Normal Anatomy and Physiology of the Female Pelvis


- Slides: 65
Normal Anatomy and Physiology of the Female Pelvis Chapter 39 Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc.

The Bony Pelvis § Consists of four bones ü Two innominate (coxal) bones- form anterior and lateral margins ü Sacrum- forms posterior wall ü Coccyx- forms posterior wall Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 2
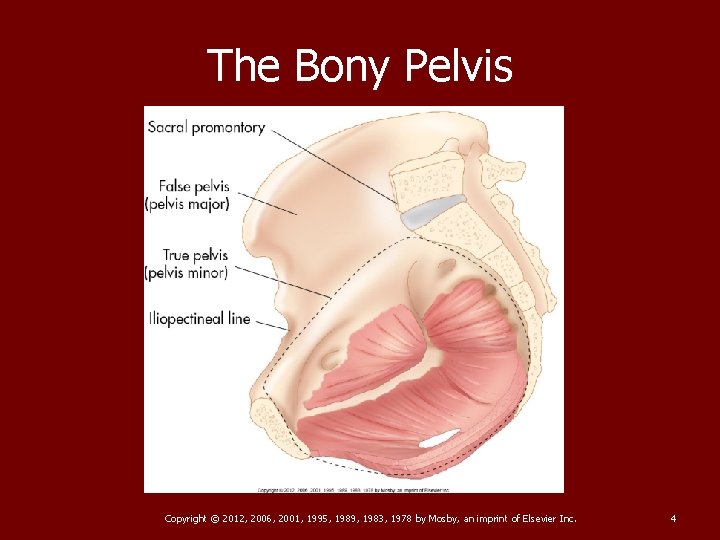
The Bony Pelvis Further divided into two continuous compartments (True and False Pelvis) § Divided by imaginary line known as the ileopectineal line. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 3
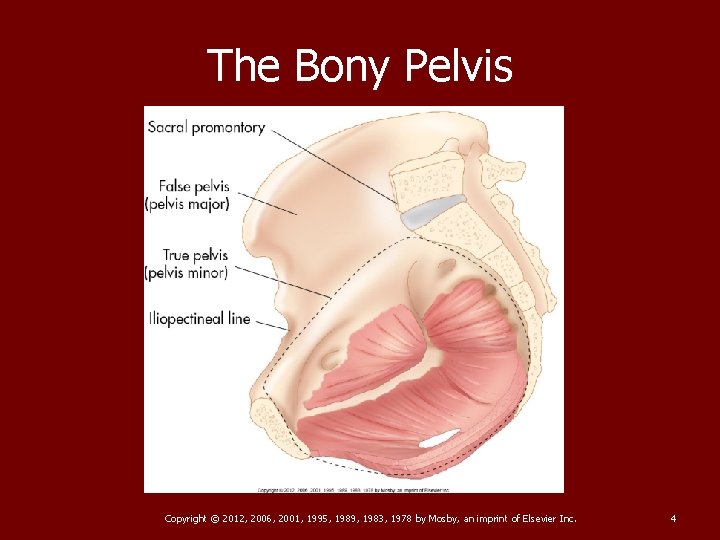
The Bony Pelvis Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 4
The Pelvic Cavity TRUE PELVIS § True pelvis is considered the pelvic cavity (Figure 39 -3). § True pelvis contains the urinary bladder, small bowel, sigmoid colon, rectum, ovaries, fallopian tubes, and uterus Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 5
The Pelvic Cavity True Pelvis § Lower margin of pelvic cavity (pelvic floor) formed by levator ani and coccygeus muscles and is known as pelvic diaphragm § The area below pelvic floor is perineum § Posterolateral wall formed by piriformis and coccygeus muscles Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 6

Bladder § Sits in Anterior portion of pelvic cavity § Functions to collect and store urine until it empties through the urethra Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 7
Ureters § Two tubes that carry urine from the kidneys to the bladder. § Run anterior and lateral to upper vagina to enter posteroinferior bladder § Are commonly imaged when evaluating kidneys for obstruction. § Pregnancy, fibroids, ovarian mass, or distal ureter calculi can lead to dilated ureters Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 8
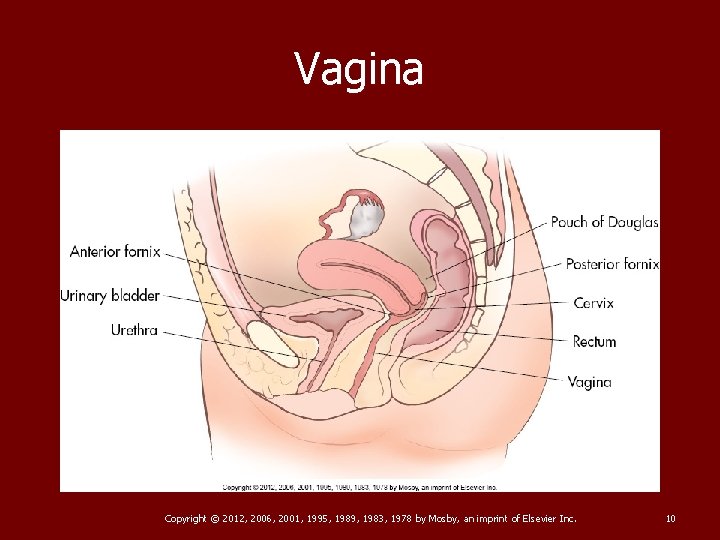
Vagina § Collapsed muscular tube that extends from external genitalia to cervix of uterus § Lies posterior to urinary bladder and urethra, anterior to rectum and anus Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 9
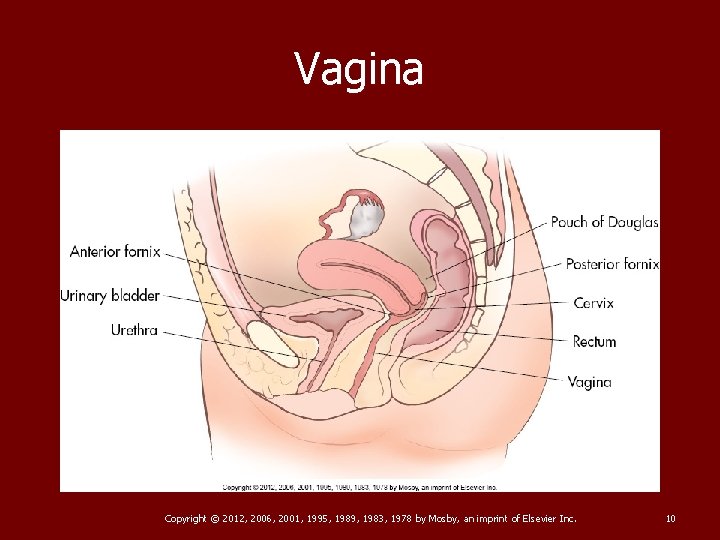
Vagina Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 10
Vagina § Normally directed upward and backward, forming 90 -degree angle with uterine cervix § Measures approximately 9 cm in length; is longest along posterior wall Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 11
