Nordic Casemix Conference 2010 Helsinki Future demands for









- Slides: 38

Nordic Casemix Conference 2010, Helsinki Future demands for DRG systems – considerations based on the Euro. DRG project Reinhard Busse, Prof. Dr. med. MPH FFPH Department of Health Care Management, Technical University Berlin (WHO Collaborating Centre for Health Systems Research and Management) & European Observatory on Health Systems and Policies 4 June 2010 Future demands for DRG systems- the Euro. DRG project 1
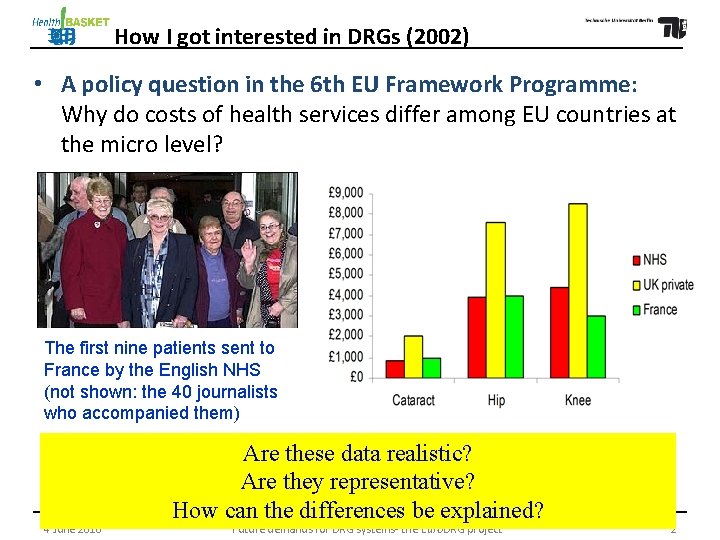
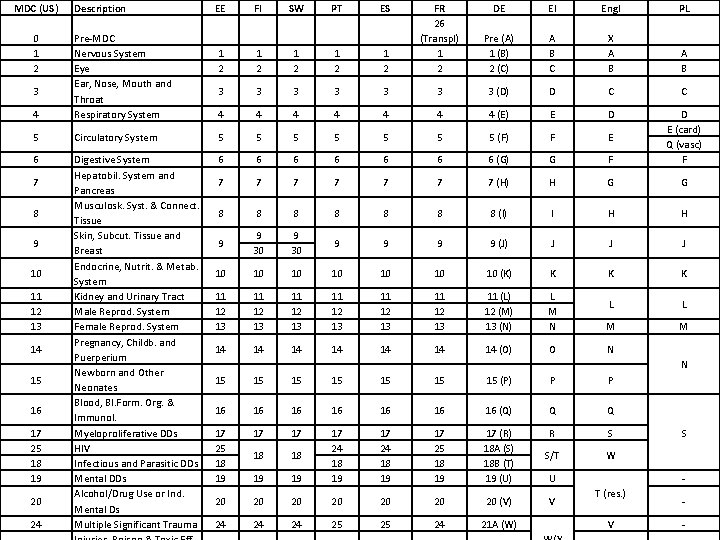
How I got interested in DRGs (2002) • A policy question in the 6 th EU Framework Programme: Why do costs of health services differ among EU countries at the micro level? The first nine patients sent to France by the English NHS (not shown: the 40 journalists who accompanied them) 4 June 2010 Are these data realistic? Are they representative? How can the differences be explained? Future demands for DRG systems- the Euro. DRG project 2
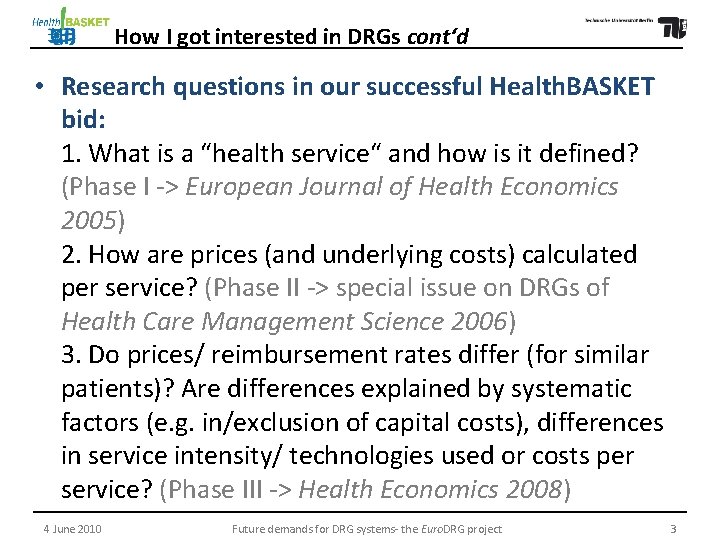
How I got interested in DRGs cont‘d • Research questions in our successful Health. BASKET bid: 1. What is a “health service“ and how is it defined? (Phase I -> European Journal of Health Economics 2005) 2. How are prices (and underlying costs) calculated per service? (Phase II -> special issue on DRGs of Health Care Management Science 2006) 3. Do prices/ reimbursement rates differ (for similar patients)? Are differences explained by systematic factors (e. g. in/exclusion of capital costs), differences in service intensity/ technologies used or costs per service? (Phase III -> Health Economics 2008) 4 June 2010 Future demands for DRG systems- the Euro. DRG project 3

Countries in Health. BASKET project
Phase I results (2005) • clear trend towards a more explicit definition of benefit baskets and benefit catalogues in European health care systems (e. g. to assure equity among the regions) • Taxonomy differs largely from country to country – even if most tend to sort ambulatory care by physician specialty and inpatient care by diagnosis and procedure (DRGs/ HRGs/ DBCs …) Conclusion: a uniform taxonomy (“European Classification of Health Services“) to explore and describe differences (not to standardise the baskets!) is urgently needed for both practical and scientific purposes 4 June 2010 Future demands for DRG systems- the Euro. DRG project 5

Phase II results (2006) • Most countries have installed activity-based remuneration schemes for in- and outpatient services; often lacking for long-term care, rehabilitation etc. • clear trend towards the use of micro-costing data (especially for inpatient services -> DRGs) to determine remuneration rates, reflecting actual costs of providers • Problems: - insufficient quality of data delivered by providers - recommendations in methodological guidelines vary 4 June 2010 Future demands for DRG systems- the Euro. DRG project 6
