Nonsurgical Periodontal Therapy NieldGehrig Chapter 19 and Perry




























- Slides: 66
Nonsurgical Periodontal Therapy Nield-Gehrig Chapter 19 and Perry Chaper 12
Nonsurgical Periodontal Therapy Other terms used to describe this phase of treatment. Initial periodontal therapy Hygienic phase Anti-infective phase Cause-related therapy Soft tissue management Phase 1 therapy Etiotropic phase Preparatory therapy

Nonsurgical Periodontal Therapy All chronic periodontitis patients should undergo nonsurgical periodontal therapy. Nonsurgical periodontal therapy is frequently successful in minimizing the extent of surgery needed.

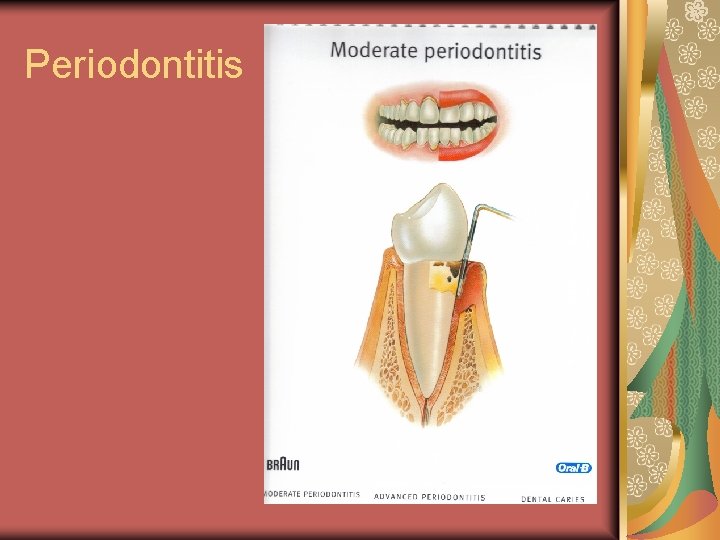
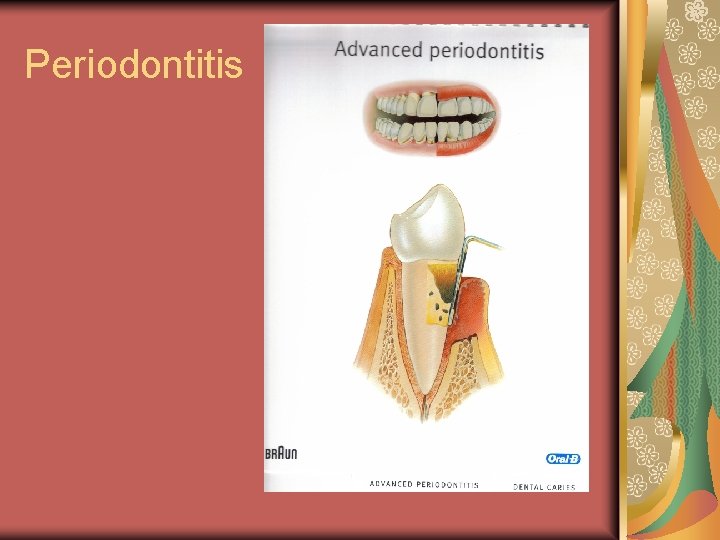
Indications Chronic Periodontitis Gingivitis and mild chronic periodontitis may be controlled with nonsurgical periodontal therapy (NSPT) alone Moderate Chronic Periodontitis can be controlled with NSPT alone for may others may require some spot periodontal surgery after NSPT.

Indications Severe Chronic Periodontitis control will probably require through NSPT followed by periodontal surgery. Although periodontal surgery is frequently indicated for patients with more advanced periodontitis, all chronic periodontitis patients should undergo nonsurgical periodontal therapy prior to periodontal surgical intervention. Nonsurgical periodontal therapy is frequently successful in minimizing the extent of surgery needed.
Goals 1. To control the bacterial challenge to the patient Intensive training of the patient in appropriate techniques for self-care and professional removal of calculus deposits and bacterial products from tooth surfaces Removal of calculus deposits and bacterial products contaminating the tooth surfaces. Calculus deposits ALWAYS are covered with living bacterial biofilms that are associated with continuing inflammation if not removed.
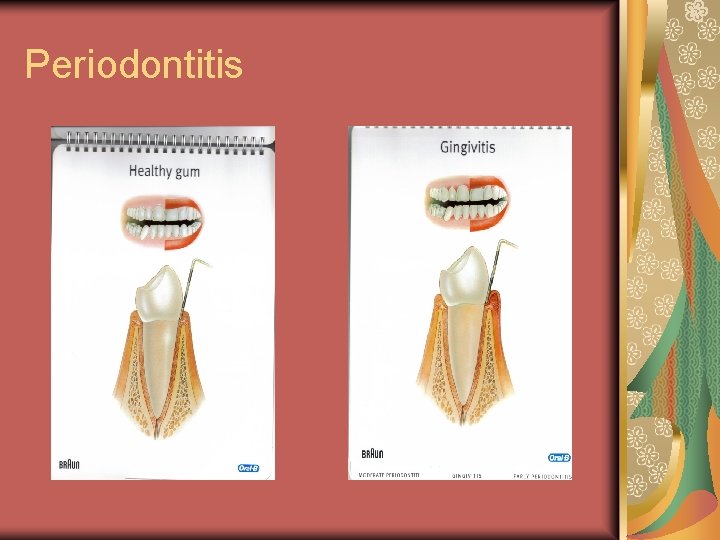
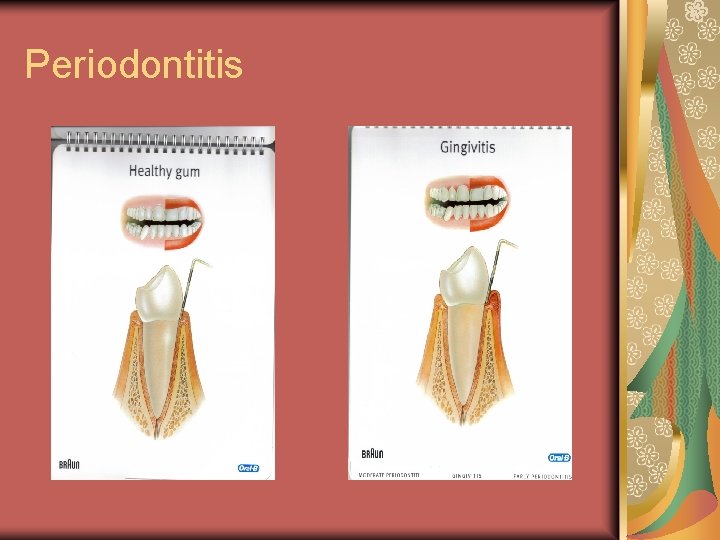
Periodontitis

