Normal Tension Glaucoma Diagnosis and Therapy Audrey KaplanMessas



- Slides: 43
Normal Tension Glaucoma Diagnosis and Therapy Audrey Kaplan-Messas Head of glaucoma service Assaf Harofe Medical center
NTG: think about it ! • How common is NTG? – Population studies • 30 -40% (Sommer 1991, Dielemans 1994, Bonomi 1998) – Clinical presentation and screening • 5% (Grodum, Heijl 2002)

NTG Diagnosis and therapy • • • Diagnosis Differential diagnosis Natural History Investigation Treatment
NTG: Description – Glaucomatous optic neuropathy – Characteristic pattern of visual field loss – IOP within the normal range – Progressive disease
NTG: Description Normal-tension glaucoma (NTG) is an optic neuropathy of unknown etiology characterized by cupping of the disc, typical visual field loss, and normal IOP. The diagnosis of NTG is made by exclusion, and an extensive differential must be considered in evaluating patients with suspected NTG.
Vascular patophysiology • Vascular and cardio-vascular risk factors associated (Broadway 1998, Hayreh 1999) • Nocturnal Hypotension (Hayreh 1999, Meyer 1996 ) • Exacerbated when topical beta- used ( Hayreh 1999) • Relationship with migraine (up to 62% VF def when both) , vasospasm (Gasser 1999)
Auto-immune patophysiology? • 30 % of NTG have an AI disease (8% OHT) (Cartwright 1992) • Monoclonal paraproteinemia, Ig. G, Ig A in RGC layer (Wax 1999) • Antiphospholipid Ab ( Kremmer 1999), Rhodopsine Ab in NTG (Romano 1999) • Ab to Heat Shock Protein NTG> POAG> control (Wax, Tezel 1998)
NTG: Differences with POAG – Thinner NR rim, inf-temporally, focal rim defect (Caprioli 1985, Jonas 2000) – Shallower cupping, saucerization (Fazio 