DRG systems – one family, but often distant cousins 4 June 2010 Future demands for DRG systems- the Euro. DRG project 7
Import of DRG systems is common – a model to analyse adopted and modified elements
Phase II results cont‘d • Prerequisites of international cost comparison: mutually accepted methodological guidance (standard costing method) and reasonably good compliance with it. • Harmonisation of methodologies not sufficient to ensure meaningful comparability; accounting systems should be coordinated and standardised --> serious dilemma: standardised “European” accounting methodology right down to provider level might be well-justified and “necessary” but enforcing one methodology conflicts with the principle of subsidiarity. we used a self-developed standardised method 4 June 2010 Future demands for DRG systems- the Euro. DRG project 9
Phase III Objectives • Do costs (and prices/ reimbursement rates) really differ? If yes, by how much? • Why? - Systematic differences in calculation (e. g. capital costs included/ not included)? - Differences in technologies used or service intensity (e. g. time spent with patient)? - Costs per resource unit (e. g. wage differences)? 4 June 2010 Future demands for DRG systems- the Euro. DRG project 10
Phase III Methodology • 10 case vignettes (“service packages”) were designed around episodes of care 4 June 2010 Future demands for DRG systems- the Euro. DRG project 11
Phase III Methodology cont‘d • To ensure homogeneity within case vignettes (i. e. to avoid risk adjustment), health status and indication of each patient was defined in detail for each vignette • To ensure comparability across vignettes, each was divided into detailed path components e. g. diagnostic procedures, care before operation etc. • Partners in each country documented technology use, service intensity and costs (prices) for case vignettes with data from at least 5 representative providers Costs (and prices) compared and differences analysed 4 June 2010 Future demands for DRG systems- the Euro. DRG project 12
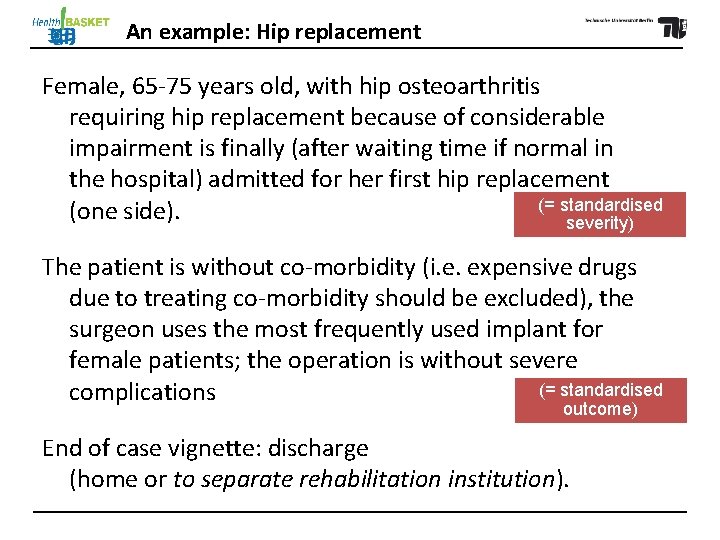
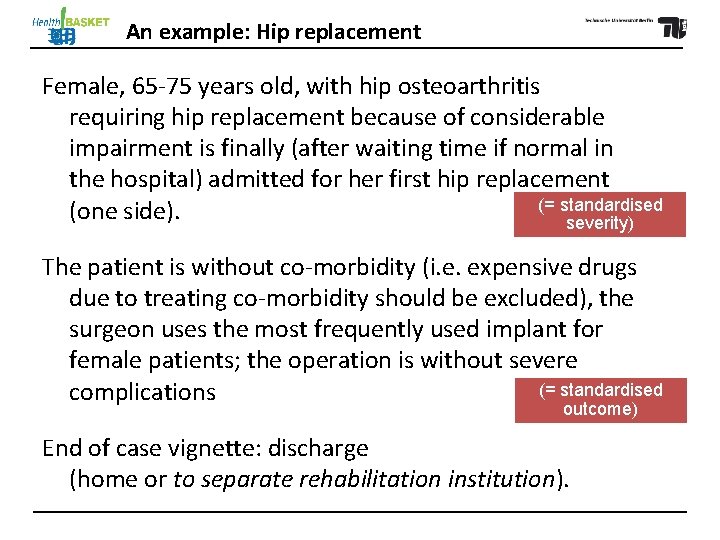
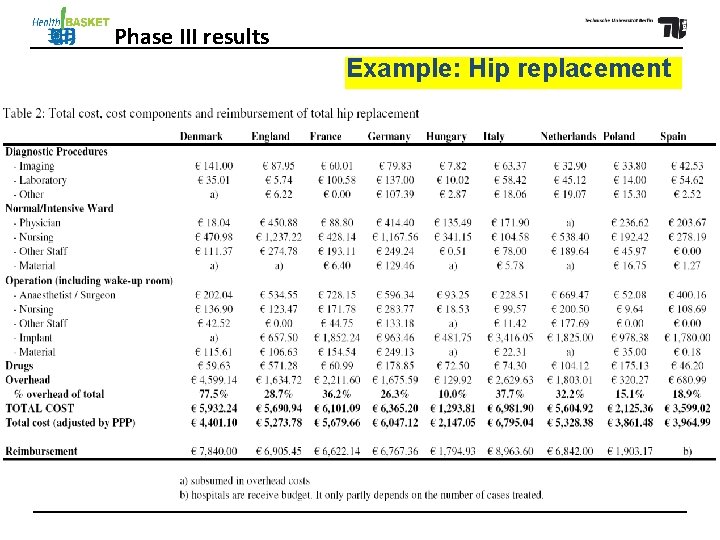
An example: Hip replacement Female, 65 -75 years old, with hip osteoarthritis requiring hip replacement because of considerable impairment is finally (after waiting time if normal in the hospital) admitted for her first hip replacement (= standardised (one side). severity) The patient is without co-morbidity (i. e. expensive drugs due to treating co-morbidity should be excluded), the surgeon uses the most frequently used implant for female patients; the operation is without severe (= standardised complications outcome) End of case vignette: discharge (home or to separate rehabilitation institution).