Periodontitis
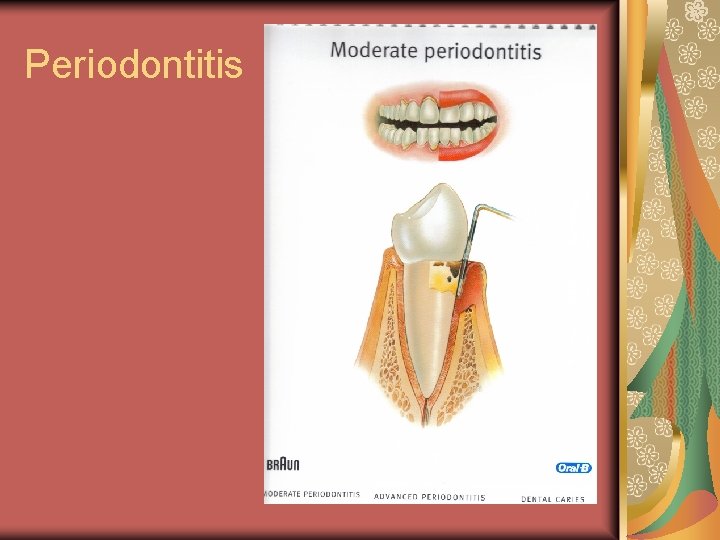
Periodontitis
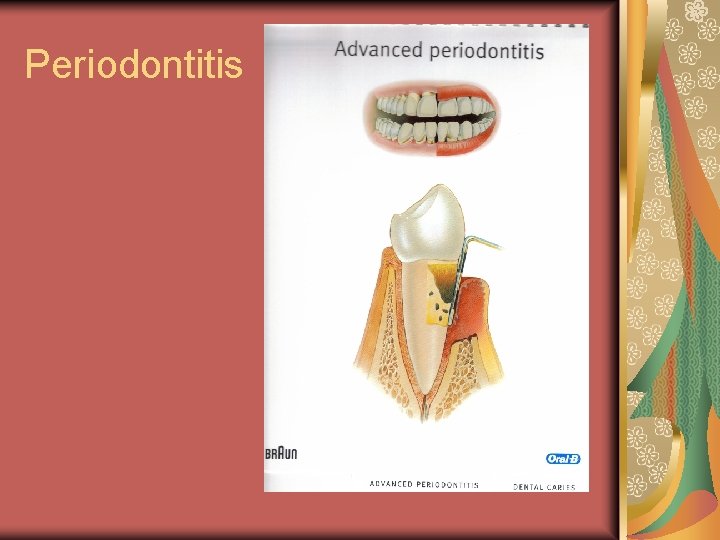
Periodontitis
Goals 2. To minimize the impact of systemic factors Certain systemic diseases or conditions can increase the risk of periodontitis and the severity. Plan must minimized the impact of systemic risk factors
Goals 3. To eliminate or control local risk factors Local environmental risk factors can increase the risk of developing periodontitis in localized sites. Plaque retention in a site allow damage over time to periodontium Local environmental risk factors should be eliminated.
Components The patients role in Nonsurgical Periodontal Therapy Daily plaque removal Professional Therapy Must be customized for the individual patient Components may included plaque control, nonsurgical instrumentation, and the adjunctive use of chemical agents
Nonsurgical Instrumentation Mechanical removal of calculus is necessary because it is a mechanical irritant and holds biofilm. Periodontal debridement is likely to remain the most important component of nonsurgical periodontal therapy for the foreseeable future.
Instrumentation Terminology Traditional Terminology Scaling = instrumentation of the crown and root surfaces of the teeth to remove plaque, calculus, and stains Root Planing = treatment procedure designed to remove cementum or surface dentin that is rough, impregnated with calculus, or contaminated with toxins or microorganisms.
Instrumentation Terminology Emerging Terminology Periodontal debridement = includes instrumentation of every square millimeter of root surface for removal of plaque and calculus, but does not include the deliberate, aggressive removal of cementum Conservation of cementum while removing all calculus and biofilm is the goal of periodontal debridement.
Instrumentation Terminology Deplaquing = the disruption or removal of subgingival microbial plaque and its byproducts from cemental surfaces and the pocket space

Instrumentation Terminology Considerations Regarding Emerging Terminology Periodontal Debridement is not currently a ADA procedure name. (no code) Some authors have redefined the definition of root planing because of this.







