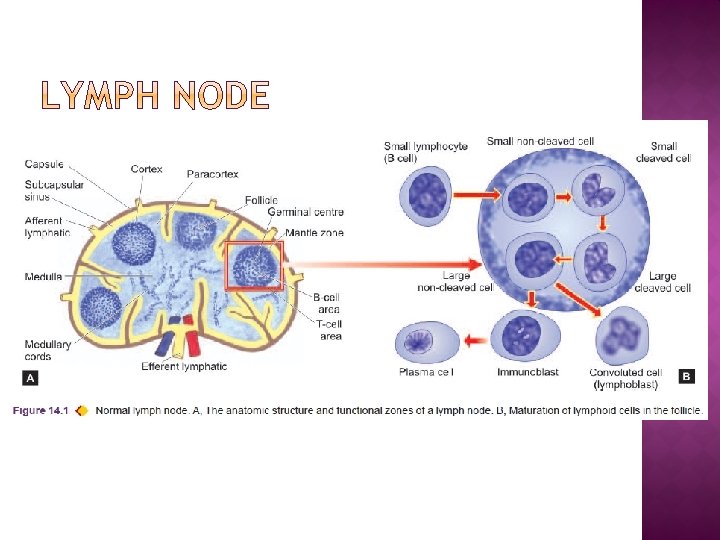
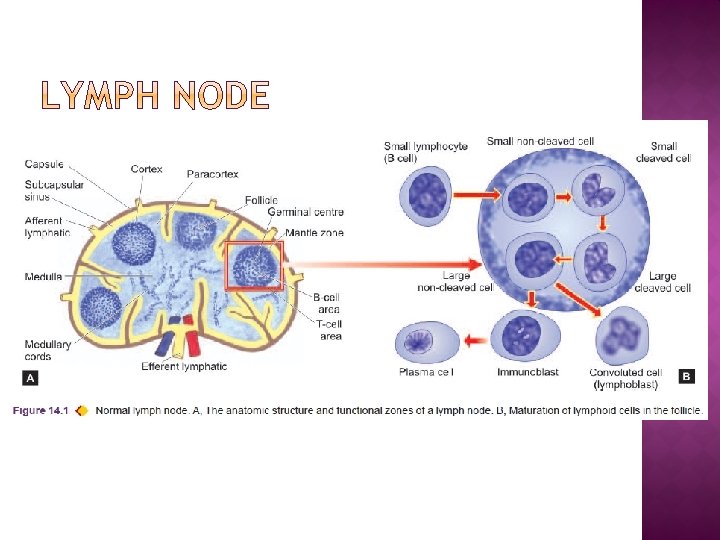
Normal lymph node structure Reactive Non specific lymphadenitis



- Slides: 46
� Normal lymph node structure � Reactive / Non specific lymphadenitis � Granulomatous � HIV lymphadenitis lymphadenopathy � Causes of spenomegaly
� In response to a wide variety of stimuli (microbial infections, drugs, environmental pollutants, tissue injury, immune-complexes and malignant neoplasms) Lymph nodes undergo reactive changes. � Most common causes of lymph node enlargement are inflammatory and immune reactions
� LN enlargement due to Ø primary inflammatory reaction reactive lymphadenitis Ø primary immune reactions lymphadenopathy � Reactive lymphadenitis is a nonspecific response � Categorised into acute and chronic types.
� All kinds of acute inflammations may cause acute nonspecific lymphadenitis in the nodes draining the area of inflamed tissue. � Most common causes are microbiologic infections or their breakdown products, and foreign bodies in the wound or into the circulation etc.
� Most frequently involved lymph nodes are: Ø Cervical (due to infections in the oral cavity) Ø Axillary (due to infection in the arm) Ø Inguinal (due to infection in the lower extremities) Ø Mesenteric (due to acute appendicitis, acute enteritis etc)
� Acute lymphadenitis is usually mild and transient � Occasionally it may be more severe. � Acutely inflamed nodes are enlarged, tender, and if extensively involved, may be fluctuant. � Overlying skin is red and hot. � After control of infection, majority of cases heal completely without leaving any scar. � If the inflammation does not subside, acute lymphadenitis changes into chronic lymphadenitis.
Grossly: � Affected lymph nodes are enlarged 2 -3 times their normal size � May show abscess formation if the involvement is extensive.

Microscopically: � Sinusoids are congested, widely dilated and oedematous and contain numerous neutrophils. � Lymphoid follicles are prominent with presence of many mitoses and phagocytosis. � In more severe cases necrosis may occur and neutrophil abscesses may form.
� Commonly called reactive lymphoid hyperplasia � Common form of inflammatory reaction of draining lymph nodes as a response to antigenic stimuli such as repeated attacks of acute lymphadenitis and lymph from malignant tumours.
� Depending upon the pattern three types are distinguished, each having its own set of causes. 1. Follicular hyperplasia 2. Paracortical hyperplasia 3. Sinus histiocytosis

Grossly: � Affected lymph nodes are usually enlarged, firm and non-tender.
Microscopically: 1. Follicular hyperplasia: � Most frequent pattern, particularly encountered in children. � Besides nonspecific stimulation, a few specific causes are: Ø Rheumatoid arthritis Ø Toxoplasmosis Ø Syphilis Ø AIDS
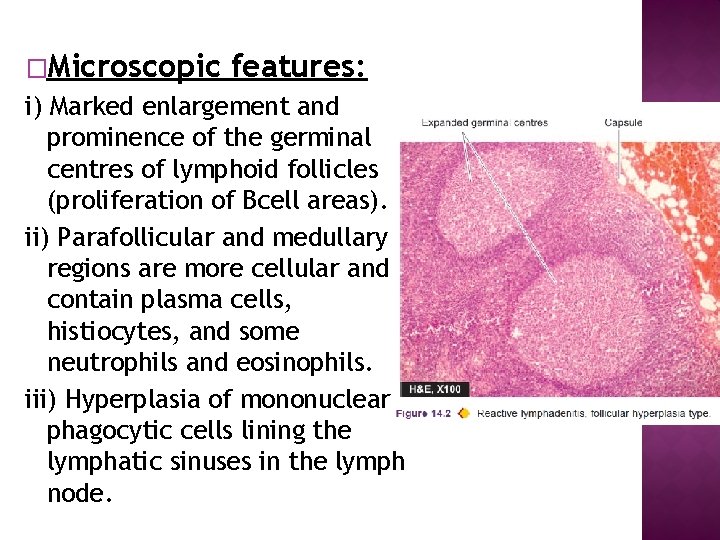
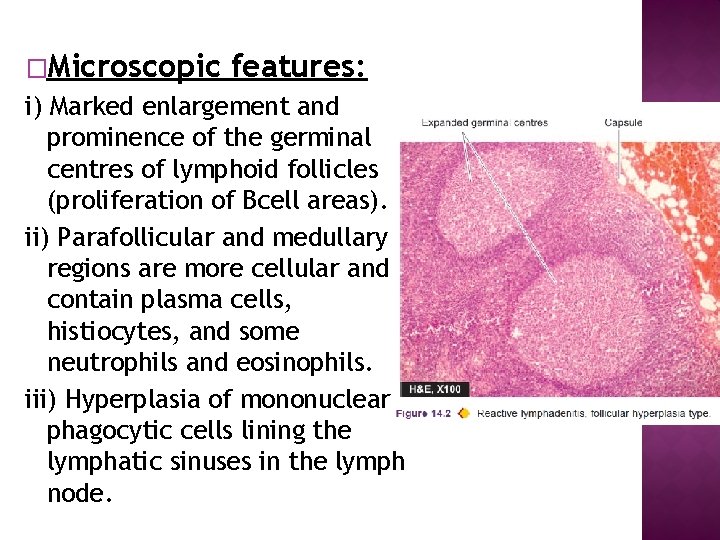
�Microscopic features: i) Marked enlargement and prominence of the germinal centres of lymphoid follicles (proliferation of Bcell areas). ii) Parafollicular and medullary regions are more cellular and contain plasma cells, histiocytes, and some neutrophils and eosinophils. iii) Hyperplasia of mononuclear phagocytic cells lining the lymphatic sinuses in the lymph node.
