NonEpileptiform Patterns Dr Lim Shih Hui Senior Consultant
- Slides: 41
Non-Epileptiform Patterns Dr Lim Shih Hui Senior Consultant Neurologist Singapore General Hospital
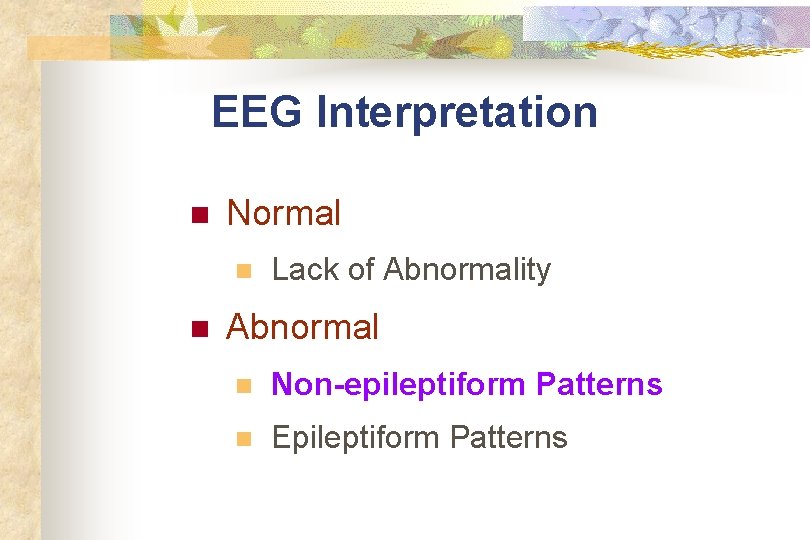
EEG Interpretation n Normal n n Lack of Abnormality Abnormal n Non-epileptiform Patterns n Epileptiform Patterns
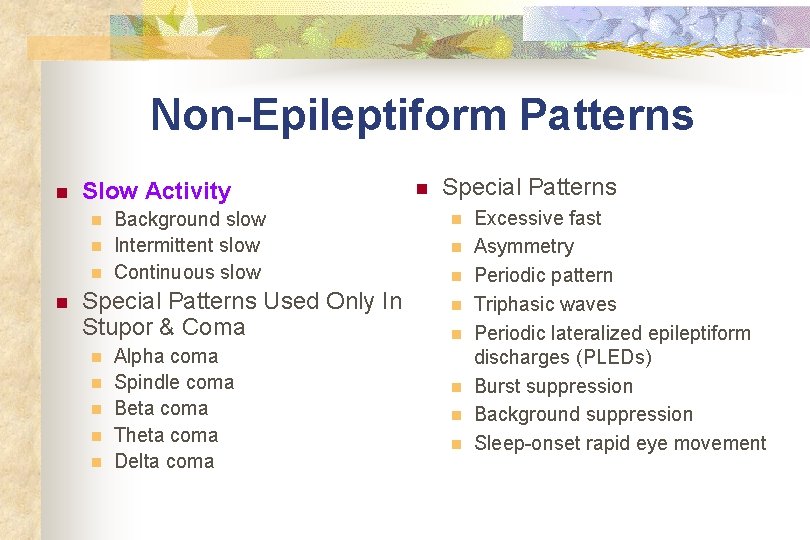
Non-Epileptiform Patterns n Slow Activity n n Background slow Intermittent slow Continuous slow Special Patterns Used Only In Stupor & Coma n n n Alpha coma Spindle coma Beta coma Theta coma Delta coma n Special Patterns n n n n Excessive fast Asymmetry Periodic pattern Triphasic waves Periodic lateralized epileptiform discharges (PLEDs) Burst suppression Background suppression Sleep-onset rapid eye movement
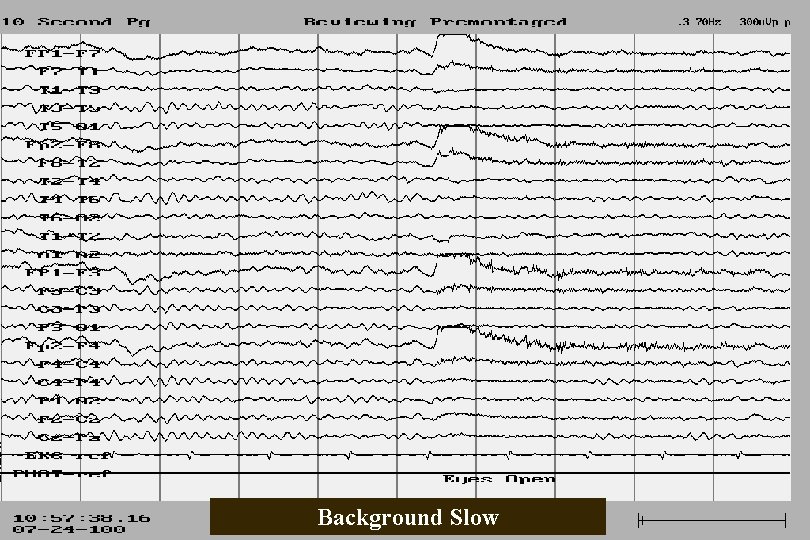
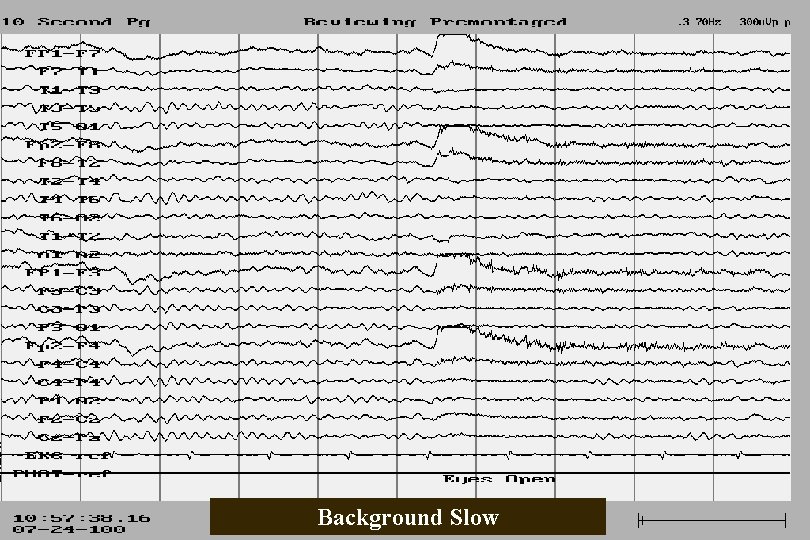
Background Slow
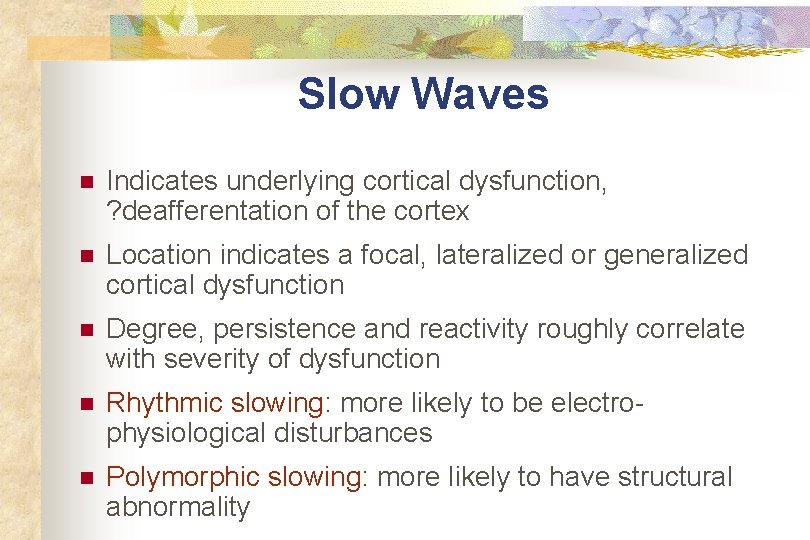
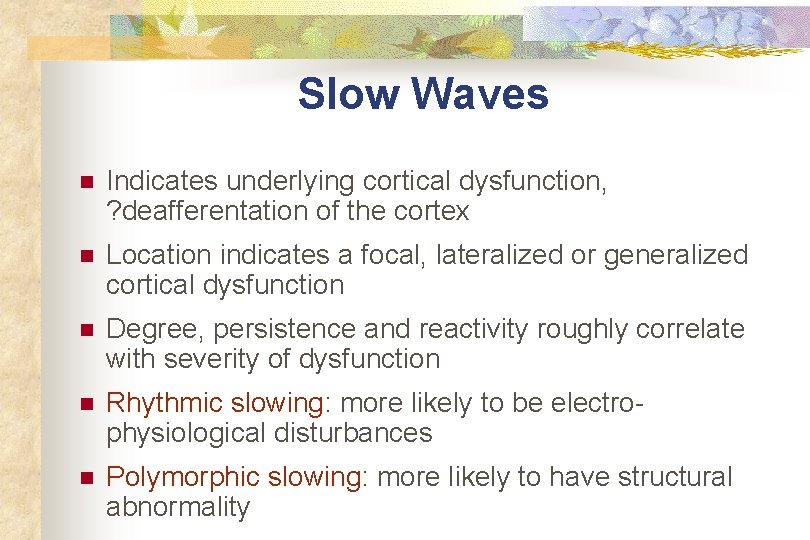