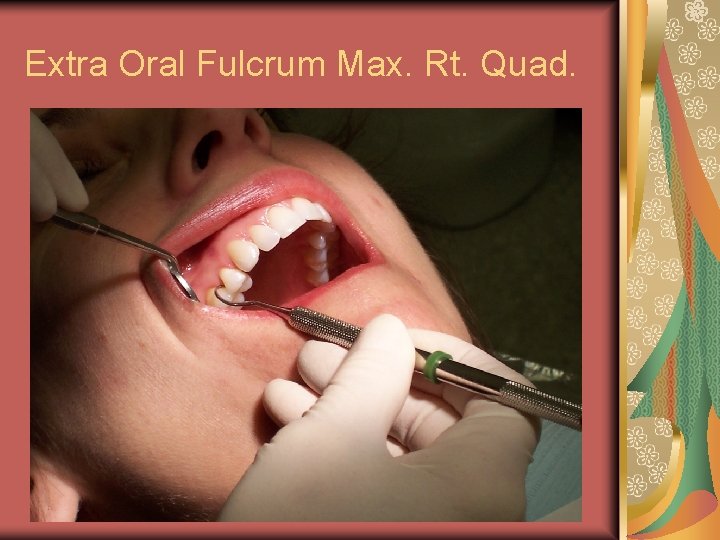
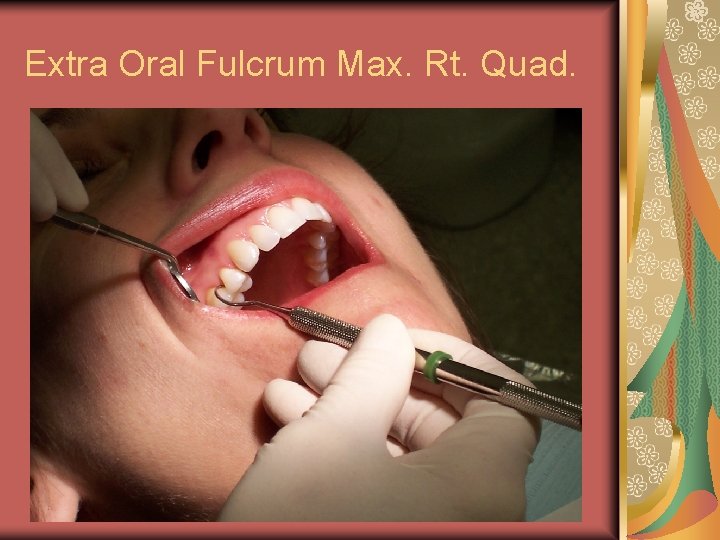
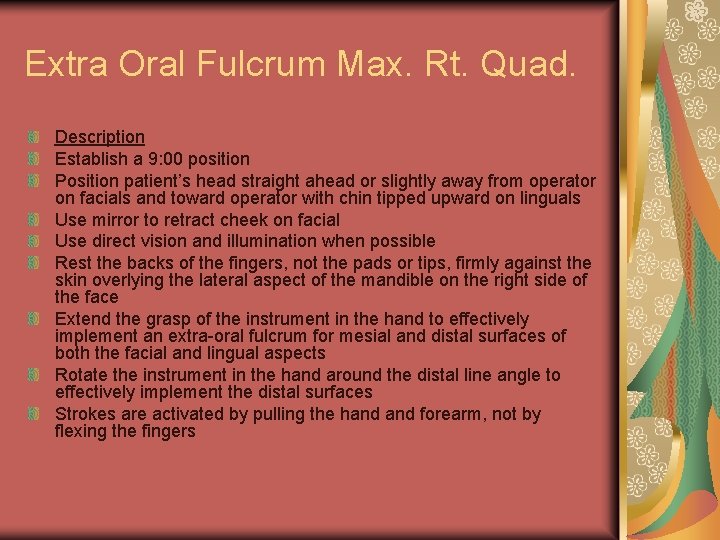
Extra Oral Fulcrum Max. Rt. Quad.

Extra Oral Fulcrum Max. Rt. Quad. Advantages Greater parallelism of lower shank to the tooth Greater parallelism for access to the base of the pocket Improved access to distal surfaces and third molar Neutral wrist position Utilizes larger muscles of palm and forearm, meaning less operator fatigue Proper use of this fulcrum provides stability and control of the instrument stroke
Extra Oral Fulcrum Max. Rt. Quad. Description Establish a 9: 00 position Position patient’s head straight ahead or slightly away from operator on facials and toward operator with chin tipped upward on linguals Use mirror to retract cheek on facial Use direct vision and illumination when possible Rest the backs of the fingers, not the pads or tips, firmly against the skin overlying the lateral aspect of the mandible on the right side of the face Extend the grasp of the instrument in the hand to effectively implement an extra-oral fulcrum for mesial and distal surfaces of both the facial and lingual aspects Rotate the instrument in the hand around the distal line angle to effectively implement the distal surfaces Strokes are activated by pulling the hand forearm, not by flexing the fingers

