NonDiabetic Hypoglycemia Medical Grand Rounds May 14 2004

Non-Diabetic Hypoglycemia Medical Grand Rounds May 14, 2004 Dr. William Harper Assistant Professor of Medicine, Mc. Master University. Endocrinologist, Hamilton General Hospital www. drharper. ca
Hypoglycemia: case based Diagnostic approach to hypoglycemia 2. Iatrogenic hypoglycemia 3. Tumor-associated hypoglycemia 1.
Case 1 l 18 year old male l Prior ADHD, school suspension-fighting l LOC, SZ, CBG 1. 8 m. M l Stepfather T 2 DM: glyburide l Grandfather T 2 DM: insulin
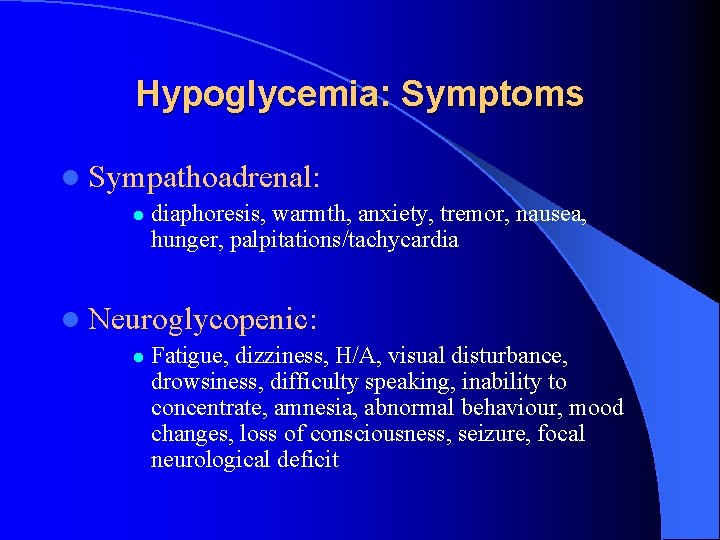
Hypoglycemia: Symptoms l Sympathoadrenal: l diaphoresis, warmth, anxiety, tremor, nausea, hunger, palpitations/tachycardia l Neuroglycopenic: l Fatigue, dizziness, H/A, visual disturbance, drowsiness, difficulty speaking, inability to concentrate, amnesia, abnormal behaviour, mood changes, loss of consciousness, seizure, focal neurological deficit
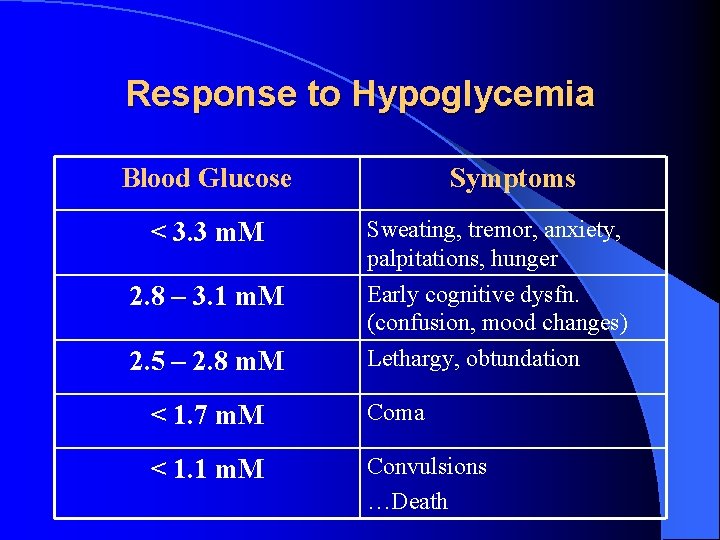
Response to Hypoglycemia Blood Glucose < 3. 3 m. M 2. 8 – 3. 1 m. M 2. 5 – 2. 8 m. M Symptoms Sweating, tremor, anxiety, palpitations, hunger Early cognitive dysfn. (confusion, mood changes) Lethargy, obtundation < 1. 7 m. M Coma < 1. 1 m. M Convulsions …Death
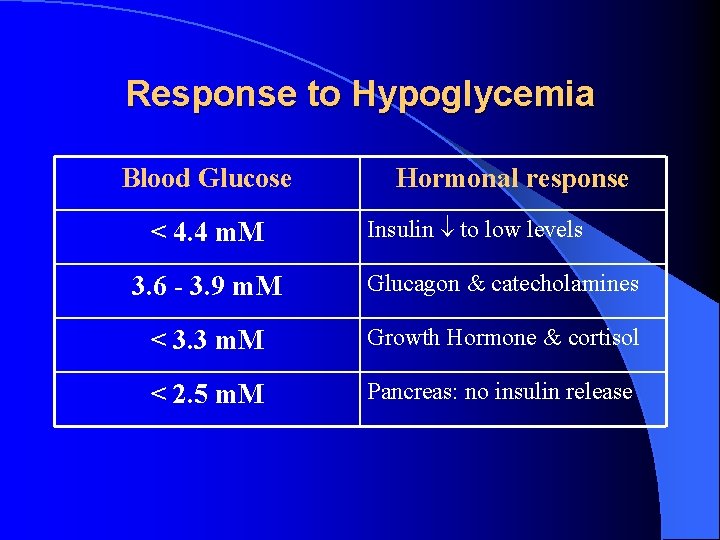
