Non Neoplastic Lesions Of Salivary Glands CLASSIFICATION OF
























- Slides: 80
Non Neoplastic Lesions Of Salivary Glands

• CLASSIFICATION OF SALIVARY GLAND DISORDERS • SALIVARY GLAND DISORDERS
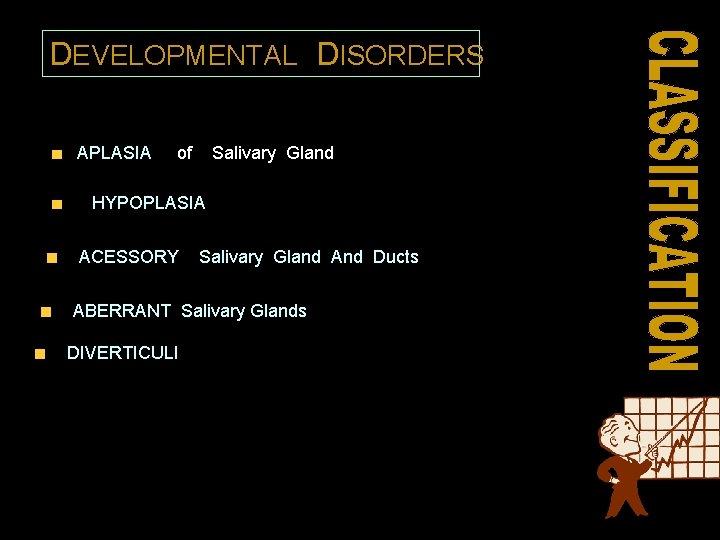
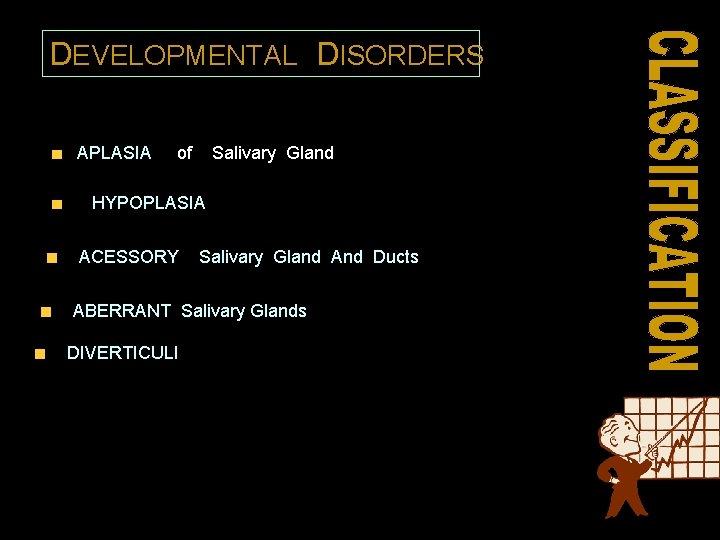
DEVELOPMENTAL DISORDERS APLASIA of Salivary Gland HYPOPLASIA ACESSORY Salivary Gland And Ducts ABERRANT Salivary Glands DIVERTICULI
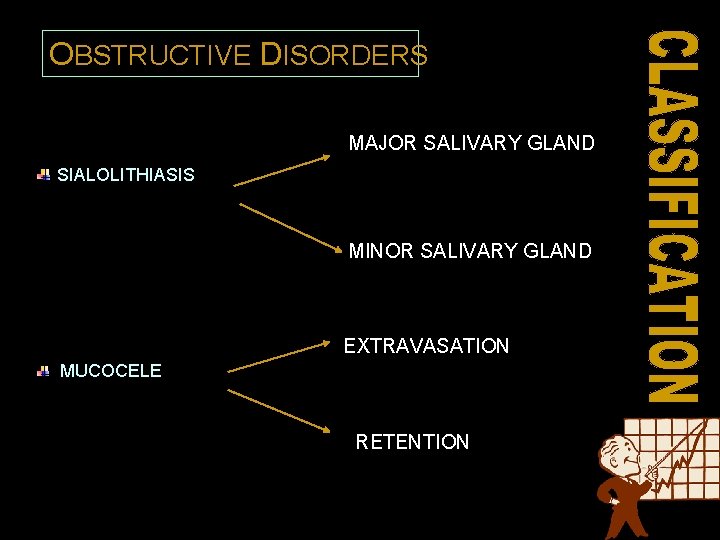
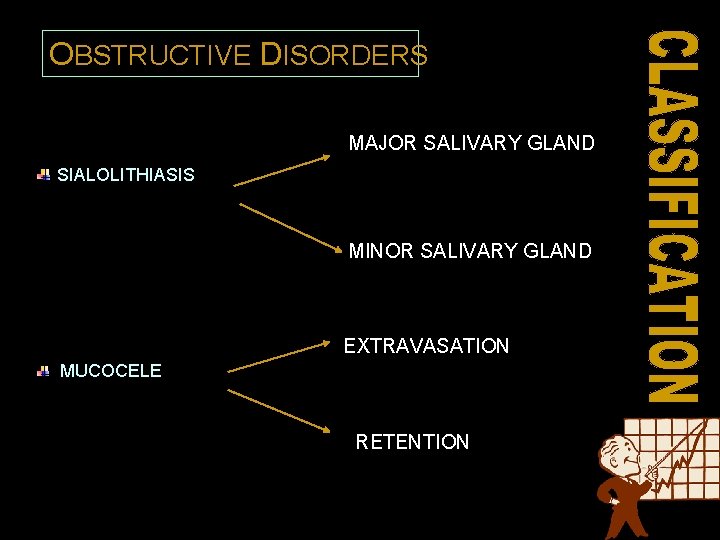
OBSTRUCTIVE DISORDERS MAJOR SALIVARY GLAND SIALOLITHIASIS MINOR SALIVARY GLAND EXTRAVASATION MUCOCELE RETENTION

OBSTRUCTIVE DISORDERS RANULA FOREIGN BODIES
FUNCTIONAL DISORDERS XEROSTOMIA PTYLASM

INFLAMMATORY & REACTIVE DISORDERS NECROTISING SIALOMETAPLASIA RADIATION INDUCED SIALADENITIS ALLERGIC SIALADENITIS

VIRAL DISEASES MUMPS q VIRAL INFECTIONS : HCV INFECTION HIV INFECTIONS CYTOMEGALOVIRUS INFECTION
BACTERIAL DISEASES q BACTERIAL : ACUTE BACTERIAL SIALADENITIS CHRONIC OR RECURRENT SIALADENITIS
SYSTEMIC CONDITIONS WITH SALIVARY GLAND INVOLVEMENT SYSTEMIC METABOLIC CONDITIONS : Diabetes mellitus anorexia Bulimia Alcoholism
AUTOIMMUNE DISEASES: SJOGREN’S SYNDROME (prim & sec) MICKULICZ’S DISEASE
GRANULOMATOUS DISEASES: TUBERCULOSIS SARCOIDOSIS
Necrotising sialometaplasia q salivary gland infarction q. Non neoplastic , inlf condition q. Significance q. Abrams et al in 1973 ØVascular ischemia Etiology ØLocal trauma ØSurgical manipulation Ølocal anesthesia ØRadiation therapy Ølocal infarction
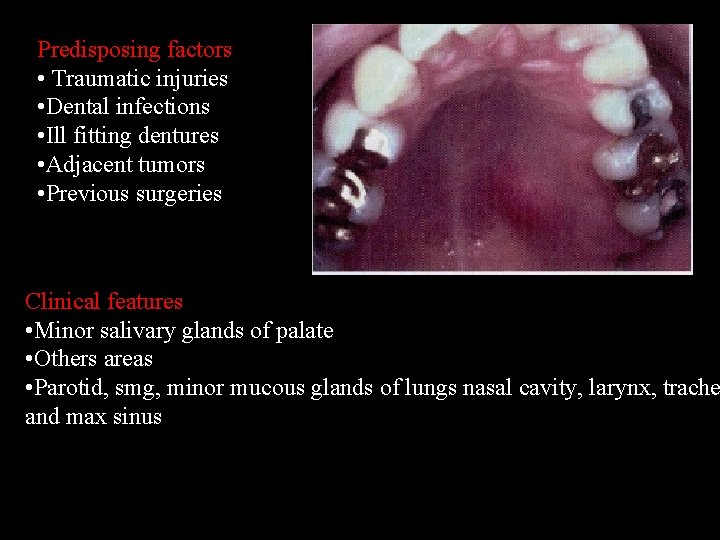
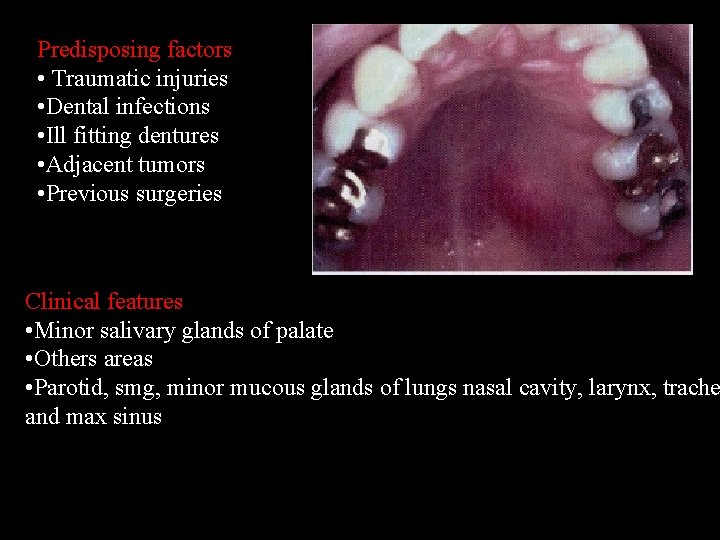
Predisposing factors • Traumatic injuries • Dental infections • Ill fitting dentures • Adjacent tumors • Previous surgeries Clinical features • Minor salivary glands of palate • Others areas • Parotid, smg, minor mucous glands of lungs nasal cavity, larynx, trache and max sinus

