Nose sinus nasopharynx Dr K Outhoff Contents Allergic

- Slides: 34
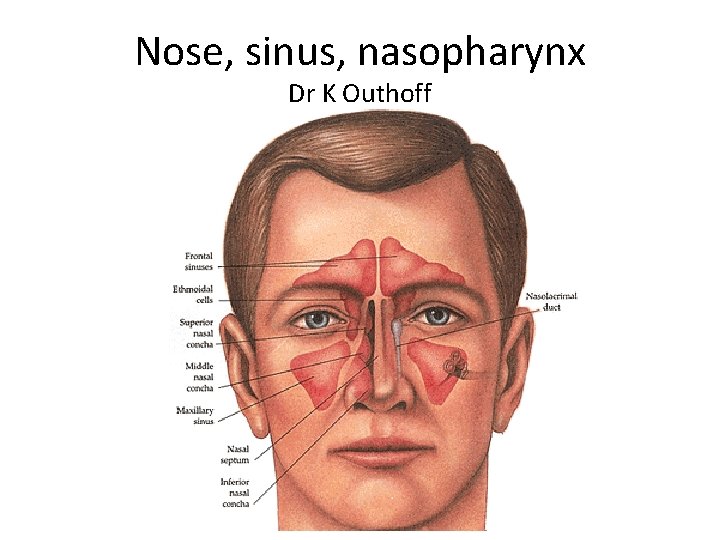
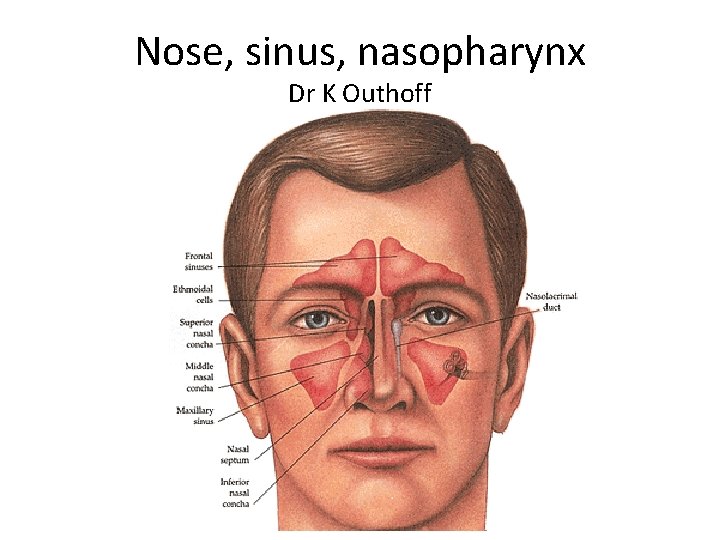
Nose, sinus, nasopharynx Dr K Outhoff
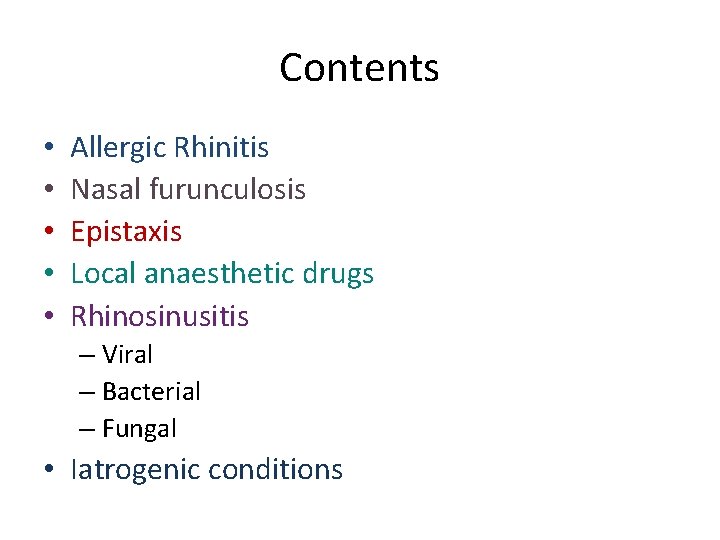
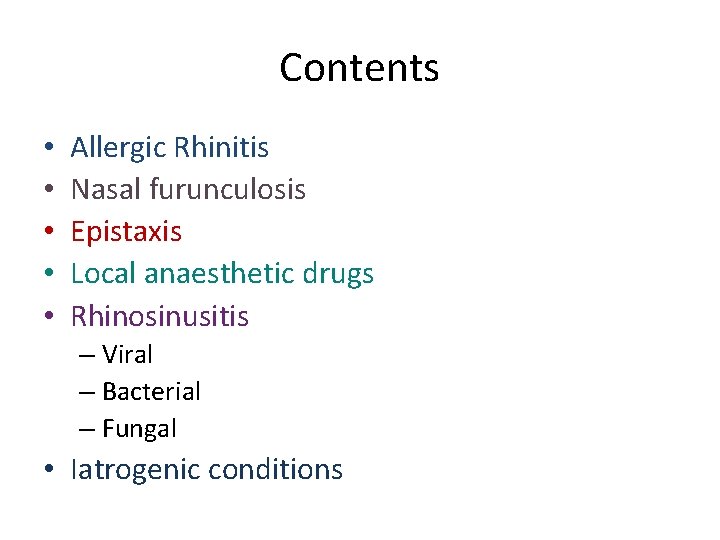
Contents • • • Allergic Rhinitis Nasal furunculosis Epistaxis Local anaesthetic drugs Rhinosinusitis – Viral – Bacterial – Fungal • Iatrogenic conditions
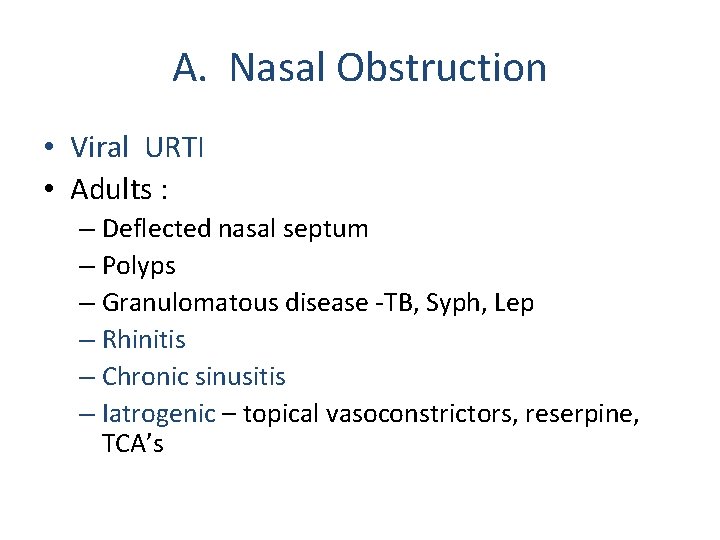
A. Nasal Obstruction • Viral URTI • Adults : – Deflected nasal septum – Polyps – Granulomatous disease -TB, Syph, Lep – Rhinitis – Chronic sinusitis – Iatrogenic – topical vasoconstrictors, reserpine, TCA’s
A. Nasal obstruction • Children: – large adenoids – choanal atresia – post nasal space tumours (angiofibromata) – foreign body – rhinitis

Allergic rhinitis
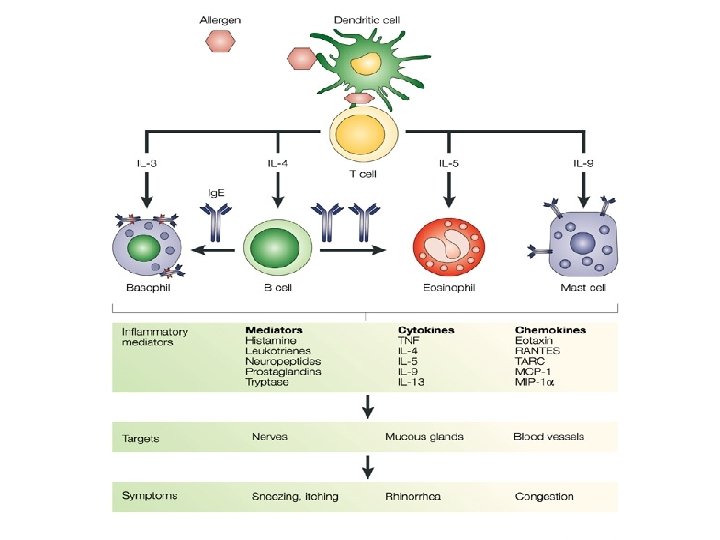
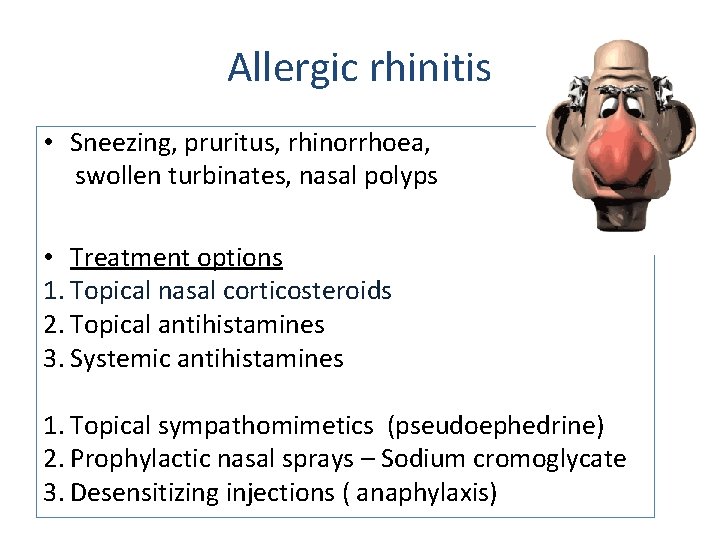
Allergic rhinitis • Sneezing, pruritus, rhinorrhoea, swollen turbinates, nasal polyps • Treatment options 1. Topical nasal corticosteroids 2. Topical antihistamines 3. Systemic antihistamines 1. Topical sympathomimetics (pseudoephedrine) 2. Prophylactic nasal sprays – Sodium cromoglycate 3. Desensitizing injections ( anaphylaxis)