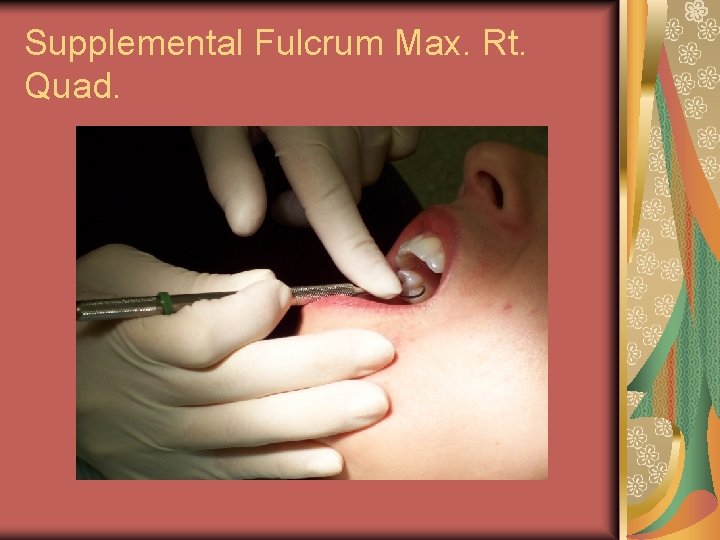
Supplemental Fulcrum Max. Rt. Quad.

Supplemental Fulcrum Advantages Neutral wrist position Utilizes larger muscles of palm and forearm Less operator fatigue Added support for the removal of tenacious subgingival calculus Reduces muscle strain and workload from the dominant hand Added control and stability Reduces instrument breakage

Supplemental Fulcrum Max. Rt. Quad. Description Establish a 9: 00 position Position patient’s head toward operator with chin up Place index finger of the non-dominant hand on the shank to apply supplemental lateral pressure to either the mesial or distal surfaces of the tooth Fulcrum may be established on the mandibular anteriors or and extra oral fulcrum is acceptable
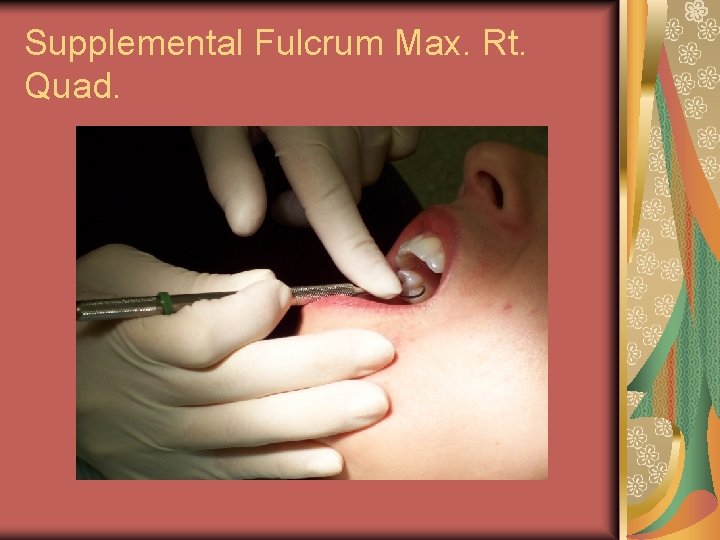
Supplemental Fulcrum Max. Rt. Quad.

Supplemental Fulcrum Max. Rt. Quad.

Rationale for Periodontal Debridement Arrest the progress of periodontal disease Induce positive changes in the subgingival bacterial flora (count and content) Create an environment that permits the gingival tissue to heal, therefore eliminating inflammation

Rationale for Periodontal Debridement Convert the pocket from an area experiencing increased loss of attachment to one in which the clinical attachment level remains the same or even gains in attachment Eliminate bleeding Improve the integrity of tissue attachment
Rationale for Periodontal Debridement Increase effectiveness of patient selfcare Permit reevaluation of periodontal health status to determine if surgery is needed Prevent recurrence of disease through periodontal maintenance therapy
Appointment planning for calculus removal Full-mouth debridement is defined as periodontal debridement completed in a single appointment or in two appointments within a 24 -hour period. Since periodontal disease is an infection, the full-mouth approach to periodontal debridement is based on the assumption that the remaining untreated areas of the mouth can reinfect the treated areas.
Appointment planning for calculus removal In research studies, the full-mouth debridement procedure was combined with the use of topical antimicrobial therapy (full-mouth disinfection), It is unclear, however, if the antimicrobial therapy actually contributed to the improved results derived form the full-mouth periodontal debridement alone.
Appointment planning for calculus removal Full-mouth debridement is best accomplished by the dental hygienist working with an assistant. Initially, patients may be resistant to the concept of scheduling one or two long appointments for the purpose of periodontal debridement. One or two long appointments, however, may in reality be less disruptive to an individual’s work schedule than four to six 1 hour appointments over several weeks. In addition, the dental hygienist should explain the rationale behind full-mouth debridement.
Appointment planning for calculus removal Planned multiple appointments. If periodontal debridement is completed in sextants or quadrants over multiple appointments, at each appointment the clinician should treat only as many teeth, sextants, or quadrants as he or she can thoroughly debride of calculus and plaque during that appointment.
Ultrasonic Instrumentation Introduction to Ultrasonic Instrumenttation Gracey curet was the primary instrument Now the precision-thin ultrasonic tip Research indicates not only that the ultrasonic instrumentation is as effective as hand instrumentation, but also that ultrasonic instrumentation is as effective as hand instrumentation in the treatment and maintenance of periodontal pockets.