C/f • Initial lesion swelling with or with out ulceration • Crateriform ulcer of palate • 1 to 3 cms • Unilateral • Erosion of the palate • Age 17 to 80 yrs • m: f 2: 1
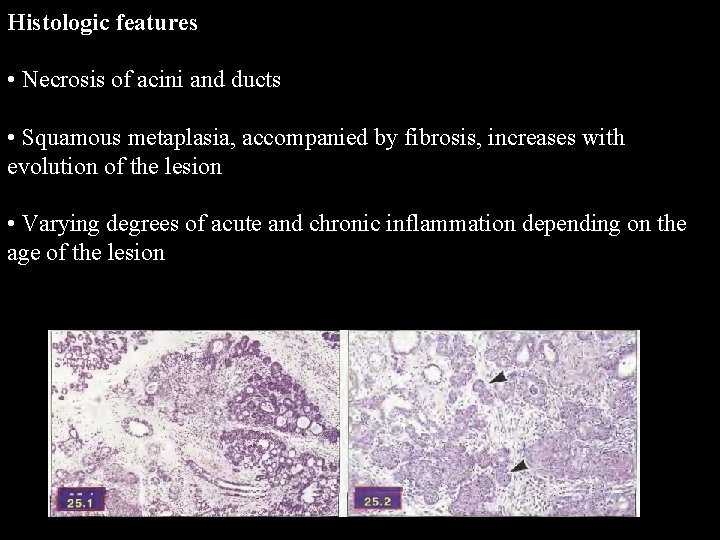
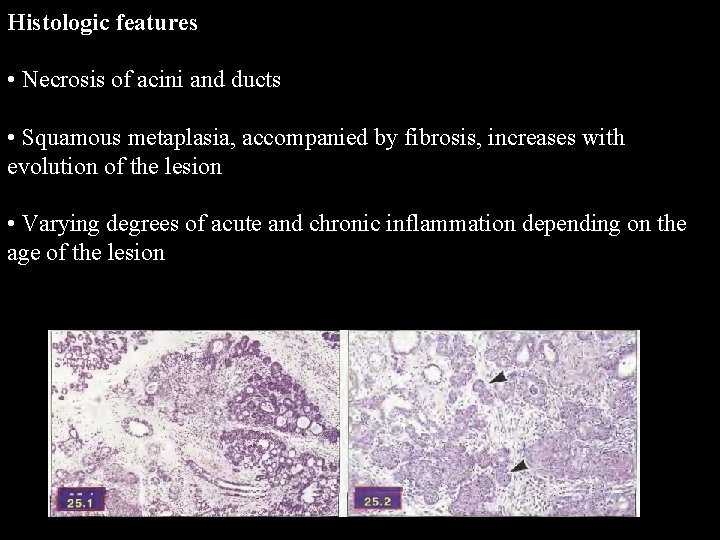
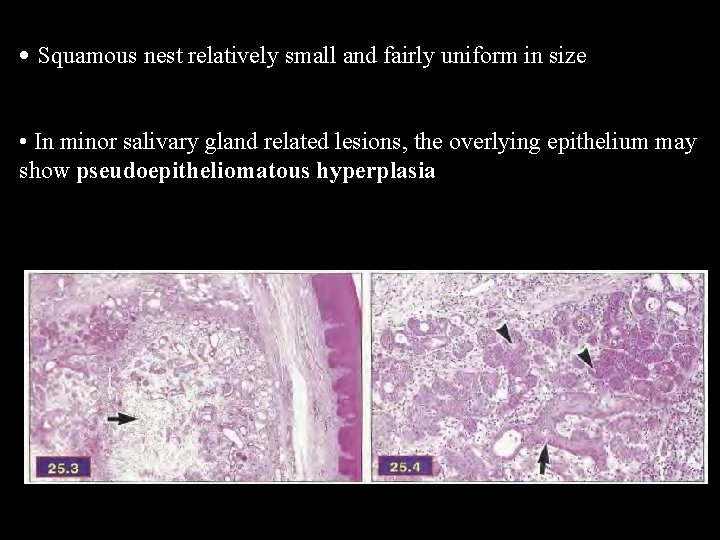
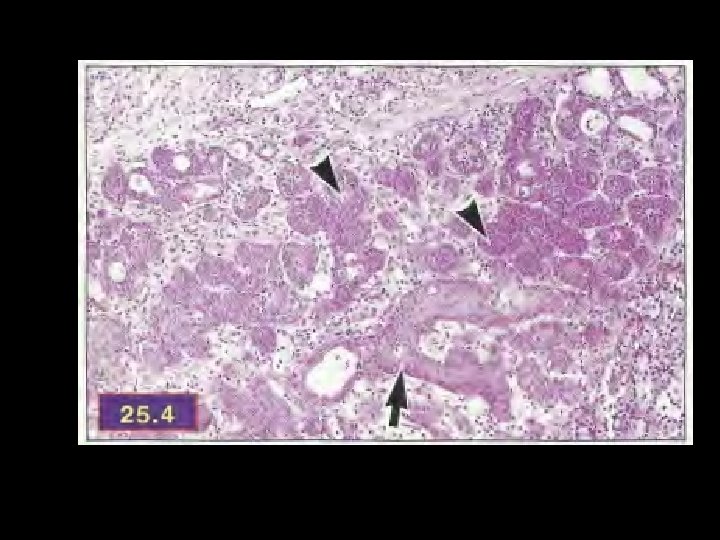
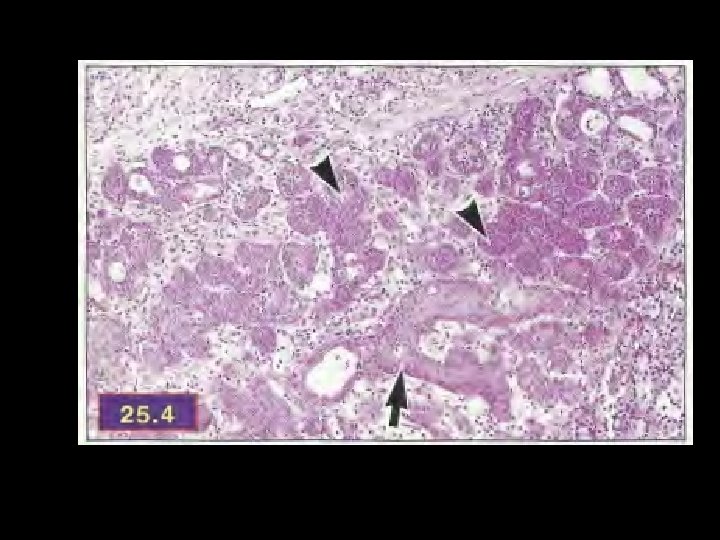
Histologic features • Necrosis of acini and ducts • Squamous metaplasia, accompanied by fibrosis, increases with evolution of the lesion • Varying degrees of acute and chronic inflammation depending on the age of the lesion
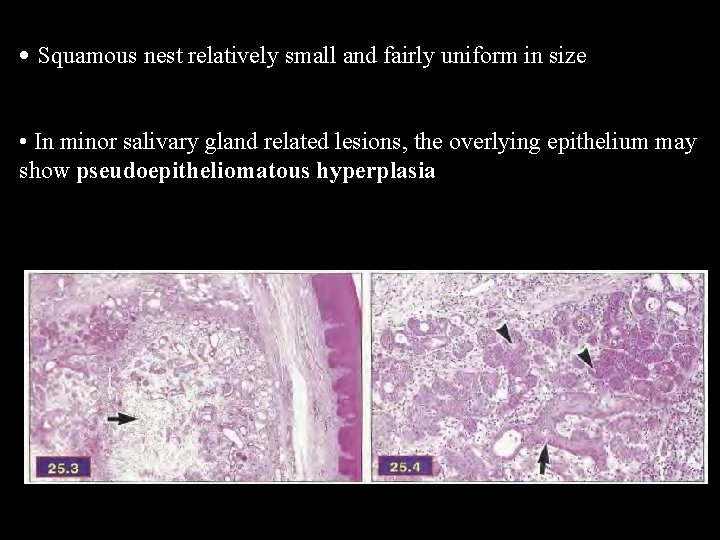
• Squamous nest relatively small and fairly uniform in size • In minor salivary gland related lesions, the overlying epithelium may show pseudoepitheliomatous hyperplasia

