North West Neonatal Operational Delivery Network Julie Mc


- Slides: 11
North West Neonatal Operational Delivery Network Julie Mc. Cabe, Network Director “Working together to provide the highest standard of care for babies and families”

What is a Clinical Network? Networks are about: � Breaking down boundaries � Cross organisational working � Focusing on the needs of the patient & cover the whole patient journey � Improving outcomes � Reducing unwarranted variation
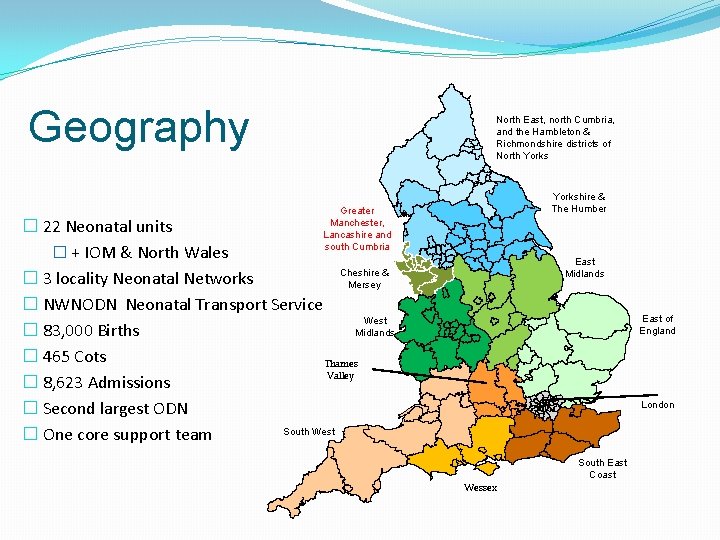
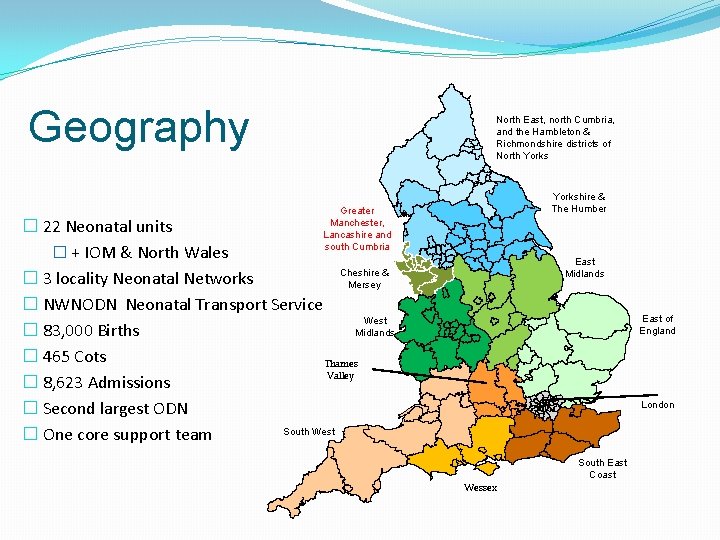
Geography North East, north Cumbria, and the Hambleton & Richmondshire districts of North Yorkshire & The Humber Greater Manchester, Lancashire and south Cumbria � 22 Neonatal units � + IOM & North Wales Cheshire & � 3 locality Neonatal Networks Mersey � NWNODN Neonatal Transport Service West Midlands � 83, 000 Births � 465 