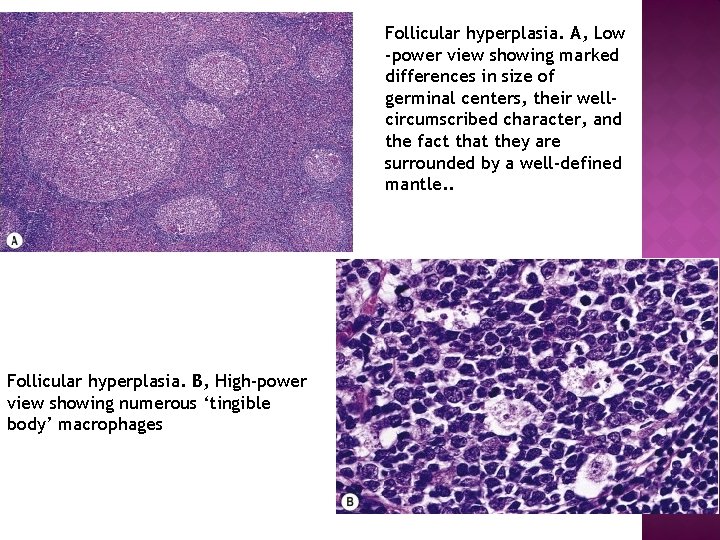
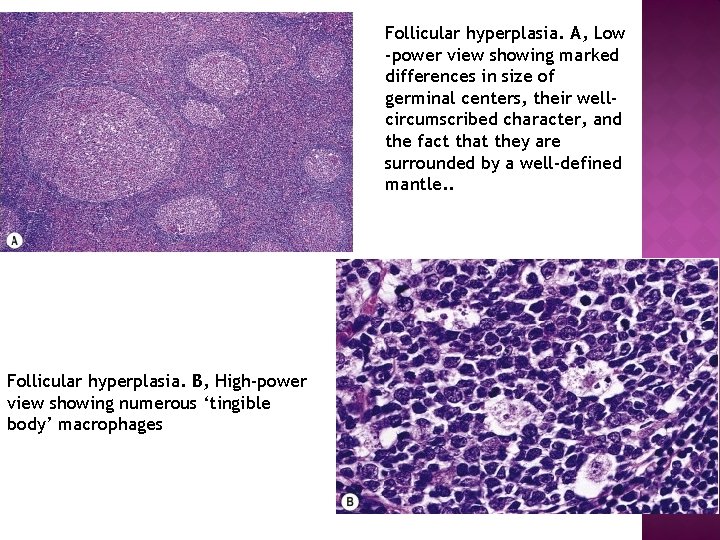
Follicular hyperplasia. A, Low -power view showing marked differences in size of germinal centers, their wellcircumscribed character, and the fact that they are surrounded by a well-defined mantle. . Follicular hyperplasia. B, High-power view showing numerous ‘tingible body’ macrophages
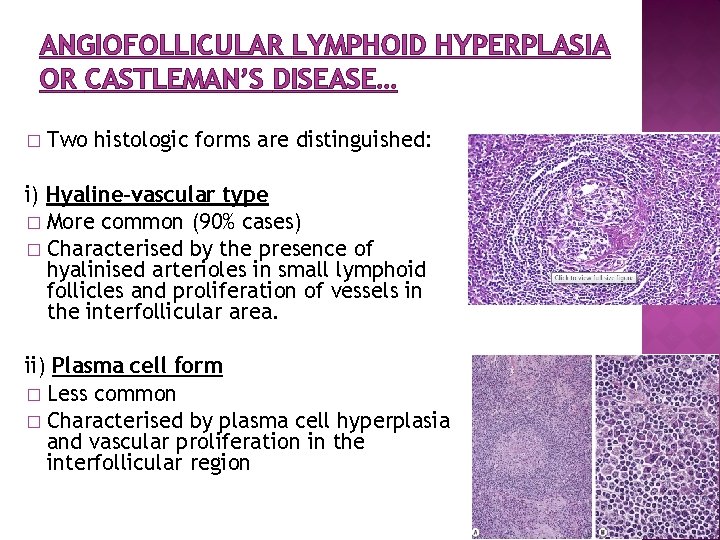
ANGIOFOLLICULAR LYMPHOID HYPERPLASIA OR CASTLEMAN’S DISEASE � Clinicopathologic variant of follicular hyperplasia. � Occur at any age � Association with Epstein-Barr virus infection
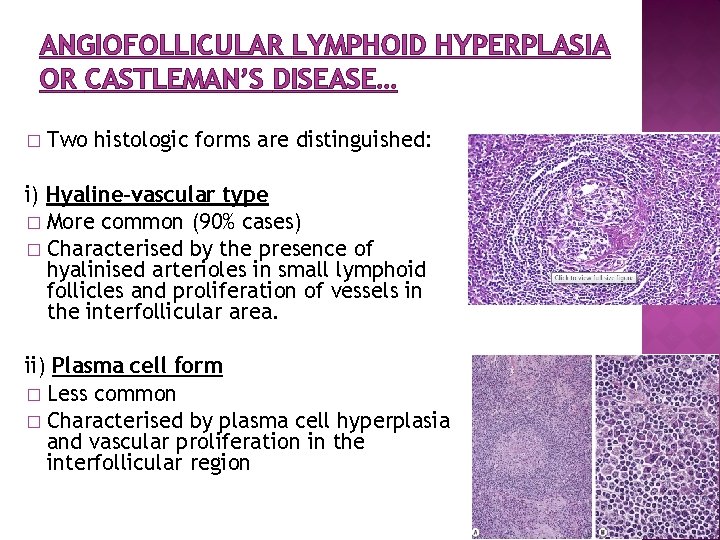
ANGIOFOLLICULAR LYMPHOID HYPERPLASIA OR CASTLEMAN’S DISEASE… � Two histologic forms are distinguished: i) Hyaline-vascular type � More common (90% cases) � Characterised by the presence of hyalinised arterioles in small lymphoid follicles and proliferation of vessels in the interfollicular area. ii) Plasma cell form � Less common � Characterised by plasma cell hyperplasia and vascular proliferation in the interfollicular region
� Hyperplasia of T-cell-dependent area of the lymph node � Causes immunologic reactions caused by drugs (e. g. dilantin), vaccination, viruses (e. g. infectious mononucleosis) and autoimmune disorders.
