NON INFECTIOUS PERIPHERAL ULCERATIVE KERATITIS PUK A Clinical
![NON INFECTIOUS PERIPHERAL ULCERATIVE KERATITIS [PUK] A Clinical Approach DR. REKHA GYANCHAND Cornea consultant, NON INFECTIOUS PERIPHERAL ULCERATIVE KERATITIS [PUK] A Clinical Approach DR. REKHA GYANCHAND Cornea consultant,](https://slidetodoc.com/presentation_image_h/c3e5a7fe424193f30bb275bb49638709/image-1.jpg)
- Slides: 37
![NON INFECTIOUS PERIPHERAL ULCERATIVE KERATITIS PUK A Clinical Approach DR REKHA GYANCHAND Cornea consultant NON INFECTIOUS PERIPHERAL ULCERATIVE KERATITIS [PUK] A Clinical Approach DR. REKHA GYANCHAND Cornea consultant,](https://slidetodoc.com/presentation_image_h/c3e5a7fe424193f30bb275bb49638709/image-1.jpg)
NON INFECTIOUS PERIPHERAL ULCERATIVE KERATITIS [PUK] A Clinical Approach DR. REKHA GYANCHAND Cornea consultant, Lions Eye Hospital BANGALORE
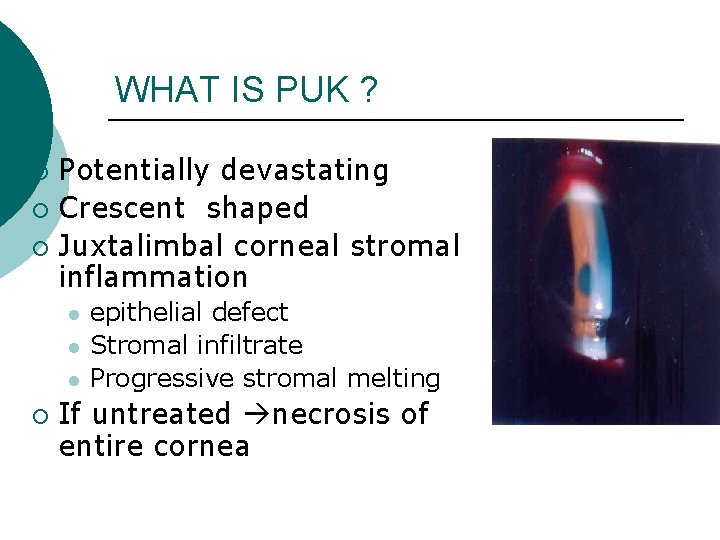
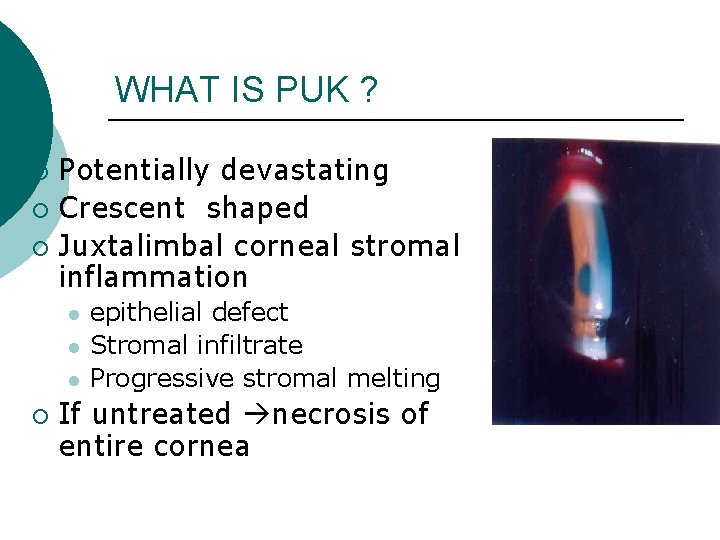
WHAT IS PUK ? Potentially devastating ¡ Crescent shaped ¡ Juxtalimbal corneal stromal inflammation ¡ l l l ¡ epithelial defect Stromal infiltrate Progressive stromal melting If untreated necrosis of entire cornea