Cots Thames Valley � 8, 623 Admissions � Second largest ODN South West � One core support team East Midlands East of England London South East Coast Wessex
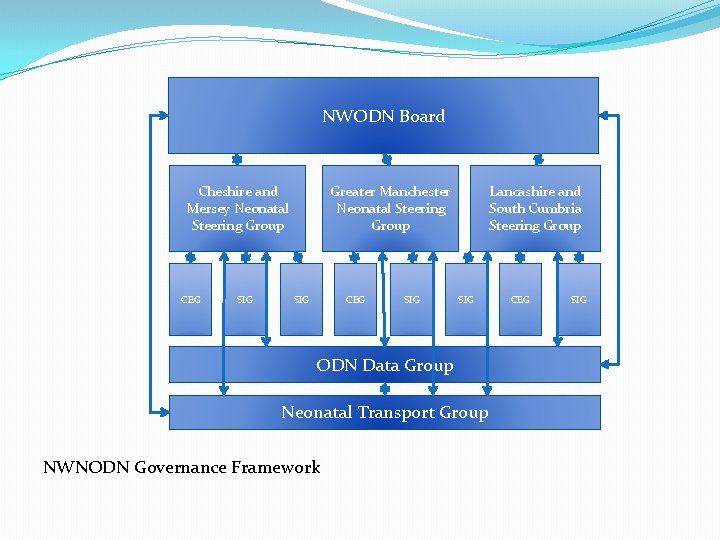
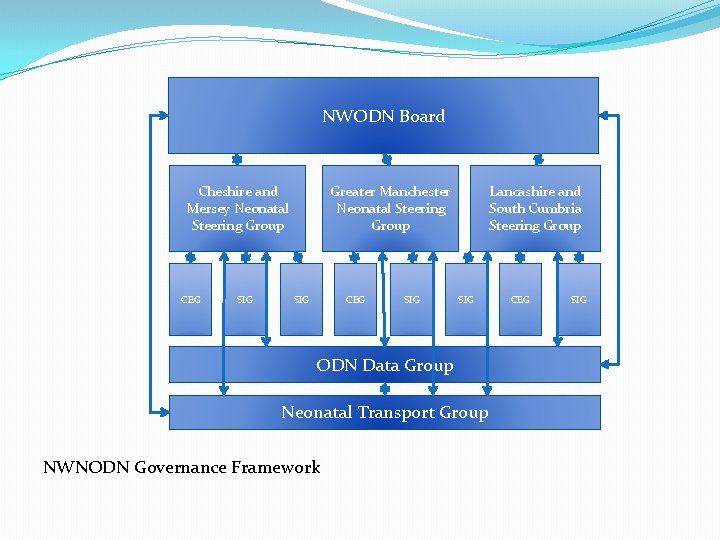
NWODN Board Cheshire and Mersey Neonatal Steering Group CEG SIG Greater Manchester Neonatal Steering Group SIG CEG SIG Lancashire and South Cumbria Steering Group SIG ODN Data Group Neonatal Transport Group NWNODN Governance Framework CEG SIG
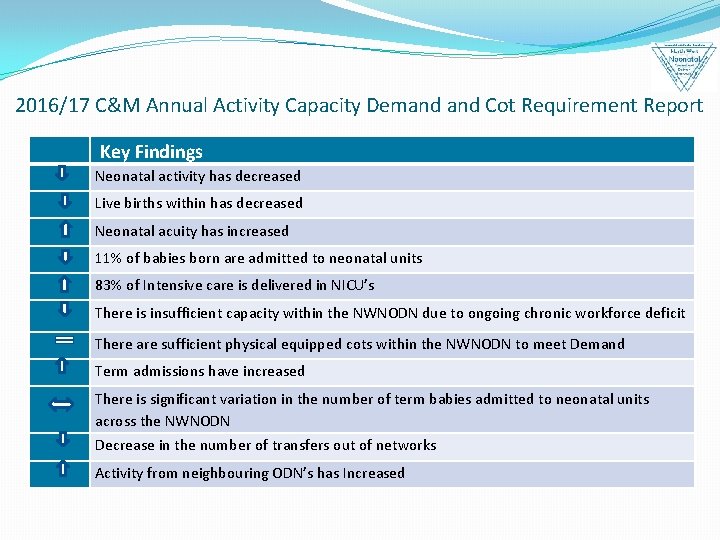
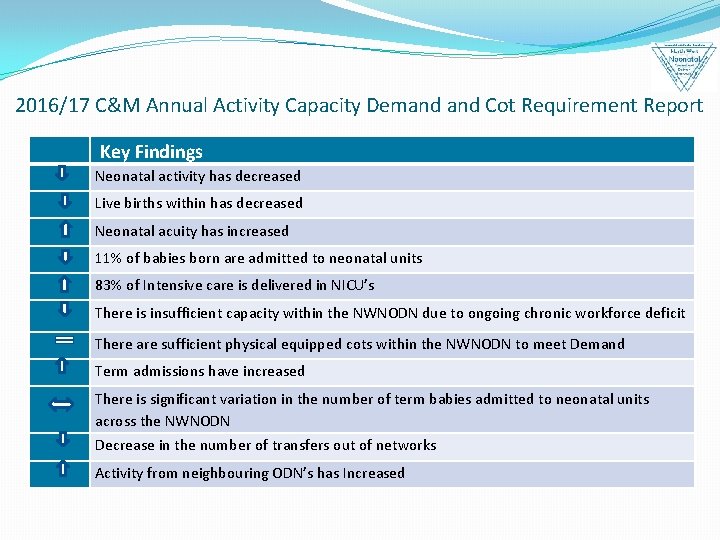
2016/17 C&M Annual Activity Capacity Demand Cot Requirement Report Key Findings Neonatal activity has decreased Live births within has decreased Neonatal acuity has increased 11% of babies born are admitted to neonatal units 83% of Intensive care is delivered in NICU’s There is insufficient capacity within the NWNODN