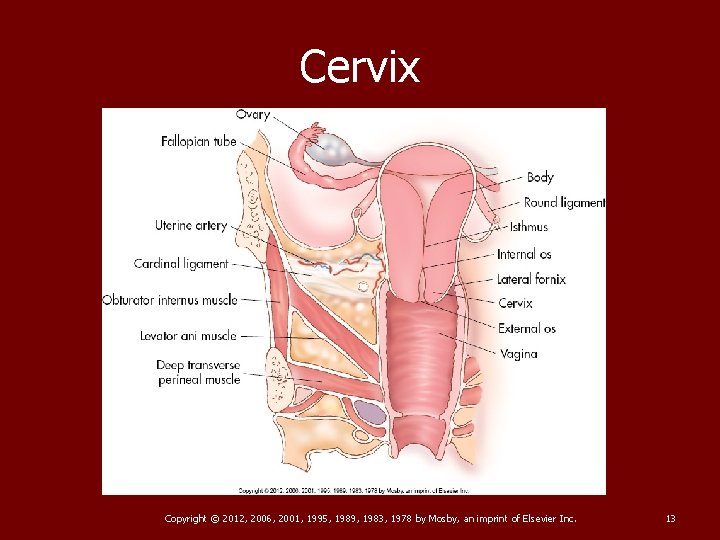
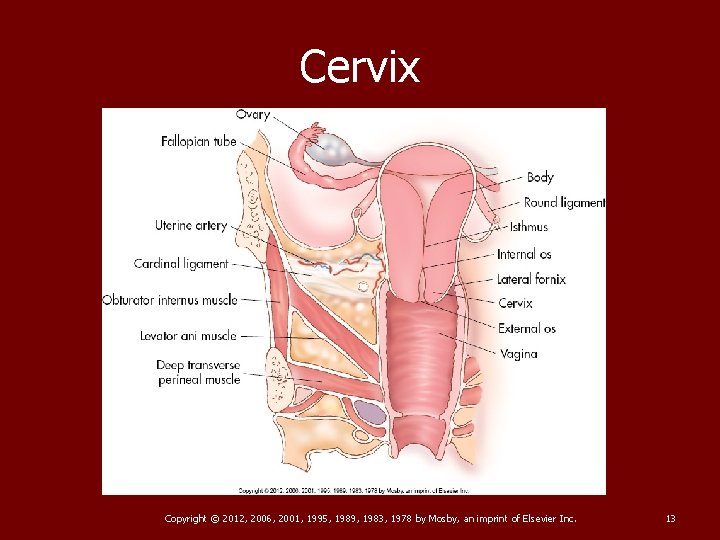
Cervix § Projects into vaginal canal § The uterine cervix protrudes into the upper portion of the vaginal canal forming arch like recesses called fornices. Cervical canal; communicates with uterine cavity by internal os; with the vagina by external os § Normally >3 cm in length In young child: twice the length of the UT body, nulliparous=1/3 to ½ length of body Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 12
Cervix Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 13
Uterus § Hollow, pear-shaped organ § Divided into fundus, body, cervix § Usually anteflexed anteverted § Fundus is the widest and most superior portion § The Body or Corpus lies between the fundus and cervix and is the largest portion of the uterus. § Is suspended in place by the broad ligaments posteriorly, laterally and anteriorly Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 14
UTERUS § Fundus is the widest and most superior portion § The lateral borders are the “cornua” where the fallopian tubes enter § The body or “corpus” lies between the fundus and the cervix and is the largest portion Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 15
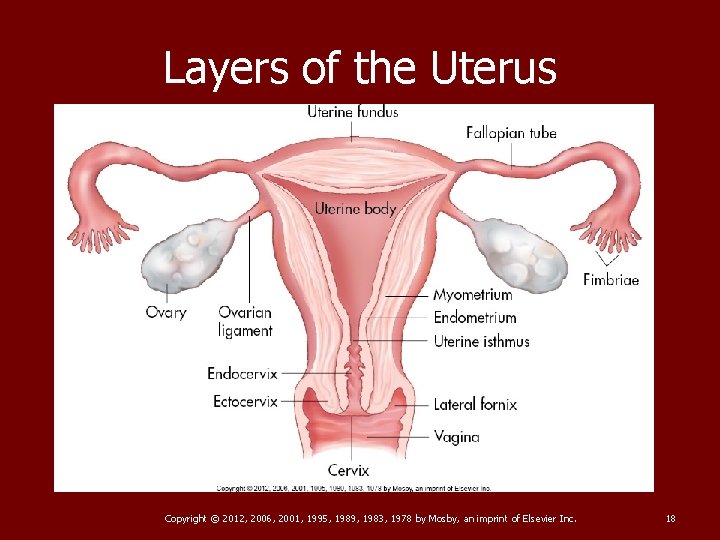
Layers of the Uterus § Perimetrium: Serous outer layer of uterus; (serosa) § Myometrium: Muscular middle layer, and the thickest layer § Endometrium: Inner mucous membrane § Both UT and vagina are derived from the embryonic mullerian ducts Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 16
Uterine Size VARIES IN SIZE DEPENDING ON AGE, PRIOR PREG § Premenarchal: 1 -3 cm long by. 5 -1. 0 cm wide § Menarchal: 6 -8 cm long by 3 -5 cm wide AP and TRV respectively § With multiparity: Increases size by 1 -2 cm § Postmenopausal: 3. 5 - 5. 5 cm long by 2 -3 cm wide Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 17
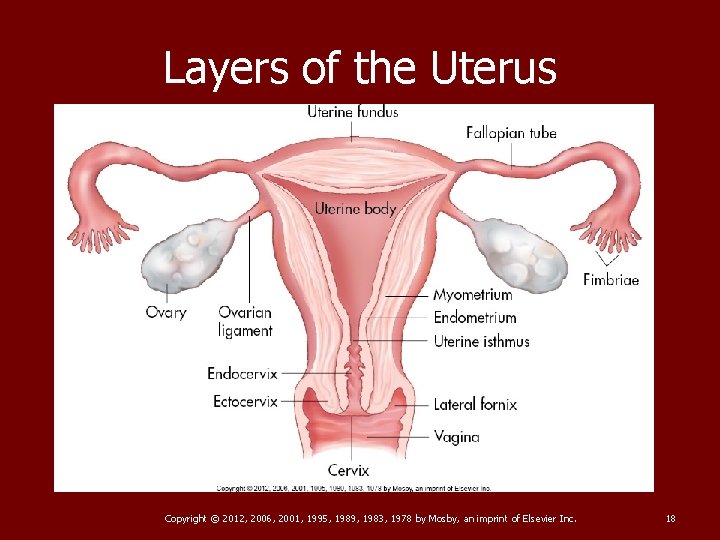
Layers of the Uterus Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 18
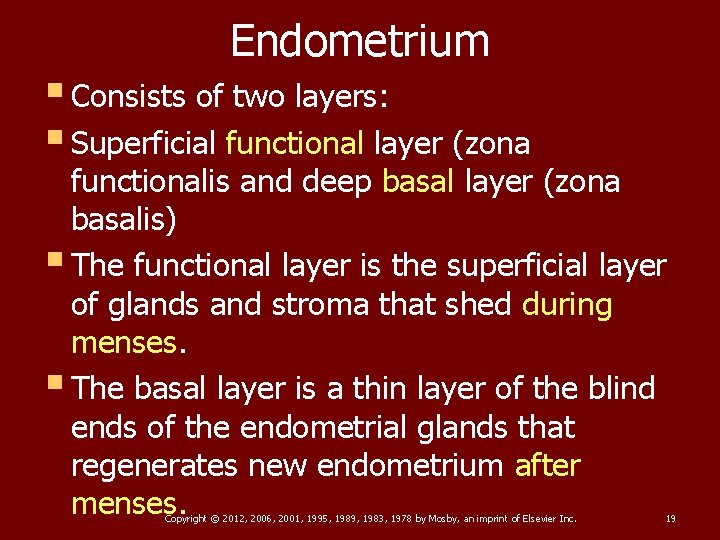
Endometrium § Consists of two layers: § Superficial functional layer (zona functionalis and deep basal layer (zona basalis) § The functional layer is the superficial layer of glands and stroma that shed during menses. § The basal layer is a thin layer of the blind ends of the endometrial glands that regenerates new endometrium after menses. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 19