Topical corticosteroid nasal sprays mainstay of treatment • Effective, fewer side effects than oral or parenteral routes, minimal absorption from nasal mucosa • Reduce swelling and stuffiness • Take a few days to work at full potential – – – Beclomethasone Budesonide Triamcinolone Mometasone Fluticasone (may dry nasal mucosa; crusting, bleeding)
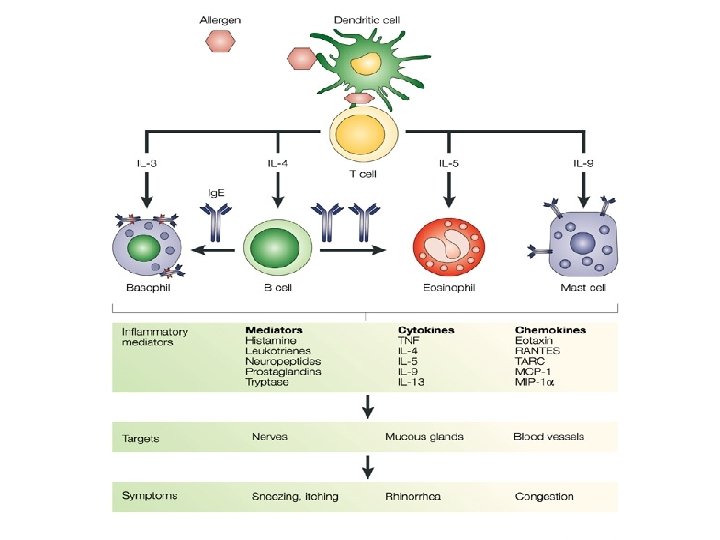
Histamine • Found largely in mast cell and basophil granules in skin, lungs, GIT • and histaminergic neurones in brain • Mediator of hypersensitivity response • Acts on H-1 receptors: – Contracts smooth muscle (ileum, bronchioles, uterus) – Dilates blood vessels – Increased vascular permeability – Itching from sensory neuronal stimulation
Topical antihistamines (H-1) for allergic rhinitis • Azelastine: – Also inhibits release of inflammatory cytokines • Levocabastine: – Long acting – For short term symptomatic treatment
Systemic Antihistamines (H-1) • • ↓rhinorrhoea sneezing, eye symptoms Not as effective as steroids for nasal congestion Newer antihistamines: relatively free of sedation, alcohol, benzo potentiation as do not cross BBB • • • Chlorpheneramine (Allergex – old generation) Cetirizine (Zyrtec) Levocetirizine Loratidine Desloratidine Fexofenadine
Systemic antihistamines Well absorbed Metabolised in liver Excreted in urine Older antihistamines: Peripheral anti-muscarinic effects : dryness of mouth, blurred vision, constipation, urinary retention, and sedation • Newer antihistamines: Less sedating, prolongation QT interval • •