1990) – Focal RNFL defects (Jonas 2000) – Visual field loss deeper and steeper paracentral, dense scotoma close to fixation (up to 50% of NTG) (Caprioli 1985, Hitchings 1984), – Prevalence of Disc Hemorrhages (up to 25%)( Kitazawa 1988, Jonas 2000) – CCT thinner in NTG (Morad 1998, Copt 1999, Whitacre 2000)
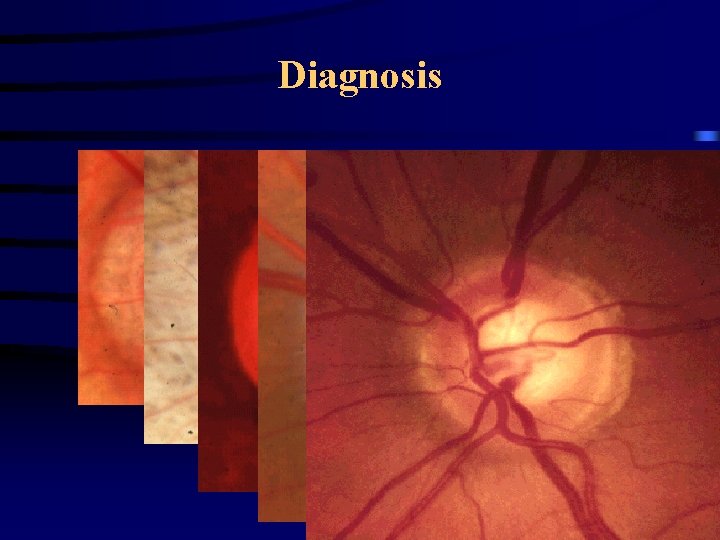
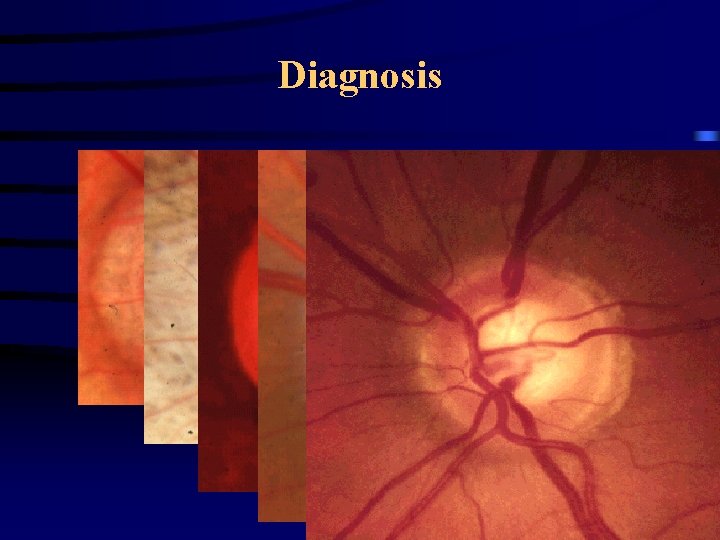
Diagnosis
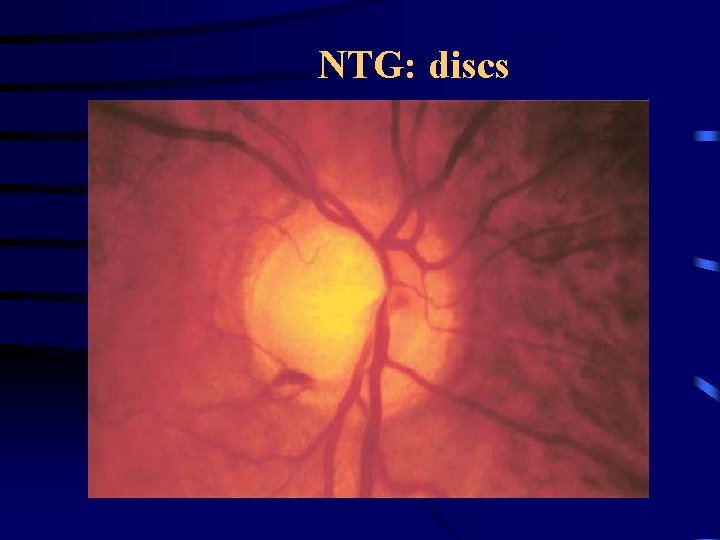
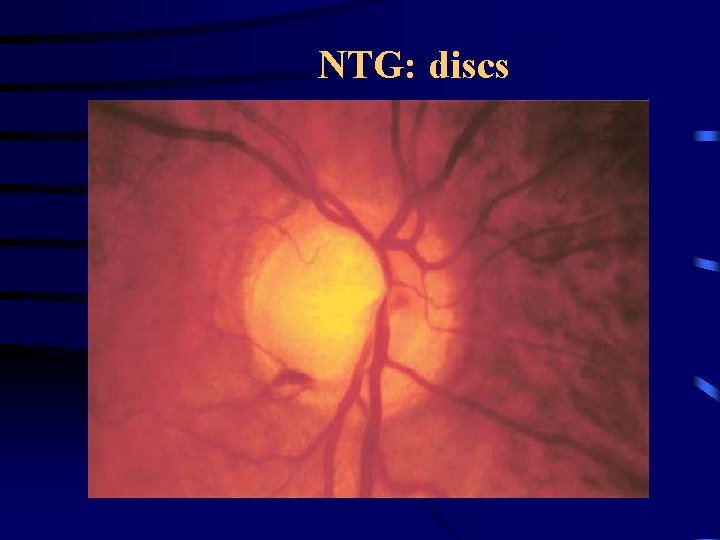
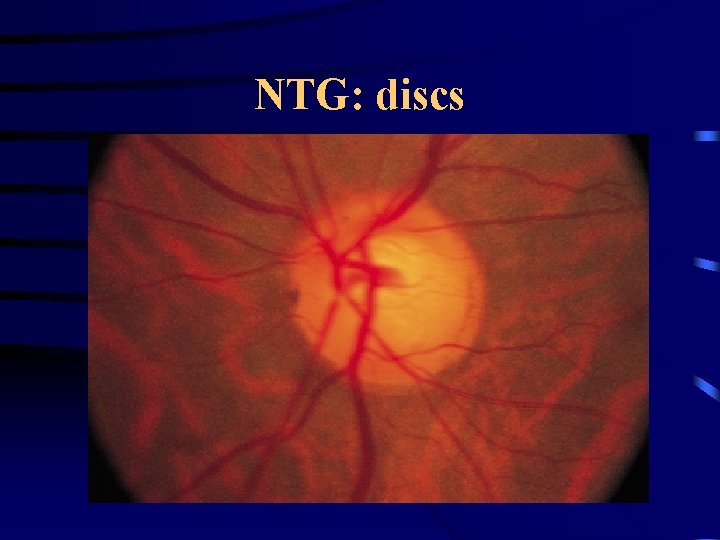
NTG: discs
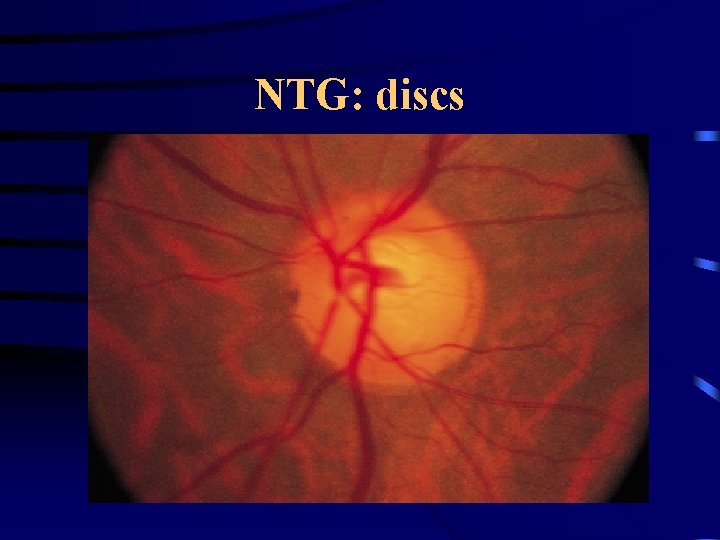
NTG: discs
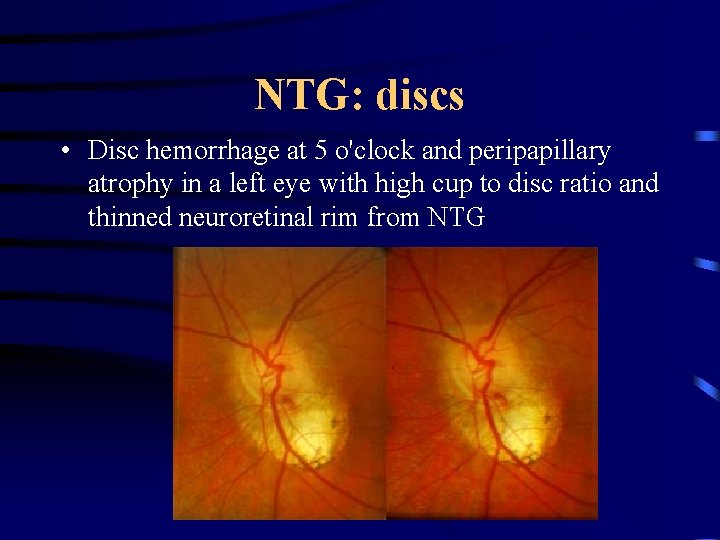
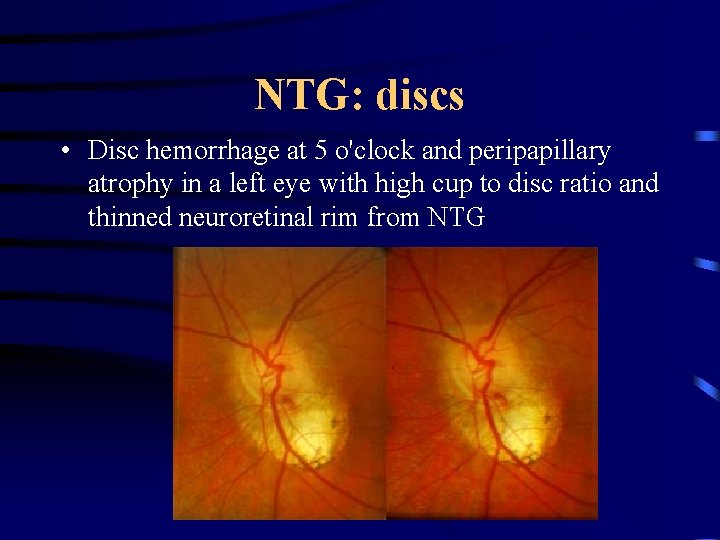
NTG: discs • Disc hemorrhage at 5 o'clock and peripapillary atrophy in a left eye with high cup to disc ratio and thinned neuroretinal rim from NTG
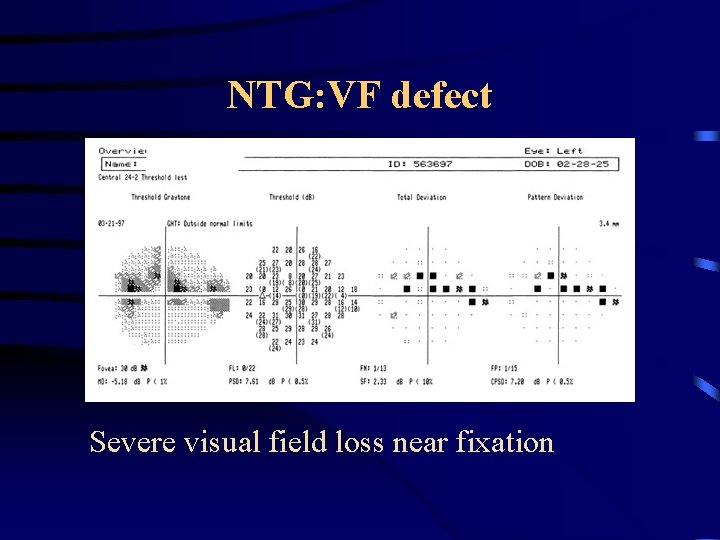
