NORTHBROOK BEHAVIORAL HEALTH HOSPITAL Understanding and Responding to
NORTHBROOK BEHAVIORAL HEALTH HOSPITAL Understanding and Responding to Behavioral and Psychiatric Symptoms of Dementia
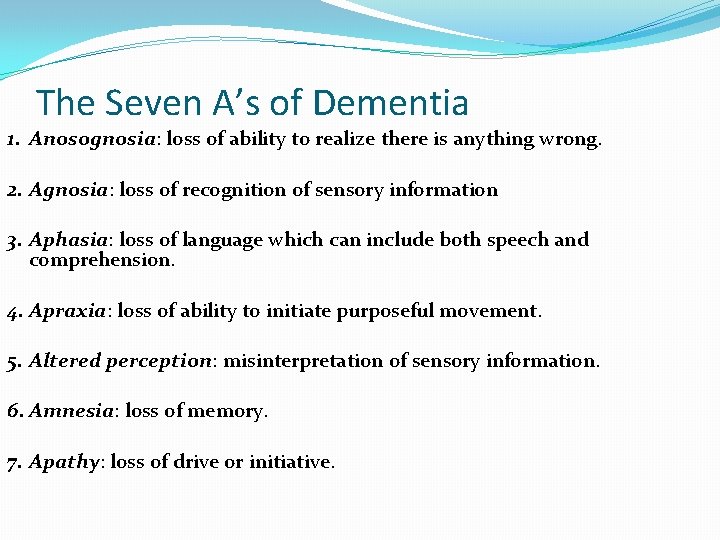
The Seven A’s of Dementia 1. Anosognosia: loss of ability to realize there is anything wrong. 2. Agnosia: loss of recognition of sensory information 3. Aphasia: loss of language which can include both speech and comprehension. 4. Apraxia: loss of ability to initiate purposeful movement. 5. Altered perception: misinterpretation of sensory information. 6. Amnesia: loss of memory. 7. Apathy: loss of drive or initiative.
Agree or Disagree? All behavior is a form of communication.
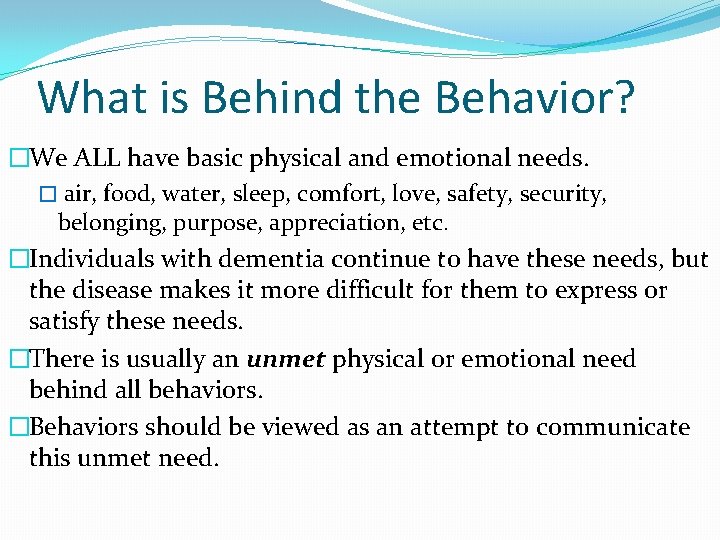
What is Behind the Behavior? �We ALL have basic physical and emotional needs. � air, food, water, sleep, comfort, love, safety, security, belonging, purpose, appreciation, etc. �Individuals with dementia continue to have these needs, but the disease makes it more difficult for them to express or satisfy these needs. �There is usually an unmet physical or emotional need behind all behaviors. �Behaviors should be viewed as an attempt to communicate this unmet need.