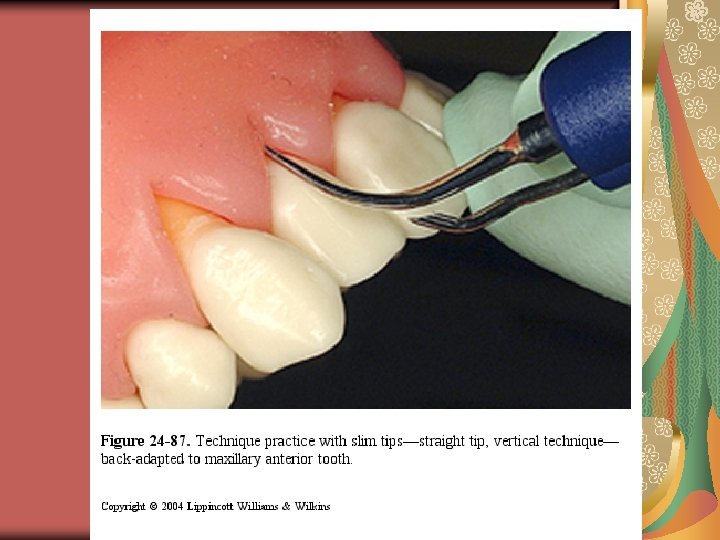
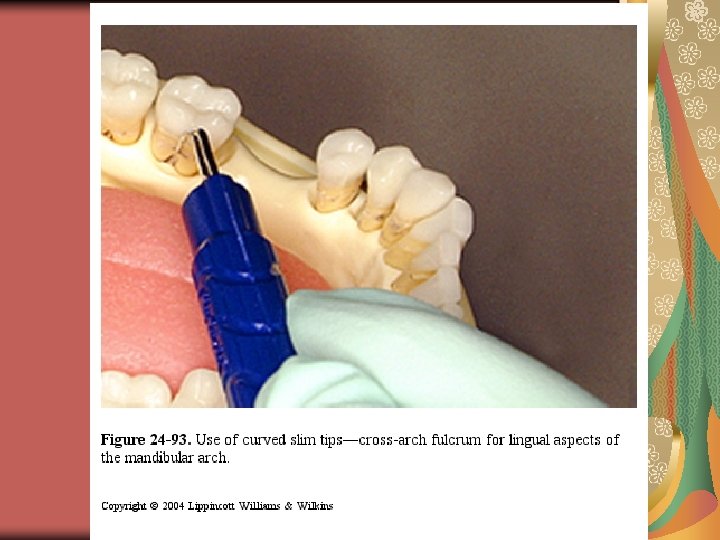
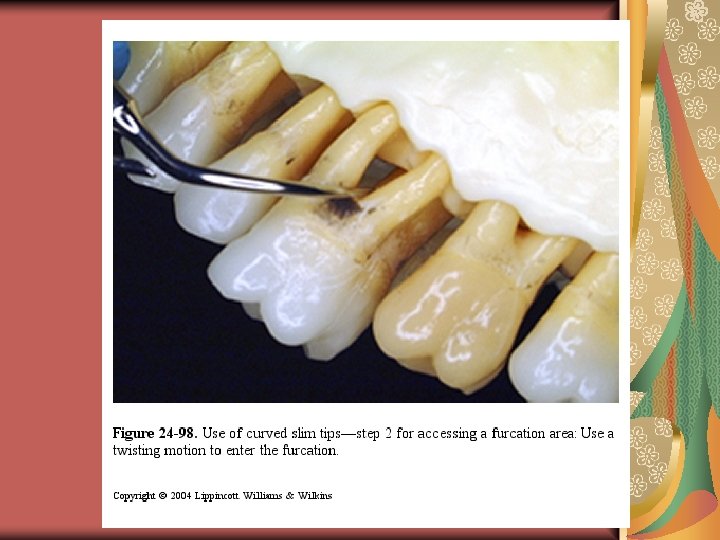
Slim-diameter curved tips Similar in design to a curved furcation probe Designed fo use on: Posterior root surfaces located more than 4 mm apical to the CEJ Root concavities and furcations on posterior tooth surfaces