Response to Hypoglycemia Blood Glucose < 4. 4 m. M Hormonal response Insulin to low levels 3. 6 - 3. 9 m. M Glucagon & catecholamines < 3. 3 m. M Growth Hormone & cortisol < 2. 5 m. M Pancreas: no insulin release
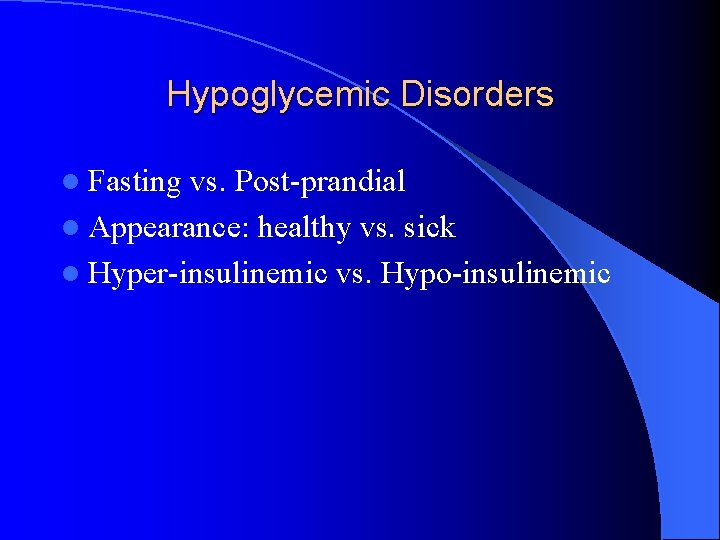
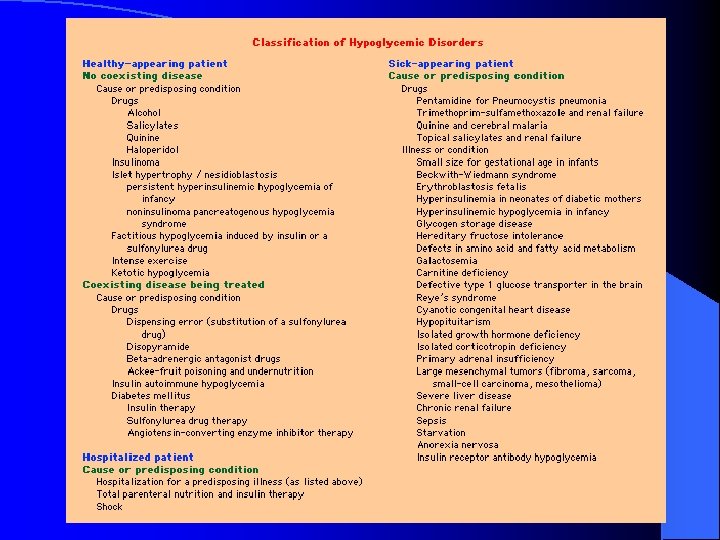
Hypoglycemic Disorders l Fasting vs. Post-prandial l Appearance: healthy vs. sick l Hyper-insulinemic vs. Hypo-insulinemic
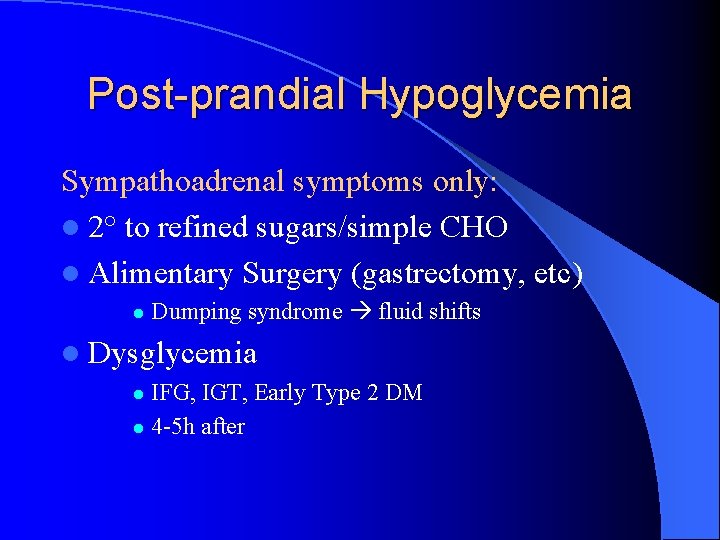
Post-prandial Hypoglycemia Sympathoadrenal symptoms only: l 2° to refined sugars/simple CHO l Alimentary Surgery (gastrectomy, etc) l Dumping syndrome fluid shifts l Dysglycemia IFG, IGT, Early Type 2 DM l 4 -5 h after l
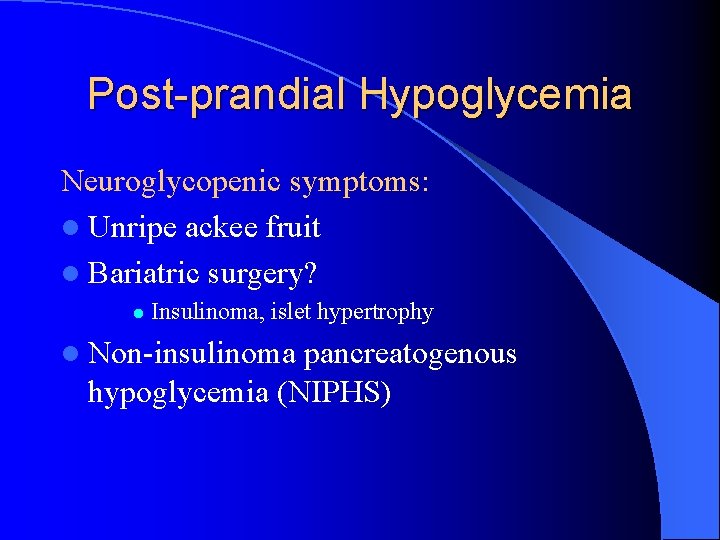
Post-prandial Hypoglycemia Neuroglycopenic symptoms: l Unripe ackee fruit l Bariatric surgery? l Insulinoma, islet hypertrophy l Non-insulinoma pancreatogenous hypoglycemia (NIPHS)
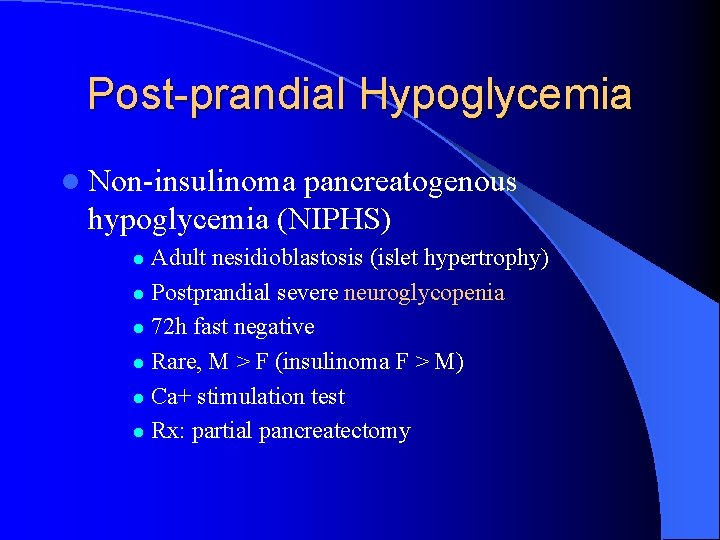
Post-prandial Hypoglycemia l Non-insulinoma pancreatogenous hypoglycemia (NIPHS) Adult nesidioblastosis (islet hypertrophy) l Postprandial severe neuroglycopenia l 72 h fast negative l Rare, M > F (insulinoma F > M) l Ca+ stimulation test l Rx: partial pancreatectomy l
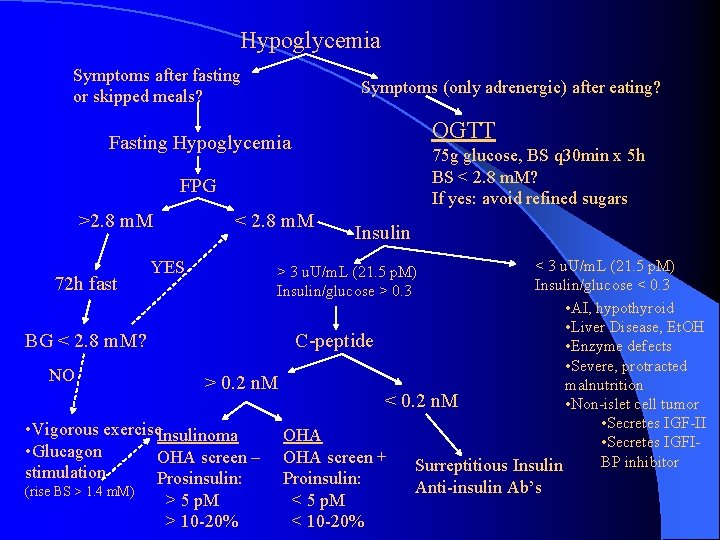
Hypoglycemia Symptoms after fasting or skipped meals? Symptoms (only adrenergic) after eating? OGTT Fasting Hypoglycemia 75 g glucose, BS q 30 min x 5 h BS < 2. 8 m. M? If yes: avoid refined sugars FPG >2. 8 m. M < 2. 