Topical sympathomimetic decongestants • Oxymetazoline (Iliadin N/Spray) • Xylometazoline • Ephedrine –containing preparations – Vasoconstrictors, ↓oedema – Useful if severe congestion preventing topical steroids, cromoglycate from working – Limit use to 2 -3 days – Beware rhinitis medicamentosa
Sodium Cromoglycate nasal spray / drops • • • May be used for allergic conjunctivitis and rhinitis Prevents release of mediators from mast cells Mucous membranes less sensitive to allergens Use long term, preventative Well tolerated Short lived sneezing, nasal irritation • NO LONGER AVAILABLE IN RSA as nose drops. (eye drops still available)
Systemic corticosteroids • • Intractable, severe allergic rhinitis Short course oral prednisolone Anti-inflammatory Prolonged use can suppress adrenal production of corticosteroids Abrupt discontinuation →nausea, vomiting, shock Mask signs of infection Impair natural immune response to infection For specialist use only • SAMF 2008: ‘systemic steroids have no role in the routine management of allergic rhinitis’
Systemic corticosteroids cont. . . • Impair calcium absorption, new bone formation • Short course prednisolone well tolerated • Prolonged use: fluid retention, weight gain, potassium loss, headache, muscle weakness, peptic ulceration, easy bruising, convulsions, psychiatric symptoms, etc!