WHY IN PERIPHERAL CORNEA ? ¡ Peripheral cornea Unique anatomical & immunological features ¡ Close to sclera / episclera / conjunctiva ¡ Limbal capillary Arcade ¡ Avascular central cornea ¡ Associated with sub conjunctival lymphatics afferent arm ¡ Ig. M in periphery large ¡ Langerhans cells ¡ Reservoir of inflammatory cells ¡ More susceptible to immunological damage
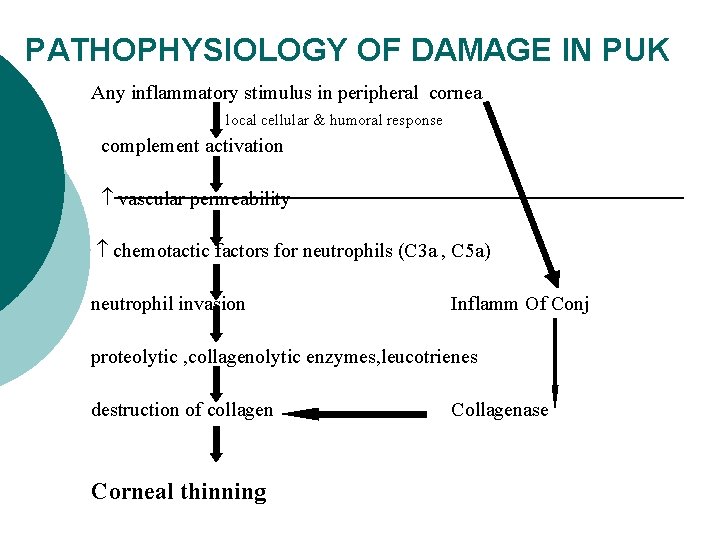
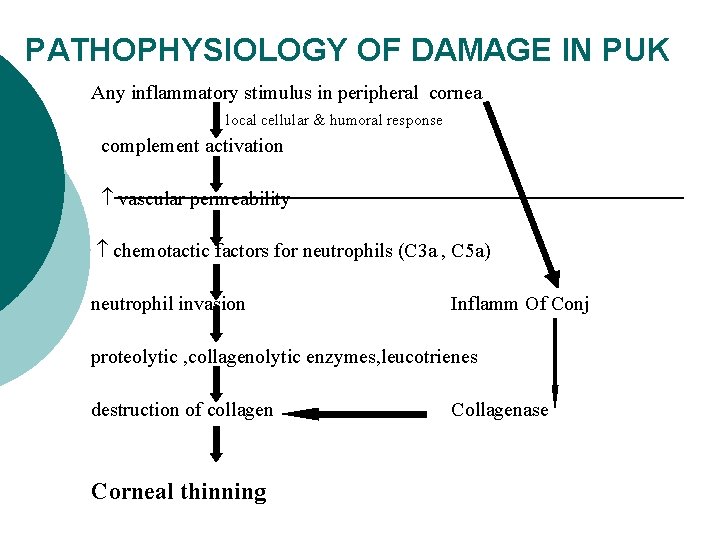
PATHOPHYSIOLOGY OF DAMAGE IN PUK Any inflammatory stimulus in peripheral cornea local cellular & humoral response complement activation vascular permeability chemotactic factors for neutrophils (C 3 a , C 5 a) neutrophil invasion Inflamm Of Conj proteolytic , collagenolytic enzymes, leucotrienes destruction of collagen Corneal thinning Collagenase
CLINICAL PRESENTATION & DIAGNOSIS ¡ ¡ 50% Of non infectious PUK due to collagen vascular disease (SLE, RP, PSS, RA, WG, PAN, GCA) 34% of non infectious PUK caused by RA (Tauber et al) PUK may be initial manifestation of WG & PAN Moorens ulcer – local autoimmune disease with PUK
CLINICAL PRESENTATION &DIAGNOSIS - II PUK due to CVD more in females ¡ PUK due to Moorens more in males ¡ Other causes include ¡ l l l Neoplasia Rosaceae Surgical trauma Blepharitis Inflammatory bowel disease
EXAMINATION IN PUK ¡ Ocular ¡ Systemic
