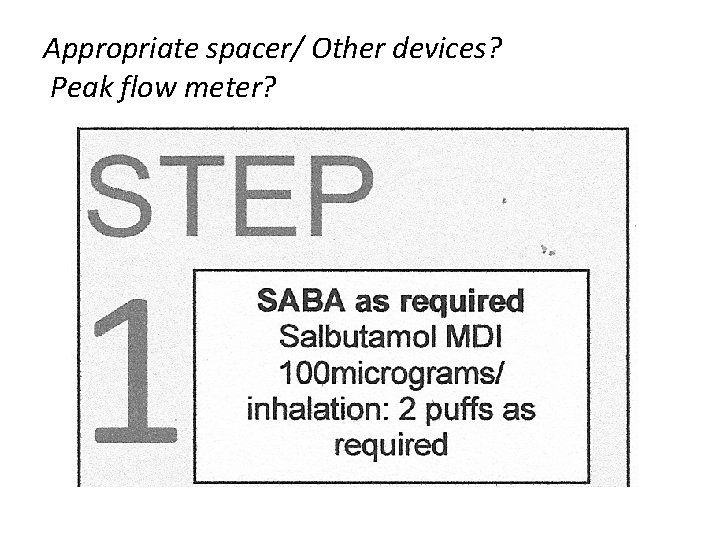
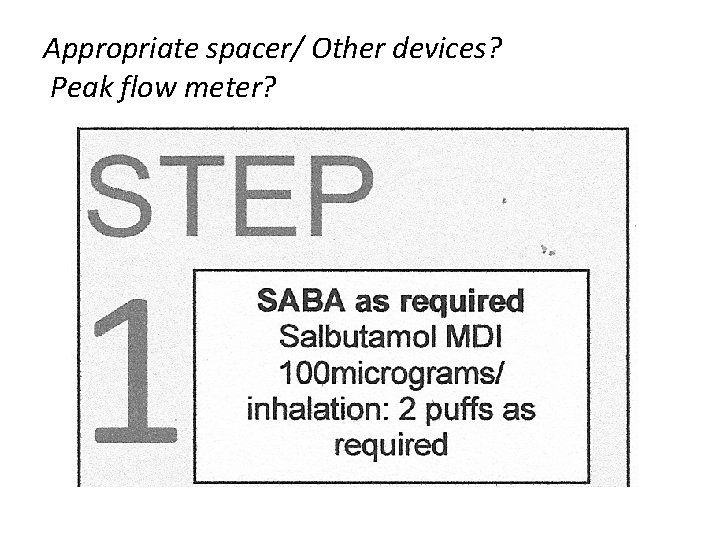
Appropriate spacer/ Other devices? Peak flow meter?
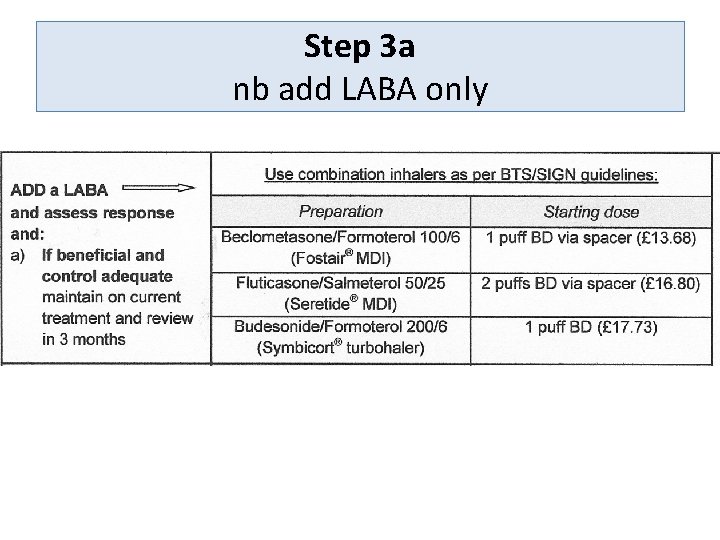
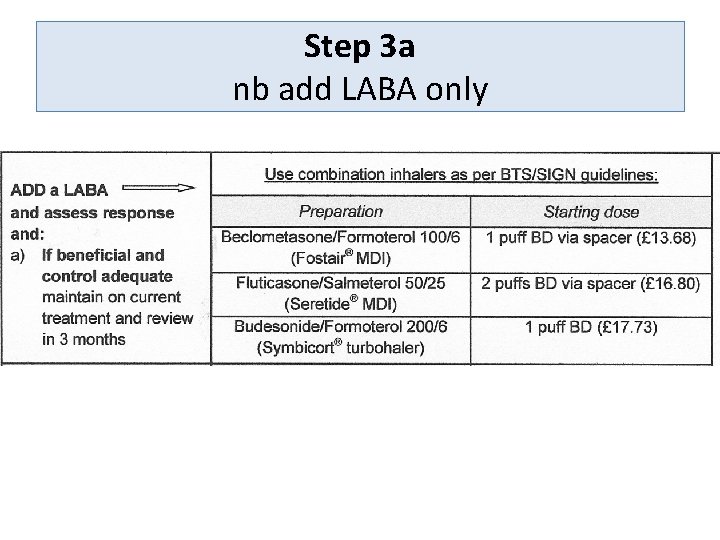
Step 3 a nb add LABA only
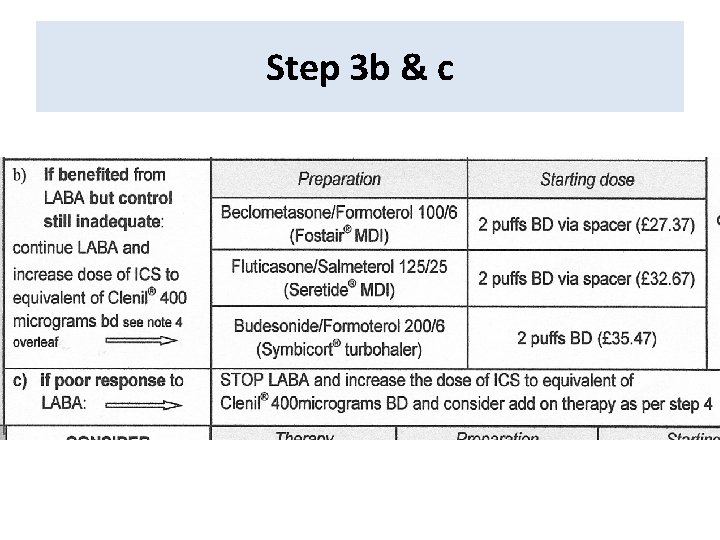
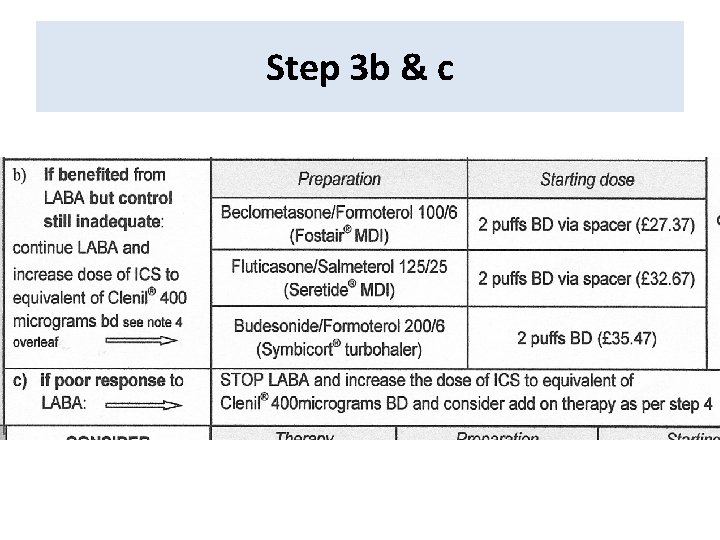
Step 3 b & c
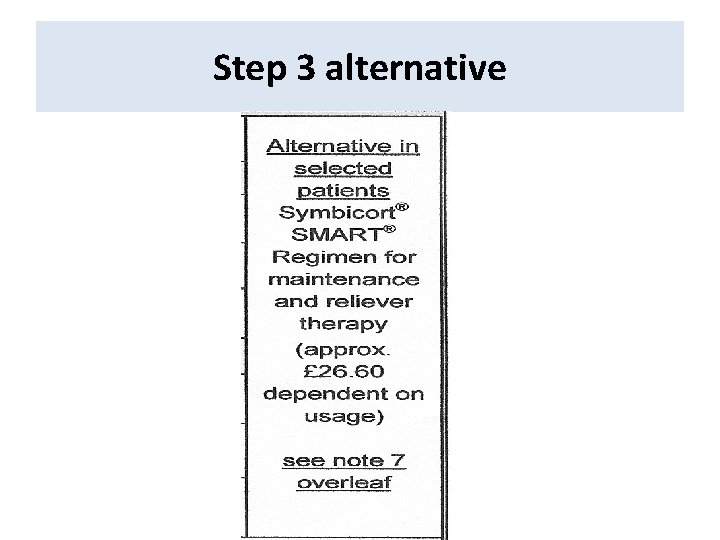
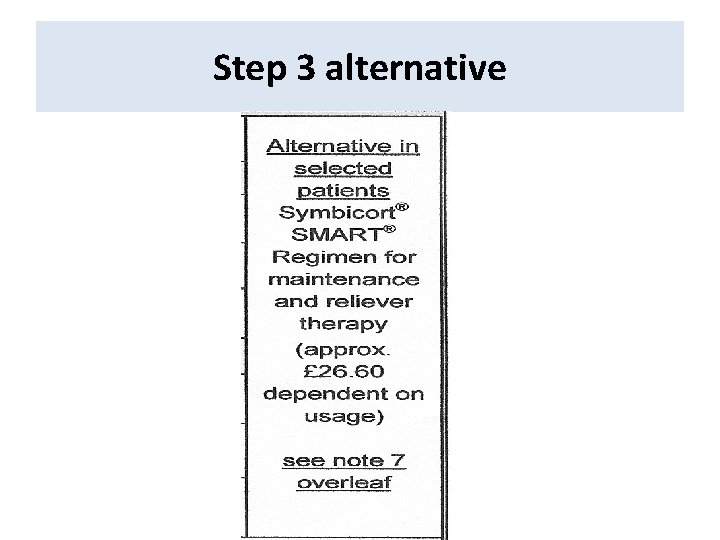
Step 3 alternative
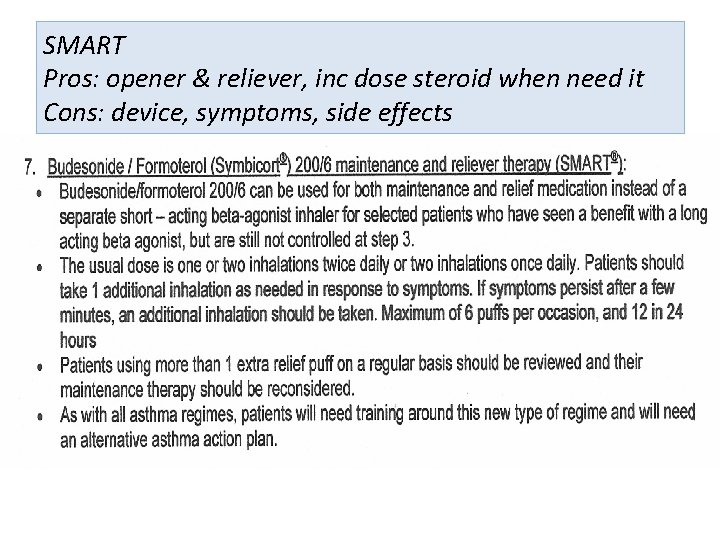
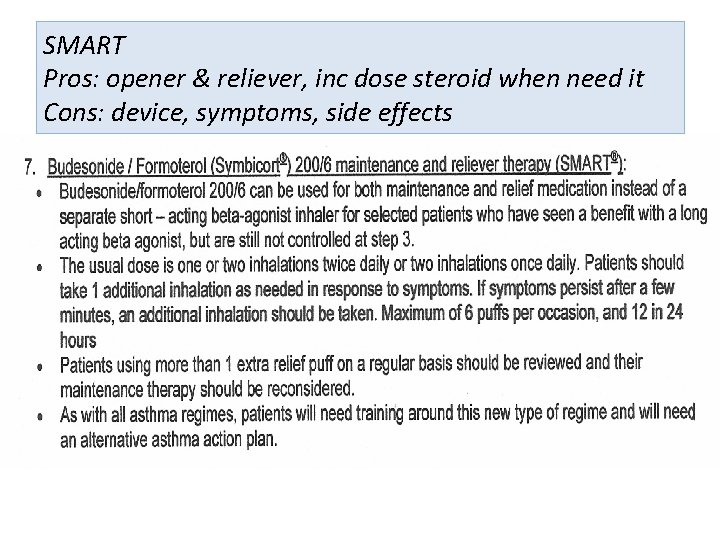