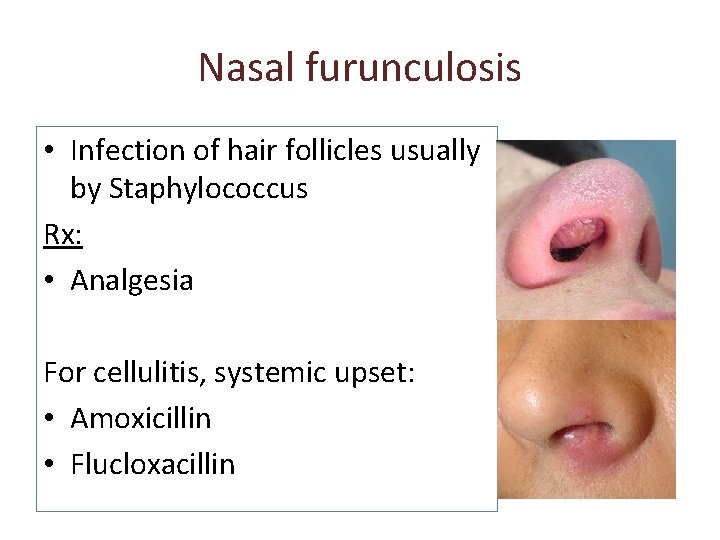
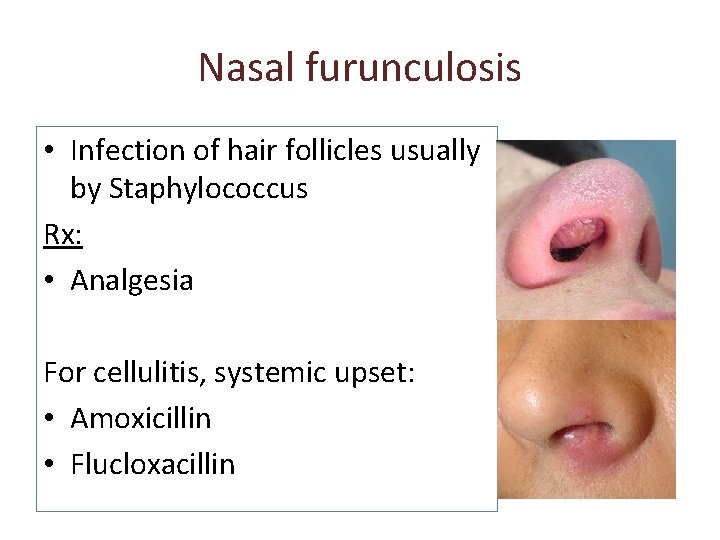
Nasal furunculosis • Infection of hair follicles usually by Staphylococcus Rx: • Analgesia For cellulitis, systemic upset: • Amoxicillin • Flucloxacillin
Drug treatment of Epistaxis • First aid, ice, transfusion • 2. 5 -10% Cocaine solution nasal spray: anaesthetises and constricts vessels • Anterior ribbon gauze pack with paraffin, iodoform paste • Posterior pack
Local Anaesthetic Drugs I: Cocaine surface local anaesthetic reuptake inhibitor of sympathomimetic amines: • intense vasoconstriction • mydriasis of pupil • anxiety • tremor • euphoria
Local Anaesthetic Drugs II: Lignocaine: • • IV regional anaesthesia Infiltration anaesthesia (with or without vasoconstrictor, adrenaline) Epidural anaesthesia Topical anaesthesia – Spray – Gel Rapid diffusion through tissues (2 -3 min) Duration of action: 1 -3 hours • Side effects: dose related: – Dizziness, agitation – Drowsiness, respiratory depression, convulsions – Heart block: direct effect – Nausea, vomiting, transient tinnitus • amide-type local anaesthetic