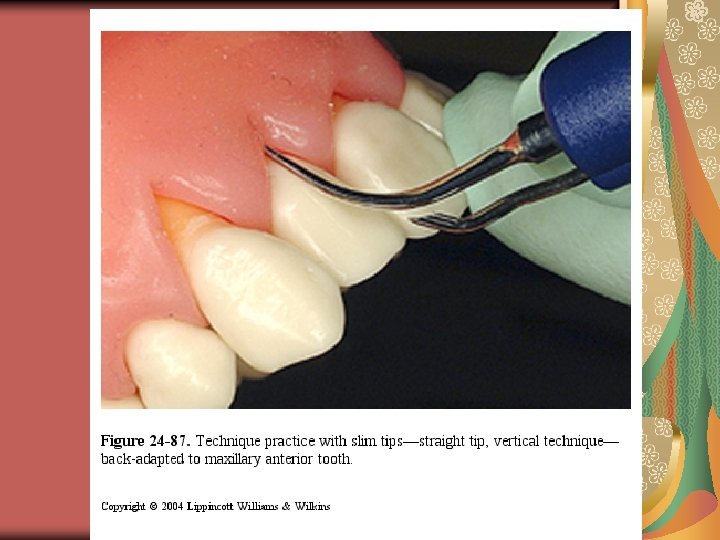

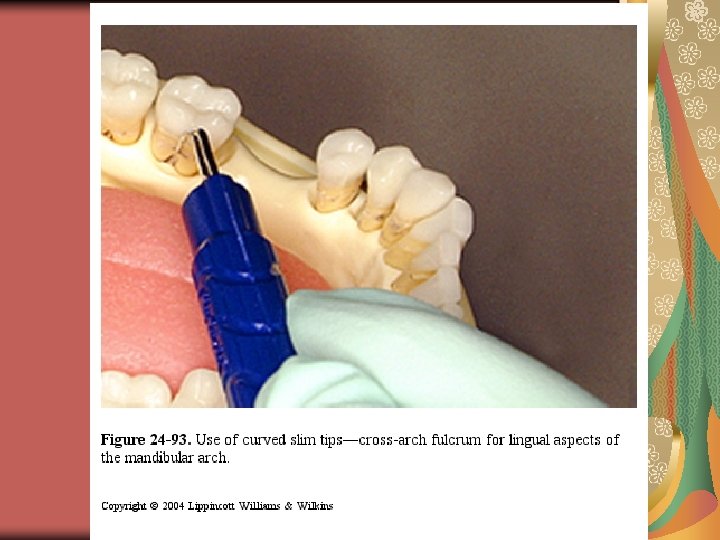
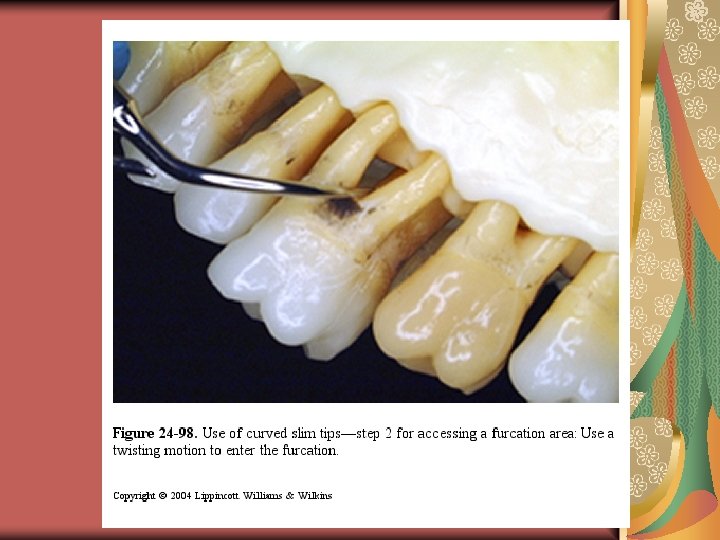



Advantages of Ultrasonic Instrumentation Mechanism of Action of Ultrasonic Instruments Ability to flush debris, bacteria, and unattached plaque from the periodontal pocket with the fluid lavage. Ultrasonic Instrument Tip Design. Precision-thin ultrasonic tips have the following advantages

Precision-thin tip advantages Thinner and smaller than the working-end of a curet. Standard Gracey curets are too wide to enter the furcation area of more than 50% of all max. and mand. first molars. Precision-thin tips have been shown to reach 1 mm deeper than hand instruments and to teach the base of the pocket in 86% of 3 -9 mm pockets
Tissue Healing: End Point of Instrumentation Tissue Health: The goal of instrumentation is to render the tooth surface and pocket space acceptable to the tissue so that healing occurs. Healing After Instrumentation The primary pattern of healing after periodontal debridement is through the formation of a long junctional epithelium There is no formation of new bone, cementum, or periodontal ligament during the healing process that occurs after periodontal debridement
Tissue Healing: End Point of Instrumentation Nonsurgical periodontal therapy can result in reduced probing depths due to the formation of a long junctional epithelium combined with the gingival recession that often occurs following NSPT
Tissue Healing: End Point of Instrumentation Assessing Tissue Healing. Re-evaluation should be scheduled for 4 – 6 weeks after completion of instrumentation. Nonresponsive sites should be carefully re-evaluated with an explorer for the presence of residual calculus or roughness
Dentinal Hypersensitivity Description – a short, sharp painful reaction that occurs when some areas of exposed dentin are subjected to mechanical, thermal, or chemical stimuli Associated with exposed dentin Usually pain is sporadic
Dentinal Hypersensitivity Precipitating Factors for Sensitivity Gingival Recession Sometimes healing results in a small amount of tooth root being exposed Conservation of cementum should be a goal of NSPT
Re-evaluation 4 -6 weeks after treatment Update medical status Perform a periodontal clinical assessment Compare data gathered at the initial periodontal assessment with the data at reevaluation Make decisions about the need for additional NSPT, periodontal maintenance, and periodontal surgery
AAP Guidelines for referrals Meant to help identify patients who are at greatest risk early and, therefore would benefit from specialty care.