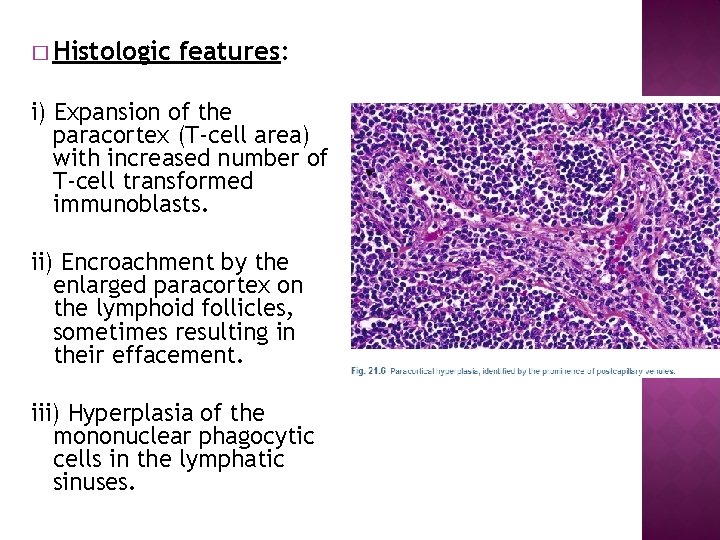
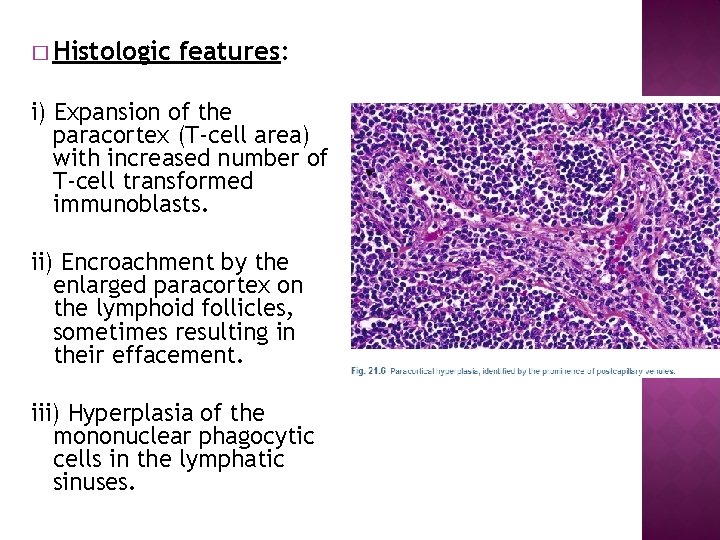
� Histologic features: i) Expansion of the paracortex (T-cell area) with increased number of T-cell transformed immunoblasts. ii) Encroachment by the enlarged paracortex on the lymphoid follicles, sometimes resulting in their effacement. iii) Hyperplasia of the mononuclear phagocytic cells in the lymphatic sinuses.
� Variants of paracortical lymphoid hyperplasia: Ø Angio-immunoblastic lymphadenopathy Ø Dermatopathic lymphadenopathy Ø Dilantin lymphadenopathy Ø Postvaccinial lymphadenopathy
Angioimmunoblastic lymphadenopathy Ø characterised by diffuse hyperplasia of immunoblasts rather than paracortical hyperplasia only, and there is proliferation of blood vessels Ø occurs in elderly patients with generalised lymph node enlargement and hypergammaglobulinaemia. Dermatopathic lymphadenopathy � occurs in lymph node draining an area of skin lesion � hyperplastic paracortex + presence of dark melanin pigment within the macrophages in the lymph node.
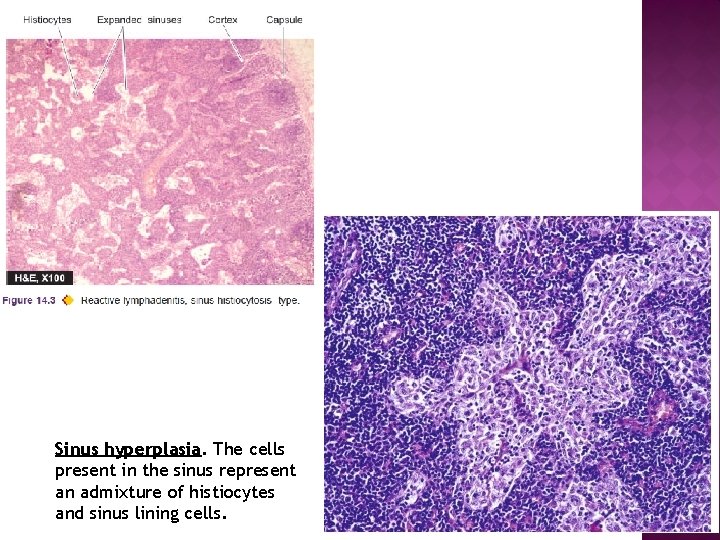
� Very common type found in regional lymph nodes draining inflammatory lesions, or as an immune reaction of the host to a draining malignant tumour or its products. � Hallmark of histologic diagnosis is the expansion of the sinuses by proliferating large histiocytes containing phagocytosed material.
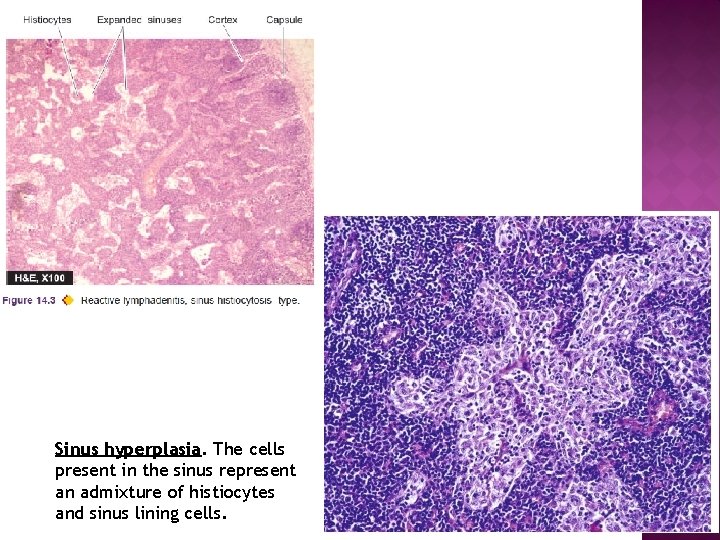
Sinus hyperplasia. The cells present in the sinus represent an admixture of histiocytes and sinus lining cells.