D/D: • SCC • Syphilic gumma, deep fungal infection • Wegener’s granulomatosis • Extranodal lymphomas Treatment: • Resolves spontaneously • Periodic evaluation • Prognosis excellent

Obstructive SG Disorders: Sialolithiasis • A stone in the salivary duct or gland • Mechanical obstruction of the salivary duct • Major cause of unilateral diffuse parotid or submandibular gland swelling • Most frequent reason for submandibular gland resection
Sialolithiasis • The exact pathogenesis of sialolithiasis remains unknown. • Thought to form via…. an initial organic nidus that progressively grows by deposition of layers of inorganic and organic substances. • May eventually obstruct flow of saliva from the gland to the oral cavity.
Sialolithiasis § Acute ductal obstruction may occur at meal time when saliva producing is at its maximum, the resultant swelling is sudden and can be painful. § Gradually reduction of the swelling can result but it recurs repeatedly when flow is stimulated. § This process may continue until complete obstruction and/or infection occurs.

Etiology • • Hypercalcemia…in rats only Xerostomic meds Tobacco smoking Smoking has an increased cytotoxic effect on saliva, decreases PMN phagocytic ability and reduces salivary proteins • Gout is the only systemic disease known to cause salivary calculi and these are composed of uric acid.
Stone Composition • Organic; often predominate in the center – Glycoproteins – Mucopolysaccharides – Bacterial products – Cellular debris • Inorganic; often in the periphery – Calcium carbonates & calcium phosphates in the form of hydroxyapatite

Parotid (PG) vs. Submandibular Gland (SMG)…. • Most authorities agree obstructive phenomemnon such as mucous plugs and sialoliths are most commonly found in the SMG – Escudier et al – Lustmann et al – Rice
Reasons sialolithiasis may occur more often in the SMG • Saliva more alkaline • Higher concentration of calcium and phosphate in the saliva • Higher mucus content • Longer duct • Anti-gravity flow
Clinical presentation • Painful swelling (60%) • Painless swelling (30%) – Sometimes described as recurrent salivary colic and spasmodic pain upon eating

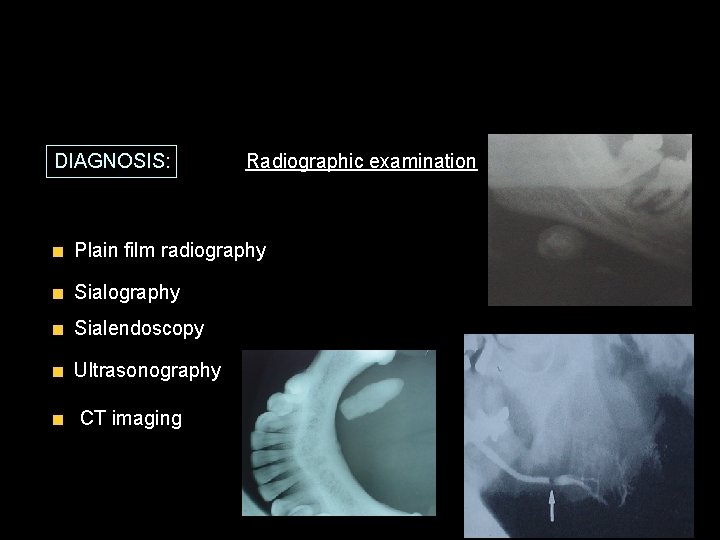
Diagnostics: Plain occlusal film • Effective for intraductal stones, while…. • intraglandular, radiolucent or small stones may be missed.
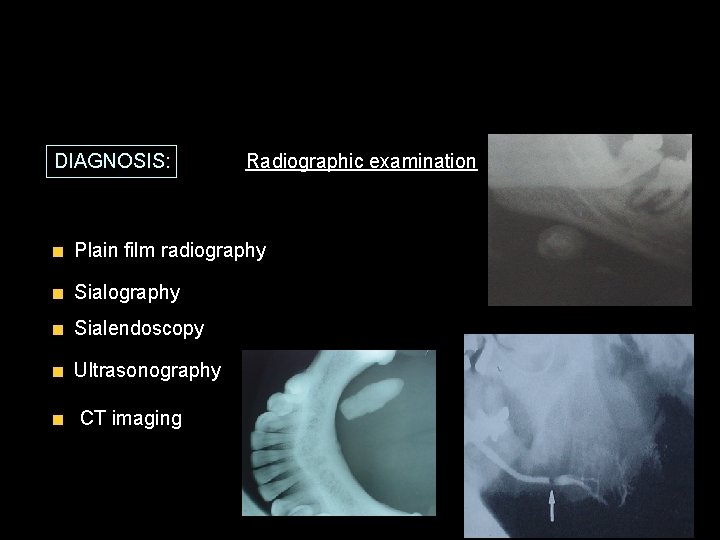
DIAGNOSIS: Radiographic examination Plain film radiography Sialendoscopy Ultrasonography CT imaging



Mucocele • Mucoceles, exclusive of the irritation fibroma, are most common of the benign soft tissue masses in the oral cavity. • Muco: mucus , coele: cavity. • Consist of a circumscribed cavity in the connective tissue and submucosa producing an obvious elevation in the mucosa • When in the oral floor, they are called ranula.

Etiology and pathogenesis • • Obstruction of minor sg duct Traumatic severance of duct Chronic partial obstruction Salivary calculus Classification • Extravasation mucocele • Retention mucocele