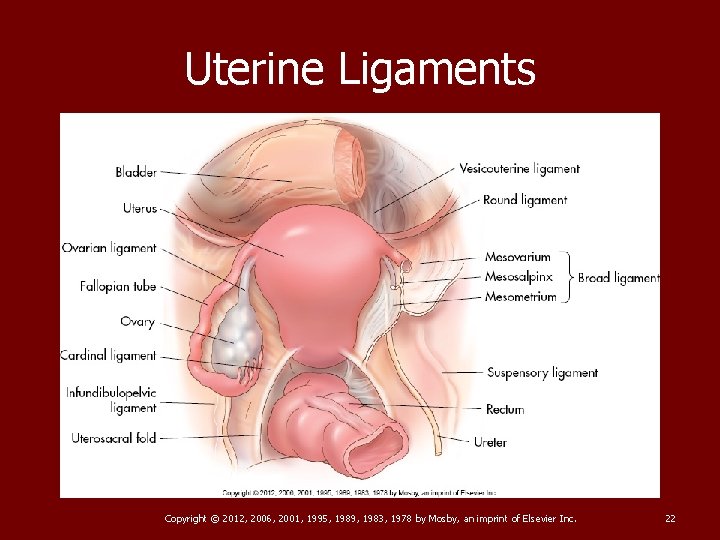
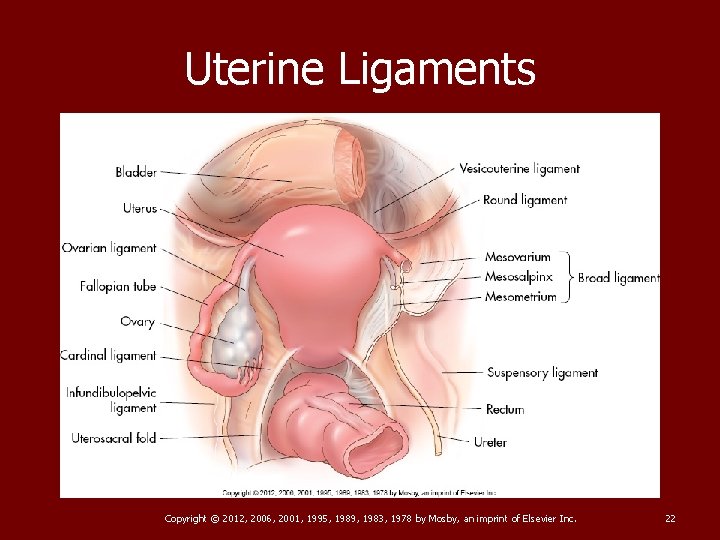
Uterine Ligaments § The uterus is supported in the midline position by paired broad ligaments, round ligaments, uterosacral ligaments and cardinal ligaments § Broad ligaments- drapes over the fallopian tubes, uterus and ovaries. Contains the uterine blood vessels and nerves. § Round ligaments- fibrous cords in front of and below the fallopian tubes. These two cords hold the uterine body in a forward positon Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 20
Uterine Ligaments The cervix is the only portion of the uterus that is firmly supported by the cardinal and uterosacral ligaments Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 21
Uterine Ligaments Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 22
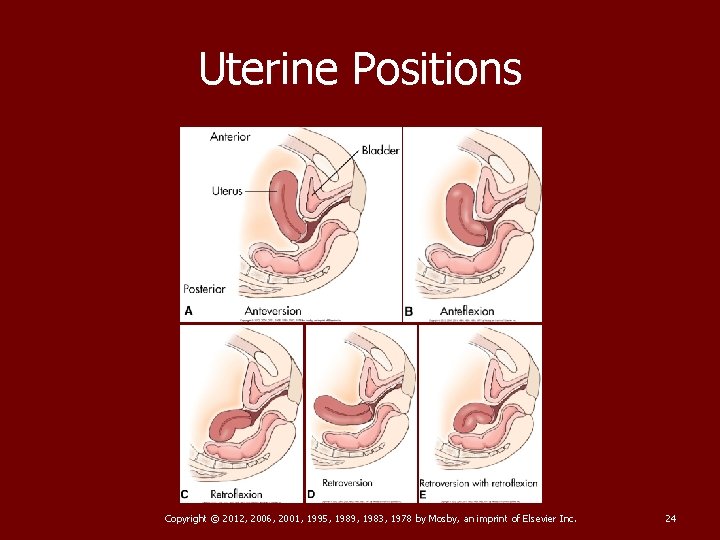
Uterine Positions § Anteversion: Most common position; cervical canal is 90 degree or less with vag canal. UT curved forward (anteriorly) upon the cervix § Anteflexion: UT body and fundus curved forward upon the cervix § Retroversion: Entire uterus tilted backward (posteriorly) § Retroflexion: UT body and fundus curve backward upon the cervix § Retroversion with retroflexion: Fundus and body bent backward(posteriorly) towards cervix Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 23
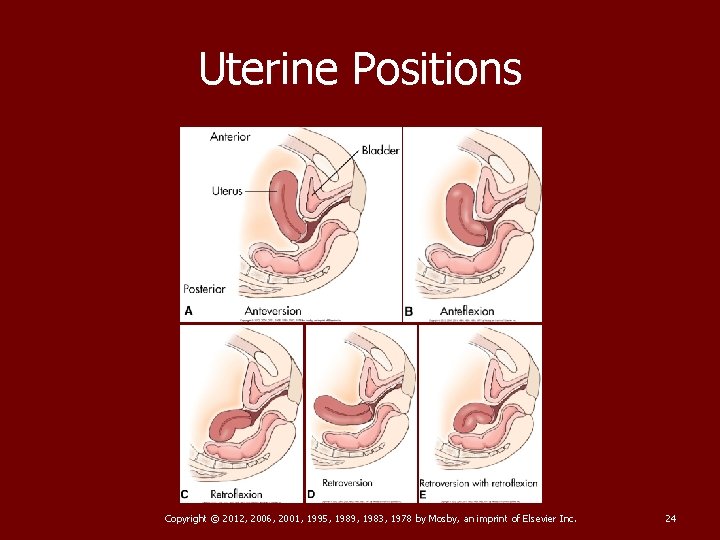
Uterine Positions Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 24
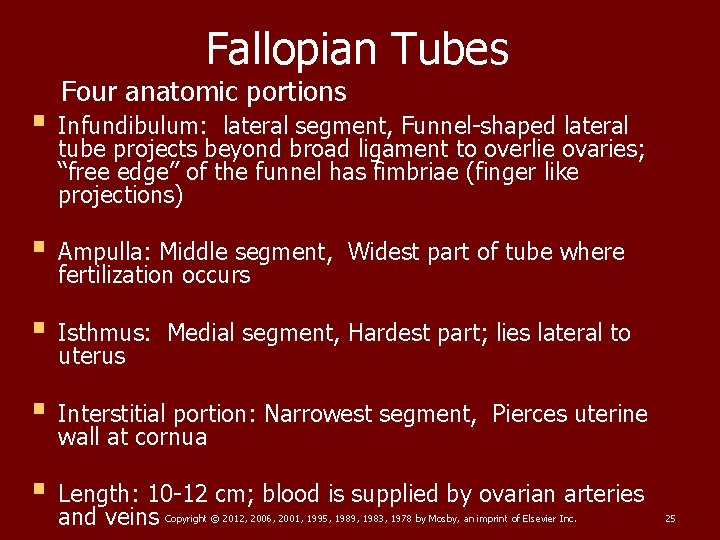
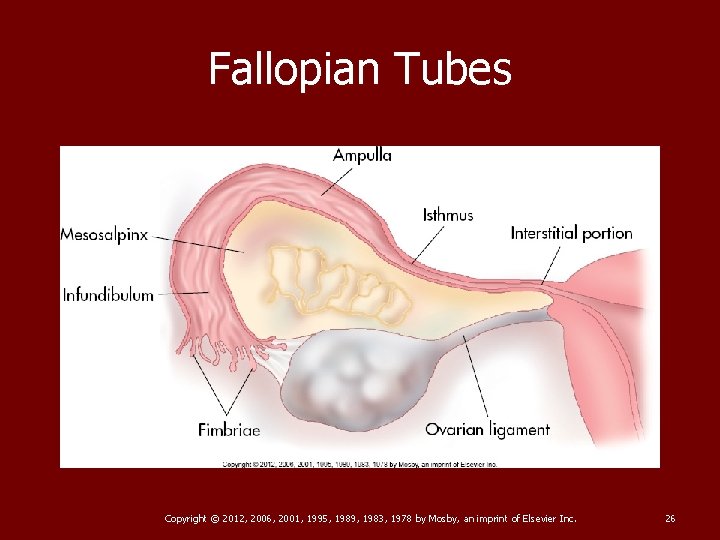
Fallopian Tubes Four anatomic portions § Infundibulum: lateral segment, Funnel-shaped lateral tube projects beyond broad ligament to overlie ovaries; “free edge” of the funnel has fimbriae (finger like projections) § Ampulla: Middle segment, fertilization occurs § Isthmus: uterus Widest part of tube where Medial segment, Hardest part; lies lateral to § Interstitial portion: Narrowest segment, wall at cornua Pierces uterine § Length: 10 -12 cm; blood is supplied by ovarian arteries and veins Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 25
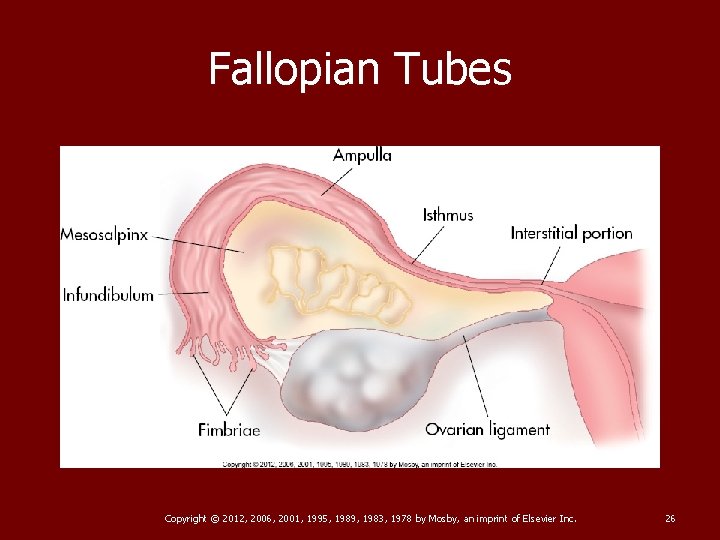
Fallopian Tubes Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 26
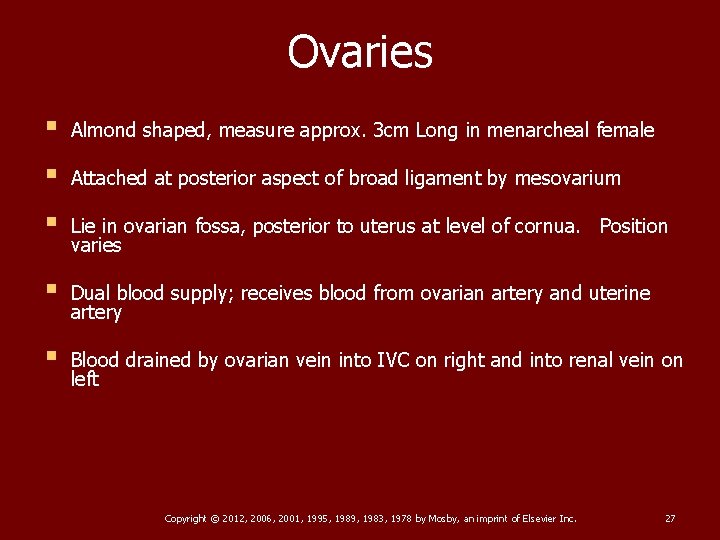