OCULAR EXAMINATION Symptoms ¡ Pain, epiphora, photophobia ¡ pain if scleritis (RA, WG, PAN, RP) ¡ pain without scleritis ( Mooren’s) ¡ Decreased VA
EXAMINATION Examination of lids ¡ Blepharitis ¡ Telengiectasis (rosaecae) Posterior segment examination ¡ Posterior scleritis ¡ Vasculitis of CVD
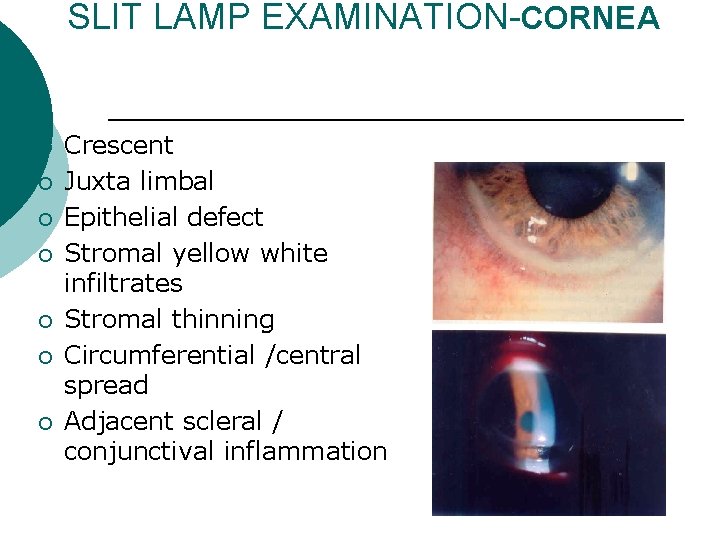
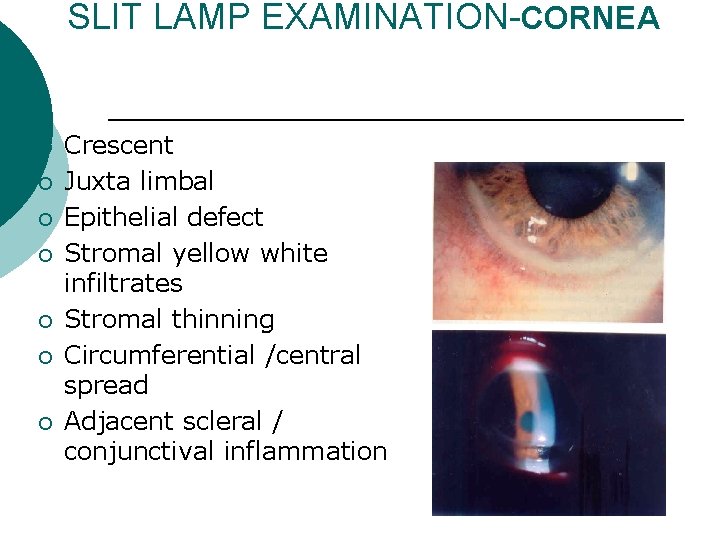
SLIT LAMP EXAMINATION-CORNEA ¡ ¡ ¡ ¡ Crescent Juxta limbal Epithelial defect Stromal yellow white infiltrates Stromal thinning Circumferential /central spread Adjacent scleral / conjunctival inflammation
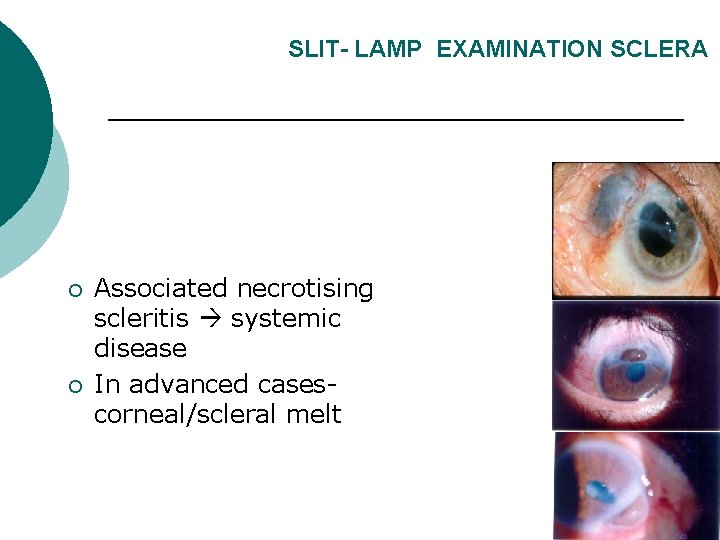
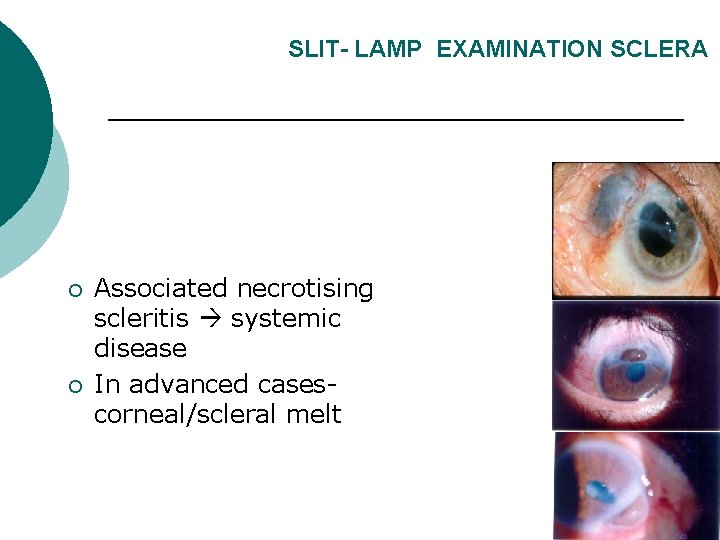
SLIT- LAMP EXAMINATION SCLERA ¡ ¡ Associated necrotising scleritis systemic disease In advanced casescorneal/scleral melt
SYSTEMIC EXAMINATION ¡ Thorough systemic history & examination mandatory Important Questionnaire? l Weight loss, fatigue l Skin – facial rashes, ulcers, periungual infarcts(SLE) l Respiratory symptoms ( WG, SLE) l GI symptoms- pain diarrhoea ( SLE, WG) l Musculoskeletal symptoms- joint pain ( RA, SLE) l Neurological – seizures, Raynauds (WG, RP, SLE) Genitourinary- hematuria ( PAN, SLE) Swollen ear lobes (RP, SLE) Deafness (WG) Nasal ulcers/ bleeds ( WG) ¡ Saddle nose ( WG, RP) ¡ ¡ ¡