Mucocele Extravasation is the leakage of fluid from the ducts or acini into the surrounding tissue. Extra: outside, vasa: vessel Retention: narrowed ductal opening that cannot adequately accommodate the exit of saliva produced, leading to ductal dilation and surface swelling. Less common phenomenon
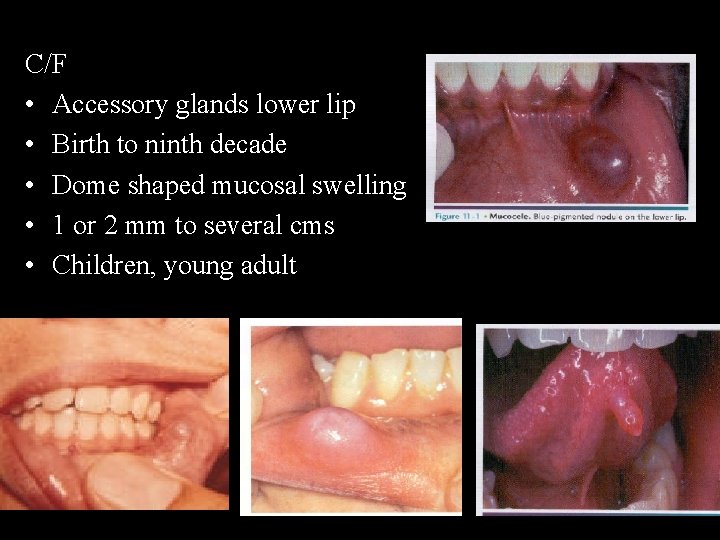
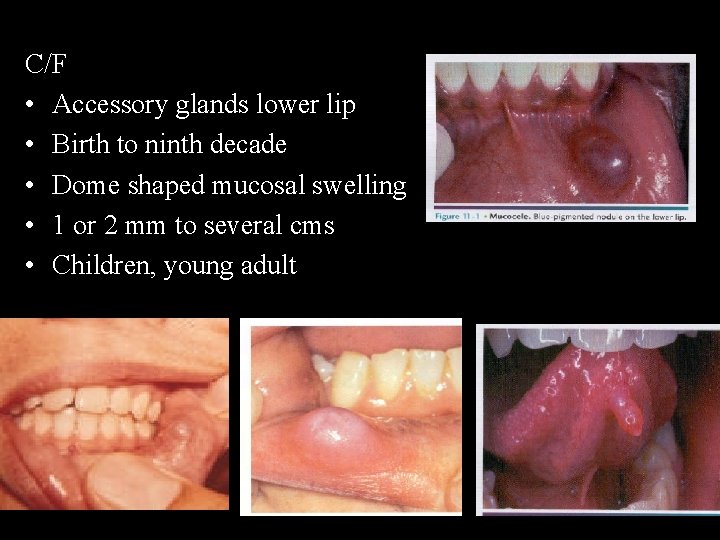
C/F • Accessory glands lower lip • Birth to ninth decade • Dome shaped mucosal swelling • 1 or 2 mm to several cms • Children, young adult
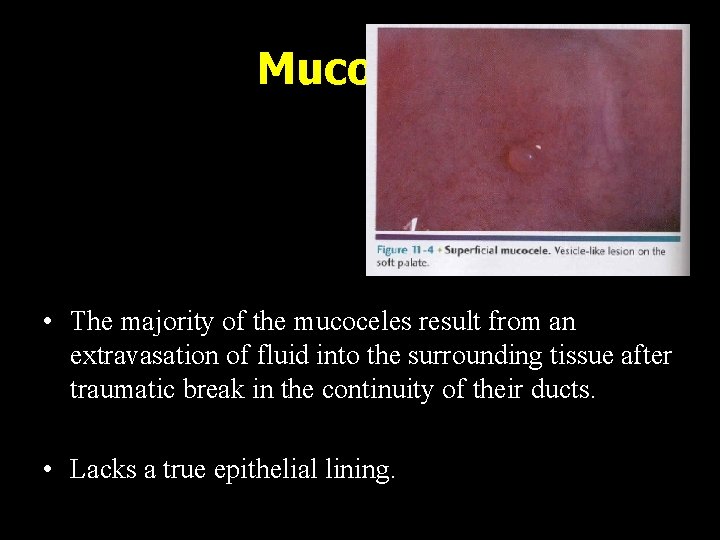
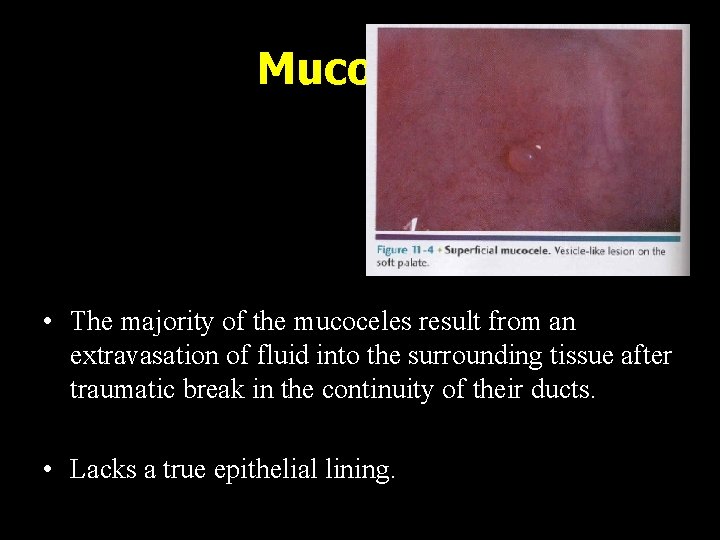
Mucocele • The majority of the mucoceles result from an extravasation of fluid into the surrounding tissue after traumatic break in the continuity of their ducts. • Lacks a true epithelial lining.