Ovaries § Almond shaped, measure approx. 3 cm Long in menarcheal female § Attached at posterior aspect of broad ligament by mesovarium § Lie in ovarian fossa, posterior to uterus at level of cornua. Position varies § Dual blood supply; receives blood from ovarian artery and uterine artery § Blood drained by ovarian vein into IVC on right and into renal vein on left Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 27
Ovaries NORMAL ANATOMY § Consist of outer cortex and inner medulla § Medulla contains the ov vasculature § Cortex consists primarily of follicles in varying stages of development § Ov are stimulated by follicle-stimulationg hormone (FSH). Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 28
Ovarian Ligaments § Ovaries supported medially by ovarian ligaments, originating bilaterally at cornua of uterus § Laterally by suspensory (infundibulopelvic) ligament, extending from infundibulum of fallopian tube and ovary to sidewall of pelvis § Ovary also attached to posterior aspect of broad ligament via mesovarium Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 29
Physiology THE MENSTRUAL CYCLE § Female’s reproductive years begin around 11 to 13 years of age at onset of menses (menstruation) § End around age 50, when menses ceases § Cycle approximately 28 days in length, beginning with first day of menstrual bleeding Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 30
The Menstrual Cycle § When cycle occurs at intervals of less than 21 days—called polymenorrheic § When cycle prolonged >35 days —called oligomenorrheic Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 31
Menstrual Status § Premenarche: Prepuberty § Menarche: Menstruating approximately every 28 days § Menopause: Cessation of menses Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 32
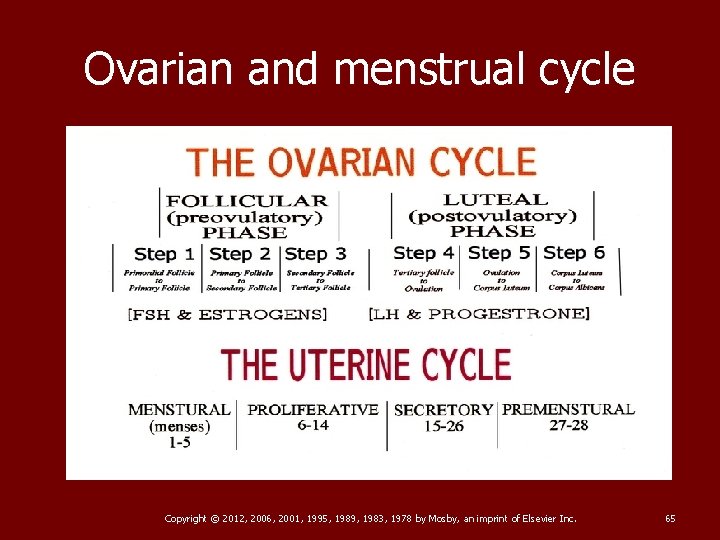
Follicular Development and Ovulation § Ovulation: During menarchal years, ovum released once a month by one of two ovaries § Ovulation normally occurs midcycle on about day 14 of 28 -day cycle § Speculated that ovum release alternates between the two ovaries; one month from right, next month from left Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 33
Follicular Development and Ovulation § All ova begin development during embryonic life. § Remain in suspended animation within preantral follicle as immature oocyte until onset of menarche § Each female ovary contains approximately 200, 000 oocytes at time of birth. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 34