8 m. M Insulin < 3 u. U/m. L (21. 5 p. M) 72 h fast Insulin/glucose < 0. 3 • AI, hypothyroid • Liver Disease, Et. OH BG < 2. 8 m. M? C-peptide • Enzyme defects • Severe, protracted NO > 0. 2 n. M malnutrition < 0. 2 n. M • Non-islet cell tumor • Secretes IGF-II • Vigorous exercise. Insulinoma OHA • Secretes IGFI • Glucagon OHA screen – OHA screen + BP inhibitor Surreptitious Insulin YES stimulation (rise BS > 1. 4 m. M) Prosinsulin: > 5 p. M > 10 -20% > 3 u. U/m. L (21. 5 p. M) Insulin/glucose > 0. 3 Proinsulin: < 5 p. M < 10 -20% Anti-insulin Ab’s
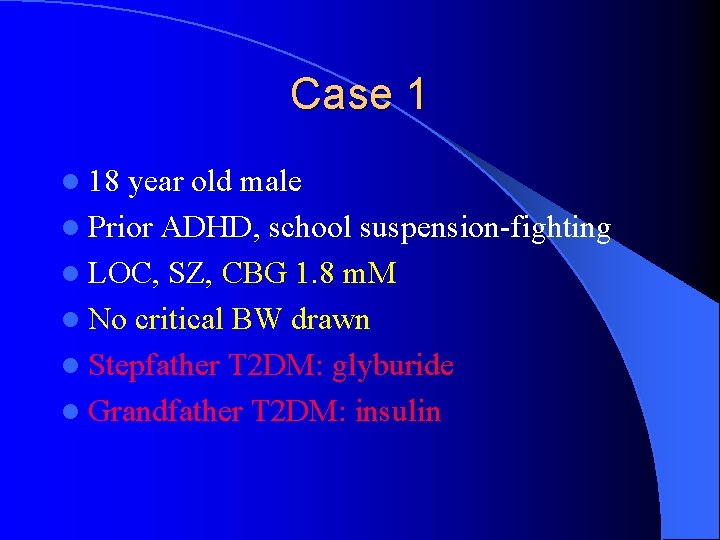
Case 1 l 18 year old male l Prior ADHD, school suspension-fighting l LOC, SZ, CBG 1. 8 m. M l No critical BW drawn l Stepfather T 2 DM: glyburide l Grandfather T 2 DM: insulin
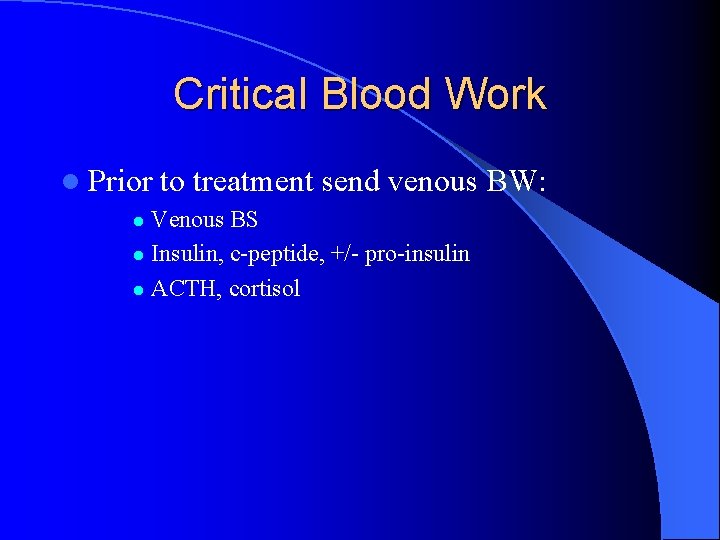
Critical Blood Work l Prior to treatment send venous BW: Venous BS l Insulin, c-peptide, +/- pro-insulin l ACTH, cortisol l
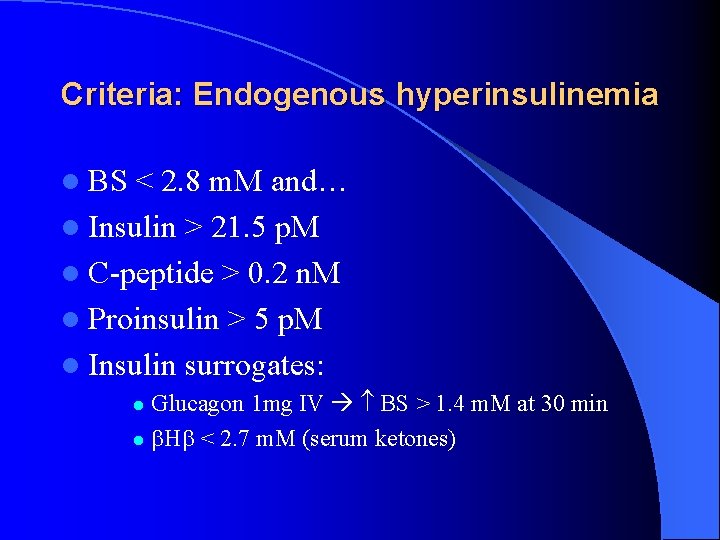
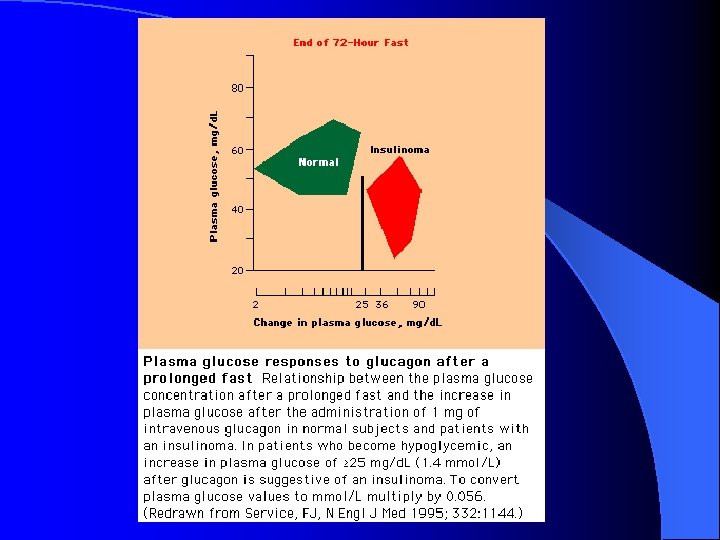
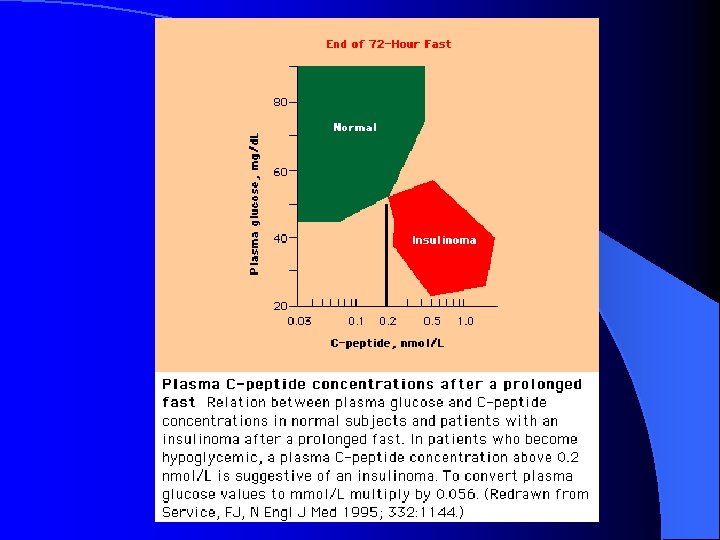
Criteria: Endogenous hyperinsulinemia l BS < 2. 8 m. M and… l Insulin > 21. 5 p. M l C-peptide > 0. 2 n. M l Proinsulin > 5 p. M l Insulin surrogates: Glucagon 1 mg IV BS > 1. 4 m. M at 30 min l H < 2. 7 m. M (serum ketones) l
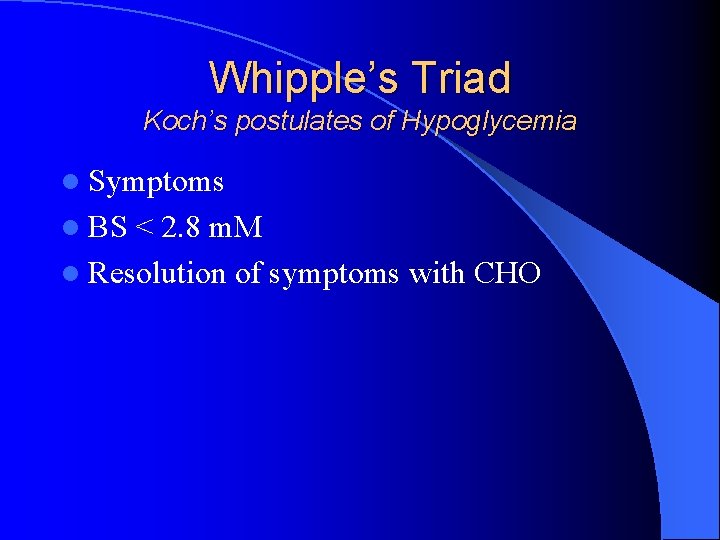