Paranasal sinuses • • • Ciliated cells sweep mucous into nose Viral infections depress cilia activity Cause oedema around sinus ostia to nose Collection of stagnating mucous May become secondarily infected by bacteria • Polyps, deflected septum, nasal mucosal swelling, tooth roots, also predispose.
Rhinosinusitis • Viral – Acute: no antibiotics • Bacterial – Acute: see next – Chronic: culture for anaerobes (Bacteroides) and Staphylococcus • Fungal – Invasive – Non-invasive
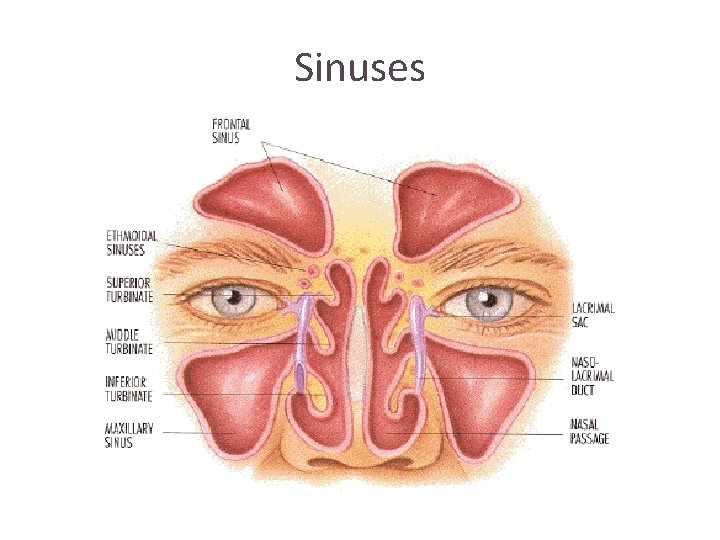
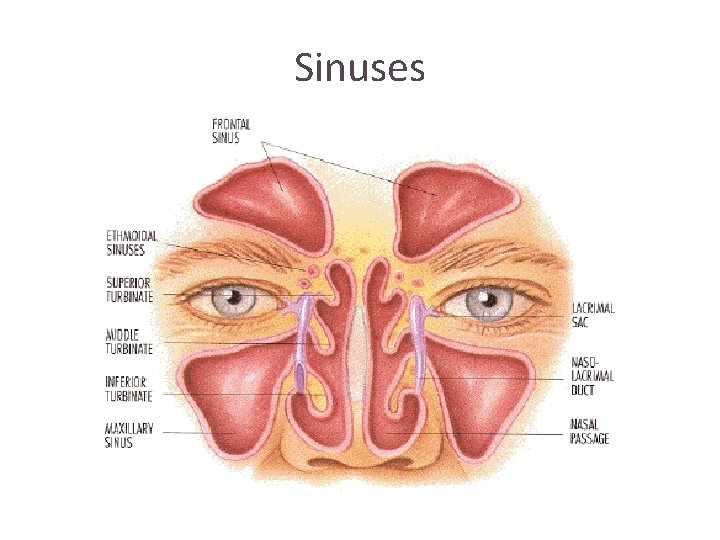
Sinuses
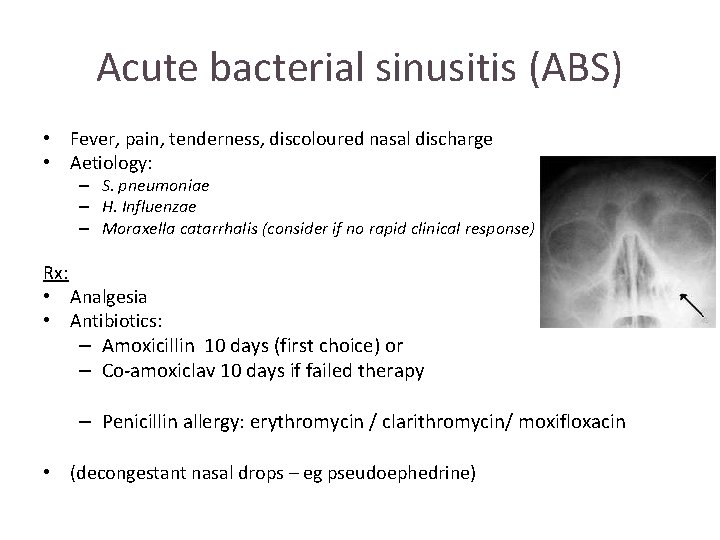
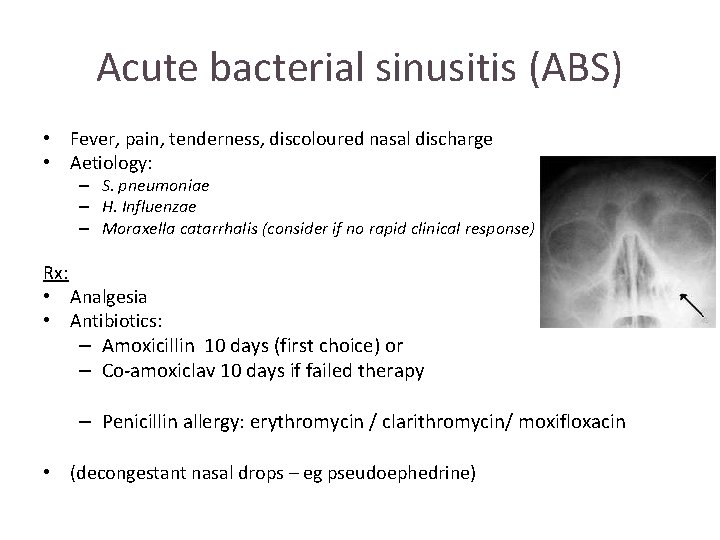
Acute bacterial sinusitis (ABS) • Fever, pain, tenderness, discoloured nasal discharge • Aetiology: – S. pneumoniae – H. Influenzae – Moraxella catarrhalis (consider if no rapid clinical response) Rx: • Analgesia • Antibiotics: – Amoxicillin 10 days (first choice) or – Co-amoxiclav 10 days if failed therapy – Penicillin allergy: erythromycin / clarithromycin/ moxifloxacin • (decongestant nasal drops – eg pseudoephedrine)