Follicular Development and Ovulation § Process of ovulation regulated by hypothalamus within brain § At puberty, hypothalamus begins pulsatile release of gonadotropin-releasing hormones (Gn. RHs) § Gnr. Hs stimulate anterior pituitary gland to secrete varying levels of gonadotropins Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 35
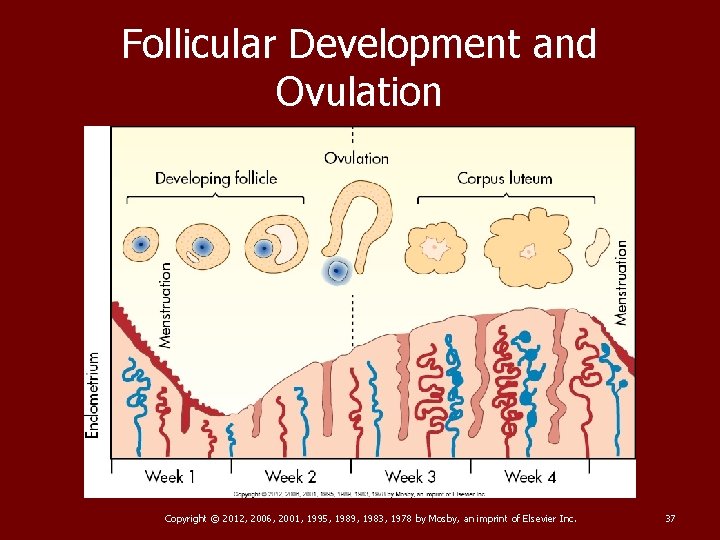
Follicular Development and Ovulation § Secretion of follicle-stimulating hormone (FSH) by anterior pituitary gland causes ovarian follicles to develop during first half of menstrual cycle. § Phase of ovulatory cycle, known as follicular phase, begins with first day of menstrual bleeding and continues until ovulation on day 14. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 36
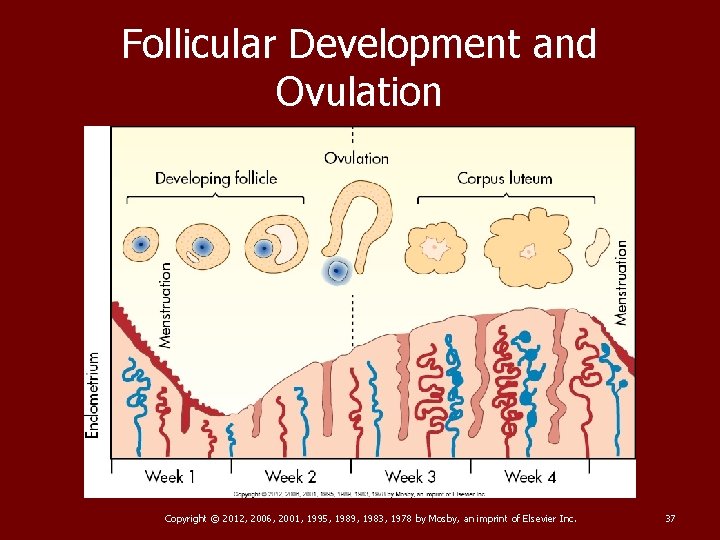
Follicular Development and Ovulation Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 37
Follicular Development and Ovulation § As ovarian follicles grow, they fill with fluid and secrete increasing amounts of estrogen. § Typically 5 -8 preantral follicles begin to develop; only one usually reaches maturity each month § Mature follicle known as graafian follicle; is typically 2 cm in size right before ovulation. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 38
Follicular Development and Ovulation § As estrogen level in blood rises with follicle development, pituitary gland is inhibited from further production of FSH and begins secreting luteinizing hormone (LH). § Luteinizing hormone level will typically increase rapidly 24 to 36 hours before ovulation in process known as LH surge. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 39
Follicular Development and Ovulation § Surge often used as predictor for timing ovulation for conception § LH level usually reaches peak 10 to 12 hours before ovulation § LH surge, accompanied by smaller FSH surge, triggers ovulation on about day 14. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 40
Follicular Development and Ovulation § Ovulation—explosive release of ovum from ruptured graafian follicle § Rupture of follicle associated with small amounts of fluid in posterior cul-de-sac midcycle § Midcycle dull ache on either side of lower abdomen lasting a few hours. Term “mittelschmerz, ” from German word meaning middle pain, often used to describe this sensation Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 41