Slow Waves n Indicates underlying cortical dysfunction, ? deafferentation of the cortex n Location indicates a focal, lateralized or generalized cortical dysfunction n Degree, persistence and reactivity roughly correlate with severity of dysfunction n Rhythmic slowing: more likely to be electrophysiological disturbances n Polymorphic slowing: more likely to have structural abnormality
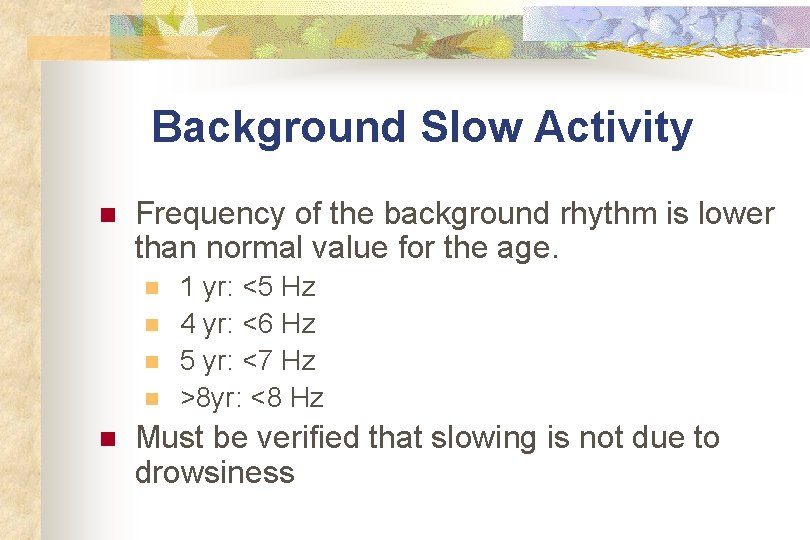
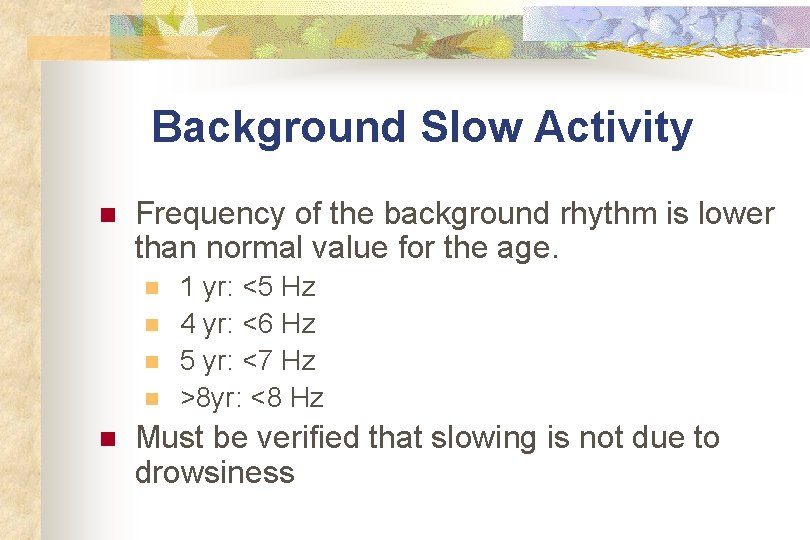
Background Slow Activity n Frequency of the background rhythm is lower than normal value for the age. n n n 1 yr: <5 Hz 4 yr: <6 Hz 5 yr: <7 Hz >8 yr: <8 Hz Must be verified that slowing is not due to drowsiness
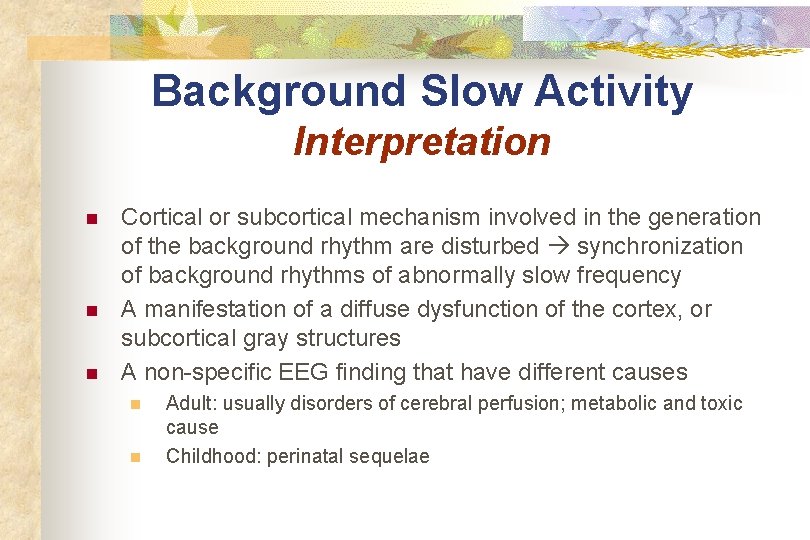
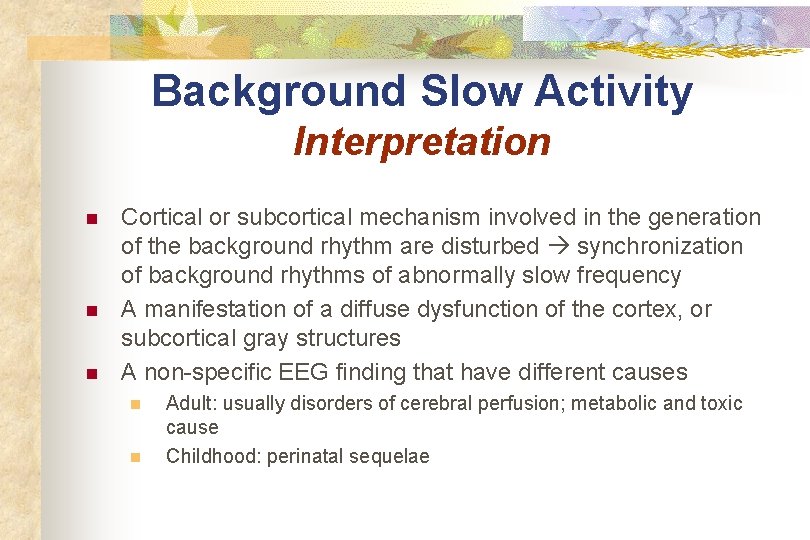
Background Slow Activity Interpretation n Cortical or subcortical mechanism involved in the generation of the background rhythm are disturbed synchronization of background rhythms of abnormally slow frequency A manifestation of a diffuse dysfunction of the cortex, or subcortical gray structures A non-specific EEG finding that have different causes n n Adult: usually disorders of cerebral perfusion; metabolic and toxic cause Childhood: perinatal sequelae
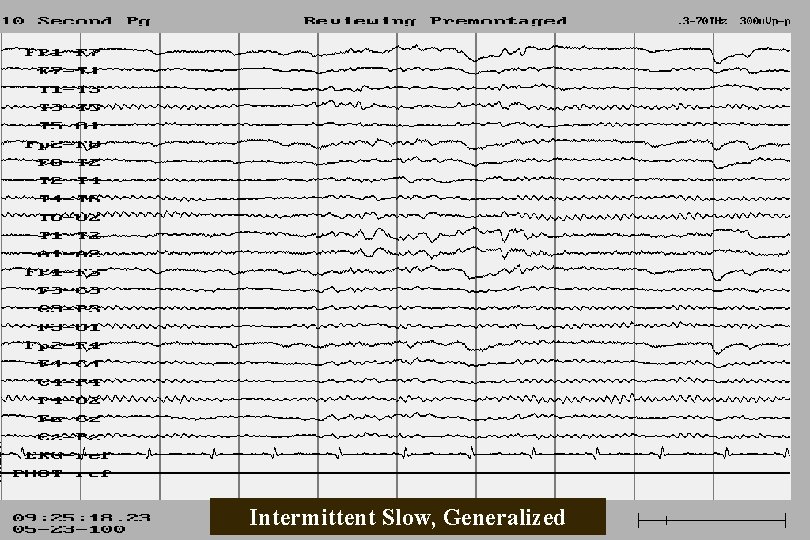