Example: Hip replacement
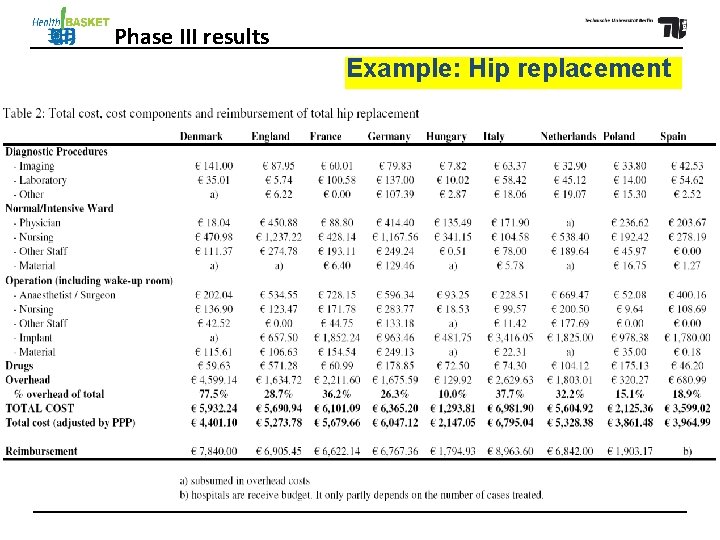
Phase III results Example: Hip replacement
Phase III results Example: Hip replacement “Profit“-making plausible through comparatively low case complexity 4 June 2010 Future demands for DRG systems- the Euro. DRG project 16
Phase III results Example: Hip replacement “Profit“-making plausible through 1: comparatively low case complexityso much Open question If costs differ within countries, why do countries develop their own DRG systems (rather than a European one)? What data would be necessary for this? 4 June 2010 Future demands for DRG systems- the Euro. DRG project 17
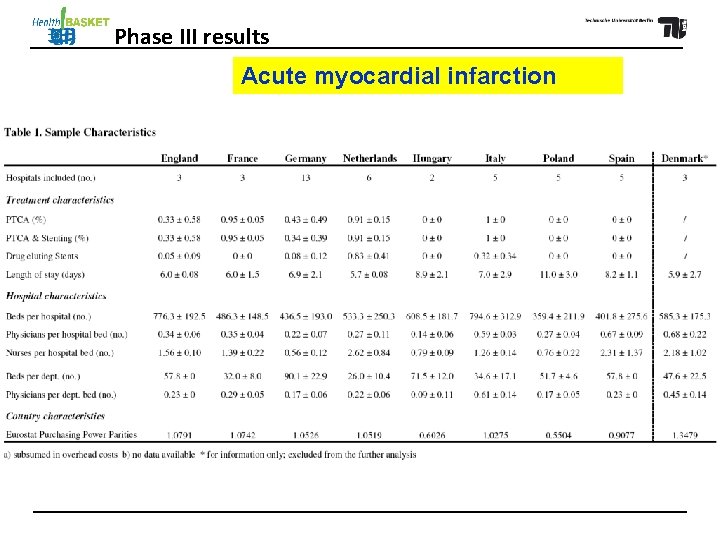
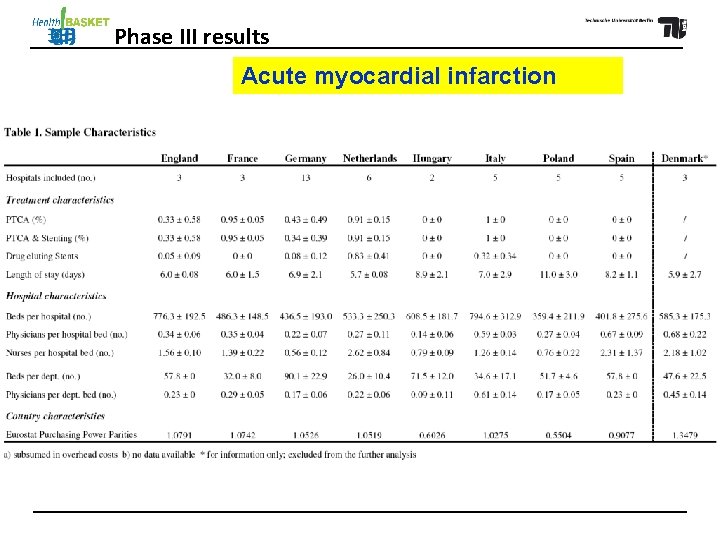
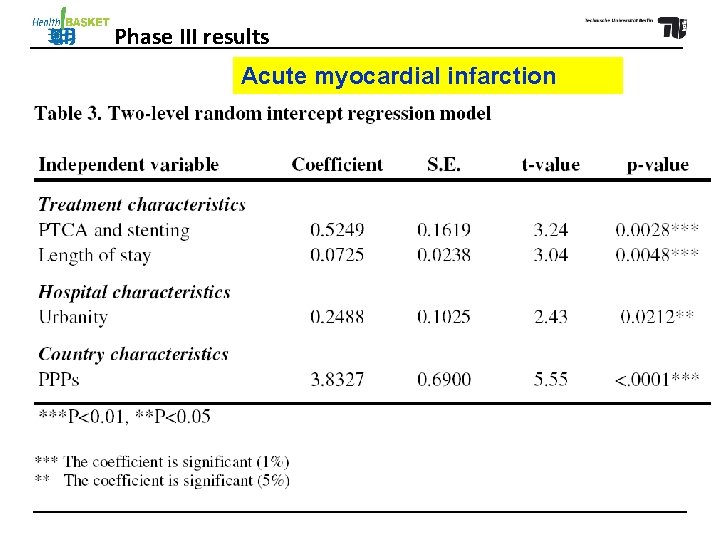
Phase III results Acute myocardial infarction
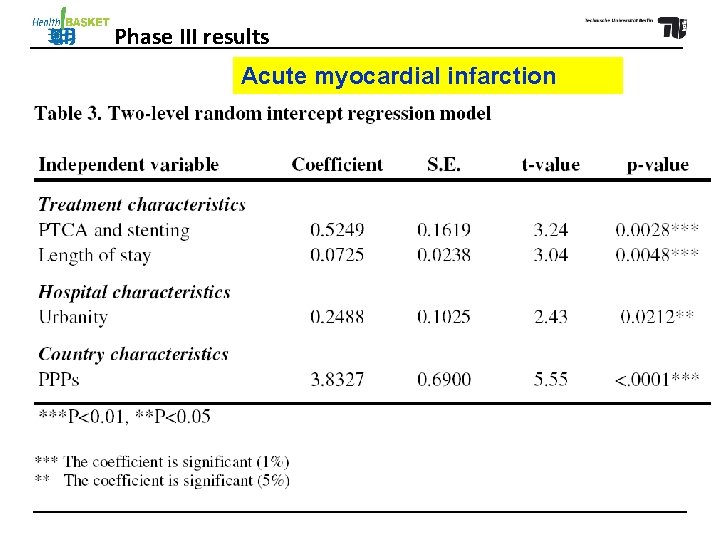
Phase III results Acute myocardial infarction

Phase III results Acute myocardial infarction: Hospitals performing PCI (PTCA/ Stenting) none mixed all > factor 4: value for money? 4 June 2010 Future demands for DRG systems- the Euro. DRG project 20

Phase III results Acute myocardial infarction: infarction Hospitals performing PCI (PTCA/ Stenting) none mixed all Open question 2: If costs differ so much with treatment, what about the quality of care? -> Euro. DRG 4 June 2010 Future demands for DRG systems- the Euro. DRG project 21

Phase III analyses show that … • use of technology is a major explanation for certain vignettes (hip replacement, acute myocardial infarction, appendectomy …) • skills mix and usage intensity make a difference (normal delivery …) • length of stay plays a role (especially if shortened by early discharge to rehabilitation; e. g. stroke) • costs per resource unit (especially for personnel) do differ – as much or more than technology usage -> for efficiency comparisons, adjustment of input costs necessary 4 June 2010 Future demands for DRG systems- the Euro. DRG project 22
The scientific numbers in detail …