� Diseases that can result in granulomatous formations in lymph nodes include: Ø Various types of infection Ø Foreign body reactions Ø Aberrant immune reactions Ø Secondary responses in lymph nodes draining carcinoma or in patients with hodgkins lymphoma and other lymphomas, whether the node is involved by the malignancy or not.
�A granuloma is a focus of chronic inflammation consisting of a microscopic aggregation of macrophages that are transformed into epithelium-like cells, called epithelioid cells � surrounded by a collar of mononuclear leukocytes, principally lymphocytes and occasionally plasma cells 26
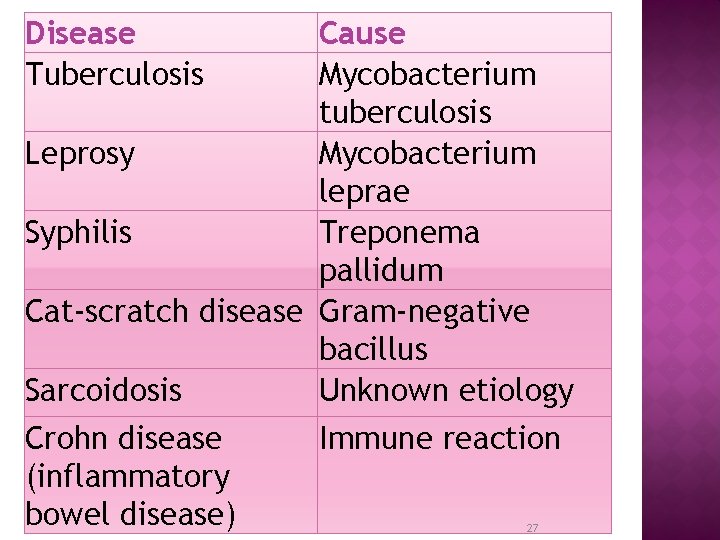
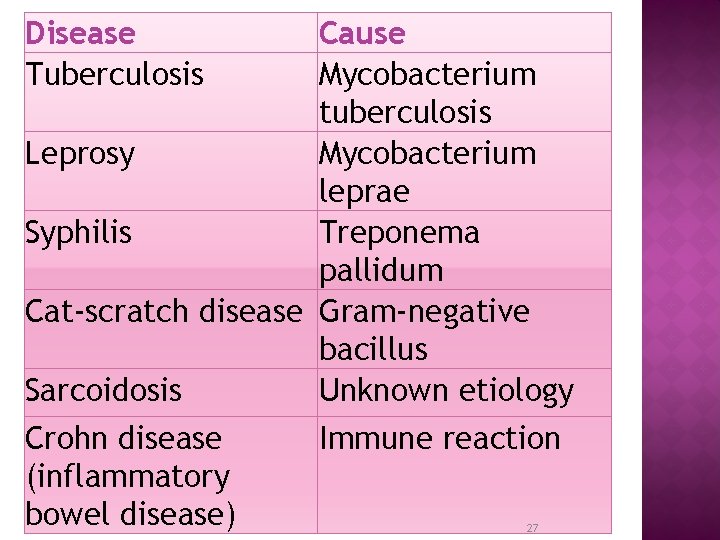
Disease Tuberculosis Cause Mycobacterium tuberculosis Leprosy Mycobacterium leprae Syphilis Treponema pallidum Cat-scratch disease Gram-negative bacillus Sarcoidosis Unknown etiology Crohn disease Immune reaction (inflammatory bowel disease) 27
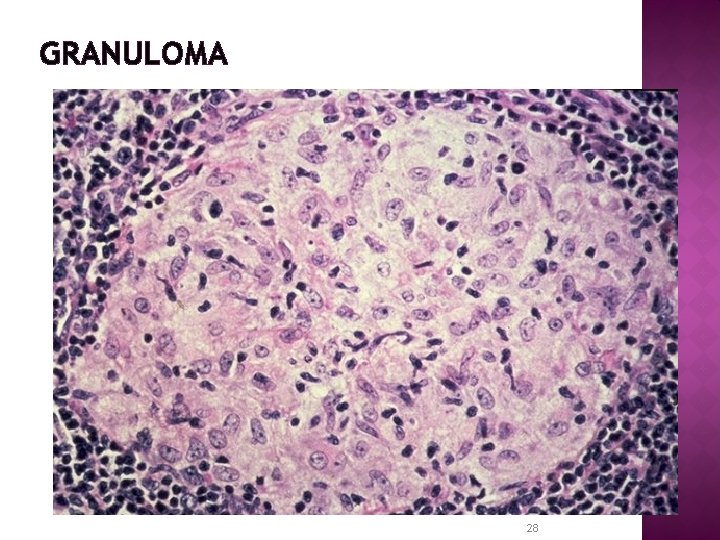
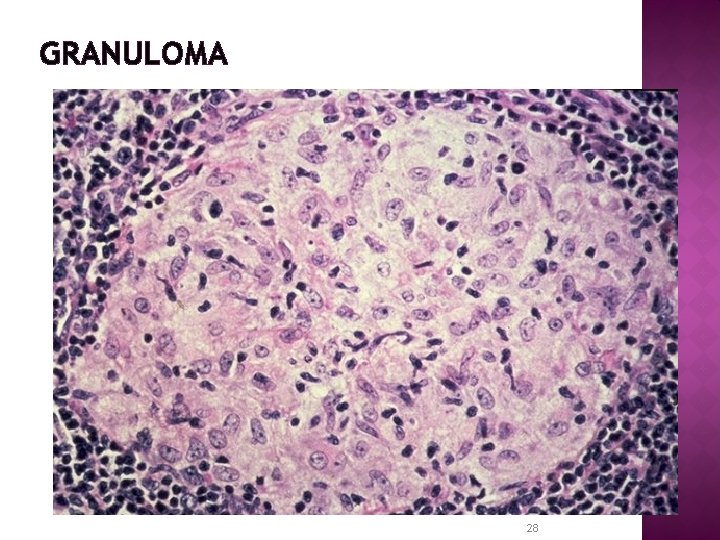
GRANULOMA 28
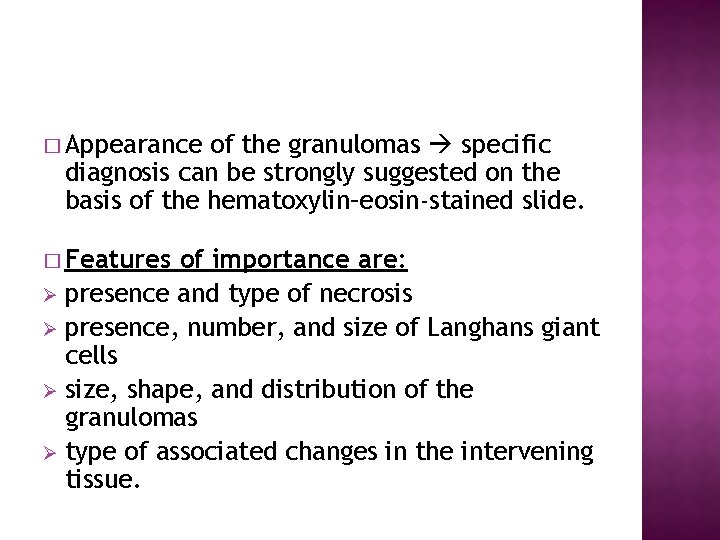
� Appearance of the granulomas specific diagnosis can be strongly suggested on the basis of the hematoxylin–eosin-stained slide. � Features of importance are: Ø presence and type of necrosis Ø presence, number, and size of Langhans giant cells Ø size, shape, and distribution of the granulomas Ø type of associated changes in the intervening tissue.