Follicular Development and Ovulation § After ovulation, ovary enters luteal phase § Phase begins with ovulation and about 14 days in length § Menstruation almost always occurs 14 days after ovulation Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 42
Follicular Development and Ovulation § During luteal phase, cells in lining of ruptured ovarian follicle begin to multiply and create the corpus luteum, or yellow body. § Process is known as luteinization and is stimulated by LH surge. § Corpus luteum immediately begins secreting progesterone. § 9 -11 days after ovulation, corpus luteum degenerates, causing progesterone levels to decline. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 43
Follicular Development and Ovulation § As progesterone levels decline, menstruation occurs and cycle begins again. § Should conception and implantation occur, human chorionic gonadotropin (h. CG) produced by zygote causes corpus luteum to persist; it will continue to secrete progesterone for 3 more months until placenta takes over. § If conception does not occur the corpus luteum becomes the corpus albicans. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 44
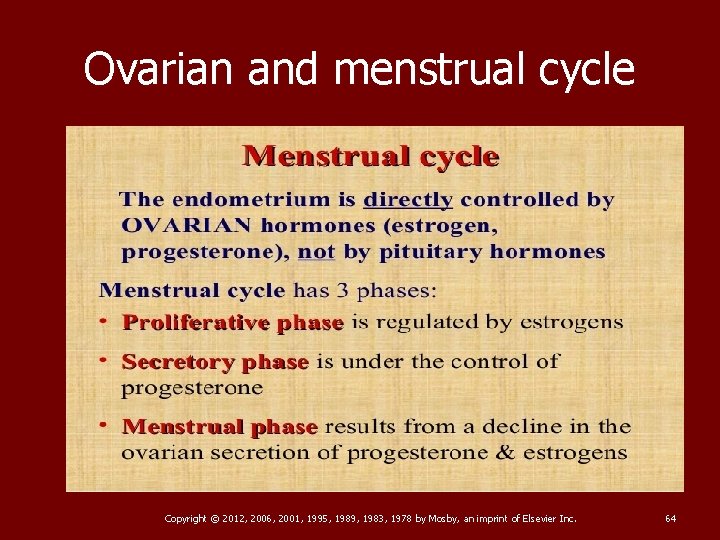
Endometrial Changes § Varying levels of estrogen and progesterone throughout course of menstrual cycle induce characteristic changes in endometrium. § Changes correlate with ovulatory cycles of ovary. § Typical endometrial cycle identified and described in three phases, beginning with menstrual phase. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 45
Endometrial Changes § Menstrual phase lasts approximately 1 to 5 days and begins with declining progesterone levels, causing spiral arterioles to constrict. § Causes decreased blood flow to endometrium, resulting in ischemia and shedding of zona functionalis § First 5 days coincide with follicular phase of ovarian cycle Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 46
Endometrial Changes § As follicles produce estrogen, estrogen stimulates superficial layer of endometrium to regenerate and grow. § Phase of endometrial regeneration is called the proliferative phase and will last until luteinization of a graafian follicle around ovulation Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 47