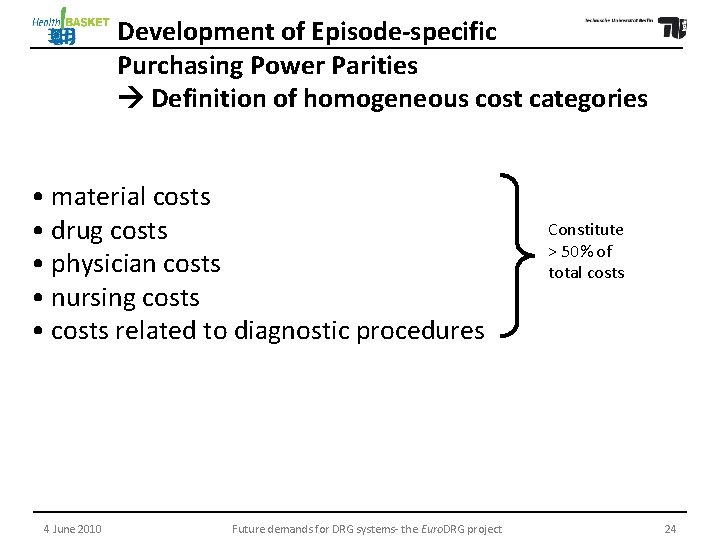
Development of Episode-specific Purchasing Power Parities Definition of homogeneous cost categories • material costs • drug costs • physician costs • nursing costs • costs related to diagnostic procedures 4 June 2010 Future demands for DRG systems- the Euro. DRG project Constitute > 50% of total costs 24
Average adjusted costs per case by country and care episode
Open question 3: Does this adjustment hold with better data? Euro-DRG: (1) routine cost and activity data for broader patient categories and Average (2) hospital benchmarking club. adjusted costs perhas more emphasis to be put on If yes, case by exogeneous factors (such as wages) country when and careusing DRGs for reimbursement? episode Could this lead to a European system with differing base rates (as in US)?
25 May 2010 Hospital Financing in Germany: The G-DRG System 27

(funded under the 7 th EU Research Framework Programme 2009 -2011) … taking up the open questions, based on the observation that costs differ due to three groups of factors: (1) Patient characteristics, i. e. main diagnosis, age, sex, secondary diagnoses (upon admission) (2) Medical/ treatment variables, i. e. procedures/ technologies used, type of ward (e. g. intensive care), intensity of inputs (e. g. personnel), length of stay, secondary diagnoses (-> complications) between (2) and (3): activity levels (3) Exogenous factors - at hospital level: size (beds, personnel), emergency room, teaching status - at regional/national level: wage level, costs of other inputs 4 June 2010 Future demands for DRG systems- the Euro. DRG project 28

Suomi Finland Countries in (Health. BASKET and) Euro. DRG projects
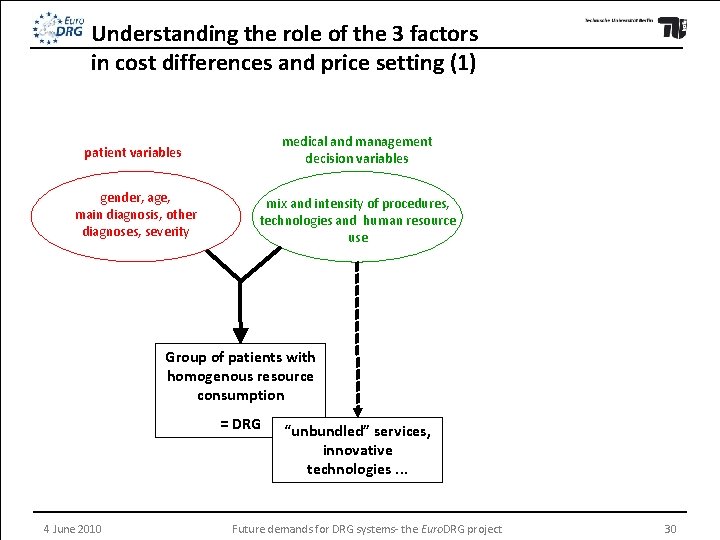
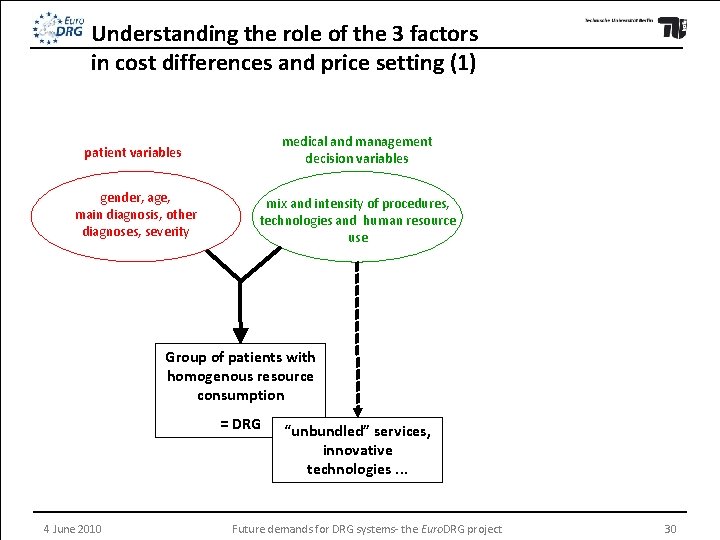
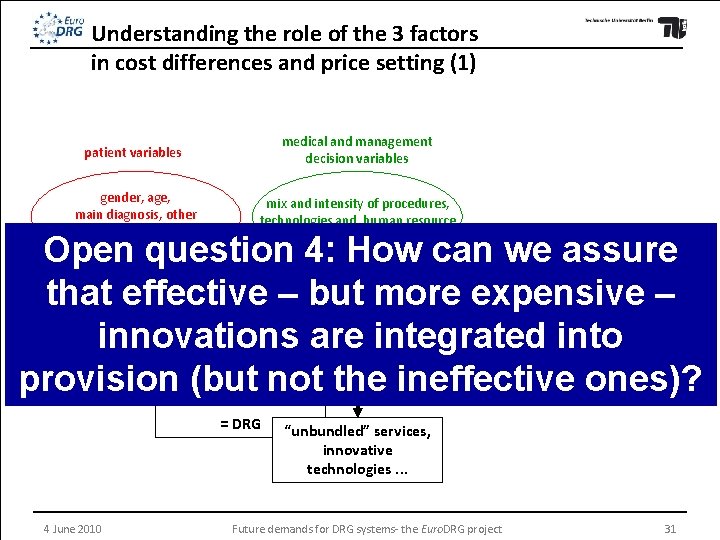