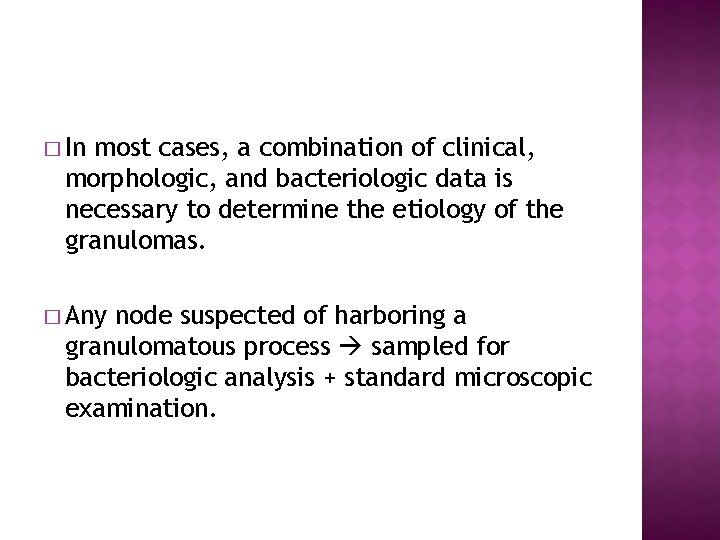
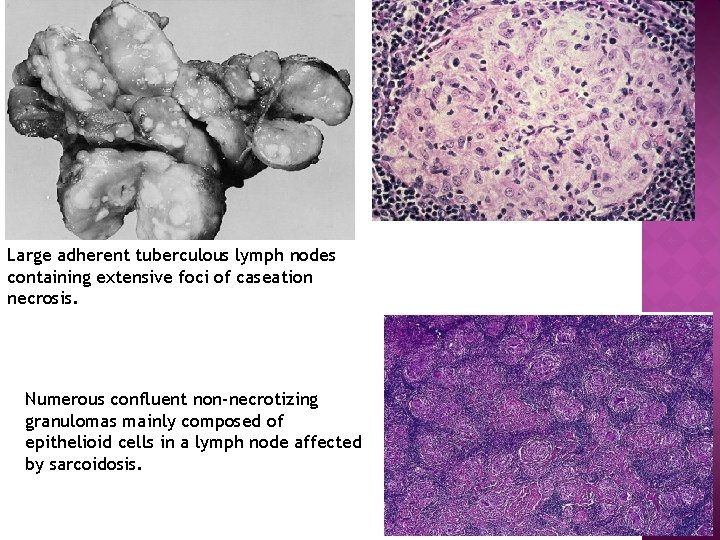
� In most cases, a combination of clinical, morphologic, and bacteriologic data is necessary to determine the etiology of the granulomas. � Any node suspected of harboring a granulomatous process sampled for bacteriologic analysis + standard microscopic examination.
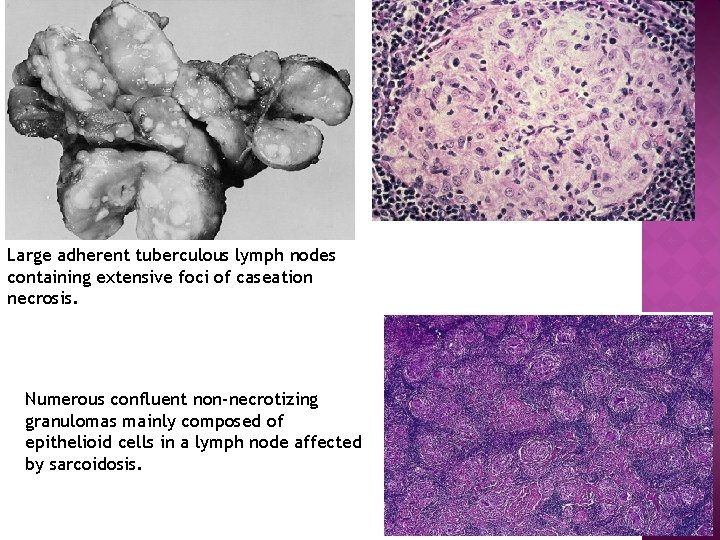
Large adherent tuberculous lymph nodes containing extensive foci of caseation necrosis. Numerous confluent non-necrotizing granulomas mainly composed of epithelioid cells in a lymph node affected by sarcoidosis.
� Persistent generalised lymphadenopathy (PGL) � Earliest symptom of primary HIV infection � Presence of enlarged lymph nodes of more than 1 cm diameter at two or more extrainguinal sites for more than 3 months without any other obvious cause.
Histologically, � Findings at biopsy of involved lymph node vary depending upon the stage of HIV infection: 1. In the early stage marked follicular hyperplasia and reflects the polyclonal B-cell proliferation. 2 In the intermediate stage combination of follicular hyperplasia and follicular involution.
3. In the last stage � Decrease in the lymph node size indicative of prognostic marker of disease progression. � Microscopic findings of node at this stage reveal follicular involution and lymphocyte depletion.
� Enlargement of the spleen termed splenomegaly � Occurs in a wide variety of disorders which increase the cellularity and vascularity of the organ. � Many of the causes are exaggerated forms of normal splenic function.