Differential Diagnosis Of PUK ¡ Other Non Inflammatory Progressive Peripheral Thinning: l l Terriens marginal degeneration Pellucid marginal degeneration
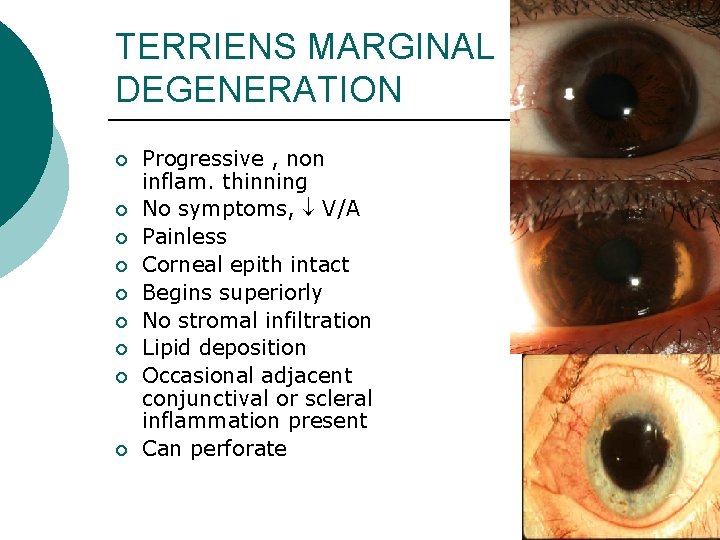
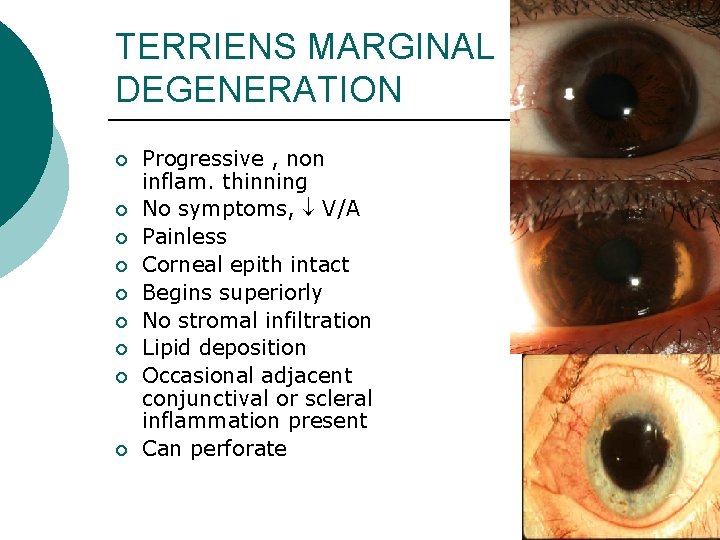
TERRIENS MARGINAL DEGENERATION ¡ ¡ ¡ ¡ ¡ Progressive , non inflam. thinning No symptoms, V/A Painless Corneal epith intact Begins superiorly No stromal infiltration Lipid deposition Occasional adjacent conjunctival or scleral inflammation present Can perforate
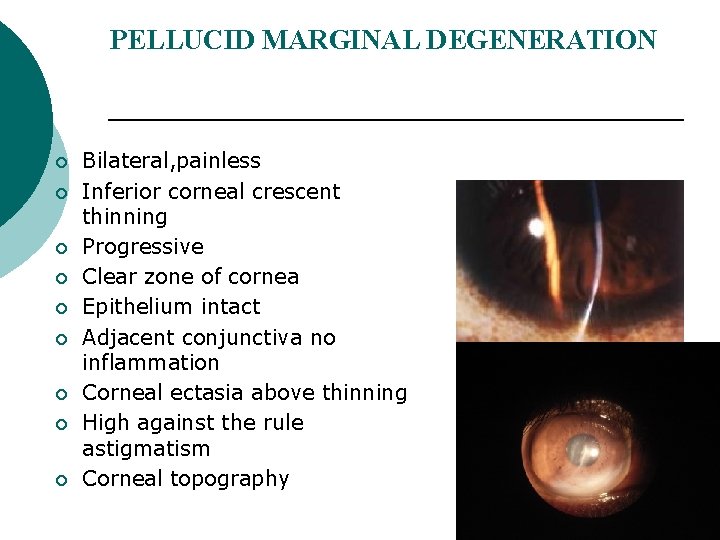
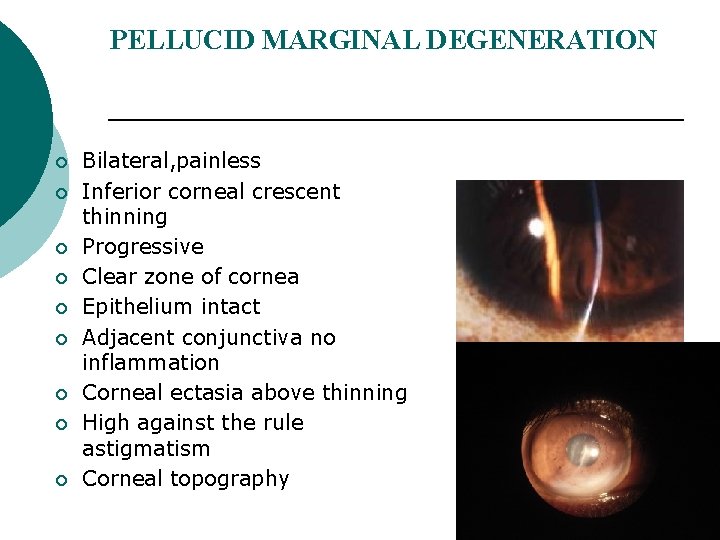
PELLUCID MARGINAL DEGENERATION ¡ ¡ ¡ ¡ ¡ Bilateral, painless Inferior corneal crescent thinning Progressive Clear zone of cornea Epithelium intact Adjacent conjunctiva no inflammation Corneal ectasia above thinning High against the rule astigmatism Corneal topography
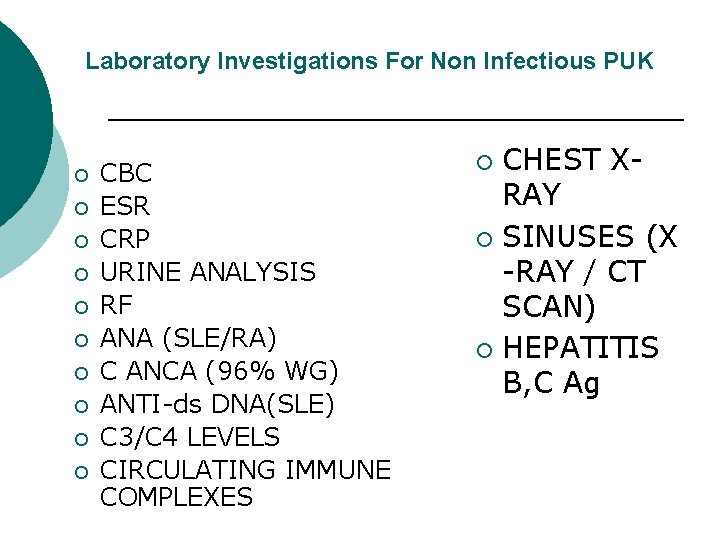
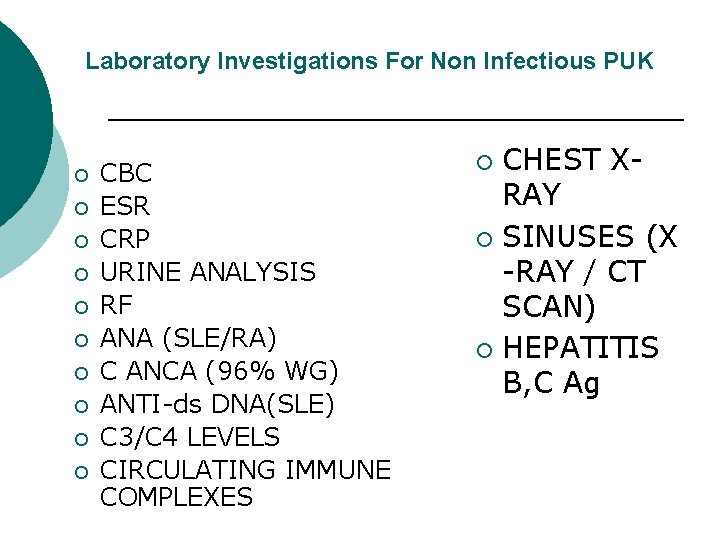
Laboratory Investigations For Non Infectious PUK ¡ ¡ ¡ ¡ ¡ CBC ESR CRP URINE ANALYSIS RF ANA (SLE/RA) C ANCA (96% WG) ANTI-ds DNA(SLE) C 3/C 4 LEVELS CIRCULATING IMMUNE COMPLEXES CHEST XRAY ¡ SINUSES (X -RAY / CT SCAN) ¡ HEPATITIS B, C Ag ¡