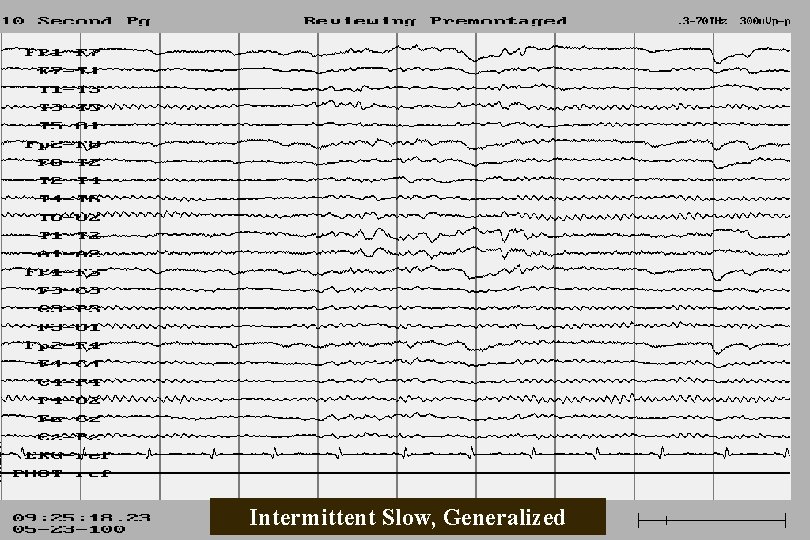
Intermittent Slow, Generalized
Intermittent Slow Activity n n n Occurs intermittently and is not caused by drowsiness Rhythmic or irregular Generalized, regional or lateralized Background rhythm is generally well preserved; indicating that cortical and subcortical mechanism involved in its generation are functionally normal A non-specific functional cerebral dysfunction Has diverse cause n Can be an early manifestation of continuous slow activity or epileptiform changes
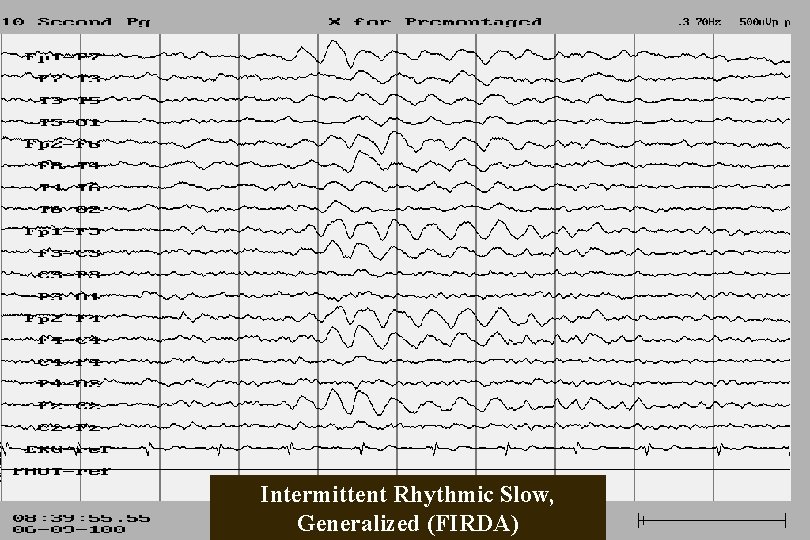
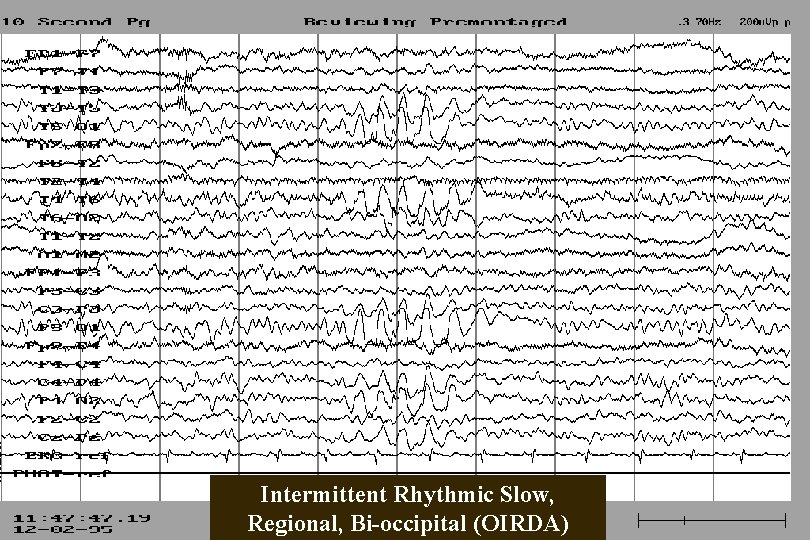
Generalized Intermittent Slow Activity n n Can be caused by infra-tentorial or supratentorial lesions Unprovoked intermittent slow n n diffuse cortical dysfunction generalized epilepsy Adult: predominantly frontal (Frontal Intermittent Rhythmic Delta Activity FIRDA) Children: predominantly occipital (OIRDA)
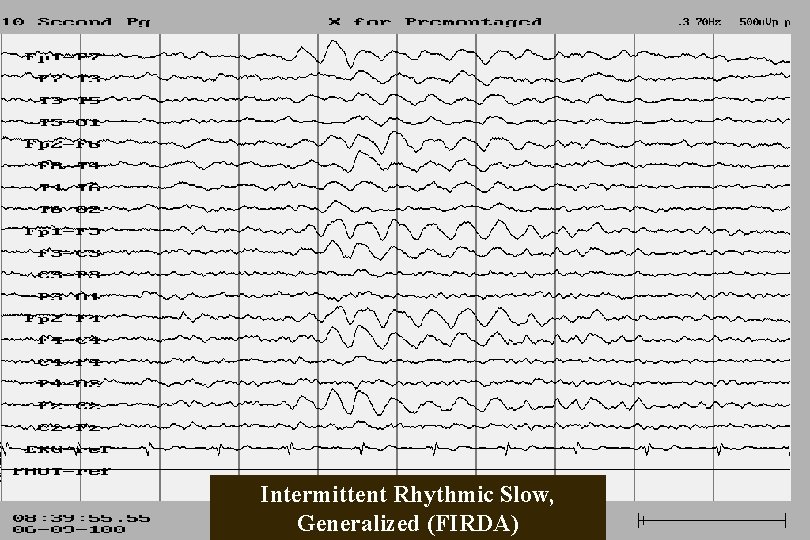
Intermittent Rhythmic Slow, Generalized (FIRDA)
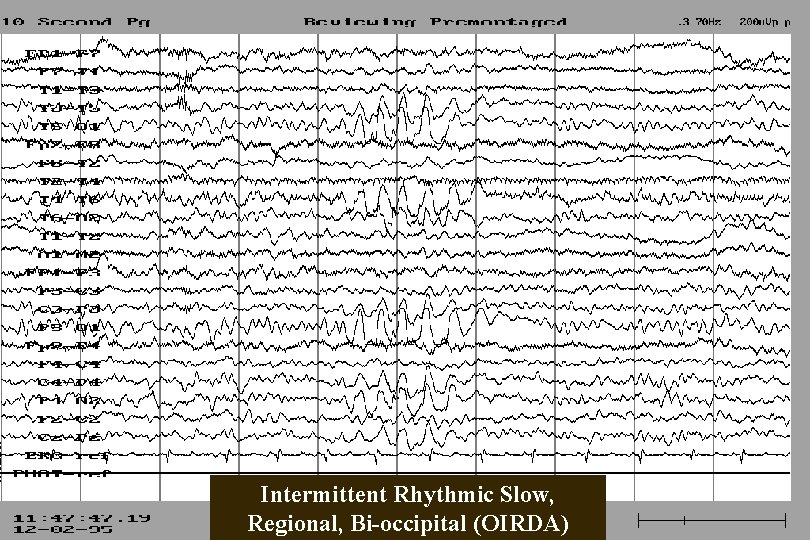
Intermittent Rhythmic Slow, Regional, Bi-occipital (OIRDA)