� Splenic enlargement may occur as a result of of the following pathophysiologic mechanisms: I. Infections II. Disordered immunoregulation III. Altered splenic blood flow IV. Lymphohaematogenous malignancies V. Diseases with abnormal erythrocytes VI. Storage diseases VII. Miscellaneous causes
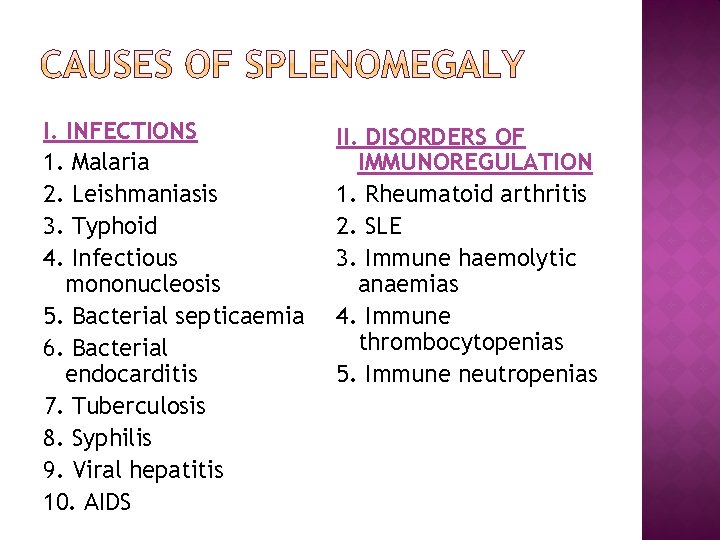
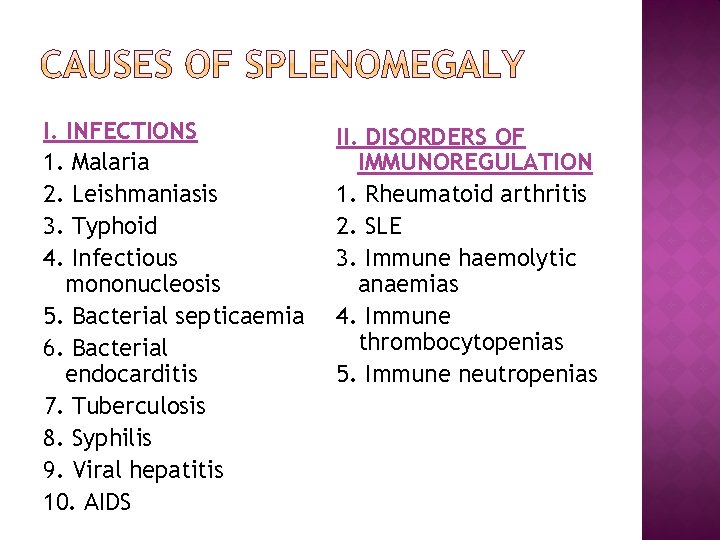
I. INFECTIONS 1. Malaria 2. Leishmaniasis 3. Typhoid 4. Infectious mononucleosis 5. Bacterial septicaemia 6. Bacterial endocarditis 7. Tuberculosis 8. Syphilis 9. Viral hepatitis 10. AIDS II. DISORDERS OF IMMUNOREGULATION 1. Rheumatoid arthritis 2. SLE 3. Immune haemolytic anaemias 4. Immune thrombocytopenias 5. Immune neutropenias
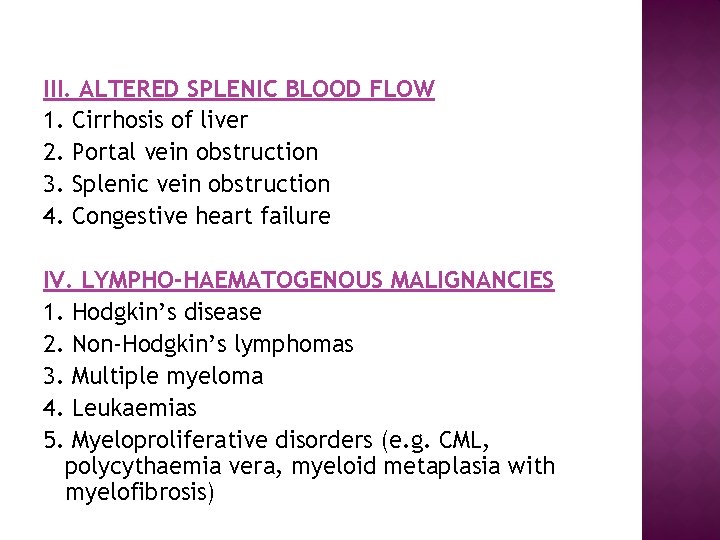
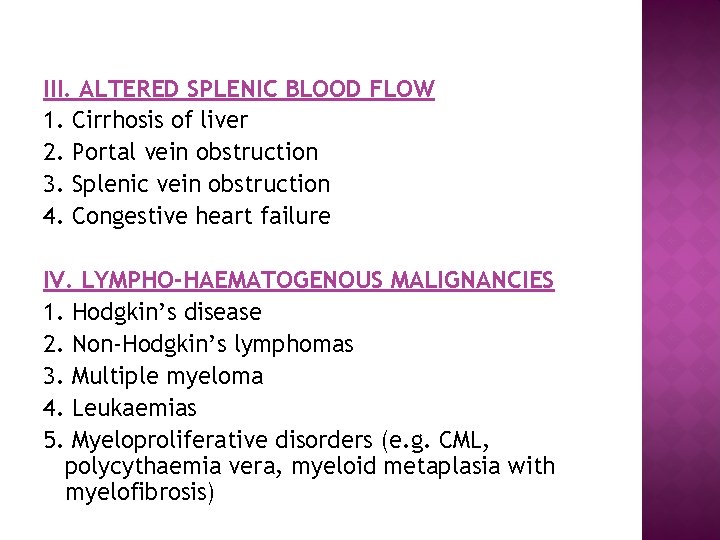
III. ALTERED SPLENIC BLOOD FLOW 1. Cirrhosis of liver 2. Portal vein obstruction 3. Splenic vein obstruction 4. Congestive heart failure IV. LYMPHO-HAEMATOGENOUS MALIGNANCIES 1. Hodgkin’s disease 2. Non-Hodgkin’s lymphomas 3. Multiple myeloma 4. Leukaemias 5. Myeloproliferative disorders (e. g. CML, polycythaemia vera, myeloid metaplasia with myelofibrosis)
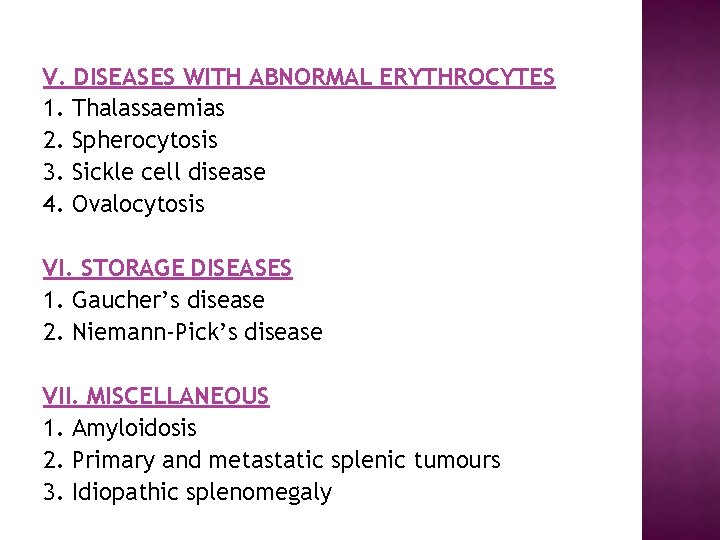
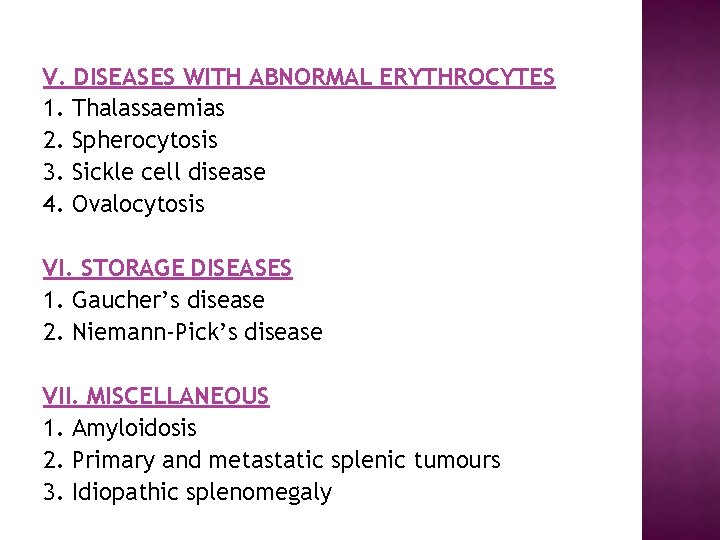