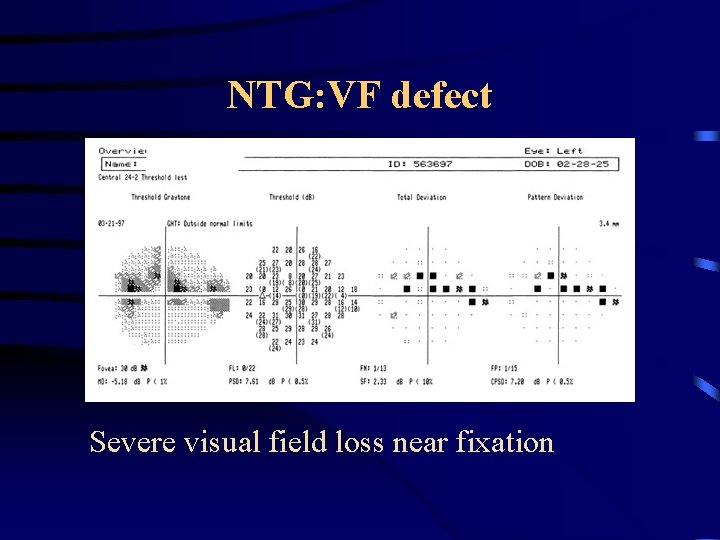
NTG: VF defect Severe visual field loss near fixation
Normal Pressure Glaucoma • Diagnosis • Differential diagnosis • Natural History • Phenotype and genotype • Investigation • Treatment
NTG Differential Diagnosis • Differential diagnosis – – Glaucoma? Optic Neuropathy? Visual pathway disease? Acquired or developmental optic nerve disease? • Does the diagnosis fit? • YES-evaluate • NO-look for other disease – Remember Co-morbidity: vascular, auto-immune
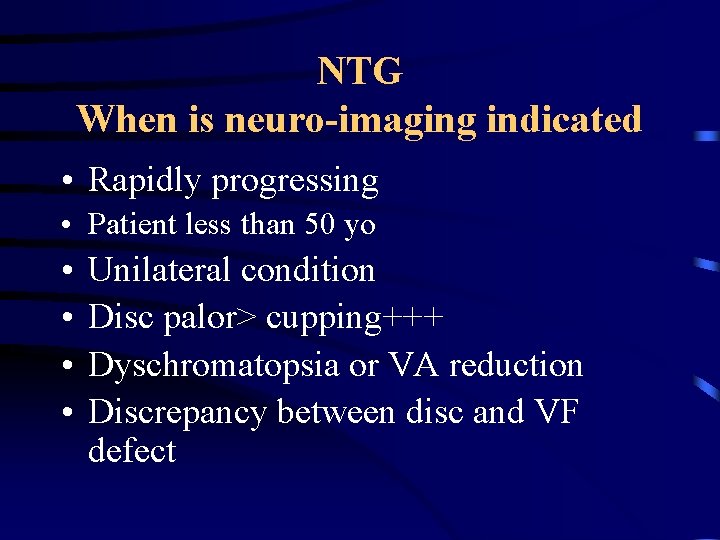
NTG When is neuro-imaging indicated • Rapidly progressing • Patient less than 50 yo • • Unilateral condition Disc palor> cupping+++ Dyschromatopsia or VA reduction Discrepancy between disc and VF defect
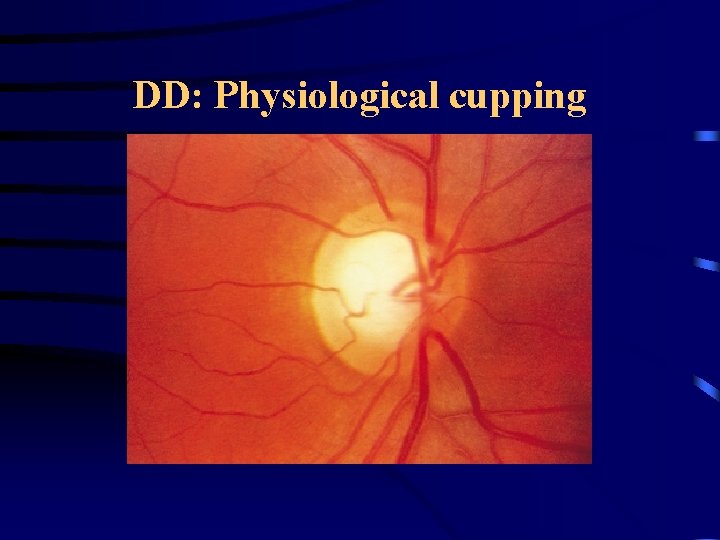
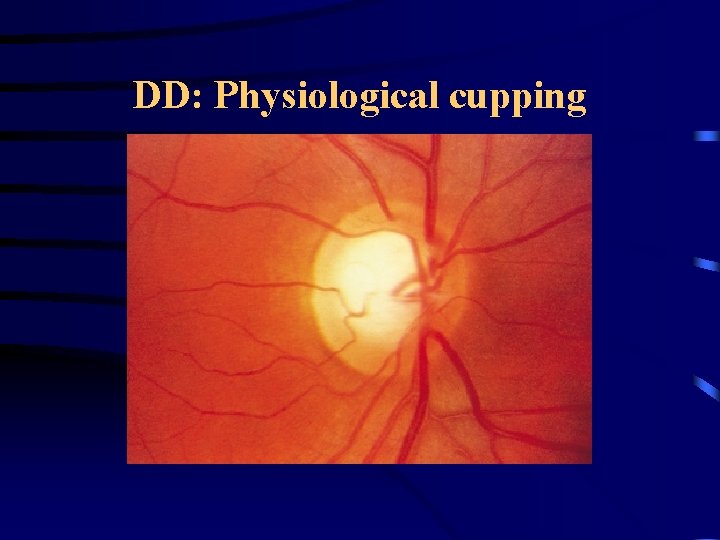