Understanding the role of the 3 factors in cost differences and price setting (1) patient variables medical and management decision variables gender, age, main diagnosis, other diagnoses, severity mix and intensity of procedures, technologies and human resource use Group of patients with homogenous resource consumption = DRG 4 June 2010 “unbundled” services, innovative technologies. . . Future demands for DRG systems- the Euro. DRG project 30
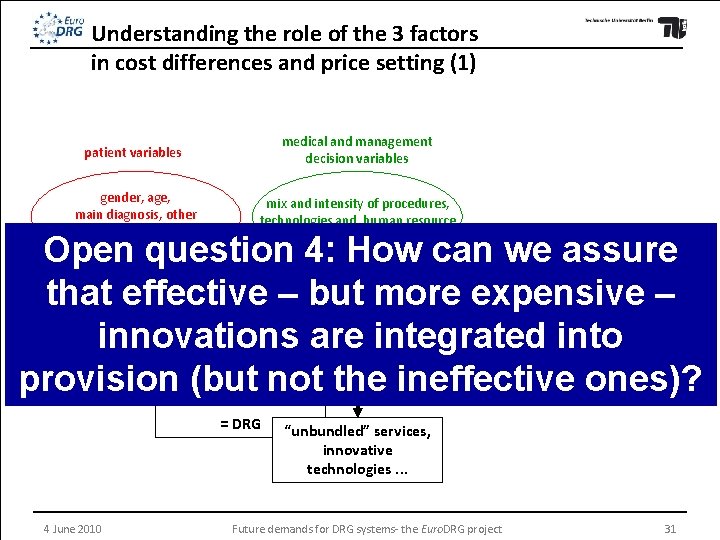
Understanding the role of the 3 factors in cost differences and price setting (1) patient variables medical and management decision variables gender, age, main diagnosis, other diagnoses, severity mix and intensity of procedures, technologies and human resource use Open question 4: How can we assure that effective – but more expensive – innovations are integrated into Group of patients with resource provisionhomogenous (but not the ineffective ones)? consumption = DRG 4 June 2010 “unbundled” services, innovative technologies. . . Future demands for DRG systems- the Euro. DRG project 31
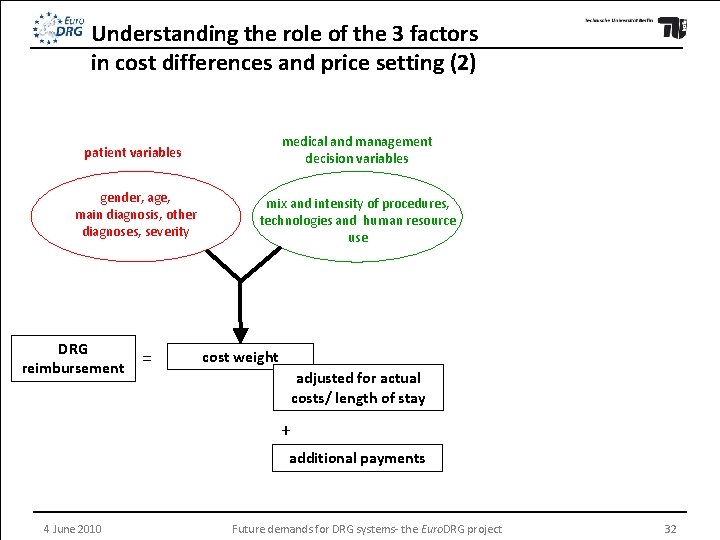
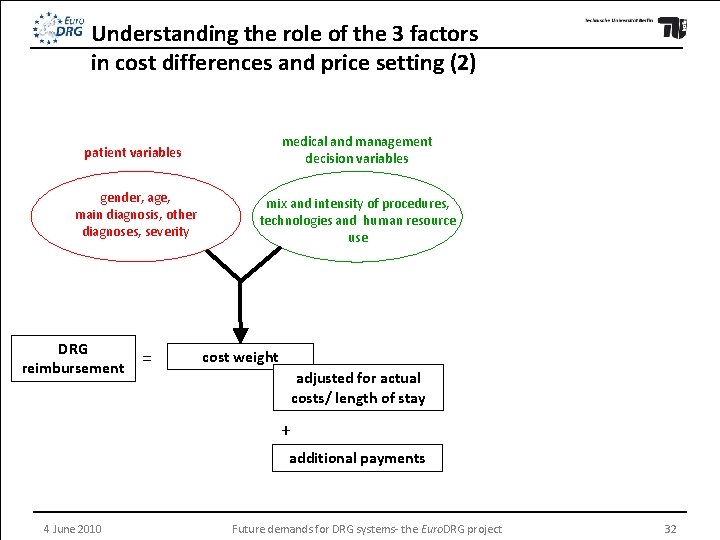
Understanding the role of the 3 factors in cost differences and price setting (2) patient variables medical and management decision variables gender, age, main diagnosis, other diagnoses, severity mix and intensity of procedures, technologies and human resource use DRG reimbursement = cost weight adjusted for actual costs/ length of stay + additional payments 4 June 2010 Future demands for DRG systems- the Euro. DRG project 32
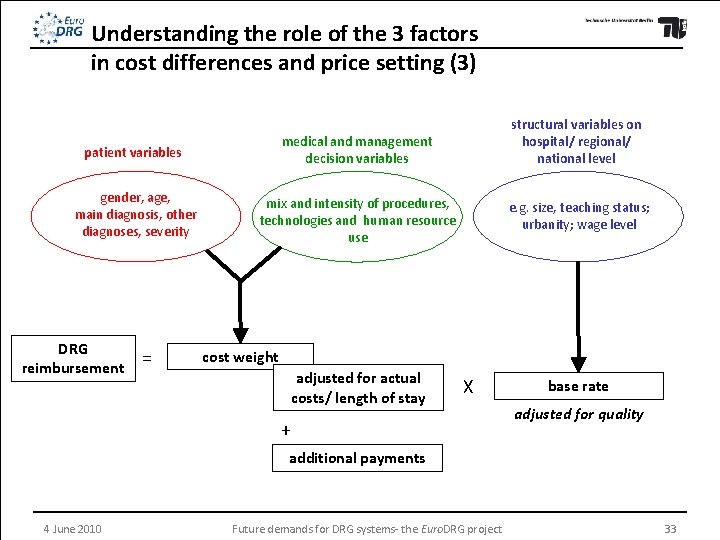
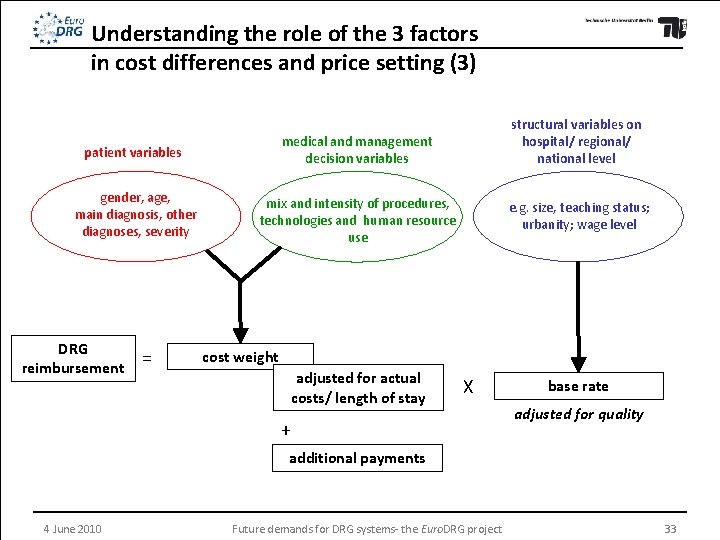
Understanding the role of the 3 factors in cost differences and price setting (3) patient variables medical and management decision variables gender, age, main diagnosis, other diagnoses, severity mix and intensity of procedures, technologies and human resource use DRG reimbursement = structural variables on hospital/ regional/ national level e. g. size, teaching status; urbanity; wage level cost weight adjusted for actual costs/ length of stay X + base rate adjusted for quality additional payments 4 June 2010 Future demands for DRG systems- the Euro. DRG project 33