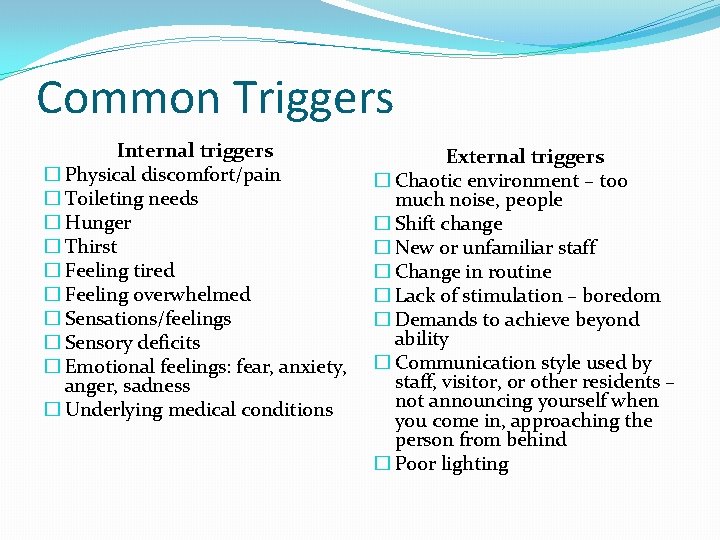
Common Triggers Internal triggers � Physical discomfort/pain � Toileting needs � Hunger � Thirst � Feeling tired � Feeling overwhelmed � Sensations/feelings � Sensory deficits � Emotional feelings: fear, anxiety, anger, sadness � Underlying medical conditions External triggers � Chaotic environment – too much noise, people � Shift change � New or unfamiliar staff � Change in routine � Lack of stimulation – boredom � Demands to achieve beyond ability � Communication style used by staff, visitor, or other residents – not announcing yourself when you come in, approaching the person from behind � Poor lighting
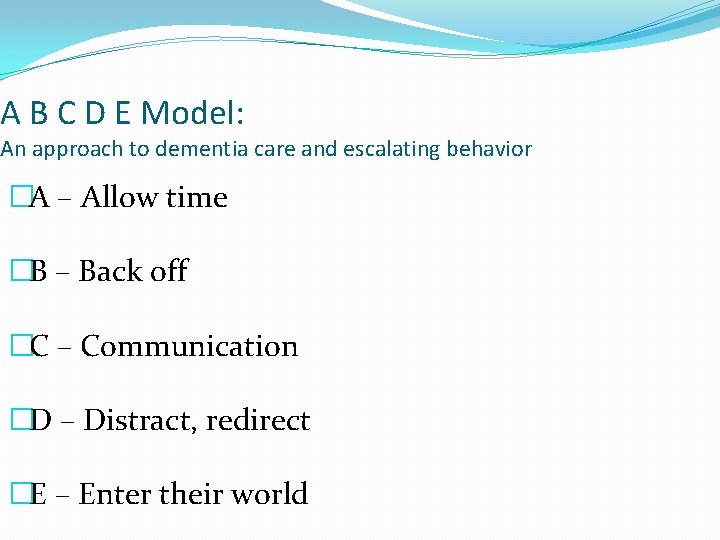
A B C D E Model: An approach to dementia care and escalating behavior �A – Allow time �B – Back off �C – Communication �D – Distract, redirect �E – Enter their world
A : Allow Time �Dementia care takes 50% more time. �Rushing care can be considered abuse. �Rushing increases anxiety, agitation, aggression and fear. �A calm caregiver can calm the client.
B : Back Off �Can this task wait until another time? �Can you try again later? �Can you get help? �Could another person do the task? IF YOU INSIST, THEY WILL RESIST!!