Endometrial Changes § With ovulation and luteinization of graafian follicle, progesterone secreted by ovary causes spiral arteries and endometrial glands to enlarge. § Prepares endometrium for implantation, should conception occur Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 48
Endometrial Changes § Endometrial phase after ovulation is referred to as the secretory phase. § Extends from approximately day 15 to onset of menses (day 28) § Secretory phase of endometrial cycle corresponds to luteal phase of ovarian cycle. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 49
The Menstrual Cycle PROLIFERATIVE PHASE § Days 1 -14 § Corresponds to follicular phase of ovarian cycle § Menstruation occurs on days 1 to 4 § Thin endometrium § Estrogen level increases as ovarian follicles develop § Increasing estrogen levels cause uterine lining to regenerate and thicken § Ovulation occurs on day 14 Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 50
The Menstrual Cycle SECRETORY PHASE § Days 15 -28 § Corresponds to luteal phase of ovarian cycle § Ruptured follicle becomes corpus luteum § Corpus luteum secretes progesterone § Endometrium thickens § If no pregnancy, estrogen and progesterone decrease § Menses on day 28 Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 51
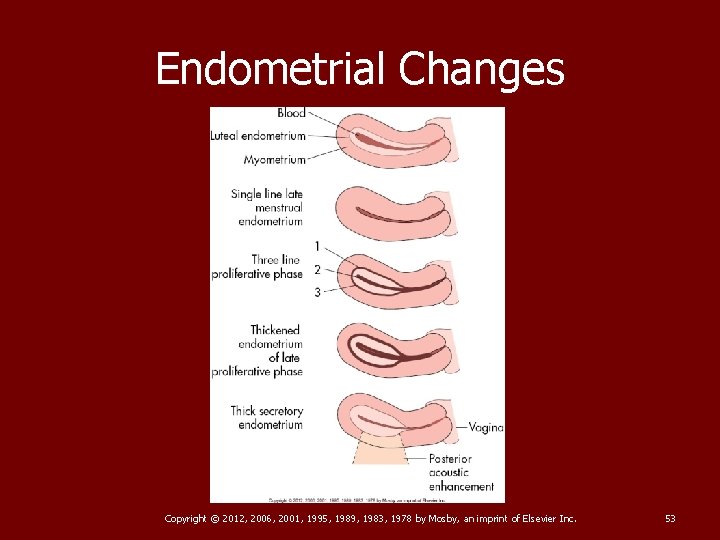
Endometrial Changes § Sonographic appearance of endometrium changes dramatically among the three phases of endometrial cycle. § Should be correlated to patient’s menstrual status Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 52
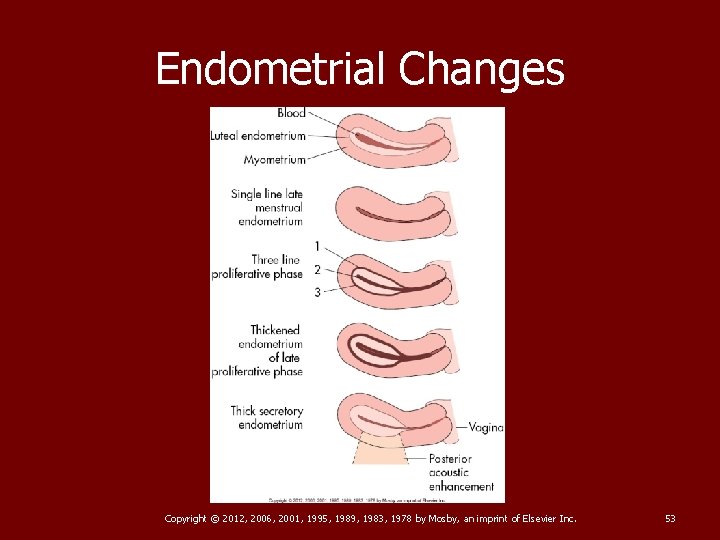
Endometrial Changes Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 53
Endometrial Changes § During menses, not uncommon to see varying levels of fluid and debris within uterine cavity § Thickness of endometrium will decrease with menstruation, becoming thin echogenic line during early proliferative phase Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 54
Endometrial Changes § As regeneration of endometrium occurs during proliferative phase, endometrium will thicken to an average of 4 -8 mm in proliferative phase, when measured as double layer from anterior to posterior. § Endometrium characteristically appears hypoechoic with appearance of “three-line” sign. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 55