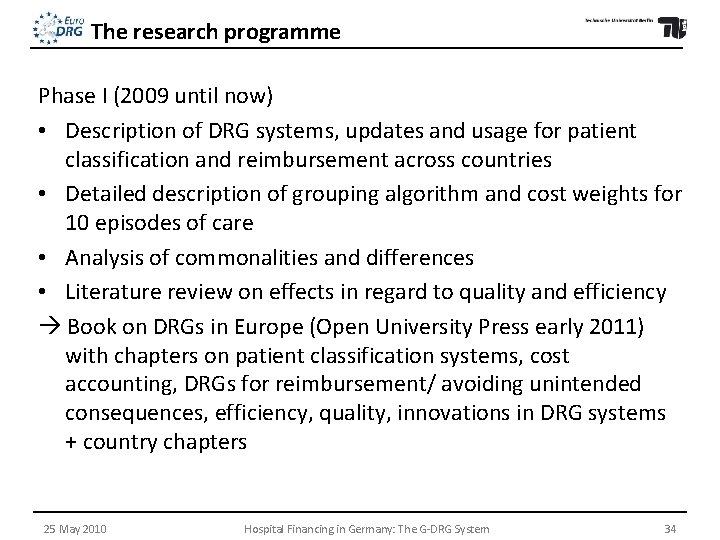
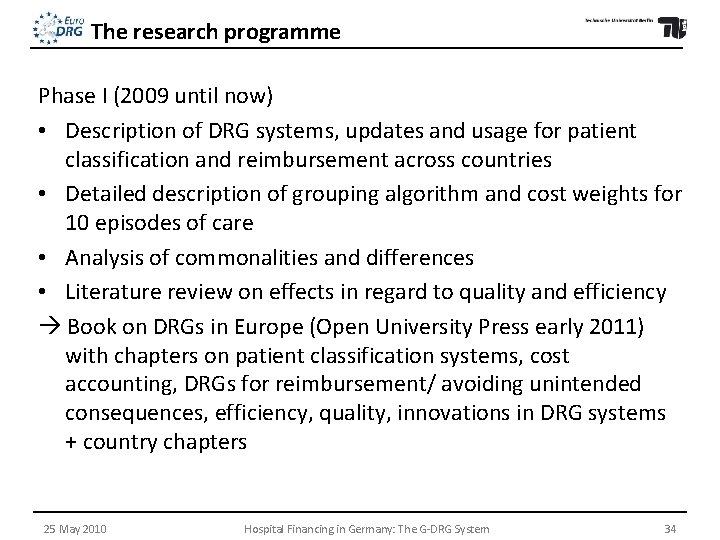
The research programme Phase I (2009 until now) • Description of DRG systems, updates and usage for patient classification and reimbursement across countries • Detailed description of grouping algorithm and cost weights for 10 episodes of care • Analysis of commonalities and differences • Literature review on effects in regard to quality and efficiency Book on DRGs in Europe (Open University Press early 2011) with chapters on patient classification systems, cost accounting, DRGs for reimbursement/ avoiding unintended consequences, efficiency, quality, innovations in DRG systems + country chapters 25 May 2010 Hospital Financing in Germany: The G-DRG System 34

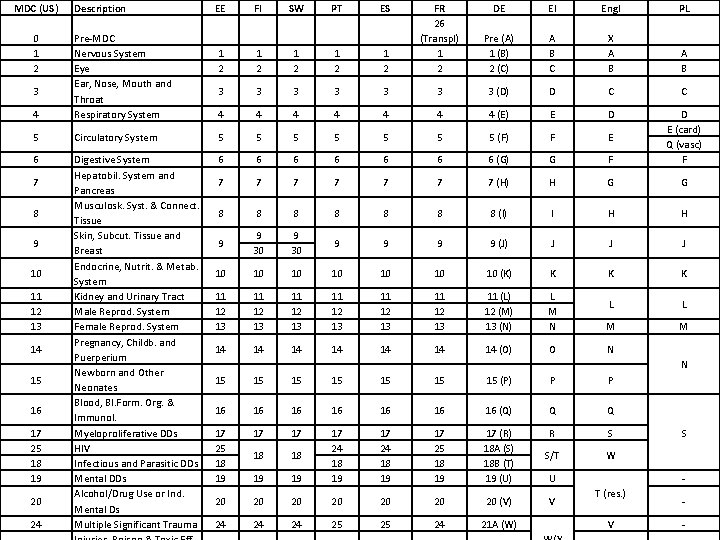
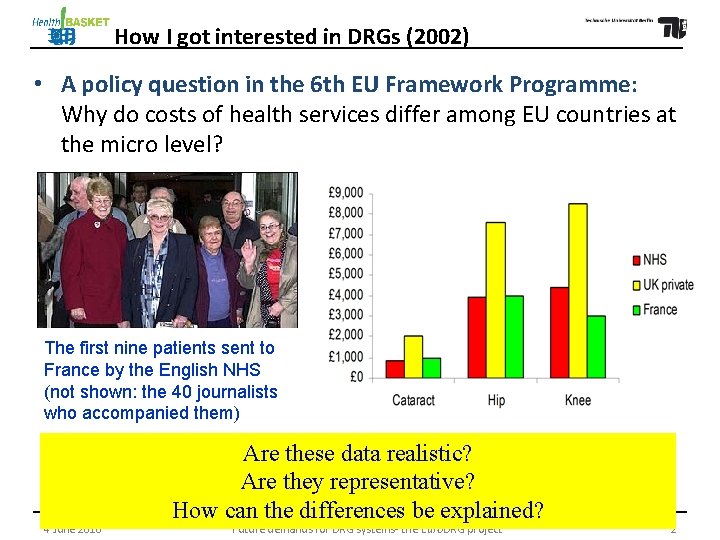
MDC (US) 0 1 2 Description EE FI SW PT ES 1 2 1 2 1 2 FR 26 (Transpl) 1 2 DE EI Engl PL Pre (A) 1 (B) 2 (C) A B C X A B 3 3 3 3 (D) D C C 4 4 4 4 (E) E D 4 Pre-MDC Nervous System Eye Ear, Nose, Mouth and Throat Respiratory System 5 Circulatory System 5 5 5 5 (F) F E 6 Digestive System Hepatobil. System and Pancreas Musculosk. Syst. & Connect. Tissue Skin, Subcut. Tissue and Breast Endocrine, Nutrit. & Metab. System Kidney and Urinary Tract Male Reprod. System Female Reprod. System Pregnancy, Childb. and Puerperium Newborn and Other Neonates Blood, Bl. Form. Org. & Immunol. Myeloproliferative DDs HIV Infectious and Parasitic DDs Mental DDs Alcohol/Drug Use or Ind. Mental Ds Multiple Significant Trauma 6 6 6 6 (G) G F D E (card) Q (vasc) F 7 7 7 7 (H) H G G 8 8 8 8 (I) I H H 9 9 30 9 9 (J) J J J 10 10 (K) K K K 11 12 13 11 12 13 11 (L) 12 (M) 13 (N) L M N L L M M 14 14 (O) O N 15 15 (P) P P 16 16 (Q) Q Q 17 25 18 19 17 17 W 19 17 (R) 18 A (S) 18 B (T) 19 (U) S/T 19 17 25 18 19 S 18 17 24 18 19 R 18 17 24 18 19 20 20 (V) V 24 24 24 25 25 24 21 A (W) 3 7 8 9 10 11 12 13 14 15 16 17 25 18 19 20 24 N U S T (res. ) V -