due to ongoing chronic workforce deficit There are sufficient physical equipped cots within the NWNODN to meet Demand Term admissions have increased There is significant variation in the number of term babies admitted to neonatal units across the NWNODN Decrease in the number of transfers out of networks Activity from neighbouring ODN’s has Increased
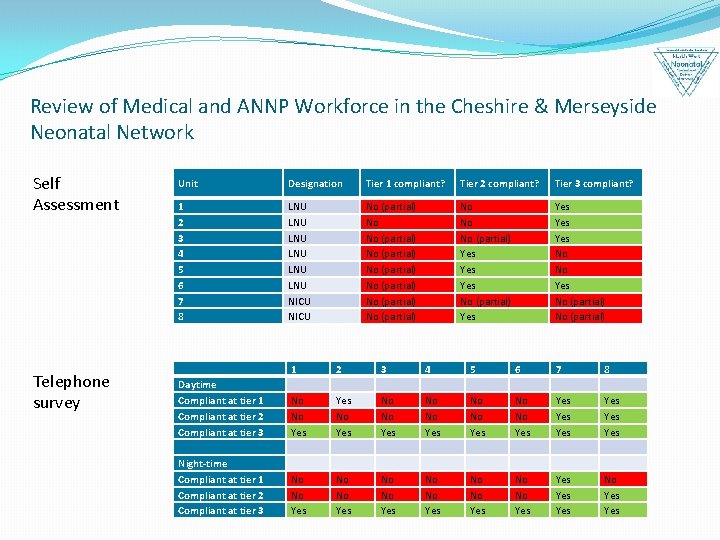
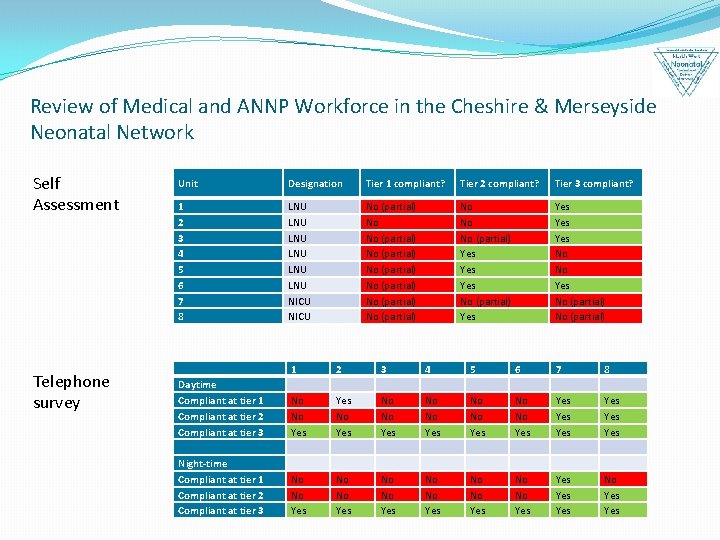
Review of Medical and ANNP Workforce in the Cheshire & Merseyside Neonatal Network Self Assessment Telephone survey Unit Designation Tier 1 compliant? Tier 2 compliant? Tier 3 compliant? 1 2 3 4 5 6 7 8 LNU LNU LNU NICU No (partial) No (partial) No No No (partial) Yes Yes No No Yes No (partial) 1 2 3 4 5 6 7 8 Daytime Compliant at tier 1 Compliant at tier 2 Compliant at tier 3 No No Yes No No Yes Yes Yes Yes Night-time Compliant at tier 1 Compliant at tier 2 Compliant at tier 3 No No Yes No No Yes Yes Yes No Yes