Whipple’s Triad Koch’s postulates of Hypoglycemia l Symptoms l BS < 2. 8 m. M l Resolution of symptoms with CHO
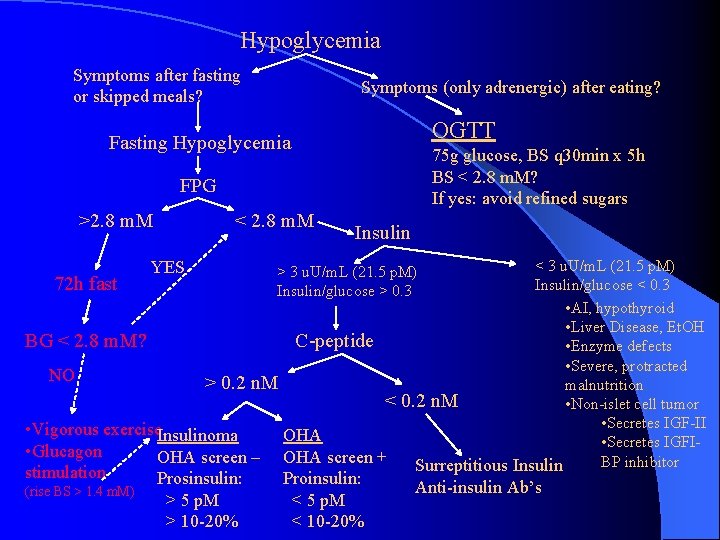
Hypoglycemia Symptoms after fasting or skipped meals? Symptoms (only adrenergic) after eating? OGTT Fasting Hypoglycemia 75 g glucose, BS q 30 min x 5 h BS < 2. 8 m. M? If yes: avoid refined sugars FPG >2. 8 m. M < 2. 8 m. M Insulin < 3 u. U/m. L (21. 5 p. M) 72 h fast Insulin/glucose < 0. 3 • AI, hypothyroid • Liver Disease, Et. OH BG < 2. 8 m. M? C-peptide • Enzyme defects • Severe, protracted NO > 0. 2 n. M malnutrition < 0. 2 n. M • Non-islet cell tumor • Secretes IGF-II • Vigorous exercise. Insulinoma OHA • Secretes IGFI • Glucagon OHA screen – OHA screen + BP inhibitor Surreptitious Insulin YES stimulation (rise BS > 1. 4 m. M) Prosinsulin: > 5 p. M > 10 -20% > 3 u. U/m. L (21. 5 p. M) Insulin/glucose > 0. 3 Proinsulin: < 5 p. M < 10 -20% Anti-insulin Ab’s
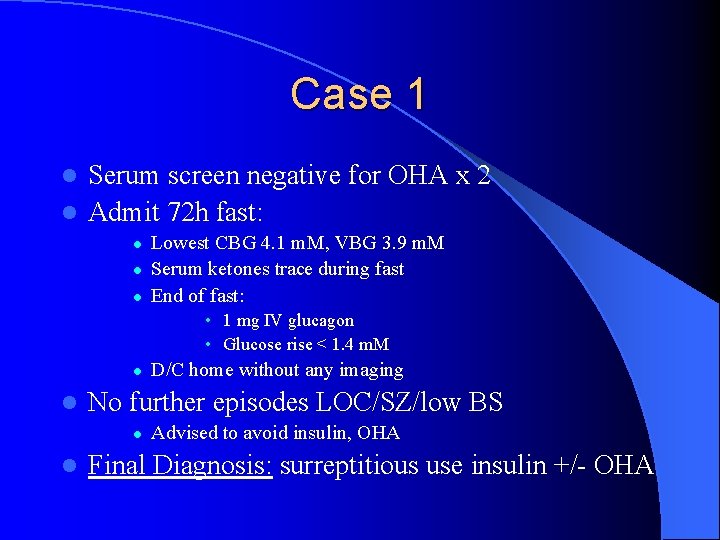
Case 1 Serum screen negative for OHA x 2 l Admit 72 h fast: l l Lowest CBG 4. 1 m. M, VBG 3. 9 m. M Serum ketones trace during fast End of fast: • 1 mg IV glucagon • Glucose rise < 1. 4 m. M l l No further episodes LOC/SZ/low BS l l D/C home without any imaging Advised to avoid insulin, OHA Final Diagnosis: surreptitious use insulin +/- OHA
Hypoglycemia: Family Hx of DM? l Access to insulin? l Access to oral hypoglycemia agents?