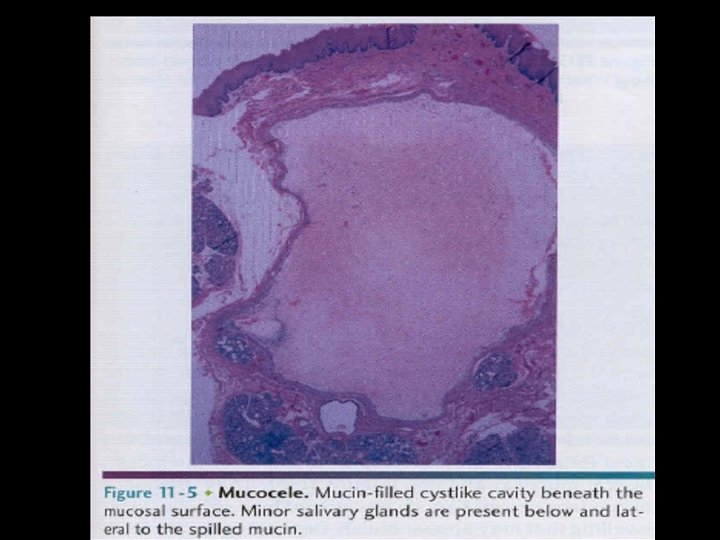
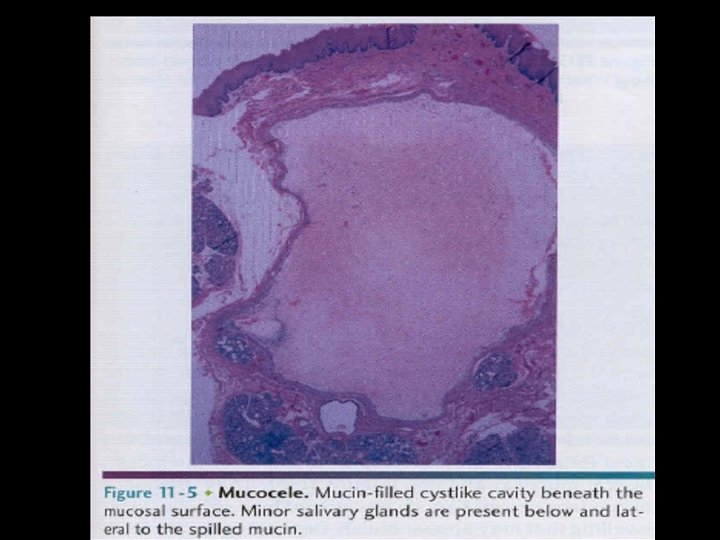
H/P • Lack of epi lining • Mucous laden tissue defect • Infiltraion of infl cells • Adj sg may be atrophic or show interstitial fibrosis
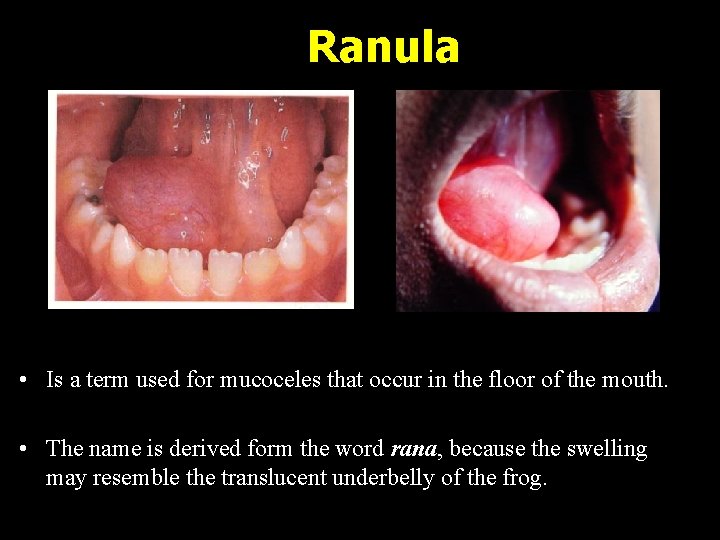
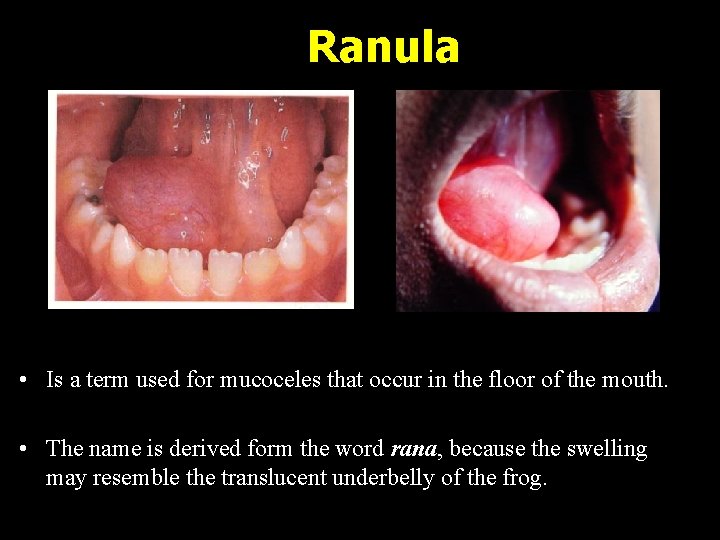
Ranula • Is a term used for mucoceles that occur in the floor of the mouth. • The name is derived form the word rana, because the swelling may resemble the translucent underbelly of the frog.
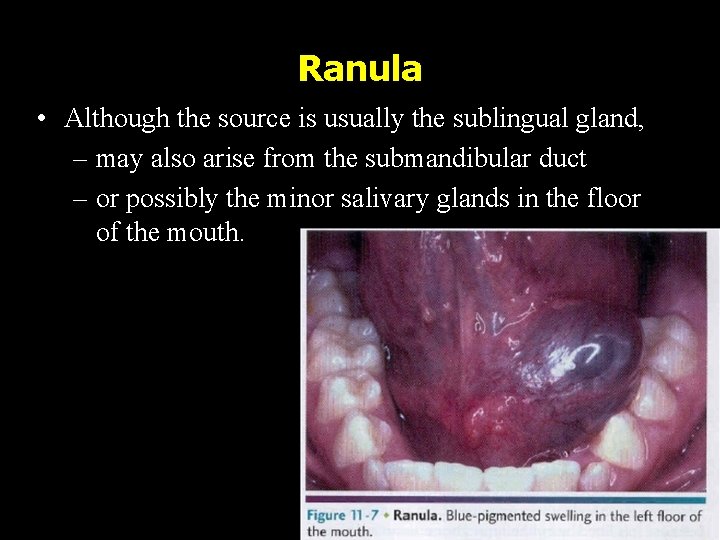
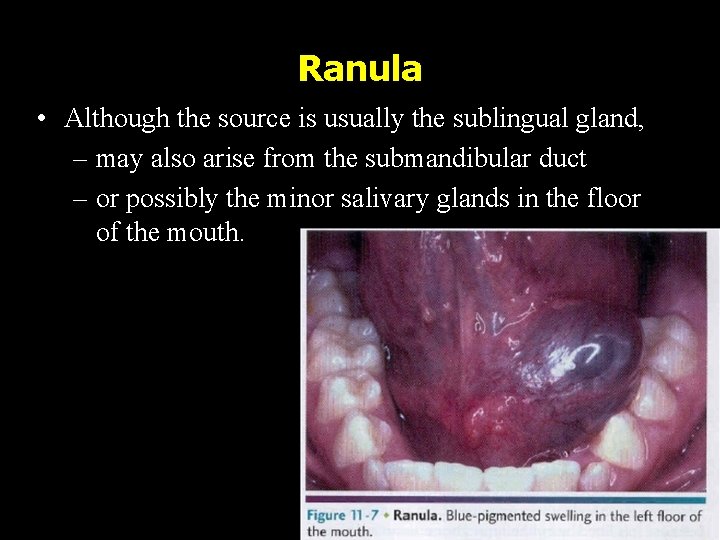
Ranula • Although the source is usually the sublingual gland, – may also arise from the submandibular duct – or possibly the minor salivary glands in the floor of the mouth.
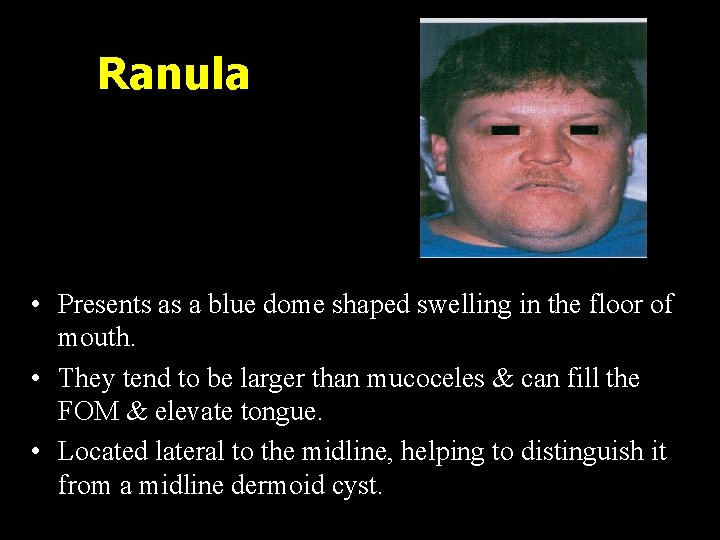
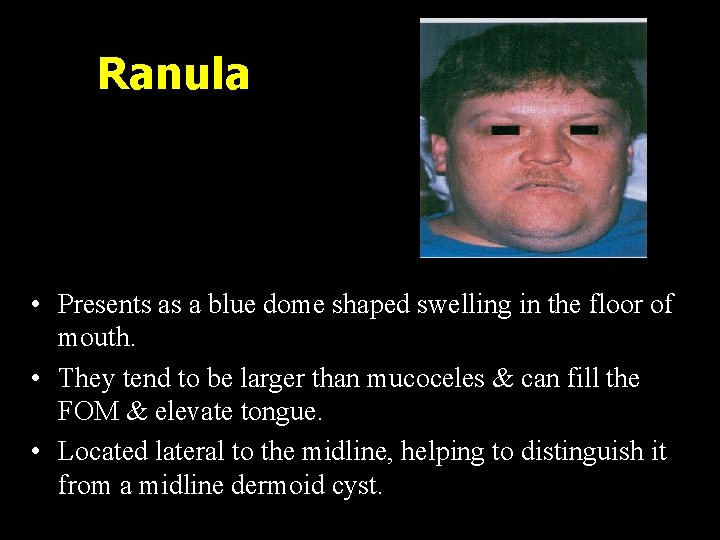
Ranula • Presents as a blue dome shaped swelling in the floor of mouth. • They tend to be larger than mucoceles & can fill the FOM & elevate tongue. • Located lateral to the midline, helping to distinguish it from a midline dermoid cyst.
Plunging or Cervical Ranula • Occurs when spilled mucin dissects through the mylohyoid muscle and produces swelling in the neck. • Concomitant FOM swelling may or may not be visible.
Treatment of Mucoceles in Lip or Buccal mucosa • Excision with strict removal of any projecting peripheral salivary glands • Avoid injury to other glands during primary wound closure
AUTOIMMUNE DISEASES: SJOGERNS SYNDROME HENRIK SJOGREN : 1933 CLINICAL TRIAD : Keratoconjunctivits sicca Xerostomia Rheumatoid arthritis
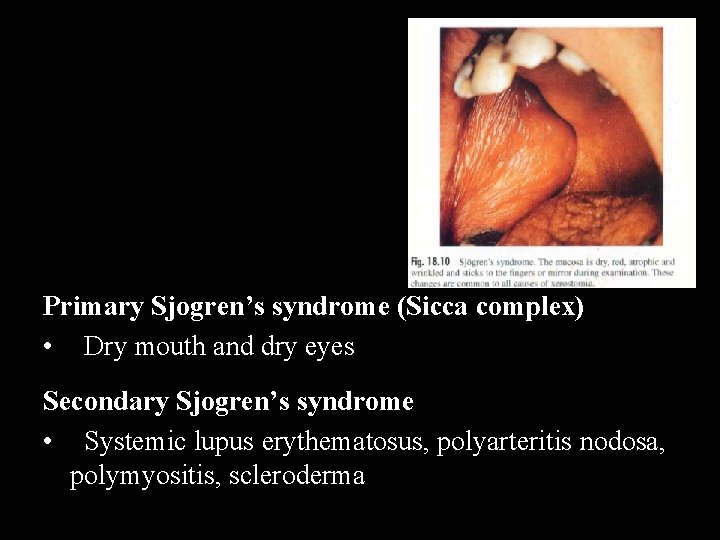
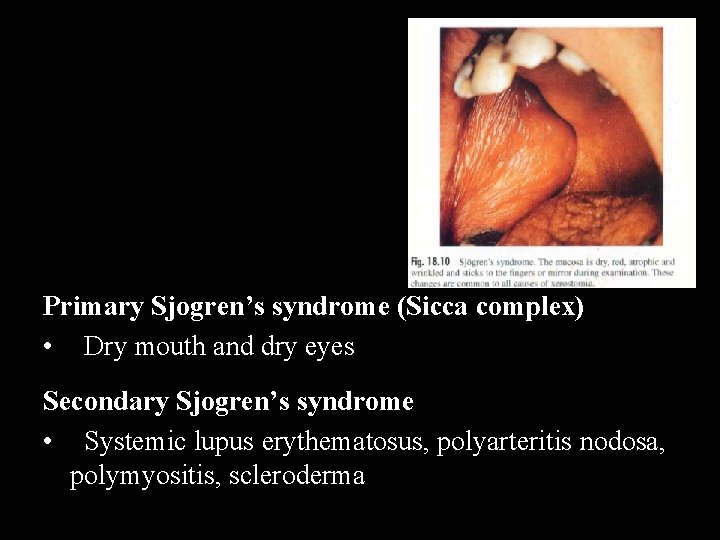
Primary Sjogren’s syndrome (Sicca complex) • Dry mouth and dry eyes Secondary Sjogren’s syndrome • Systemic lupus erythematosus, polyarteritis nodosa, polymyositis, scleroderma
Etiology • Genetic • Hormonal • Infectious • Immunologic – antisalivary duct antibody • Combinations of factors
C/F: • • • Usually in females over 40 yrs Children & young adults may be affected F: M– 10: 1 Dryness of eyes and mouth Painful, burning sensation of oral mucosa Lymphadenopathy is more common in primary form