Intermittent Rhythmic Slow (IRS) n n More specific subclass of intermittent slow Appeared grouped in bursts Relatively rhythmic Generalized IRS: n n n Diffuse involvement of cortical and subcortical grey structures (e. g. diffuse encephalopathy or generalized non-focal epilepsy) Mesial cortical lesion Focal subcortical grey matter lesion; infra- or supratentorial destructive process e. g. tumors or raised intracranial pressure
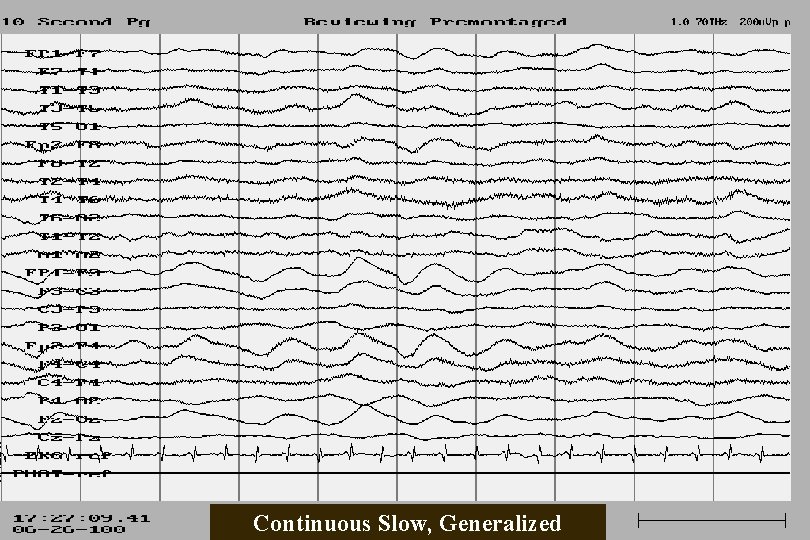
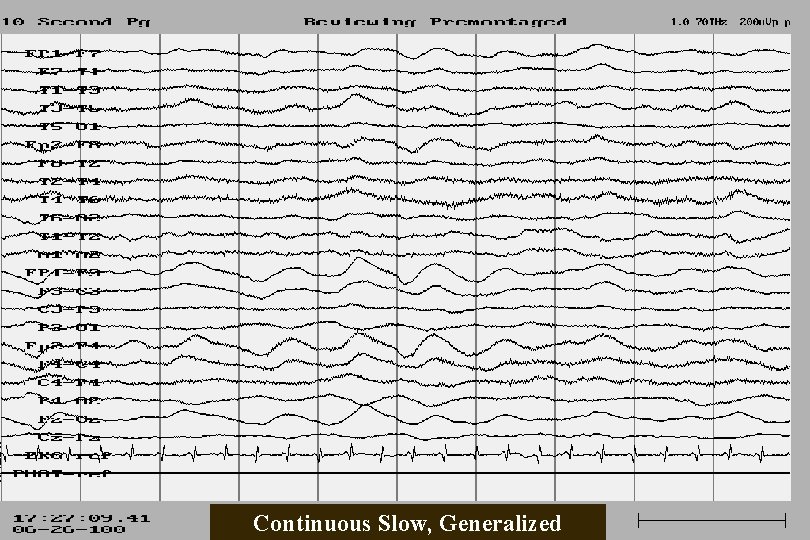
Continuous Slow, Generalized
Continuous Slow Activity n n n Occurs continuously Irregular (polymorphic) Lies within frequency range of delta/theta waves Non-responsive to external stimuli Clearly exceeds the amount considered physiologically normal for the patient’s age Severe disturbances of interneuronal connections or of the biochemical environment of cortical neurons continuous slow activity
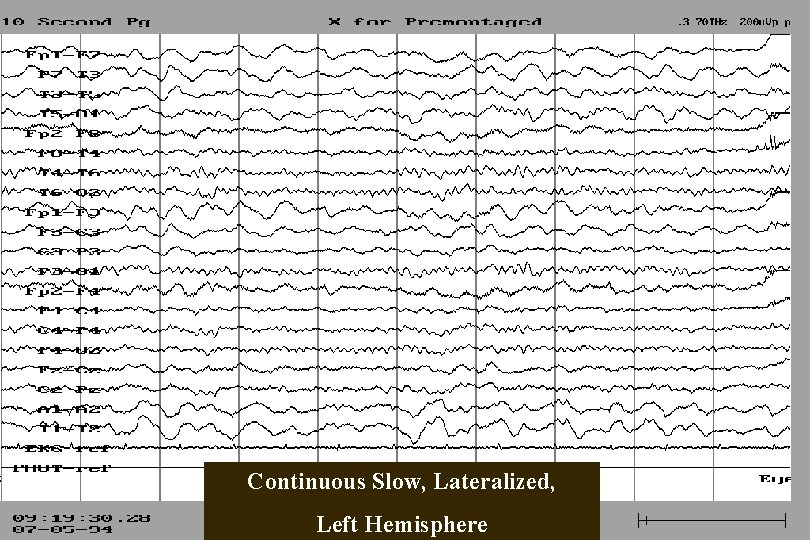
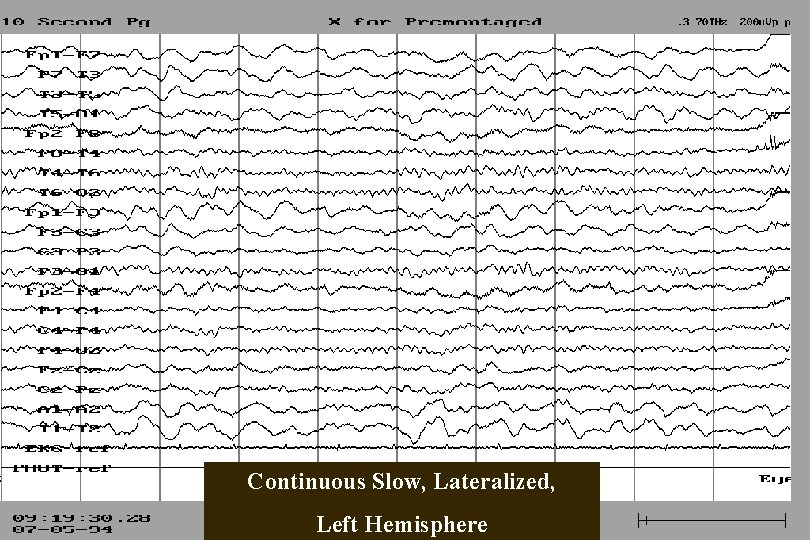
Continuous Slow, Lateralized, Left Hemisphere
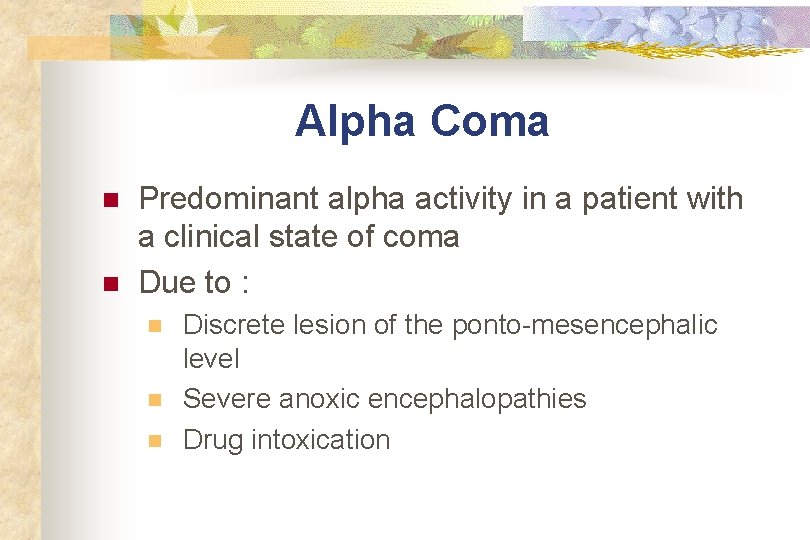
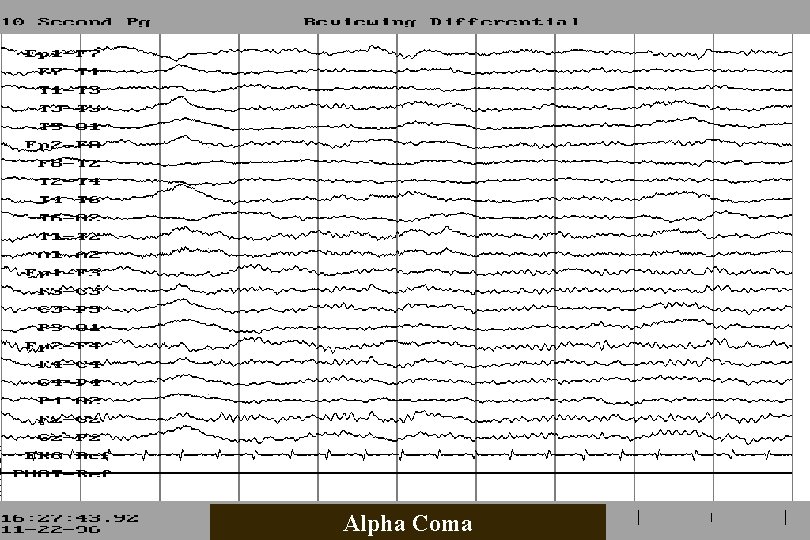