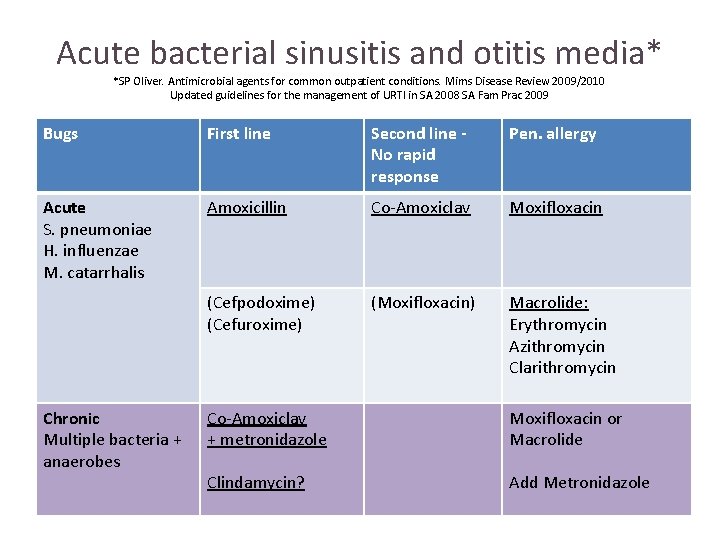
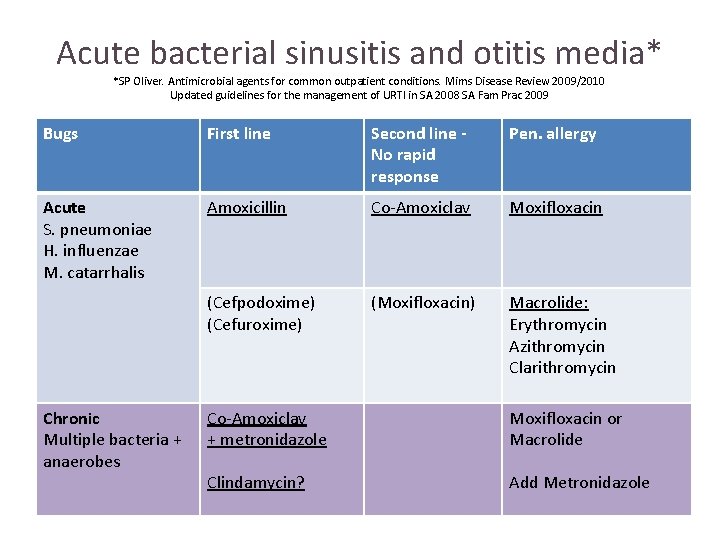
Acute bacterial sinusitis and otitis media* *SP Oliver. Antimicrobial agents for common outpatient conditions. Mims Disease Review 2009/2010 Updated guidelines for the management of URTI in SA 2008 SA Fam Prac 2009 Bugs First line Second line No rapid response Pen. allergy Acute S. pneumoniae H. influenzae M. catarrhalis Amoxicillin Co-Amoxiclav Moxifloxacin (Cefpodoxime) (Cefuroxime) (Moxifloxacin) Macrolide: Erythromycin Azithromycin Clarithromycin Chronic Multiple bacteria + anaerobes Co-Amoxiclav + metronidazole Moxifloxacin or Macrolide Clindamycin? Add Metronidazole
Amoxicillin • • Beta-lactam penicillin Inhibits bacterial cell wall synthesis Stomach upset Allergic reactions
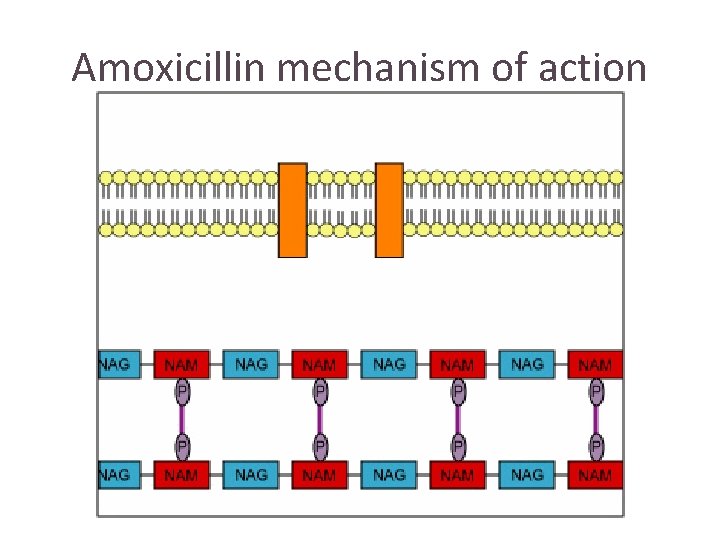
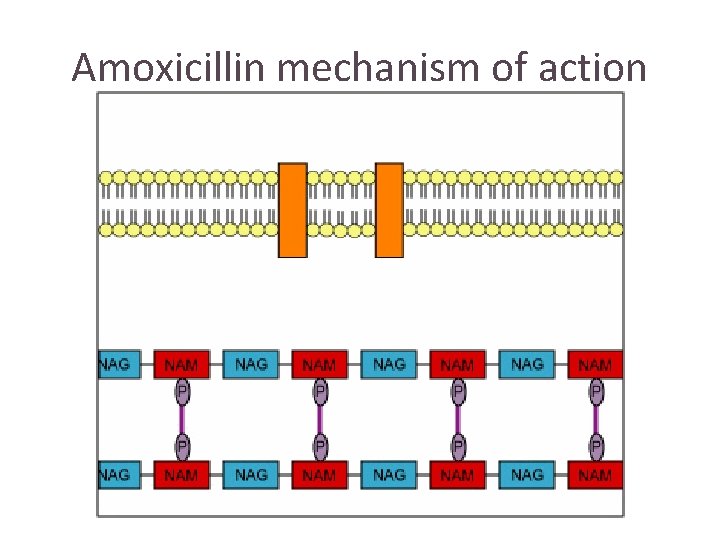
Amoxicillin mechanism of action
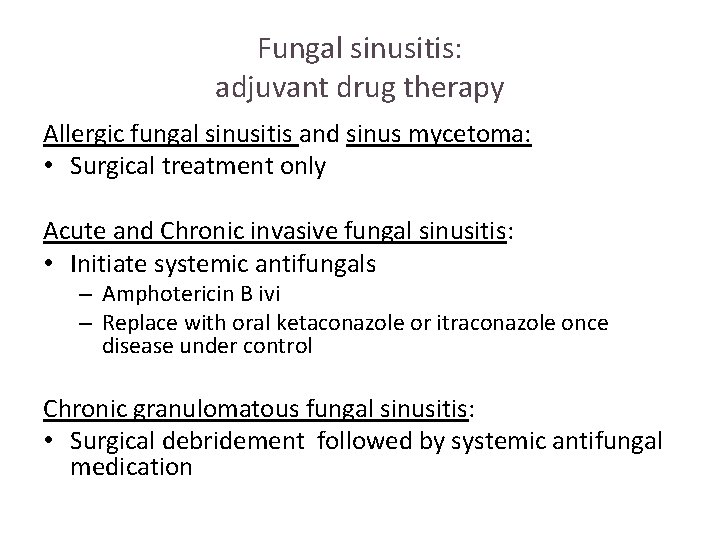
Fungal sinusitis • Recently been blamed for causing most cases of chronic rhinosinusitis • Most are benign except when occur in immunocompromised patients where they