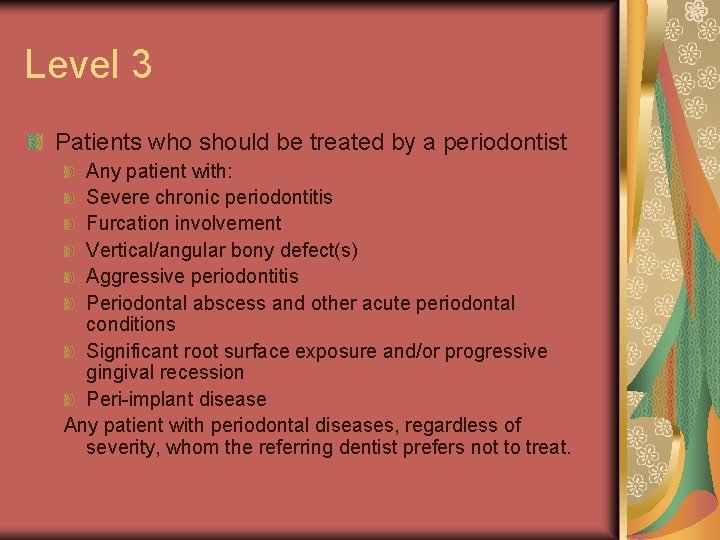
Level 3 Patients who should be treated by a periodontist Any patient with: Severe chronic periodontitis Furcation involvement Vertical/angular bony defect(s) Aggressive periodontitis Periodontal abscess and other acute periodontal conditions Significant root surface exposure and/or progressive gingival recession Peri-implant disease Any patient with periodontal diseases, regardless of severity, whom the referring dentist prefers not to treat.
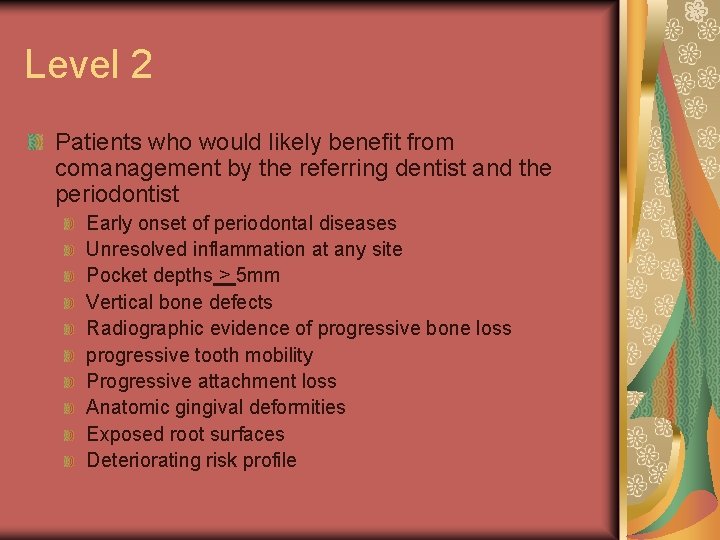
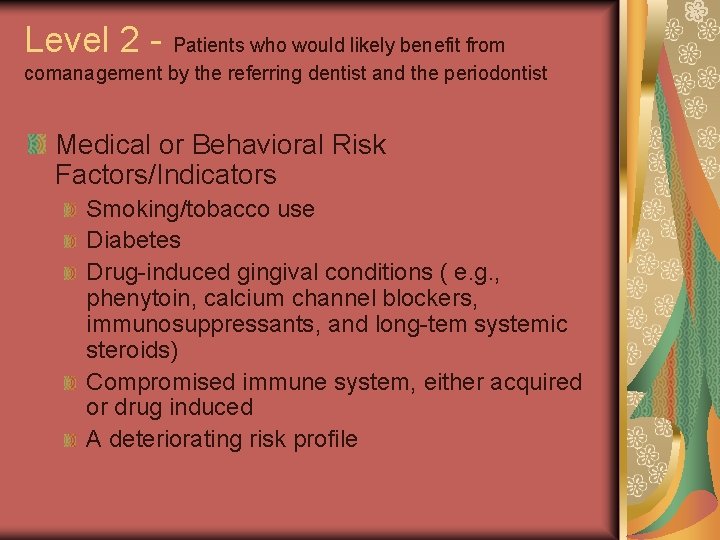
Level 2 Patients who would likely benefit from comanagement by the referring dentist and the periodontist Early onset of periodontal diseases Unresolved inflammation at any site Pocket depths > 5 mm Vertical bone defects Radiographic evidence of progressive bone loss progressive tooth mobility Progressive attachment loss Anatomic gingival deformities Exposed root surfaces Deteriorating risk profile
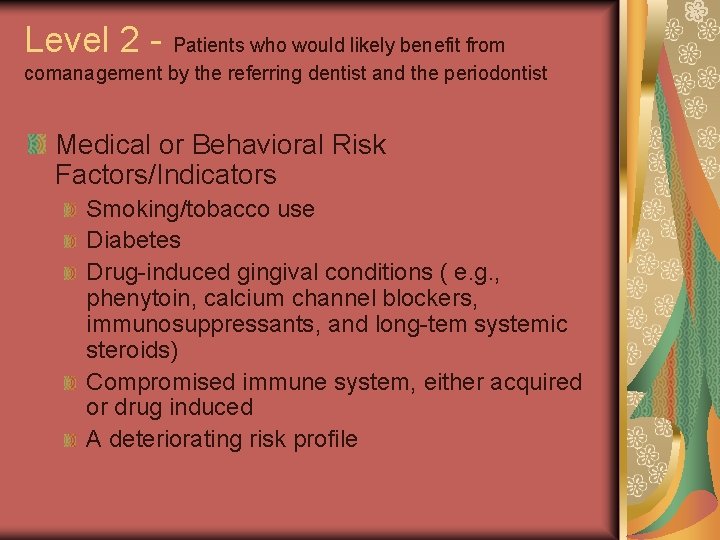
Level 2 - Patients who would likely benefit from comanagement by the referring dentist and the periodontist Medical or Behavioral Risk Factors/Indicators Smoking/tobacco use Diabetes Drug-induced gingival conditions ( e. g. , phenytoin, calcium channel blockers, immunosuppressants, and long-tem systemic steroids) Compromised immune system, either acquired or drug induced A deteriorating risk profile
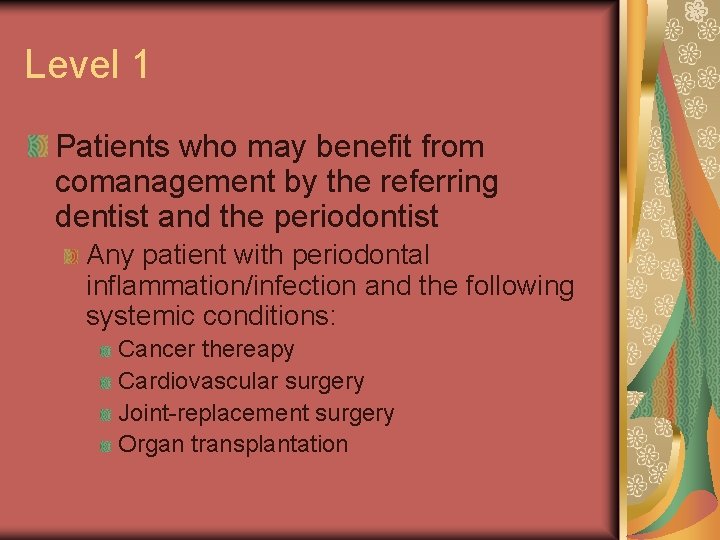
Level 1 Patients who may benefit from comanagement by the referring dentist and the periodontist Any patient with periodontal inflammation/infection and the following systemic conditions: Cancer thereapy Cardiovascular surgery Joint-replacement surgery Organ transplantation
 Perimylolysis
Perimylolysis Corrective phase
Corrective phase Rationale for periodontal treatment
Rationale for periodontal treatment Maintenance phase of periodontal therapy
Maintenance phase of periodontal therapy Both psychoanalysis and humanistic therapy stress
Both psychoanalysis and humanistic therapy stress Bioness bits cost
Bioness bits cost Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Dualism multiplicity and relativism
Dualism multiplicity and relativism Katy perry relient k
Katy perry relient k Periodontal instruments classification
Periodontal instruments classification Periodontal tedavi fazları
Periodontal tedavi fazları Ligament synonym
Ligament synonym Gingival description
Gingival description Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Plaque index scoring criteria