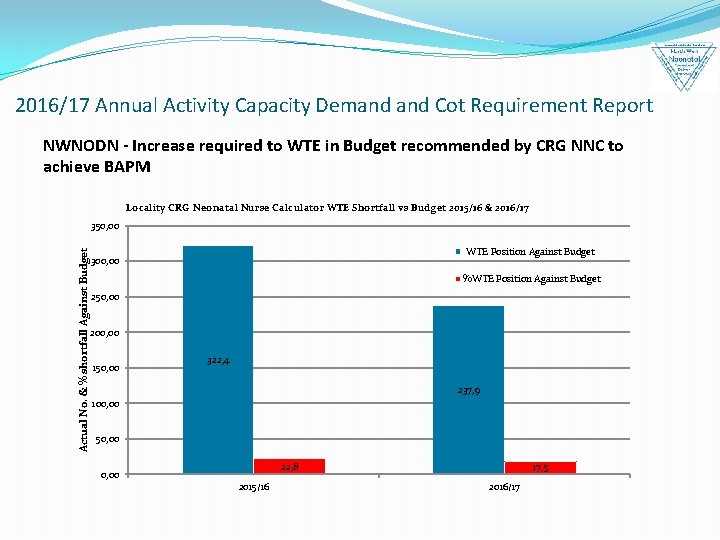
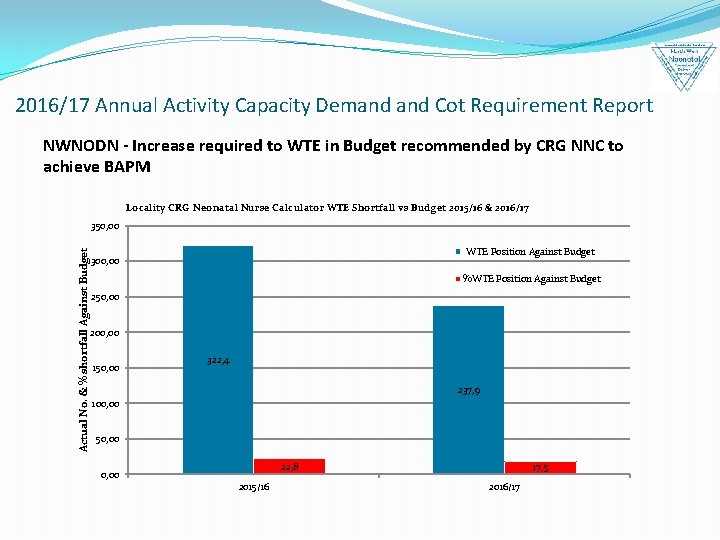
2016/17 Annual Activity Capacity Demand Cot Requirement Report NWNODN - Increase required to WTE in Budget recommended by CRG NNC to achieve BAPM Locality CRG Neonatal Nurse Calculator WTE Shortfall vs Budget 2015/16 & 2016/17 Actual No. & % shortfall Against Budget 350, 00 WTE Position Against Budget 300, 00 %WTE Position Against Budget 250, 00 200, 00 150, 00 322, 4 237, 9 100, 00 50, 00 22, 8 0, 00 2015/16 17, 5 2016/17
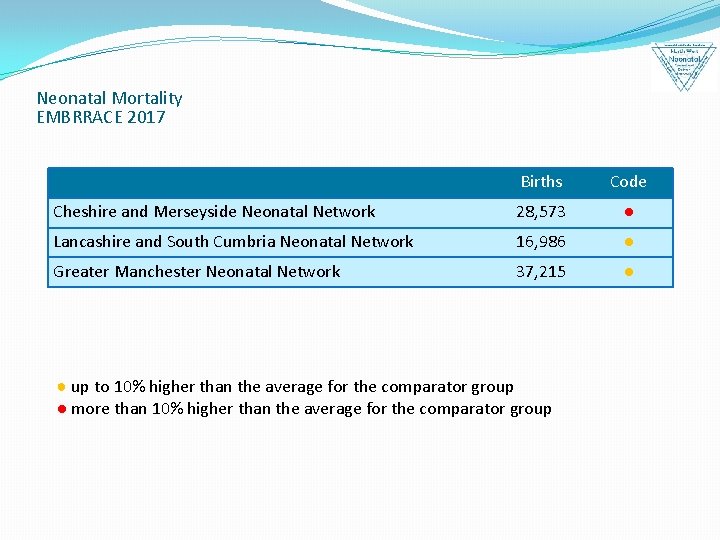
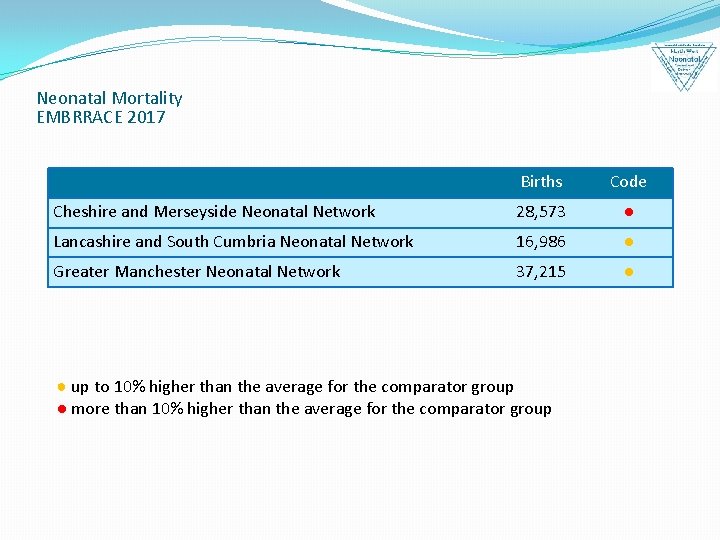
Neonatal Mortality EMBRRACE 2017 Births Code Cheshire and Merseyside Neonatal Network 28, 573 ● Lancashire and South Cumbria Neonatal Network 16, 986 ● Greater Manchester Neonatal Network 37, 215 ● ● up to 10% higher than the average for the comparator group ● more than 10% higher than the average for the comparator group