become invasive (acute and chronic) • Prognosis is different for each • Pathogens: – Aspergillus and – Mucor species Rx: Surgical debridement for all. Adjuvant medical Ramadan HH. Fungal sinusitis 2009. emedicine. medscape. com
Fungal sinusitis: adjuvant drug therapy Allergic fungal sinusitis and sinus mycetoma: • Surgical treatment only Acute and Chronic invasive fungal sinusitis: • Initiate systemic antifungals – Amphotericin B ivi – Replace with oral ketaconazole or itraconazole once disease under control Chronic granulomatous fungal sinusitis: • Surgical debridement followed by systemic antifungal medication
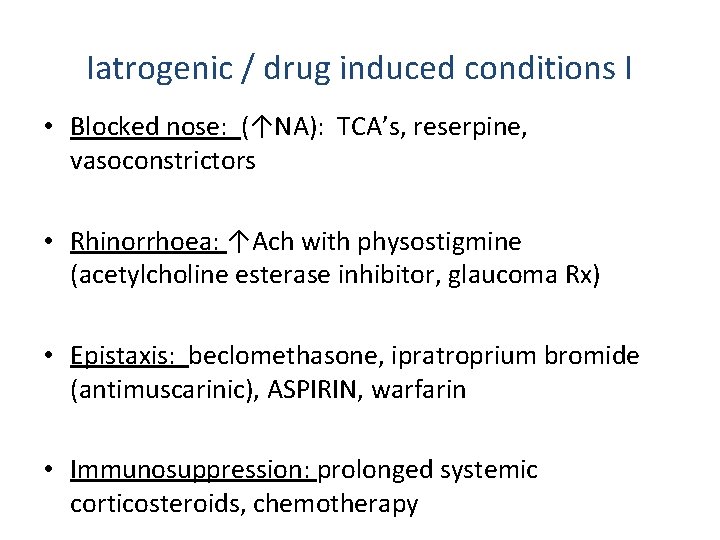
Iatrogenic / drug induced conditions I • Blocked nose: (↑NA): TCA’s, reserpine, vasoconstrictors • Rhinorrhoea: ↑Ach with physostigmine (acetylcholine esterase inhibitor, glaucoma Rx) • Epistaxis: beclomethasone, ipratroprium bromide (antimuscarinic), ASPIRIN, warfarin • Immunosuppression: prolonged systemic corticosteroids, chemotherapy
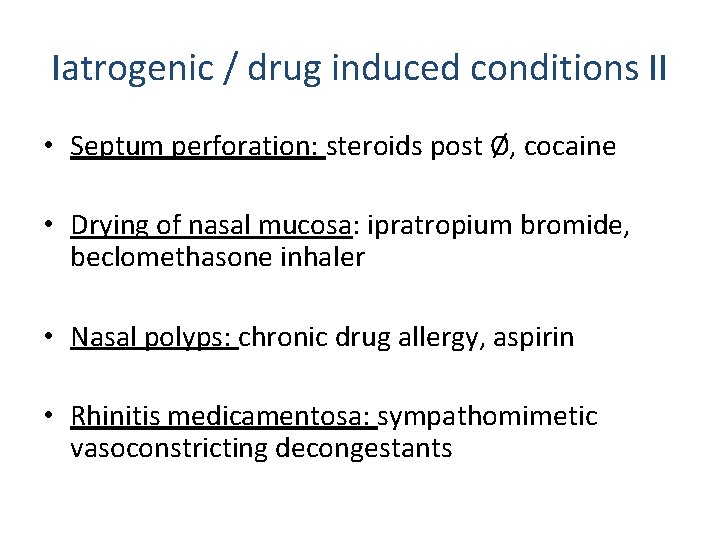