Alpha Coma n n Predominant alpha activity in a patient with a clinical state of coma Due to : n n n Discrete lesion of the ponto-mesencephalic level Severe anoxic encephalopathies Drug intoxication
Alpha Coma
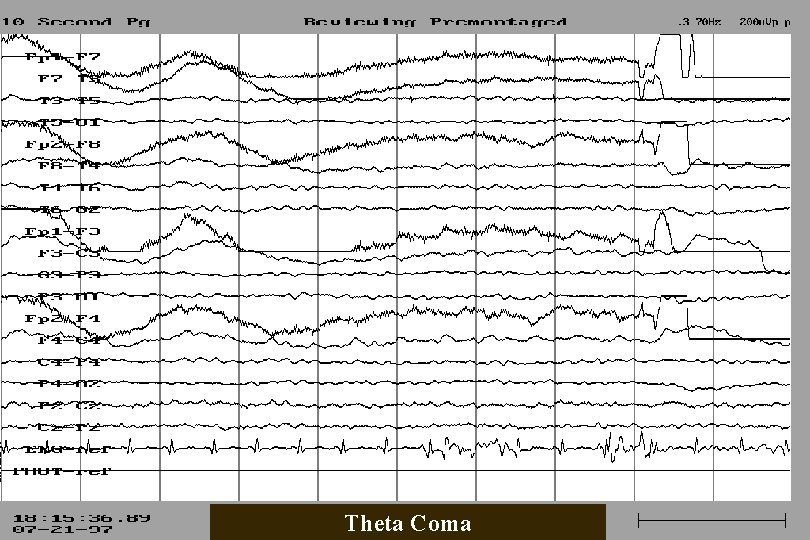
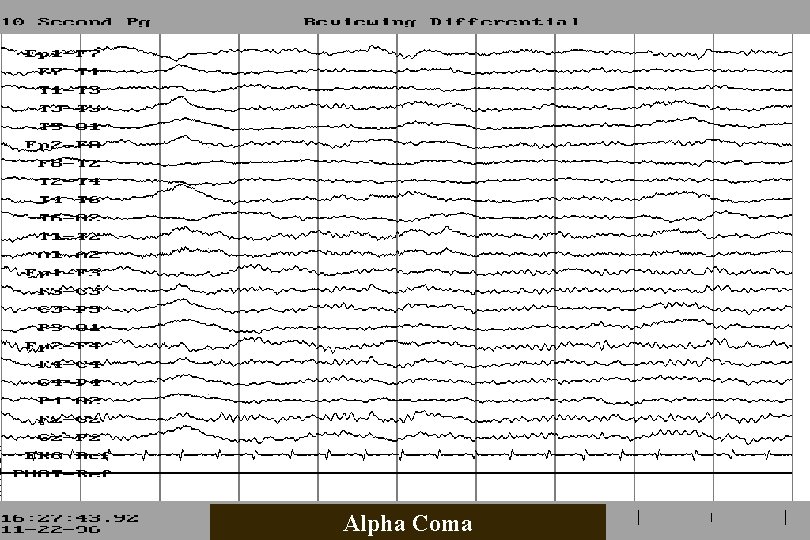
Theta Coma n n n Predominant theta activity in patient in coma Due to severe diffuse encephalopathy Potentially reversible; prognosis depends on underlying condition
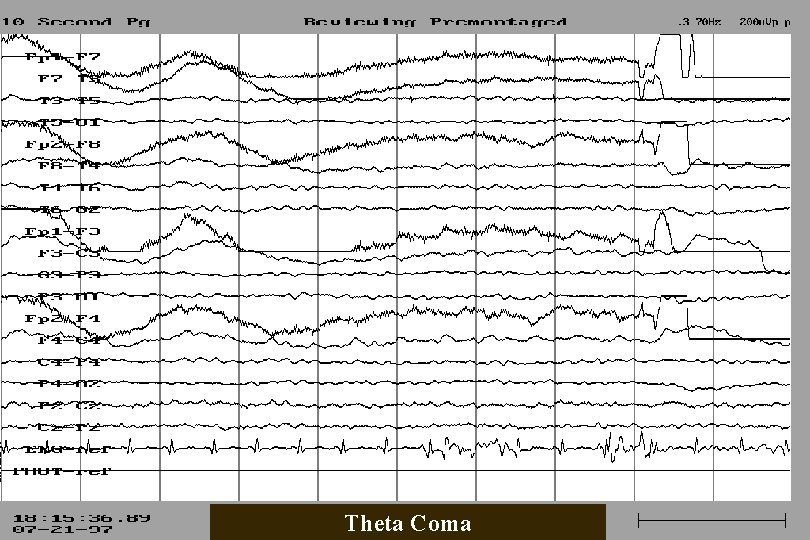
Theta Coma
Other Coma Patterns n Spindle Coma n n n Beta Coma n n Due to lesion at high mesencephaic level If not due to progressive lesion good prognosis Most frequently due to drug intoxication; potentially reversible Delta Coma n n Severe diffuse encephalopathy Reversibility depends on underlying condition
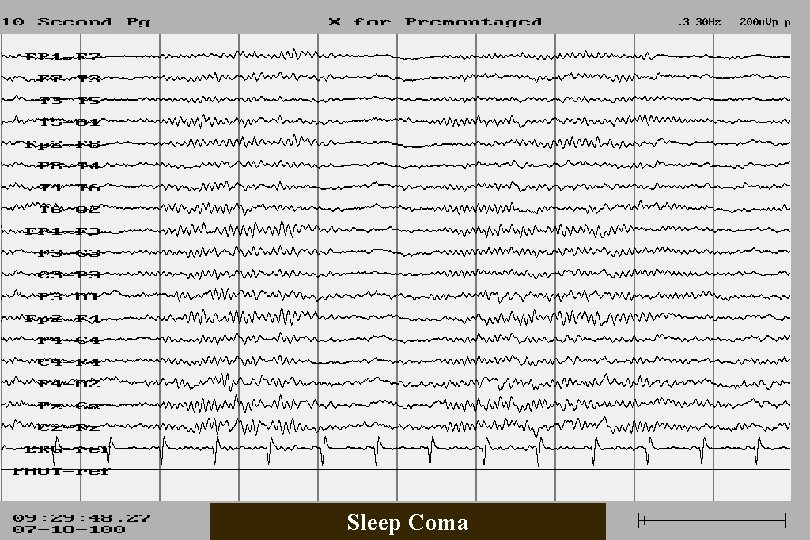
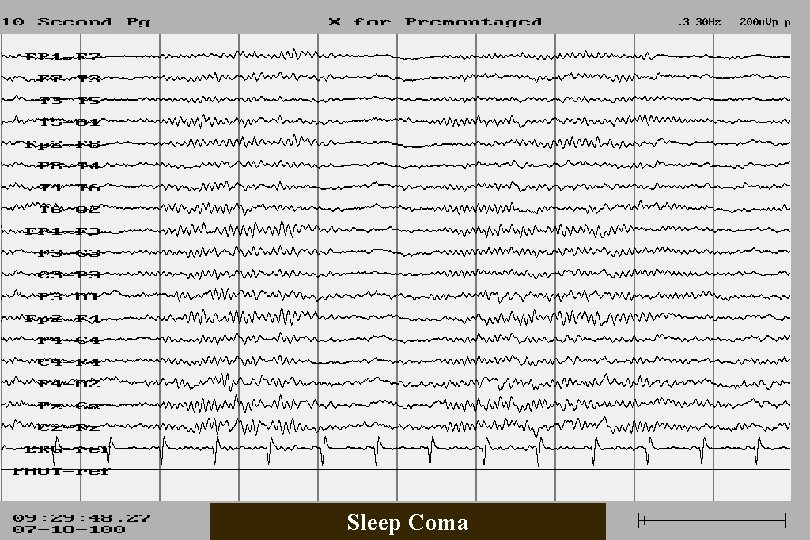
Sleep Coma
Excessive Fast n n n Beta activity of > 50 u. V Present during at least 50% of awake recording Frequently due to sedative medication
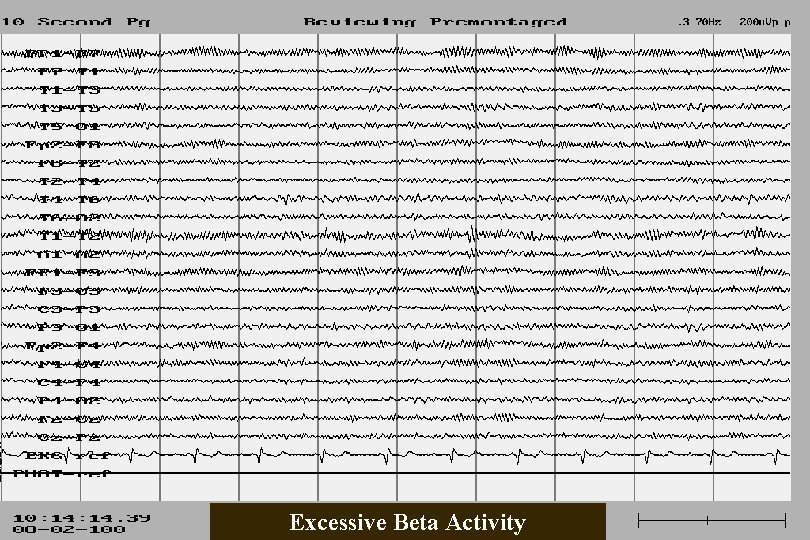
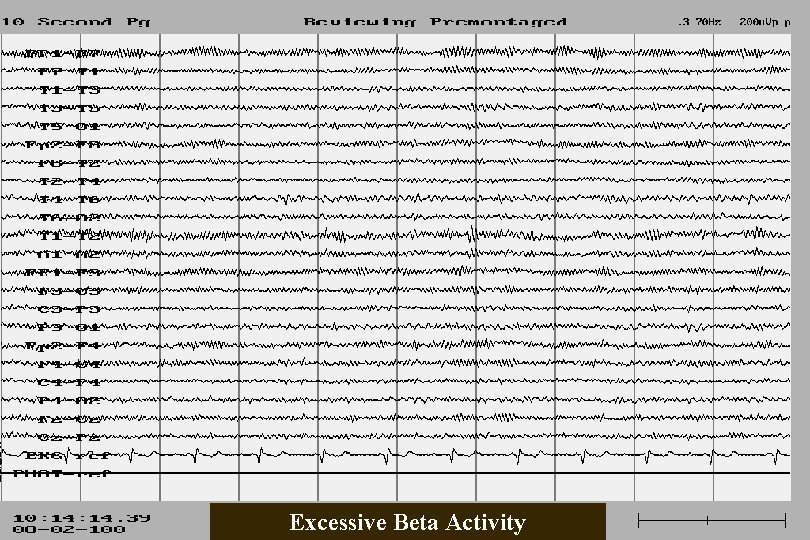