V. DISEASES WITH ABNORMAL ERYTHROCYTES 1. Thalassaemias 2. Spherocytosis 3. Sickle cell disease 4. Ovalocytosis VI. STORAGE DISEASES 1. Gaucher’s disease 2. Niemann-Pick’s disease VII. MISCELLANEOUS 1. Amyloidosis 2. Primary and metastatic splenic tumours 3. Idiopathic splenomegaly
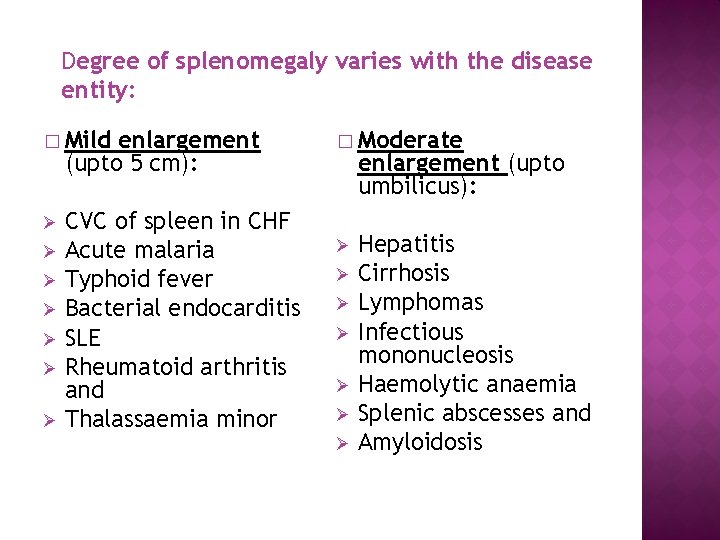
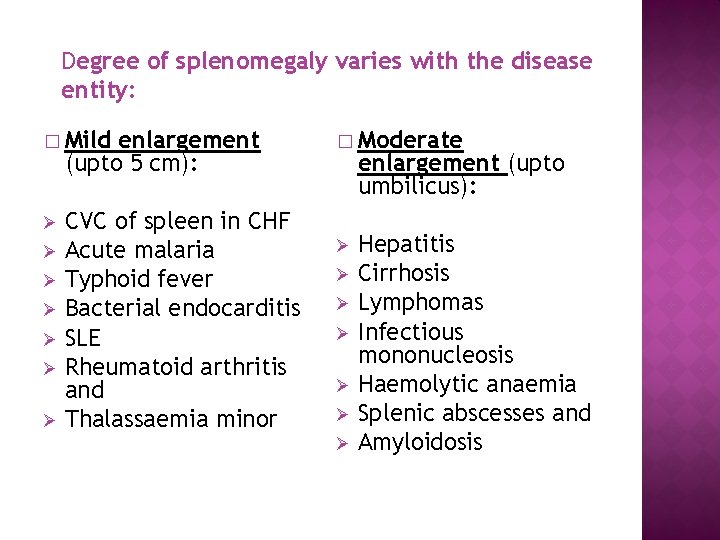
Degree of splenomegaly varies with the disease entity: � Mild enlargement (upto 5 cm): Ø Ø Ø Ø CVC of spleen in CHF Acute malaria Typhoid fever Bacterial endocarditis SLE Rheumatoid arthritis and Thalassaemia minor � Moderate enlargement (upto umbilicus): Ø Ø Ø Ø Hepatitis Cirrhosis Lymphomas Infectious mononucleosis Haemolytic anaemia Splenic abscesses and Amyloidosis
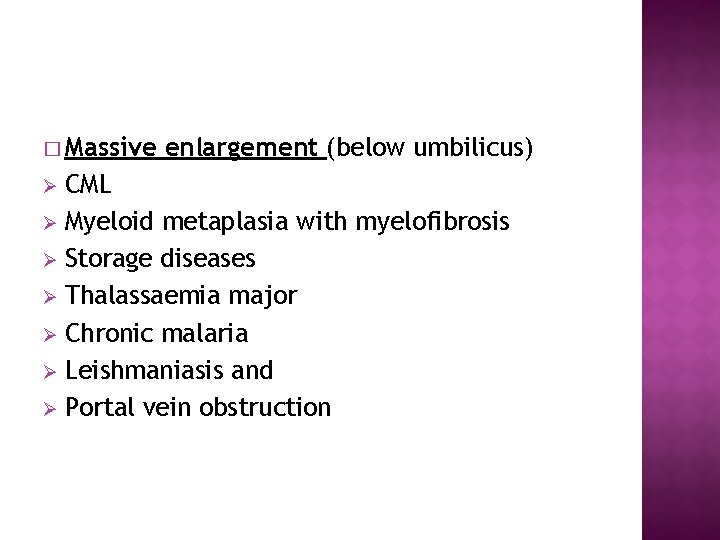
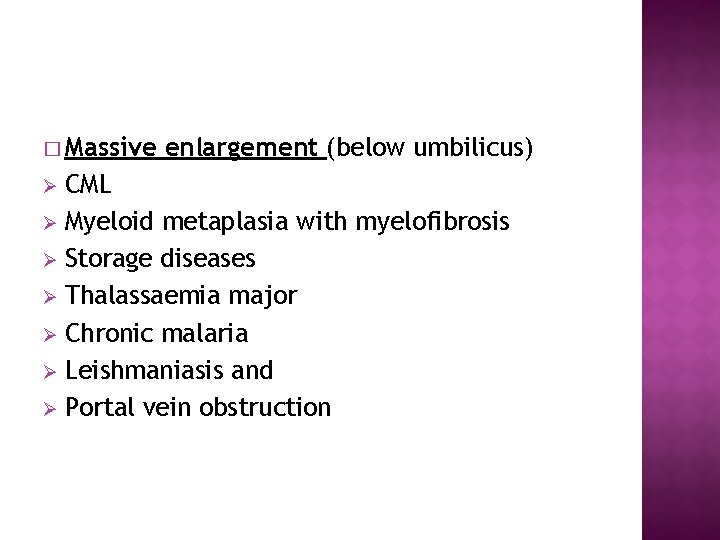
� Massive enlargement (below umbilicus) CML Ø Myeloid metaplasia with myelofibrosis Ø Storage diseases Ø Thalassaemia major Ø Chronic malaria Ø Leishmaniasis and Ø Portal vein obstruction Ø
� Mild to moderate splenomegaly is usually symptomless � Massively enlarged spleen may cause dragging sensation in the left hypochondrium � Spleen becomes palpable only when it is enlarged.