Iatrogenic / drug induced conditions II • Septum perforation: steroids post Ø, cocaine • Drying of nasal mucosa: ipratropium bromide, beclomethasone inhaler • Nasal polyps: chronic drug allergy, aspirin • Rhinitis medicamentosa: sympathomimetic vasoconstricting decongestants
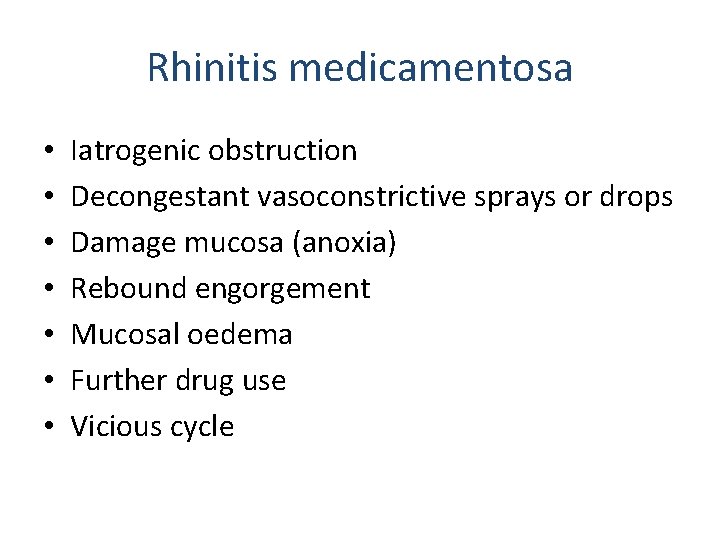
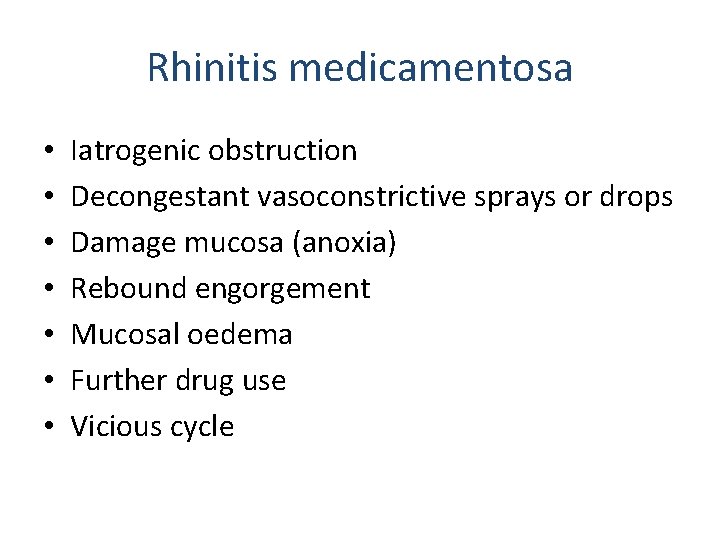
Rhinitis medicamentosa • • Iatrogenic obstruction Decongestant vasoconstrictive sprays or drops Damage mucosa (anoxia) Rebound engorgement Mucosal oedema Further drug use Vicious cycle
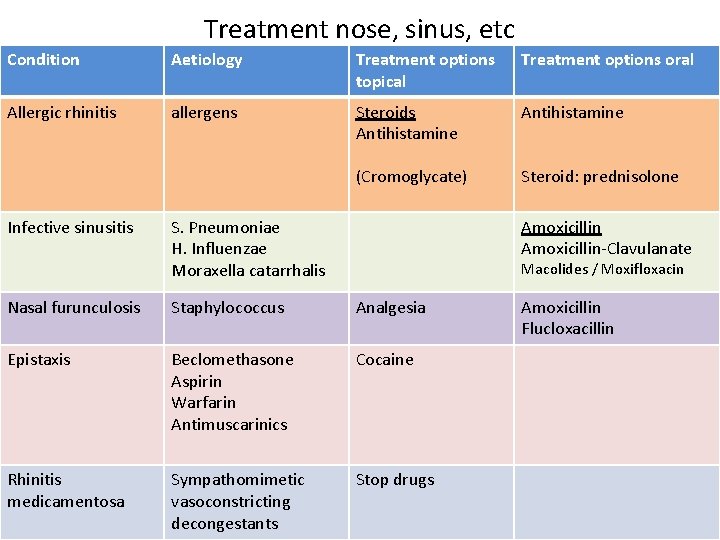
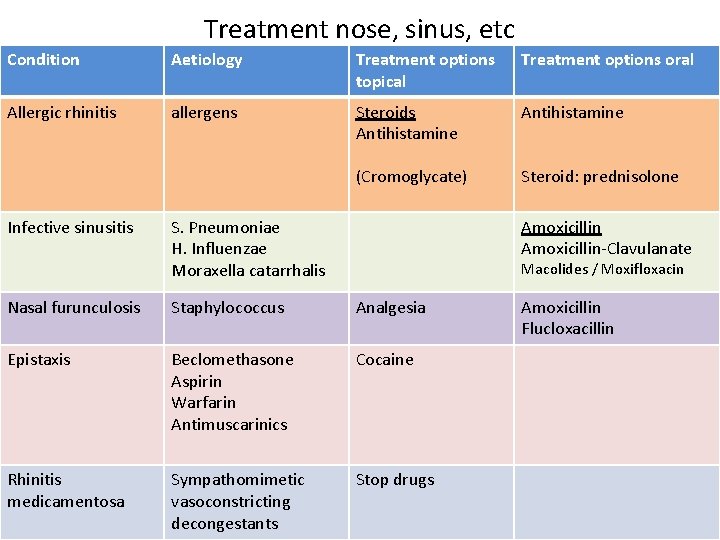
Treatment nose, sinus, etc Condition Aetiology Treatment options topical Treatment options oral Allergic rhinitis allergens Steroids Antihistamine (Cromoglycate) Steroid: prednisolone Infective sinusitis S. Pneumoniae H. Influenzae Moraxella catarrhalis Amoxicillin-Clavulanate Macolides / Moxifloxacin Nasal furunculosis Staphylococcus Analgesia Epistaxis Beclomethasone Aspirin Warfarin Antimuscarinics Cocaine Rhinitis medicamentosa Sympathomimetic vasoconstricting decongestants Stop drugs Amoxicillin Flucloxacillin