Excessive Beta Activity
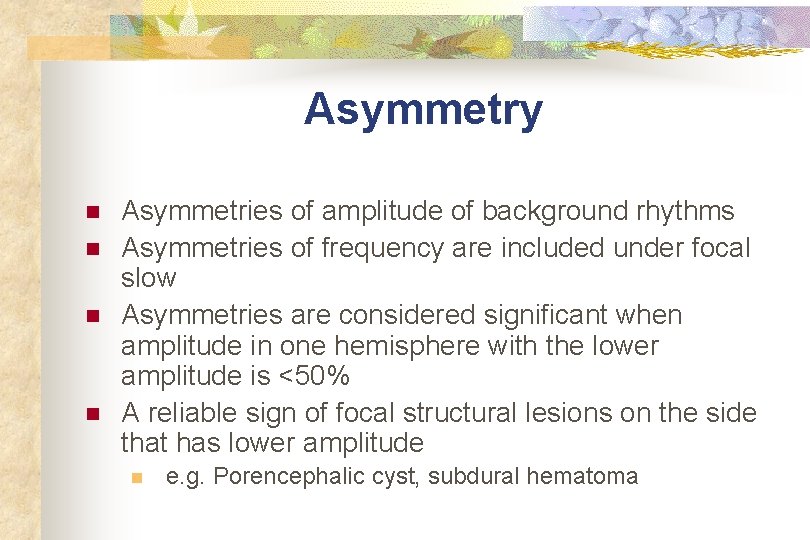
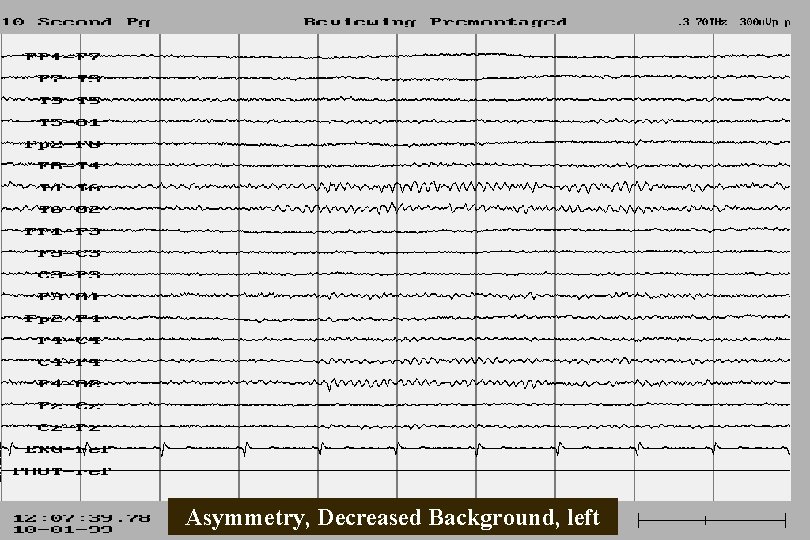
Asymmetry n n Asymmetries of amplitude of background rhythms Asymmetries of frequency are included under focal slow Asymmetries are considered significant when amplitude in one hemisphere with the lower amplitude is <50% A reliable sign of focal structural lesions on the side that has lower amplitude n e. g. Porencephalic cyst, subdural hematoma
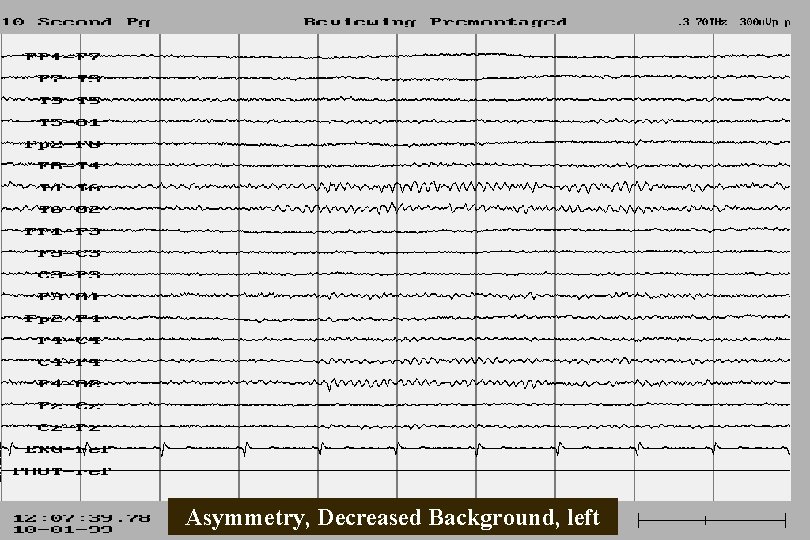
Asymmetry, Decreased Background, left
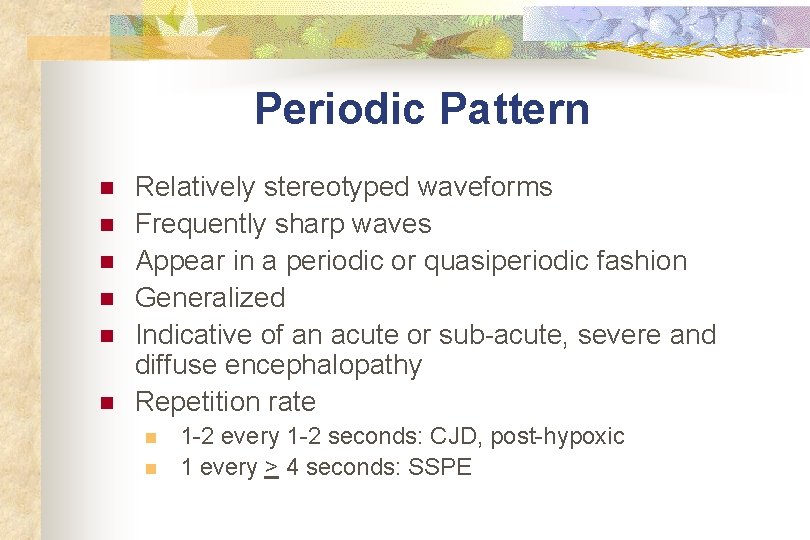
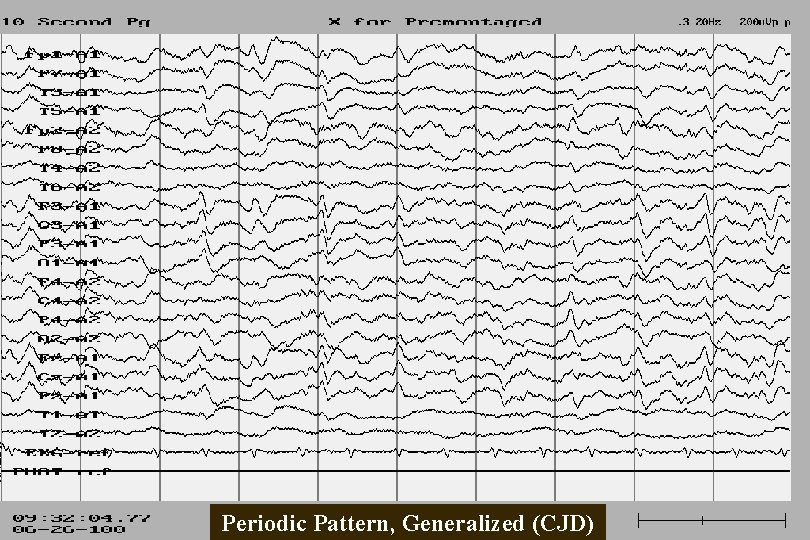
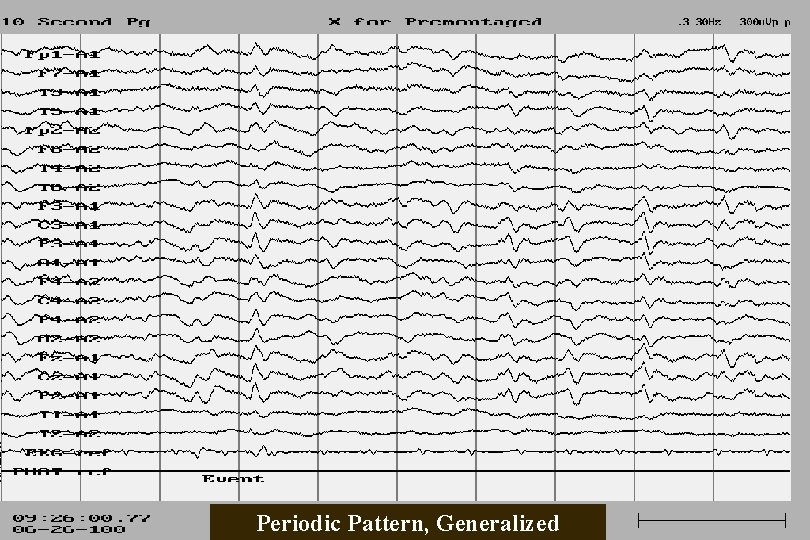
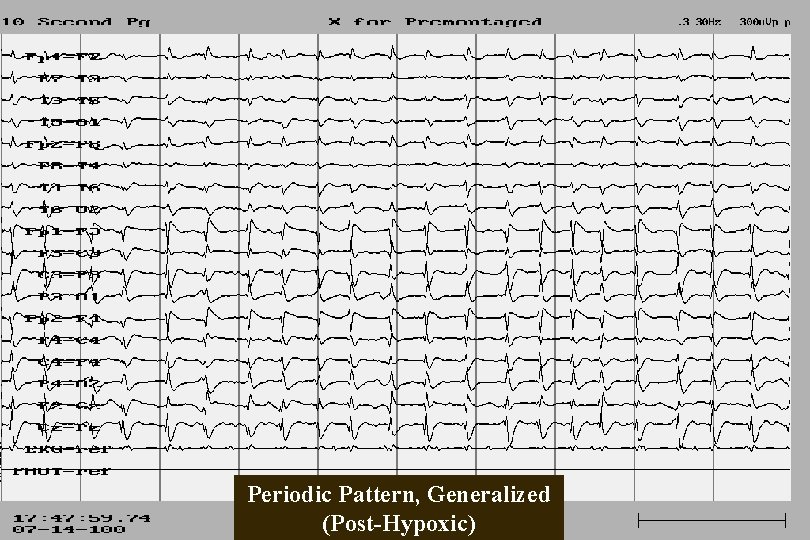
Periodic Pattern n n n Relatively stereotyped waveforms Frequently sharp waves Appear in a periodic or quasiperiodic fashion Generalized Indicative of an acute or sub-acute, severe and diffuse encephalopathy Repetition rate n n 1 -2 every 1 -2 seconds: CJD, post-hypoxic 1 every > 4 seconds: SSPE
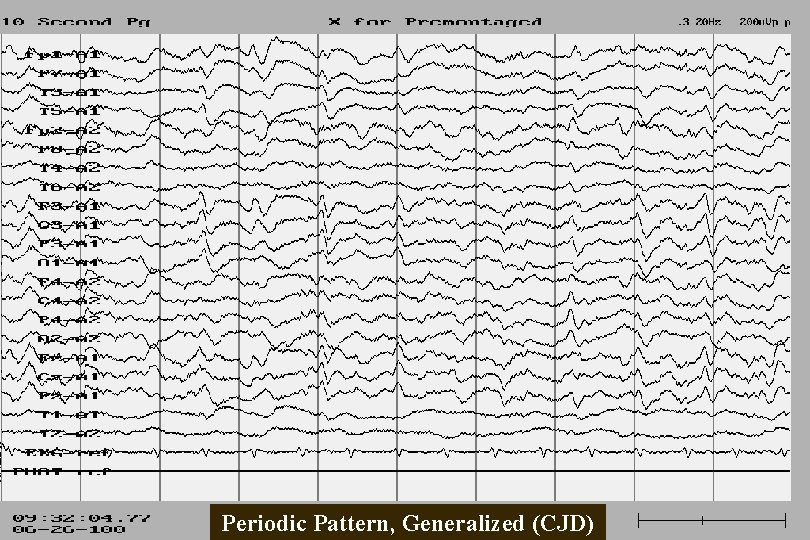
Periodic Pattern, Generalized (CJD)
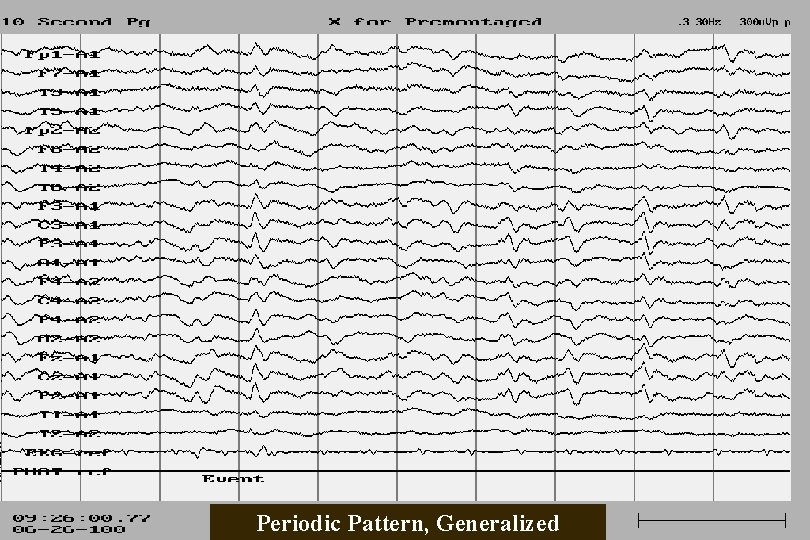