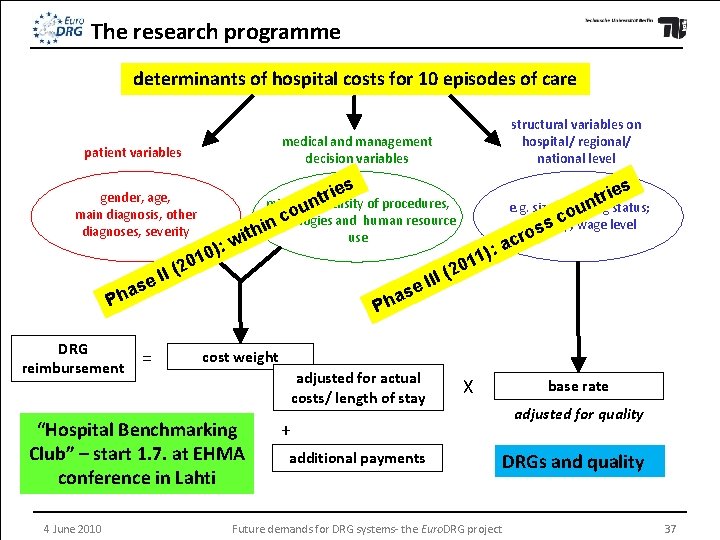
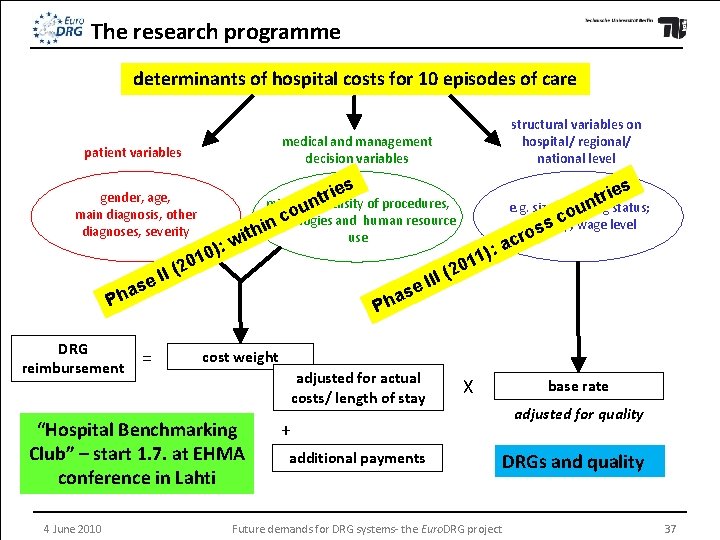
The research programme determinants of hospital costs for 10 episodes of care medical and management decision variables patient variables gender, age, main diagnosis, other diagnoses, severity ): 0 1 0 s e i r t mix and unintensity of procedures, o c technologies and human resource n i h t use i w as Ph = ies r t n e. g. size, teaching ou status; c urbanity; ss wage level o r ac I( I I e s a Ph cost weight adjusted for actual costs/ length of stay “Hospital Benchmarking Club” – start 1. 7. at EHMA conference in Lahti 4 June 2010 : ) 1 1 20 (2 I I e DRG reimbursement structural variables on hospital/ regional/ national level X + additional payments Future demands for DRG systems- the Euro. DRG project base rate adjusted for quality DRGs and quality 37
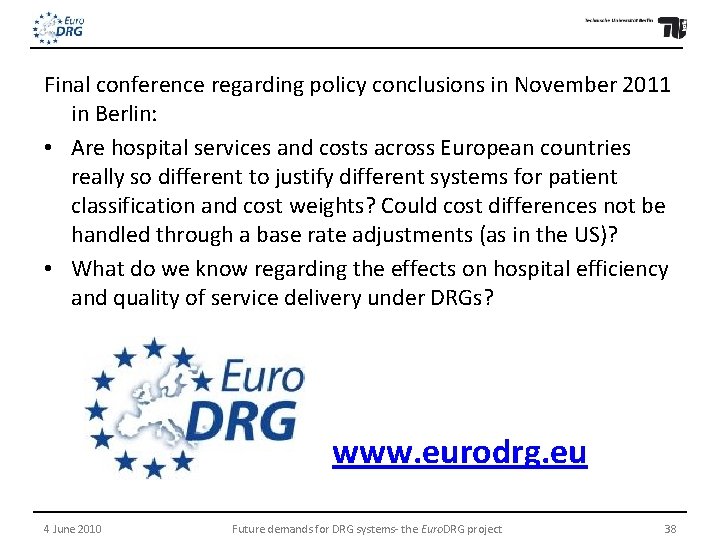
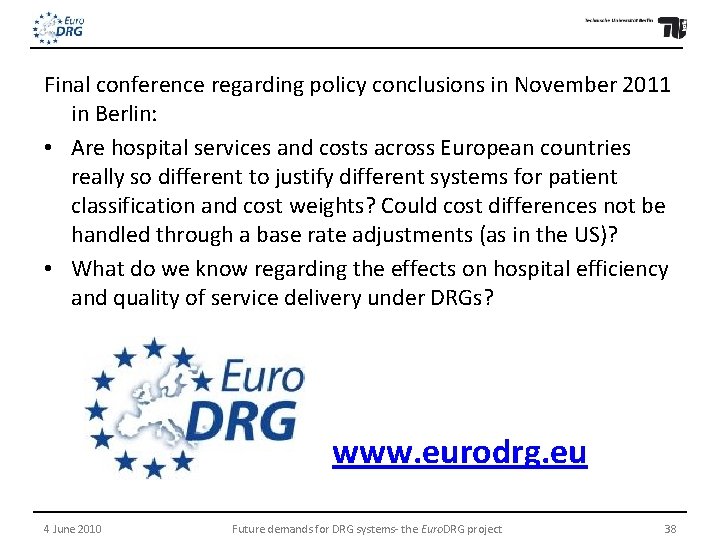
Final conference regarding policy conclusions in November 2011 in Berlin: • Are hospital services and costs across European countries really so different to justify different systems for patient classification and cost weights? Could cost differences not be handled through a base rate adjustments (as in the US)? • What do we know regarding the effects on hospital efficiency and quality of service delivery under DRGs? www. eurodrg. eu 4 June 2010 Future demands for DRG systems- the Euro. DRG project 38
 A stock of items held to meet future demands.
A stock of items held to meet future demands. Future perfect e future continuous
Future perfect e future continuous Future simple future continuous future perfect exercises
Future simple future continuous future perfect exercises Komponen casemix
Komponen casemix Casemix rekam medis
Casemix rekam medis Case mix adalah
Case mix adalah Wies funding
Wies funding Casemix main group adalah
Casemix main group adalah Customer experience management conference 2011