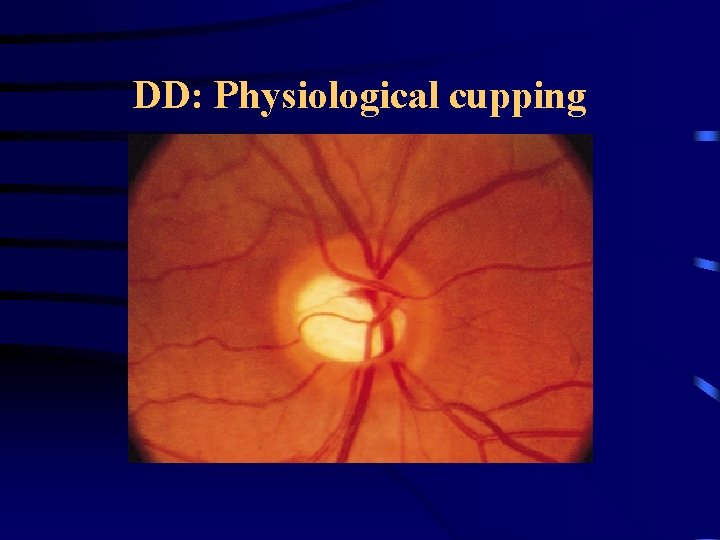
DD: Physiological cupping
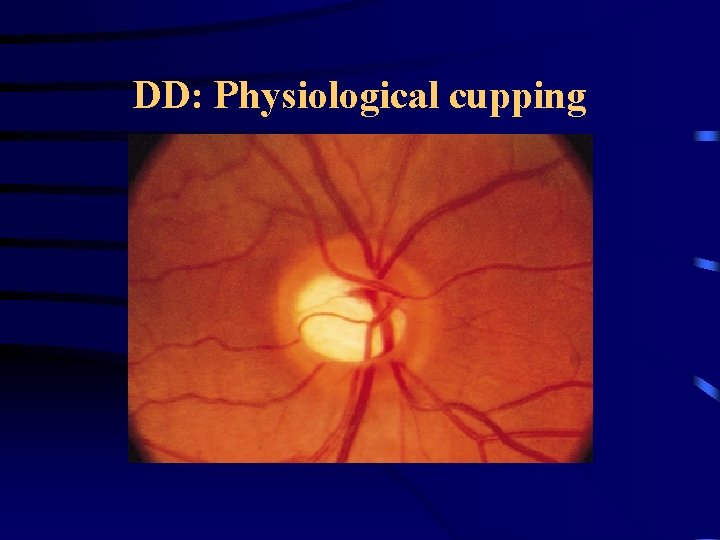
DD: Physiological cupping
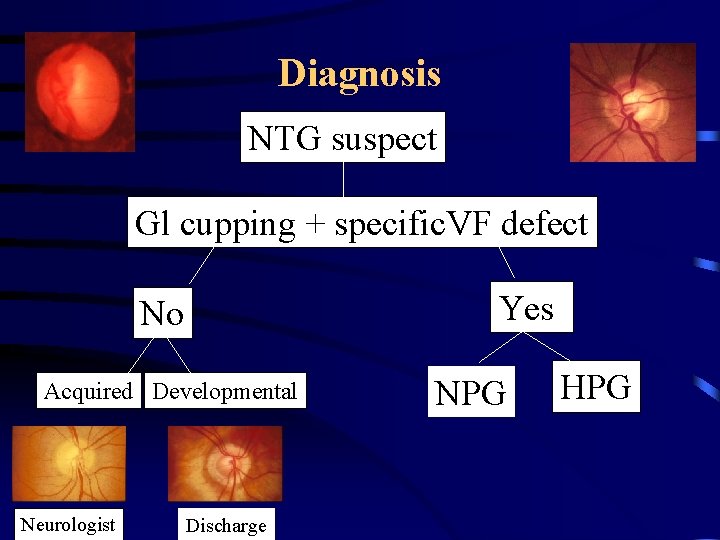
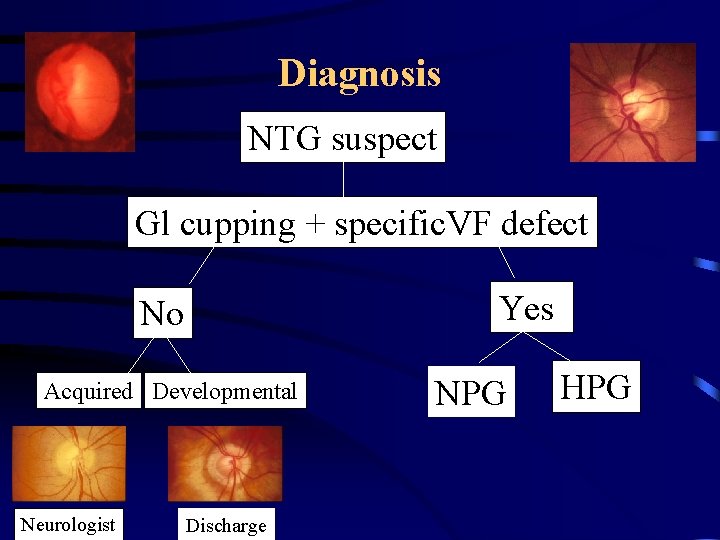
Diagnosis NTG suspect Gl cupping + specific. VF defect Yes No Acquired Developmental Neurologist Discharge NPG HPG
Normal Pressure Glaucoma • Diagnosis • Differential diagnosis • 3 -Natural History • Investigation • Treatment
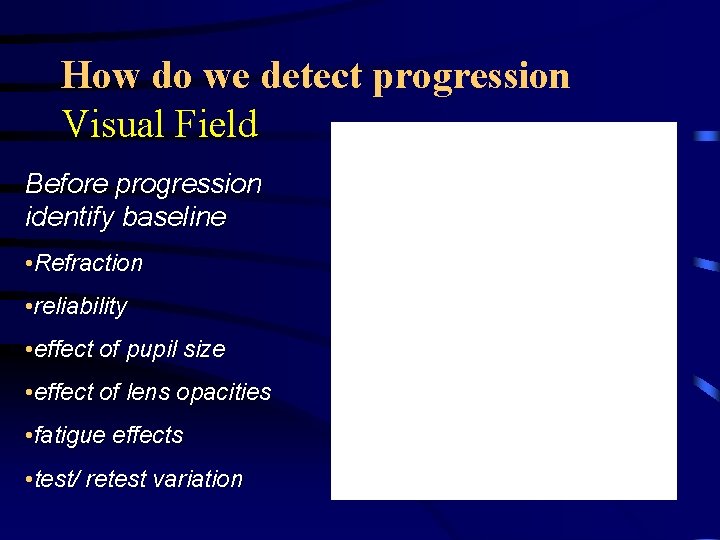
How do we detect progression Visual Field Before progression identify baseline • Refraction • reliability • effect of pupil size • effect of lens opacities • fatigue effects • test/ retest variation
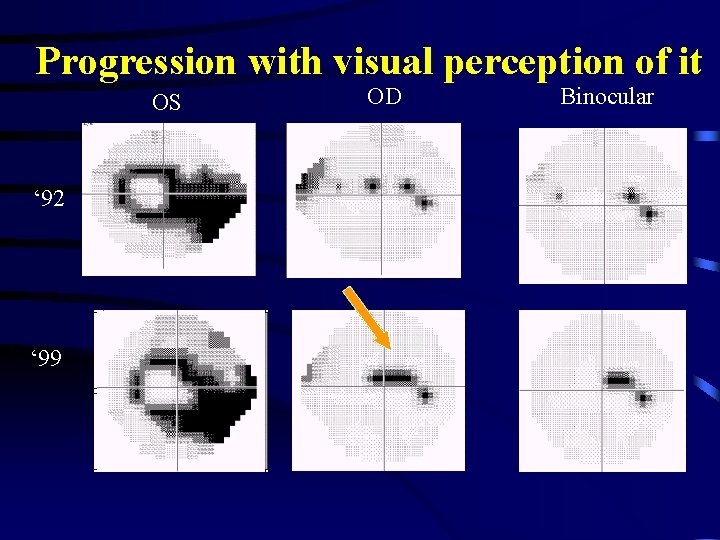
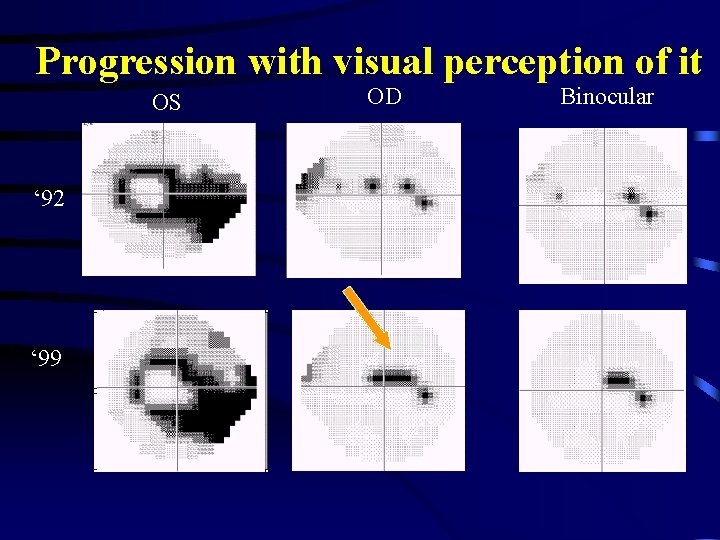
Progression with visual perception of it OS ‘ 92 ‘ 99 OD Binocular