Periodic Pattern, Generalized
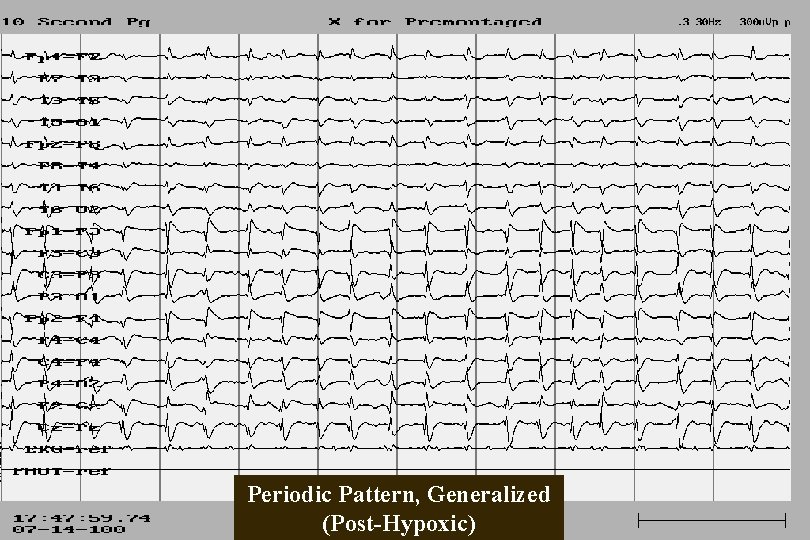
Periodic Pattern, Generalized (Post-Hypoxic)
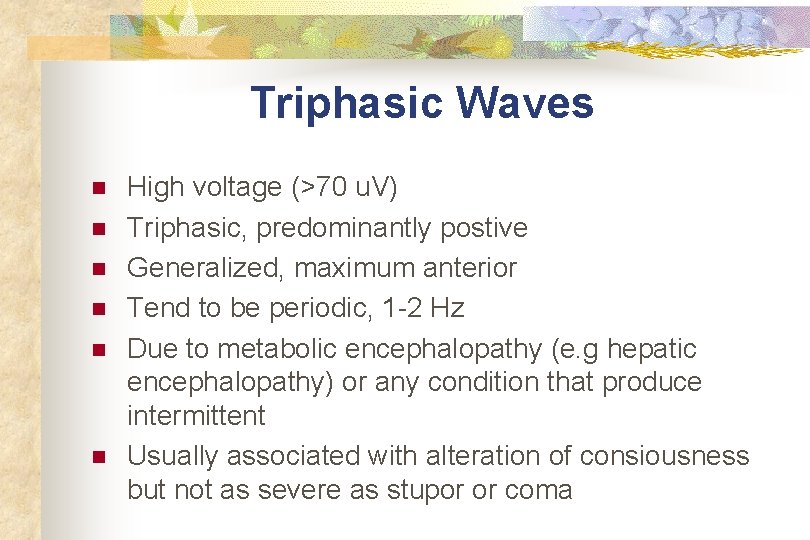
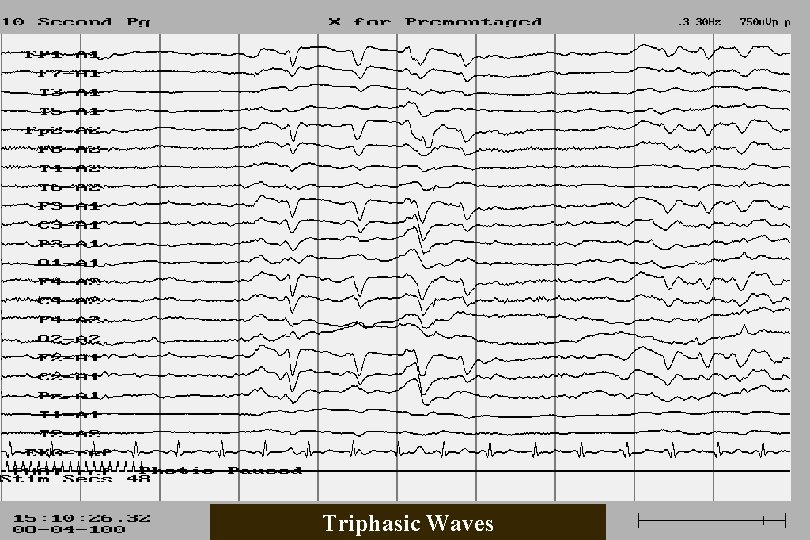
Triphasic Waves n n n High voltage (>70 u. V) Triphasic, predominantly postive Generalized, maximum anterior Tend to be periodic, 1 -2 Hz Due to metabolic encephalopathy (e. g hepatic encephalopathy) or any condition that produce intermittent Usually associated with alteration of consiousness but not as severe as stupor or coma
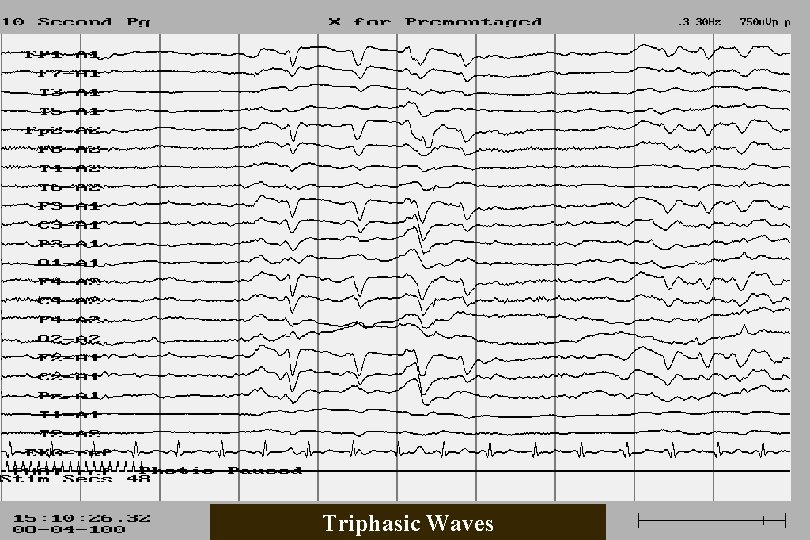
Triphasic Waves
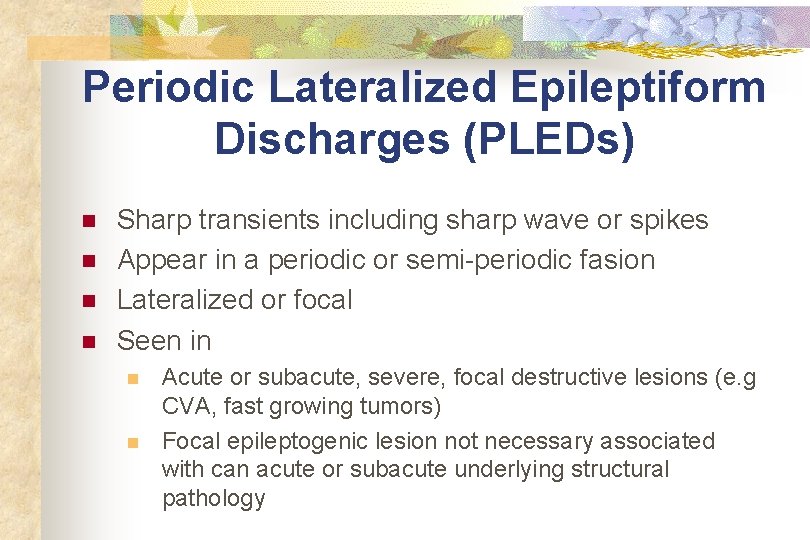
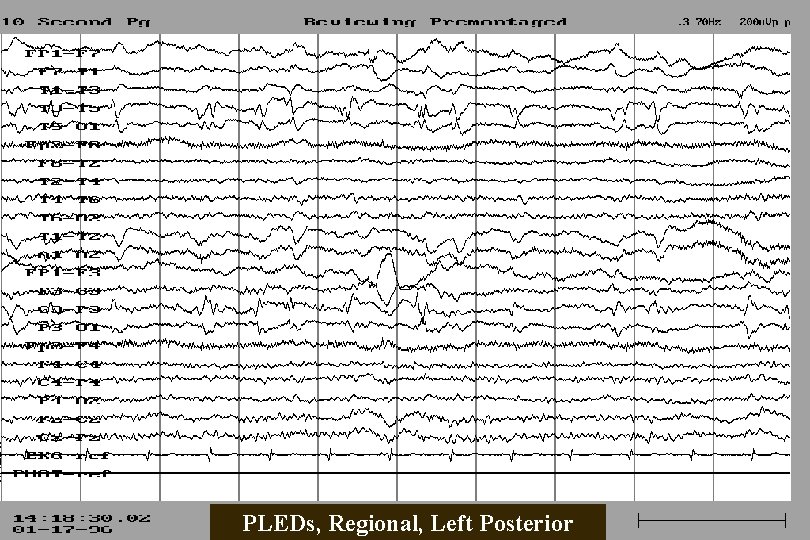
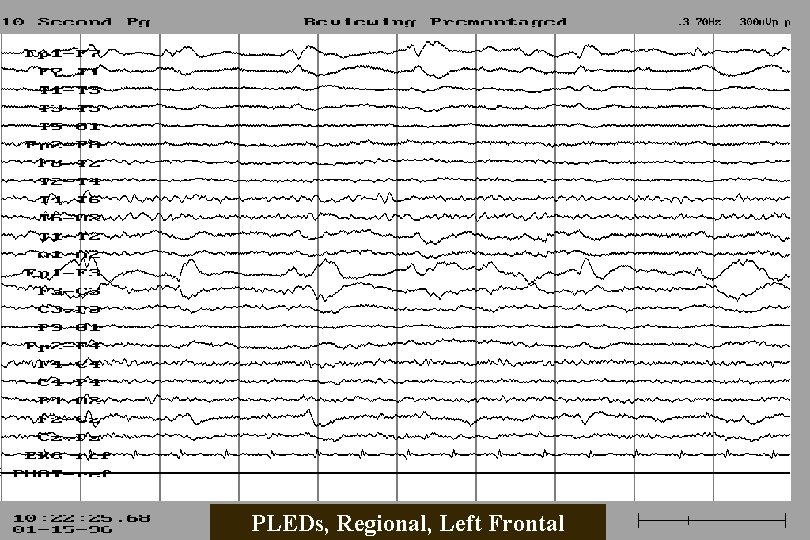
Periodic Lateralized Epileptiform Discharges (PLEDs) n n Sharp transients including sharp wave or spikes Appear in a periodic or semi-periodic fasion Lateralized or focal Seen in n n Acute or subacute, severe, focal destructive lesions (e. g CVA, fast growing tumors) Focal epileptogenic lesion not necessary associated with can acute or subacute underlying structural pathology