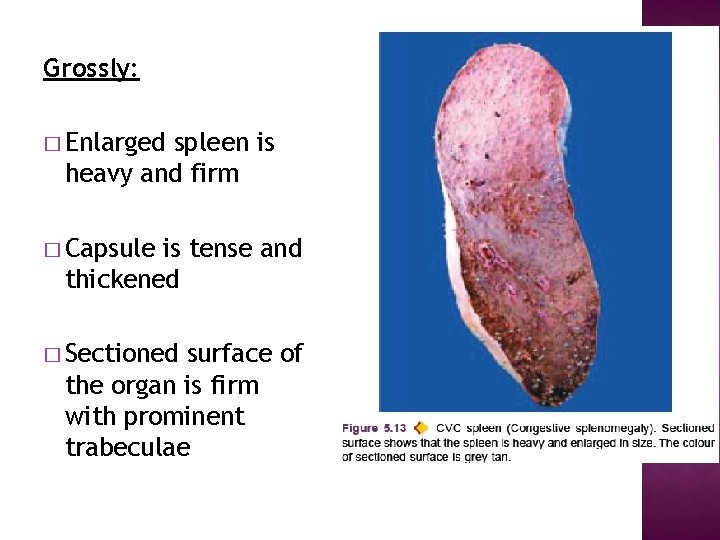
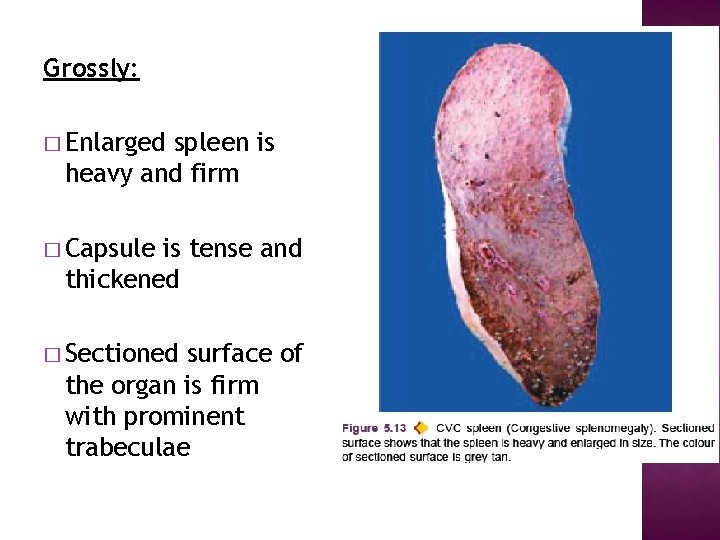
Grossly: � Enlarged spleen is heavy and firm � Capsule is tense and thickened � Sectioned surface of the organ is firm with prominent trabeculae
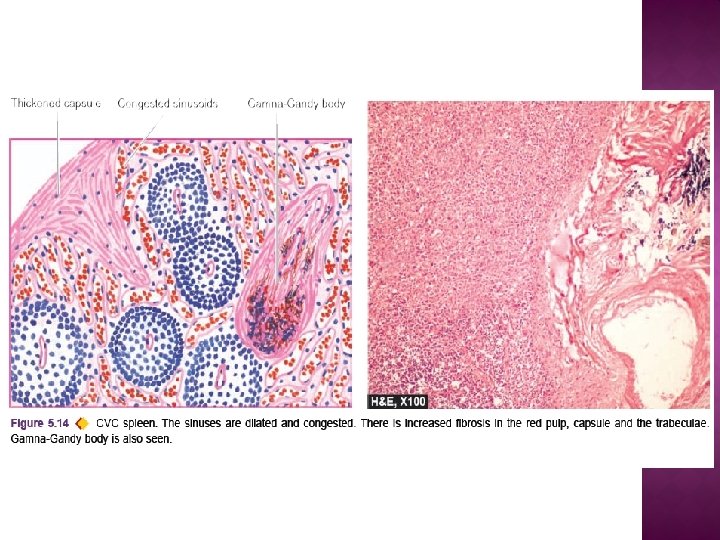
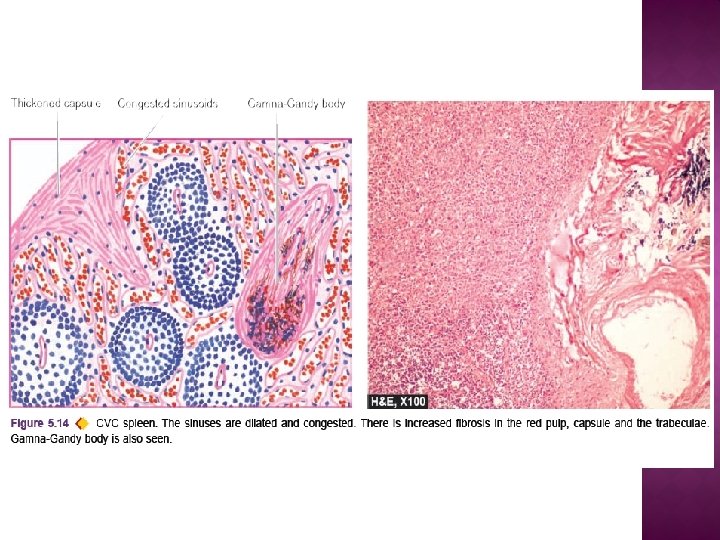
Microscopically: � Dilatation of sinusoids with prominence of splenic cords. � White pulp is atrophic while the trabeculae are thickened. � Long-standing congestion haemorrhages and Gamna-Gandy bodies resulting in fibrocongestive splenomegaly, also called Banti’s spleen