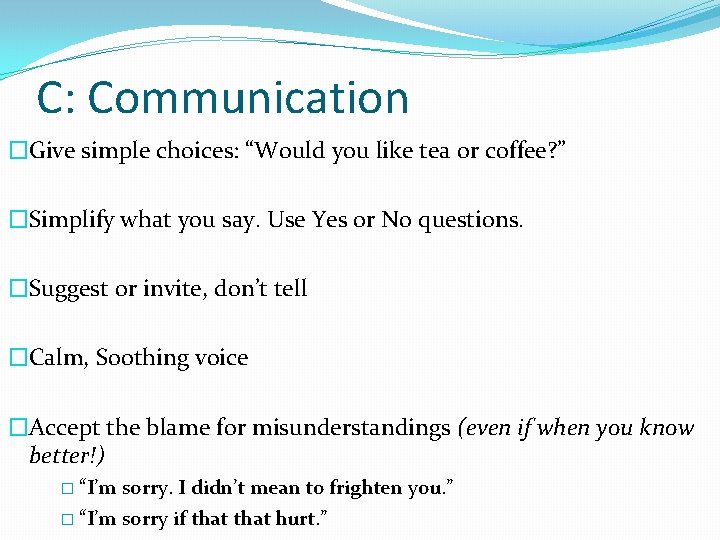
C: Communication �Give simple choices: “Would you like tea or coffee? ” �Simplify what you say. Use Yes or No questions. �Suggest or invite, don’t tell �Calm, Soothing voice �Accept the blame for misunderstandings (even if when you know better!) � “I’m sorry. I didn’t mean to frighten you. ” � “I’m sorry if that hurt. ”
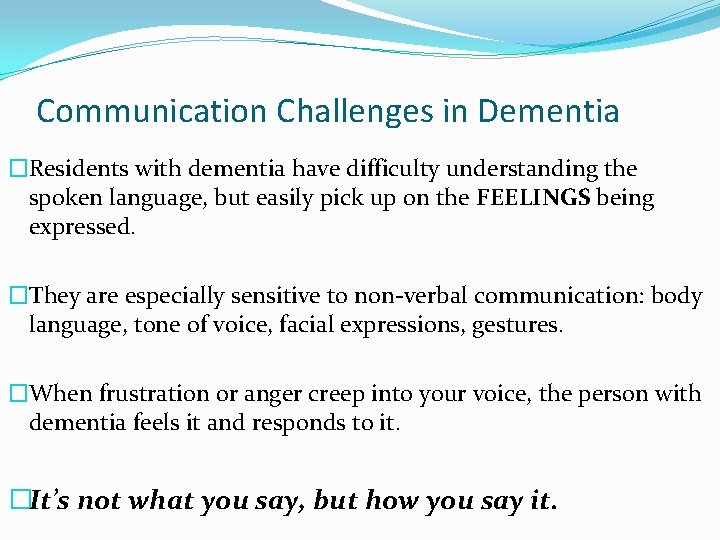
Communication Challenges in Dementia �Residents with dementia have difficulty understanding the spoken language, but easily pick up on the FEELINGS being expressed. �They are especially sensitive to non-verbal communication: body language, tone of voice, facial expressions, gestures. �When frustration or anger creep into your voice, the person with dementia feels it and responds to it. �It’s not what you say, but how you say it.
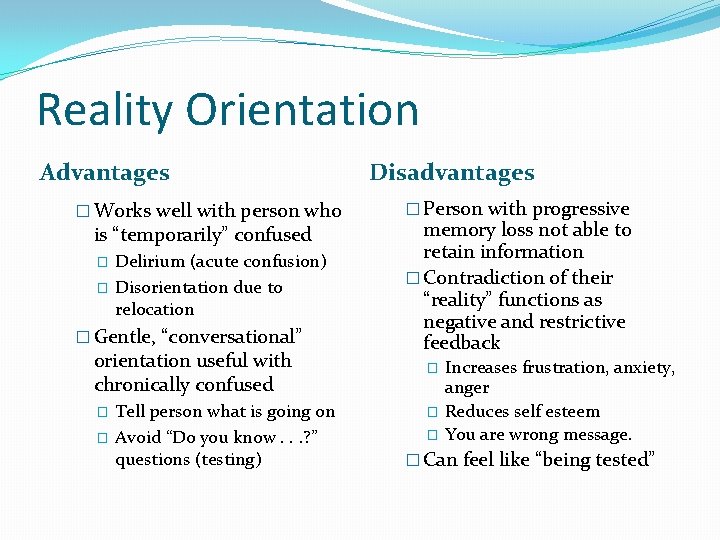
Reality Orientation Advantages � Works well with person who is “temporarily” confused � � Delirium (acute confusion) Disorientation due to relocation � Gentle, “conversational” orientation useful with chronically confused � � Tell person what is going on Avoid “Do you know. . . ? ” questions (testing) Disadvantages � Person with progressive memory loss not able to retain information � Contradiction of their “reality” functions as negative and restrictive feedback � � � Increases frustration, anxiety, anger Reduces self esteem You are wrong message. � Can feel like “being tested”
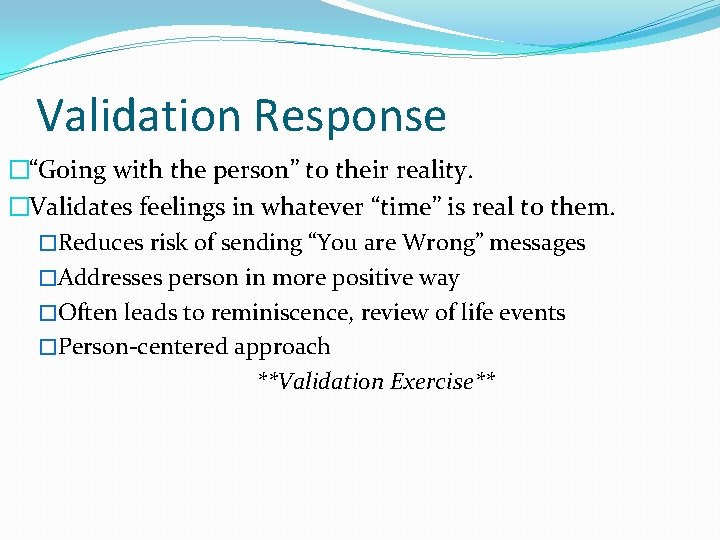
Validation Response �“Going with the person” to their reality. �Validates feelings in whatever “time” is real to them. �Reduces risk of sending “You are Wrong” messages �Addresses person in more positive way �Often leads to reminiscence, review of life events �Person-centered approach **Validation Exercise**
Validation Approaches �Don’t: �Reason �Argue �Correct �Criticize �Confront �Avoid: No you can’t! Don’t do that! I told you already! That’s not yours! �Take it personally!!!
D : Distract �Distract with another activity the person enjoys �Remember to use a suggestive tone �Leave the room to avoid confrontations �“I’m going to the kitchen now. I’ll be back. ” �“Let’s stop now. We’ll do this later. ”