Case 2 admit with ascites l Known cirrhotic 2° Et. OH, abstinate x 7 y l BS 6 -8 m. M in-hospital until day 14 l Awoke with BS 3. 4 m. M l BS 2. 0 -2. 9 despite + + po CHO intake l Next day BS 1. 5 -1. 9 m. M l D 10 W IV gtt @ 100 -150/h x 2 -3 d l 71 M,
Case 2 l Meds: amiodarone, altace, ASA, lasix, aldactone, cipro, ativan qhs PRN l AST, ALT, GGT mildly elevated l Albumin 39, INR 1. 2 l Critical BW: Venous BS 1. 5 m. M l Insulin 317 p. M, C-peptide 4. 0 n. M l ACTH 7 p. M, cortisol 751 n. M l
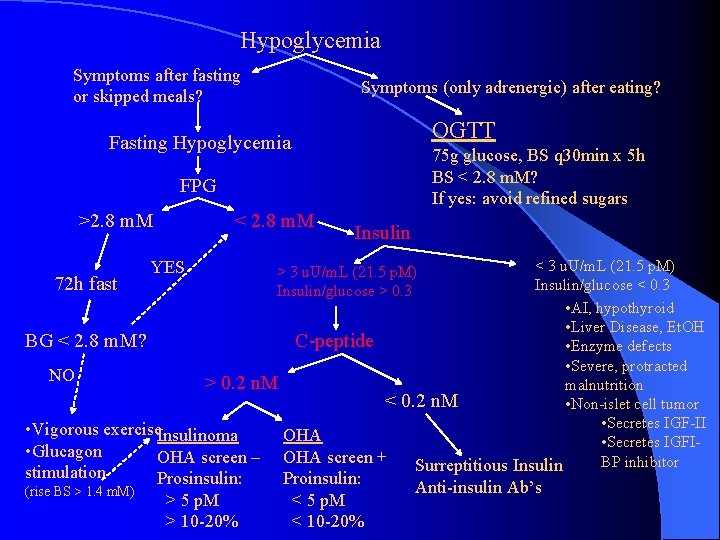
Hypoglycemia Symptoms after fasting or skipped meals? Symptoms (only adrenergic) after eating? OGTT Fasting Hypoglycemia 75 g glucose, BS q 30 min x 5 h BS < 2. 8 m. M? If yes: avoid refined sugars FPG >2. 8 m. M < 2. 8 m. M Insulin < 3 u. U/m. L (21. 5 p. M) 72 h fast Insulin/glucose < 0. 3 • AI, hypothyroid • Liver Disease, Et. OH BG < 2. 8 m. M? C-peptide • Enzyme defects • Severe, protracted NO > 0. 2 n. M malnutrition < 0. 2 n. M • Non-islet cell tumor • Secretes IGF-II • Vigorous exercise. Insulinoma OHA • Secretes IGFI • Glucagon OHA screen – OHA screen + BP inhibitor Surreptitious Insulin YES stimulation (rise BS > 1. 4 m. M) Prosinsulin: > 5 p. M > 10 -20% > 3 u. U/m. L (21. 5 p. M) Insulin/glucose > 0. 3 Proinsulin: < 5 p. M < 10 -20% Anti-insulin Ab’s
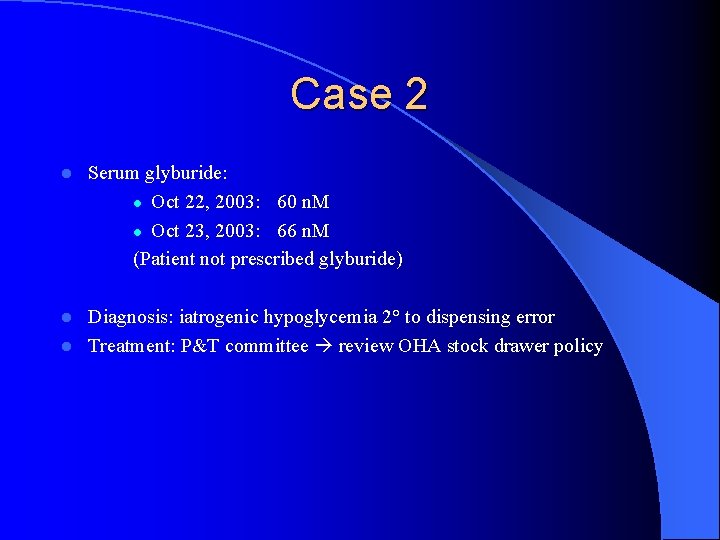
Case 2 l Serum glyburide: l Oct 22, 2003: 60 n. M l Oct 23, 2003: 66 n. M (Patient not prescribed glyburide) Diagnosis: iatrogenic hypoglycemia 2° to dispensing error l Treatment: P&T committee review OHA stock drawer policy l