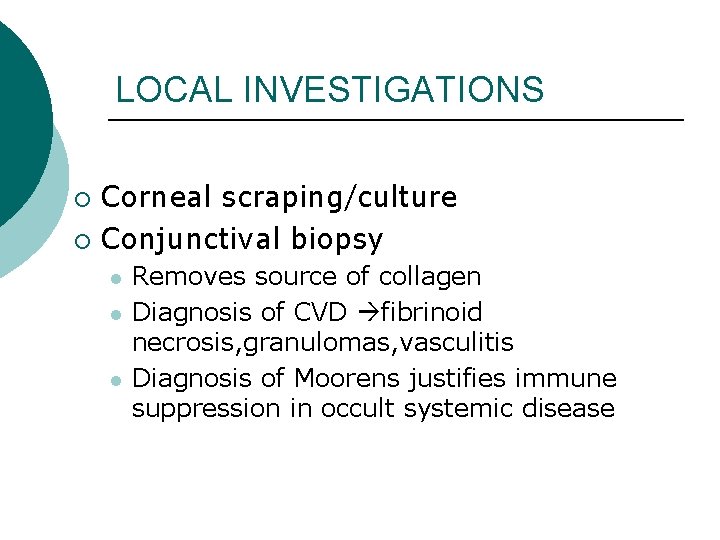
LOCAL INVESTIGATIONS Corneal scraping/culture ¡ Conjunctival biopsy ¡ l l l Removes source of collagen Diagnosis of CVD fibrinoid necrosis, granulomas, vasculitis Diagnosis of Moorens justifies immune suppression in occult systemic disease
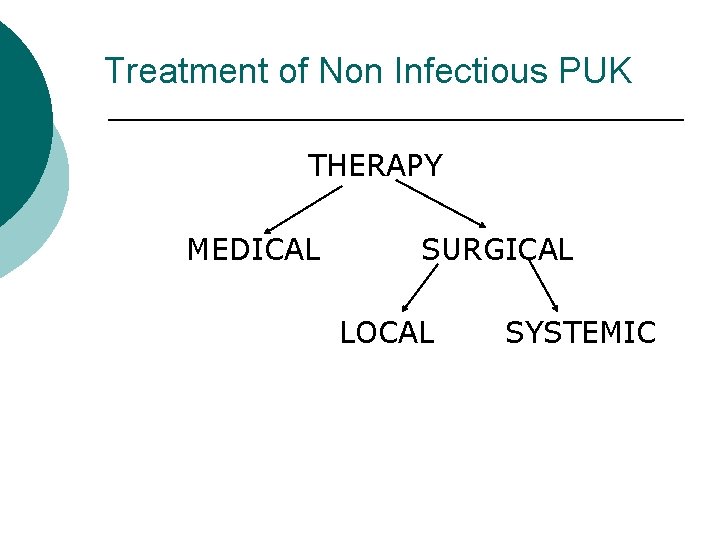
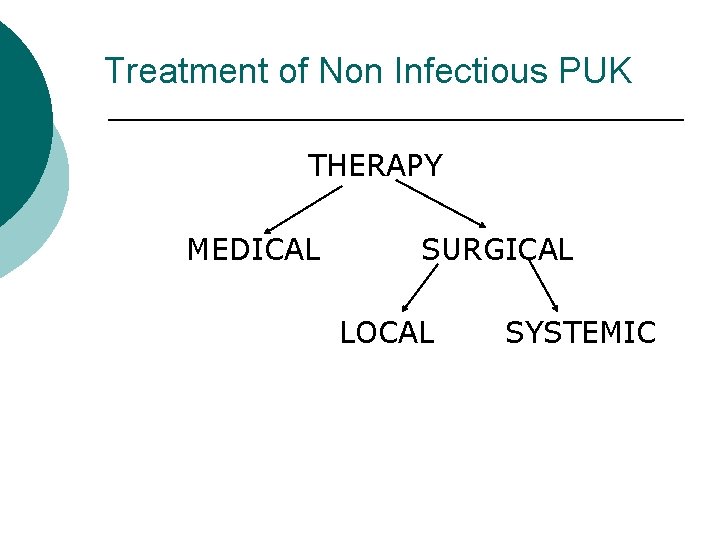
Treatment of Non Infectious PUK THERAPY MEDICAL SURGICAL LOCAL SYSTEMIC
LOCAL THERAPY Goals Promote epithelial healing– stromal thinning ¡ Control of inflammation ¡ Collagenase inhibition– stromal thinning ¡
Promote epithelial healing Lubricating drops, gels ¡ Avoid epitheliotoxic drugs ( aminoglycosides – tobra, genta; fluroquinolones—ciprofloxacin) ¡ No role of topical antibiotics / antifungals unless secondary infection •
Control of inflammation ¡ ¡ ¡ ¡ No role of topical steroids/ NSAIDS ( inhibits collagen synthesis—increases melt) Use topical 1% medroxy progesterone (good anti inflammatory, no collagen synthesis inhibition) Can use topical cyclosporine 0. 5 - 1% ( local T cell immune modulation) Low dose topical steroids Lid hygeine only in marginal infiltrates with blepharitis ( staph antigen)
Other local medical treatment ¡ Blepharitis: lid hygeine ¡ Rosaecae: erythromycin ointment; metronidazole