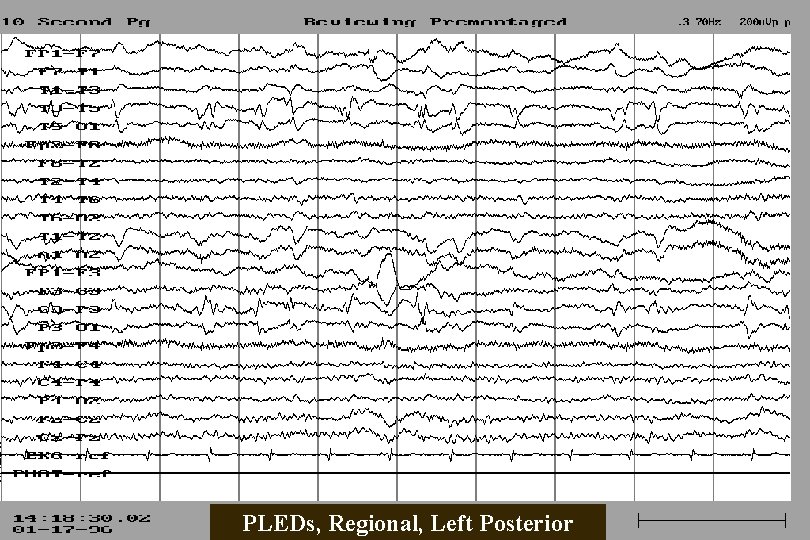
PLEDs, Regional, Left Posterior
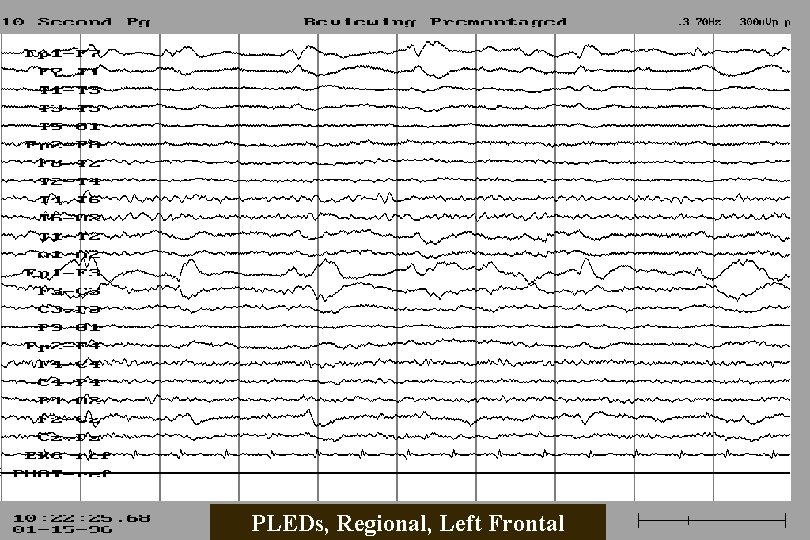
PLEDs, Regional, Left Frontal
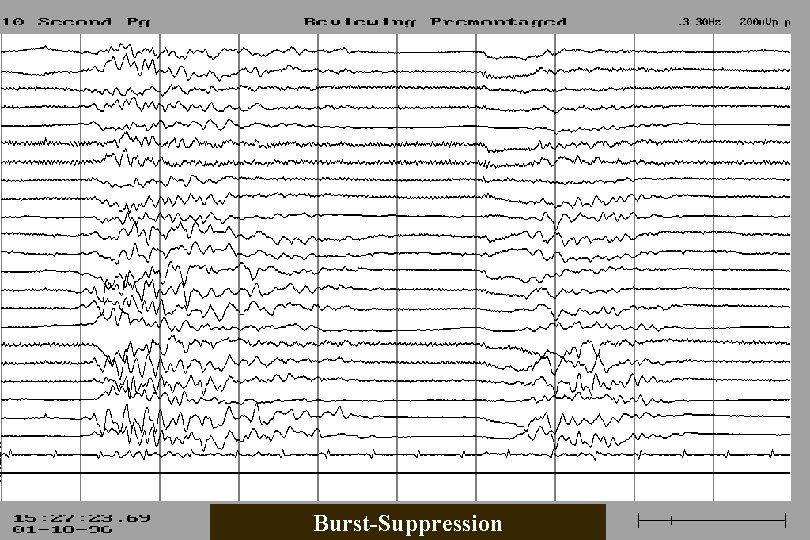
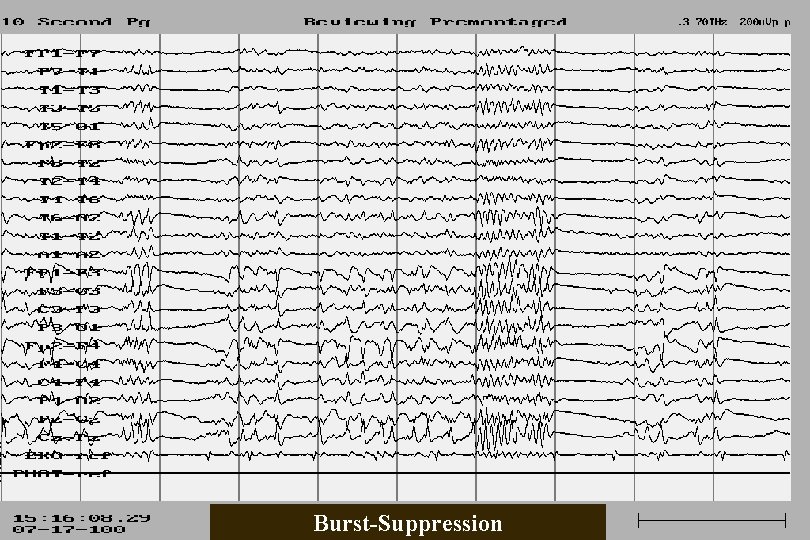
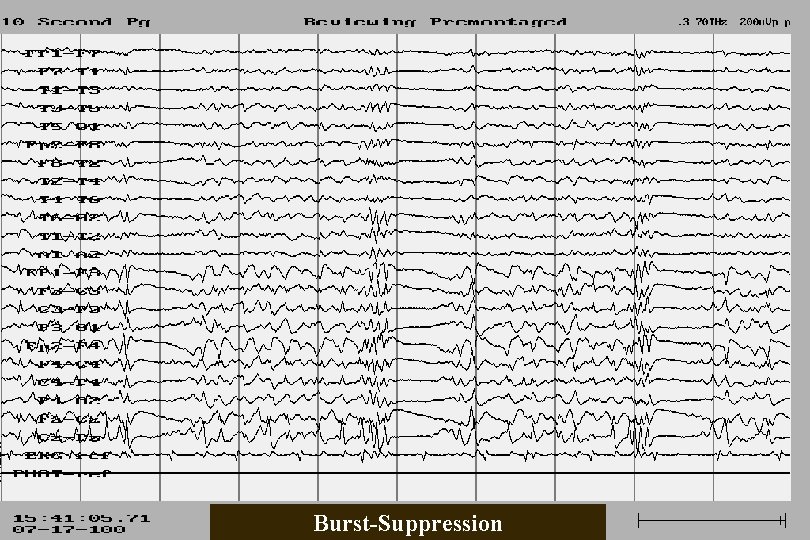
Burst Suppression n n A subgroup of periodic patterns in which activity between complexes is suppressed Generalized Seen in extremely severe toxic or anoxic encephalopathy; may precede electrocerebral inactivity Patients always in stupor or coma
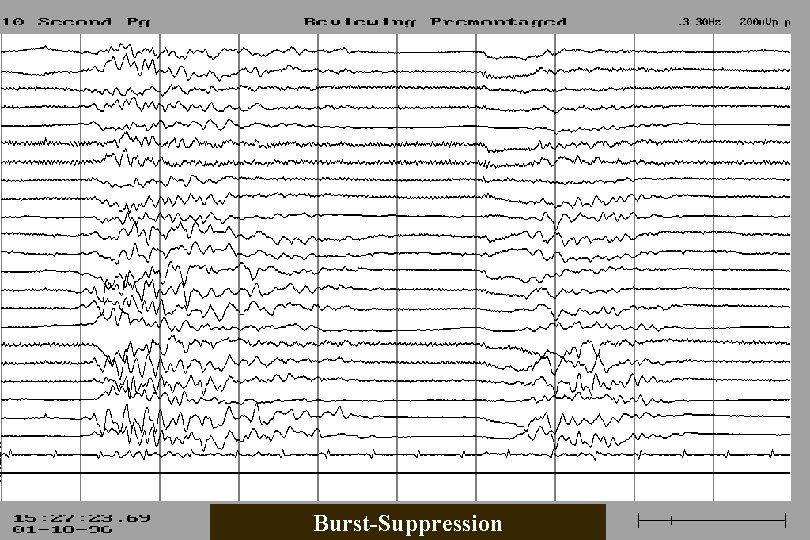
Burst-Suppression
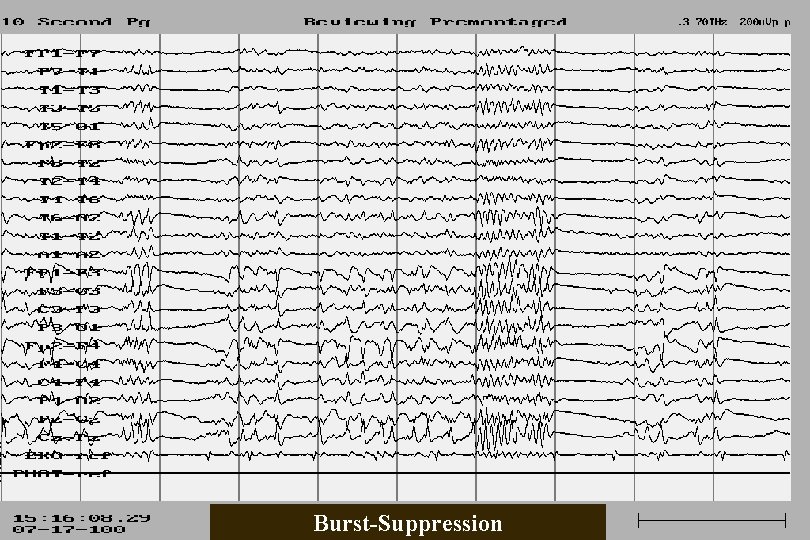
Burst-Suppression
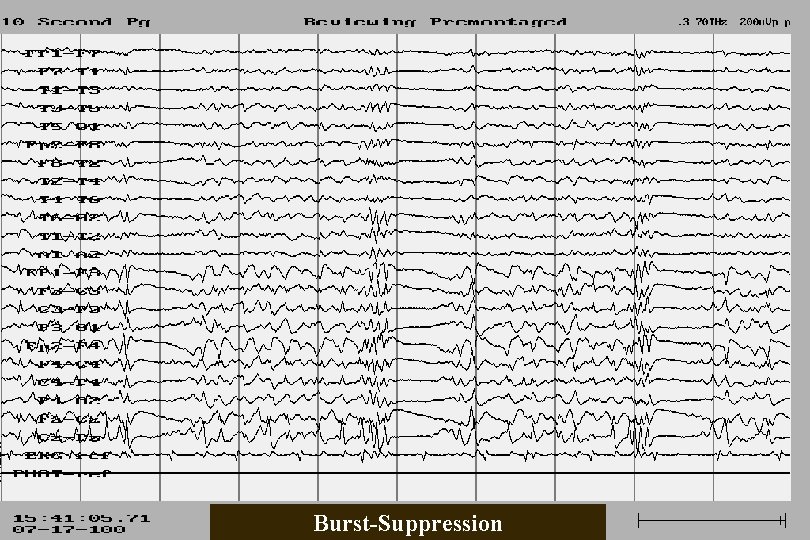
Burst-Suppression
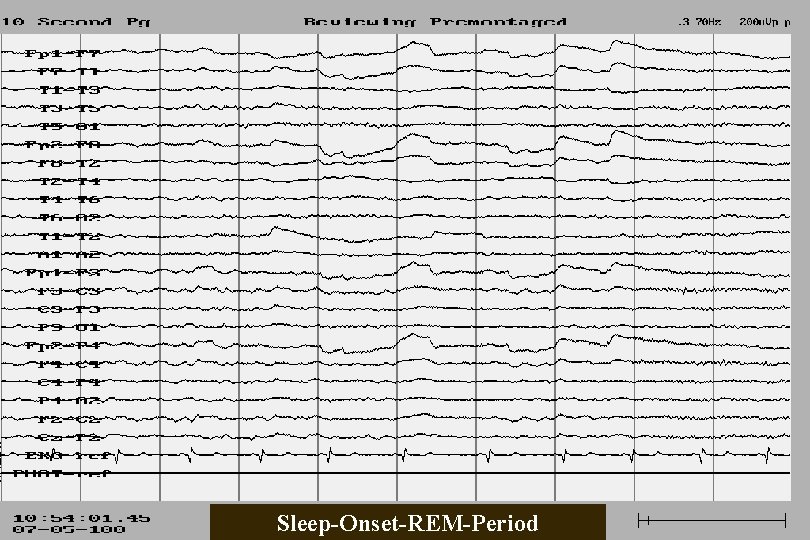
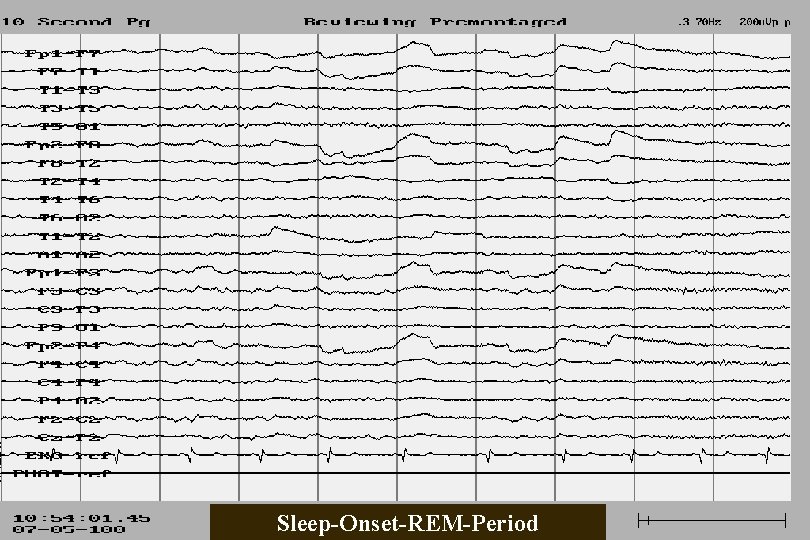
Sleep-Onset-REM-Period
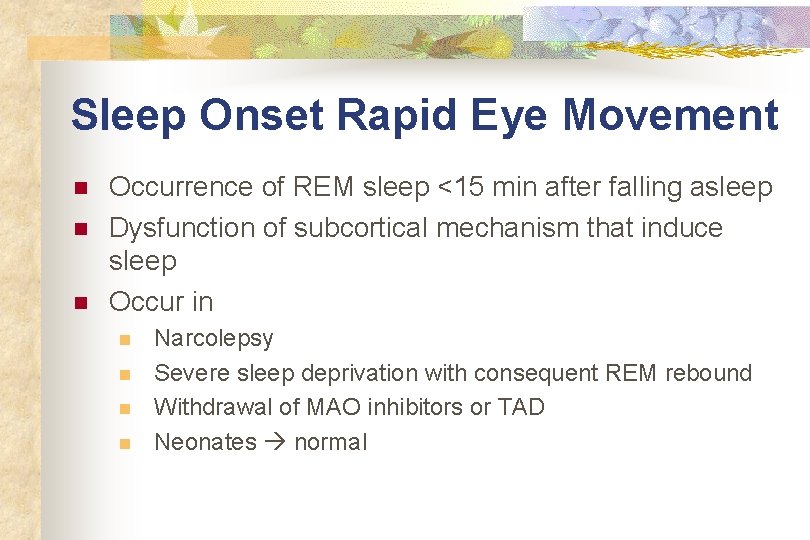
Sleep Onset Rapid Eye Movement n n n Occurrence of REM sleep <15 min after falling asleep Dysfunction of subcortical mechanism that induce sleep Occur in n n Narcolepsy Severe sleep deprivation with consequent REM rebound Withdrawal of MAO inhibitors or TAD Neonates normal