Case 3 l 49 M, Fall 2002: LBP & abdominal mass l Retroperitoneal seminoma l Chemotherapy: l Etoposide, Cisplatinum, Bleomycin l Tumor: good response
Case 3 anorexia l Spells of bizzare behaviour, confusion, lethargy l Random BS 3. 6 m. M, Hb. A 1 c 3. 4% l PHx: 10 y of early AM spells, relieved with snacks/O. J. , weight gain > 100 lbs. l Chemo
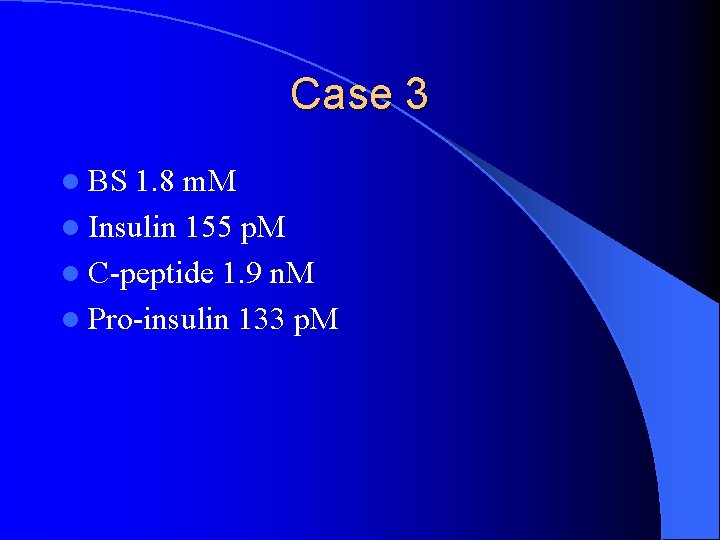
Case 3 l BS 1. 8 m. M l Insulin 155 p. M l C-peptide 1. 9 n. M l Pro-insulin 133 p. M

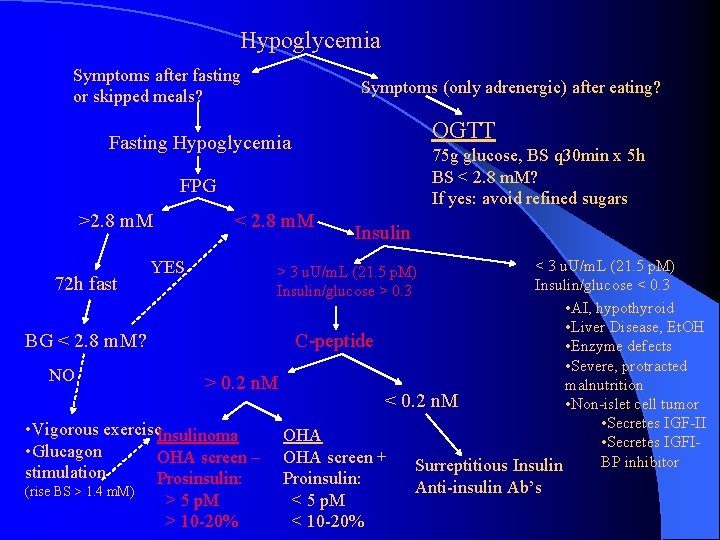
Hypoglycemia Symptoms after fasting or skipped meals? Symptoms (only adrenergic) after eating? OGTT Fasting Hypoglycemia 75 g glucose, BS q 30 min x 5 h BS < 2. 8 m. M? If yes: avoid refined sugars FPG >2. 8 m. M < 2. 8 m. M Insulin < 3 u. U/m. L (21. 5 p. M) 72 h fast Insulin/glucose < 0. 3 • AI, hypothyroid • Liver Disease, Et. OH BG < 2. 8 m. M? C-peptide • Enzyme defects • Severe, protracted NO > 0. 2 n. M malnutrition < 0. 2 n. M • Non-islet cell tumor • Secretes IGF-II • Vigorous exercise. Insulinoma OHA • Secretes IGFI • Glucagon OHA screen – OHA screen + BP inhibitor Surreptitious Insulin YES stimulation (rise BS > 1. 4 m. M) Prosinsulin: > 5 p. M > 10 -20% > 3 u. U/m. L (21. 5 p. M) Insulin/glucose > 0. 3 Proinsulin: < 5 p. M < 10 -20% Anti-insulin Ab’s

Case 3 l Hypoglycemia treated with: Diazoxide l Prednisone (bleomycin lung toxicity) l l ICC of retroperitoneal tumor negative for insulin l CT scan: bulky pancreatic tail l Octreoscan: negative l MRI: tumor in tail of pancreas
Case 3 l Intraoperative U/S: single tumor confirmed at tail of pancreas resected l Postop: no further spells, weight loss l MOT contacted for license resinstatement