SYSTEMIC THERAPY Systemic collagenase inhibitors ¡ Tetracycline 250 mg QID ¡ Doxycycline 100 mg OD ¡ Systemic steroids + cytotoxic immunosuppressives
INDICATIONS FOR IMMUNE SUPPRESSION PUK associated with proven CVD like RA, PAN, RP, WG, PSS, GCA, Churgstrauss angitis ¡ If PUK associated with necrotising scleritis ¡ If PUK unresponsive to aggressive conventional medical or surgical therapy ¡
DRUGS USED High dose oral prednisolone 1 - 1. 5 mg / kg BW or Pulsed IV methyl prednisolone ( 0. 51 g) started first as cytotoxic immunosuppression takes 4 – 6 weeks for action Drug of choice– oral cyclophosphamide ( 2 mg/ kg / day) adjust to clinical response, adverse effects
DRUGS USED ¡ ¡ ¡ ¡ Methotrexate, azathioprine, cyclosporine. A Methotrexate : DOC in RA ( 7. 5 - 12. 5 mg / wk) Azathioprine: 1. 3 mg/kg/day Cyclosporine-A: 2. 5 -5 mg/kg/day Monitor CBC, LFT, renal function tests Role of immunologist important Good patient education: long term follow up systemic nature of disease
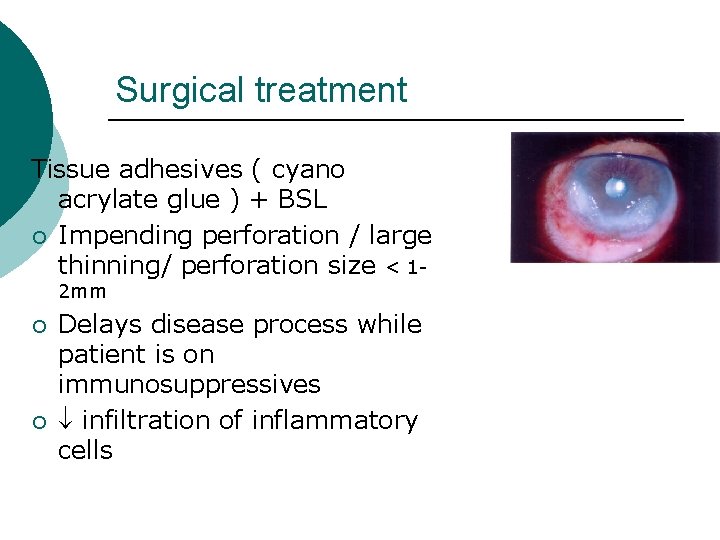
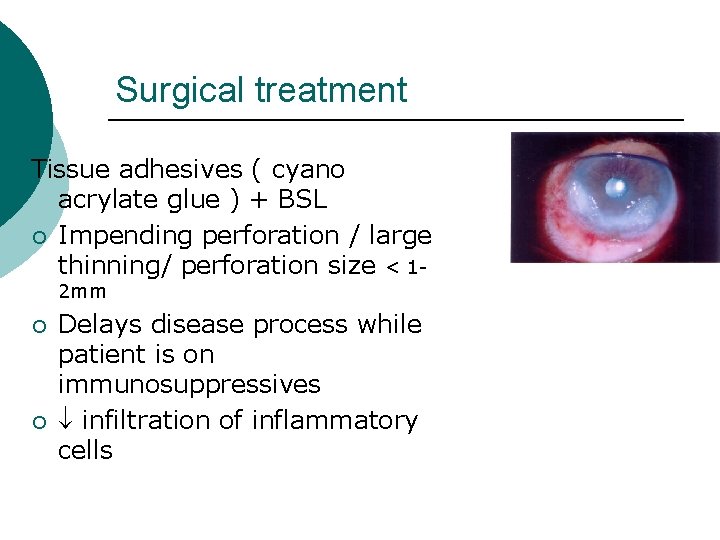
Surgical treatment Tissue adhesives ( cyano acrylate glue ) + BSL ¡ Impending perforation / large thinning/ perforation size < 12 mm ¡ ¡ Delays disease process while patient is on immunosuppressives infiltration of inflammatory cells