Diagnosis : History & Exam Investigations: Opthalmologic test Salivary gland function test Connective tissue disorder test Opthalmologic test: v. Schirmer’s test v. Break up time test (BUT) v. Rose Bengal Dye test
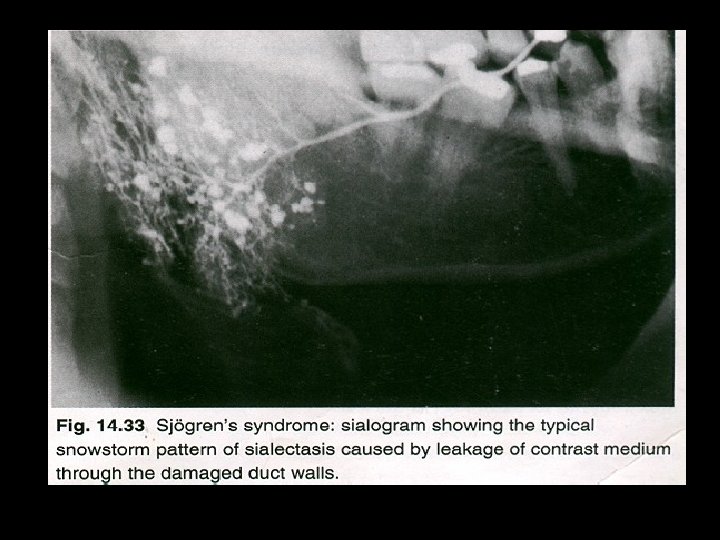
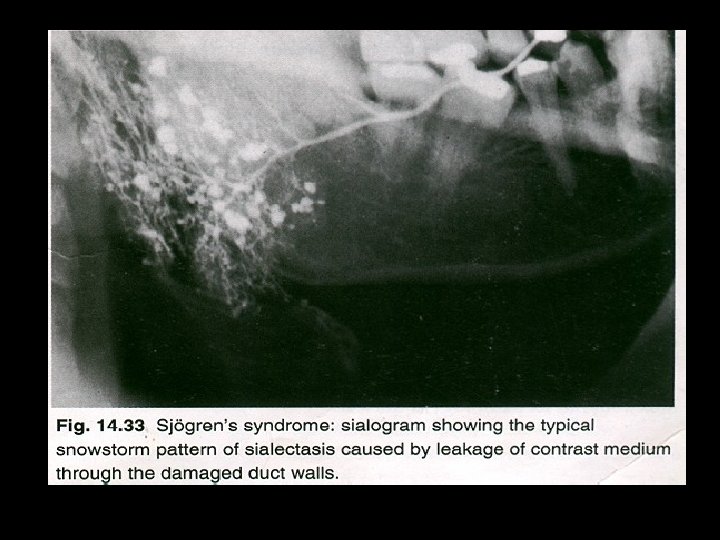
Salivary gland function test: Salivary flow rate Salivary gland biopsy Scintigraphy & Sialography Connective tissue disorder test: +ve antisalivary antibody +ve rheumatoid factor
Lab finding • Polyclonal hyperglobulinemia • Antisalivary duct antibodies, rheumatoid factor and antinuclear antibodies. • An increased sedimentation rate Radiography • formation of punctate cavity defect which are filled with radio-opaque contrast media • Cherry blossom or branchless fruit laden tree appearance
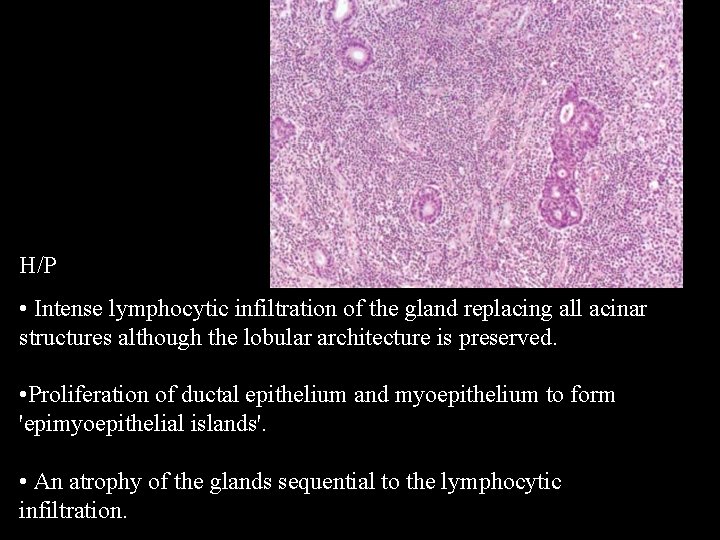
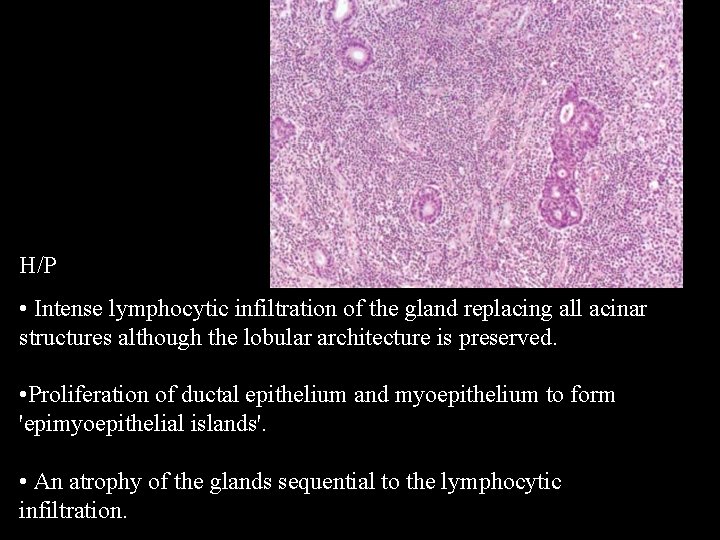
H/P • Intense lymphocytic infiltration of the gland replacing all acinar structures although the lobular architecture is preserved. • Proliferation of ductal epithelium and myoepithelium to form 'epimyoepithelial islands'. • An atrophy of the glands sequential to the lymphocytic infiltration.
Treatment: • Symptomatic treatment • Salivary substitutes • Ocular lubricants Complication– Development of lymphomas

Mikulicz’s disease • Condition characterized by an abnormal enlargement of the SG and lacrimal glands • Johan Mikuliczs in 1888 Etiology • Autoimmune • Viral • genetic