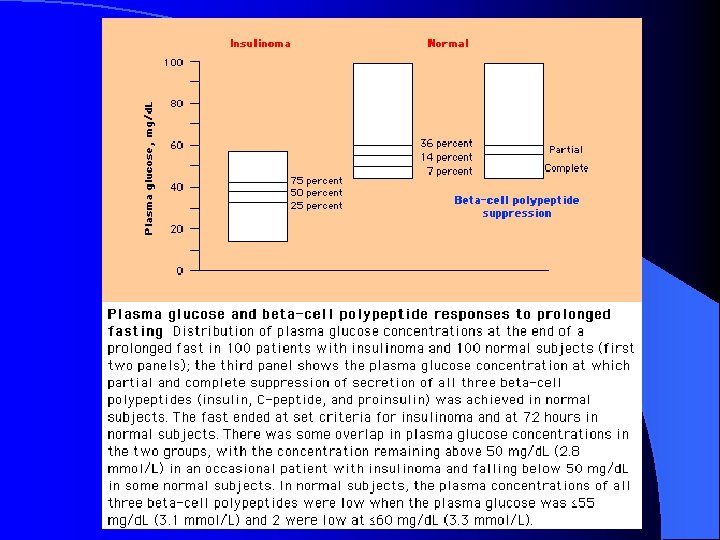
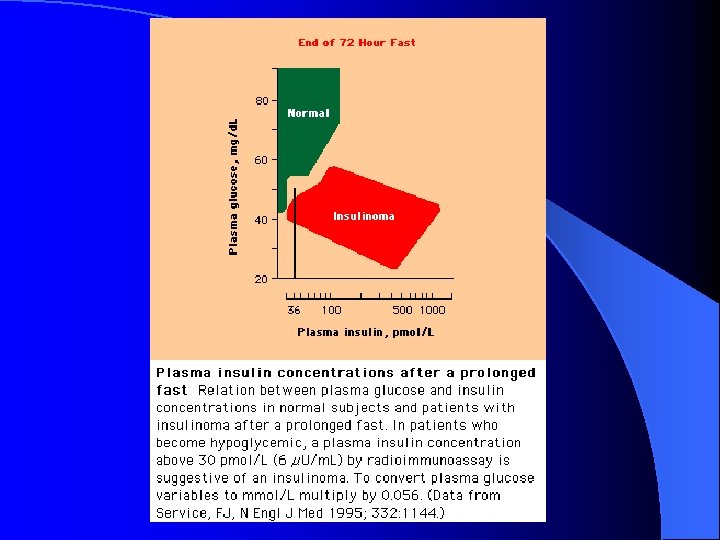
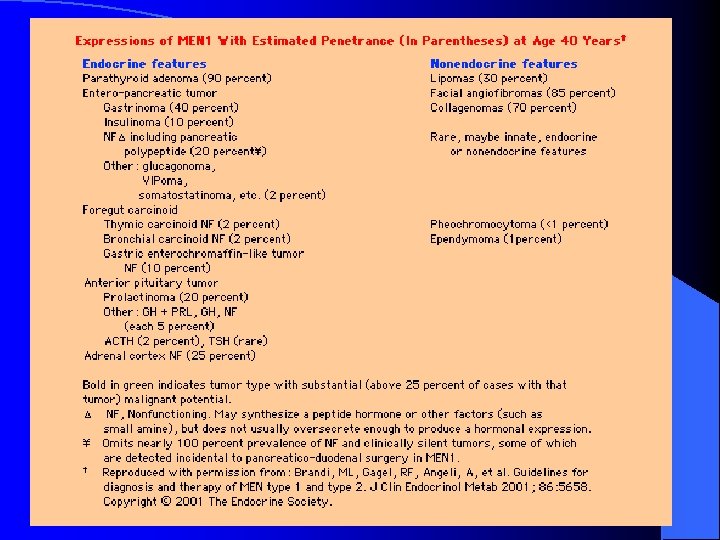
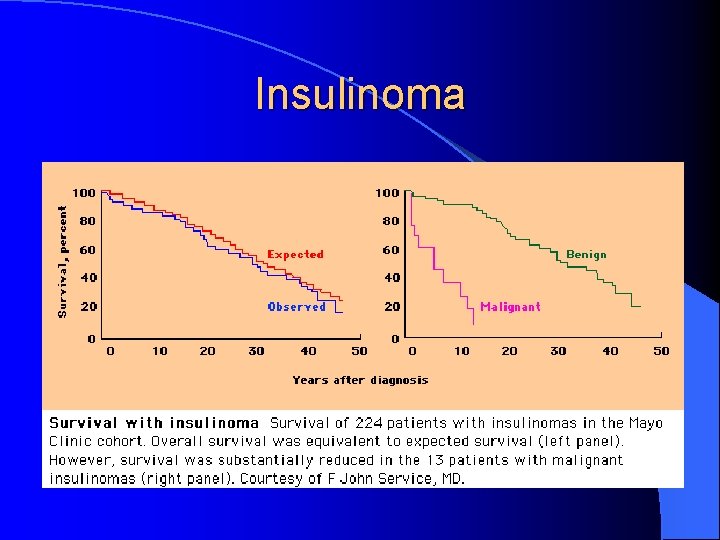
Insulinoma l Rare l neuroendocrine tumor of pancreas 4 cases/million person-years l Originating outside pancreas: 1 -2 cases reports only (cervical cancer) l 59% female l Most (80 -90%) benign l Sporadic or part of MEN-1
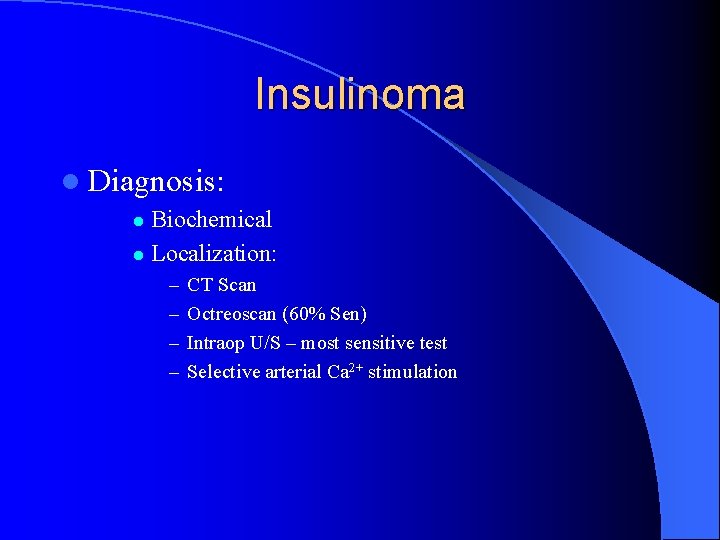
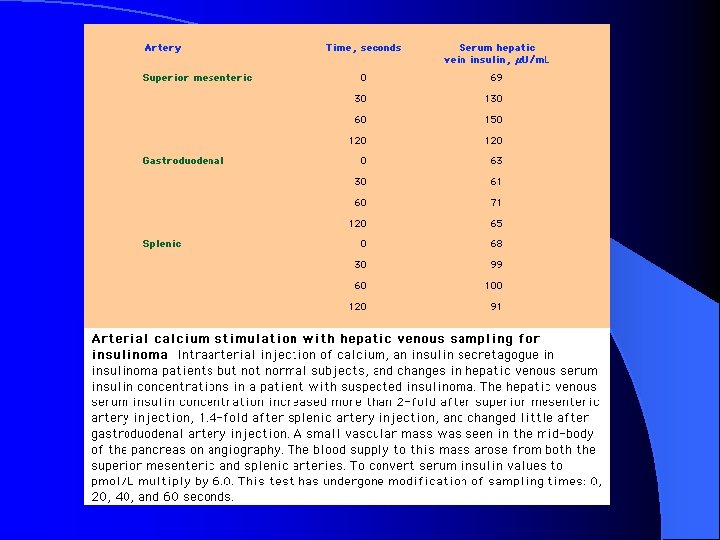
Insulinoma l Diagnosis: Biochemical l Localization: l – – CT Scan Octreoscan (60% Sen) Intraop U/S – most sensitive test Selective arterial Ca 2+ stimulation
Insulinoma
Insulinoma l Treatment: Surgical resection l Diazoxide l Octreotide l Inteferon alpha l Malignant: l • Octreotide-idium 111 • Chemo: streptozozin, doxorubicin
Case 4 l 57 M, well until Oct 2003 l Transient spells: drowsiness, vertigo or dysequilibrium l No relationship with food l Florida over the winter… l Mar 5, 04: felt drunk despite no Et. OH, went to sleep early, next AM was unable to be aroused
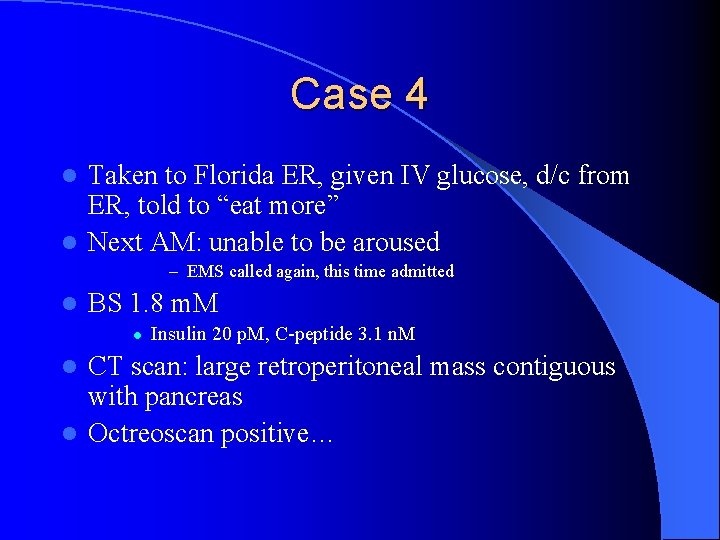
Case 4 Taken to Florida ER, given IV glucose, d/c from ER, told to “eat more” l Next AM: unable to be aroused l – EMS called again, this time admitted l BS 1. 8 m. M l Insulin 20 p. M, C-peptide 3. 1 n. M CT scan: large retroperitoneal mass contiguous with pancreas l Octreoscan positive… l
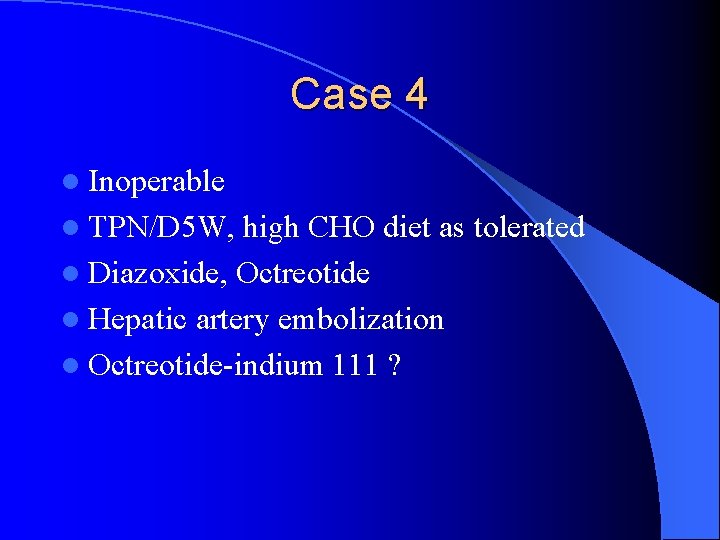
Case 4 l Inoperable l TPN/D 5 W, high CHO diet as tolerated l Diazoxide, Octreotide l Hepatic artery embolization l Octreotide-indium 111 ?