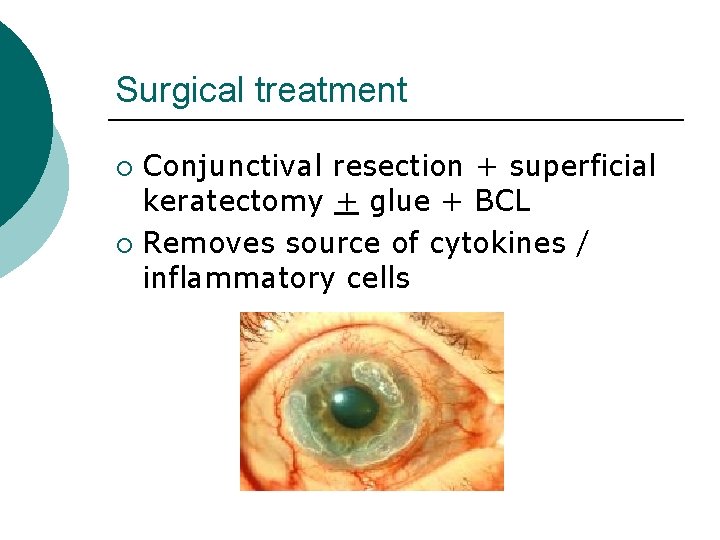
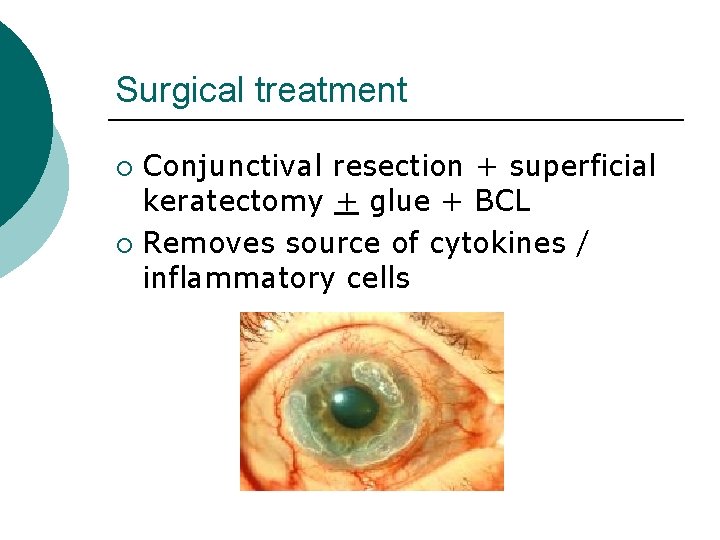
Surgical treatment Conjunctival resection + superficial keratectomy + glue + BCL ¡ Removes source of cytokines / inflammatory cells ¡
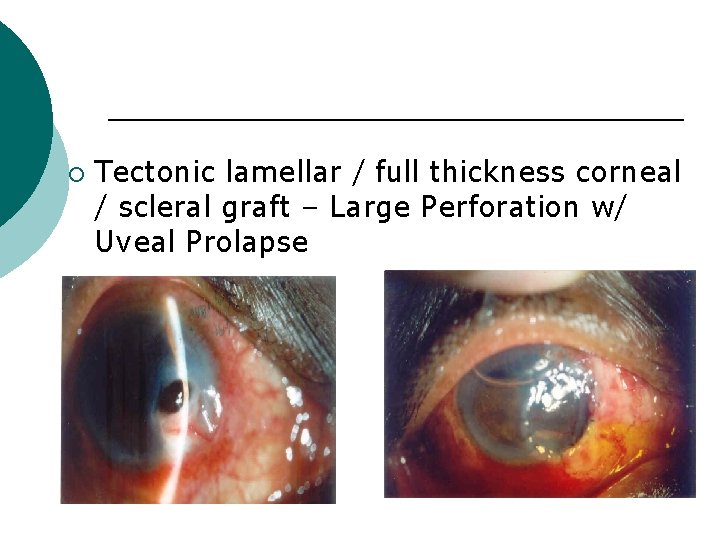
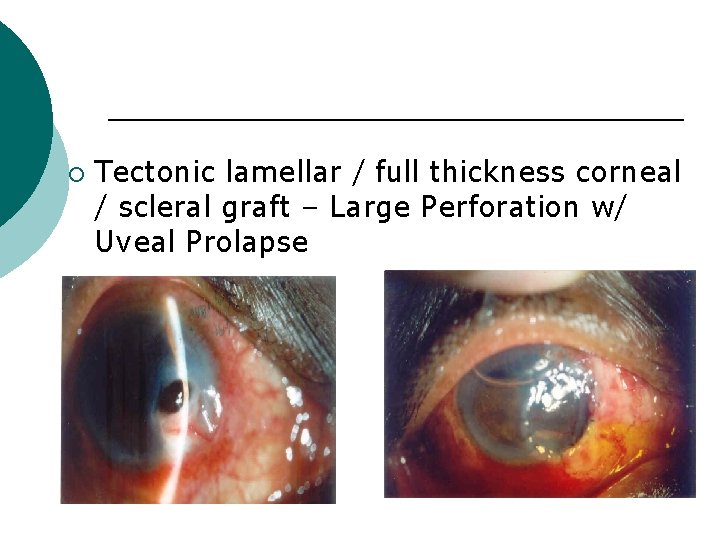
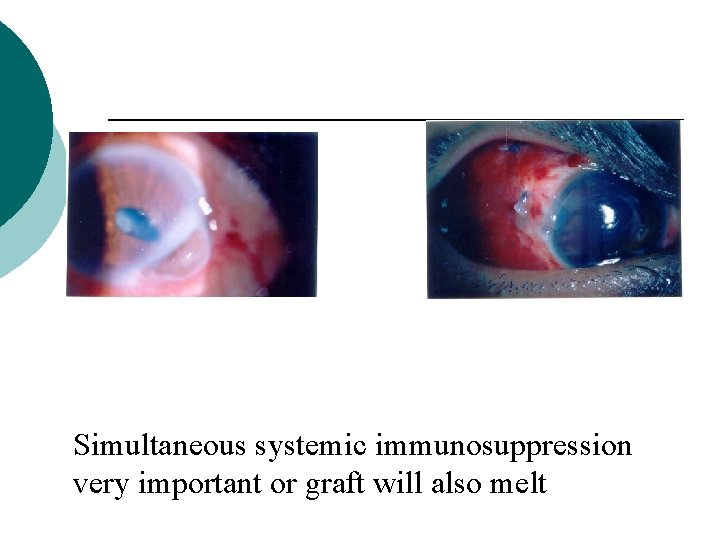
¡ Tectonic lamellar / full thickness corneal / scleral graft – Large Perforation w/ Uveal Prolapse
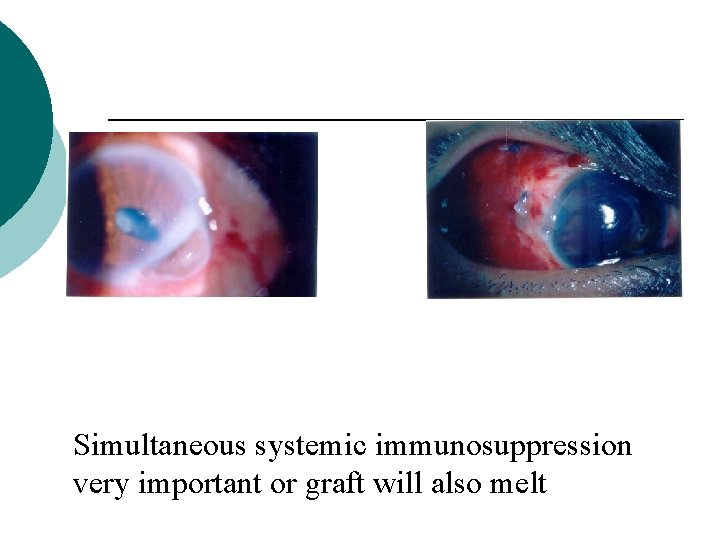
Simultaneous systemic immunosuppression very important or graft will also melt
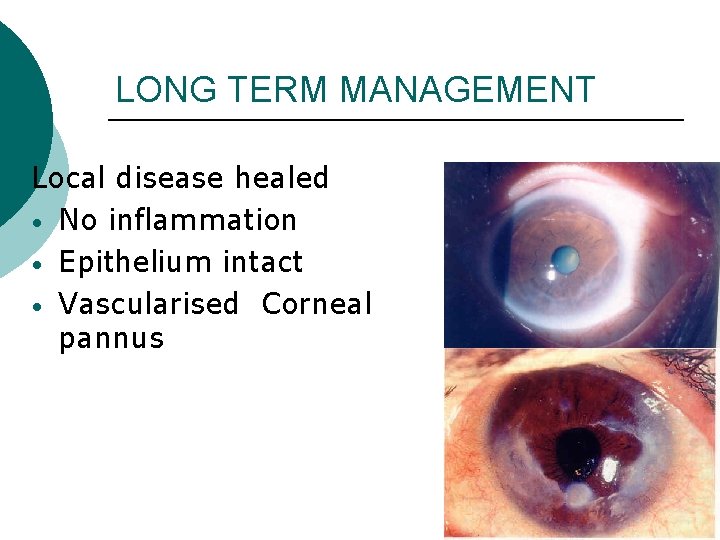
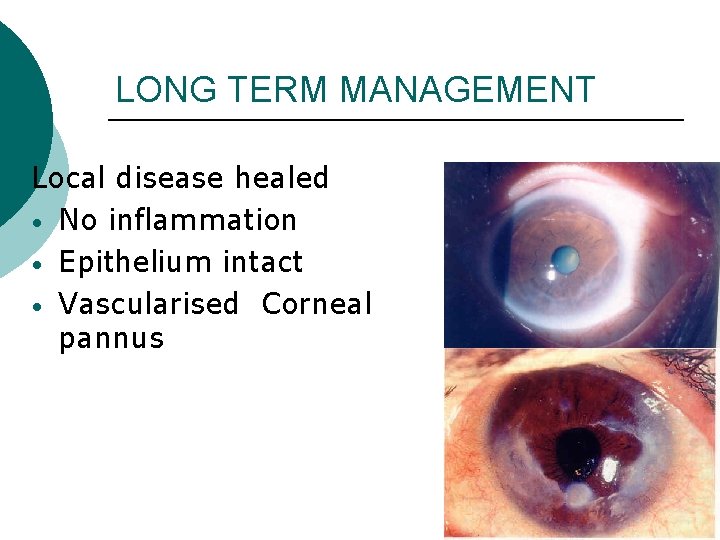
LONG TERM MANAGEMENT Local disease healed • No inflammation • Epithelium intact • Vascularised Corneal pannus
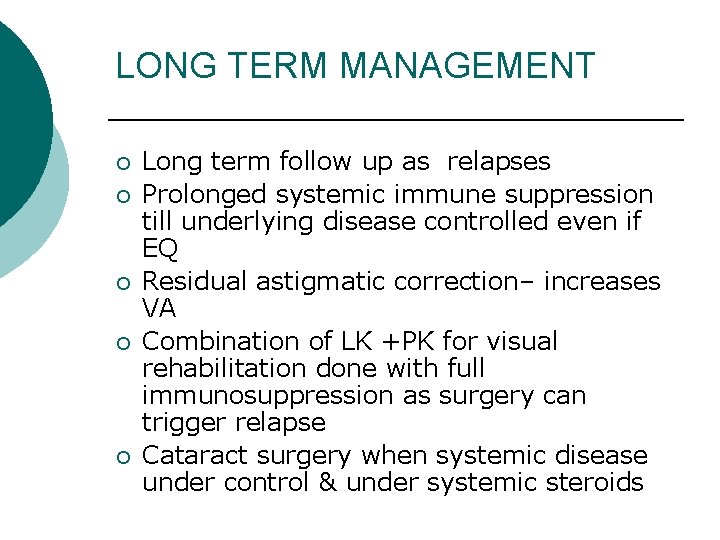
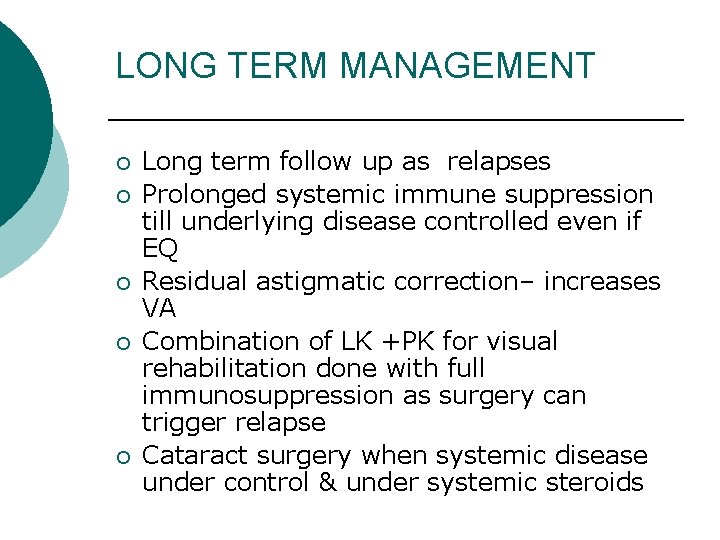
LONG TERM MANAGEMENT ¡ ¡ ¡ Long term follow up as relapses Prolonged systemic immune suppression till underlying disease controlled even if EQ Residual astigmatic correction– increases VA Combination of LK +PK for visual rehabilitation done with full immunosuppression as surgery can trigger relapse Cataract surgery when systemic disease under control & under systemic steroids