E : Enter their World �Your client’s reality is unique �People with dementia live in the moment �Go where they are at that moment �Validation
Combative Behaviors During Care �Combativeness during personal care can come in the forms of the following behaviors: �pulling away from staff �tightening limbs, stiffening the body, deliberately ceasing �refusing to weight bear during care �waving arms and legs �hitting �verbally objecting to care using words and/or sounds
Combative Behaviors During Personal Care: Underlying Causes? �The care is too “rough. ” �The room or water temperature is uncomfortable. �The door or windows are not shut. �The resident feels embarrassed. �There are cultural differences. �Timing issue.
Combative Behaviors During Personal Care: Care Approaches �Approach from the front calmly and slowly. Make eye contact before speaking. �Start interaction with a positive and social approach. Be conversational. �Introduce yourself: who you are and why you are there. �It makes a big difference if we introduce ourselves in a calm, pleasant tone. For example, “Hi, I’m Mary. I’m here to give you a bath. It’s so nice to work with you today. ” Your tone tells the resident, “You’re a great person and you’re safe with me. ”
Care Approaches �Softly talk to the person about something they are interested in first or during care to relax/distract them from the unpleasantness of the task. �Always explain step-by-step what you are going to do before assisting with personal care. �Just because you can’t have a conversation with the resident, doesn’t mean that you don’t have to tell them what you are doing.
Care Approaches �Soft, soothing music can be helpful for some patients because it creates a more relaxed mood, reduces agitation, and improves their cooperation. �A thin towel can be used to cover the torso or private area while the caregiver soaps the rest of the body. �Avoid appearing rushed or impatient.
Care Approaches: Visual Cueing �Modeling the desired behavior. �For example, Mrs. Brown may begin to brush her hair when you hand her a toothbrush. �If you stick the toothbrush in her mouth and rapidly brush her teeth, you may get spitting, biting, and clamping of the jaw because it’s an intrusive, foreign object. �Instead, try modeling the behavior for her by demonstrating how it is done.