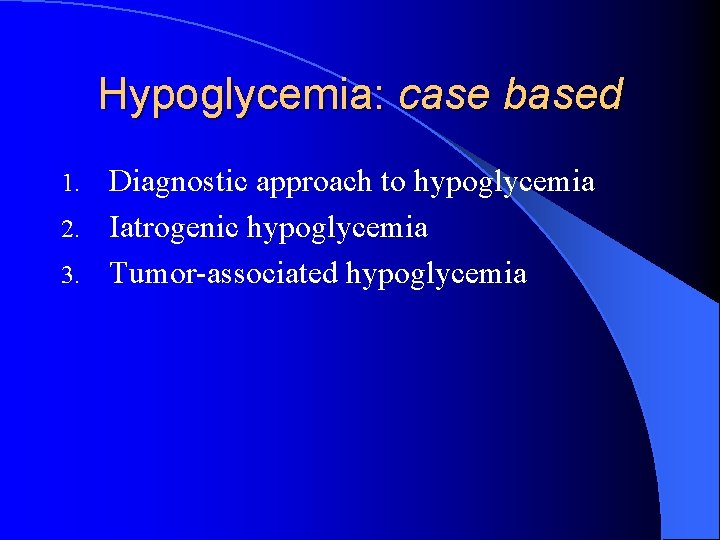
Hypoglycemia: case based Diagnostic approach to hypoglycemia 2. Iatrogenic hypoglycemia 3. Tumor-associated hypoglycemia 1.
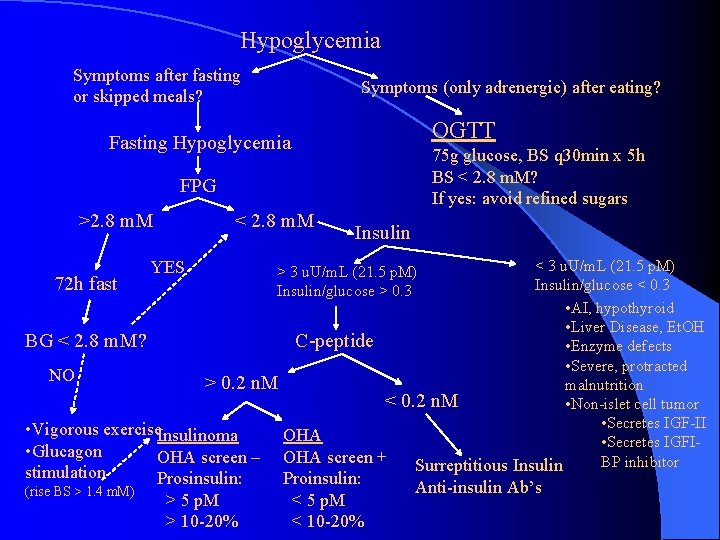
Hypoglycemia Symptoms after fasting or skipped meals? Symptoms (only adrenergic) after eating? OGTT Fasting Hypoglycemia 75 g glucose, BS q 30 min x 5 h BS < 2. 8 m. M? If yes: avoid refined sugars FPG >2. 8 m. M < 2. 8 m. M Insulin < 3 u. U/m. L (21. 5 p. M) 72 h fast Insulin/glucose < 0. 3 • AI, hypothyroid • Liver Disease, Et. OH BG < 2. 8 m. M? C-peptide • Enzyme defects • Severe, protracted NO > 0. 2 n. M malnutrition < 0. 2 n. M • Non-islet cell tumor • Secretes IGF-II • Vigorous exercise. Insulinoma OHA • Secretes IGFI • Glucagon OHA screen – OHA screen + BP inhibitor Surreptitious Insulin YES stimulation (rise BS > 1. 4 m. M) Prosinsulin: > 5 p. M > 10 -20% > 3 u. U/m. L (21. 5 p. M) Insulin/glucose > 0. 3 Proinsulin: < 5 p. M < 10 -20% Anti-insulin Ab’s
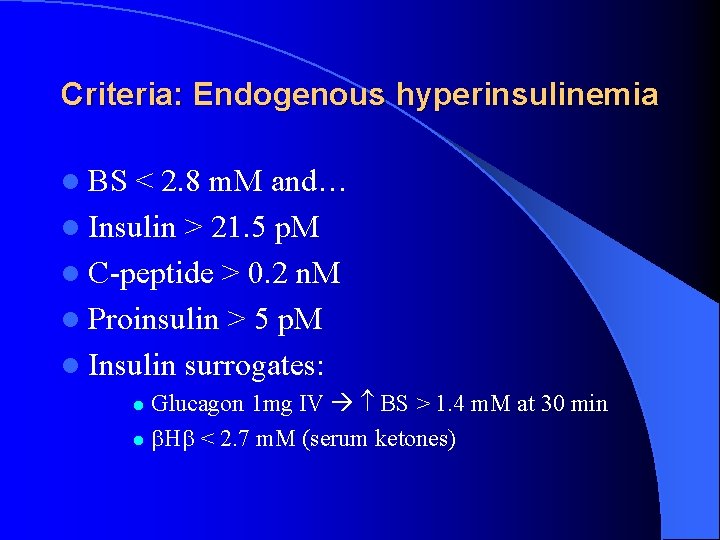
Criteria: Endogenous hyperinsulinemia l BS < 2. 8 m. M and… l Insulin > 21. 5 p. M l C-peptide > 0. 2 n. M l Proinsulin > 5 p. M l Insulin surrogates: Glucagon 1 mg IV BS > 1. 4 m. M at 30 min l H < 2. 7 m. M (serum ketones) l
END
- Slides: 49