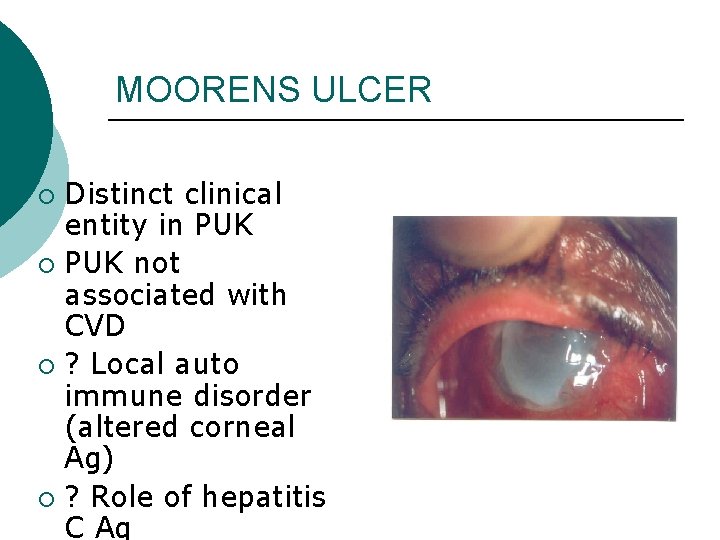
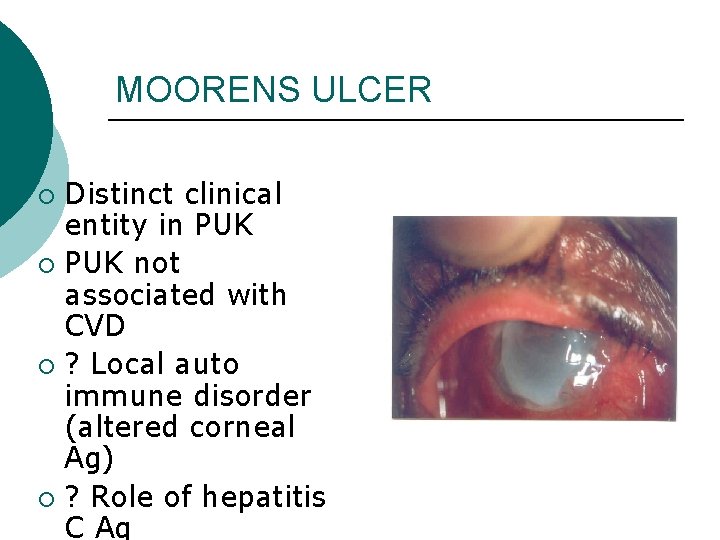
MOORENS ULCER Distinct clinical entity in PUK ¡ PUK not associated with CVD ¡ ? Local auto immune disorder (altered corneal Ag) ¡ ? Role of hepatitis C Ag ¡
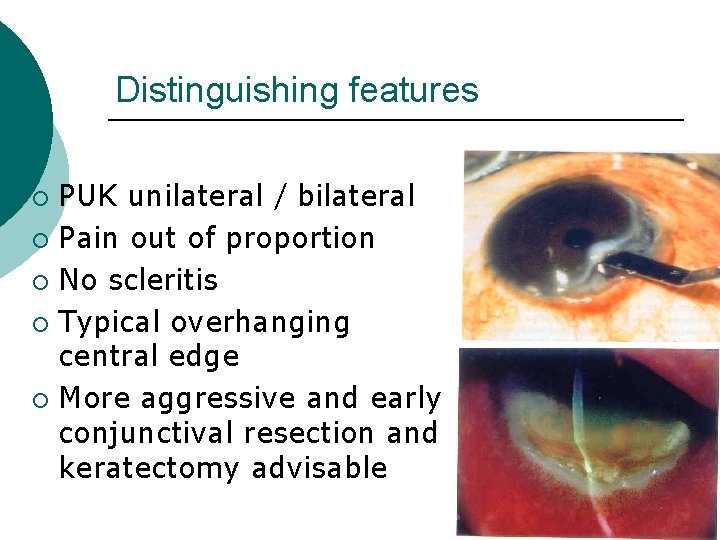
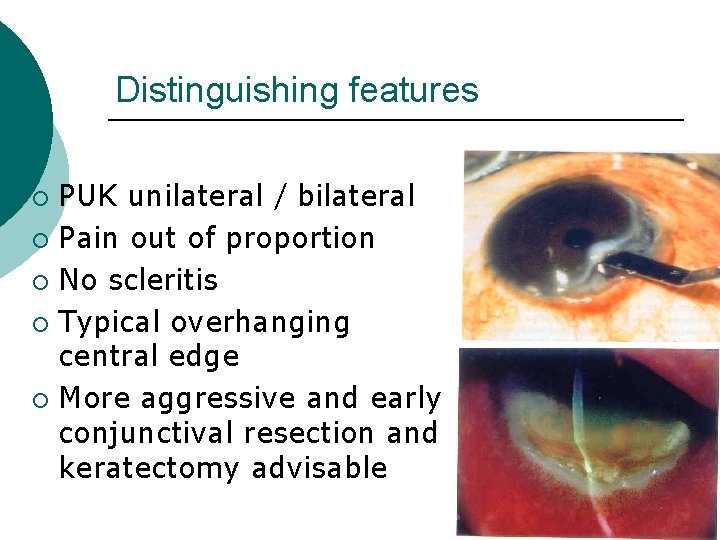
Distinguishing features PUK unilateral / bilateral ¡ Pain out of proportion ¡ No scleritis ¡ Typical overhanging central edge ¡ More aggressive and early conjunctival resection and keratectomy advisable ¡
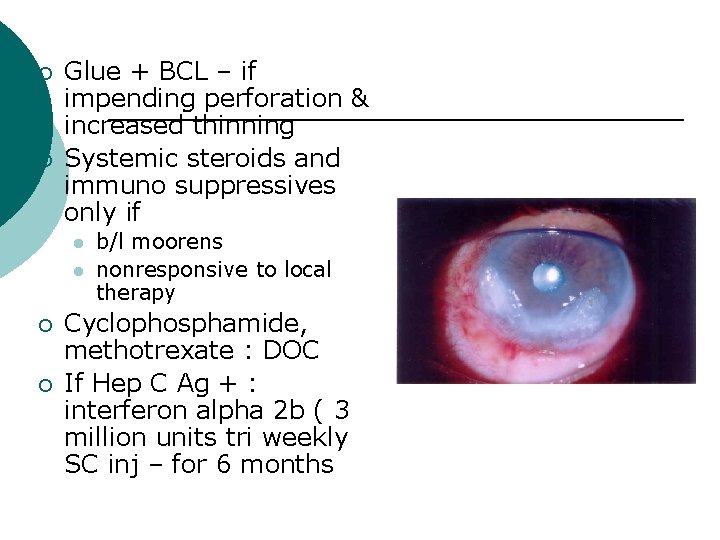
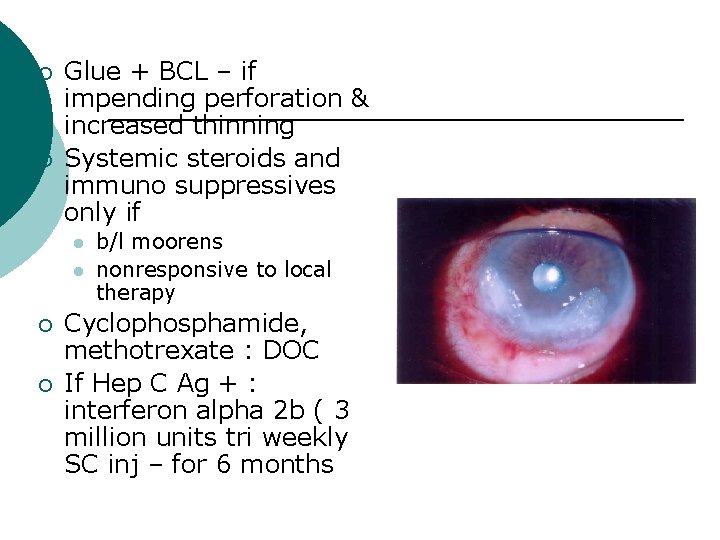
¡ ¡ Glue + BCL – if impending perforation & increased thinning Systemic steroids and immuno suppressives only if l l ¡ ¡ b/l moorens nonresponsive to local therapy Cyclophosphamide, methotrexate : DOC If Hep C Ag + : interferon alpha 2 b ( 3 million units tri weekly SC inj – for 6 months
Conclusion. . ¡ Non Infectious PUK is a potentially devastating disorder, can be the initial presentation of a serious collagen vascular disorder. Hence proper diagnosis and aggressive therapy could improve local and systemic morbidity.
THANK YOU!