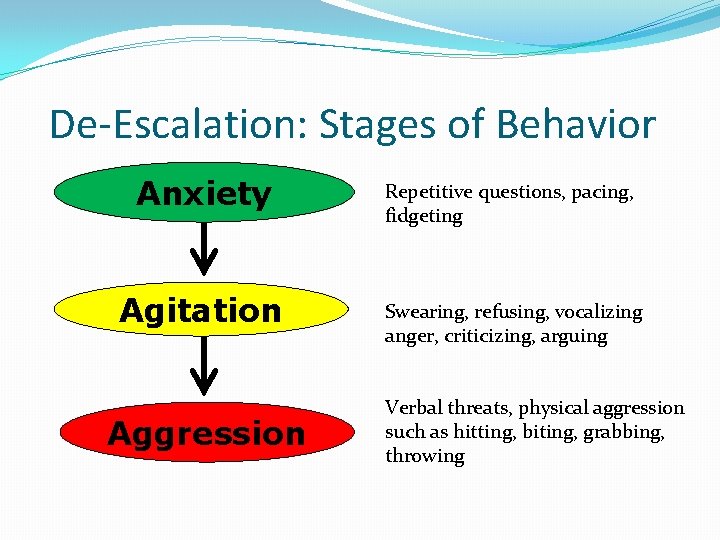
De-Escalation: Stages of Behavior Anxiety Repetitive questions, pacing, fidgeting Agitation Swearing, refusing, vocalizing anger, criticizing, arguing Aggression Verbal threats, physical aggression such as hitting, biting, grabbing, throwing
Anxiety �Restlessness, pacing, rocking, withdrawal, fidgeting. �When a client is experiencing anxiety, the best response is to be SUPPORTIVE. �This means you try to reduce the resident’s anxiety by showing care and concern. �It is not always possible to stop behavior at the anxiety level – we may notice it, we may be busy, or our interventions may not work.
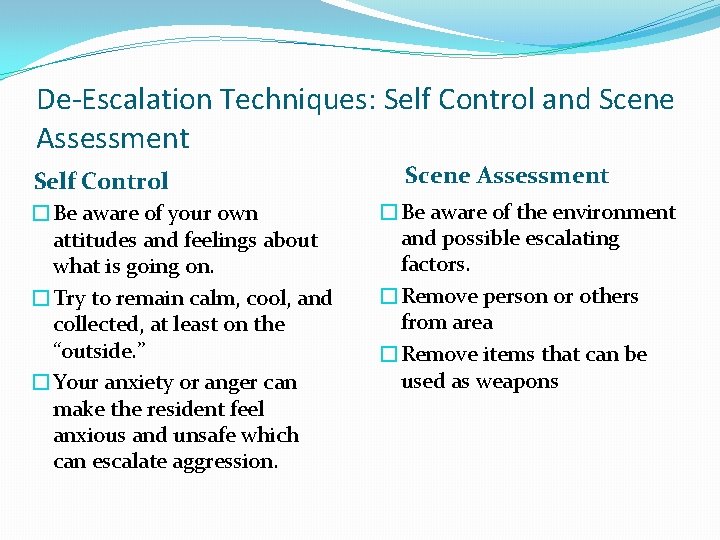
De-Escalation Techniques: Self Control and Scene Assessment Self Control �Be aware of your own attitudes and feelings about what is going on. �Try to remain calm, cool, and collected, at least on the “outside. ” �Your anxiety or anger can make the resident feel anxious and unsafe which can escalate aggression. Scene Assessment �Be aware of the environment and possible escalating factors. �Remove person or others from area �Remove items that can be used as weapons
De-Escalation Techniques: Stance �Approach slowly and calmly �Approach from the side. Never approach from behind or stand fully in front of the individual. �DO not crowd or corner the person. �Allow yourself at least three feet in between yourself and the individual. �Do not turn your back on the resident. �Know where the door is and stand between it and the individual. �Avoid making continuous eye contact. �Avoid touching the person. �Stay at the same eye level
Personal Space �Individuals with mental illness often develop an altered sense of personal space. They require more space to feel comfortable and feel threatened when other people close in on them with no warning. �Invasion or encroachment of personal space tends to heighten or escalate anxiety.