Mikulicz disease • If the cause is unknown Mikulicz’s syndrome • If enlargement of the glands are associated with known dieseases – tuberculosis, sarcoidosis or lymphoma
C/F • Often affects females • Middle age • Occurs with SS • Sudden onset of xerostomia, difficulty in swallowing • Tooth decay • Eyes - Enlarged lacrimal glands , decreased lacrimation • Fever
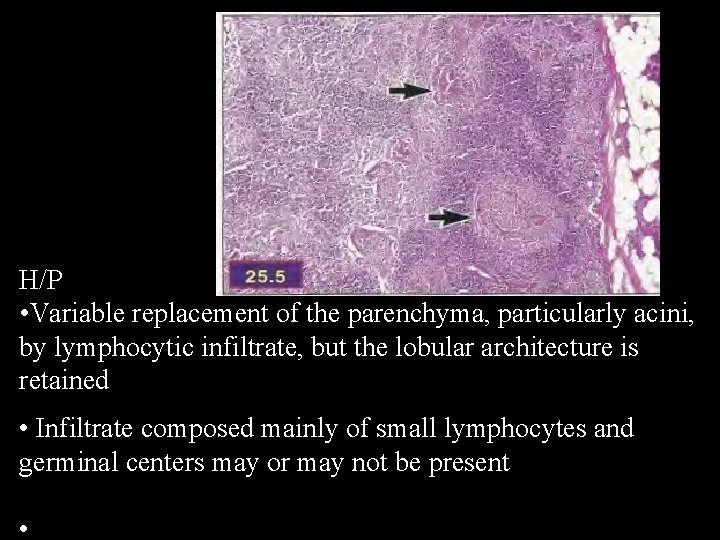
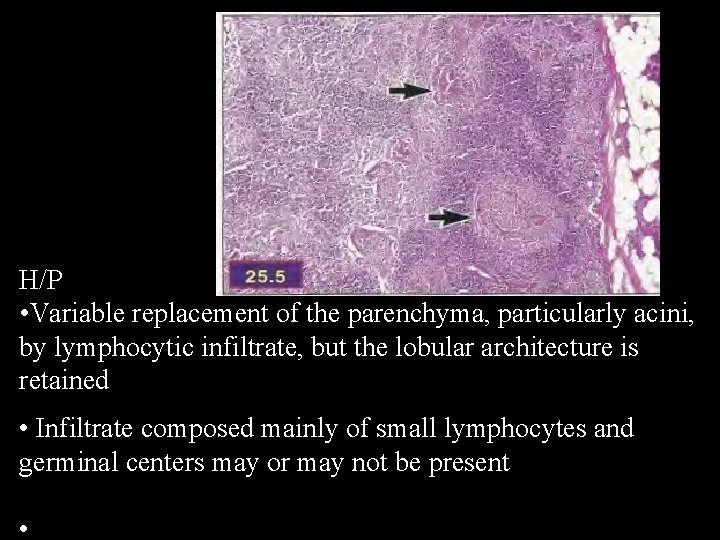
H/P • Variable replacement of the parenchyma, particularly acini, by lymphocytic infiltrate, but the lobular architecture is retained • Infiltrate composed mainly of small lymphocytes and germinal centers may or may not be present •
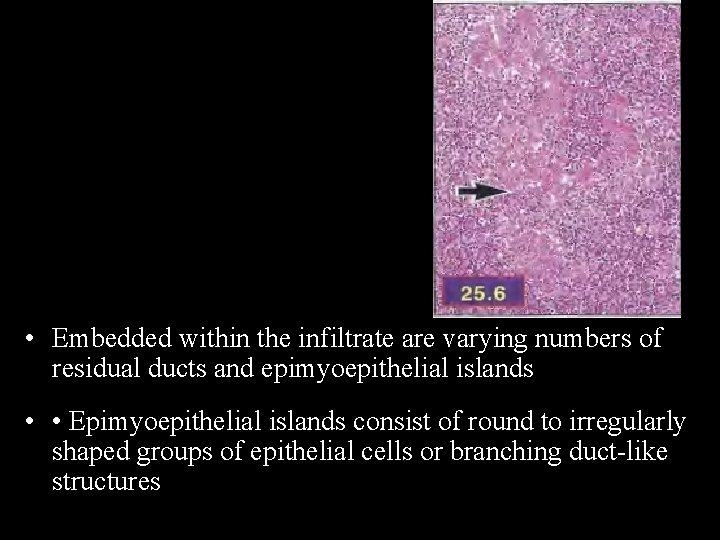
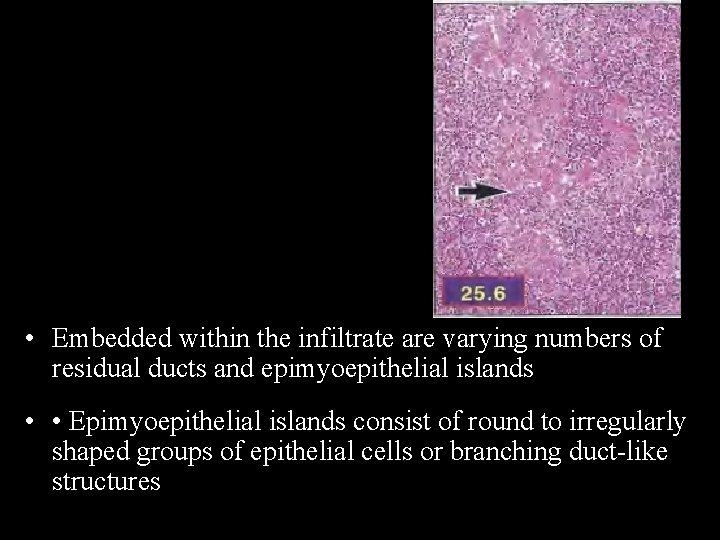
• Embedded within the infiltrate are varying numbers of residual ducts and epimyoepithelial islands • • Epimyoepithelial islands consist of round to irregularly shaped groups of epithelial cells or branching duct-like structures
Treatment: • Symptomatic
FUNCTIONAL DISORDERS XEROSTOMIA SIALORRHEA
XEROSTOMIA Risk factors: Developmental : Iatrogenic : Salivary gland aplasia v Medications v Radiation therapy Water metabolite loss: v Impaired fluid intake v Vomiting /diarrohea
XEROSTOMIA Local factors : v Smoking v Mouth breathing Systemic diseases : v Sjogerns syndrome v Diabetes mellitus v Sarcoidosis & HIV
XEROSTOMIA • Causes; – Depression / chronic anxiety – Dehydration – Drugs – Diseases
XEROSTOMIA Clinical features : Dry mucosa Residual saliva : thick and ropey PT c/o diff in mastication & swallowing Diagnosis : Diseases : History Oral candidiasis radiation induced caries Clinical examination Investigations

XEROSTOMIA • MANAGEMENT – Preventive therapy – Symptomatic treatment – Local or topical salivary stimulation – Systemic salivary stimulation
XEROSTOMIA Treatment : Hydration Symptomatic : Discontinue the drugs Artificial saliva Chewing gums Sialogogues: pilocarpine
SIALORRHEA Excess saliva production Risk factors: Medications Rabies clinical sign Heavy metal poisoning Ill fitting dentures Local irritations New complete denture Mentally retarded pts Gastrointestinal reflux disease
SIALORRHEA Clinical features : Constant soiling of clothes Diagnosis : Past medical history Diagnostic tests – salivary flow rate
SIALORRHEA Treatment: Medications: Antihistamine Anti cholinergics Injection : BOTULINUM TOXIN- PAROTID Surgical intervention: salivary gland excision (permanent relief) salivary duct ligation