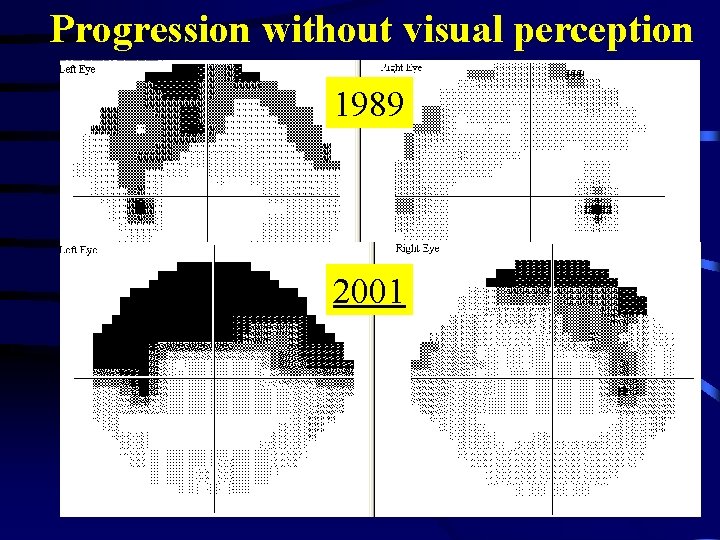
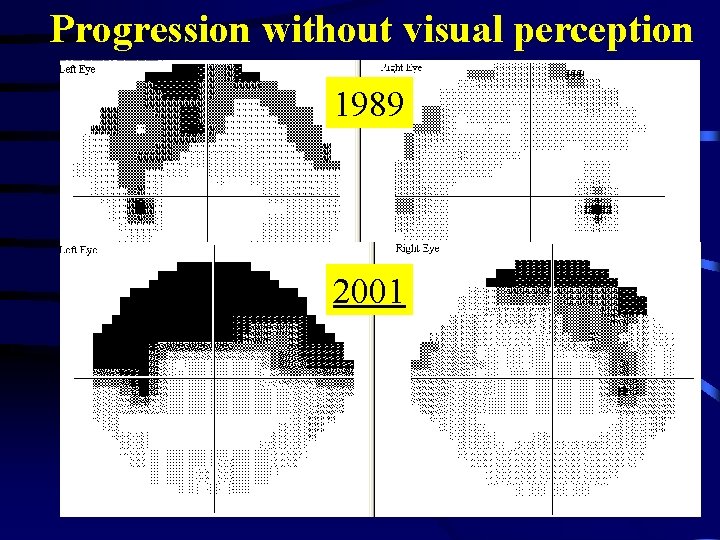
Progression without visual perception 1989 2001
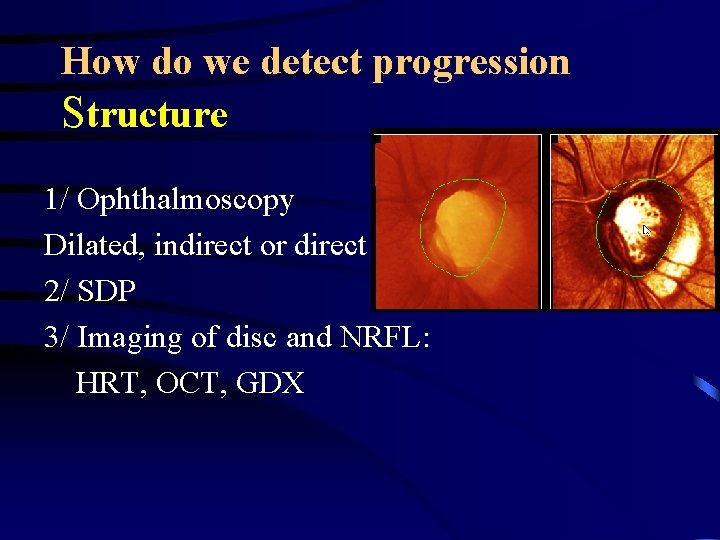
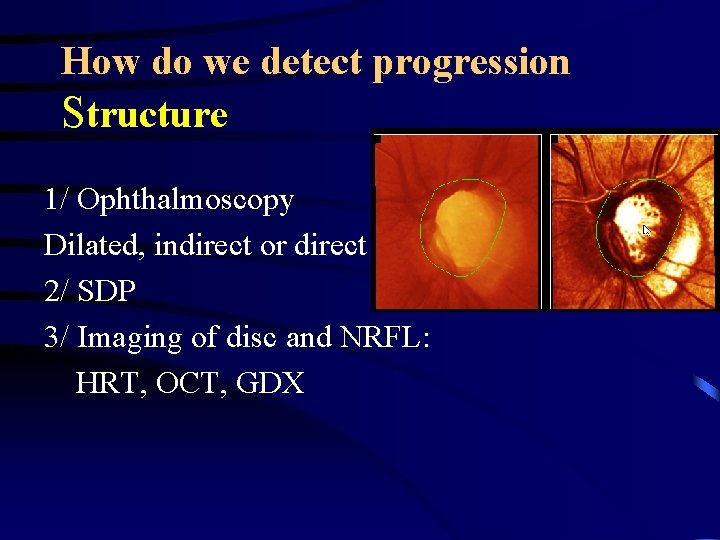
How do we detect progression Structure 1/ Ophthalmoscopy Dilated, indirect or direct 2/ SDP 3/ Imaging of disc and NRFL: HRT, OCT, GDX
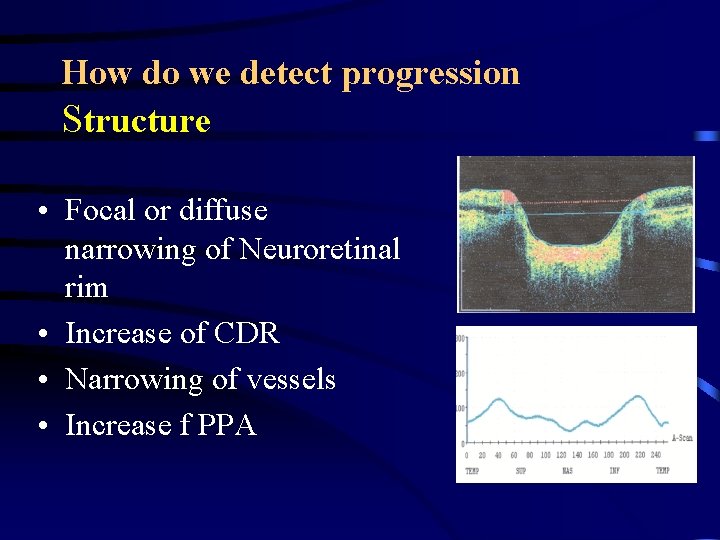
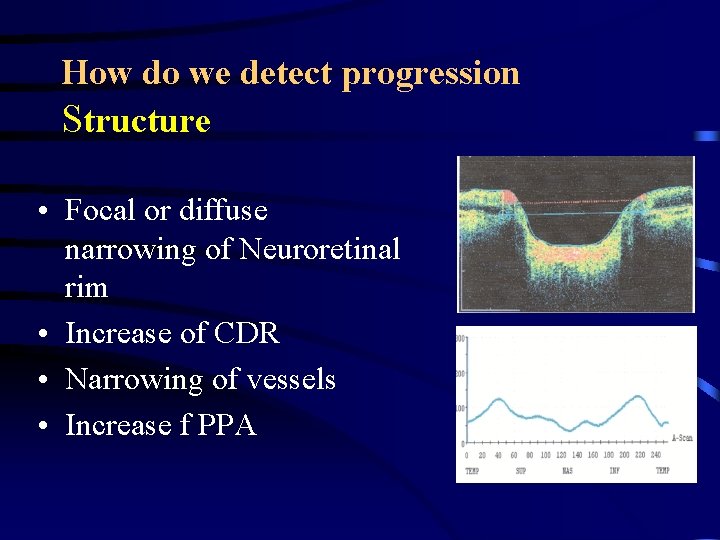
How do we detect progression Structure • Focal or diffuse narrowing of Neuroretinal rim • Increase of CDR • Narrowing of vessels • Increase f PPA
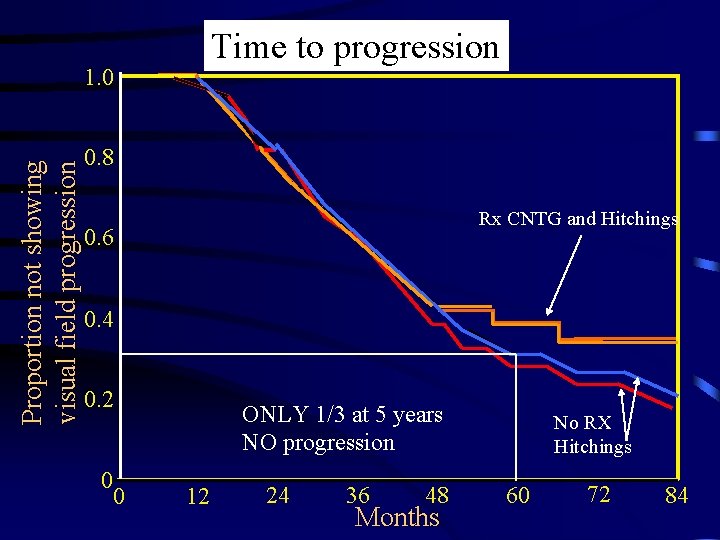
Natural history: CNTG Study
CNTG study: purpose • Is IOP part of the pathophy in NTG? • Does aggressive IOP lowering halt damage (ON and VF) in NTG at high risk of progression? • What are the risk and side effects of aggressive Rx?