SMART Pros: opener & reliever, inc dose steroid when need it Cons: device, symptoms, side effects
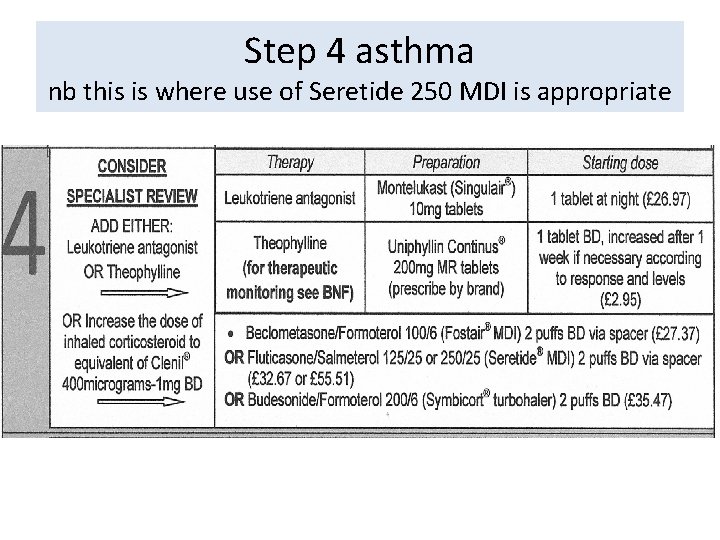
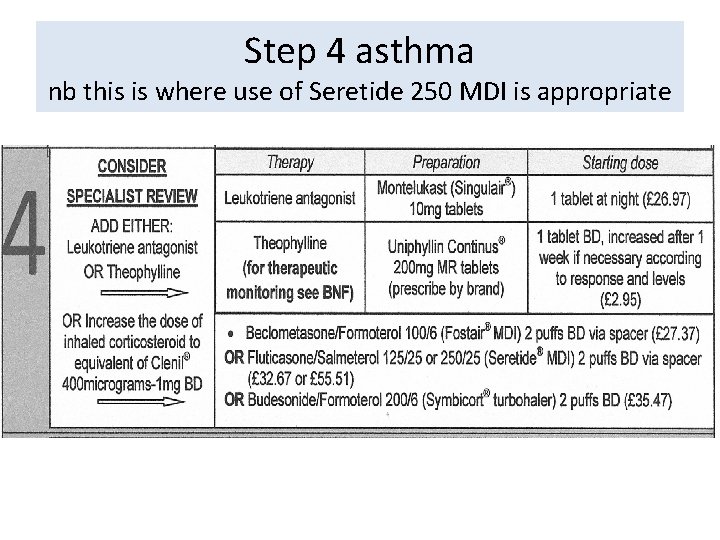
Step 4 asthma nb this is where use of Seretide 250 MDI is appropriate
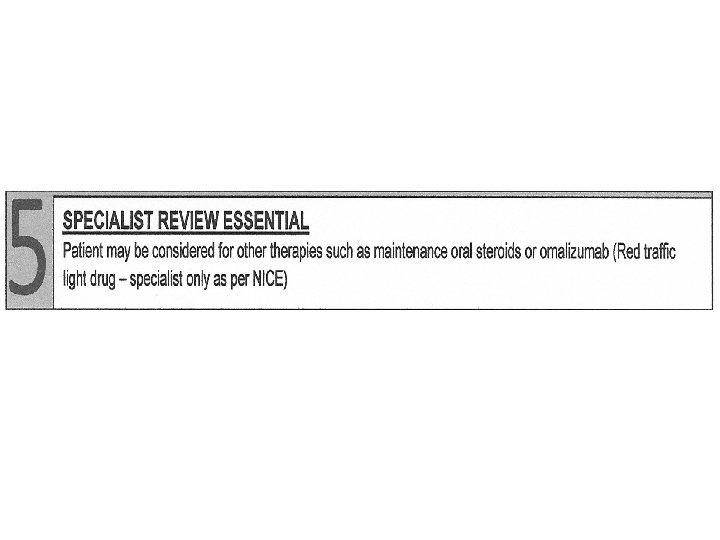
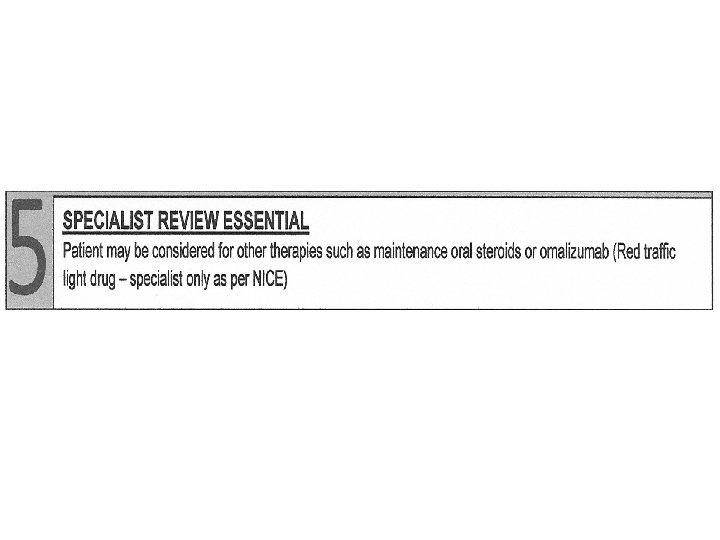
nb • Oral steroid - sometimes higher dose & shorter course than COPD • Same steroid risks as for COPD • Written Self-Management Plan/lifestyle/house dust mite/patient beliefs/info • Co-morbidity