Sialoadenosis • • Non neoplastic non infl enlargement of parotid gland Bilaterally and may manisfest recurrence or pain or both Assos with systemic d/o; this forms the basis for classification Hormonal sex hormone • Dysenymatic diabetic • Hepatogenic thyroid • Pancreotogenic adreno cortical d/o • Nephrogenic • dysprotienimic • Neurohormonal peripheral central • Malnutrional sialadenois • Drug induced sialoadenosis
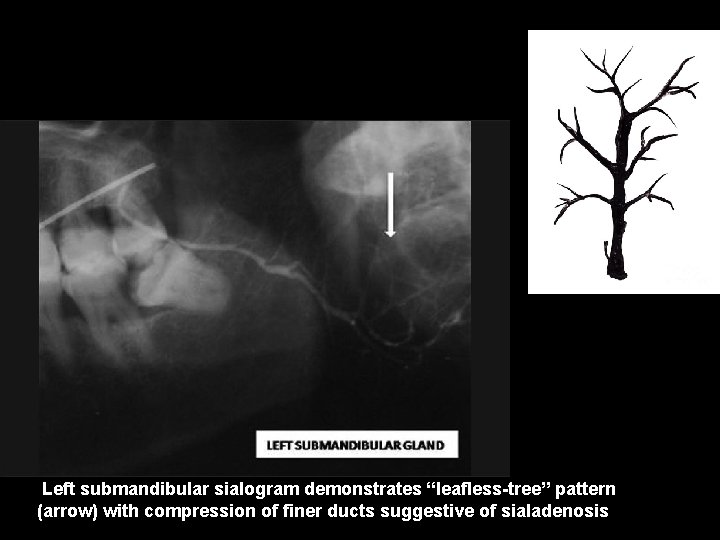
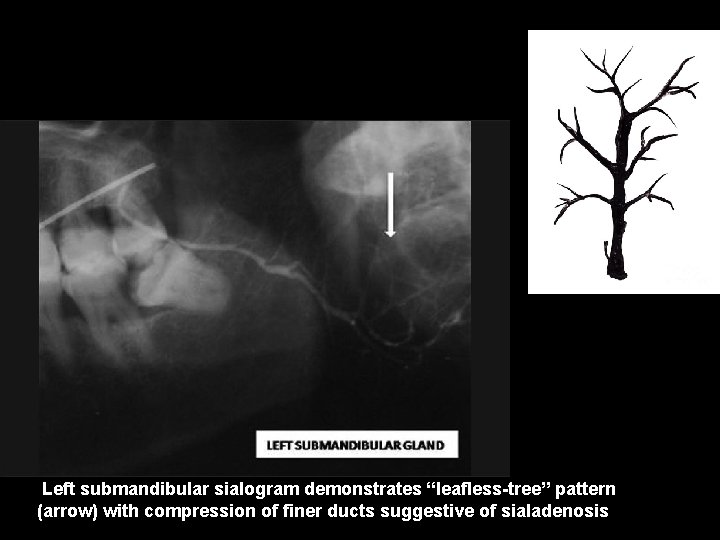
Left submandibular sialogram demonstrates “leafless-tree” pattern (arrow) with compression of finer ducts suggestive of sialadenosis
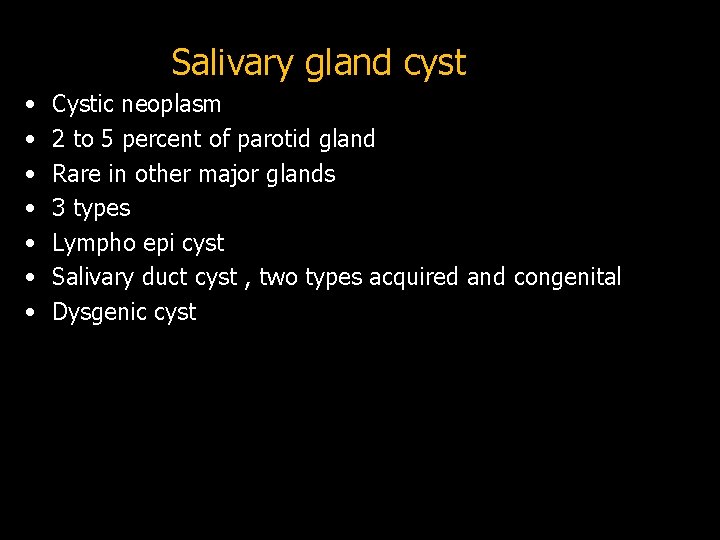
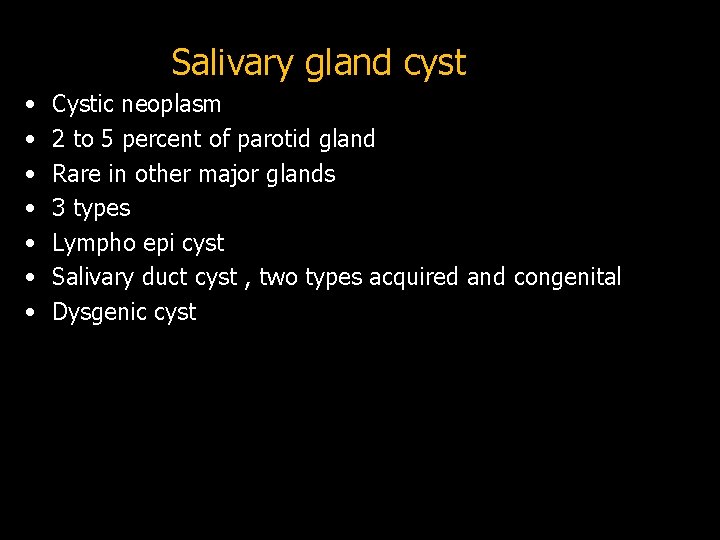
Salivary gland cyst • • Cystic neoplasm 2 to 5 percent of parotid gland Rare in other major glands 3 types Lympho epi cyst Salivary duct cyst , two types acquired and congenital Dysgenic cyst
• Clinical features • Parotid gland , unilateral painless swellings with no involvement of facial nerve and no fixation to the overlying skin. • Patients are over 40 years of age. • 0. 8 -10. 0 cm with an average size of approximately 1 -3 cms.
• H/P • Unilocular cysts are lined by single or multilayered cuboidal or columnar epithelium. • Mucus containing goblet cells and areas of • Oncocytic differentiation may be seen. • Completely or partially lined by squamous epithelium. • Lymphocytic infiltration in the cyst wall.
Chronic sclerosing sialadenitis of SMG • Benign inflammatory condition of the submandibular gland that mimics a malignant neoplasm clinically because of presentation as a hard mass. • H/P • preserved lobular architecture, thickening of interlobular septa by sclerotic tissue, dense lymphoplasmacytic infiltrate, • preservation of ducts with periductal fibrosis, and variable loss of acini

References • • • Salivary gland Pathlogy. Irving Dardick Surgical Pathology of salivary glands. Gary L. Ellis Textbook of Oral Pathology. Shafer 6 th edition Oral and Maxillofacial pathology. Neville, 3 rd edition Essentials of oral medicine and oral pathology. Cawson, 7 th edition.

Thank you
 Non neoplastic epithelial disorders
Non neoplastic epithelial disorders Incision for parotid abscess
Incision for parotid abscess Nie wiem association
Nie wiem association Ginivitis
Ginivitis Submandibular gland excision
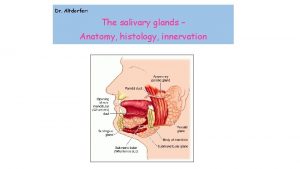
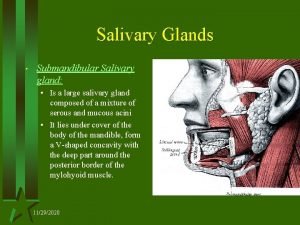
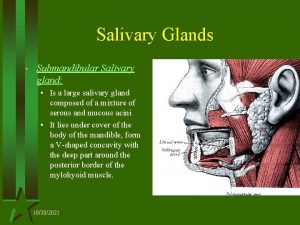
Submandibular gland excision Anatom
Anatom Minor salivary glands
Minor salivary glands Difference between serous and mucous acini slideshare
Difference between serous and mucous acini slideshare Testing cranial nerves
Testing cranial nerves Minor salivary glands
Minor salivary glands Minor salivary glands
Minor salivary glands Youtube
Youtube Saliva formation
Saliva formation Parotid nest
Parotid nest Simple squamous epithelium
Simple squamous epithelium Reed sternberg cells
Reed sternberg cells White appearance
White appearance Periradicular
Periradicular Salivary gland disease classification
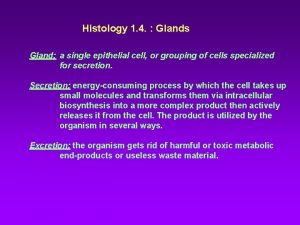
Salivary gland disease classification Classification of exocrine glands
Classification of exocrine glands Pie on the floor visual field defect
Pie on the floor visual field defect Extrapyramidal tract function
Extrapyramidal tract function Describing skin lesions
Describing skin lesions Esophagus
Esophagus Dermatology morphology
Dermatology morphology Olneys lesions
Olneys lesions Pyramidal and extrapyramidal tracts
Pyramidal and extrapyramidal tracts Gj mount classification of caries
Gj mount classification of caries Amiante
Amiante Don't touch lesions
Don't touch lesions Glossopharyngeal lesion
Glossopharyngeal lesion Oral pathology
Oral pathology Pr��ca projektov�� mana����r
Pr��ca projektov�� mana����r Scattered white matter lesions
Scattered white matter lesions Daughter mother grandmother pancreatic lesions
Daughter mother grandmother pancreatic lesions Monocular visual field
Monocular visual field Convergence insufficiency athens
Convergence insufficiency athens White lesions
White lesions Lésions
Lésions Vesiculobullous lesions
Vesiculobullous lesions Site:slidetodoc.com
Site:slidetodoc.com Recueil de chant jeunesse adventiste
Recueil de chant jeunesse adventiste Tyroid cartilage
Tyroid cartilage Warthin tumor
Warthin tumor Types of exocrine glands
Types of exocrine glands Albans test is an example of
Albans test is an example of Snyder test for dental caries
Snyder test for dental caries Oncocytoma salivary gland
Oncocytoma salivary gland Pathogenesis of pleomorphic adenoma
Pathogenesis of pleomorphic adenoma Oncocytoma salivary gland
Oncocytoma salivary gland Xerotrachea
Xerotrachea Oncocytoma salivary gland
Oncocytoma salivary gland Oncocytoma salivary gland
Oncocytoma salivary gland Salivary amylase digestion of starch
Salivary amylase digestion of starch Physiology
Physiology Submadibular
Submadibular Gastric glands
Gastric glands Tissue
Tissue Cutaneous membrane
Cutaneous membrane Poem about female reproductive system
Poem about female reproductive system Major endocrine glands male and female
Major endocrine glands male and female Chapter 16 endocrine system
Chapter 16 endocrine system Intestinal glands
Intestinal glands Where are the gastric glands located
Where are the gastric glands located What is serous secretion
What is serous secretion Propolis block factories
Propolis block factories Glands of littre
Glands of littre Simple tubular gland example
Simple tubular gland example Difference between endocrine and exocrine glands
Difference between endocrine and exocrine glands Urethral opening female
Urethral opening female Exocrine glands are ductless
Exocrine glands are ductless What is the function of sebaceous glands
What is the function of sebaceous glands It has fur and mammary glands
It has fur and mammary glands Thyroid
Thyroid What is gonads
What is gonads Pylorus histology
Pylorus histology Gonads glands
Gonads glands Short tube that receives purified lymph
Short tube that receives purified lymph Steroids endocrine system
Steroids endocrine system Thyroid
Thyroid Pathology
Pathology