CNTGS methods • • 230 eyes NTG defined as: Glaucomatous cupping of disc Characteristic VF defect Median IOP 20 mm. Hg or less in 10 baseline measurements
CNTGS results • One eye randomized to – no Rx – Meds, LTP or filter 30% IOP – • IOP from mean 16 to 11 mm. Hg • Progression is reduced from 60 to 20% in treated (after correction for cataract)
CNTG study: results • IOP is part of the pathogenic process • Lowering IOP by 30% slows VF loss – Hidden by cataract – Achieved in 50% of medical Rx • Rate of VF progression in NTG very variable • Risk factors for progression: DH, migraine, female
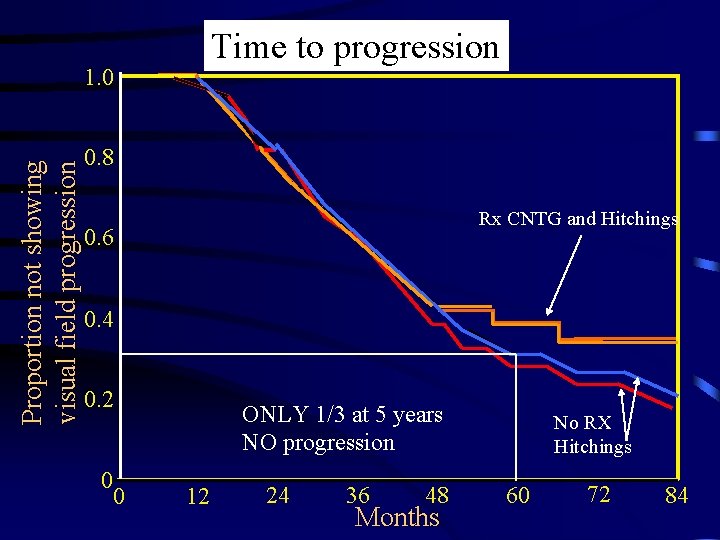
Time to progression Proportion not showing visual field progression 1. 0 0. 8 Rx CNTG and Hitchings 0. 6 0. 4 0. 2 0 0 ONLY 1/3 at 5 years NO progression 12 24 36 48 Months No RX Hitchings 60 72 84
Normal Pressure Glaucoma Diagnosis and therapy • Diagnosis • Differential diagnosis • Natural History • Investigation • Treatment
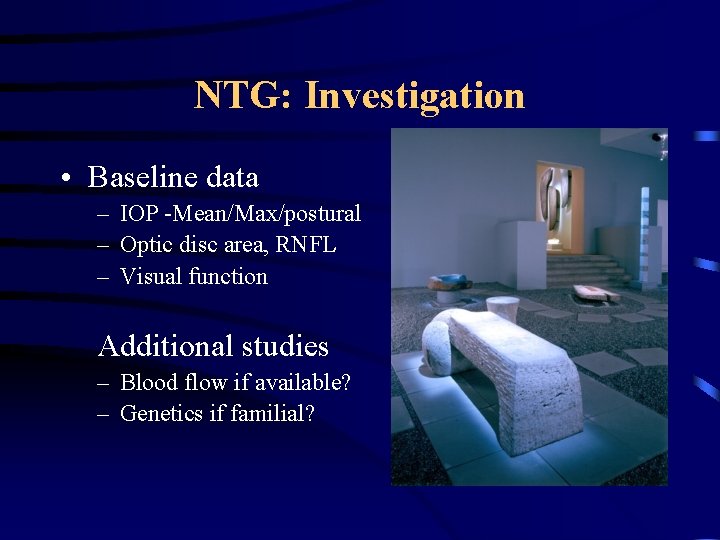
NTG: Investigation • Baseline data – IOP -Mean/Max/postural – Optic disc area, RNFL – Visual function Additional studies – Blood flow if available? – Genetics if familial?