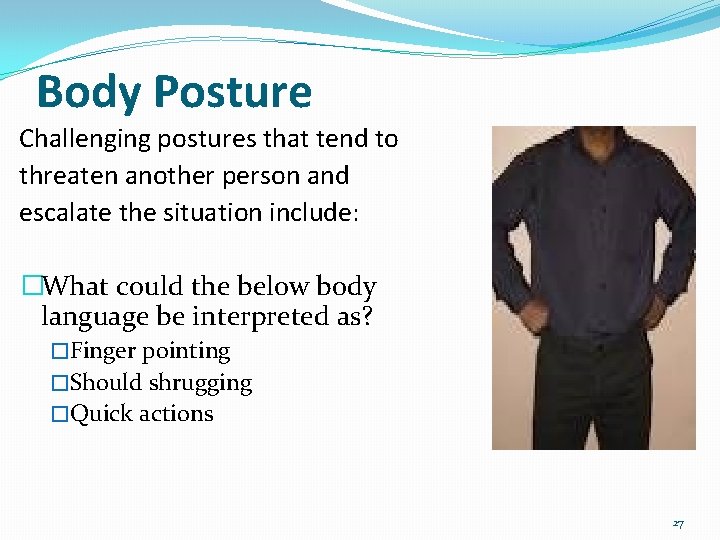
Body Posture Challenging postures that tend to threaten another person and escalate the situation include: �What could the below body language be interpreted as? �Finger pointing �Should shrugging �Quick actions 27
De-Escalation Techniques: Communication �Empathize with feelings but NOT with the behavior �Do NOT argue or try to convince. A person in crisis is not rational. �Suggest alternative behaviors where appropriate �Use positive consequences first; there is more of a chance they will be open and compliant:
Communication �Do not get loud and try to yell over a screaming person. �Wait until the individual takes a breath, then talk �Speak calmly and at an average volume. �Avoid sarcasm, insulting remarks, and even humor (which can be easily misinterpreted). �Answer all informational questions, no matter how rudely asked: � Ex: “Why do I have to fill out these (expletive) forms? ” � Do NOT answer abusive questions: “Why are you being such an (insult)? ” � This question should get no response whatsoever (verbally or via body language).
Avoid �Expressing anger, impatience or irritation �Inflammatory language (“You are acting crazy. ”) �Rushing the resident to resolve the crisis. �Intervening too quickly or trying too hard to control the interaction by interrupting or talking over the resident. �Saying “You need to calm down. ” Retaliating or withdrawing. Getting pulled into a power struggle. • Try not to be defensive. � Setting limits in a condescending tone. Shouting or giving rapid commands. � Arguing with the resident. � Asking “why? ” • • 30
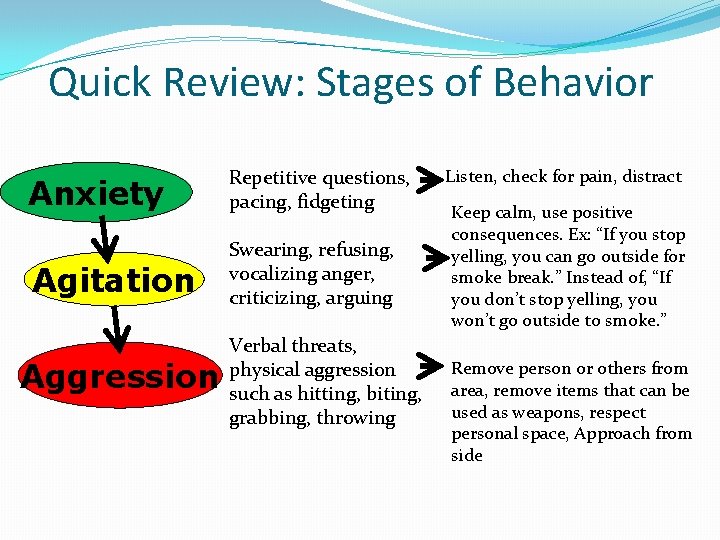
Quick Review: Stages of Behavior Anxiety Repetitive questions, pacing, fidgeting Agitation Swearing, refusing, vocalizing anger, criticizing, arguing Aggression Verbal threats, physical aggression such as hitting, biting, grabbing, throwing Listen, check for pain, distract Keep calm, use positive consequences. Ex: “If you stop yelling, you can go outside for smoke break. ” Instead of, “If you don’t stop yelling, you won’t go outside to smoke. ” Remove person or others from area, remove items that can be used as weapons, respect personal space, Approach from side
�Remember: Residents with Dementia are trying very hard to make sense of the world around them. It is our jobs to help them navigate it. �“Long-term care isn’t rocket science, it’s harder, longterm care workers are the angels of the world. ” Dorothy Seman, “Listen with the Ears of Your Heart”
- Slides: 32