Neonatal ODN contribution to FYFV Better Health Improving Outcomes • • • Family integrated care Reducing the number of babies separated from their mothers Optimising Place of delivery Network approach to the reduction in neonatal mortality Workforce development Better care Improving Quality • • Cardiac pathway Integrated palliative care Surgical pathway Single surgical service Neonatal outreach CQUIN Network education and training Workforce development • • • Better value Right care, right place, right professional Activity Capacity Demand review Central capacity cot/bed management system Network procurement New Pricing and contracting models Workforce planning
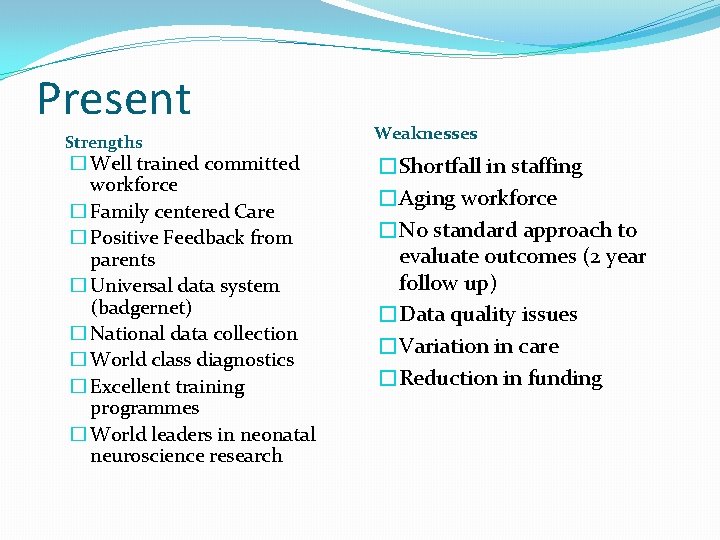
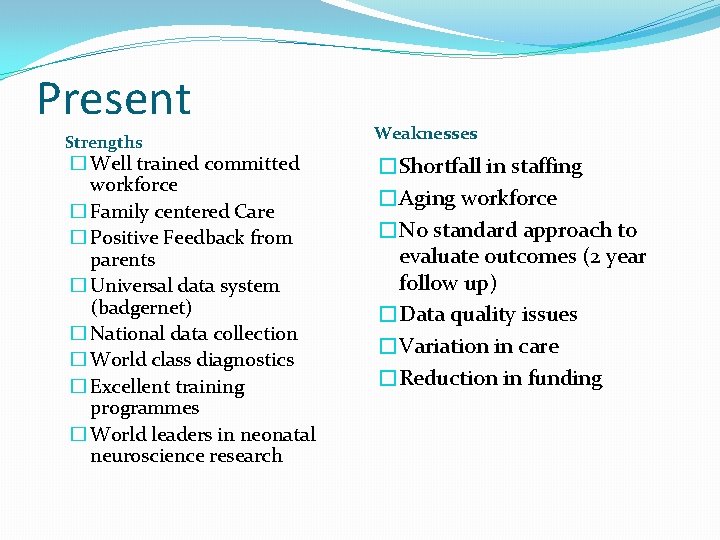