NTG: Investigation • Causation – IOP – Perfusion pressure – Other Neurological • Investigations – – CCT, Diurnal, postural IOP Vascular, vasospasm Visual pathways-MRI
Normal Pressure Glaucoma Diagnosis and therapy • Diagnosis • Differential diagnosis • Natural History • Investigation • Treatment
NTG: Treatment • Nil • IOP reduction • Medical • Laser • Surgery • Non IOP reducing • Ca channel blockers • Neuroprotection
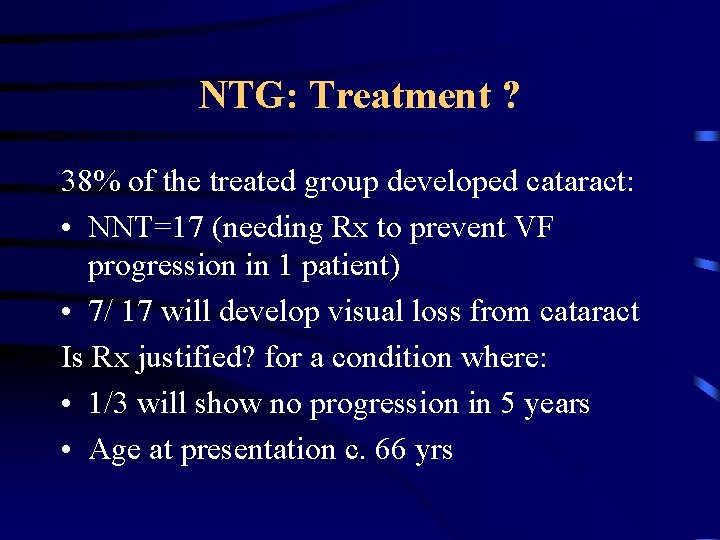
NTG: Treatment ? 38% of the treated group developed cataract: • NNT=17 (needing Rx to prevent VF progression in 1 patient) • 7/ 17 will develop visual loss from cataract Is Rx justified? for a condition where: • 1/3 will show no progression in 5 years • Age at presentation c. 66 yrs
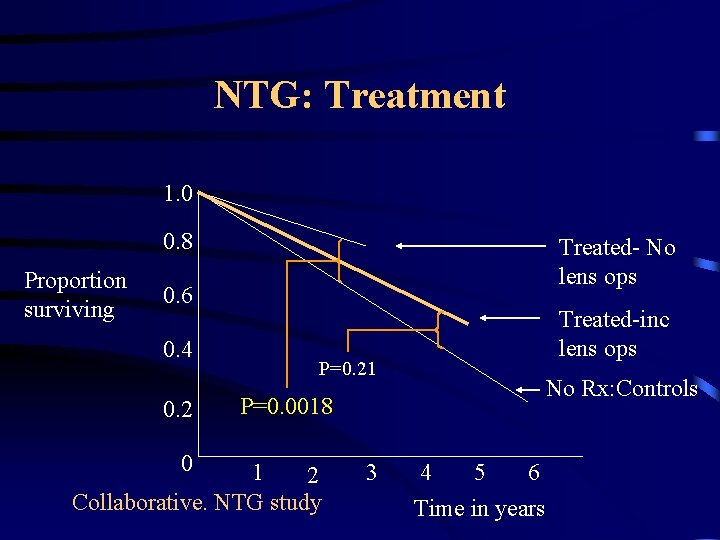
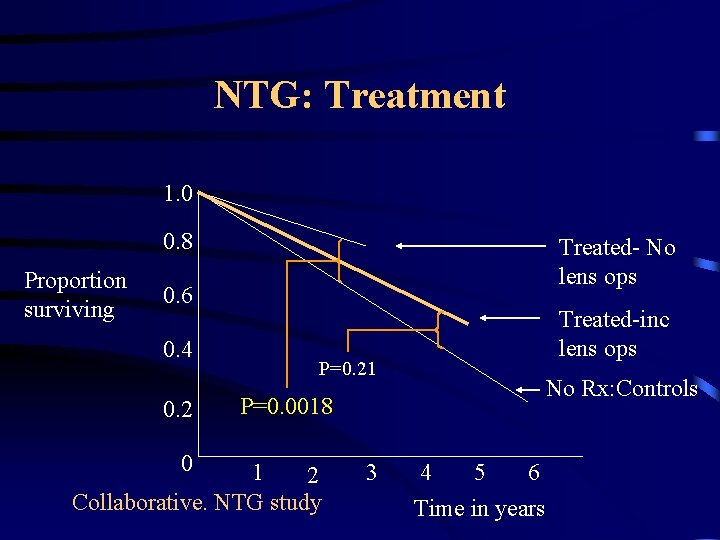
NTG: Treatment 1. 0 0. 8 Proportion surviving Treated- No lens ops 0. 6 0. 4 0. 2 0 Treated-inc lens ops P=0. 21 No Rx: Controls P=0. 0018 1 2 Collaborative. NTG study 3 4 5 6 Time in years
NTG: Treatment Medical – Avoid the Beta –blockers and Alphaadrenergic agonists: they may affect perfusion pressure – PG can give 15 -30% IOP reduction – PG good in the NTG range, – PG increase pulsatile OBF – Brimonidine reduce 20% and may be neuroprotective – If necessary consider SLT

NTG: Treatment Surgery • CNGTS 30% IOP • EMGT 25% IOP on meds in 50% cases on Betaxolol and ALTP Surgery + 25 % Traby + 5 FU (Membrey et al) Traby in CNGTS 50% cases
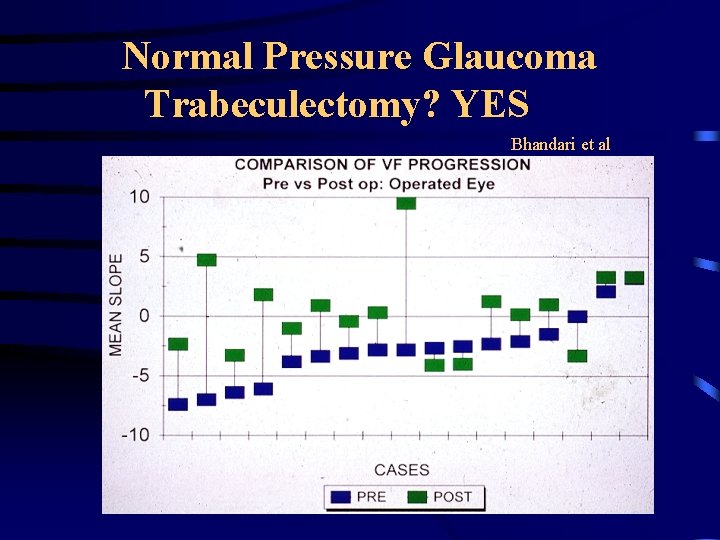
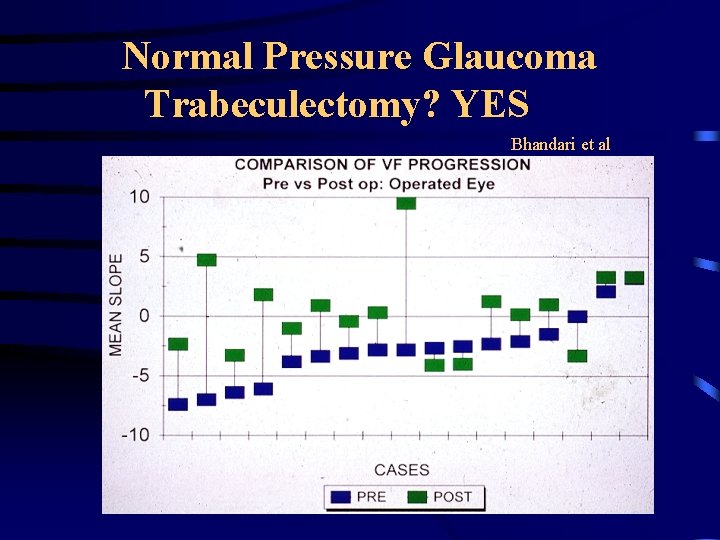
Normal Pressure Glaucoma Trabeculectomy? YES Bhandari et al

NTG-diagnosis and therapy • Is the diagnosis correct? GON + VF • What investigations do I need? Risk factors • What type of follow-up tests? VF, Imaging • Do I treat? YES! -30%
Thank you