Endometrial Changes § Three echogenic lines seen in proliferative endometrium represent zona basalis anteriorly and posteriorly, with central line representing uterine cavity § Right before ovulation, endometrium measures 6 -10 mm and becomes isoechoic with myometrium. Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 56
Endometrial Changes § After ovulation, during secretory phase, endometrium reaches thickest dimension, averaging 7 -14 mm § Becomes echogenic, blurring “three-line” appearance Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 57
Endometrial Changes § Postmenopausal patients who are not on HRT should have endometrial thickness of <5 mm § Postmenopausal patients on HRT or taking tamoxifen may demonstrate normal endometrial thicknesses up to 8 mm Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 58
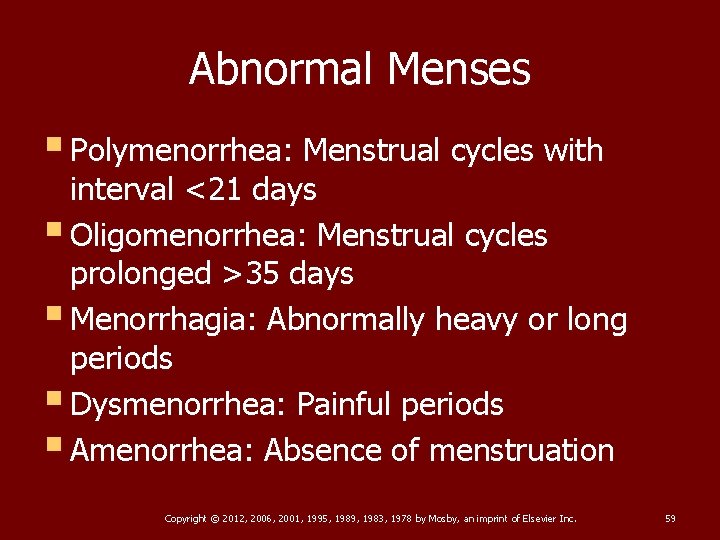
Abnormal Menses § Polymenorrhea: Menstrual cycles with interval <21 days § Oligomenorrhea: Menstrual cycles prolonged >35 days § Menorrhagia: Abnormally heavy or long periods § Dysmenorrhea: Painful periods § Amenorrhea: Absence of menstruation Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 59
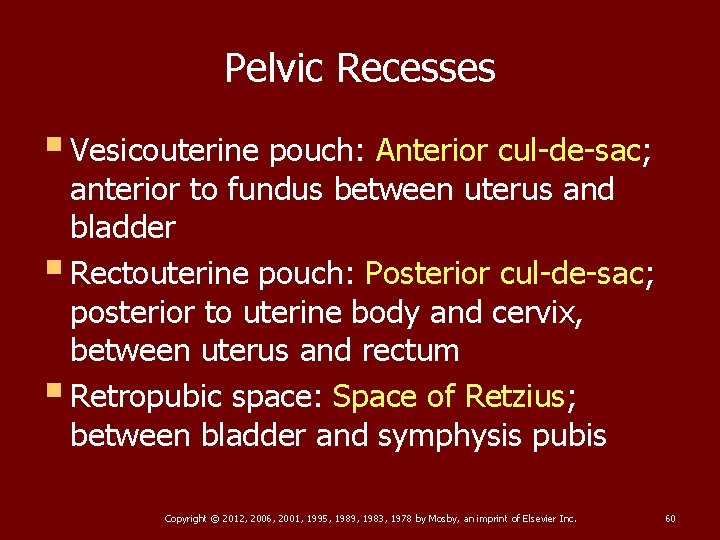
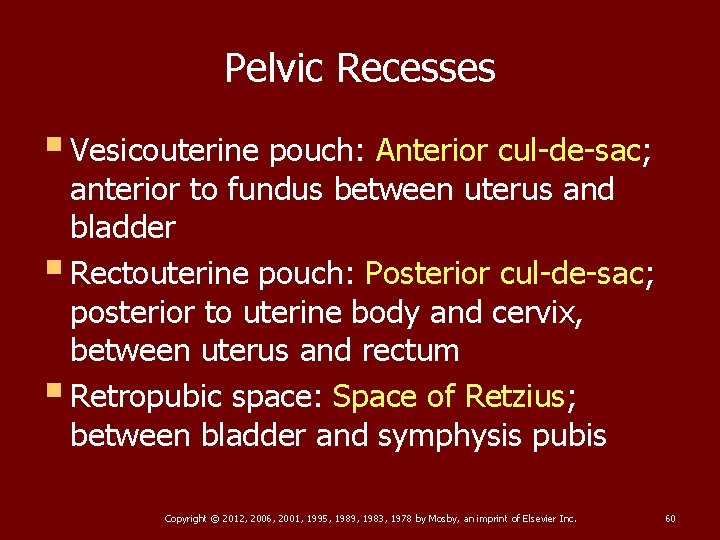
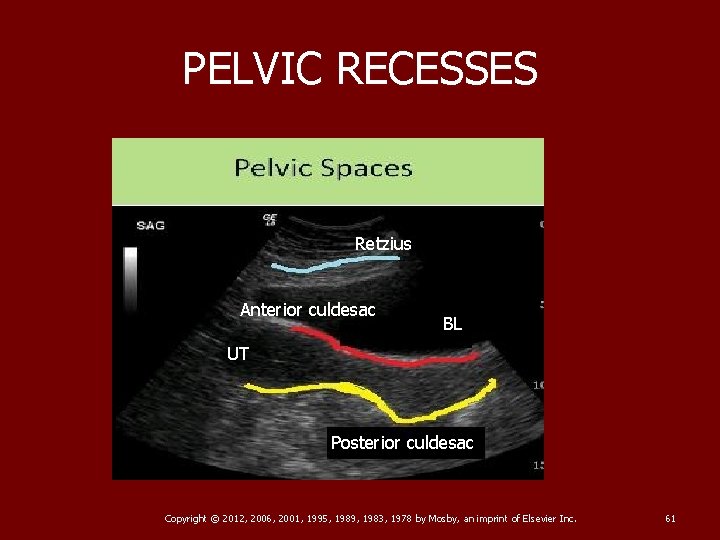
Pelvic Recesses § Vesicouterine pouch: Anterior cul-de-sac; anterior to fundus between uterus and bladder § Rectouterine pouch: Posterior cul-de-sac; posterior to uterine body and cervix, between uterus and rectum § Retropubic space: Space of Retzius; between bladder and symphysis pubis Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 60
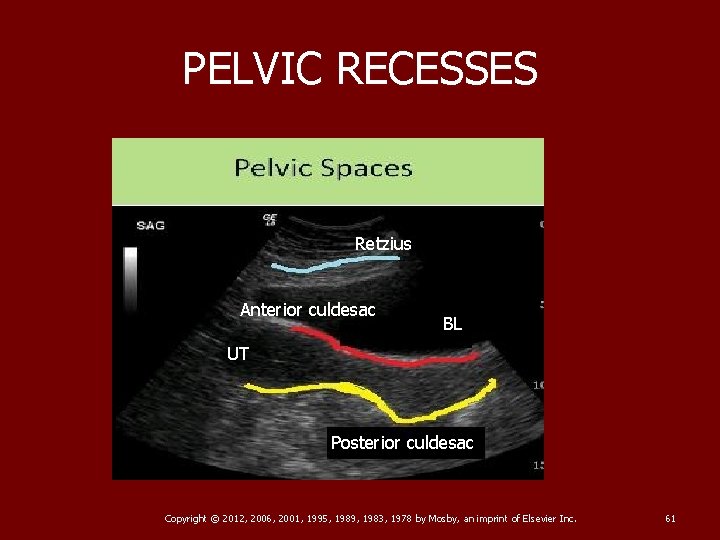
PELVIC RECESSES Retzius Anterior culdesac BL UT Posterior culdesac Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 61
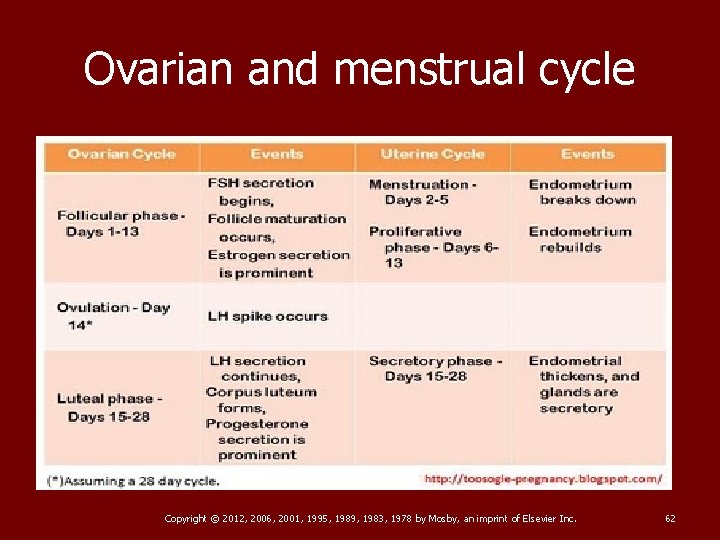
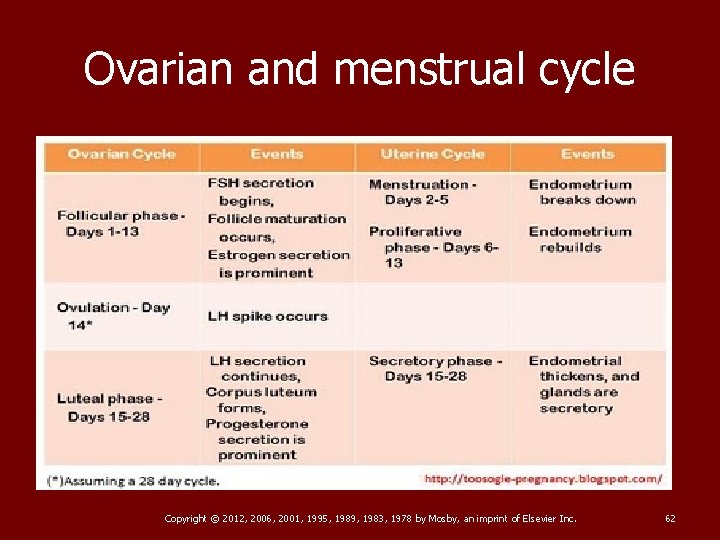
Ovarian and menstrual cycle Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 62
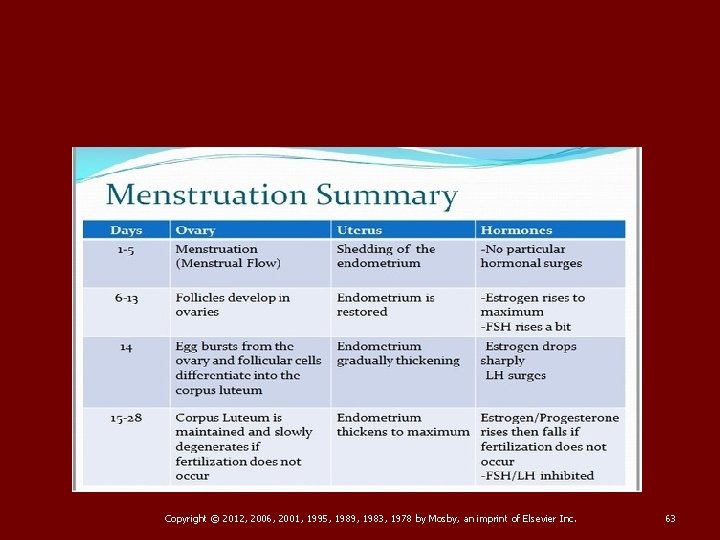
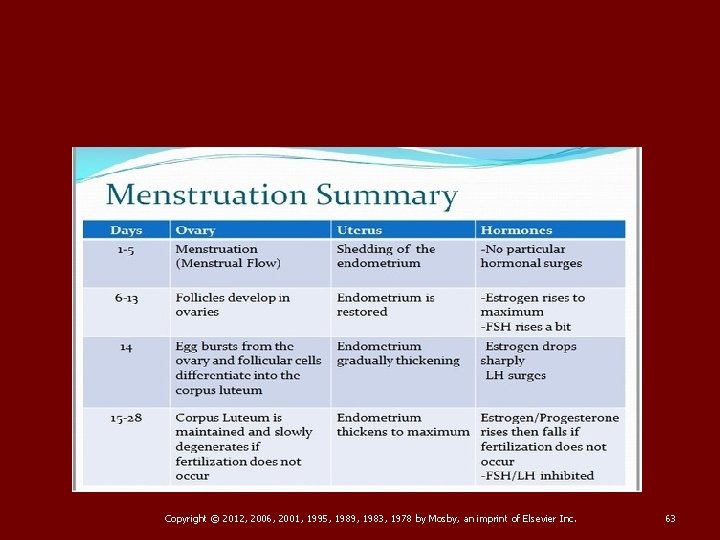
Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 63
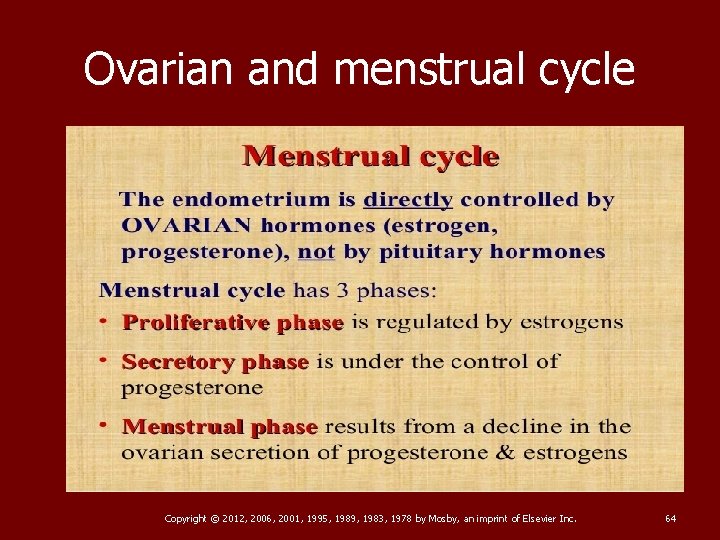
Ovarian and menstrual cycle Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 64
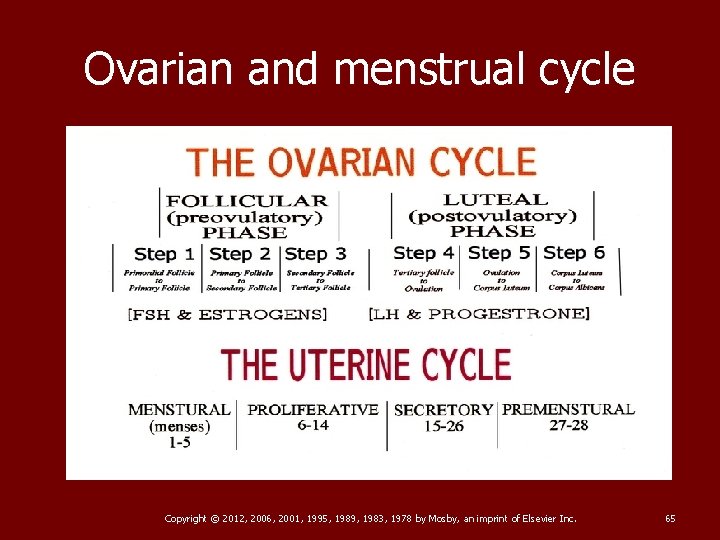
Ovarian and menstrual cycle Copyright © 2012, 2006, 2001, 1995, 1989, 1983, 1978 by Mosby, an imprint of Elsevier Inc. 65