Present Strengths � Well trained committed workforce � Family centered Care � Positive Feedback from parents � Universal data system (badgernet) � National data collection � World class diagnostics � Excellent training programmes � World leaders in neonatal neuroscience research Weaknesses �Shortfall in staffing �Aging workforce �No standard approach to evaluate outcomes (2 year follow up) �Data quality issues �Variation in care �Reduction in funding
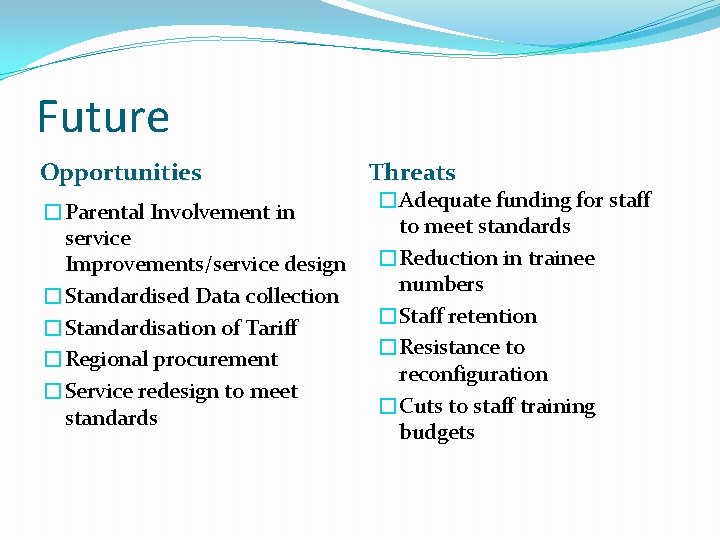
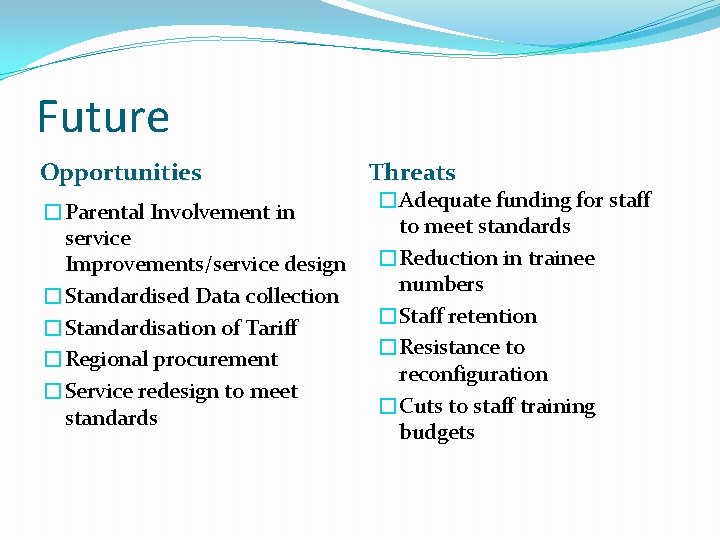
Future Opportunities �Parental Involvement in service Improvements/service design �Standardised Data collection �Standardisation of Tariff �Regional procurement �Service redesign to meet standards Threats �Adequate funding for staff to meet standards �Reduction in trainee numbers �Staff retention �Resistance to reconfiguration �Cuts to staff training budgets