Plaque index scoring criteria Fases del tratamiento periodontal
Fases del tratamiento periodontal Enap periodontal adalah
Enap periodontal adalah Periodontal cep
Periodontal cep Osteocitos
Osteocitos Glickman's concept
Glickman's concept Cva
Cva Akut streptokokal gingivitis
Akut streptokokal gingivitis Tecnica step back
Tecnica step back Helicobacter pylori transmision
Helicobacter pylori transmision Periodontal ligament meaning
Periodontal ligament meaning Sharpey lifleri
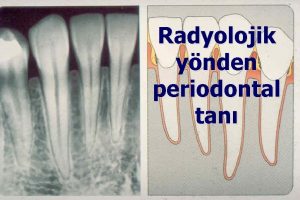
Sharpey lifleri Diagnosis of periodontal disease
Diagnosis of periodontal disease Lateral periodontal cyst
Lateral periodontal cyst Periapical granuloma vs abscess
Periapical granuloma vs abscess Periodontal abscess
Periodontal abscess Periodontal ligament injection definition
Periodontal ligament injection definition Periodontal disease
Periodontal disease Kista residual adalah
Kista residual adalah Dental charting abbreviations
Dental charting abbreviations Gtr indications
Gtr indications General principles of periodontal surgery
General principles of periodontal surgery Raphe mylohyoidea
Raphe mylohyoidea Componentes del periodonto de proteccion
Componentes del periodonto de proteccion Modified widman flap vs undisplaced flap
Modified widman flap vs undisplaced flap Ligamento periodontal
Ligamento periodontal Who sondu
Who sondu Interdental septum
Interdental septum Murat alikan
Murat alikan Periodontal case study
Periodontal case study Infrabony pocket
Infrabony pocket Stress strain curve physiotherapy
Stress strain curve physiotherapy Kalani perry
Kalani perry Perry glasser
Perry glasser Words that rhyme with jennifer
Words that rhyme with jennifer Dr richard perry neurologist
Dr richard perry neurologist Onamonapeia
Onamonapeia Commodore matthew perry apush
Commodore matthew perry apush Perry reece map
Perry reece map William g perry
William g perry Theme of trojan war
Theme of trojan war Sunrise sunset perry como
Sunrise sunset perry como Katy perry poem
Katy perry poem Perry laroque
Perry laroque Dr. perry sugar
Dr. perry sugar Perry grigsby
Perry grigsby Trans siberian railroad definition ap world history
Trans siberian railroad definition ap world history Katy perry firework figurative language
Katy perry firework figurative language Brian perry lawyer
Brian perry lawyer Importance of the study example
Importance of the study example Perry high school marching band
Perry high school marching band Dog vaccination perry county
Dog vaccination perry county Perry babb
Perry babb