Key points summary • Step up and down • Always give LABA and ICS in combination inhaler (unlike COPD) • Step 3 a is addition of LABA not increase ICS too • Be aware potency of ICS Inhaler and equivalent steroid doses
 Brett gladman
Brett gladman Spirometry
Spirometry Asthma vs copd spirometry
Asthma vs copd spirometry Nottingham and nottinghamshire ics
Nottingham and nottinghamshire ics Status asthmaticus pathophysiology
Status asthmaticus pathophysiology Nottinghamshire
Nottinghamshire Connected nottinghamshire
Connected nottinghamshire Gina
Gina Asthma grading
Asthma grading Ipassbaton
Ipassbaton Interstitialis rajzolat a tüdőben
Interstitialis rajzolat a tüdőben Bipap settings for copd
Bipap settings for copd Cat score copd
Cat score copd Cat score copd
Cat score copd Tam chứng anthonisen
Tam chứng anthonisen Gina asthma
Gina asthma Non pharmacological treatment for copd
Non pharmacological treatment for copd Copd netwerk
Copd netwerk Lets be copd
Lets be copd Sbar copd
Sbar copd Barrel chested
Barrel chested Copd exacerbation nursing management
Copd exacerbation nursing management Copd v/q mismatch
Copd v/q mismatch Copd national action plan
Copd national action plan Bitemporal wasting in copd
Bitemporal wasting in copd Copd exacerbation nursing management
Copd exacerbation nursing management Copd abcd assessment
Copd abcd assessment Left parasternal heave
Left parasternal heave Exacerbatie copd
Exacerbatie copd Terminale copd
Terminale copd Copd stervensfase
Copd stervensfase Centrilobular emphysema
Centrilobular emphysema Yellow phlegm cough
Yellow phlegm cough Copd full form
Copd full form