Customer experience management conference 2011 Pegawai pemasaran
Pegawai pemasaran Paralinguistic demands
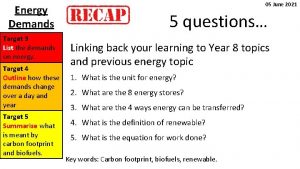
Paralinguistic demands Overload means increased demands made on the body
Overload means increased demands made on the body Health skills definition
Health skills definition Management demands of international growth
Management demands of international growth Management demands of international growth
Management demands of international growth Demands and capacities model
Demands and capacities model Vocabulary workshop level g unit 12 synonyms
Vocabulary workshop level g unit 12 synonyms You looked pretty ugly in that dress.
You looked pretty ugly in that dress. Good design demands good compromises
Good design demands good compromises Needs wants and demands
Needs wants and demands Service output demands
Service output demands When backed by buying power, wants become demands.
When backed by buying power, wants become demands. Future perfect future continuous exercises
Future perfect future continuous exercises Future continuous and future perfect objasnjenje
Future continuous and future perfect objasnjenje Tenses summary
Tenses summary Future nurse future midwife
Future nurse future midwife Future plans and finished future actions
Future plans and finished future actions Future perfect interrogative
Future perfect interrogative For interrupted actions in the future
For interrupted actions in the future Present tense to past tense
Present tense to past tense Present continuous plan
Present continuous plan Future continuous vs future perfect
Future continuous vs future perfect Teremok helsinki
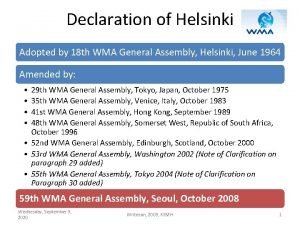
Teremok helsinki Declaracion de helsinki
Declaracion de helsinki Outlook helsingin yliopisto
Outlook helsingin yliopisto Helsinki university physics
Helsinki university physics Varaamo helsinki
Varaamo helsinki Pertti joona
Pertti joona Wma helsinki declaration
Wma helsinki declaration